Abstract
Background:
Mental health problems increased during the COVID-19 pandemic. Knowledge that one is less at risk after being vaccinated may alleviate distress, but this hypothesis remains unexplored. Here we test whether psychological distress declined in those vaccinated against COVID-19 in the US and whether changes in perceived risk mediated any association.
Methods:
A nationally-representative cohort of U.S. adults (N=5,792) in the Understanding America Study were interviewed every two weeks from March 2020 to June 2021 (28 waves). Difference-in-difference regression tested whether getting vaccinated reduced distress (PHQ-4 scores), with mediation analysis used to identify potential mechanisms, including perceived risks of infection, hospitalization, and death.
Results:
Vaccination was associated with a 0.09 decline in distress scores (95% CI: −0.15 to −0.04) (0–12 scale), a 5.7% relative decrease compared to mean scores in the wave prior to vaccination. Vaccination was also associated with an 8.44 percentage point reduction in perceived risk of infection (95% CI: −9.15% to −7.73%), a 7.44-point reduction in perceived risk of hospitalization (95% CI: −8.07% to −6.82%), and a 5.03-point reduction in perceived risk of death (95% CI: −5.57% to −4.49%). Adjusting for risk perceptions decreased the vaccination-distress association by two-thirds. Event study models suggest vaccinated and never vaccinated respondents followed similar PHQ-4 trends pre-vaccination, diverging significantly post-vaccination. Analyses were robust to individual and wave fixed effects, time-varying controls, and several alternative modelling strategies. Results were similar across sociodemographic groups.
Conclusion:
Receiving a COVID-19 vaccination was associated with declines in distress and perceived risks of infection, hospitalization, and death. Vaccination campaigns could promote these additional benefits of being vaccinated.
Introduction
On May 13th 2020, the United Nations warned that although COVID was primarily an infectious disease, it was also sowing the “seeds of a major mental health crisis”(1). Surveys in the United States reveal elevated levels of psychological distress, anxiety, and suicidal ideation since the onset of the pandemic.(2–6) Several factors have contributed to these findings, including loss of income and work, food insecurity, social isolation, additional care-giving burdens, substance use, and racialized discrimination.(7–18) Personal experience of COVID-related illness and death or hospitalization of a loved one may also contribute.(19, 20) One recent study points to anticipatory fears, with perceived risk of infection and mortality explaining 20.7% of the increased distress between March and June 2020.(21)
High rates of vaccination are crucial to prevent the spread of COVID-19 and its many consequences, including worsening mental health. Yet, as of July 4th, only 67.1% percent of US adults have been vaccinated,(22) falling short of President Biden’s target of 70% by the same date, and daily vaccination rates have fallen sharply.(23) While side effects and safety top the list of concerns of those not vaccinated, lack of information and access remain barriers for vulnerable individuals, particularly people of color.(24) Many people of color who are not yet vaccinated express vaccine hesitancy but also high perceived risk from COVID-19 infection.(25) Meanwhile, although the poor and those facing food and housing insecurity are less likely to be vaccinated, many, especially those with children, want a vaccine.(26)
Are there individual and social benefits of vaccination beyond preventing infection? One hypothesis, so far unexplored, is whether vaccination improves mental health by reducing anticipatory fears of infection, hospitalization, and death. We use a difference-in-difference method with nationally-representative longitudinal data to test whether vaccination for COVID-19 reduces psychological distress and, if so, whether lower perceived risk mediates this association.
Study Design and Methods
Data Source
We used data from the Understanding Coronavirus in America (UCA) study,(27) an extension of an internet-based, nationally representative longitudinal survey.
We examined 28 survey waves, between March 2020 and June, 2021. We restricted the sample to participants in at least 2 survey waves with non-missing values for our exposure, outcome, and covariates and excluded person-period observations in which respondents indicated being unsure of their vaccination status. Our primary analytic sample included 5,792 individuals. Table 1A in the supplement shows dates of each study wave.
Exposure
Our primary exposure was vaccination status, coded as 1 beginning in the first wave in which the respondent answered yes to the question “Have you gotten vaccinated for the coronavirus?” and imputed as 1 thereafter. It was coded as 0 for “No” and imputed as 0 in each period prior to Wave 21 (December 23, 2020 to January 18, 2021), the first time this question was asked.
Outcome
Psychological distress was assessed using the Patient Health Questionnaire (PHQ-4) developed by Kroenke et al.(28), and validated by Lowe et al.(29) The scale consists of the first two items from the PHQ-9 and the Generalized Anxiety Disorder-7 (GAD-7) which assess core criteria for depressive (e.g. “Little interest or pleasure in doing things”) and anxiety disorders (e.g. “Feeling nervous, anxious or on edge”) respectively. Participants report how often they have been bothered by these problems over the last 2 weeks on a four-point scale scored as 0 (“not at all”), 1 (“several days”), 2 (“more than half the days”), or 3 (“nearly every day”). Scores on the scale range from 0 to 12 with higher scores indicating greater distress. Our main analyses use total PHQ-4 scores. We also use a variable for severe distress in supplementary analyses, coded 1 if PHQ-4 scores 9 or above and 0 for those below.(28)
Mediators
Participants were asked “On a scale from 0 to 100%, what is the chance that you will get the coronavirus in the next three months?” and then “If you do get the coronavirus, what is the percent chance you will be hospitalized (spend at least one night in the hospital) from it?” Finally, perceived infection-fatality risk was assessed by asking “If you do get infected with the coronavirus, what is the chance you will die from it?”, with responses also recorded as 0 to 100%.
Covariates
In our main analyses we included individual fixed effects (separate indicators for each person) to adjust for all time-invariant respondent characteristics. We included survey wave fixed effects (separate indicators for each wave) to adjust for national secular trends in mental health. We also adjusted for several time-varying, self-reported covariates: receiving Supplemental Nutrition Assistance Program (SNAP) benefits in the month prior to the survey, receiving unemployment insurance past 14 days, and employment status at the time of the survey.
Statistical Analysis
We first described the demographic characteristics of the sample by vaccination status, which are shown in Table 2A of the supplement. We then use graphical methods to visualize unadjusted temporal trends in psychological distress scores (Figure 1A) and perceived risk factors (Figure 2A) in the supplementary appendix.
Next, we use two-way fixed effects models to assess the association between receiving a COVID-19 vaccination and changes in mental health. These models take the form:
Where γit denotes psychological distress for individual i at wave t. μi and Wt are individual and wave fixed effects respectively, Xit represents time-varying controls. Vaccinatedit is an indicator variable that switches to 1 in first wave in which the respondent answered yes to the question “Have you gotten vaccinated for the coronavirus?” and remains as 1 thereafter.
To assess how the outcomes of interested changed over time before and after vaccination, we estimated so-called “event study” models, wherein Vaccinatedit was replaced with dummy variables indicating the number of periods prior to or following a respondent’s first report of COVID-19 vaccination.(30, 31) We binned dummy variables for lags at 4 or more waves (8 or more weeks) post-vaccination, reflecting the 99th percentile of the distribution of observations in our sample. The event study specification provides two important pieces of information not observable in the single-coefficient two-way fixed effects model.(32) First, that model assumes that distress would have continued along the same trajectory in those who were or were not vaccinated. While this cannot be tested explicitly, including all event leads reveals in the pre-treatment period when coefficients for leads (pre-vaccination) differing significantly from zero would suggest violation of the parallel trends assumption. By contrast, non-zero coefficients for lags (post-vaccination) indicate statistically significant treatment effects. Second, the lags make it possible to see whether the effects grow or shrink over time, and whether they persist. For all analyses, we clustered standard errors by individuals to account for serial correlation.
We conducted several sensitivity checks to test whether the effects of vaccination vary by demographic subgroups, and whether they are robust to alternative modelling strategies.
Results
Table 2A in the supplement shows a gradient in vaccination status by age, income, and education, with higher rates of vaccination observed among older respondents and those at the higher end of the socioeconomic status spectrum. Among self-reported race categories, Asians had the highest rates of vaccination (69%), followed by Hawaiian/Pacific Islander (59%), Whites (57%), mixed race respondents (49%), Black respondents (48%), and American Indian and Alaska Natives (38%). Males had slightly higher rates of vaccination (59%) compared to females (54%) in our sample. Married individuals living with partners had the highest rates of vaccination (61%) among marital status groups, while separated individuals had the lowest (36%).
Figure 1A shows the secular trends in distress scores for never vaccinated respondents and respondents who became vaccinated during our study period. Distress scores increase for both groups at the outset of the pandemic, peaking in Wave 2 (4/1/2020 to 4/27/2020), then decline steadily until Wave 7 (6/10/2020 to 7/6/2020). Notwithstanding some fluctuations, distress scores then remain relatively stable for both groups until Wave 26 (3/17/2021 to 4/27/2021), after which distress declines slightly for respondents who became vaccinated and increases slightly for never vaccinated respondents. Wave 26 corresponds to the median wave of vaccination in our sample.
Figure 2A shows secular trends in risk perceptions for never vaccinated respondents and respondents who became vaccinated during our study period. Here, while respondents who became vaccinated exhibited slightly higher levels of risk perceptions for the majority of the study period, both groups shared similar trends until Wave 25 (2/17/2021 to 3/29/2021), corresponding to the wave prior to the median wave of vaccination in our sample. Risk perceptions then decline for respondents who became vaccinated, falling below the mean risk perception levels of respondents who did not become vaccinated.
Table 1 shows our difference-in-difference estimates for the association between vaccination and perceived risk of infection in Model 1, perceived risk of hospitalization in Model 2, and perceived risk of death in Model 3. All models adjust for individual and wave fixed effects, and time-varying unemployment insurance, SNAP, and employment status. Here, vaccination is associated with an 8.44 percentage point reduction in perceived risk of infection (95% CI: −9.15% to −7.73%), a 7.44-point reduction in perceived risk of hospitalization (95% CI: −8.07% to −6.82%), and a 5.03-point reduction in perceived risk of death (95% CI: −5.57% to −4.49%).
Table 1.
Two-way fixed effects models with perceived risk factors regressed on vaccination status, April 2020 to June 2021 (N= 5,792)
| Model 1. Risk of Infection | Model 2. Risk of Hospitalization | Model 3. Risk of death | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Received Vaccination (ref: no) | −8.44*** | −9.15 to −7.73 | −.744*** | −8.07 to −6.82 | −5.03*** | −5.57 to −4.49 |
| Received UI (ref: no) | ||||||
| Yes | 0.81 | −0.14 to 1.75 | 0.90* | 0.07 to 1.74 | 1.05** | 0.40 to 1.70 |
| Unsure | 1.15 | −0.33 to 2.63 | 0.63 | −1.18 to 2.44 | −0.02 | −1.65 to 1.60 |
| Received SNAP (ref: no) | ||||||
| Yes | 0.46 | −0.49 to 1.41 | 0.23 | −0.69 to 1.15 | −0.38 | −1.17 to 0.41 |
| Unsure | −1.11 | −2.31 to 0.09 | −1.32* | −2.64 to −0.00 | −0.57 | −1.79 to 0.66 |
| Currently working (ref: no) | 0.72 | −0.34 to 1.78 | 0.44 | −0.55 to 1.43 | −0.23 | −0.99 to 0.54 |
| Individual fixed effects | Yes | Yes | Yes | |||
| Wave fixed effects | Yes | Yes | Yes | |||
| Constant | 21.69*** | 20.78 to 22.59 | 32.35*** | 31.25 to 33.46 | 23.49*** | 22.66 to 24.32 |
| N. of cases | 5,792 | 5,792 | 5,792 | |||
p<0.05,
p<0.01,
p<0.001
Table 2 shows our primary difference-in-difference analyses. In Model 1, receiving vaccination is associated with a −.09 decrease in distress scores (p < 0.001; 95% CI: −0.15 to −0.04), and this relationship remains unchanged after adjusting for unemployment insurance, SNAP, and employment status in Model 2. This estimate corresponds to a 5.7% relative reduction in distress compared to mean distress scores in the wave prior to vaccination.
Table 2.
Two-way fixed effects models with psychological distress (PHQ-4) regressed on vaccination status and perceived risk factors, April 2020 to June 2021 (N= 5,792)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Received Vaccination (ref: no) | −0.09*** | −0.15 to −0.04 | −0.09*** | −0.15 to −0.04 | −0.03 | −0.09 to 0.02 |
| Received UI (ref: no) | ||||||
| Yes | 0.07 | −0.04 to 0.18 | 0.06 | −0.05 to 0.17 | ||
| Unsure | 0.01 | −0.29 to 0.31 | 0.00 | −0.30 to 0.31 | ||
| Received SNAP (ref: no) | ||||||
| Yes | 0.03 | −0.09 to 0.15 | 0.03 | −0.09 to 0.15 | ||
| Unsure | −0.22* | −0.40 to −0.04 | −0.21* | −0.39 to −0.03 | ||
| Currently working (ref: no) | ||||||
| Yes | 0.07 | −0.05 to 0.20 | 0.07 | −0.05 to 0.19 | ||
| Risk of infection | 0.04*** | 0.03 to 0.05 | ||||
| Risk of Hospitalization | 0.02** | 0.01 to 0.03 | ||||
| Risk of death | 0.03*** | 0.01 to 0.04 | ||||
| Individual fixed effects | Yes | Yes | Yes | |||
| Wave fixed effects | Yes | Yes | Yes | |||
| Constant | 2.25*** | 2.17 to 2.33 | 2.21*** | 2.10 to 2.32 | 2.00*** | 1.89 to 2.12 |
| N. of cases | 5,792 | 5,792 | 5,792 | |||
p<0.05,
p<0.01,
p<0.001
Notes: Standard errors are clustered at the individual level. Coefficients for perceived risk factors are expressed as a 10-percentage point increase.
Model 3 adjusts for risk perceptions, which are all independently associated with distress net of each other. A 10-percentage point increase in perceived risk of infection is associated with a 0.04 increase in psychological distress scores (p <0.001; 95% CI: 0.03 to 0.05); perceived risk of hospitalization is associated with a 0.02 increase in psychological distress scores (p <0.01; 95% CI: 0.01 to 0.03); death is associated with a 0.03 increase in psychological distress scores (p <0.001; 95% CI: 0.01 to 0.04). Importantly, adjusting for risk perceptions in Model 3 reduces the coefficient for vaccination by two-thirds, to −0.03, which is no longer statistically significant (p = 0.22; 95% CI: −0.09 to 0.02). Taken together, these models suggest that the receiving the COVID-19 vaccination reduces psychological distress, and that this effect is transmitted largely through declines in perceived risk of infection, hospitalization, and death.
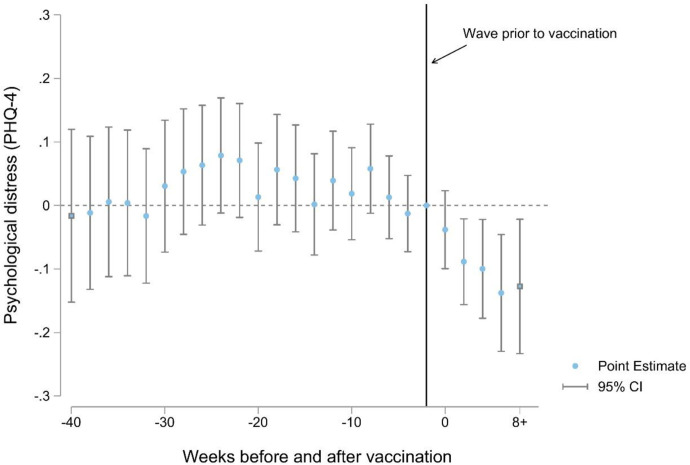
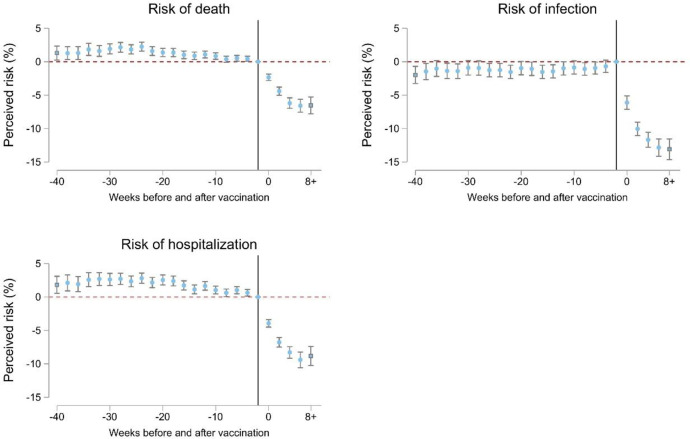
The event study analyses in Figures 1 and 2 provide additional support for our findings in Table 2. Figure 1 shows vaccinated and never vaccinated respondents followed similar trends in distress scores prior to vaccination, and that these diverged significantly afterwards, with vaccinated respondents experiencing significant declines in distress. Importantly, these treatment effects persist for 8 weeks post vaccination. It takes a few waves for the effect to be fully realized, which suggests that our regression estimates likely underestimate the true effect. In Figure 2 we observe slight differences in risk perceptions between vaccinated and never vaccinated respondents in the pre-treatment period, although these are stable over time. Following vaccination, these trends diverge, with vaccinated individuals experiencing large reductions risk perceptions relative to those who were never vaccinated in our sample. Finally, Figure 1A (supplement) shows the event study results for the effect of vaccination on distress after adjusting for risk perceptions. Consistent with Model 3 in Table 2, we observe no significant treatment effects of vaccination after accounting for changing risk perceptions associated with vaccination.
Figure 1.
Difference-in-Differences Estimates of the Association Between Receiving the COVID-19 Vaccine and Psychological Distress
Notes: Each point estimate refers to the change in distress between vaccinated and never vaccinated individuals, compared to their baseline differential in the wave immediately prior to vaccination. Models control for individual and wave fixed effects, receiving Supplemental Nutrition Assistance Program (SNAP) benefits in the month prior to the survey, whether the respondent received unemployment insurance in the past 14 days, and employment status at the time of the survey.
Figure 2:
Difference-in-Differences Estimates of the Association Between Receiving the COVID-19 Vaccine and Perceived Risk Factor
Notes: Each point estimate refers to the change in risk perceptions between vaccinated and never vaccinated individuals, compared to their baseline differential in the wave immediately prior to vaccination (reference line on the x-axis). Models control for individual and wave fixed effects, receiving Supplemental Nutrition Assistance Program (SNAP) benefits in the month prior to the survey, whether the respondent received unemployment insurance in the past 14 days, and employment status at the time of the survey.
Sensitivity checks
Figures 4A–8A in the supplement test whether the effects of vaccination vary by demographic subgroups. Each figure represents two-way fixed effects models with psychological distress scores regressed on vaccination status stratified by age groups (Figure 4A), race/ethnicity (Figure 5A), education (Figure 6A), gender (Figure 7A), and household income (Figure 8A). Here, we do not observe substantive differences in the effect of vaccination across sociodemographic groups.
Tables 3A–6A show how the patterns described in our main analyses remain robust after using sample weights, restricting our models to respondents aged 65+, including state-by-wave fixed effects, and when using an indicator for severe psychological (PHQ-4 scores ≥ 9) as the dependent variable. With respect to the latter, we found that vaccination was associated with a 0.6 percentage point reduction in severe distress from a baseline prevalence of 0.04% in the wave prior to vaccination, corresponding to a 15% relative decline.
Discussion
This study has several important findings. First, vaccination was associated with a 5.7% reduction in PHQ-4 distress scores and a 15% reduction in severe distress (PHQ-4 scores ≥ 9). Vaccination was also associated with an 8.44 percentage point reduction in perceived risk of infection, a 7.44-point reduction in perceived risk of hospitalization, and a 5.03-point reduction in perceived risk of death. Adjusting for risk perceptions decreased the association between vaccination and distress by two-thirds, to statistical insignificance. Complementary panel event study models suggest that vaccinated and never vaccinated respondents shared similar trends in distress prior to vaccination, and that these trends diverged significantly following vaccination.
As with all observational analyses, our study has clear limitations. First, measurements of both the distress and vaccination rely on self-report, which may be biased. Second, the web-based sample may not be truly representative of the US population and individuals from underrepresented racial and ethnic groups. Third, our analysis was designed to capture only the direct effect of an individual becoming vaccinated on their own mental health. However, vaccination is likely to have myriad positive spillover effects on mental health that are not captured in this study. Mental health may improve as friends and family become vaccinated, as the economy rebounds, as community prevalence of virus falls, and as fewer people suffer major illness or death. The respondents in the UCA study likely benefited from vaccine scale-up beyond their own vaccination status. Additionally, their getting vaccinated likely benefited other peoples’ mental health. As a result, our findings likely substantially underestimate the beneficial effect of vaccination for mental health at the population level.
Notwithstanding these limitations, our study has several key strengths. First, to our knowledge, this is the first study to assess the psychological impacts of COVID-19 vaccination. Second, our main findings are robust to time-varying controls, individual and wave fixed effects, and several alternative modelling strategies. Importantly, our analyses were robust to state-by-wave fixed effects, ruling out confounding due to time-varying factors at the state-level, such as rates of infection or policy implementation. Third, our event study models show that the mental health benefits of vaccination persist for at least 8 weeks, suggesting that these effects are not a signal of fleeting relief.
Our results have important public health and policy implications. Murphy and colleagues(35) suggest that messages tailored to vaccine hesitant or resistant individuals could emphasize the personal benefits of vaccination against COVID-19. We provide an evidence base for these personal benefits that underscore mental health improvements following vaccination in a nationally representative sample of U.S. adults. We also demonstrate that vaccination is a key lever in reducing the mental health burdens associated with the COVID-19 pandemic.
Supplementary Material
Acknowledgements:
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 tracking data is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging, and many others. The authors would also like to thank Atheendar Venkataramani for his helpful comments on an earlier version of this manuscript.
Footnotes
Competing interests: none to declare.
References
- 1.UN. COVID-19 and the Need for Action on Mental Health. 2020. Available from: https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf.
- 2.O’Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. The British Journal of Psychiatry. 2021;218(6):326–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. Journal of psychiatric research. 2021;136:603–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA network open. 2020;3(9):e2019686–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of affective disorders. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Purtle J. COVID-19 and mental health equity in the United States. Social psychiatry and psychiatric epidemiology. 2020;55(8):969–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pancani L, Marinucci M, Aureli N, Riva P. Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown. Frontiers in Psychology. 2021;12:1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hertz-Palmor N, Moore TM, Gothelf D, DiDomenico GE, Dekel I, Greenberg DM, et al. Association among income loss, financial strain and depressive symptoms during COVID-19: evidence from two longitudinal studies. Journal of affective disorders. 2021;291:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. Journal of occupational and environmental medicine. 2020;62(9):686–91. [DOI] [PubMed] [Google Scholar]
- 11.Witteveen D, Velthorst E. Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences. 2020;117(44):27277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donnelly R, Farina MP. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Social science & medicine. 2021;269:113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panchal N, Kamal R, Orgera K, Cox C, Garfield R, Hamel L, et al. The implications of COVID-19 for mental health and substance use. Kaiser family foundation. 2020;21. [Google Scholar]
- 14.Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry & Human Development. 2020;51(5):671–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wade M, Prime H, Johnson D, May SS, Jenkins JM, Browne DT. The disparate impact of COVID-19 on the mental health of female and male caregivers. Social Science & Medicine. 2021;275:113801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu C, Qian Y, Wilkes R. Anti-Asian discrimination and the Asian-white mental health gap during COVID-19. Ethnic and Racial Studies. 2021;44(5):819–35. [Google Scholar]
- 17.Chae DH, Yip T, Martz CD, Chung K, Richeson JA, Hajat A, et al. Vicarious racism and vigilance during the CoViD-19 pandemic: mental health implications among Asian and Black Americans. Public Health Reports. 2021:00333549211018675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang D, Thomsen MR, Nayga RM. The association between food insecurity and mental health during the COVID-19 pandemic. BMC public health. 2021;21(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simon NM, Saxe GN, Marmar CR. Mental Health Disorders Related to COVID-19–Related Deaths. JAMA. 2020;324(15):1493–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joaquim RM, Pinto ALCB, Guatimosim RF, de Paula JJ, Souza Costa D, Diaz AP, et al. Bereavement and psychological distress during COVID-19 pandemics: The impact of death experience on mental health. Current Research in Behavioral Sciences. 2021;2:100019. [Google Scholar]
- 21.Robinson E, Daly M. Explaining the rise and fall of psychological distress during the COVID‐19 crisis in the United States: Longitudinal evidence from the Understanding America Study. British journal of health psychology. 2021;26(2):570–87. [DOI] [PubMed] [Google Scholar]
- 22.COVID-19 Vaccinations in the United States. Centers for Disease Control and Prevention [Internet]. 2021. July 4 2021. Available from: https://covid.cdc.gov/covid-data-tracker/#vaccinations.
- 23.See How Vaccinations Are Going in Your County and State July 4 2021. Available from: https://www.nytimes.com/interactive/2020/us/covid-19-vaccine-doses.html.
- 24.Hamel Liz, Lopes Lunna, Kearney Audrey, Sparks Grace, Stokes Mellisha, and Brodie Mollyann. KFF COVID-19 Vaccine Monitor: June 2021 2021. Jun 30, 2021. Available from: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-june-2021/.
- 25.Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, et al. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clinical and Translational Science. 2021: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Julia Raifman AS, and Michaels David. Something to celebrate: delivering vaccines to essential workers. STAT [Internet]. 2021. July 5, 2021. Available from: https://www.statnews.com/2021/07/01/essential-workers-getting-vaccinated-something-to-celebrate/?utm_content=buffer1810c&utm_medium=social&utm_source=twitter&utm_campaign=twitter_organic. [Google Scholar]
- 27.Understanding Coronavirus in America Survey. [Internet]. Center for Economic and Social Research (CESR). [cited July 1, 2021.]. Available from: https://uasdata.usc.edu/index.php.
- 28.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–21. [DOI] [PubMed] [Google Scholar]
- 29.Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of affective disorders. 2010;122(1–2):86–95. [DOI] [PubMed] [Google Scholar]
- 30.Venkataramani AS, Bair EF, O’Brien RL, Tsai AC. Association Between Automotive Assembly Plant Closures and Opioid Overdose Mortality in the United States: A Difference-in-Differences Analysis. JAMA Internal Medicine. 2020;180(2):254–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raifman J, Bor J, Venkataramani A. Association Between Receipt of Unemployment Insurance and Food Insecurity Among People Who Lost Employment During the COVID-19 Pandemic in the United States. JAMA Network Open. 2021;4(1):e2035884–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clarke D, Schythe K. Implementing the panel event study 2020. Available from: http://www.damianclarke.net/research/papers/panelEvent.pdf.
- 33.CSUSB. Report to the Nation: Anti-Asian Prejudice & Hate Crime. San Bernardino, CA: Center for the Study of Hate & Extremism.; [updated Accessed: July 11, 2021. Available from: https://www.csusb.edu/sites/default/files/Report%20to%20the%20Nation%20-%20Anti-Asian%20Hate%202020%20Final%20Draft%20-%20As%20of%20Apr%2030%202021%206%20PM%20corrected.pdf. [Google Scholar]
- 34.Goodman-Bacon A, Marcus J. Using difference-in-differences to identify causal effects of COVID-19 policies. 2020.
- 35.Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature communications. 2021;12(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.