Abstract
Background:
Preliminary reports suggest that during the COVID-19 pandemic, telecounseling could be an effective model of psychological intervention for the frontline healthcare workers (fHCW) with psychological problems. Literature is sparse in this area, particularly from low- and middle-income countries, including India. We aimed to investigate the feasibility and the effectiveness of telecounseling (vs. general education) on the psychological problems of the fHCW over three time-points (baseline vs. end-of-session and at two and four weeks after the intervention).
Methods:
The study followed a single-blind, active arm versus general education, parallel-group randomized control design, with participant allocation in 1:1. Active healthcare workers (HCWs) with mild- to-severe or clinically concerning scores on any of the sub-scales of Depression, Anxiety and Stress Scale (DASS-21) or Impact of Event Scale-Revised (IES-R; represented by higher scores) were included, while those with known psychiatric illness were excluded. Chi-square and Mann-Whitney U test and linear-mixed effect model (group-, time, and group by time-effect) were used for analysis.
Results:
There were no baseline group differences (telecounseling group, active arm, n = 9; general education group, control arm, n = 10). A significant time-effect (P = 0.044 to <.001) was found on DASS-21 on intention-to-treat analysis. Per-protocol analysis, additionally, found a significant group effect on Impact of Event Scale-Revised (IES-R; P = 0.036). A significant random effect of the participants was also found (P <.001).
Conclusion:
Telecounseling could be a feasible and scalable model of psychological interventions for the fHCW with psychological problems, albeit with some feasibility challenges.
Keywords: Frontline, Healthcare workers, Telecounseling, COVID-19, Randomize-control trial
Key Messages:
COVID-19 pandemic resulted in significant psychological problems such as depression, anxiety, stress, and posttraumatic stress disorder among the frontline healthcare workers.
Telecounseling is an affordable, feasible, and scalable way of providing psychological support to healthcare workers (HCWs) having significant psychological problems.
Policymakers must spread awareness about common psychological problems that HCWs tend to face during the pandemic, and encourage them to seek help when they are of considerable severity.
Hospitals and service providers need to utilize the digital model of mental health service delivery during the COVID-19 period.
COVID-19 pandemic, being an unprecedented situation, resulted in huge mental health challenges not only for the general population, including the COVID-19 positive (COVID-19+) patients, but also for frontline healthcare workers (fHCW).1–3 Literature suggests that during pandemic, including those from the COVID-19, fHCW often experience burnouts, insomnia, anxiety, depression, acute stress reaction, posttraumatic stress disorders (PTSD), etc. 1,4–6 These are mediated by several biopsychosocial risk factors.5–7 The mental health burden on the fHCW is compounded by the difficulty accessing mental health services and perceived stigma in seeking mental health treatment, resulting in a huge treatment gap.5,8,9
The digital platform has been increasingly used as a scalable model for mental health services delivery, particularly for low- and middle-income countries (LAMIC) with a huge mental health treatment gap, including India.10,11 Literature from Asia has substantiated the effectiveness of the digitally (telecounseling, video-conferencing, text messaging, etc.) delivered mental health service, particularly for common mental disorders (CMDs).12 Emerging literature during COVID-19 has also shown the effectiveness of digitally delivered psychological interventions to vulnerable groups such as fHCW, COVID-19+ patients, and individuals with preexisting mental illnesses.13–15 Their utility has also been recognized by various governmental organizations and policymakers, exemplified by the promotion of various online self-help psychological tool kits for the general population and the launching of the telecounseling/telepsychiatry guidelines for mental health professionals (MHP).16,17 However, their usability in the COVID-19 times has been marred by (a) unfamiliarity of both the therapist and the patients with the digital platform, (b) risk of normal psychological responses getting wrongly labeled as pathological, and (c) still-emerging evidence-based treatment approach.14,18,19 Brief-psychoeducation sessions, behavioral interventions such as stress management training, coping skill training, and cognitive behavioral therapy are psychological interventions effective for the CMDs and subsyndromal conditions.12,20–22
Despite the potential utility of telecounseling services as a form of mental health service delivery amidst COVID-19, literature is sparse from the LAMIC, including India, that would establish its feasibility and effectiveness for the fHCW with psychological problems. Therefore, the current study was conducted to assess the feasibility and effectiveness of the telecounseling services for the fHCW with psychological problems amidst COVID-19.
We hypothesized that telecounseling would significantly reduce the psychological problems among the fHCW as compared to general advice. The objective of the current study was to compare the level of improvement in depression, anxiety, stress, and posttraumatic stress (PTS) symptoms among the fHCW receiving the telecounseling services (telecounseling group, TCG vs. general psychoeducation group, GEG) at various time-points (at the end of session (EOS) and two weeks (W2) and four weeks (W4) after the intervention).
Material and Methods
Trial Design and Setting
This present study was part of a larger study (an online survey) conducted to assess the magnitude and determinants of the psychological problems among the HCW (doctors, nursing officers, laboratory technicians, and allied staff such as dieticians, security personnel, and housekeeping staff). The parent study was conducted from April 2020 to June 2020, when the pandemic was still evolving, and there was limited knowledge and resources to handle the ongoing pandemic. Moreover, the government had imposed the nation-wide lockdown and social-distancing norms that posed considerable difficulties in managing the daily affairs, including accessing the mental health services, both for the general population and HCW.
The current setting is a 500-bedded, government-sponsored, tertiary-care multispecialty hospital. During the pandemic, 350 beds were earmarked for providing care to COVID-19+ patients. The COVID-19 services include observation wards, general wards, and intensive-care unit (ICU). The hospital is one of the largest tertiary-care referral center of the central India. In our setting, the fHCW (clinicians, nurses, supporting staff) were posted in the COVID-19 units on a rotational basis (ten days posting each in COVID-19 units, self-quarantine, and nonCOVID-19 duties). Those fHCWs who were found to have a considerable psychological problem (based on the online survey) were approached for the interventional study.
The study was a single-blind, active arm versus general education, parallel-group (general education vs. telecounseling) randomized control trial (RCT) with participants allocation in 1:1.
Participant Recruitment
Inclusion criteria for the study were: HCWs (doctors and nursing staff, but not other fHCWs described above, as the telecounseling services were focused on the HCWs directly involved in patient care, and supposedly, telecounseling delivery could be feasible in these professionals only) working actively in hospital irrespective of their work-setting (working in COVID-19 or nonCOVID-19 area) or currently in the quarantine; having depression, anxiety, and stress scale-21 (DASS21) sub-scale score in mild-severe range (depression, 10–27; anxiety 8–19; and stress 15–33) or impact of event scale-revised (IES-R) score in the range of COVID-related stress symptoms/probable PTSD (score: 24–38; discussed below); and willing to provide informed consent. However, those having scores beyond the target range on DASS21 or IES-R (normal or very severe/clinically dysfunctional range) and those previously diagnosed with psychiatric disorders were excluded from the study.
Randomization and Allocation Concealment
The fHCWs (described above) were contacted by the investigators (Snehil Gupta and Abhijit R. Rozatkar), informing them about their current level of psychological problems and inviting them for the study. They were informed that two modules are being assessed as the psychological interventions to allay their psychological problems, which comprise general advice, COVID-19-related facts, counseling, and some of the behavioral practices. However, it was not revealed to them which module is the active intervention under study and which arm is serving as control, thus utilizing the dual blind technique for participants blinding.23 The potential participants were also informed about the option to physically consult an MHP before the commencement of or during the sessions if they or their therapist felt so; in such cases, they were excluded from the study. Upon obtaining their consent, they were randomly assigned (by Snehil Gupta) into one of the two arms (TCG, intervention-arm; GPG, control arm) based on a computer-generated random number sequence.24 However, no measures were undertaken for allocation concealment. The tele-sessions were provided during July 2020 to September 2020.
The timings of the tele-sessions were mutually decided by the participant and the therapist, keeping in mind the hectic work schedule of both the parties. It was delivered in three sessions, each of duration 30±5minutes (depending upon the participants’ level of comprehension and the progress of the therapy), spanning over 7 days to 10 days (Table S1).
Interventions
The active-intervention arm (TCG) received brief eclectic psychotherapy. The therapy module was designed based on the extant literature and the personal experiences of the investigators as a part of the institutes’ COVID-19-support team (Mohit Kumar and Abhijit R. Rozatkar).25 The active intervention involved three sessions of eclectic counseling that involved expressing empathy, emphasizing the strengths among the clients, psychoeducation about myths and facts about the psychological problems and COVID-19, relaxation training, motivational interviewing, life skill training, and problem-solving training (sessions details provided in Table S1).
The control-arm received information on COVID-19 prevention, standard treatment guidelines, common psychological problems that fHCW experience during COVID times, dietary measures, positive role of social interactions, involvement in recreational activities, and a potential source of self-help tools (Table 1).
Table 1.
Baseline Characteristics of the Participants (n = 19)
| Characteristics | Control Arm (n = 10) | Intervention Arm (n = 9) | Statistical Values |
|
Age group (n [%]) 18–30 years >30 years |
8 (80) 2 (20) |
8 (88.1) 1(12.5) |
P = 0.59 |
|
Sex (n [%]) Male Female |
3 (30) 7 (70) |
4 (44.4) 5 (55.6) |
P = 0.51 |
|
Marital status (n
[%]) Married Unmarried |
3 (30) 7 (70) |
3 (22.2) 7 (77.8) |
P = 0.70 |
|
Designation (n [%]) Nursing officer* Interns/postgraduate trainee# Senior resident@ |
4 (40) 5 (50) 1 (10) |
1 (11.1) 8 (88.8) 0 (0.00) |
P = 0.41 |
|
Level of involvement in clinical care (n
[%]) Working in nonCOVID area and not involved in patient care Working in nonCOVID Area, but involved inpatient care (e.g. lab. workers) Active involvement in treatment or screening |
5 (50.0) 1 (10.0) 4 (40.0) |
4 (44.4) 0 (0.0) 5 (55.6) |
P = 0.44 |
|
Do you stay with your family? (n
[%]) Yes No |
8 (80.0) 2 (20.0) |
7 (77.8) 2 (22.2) |
P = 0.90 |
| Professional experience, y (SD) | 1.40 (2.06) | 1.89 (0.9) | P = 0.42 |
| Days since last clinical duty, d (SD) | 45.90 (47.1) | 45.11 (42.9) | P = 0.47 |
| Depression score (DASS21) (mean [SD]) | 11.80 (4.15) | 8.0 (4.2) | P = 0.065 |
| Anxiety score (DASS21) (mean [SD]) | 7.40 (4.32) | 7.11 (4.8) | P = 0.89 |
| Stress score (DASS21) (mean [SD]) | 12.20 (6.14) | 11.0 (10.3) | P = 0.32 |
| Posttraumatic scale score (IES-R) (mean [SD]) | 18.20 (10.25) | 11.0 (10.25) | P = 0.14 |
* Having bachelor or master’s degree in nursing, # passed final professional MBBS exam and pursuing internship, PG trainees are pursuing postgraduate medical course after finishing their MBBS,@senior residents have finished their PG -medical course and currently employed in three-year teaching/research program
In both the groups, telecounseling sessions were conducted through telephonic audio conversation. However, links related to some of the behavioral practices such as Jacobsons’ progressive muscle relaxation technique, facts about COVID-19, etc. were also shared over whatsapp or email.
Outcome Measures
The level of depression, anxiety, and stress were measured by DASS-21. It is a set of three self-report scales; each of the three sub-scales contains seven items, with item scores ranging from 0 to 3 (0: does do not apply to me at all, 3: apply to me very much/most of the time). The score for each item is multiplied by two to get the final score (maximum sub-scale score: 42). The sub-scale scores are categorized into mild, moderate, severe, and very severe. The tool has got a good psychometric property. 26
IES-R was used to assess the symptoms of stress related to COVID-19 in fHCW. It is a short and self-administered questionnaire having 22 items and enquires about the recent events. It also has Likert-scoring: 0 = Not at all; 1 = A little bit; 2 = Moderately; 3 = Quite a bit; 4 = Extremely. While there is no specific cut-off score, scores higher than 24 are of concern (24–32: COVID-related (posttraumatic) stress symptoms present, 33–38: probable diagnosis of COVID-related PTSD, and >39: Dysfunction).27
The outcomes of the study were the change, from the baseline, in the mean score of the participants (TCG vs. GPG) on DASS21 and IES-R at the EOS, W2, and W4.
Sample Size
The initial sample size was calculated by considering the small to medium effect size of the telecounseling (vs. control intervention).28 Keeping the power of 80% and an α-error of 5%, the total sample size of 58 (n = 29 in each arm) was found to be adequate.29 However, with the progress of the trial, the sample size had to be reduced based on low take-up by the participants and considerable attrition rate (elaborated in result section).
Data Analysis
The baseline characteristics (socio-demographics, professional details, scores on DASS21 and IES-R, etc.) of the participants were represented by descriptive statistics. The normality of the data was explored through the Shapiro-Wilk test. The baseline differences between the two arms were compared by the chi-square test and Mann-Whitney U test. Linear mixed effect model (LMEM) was used to assess the effect of the intervention (group effect, TCG vs. GEG), time effect (at EOS, W2, and W4), and group*time effect. Both fixed effect and random effect (random intercept and residual effect) were calculated and were represented as mean difference (t, 95% confidence interval [95% CI]) and variance (σ², standard error [SE]), respectively. The best model fit for the analysis (including the random effect of the time gap between the initial assessment and delivery of the telecounseling sessions, current work-area, etc.) was determined by Schwarz’s Bayesian Criterion (BIC), with a smaller value representing the better model.30 GEG group (control arm) and baseline scores formed the reference categories for the analysis. Both intention-to-treat (ITT) analysis and per-protocol analysis (PPA) were performed. Missing value imputation in ITT was carried out as per the principle of the last observation carried forward. The data was analyzed using the licensed Statistical Package for the Social Sciences Version 21 (SPSS).31
The investigation was carried out following the latest version of the declaration of Helsinki. The study design was approved by the institute human ethics committee, and the trial was registered under the clinical trial registry of India (CTRI/2020/06/025917). Those scoring above the cut-off score were informed about their psychological status and were requested to consult an MHP for further assessment and management.
Results
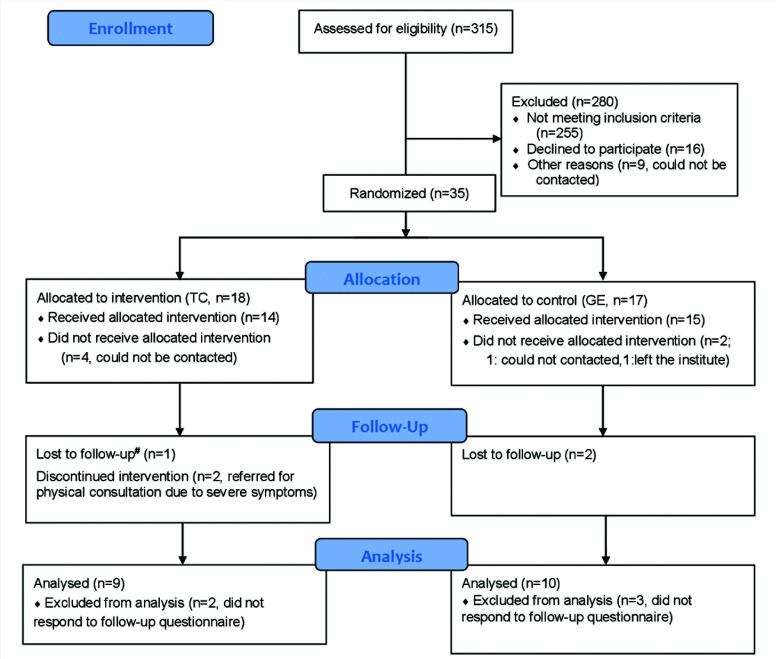
A total of 59 potential participants were approached for the intervention. However, a sizeable proportion of the potential participants (n = 16, 27.1%) refused to participate in the study. Further, another 13.5% (n = 8) of the potential participants could not be contacted (probable reasons discussed in the discussion section). Finally, 35 participants were randomized into the two arms. The flow of the participants has been depicted in Figure 1.
Figure 1. CONSORT Flow Diagram depicting the procedure of participants recruitment.
CONSORT: CONsolidated Standards of Reporting Trials, TC: tele-counseking, GE: General education, #follow-up at end-of-session, 2 and 4 weeks after the intervention
Participant Characteristics
The majority of the participants in both the arms were of age <30 years, unmarried, and staying with their families, with a slight preponderance of females and postgraduate trainees. No significant baseline differences were found between the two groups (Table 1). None of the participants reported any adverse effects with the assigned intervention. However, the intervention had to be stopped in two of the participants of TCG because of the worsening of the symptoms.
Effectiveness of the Intervention vs. General Education:
On ITT analysis, we did not find any significant difference between the two groups (no group effect) or group-by-time interaction (group*time effect) regarding the change in the mean scores on DASS21 or IES-R (t = -1.65 to 0.31; P = 0.75 to 0.11). On the contrary, a significant improvement in symptoms over time was observed (time-effect) on the measures on depression (P = 0.019 to <.001), anxiety (P = 0.044 to <.001), and stress (P = 0.007 to <.001), but not on PTS symptoms. Furthermore, the LME model revealed a significant random effect on all outcome variables, both in terms of random intercept (P = 0.027 to <.001) and the residual effect (P<.001; Table 2).
Table 2.
Effect of Telecounseling (vs. General Education) on the Psychological Parameters of the Participants (ITT Analysis)
| Within-Subject Diff. (Time-Effect): t (Mean Diff.) (95%CI) | P-Value | Between Subject Diff. (Group Effect): t (Mean Diff.) (95%CI) | P-value | Group*Time Interaction: t (Mean Diff.) (95%CI) | P-Value | |
|
Depression scores
2 Fixed effect Baseline (ref.) EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –2.53 (–7.3, –0.7) –1.95 (–8.2, 0.19) –5.33 (–10.8, –4.7) |
0.019* 0.061 <0.001* |
– –1.65 (–6.9, 0.8) |
0.11 | – –0.53 (–6.1, 3.6) –0.81 (–8.7, 3.8), 0.82 (–8.7, 3.8) σ² = 13.3 (5.7) σ² = 14.9 (2.8) |
0.60 0.42 0.42 0.020 <0.001* |
|
Anxiety score Fixed effect Baseline (ref.) EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –2.711 (–6.4, –0.81) –2.167 (–6.7, –0.10) –4.077 (–8.5, –2.7) |
0.001*
0.044* 0.014* |
– 0.31 (–3.4, 4–6) |
0.75 | – –0.82 (–5.8, 2.5) –1.21 (–7.8, 2.1) –0.92 (–6.2, 2.4) σ² = 7.11(3.2) σ² = 9.77(1.8) |
0.42 0.24 0.37 0.027* <0.001* |
|
Stress score Fixed effect Baseline (ref.) EOS |
– –3.05 (–8.4, –1.6) |
0.007* | – –0.91 (–7.4, 2.9) |
0.37 | ||
| W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
–3.25 (–8.3, – 1.7) –4.85 (–10.3, –4.0) |
0.006*
<0.001* |
–0.70 | 0.49 | –1.30 (–7.9, 1.9) –1.03 (–7.0, 2.4) σ² = 17.34(6.63) σ² = 10.05(1.93) |
0.21 0.31 0.009* <0.001* |
|
IES-R score Fixed effect Baseline EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –2.88 (–26.7, –9.8) –3.48 (–23.7, 1.5) –4.54 (–3.6*10–4, 3.6*10+4) |
0.14 0.06 0.67 |
–1.453 | 0.17 | – 0.65 (–24.5, 30.3) 0.36 –17.2, 20.6) 0.88 (–5..5*10–4, 5.5*10+4) σ² = 35.36 σ² = 34.93 |
0.60 0.76 0.61 0.017* <0.001* |
Baseline scores, control arm, and baseline*control arm are the reference category; SE: standard error; EOS: at end of sessions, W2: at two weeks, W4: at four weeks
The findings on the PPA (per protocol analysis) were similar to that of ITT. Additionally, PPA showed a significant group difference in PTS scores (group effect; greater improvement in TCG vs. GEG; P = 0.036; Table 3).
Table 3.
Effect of Telecounseling (vs. General Education) on the Psychological Parameters of the Participants (Per Protocol)
| Within-Subject Diff. (Time-Effect): t (Mean Diff.) (95%CI) | P-Value | Between Subject Diff. (Group Effect): t (Mean Diff.) (95%CI) | P-Value | Group*Time Interaction: t (Mean Diff.) (95%CI) | P-Value | |
|
Depression scores
2 Fixed effect Baseline (ref.) EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –2.04 (–8.7, –0.03) –2.12 (–8.8, –0.2) –4.14 (–16.2, –5.6) |
0.048* 0.040* <0.001* |
– –1.56 (8.4, 15.2) |
0.126 | – –0.62 (–8.3, 4.4) –0.42 (–8.3, 5.5) –1.48 (–1.9, 12.2) σ² = 10.09 σ² = 17.99 |
0.54 0.68 0.15 0.08 <0.001* |
|
Anxiety score Fixed effect Baseline EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –2.77 (–8.0, –1.2) –1.61 (–6.1, –0.6) –3.50 (–11.5, –3.2) |
0.009* 0.115 0.001* |
– –0.163 (–3.8, 2.9) |
0.872 | – –0.87 (–7.1, 2.8) –1.39 (–9.1, 1.7) 0.19 (–4.9, 5.9) σ² = 3.79 σ² = 11.7 |
0.39 0.17 0.84 0.177 <0.001* |
|
Stress score Fixed effect Baseline EOS W2 W4 Random effect Intercept (variance [σ²]) (SE) Residual effect |
– –4.04 (–9.5, –3.1) –3.08 (–8.0, –1.6) –5.24 (–14.1, –6.3) |
<0.001* 0.004* <0.001* |
– –1.21 (–7.1, 1.8) |
0.23 | – –1.14 (–7.3, 2.0) –0.79 (–7.1, 3.1) 0.50 (–3.8, 6.4) σ² = 13.04 σ² = 09.49 |
0.25 0.43 0.025 <0.001* |
|
IES-R score Fixed effect Baseline EOS W2 W4 Random effect Intercept Residual effect |
– –3.89 (–17.5, –5.5) –4.71 (–19.9, –7.9) –4.36 (–23.4, –8.5) |
<0.001* <0.001* <0.001* |
– –2.16 (–13.9, –0.4) |
0.036* | – 0.68 (–5.8, 11.7) 0.79 (–5.8, 13.3) 1.09 (–4.4, 14.7) σ² = 18.22 σ² = 34.25 |
0.28 0.43 0.29 0.119 <0.001* |
1 reference is the control group. 2 DASS21, 2 random effect of the subjects (participants)
- Baseline is the reference category, - control group is the reference category, -c control group*baseline interaction is the reference category, SE: Standard error
Discussion
The current RCT aimed to assess the feasibility and effectiveness of telecounseling vis-à-vis general psychoeducation on the psychological problems of the fHCW. We found a significant improvement in their level of depression, anxiety, and stress over time on ITT analysis and PPA. On PPA, additionally, we found a significant improvement in PTS symptoms in TCG vs. GEG. However, the telecounseling sessions were marred by a considerable refusal rate and attrition of the participants, reflecting low uptake of telecounseling in the current setting. The study findings add to the limited literature on the feasibility and effectiveness of the telephone-based psychological intervention for the fHCW amidst the pandemic. These findings become particularly important when the pandemic has adversely affected the availability and accessibility of mental health services, especially in LAMIC, and when telecounseling seems to be a scalable model of service delivery.12,18,32 These findings could stimulate future research on this area, especially in developing psychological interventions based on the local needs.
It may be argued that we included participants with a wide range of severity (mild to severe) of psychological problems. The inclusion of those with severe spectrum of psychological problems was to account for the potential overestimation of the problems on the online mode of the survey, and the time-frame of last one week only that is liable to get affected by the dynamic socio-environmental stressors.33–35 Moreover, having the provision of physical consultations with an MHP, if deemed necessary, provided us some leverage to include the severe spectrum of participants. Indeed, we excluded participants with a very severe level of psychological distress/dysfunction as assessed on the outcome measures, as they would need an extensive psychiatric assessment and treatment.
The present study faced certain feasibility challenges. The intervention was marred by a higher refusal rate (for participation) and a high attrition rate. This could be attributed to (a) time-constraint on the part of the participants because of their heavy duty schedules, (b) the stigma associated with the mental disorders, (c) spontaneous improvement in their psychological problems with time, and (d) a change in the work environment, and (e) a tendency towards self-help and lack of perceived need of professional interventions.1,14 These findings highlight the potential logistic problems MHP may face while delivering telecounseling services in a country like India where the stigma with mental illnesses is still higher.36 Furthermore, it underscores the need to increase awareness among the fHCW about work-related mental health problems and the need to avail mental health services, thereby reducing stigma.
In telecounseling, we utilized an eclectic approach to psychotherapy. The emerging literature on COVID-19 has suggested the effectiveness of such approaches for CMDs.37 Furthermore, to maintain the equipoise (not providing any kind of psychological support to the participants of the control arm would be unethical), the control group was provided with general counseling and advice, a strategy frequently used in yoga-based interventions for CMDs. Moreover, this also ensured participants’ blinding and prevented the bias that arises because of demand characteristics.23,38
We found a significant time-effect in reducing the depression, anxiety, and stress of the participants. This time-dependent improvement could be attributed to the acquisition of knowledge about COVID-19 and better coping skills and better environmental factors within the hospital (evidence-based guidelines for infection control and treatment, duty-offs, duty in the nonCOVID-19 area) and outside (relaxation in the lockdown, decrease in perceived-stigma, etc.).13,39,40 Importantly, since both the groups were receiving some forms of psychological support from their therapists, including the opportunity for emotional ventilation, it might itself have some therapeutic effect. Literature suggests that even brief-supportive psychotherapy during the pandemic has a beneficial effect on the patients or HCWs in quarantine or isolation.1,14,41,42
No group effect was found on the outcome measures, as revealed by the ITT analysis. Again, this could be attributed to the therapy and environment-related factors as discussed above; moreover, because of the small sample size, the study might have been underpowered to capture any small yet significant difference between the groups.
PPA also revealed a significant group effect for the PTS symptoms, with TCG faring better than GEG. Literature suggests that cognitive and behavioral interventions have positive effects in managing the intrusiveness and avoidance of COVID-19-related traumatic memories such as the serious medical conditions or death of the patients and their acquaintances.15,42–44 In the present study, an eclectic approach of counselling involving both the cognitive (psychoeducation, life-skill training, and problem-solving) and behavioral interventions (relaxation technique, activity-scheduling, and sharing of their feelings with their colleague/family members) might have resulted greater positive effect in the intervention arm (vs. GEG), although limited sample size precludes us in drawing any firm conclusion on this.
Lastly, we did not find any group by time effect between the two arms. This finding is in contrast to previous literature on pandemics, including COVID-19, that reported that over time, the fHCW who received telephone-based psychological intervention fared better than the General Education (GE) group.13,41 Again, this negative finding could be attributed to the limited sample size, higher rate of nonparticipation, and high attrition rate. This warrants more research on this area, especially involving a higher sample size and robust methodologies, particularly in addressing the issues of nonparticipation, and reducing the selection bias and attrition rate.
Despite many strengths, this study has certain limitations. First and foremost is the low participation rate. There is a possibility that individuals with particular characteristics and disposition agreed to take part in the study; therefore, a possibility of selection bias could not be ruled out. Secondly, because of only a modest acceptance rate for the intervention and a high attrition rate, the sample size was only modest (lower than what was initially proposed); thus, the study was underpowered. Thirdly, because of logistic issues, allocation concealment and investigators’ blinding during data analysis could not be ensured. Fourthly, the psychological module was not validated in the study population; thus, its clinical utility might be questioned. Fourthly, the assessor was not blind to the overall scoring and analysis of data. Lastly, the study was conducted in a tertiary care institute; thus, the findings may not be generalized to other settings.
Conclusion
Digital methods such as telephone-based psychological interventions could be a feasible and effective way of mental health service delivery to the fHCW with common psychological problems amidst the COVID-19 pandemic, albeit with some roadblocks. A brief counseling or general psychoeducation can also positively affect the depression, anxiety, and stress of the HCWs, particularly in a resource-constrained set-up. However, such interventions, particularly in the Indian setting, where mental health stigma is higher and there are time-constraints to avail such services, also face many logistic challenges. Hospital authorities must endeavor to address mental health issues of the fHCW amidst health emergencies, including COVID-19, by spreading awareness about the mental health issues, providing mental health support to those in need, and encouraging the HCW to avail such services. More research is required in this area, especially by involving different populations and different technologies, to bridge the mental health treatment gap.
Supplemental Material
Supplemental material for this article is available online.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 2020; 7: e15–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus disease 2019 (COVID-19) situation report -70.pdf. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200330-sitrep-70-covid-19.pdf?sfvrsn=7e0fe3f8_2 (accessed April20, 2020)
- 3.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatry, 2020; 52: 102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta S and Sahoo S. Pandemic and mental health of the front-line healthcare workers: A review and implications in the Indian context amidst COVID-19. Gen Psychiatry, 2020; 33: e100284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: Lessons learned. Philos Trans R Soc Lond B Biol Sci, 2004; 359 1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 2020; 7 228–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai J, Ma S, Wang Y, et al. Factors associated with mental health Outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open, 2020. March 23; 3. DOI: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson E, Hershenfield K, Grace SL, et al. The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. Can J Psychiatry Rev Can Psychiatr, 2004; 49 403–407. [DOI] [PubMed] [Google Scholar]
- 9.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis, 2020; 20: 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization Mental health action plan 2013−2020. World Health Organization, 2013. https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf;jsessionid=25351DBFB34A754D264EA8E8DEC485E4?sequence=1 (accessed September21, 2020). [Google Scholar]
- 11.Patel V, Saxena S, Lund C, et al. The lancet commission on global mental health and sustainable development. Lancet Lond Engl, 2018; 392 1553–1598. [DOI] [PubMed] [Google Scholar]
- 12.Li H, Lewis C, Chi H, et al. Mobile health applications for mental illnesses: An Asian context. Asian J Psychiatry, 2020; 54: 102209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng W, Zhang F, Liu Z, et al. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen Psychiatry, 2020; 33: e100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inchausti F, MacBeth A, Hasson-Ohayon I, et al. Psychological intervention and COVID-19: What we know so far and what we can do. J Contemp Psychother, 2020; 27 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu X, Hu M, Song Y, et al. Effect of positive psychological intervention on posttraumatic growth among primary healthcare workers in China: A preliminary prospective study. Sci Rep, 2016; 6 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Math SB, Manjunatha N, Kumar N, et al. Guidelines for Tele-Psychotherapy Services, 2020. https://nimhans.ac.in/wp-content/uploads/2020/04/Guidelines-for-Telepsychotherapy-Services-17.4.2020.pdf
- 17.COVID-19 Korean medicine clinical guidance (2nd edition), 2020. https://www.kmcric.com/news/newspaper/view/41842.
- 18.Jung SJ and Jun JY. Mental health and psychological intervention amid COVID-19 outbreak: Perspectives from South Korea. Yonsei Med J, 2020; 61 271–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serrano-Ripoll MJ, Ricci-Cabello I, Jiménez R, et al. Effect of a mobile-based intervention on mental health in frontline healthcare workers against COVID-19: Protocol for a randomized controlled trial. J Adv Nurs, 2021; 77 2898–2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Langarizadeh M, Tabatabaei MS, Tavakol K, et al. Telemental health care, an effective alternative to conventional mental care: A systematic review. Acta Inform Medica, 2017; 25 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leach LS and Christensen H. A systematic review of telephone-based interventions for mental disorders. J Telemed Telecare, 2006; 12 122–129. [DOI] [PubMed] [Google Scholar]
- 22.Naslund JA, Aschbrenner KA, Araya R, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. Lancet Psychiatry, 2017; 4 486–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maccoon DG, Imel ZE, Rosenkranz MA, et al. The validation of an active control intervention for mindfulness based stress reduction (MBSR). Behav Res Ther, 2012; 50 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haahr M. RANDOM.ORG: True random number service. https://www.random.org (accessed November29, 2020).
- 25.Rozatkar A. Patient support services for COVID-19 patients. Indian J Soc Psychiatry, 2020; 36 9–10. [Google Scholar]
- 26.Osman A, Wong JL, Bagge CL, et al. The depression anxiety stress scales—21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J Clin Psychol, 2012; 68 1322–1338. [DOI] [PubMed] [Google Scholar]
- 27.Beck JG, Grant DM, Read JP, et al. The impact of event scale –revised: Psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord, 2008; 22 187–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradbury CL, Christensen BK, Lau MA, et al. The efficacy of cognitive behavior therapy in the treatment of emotional distress after acquired brain injury. Arch Phys Med Rehabil, 2008; 89: S61–68. [DOI] [PubMed] [Google Scholar]
- 29.Faul F, Erdfelder E, Lang A-G, et al. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods, 2007; 39 175–191. [DOI] [PubMed] [Google Scholar]
- 30.SAS Publishing Chapter 15: Mixed Models. In The Analyst Application, Second Edition, p. 116. http://www.stat.cmu.edu/~hseltman/309/Book/chapter15.pdf (accessed December4, 2020).
- 31.NY: IBM Corp SPSS statistics for Mac. Version 21.0. NY: IBM Corp., 2012. [Google Scholar]
- 32.Huang J, Liu F, Teng Z, et al. Care for the psychological status of frontline medical staff fighting against COVID-19. Clin Infect Dis Off Publ Infect Dis Soc Am, 2020. April 3; 71(12):3268-3269. DOI: 10.1093/cid/ciaa385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Junaid K, Ali H, and Nazim R. Depression among healthcare workers during the COVID-19 pandemic in low and middle-income countries: A systematic review. Ann King Edw Med Univ, 2020; 26 252–258. [Google Scholar]
- 34.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun, 2020. March 30; 87:11–17. DOI: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Que J, Shi L, Deng J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. Gen Psychiatry, 2020. June 14; 33. DOI: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naik SS, Manjunatha N, Kumar CN, et al. Patient’s perspectives of telepsychiatry: The past, present and future. Indian J Psychol Med, 2020; 42: 102S–107S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed E-Health, 2020; 26 377–379. [DOI] [PubMed] [Google Scholar]
- 38.Rabinstein AA, Waleed B, and Kallmes DF. Equipoise in clinical trials. Circ Res, 2016; 119 798–800. [DOI] [PubMed] [Google Scholar]
- 39.McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry, 2007; 52 241–247. [DOI] [PubMed] [Google Scholar]
- 40.Su T-P, Lien T-C, Yang C-Y, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J Psychiatr Res, 2007; 41 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fagiolini A, Cuomo A, and Frank E. COVID-19 diary from a psychiatry department in Italy. J Clin Psychiatry, 2020; 81(3): 20com13357. [DOI] [PubMed] [Google Scholar]
- 42.Feinstein RE, Kotara S, Jones B, et al. A health care workers mental health crisis line in the age of COVID-19. Depress Anxiety, 2020; 37 822–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson SU, Ebrahimi OV, and Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLOS ONE, 2020; 15: e0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vasile C. An analysis of psychological trauma interventions. Procedia - Soc Behav Sci, 2014, 127 781–785. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for this article is available online.