Abstract
Purpose:
To describe follow-up rates for patients referred for outpatient ophthalmic care after emergency department (ED) discharge and identify patient and visit characteristics associated with loss to follow-up (LTFU).
Design:
Single-institution retrospective cohort study.
Methods:
We analyzed the medical records of 2,206 patients seen in the ED for an eye-related issue who were subsequently scheduled for ophthalmology follow-up between 2013-2019 at a single tertiary health system. The main outcome measures were the frequency of and risk factors for LTFU and ED revisits.
Results:
In total, 1649 (74.8%) completed follow-up within 2-months of an index ED visit. On multivariable analysis, younger age (p<0.001), a nonurgent ophthalmic condition or non-ophthalmic primary diagnosis (p<0.001), scheduled follow-up >5 days after the ED visit (p<0.001), additional follow-up appointments (<0.001), no prior history of ophthalmology appointments (p=0.045), visual acuity of 20/40 or better (p=0.027), and having Medicaid or being uninsured (p<0.001) were significantly associated with LTFU. The presence of an interpreter significantly increased the likelihood of follow-up among non-English speaking patients (p<0.001). LTFU was significantly associated with an ED revisit within 4-months of an index visit and the ED revisit rate was significantly higher for patients LTFU versus those who completed follow-up (5.7% vs. 1.1%; p<0.001).
Conclusions:
A quarter of patients referred for ophthalmic care following an ED presentation were LTFU. We identified multiple factors associated with LTFU that could be used to develop interventions to enhance follow-up. Additionally, patients who were LTFU were more likely to revisit the ED for the same ophthalmic condition.
INTRODUCTION
The number of emergency department (ED) visits for ophthalmic conditions has continued to increase each year; recent estimates report nearly 2 million eye-related ED encounters annually.1 In the vast majority of cases, hospitalization is not warranted and patients are discharged home with scheduled follow-up care.1 Follow-up care for ophthalmic conditions is important for several reasons. First, it ensures appropriate treatment continuation, reducing the likelihood of patients re-presenting to the ED due to complications or treatment failure,2 which can be costly and clinically inefficient.3 Second, it can facilitate correction of misdiagnoses, which have been reported to be as common as 40% among eye-related presentations in the ED.4,5 Third, follow-up can facilitate the transition to long-term ophthalmic management for previously undiagnosed conditions, which can improve functional and anatomic outcomes.6
Despite the importance of timely follow-up after an ED visit, previous studies in other medical specialties have reported that nearly half of patients referred for follow-up care after ED discharge do not complete follow-up.7–9 Among eye-related ED presentations specifically, estimates of follow-up rates from small observational studies are reported to be approximately 60%.10,11 However, while several factors have been found to be associated with outpatient follow-up after ED discharge for other medical conditions, we are unaware of any studies reporting factors impacting loss to follow-up (LTFU) after general eye-related ED visits or the association between LTFU and ED revisit rates and could find no reference to these in a computerized search of PubMed and Ovid Medline.
Accordingly, we determined rates of LTFU after an eye-related ED index visit and identified factors associated with LTFU at a single academic institution. We hypothesized that specific patient demographic populations would be at higher risk of LTFU and that patients LTFU would be at higher risk of an ED revisit.
METHODS
This is a 7-year single-institution retrospective cohort study of patients within the Yale New Haven Hospital (YNHH) health system. The Yale University Institutional Review Board (IRB) approved this study prospectively and waived informed patient consent due to the retrospective observational nature of the study. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Population
We queried the YNHH health system for patients who scheduled an initial ophthalmic ED follow-up appointment between January 1, 2013 and June 1, 2019 within 30 days of presentation to either of two YNHH hospital-affiliated EDs. This duration of time was chosen to allow for varying recommended follow-up intervals for both urgent and nonurgent conditions. Very few patients at this institution were recommended to follow-up more than 30 days from the index ED visit. We included patients who were 18 years or older, and discharged home or to their location of residence from the ED. We excluded patients who were transferred, admitted or received surgery during their index ED visit as well as patients presenting to the ED for post-op checks.
We also took several measures to exclude patients who may have followed-up with an ophthalmologist outside of the YNHH system. First, we excluded participants who were referred for follow-up ophthalmic care but did not subsequently schedule an appointment as they may have instead seen an external ophthalmologist. Second, we excluded patients with an outside ophthalmologist listed in any chart documentation. Third, we searched each chart for ophthalmologist follow-up appointments recorded outside of YNHH affiliated institutions but within the electronic health record’s network of state- and nationwide clinics.12 Lastly, we excluded patients who cancelled or missed their follow-up appointment and reported the reason for doing so as seeing an outside ophthalmologist. In total, 2,206 patients satisfied all criteria (Figure 1).
Figure 1.
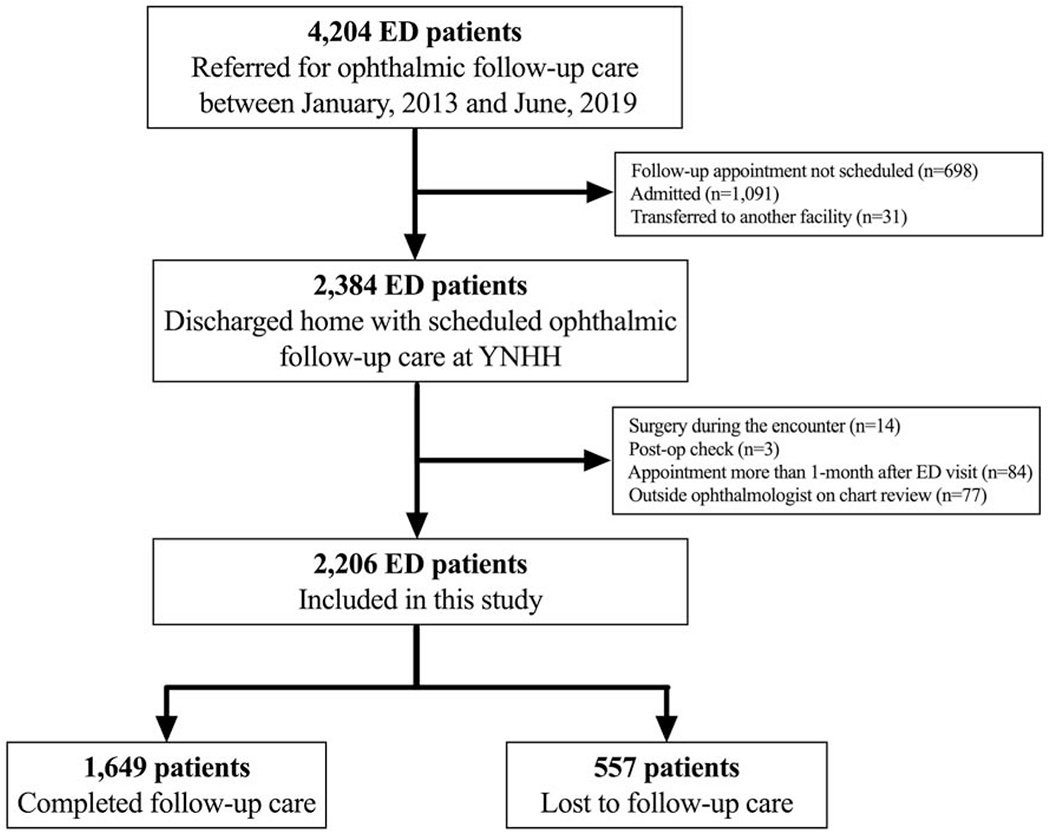
Study inclusion and exclusion criteria flowchart. ED = emergency department; YNHH = Yale New Haven Hospital.
Institutional referral pathway
Patients seen in the ED who were referred for follow-up ophthalmic care either received an appointment prior to discharge in the ED or were informed to call the follow-up clinic to schedule an appointment. All patients received an automated telephone reminder 24 hours prior to their appointment, per YNHH institutional practices.
Measures
LTFU was defined as the absence of any completed ophthalmology follow-up appointments after discharge from the ED within 2 months after the index ED visit. This duration threshold was chosen to provide adequate time for patients who may have missed an initial scheduled appointment to reschedule for a more suitable time.
We coded patient diagnoses using the International Classification of Disease, Ninth and Tenth Revision, Clinical Modification (ICD-9-CM and ICD-10-CM). We classified presenting ophthalmic conditions as urgent or non-urgent using definitions derived from prior studies.1,13 Diagnoses with an undefined urgency status in the literature were independently assigned urgent or non-urgent status by two authors (EC and RP). Disagreements were resolved by an experienced ophthalmologist (KN). Categorization of ophthalmic conditions by urgency status are shown in Supplemental Table 1 and Supplemental Table 2 (Supplemental Material at AJO.com).
From chart review, we abstracted demographic variables including patient age, sex, ethnicity/race, primary payer information, primary language (English vs. non-English) and home address. Ethnicity/race was patient-reported and categorized into mutually exclusive groups as non-Hispanic Black or African American, non-Hispanic white, Hispanic or Latino, and other. We simplified primary payer status into four categories: privately insured, insured by Medicaid, insured by Medicare and uninsured. Private insurance included any commercial health plan as well as workers compensation. We also examined clinical variables related to the ED encounter including whether a follow-up appointment time was provided at discharge, whether the primary diagnosis was an ophthalmic condition, the presence of other non-ophthalmic follow-up appointments scheduled at discharge, the presence of an ophthalmology consult, the presence of an interpreter (in person or via phone or video), and the best-corrected visual acuity (BCVA) of the affected eye. BCVA was dichotomized into 20/40 or better and worse than 20/40 in the affected eye.14 If both eyes were affected, the BCVA of the worse eye was utilized. The presence of an ophthalmology consult was defined as an ophthalmologist examining the patient and recording a clinical encounter.
Additionally, we collected variables related to follow-up care including the number of days from the ED visit to the follow-up appointment, the estimated travel time (ETT) to the follow-up appointment, history of a prior ophthalmology appointment, and history of a missed ophthalmology appointment (“No-show” status) within the YNHH electronic medical record system. The ETT was the shortest route, in terms of time with adherence to specified speed limits, from each patient’s home address to the follow-up location using geographic and speed limit data from OpenStreetMap and the ”osrm” package in R.15,16 Patients with an address associated with an advanced care facility, PO box or non-Connecticut location were excluded from this analysis.
Lastly, we examined ED revisits, which were defined as any additional ED encounters for the initial presenting ophthalmic condition that occurred after the date of the scheduled follow-up appointment and within 4 months of the index ED presentation. Revisits that occurred more than 4 months after the index ED presentation were considered as separate encounters. Patients who missed an initial follow-up appointment and subsequently re-presented to the ED for the same ophthalmic condition were defined as LTFU even if the 2-month duration threshold had not been reached.
Statistical Analysis
We reported mean and standard deviation (SD) for continuous variables and proportion for categorical variables unless otherwise specified. Logistic regression modeling assessed the association between LTFU and various factors as well as the association between ED revisits and LTFU. We also conducted gender-stratified regression models and included interaction terms for significant covariates in a combined multivariable regression to identify gender differences in factors associated with LTFU.17 We clustered standard errors at the patient level, assuming no intra-group correlation, using cluster-correlated robust sandwich covariance estimates to account for the same patients presenting multiple times for different eye conditions during this period. The multivariable logistic regression included factors with p<0.2 on bivariate regression. To identify a threshold cutoff for appointment scheduling, we used receiver-operating characteristic (ROC) curves to identify a threshold lag time between the index ED visit and follow-up appointment that maximized the Youden index.18,19 To assess if follow-up rates had significantly changed over time we performed linear regression analysis with follow-up rates as the outcome and time (in years) as the predictor. Lastly, due to the potential ambiguity and accuracy of a patient’s primary diagnosis, we conducted a sensitivity analysis of our multivariate logistic regression excluding the covariates pertaining to the urgency of a primary diagnosis and whether the patient’s primary diagnosis was ophthalmic. All statistical analyses were conducted in R 3.6.0 (R foundation for Statistical Computing). Graphpad Prism 8 (Graphpad Software, San Diego, CA) was used for graphical depictions. A 2-sided p-value <0.05 was considered statistically significant.
RESULTS
Between January 1, 2013 and June 1, 2019, there were 2,206 scheduled appointments for follow-up ophthalmic care after an ED encounter for an eye-related issue. Of all encounters, there were 2,106 unique patients, of whom 2,025 presented to the ED once. Table 1 summarizes characteristics of the study population on an encounter-level. The mean (SD) patient age was 43.7 (16.1) years and 905 (41.0%) patients were female. The median ETT for patients to the location of the scheduled follow-up appointment was 12.8 minutes (mean, 19.0; SD, 33.6). Among the 2,181 encounters for which an ophthalmic condition was designated as the primary or secondary ED diagnosis, 852 (39.1%) diagnoses were urgent and 1,329 (60.9%) were non-urgent according to our criteria. Fifteen ophthalmic diagnosis sub-categories accounted for 76.2% of all visits (Figure 2). In total, 1,345 (61.0%) patients had a follow-up appointment scheduled by a provider prior to ED discharge and 861 (39.0%) self-scheduled an appointment after discharge upon recommendation to call.
Table 1.
Baseline study group characteristics in the total population and by follow-up completion status
| Total Population | Followed-up | Lost to follow-up | |
|---|---|---|---|
| Total no. (%) | 2206 (100.0) | 1649 (74.8) | 557 (25.2) |
| Age, years; mean (SD) | 43.7 (16.1) | 44.9 (16.5) | 40.5 (14.4) |
| Gender Female Male |
905 (41.0) 1301 (59.0) |
689 (41.8) 960 (58.2) |
216 (38.8) 341 (61.2) |
| Race Black or African American Hispanic or Latino Non-Hispanic White Other |
696 (31.6) 595 (27.0) 795 (36.0) 120 (5.4) |
498 (30.2) 445 (27.0) 603 (36.6) 103 (6.2) |
198 (35.5) 150 (26.9) 192 (34.5) 17 (3.1) |
| Insurance Status Private Medicare Medicaid Uninsured Other |
377 (17.1) 579 (26.2) 894 (40.5) 347 (15.7) 9 (0.4) |
309 (18.7) 478 (29.0) 606 (36.7) 250 (15.2) 6 (0.4) |
68 (12.2) 101 (18.1) 288 (51.7) 97 (17.4) 3 (0.5) |
| Language English Non-English |
1836 (83.2) 370 (16.8) |
1363 (82.7) 286 (17.3) |
473 (84.9) 84 (15.1) |
| Appointment at discharge No Yes |
861 (39.0) 1345 (61.0) |
597 (36.2) 1052 (63.8) |
264 (47.4) 293 (52.6) |
| Non-ophthalmic referrals at discharge No Yes |
1695 (76.8) 511 (23.2) |
1324 (80.3) 325 (19.7) |
371 (66.6) 186 (33.4) |
| Ophthalmology consult No Yes |
701 (31.8) 1505 (68.2) |
529 (32.1) 1120 (67.9) |
172 (30.9) 385 (69.1) |
| Nonurgent ophthalmic conditiona No Yes |
852 (39.1) 1329 (60.9) |
713 (39.8) 917 (60.2) |
224 (37.0) 328 (63.0) |
| Primary ophthalmic condition No Yes |
113 (5.1) 2093 (94.9) |
40 (2.4) 1634 (97.6) |
73 (13.1) 484 (86.9) |
| Days from ED visit to follow-up; mean (SD) | 5.5 (5.7) | 4.7 (4.9) | 8.1 (6.8) |
| BCVA of affected eyeb Worse than 20/40 20/40 or better |
500 (38.8) 1236 (71.2) |
411 (32.5) 853 (67.5) |
98 (20.4) 383 (79.6) |
| History of ophthalmology appointment in system No Yes |
1902 (86.2) 304 (13.8) |
1408 (85.4) 241 (14.6) |
494 (88.7) 63 (11.3) |
| History of missed follow-up No Yes |
2002 (90.8) 204 (9.2) |
1492 (90.5) 157 (9.5) |
510 (91.6) 47 (8.4) |
| Travel time to follow-up (min); mean (SD) | 19.0 (33.6) | 19.6 (38.0) | 17.4 (13.9) |
| Interpreter present if non-English speaker Yes No |
198 (53.5) 172 (46.4) |
172 (60.1) 114 (39.9) |
26 (40.0) 58 (60.0) |
Proportions calculated from 2,181 patients with an ophthalmic diagnosis classified into urgent or non-urgent status. Twenty-five patients did not have a primary or secondary ophthalmic diagnosis code and were not classified.
If both eyes affected, BCVA of worse eye
ED = Emergency department; SD = Standard deviation; BCVA = Best corrected visual acuity
Figure 2.
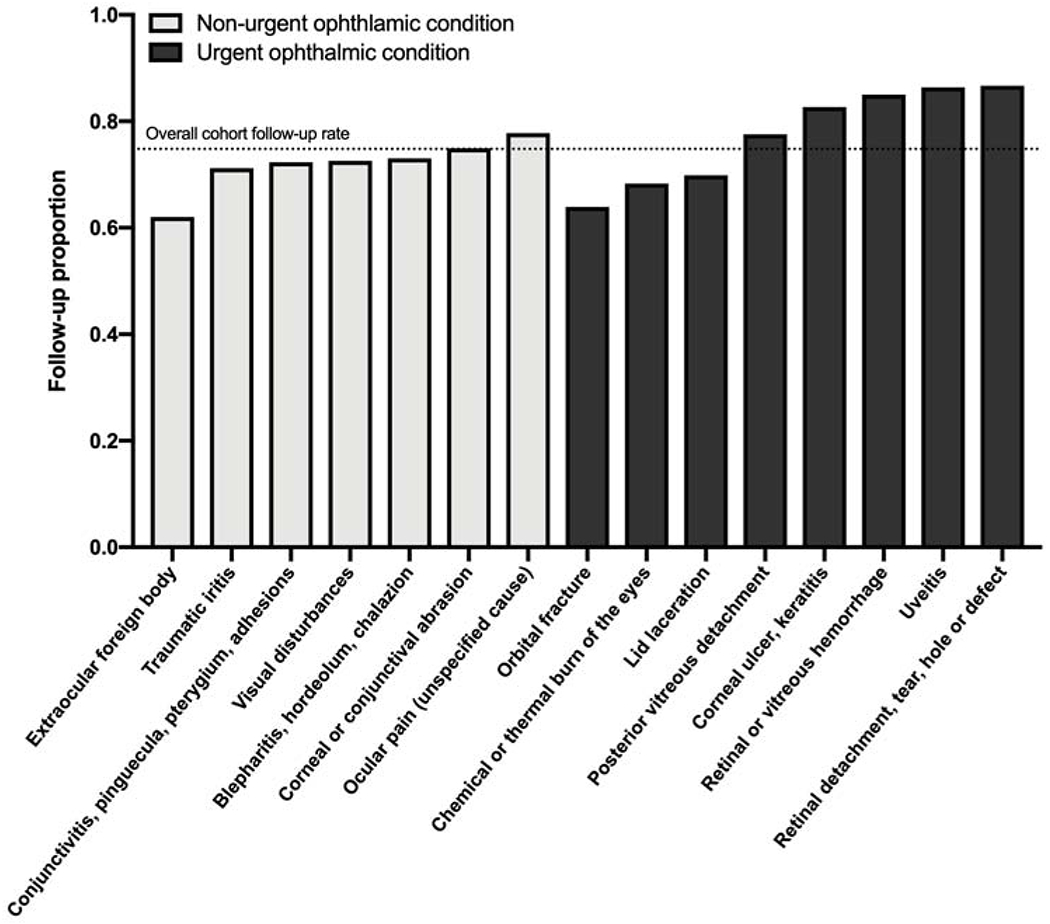
Follow-up rates of the 15 most commonly presenting ophthalmic conditions within this cohort. The follow-up rate of the entire cohort, 74.8%, is noted by a dotted line.
LTFU Rates
Overall, 557 (25.2%) patients were LTFU while 1,649 (74.8%) completed an ophthalmic follow-up visit within 2 months of the index ED visit. Figure 2 shows follow-up rates for the 15 most common ophthalmic diagnoses in this cohort. LTFU was more common among patients presenting with non-urgent diagnoses (26.3%) compared to urgent diagnoses (23.9%). From 2013 to 2018, the number of annual scheduled ophthalmic follow-ups increased more than four-fold from 109 to 528. However, the LTFU rate did not significantly change (30.3% in 2013 vs 29.2% in 2019; p=0.91).
Figure 3 depicts rates of follow-up as a function of time from the ED visit to the scheduled follow-up appointment. The average lag time between the index ED visit and the follow-up appointment was 5.5 (5.7) days, and on average, follow-up rates decreased as a function of time. Patients who had a follow-up within one week of ED presentation had a follow-up completion rate of 80.2%, compared to a rate of 43.5% for those whose follow-up was more than 3 weeks after the index ED visit. The maximum Youden index was achieved at a threshold of 5.5 days, which was subsequently used as a cutoff for logistic regression analyses.
Figure 3.
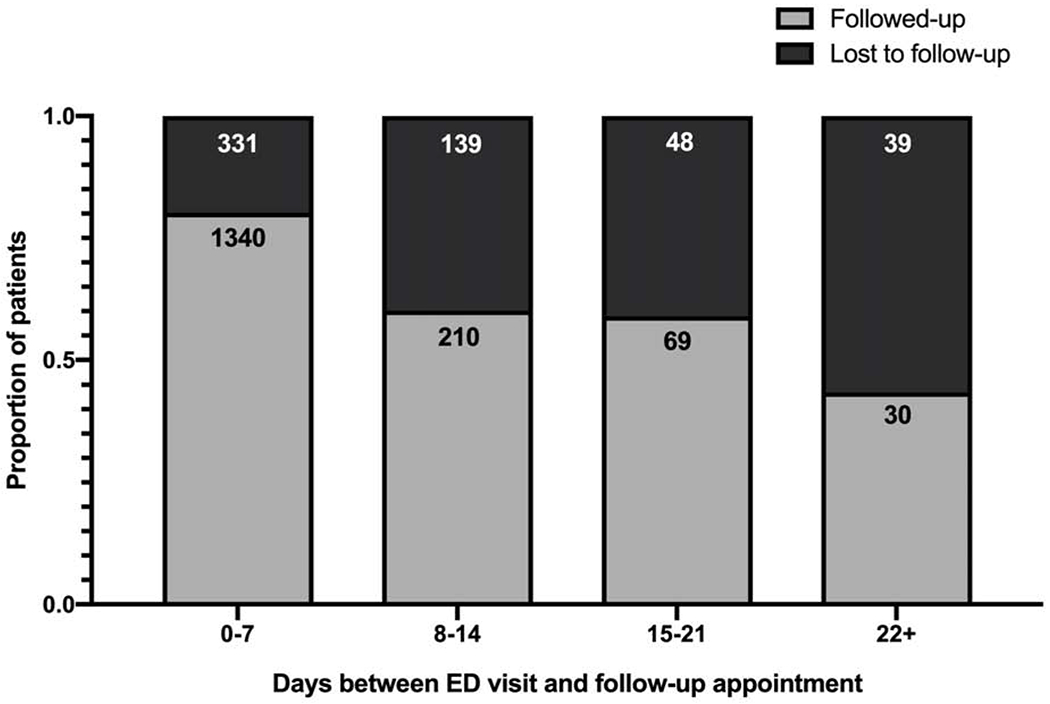
Follow-up rates by time between the emergency department visit and follow-up appointment. Numbers above each bar chart indicate the number of encounters per group.
Predictors of Lost to Follow-up Ophthalmic Care
Demographic factors associated with LTFU on multivariable analysis included younger age (odds ratio [OR], 0.98; 95% CI, 0.97-0.98; p<0.001), and having Medicaid coverage (OR, 1.87; 95% CI, 1.29-2.71; p<0.001) or being uninsured (OR, 2.32; 95% CI, 1.48-3.64; p<0.001) (Table 2). Clinically, patients who had other non-ophthalmic referrals on discharge (OR, 1.73; 95% CI, 1.30-2.30; p<0.001), a nonurgent ophthalmic condition (OR, 1.59; 95% CI, 1.23-2.03; p<0.001), a follow-up appointment scheduled more than 5 days after the ED visit (OR, 2.71; 95% CI, 2.10-3.51; p<0.001) and visual acuity of 20/40 or better on ED presentation (OR, 1.40; 95% CI, 1.04-1.90; p=0.02) were significantly more likely to be LTFU. Conversely, patients whose primary diagnosis was an ophthalmic condition (OR, 0.07; 95% CI, 0.03-1.15; p<0.001) or who had a history of prior ophthalmology appointments (OR, 0.68; 95% CI, 0.47-0.99; p=0.045) were less likely to be LTFU. Among non-English speakers, the absence of an interpreter (OR, 3.19; 95% CI, 1.84-5.78; p<0.001) was also independently associated with LTFU. In sensitivity analysis excluding factors pertaining to a patient’s primary diagnosis, the association between factors and ED LTFU that were significant on primary analysis remained significant.
Table 2:
Bivariable and multivariable logistic regression analyses of factors associated with loss to follow-up ophthalmic care. Multivariable regression includes covariates with p<0.2 on univariate analysis.
| Univariate analysis Odds ratio (95% CI) |
p-value | Multivariate analysis Odds ratio (95% CI) |
p-value | |
|---|---|---|---|---|
| Age | 0.98 (0.98-0.99) | <0.001 | 0.98 (0.97-0.98) | <0.001 |
| Gender Female Male |
1.00 1.13 (0.93-1.38) |
0.21 |
||
| Race Non-Hispanic White Black or African American Hispanic or Latino Other |
1.00 1.25 (0.99-1.57) 1.06 (0.83-1.35) 0.52 (0.29-0.87) |
0.06 0.65 0.02 |
1.00 0.99 (0.73-1.36) 0.80 (0.56-1.13) 0.58 (0.30-1.14) |
0.97 0.21 0.11 |
| Insurance Status Private Medicare Medicaid Uninsured |
1.00 0.96 (0.69-1.35) 2.20 (1.61-2.93) 1.76 (1.24-2.51) |
0.81 <0.001 0.002 |
1.00 1.11 (0.74-1.67) 1.87 (1.29-2.71) 2.32 (1.48-3.64) |
0.62 <0.001 <0.001 |
| Language English Non-English |
1.00 0.85 (0.65-1.10) |
0.22 |
|
|
| Appointment at discharge No Yes |
1.00 0.63 (0.52-0.76) |
<0.001 |
1.00 0.89 (0.68-1.16) |
0.40 |
| Non-ophthalmic referrals at discharge No Yes |
1.00 2.05 (1.65-2.54) |
<0.001 |
1.00 1.73 (1.30-2.30) |
<0.001 |
| Ophthalmology consult No Yes |
1.00 1.06 (0.86-1.30) |
0.60 |
|
|
| Nonurgent ophthalmic condition No Yes |
1.00 1.14 (0.94-1.39) |
0.20 |
1.00 1.59 (1.23-2.03) |
<0.001 |
| Primary ophthalmic condition No Yes |
1.00 0.16 (0.11-0.24) |
<0.001 |
1.00 0.07 (0.03-0.15) |
<0.001 |
| Days from ED visit to follow-up ≤5 days >5 days |
1.00 3.16 (2.59-3.86) |
<0.001 |
2.71 (2.10-3.51) |
<0.001 |
| BCVA of affected eye Worse than 20/40 20/40 or better |
1.00 1.88 (1.47-2.43) |
<0.001 |
1.00 1.40 (1.04-1.90) |
0.027 |
| History of ophthalmology appointment in system No Yes |
1.00 0.75 (0.55-1.00) |
0.05 |
1.00 0.68 (0.47-0.99) |
0.045 |
| History of missed follow-up No Yes |
1.00 0.88 (0.62-1.22) |
0.45 |
||
| Travel time to follow-up (minutes) | 0.99 (0.99-1.00) | 0.13 | 0.99 (0.99-1.00) | 0.18 |
| Interpreter present if non-English speaker Yes No |
1.00 2.38 (1.58-3.71) |
<0.001 |
1.00 3.19 (1.84-5.78) |
<0.001 |
ED = Emergency department; BCVA = Best corrected visual acuity; CI = Confidence interval
Gender-stratified Predictors of Lost to Follow-up
The results of gender-stratified analysis are displayed in Supplemental Table 3 (Supplemental Material at AJO.com). Males who were uninsured, younger and with a visual acuity of 20/40 or better were significantly more likely to be LTFU while female counterparts in these demographics were not. Females who had multiple non-ophthalmic referrals on discharge were significantly more likely to be LTFU unlike males. The interaction term between gender and additional non-ophthalmic referrals on discharge was significant, males with multiple referrals were less likely to be LTFU (OR 0.55; 95% CI, 0.31-0.97; p=0.04).
ED Revisits
A total of 50 (2.2%) patients with scheduled ophthalmology appointments revisited the ED within 4 months of an index ED encounter for the same presenting condition. A significantly higher proportion of patients who were LTFU revisited the ED compared to patients who completed follow-up (5.7% vs. 1.1%; p<0.001). On logistic regression, patients who were LTFU were significantly more likely to revisit the ED even while controlling for factors significantly associated LTFU in multivariable regression (OR, 21.4; 95% CI, 4.31-179.36; p<0.001). The median length of time between the index ED encounter and an ED revisit was 10 days (mean 18.5, SD 16.5).
DISCUSSION
Our study examined LTFU ophthalmic care rates after an ED visit. We found that in a well-resourced tertiary care center, over a quarter of patients were LTFU after an eye-related ED presentation. We also identified several patient and clinical characteristics that were independently associated with LTFU. Notably, patients LTFU were significantly more likely to revisit the ED compared to those who completed follow-up.
Low rates of follow-up after ED discharge for various conditions have been extensively described in the literature, with estimates ranging from 40-70%.8,9,20–22 The proportion of patients who completed follow-up in our study (75%) exceeds reports from previous studies, including those examining ophthalmic follow-up rates,10,11 which may reflect specific characteristics of the study institution, such as the substantial availability of ophthalmology consultations and automated appointment telephone reminders. Additionally, patients who were referred for ophthalmic follow-up but did not receive or schedule an appointment were not included, which likely inflated the follow-up rate. Lastly, our ED follow-up window was longer in duration than prior studies. It is also possible that rates of follow-up are higher for ophthalmic complaints compared to other ED presentations, as patients may be more motivated to seek follow-up care when their vision is affected.23 Although the follow-up rates in our study are higher than in other conditions, and follow-up may not be crucial for all eye-related presentations, more than one quarter of patients recommended to receive follow-up ophthalmic care were LTFU. These findings suggest that ophthalmic follow-up completion rates still require improvement and further investigation, particularly given high rates of misdiagnoses of ophthalmic conditions in ED settings.4,5
The factors we found to be independently associated with LTFU were younger age, having Medicaid or being uninsured, an increased length of time between the ED visit and follow-up appointment, the presence of additional non-ophthalmic follow-up appointments after ED discharge, a non-urgent ophthalmic condition, a non-ophthalmic primary ED diagnosis and a BCVA of 20/40 or better in the affected eye. Younger age has been associated with decreased ED follow-up rates as well as nonadherence to diabetic retinopathy (DR) screening, and may reflect more restrictive employment schedules or a lower prioritization of seeking healthcare among patients in this demographic.24
Insurance status has also been strongly associated with adherence to follow-up care and was identified as the strongest predictor of failure to receive recommended eye examinations in a recent national cohort study.9,24–27 While uninsured patients in this study had access to medical fee assistance programs, they may have been unaware of the extent to which medical fees could be covered.28 Additionally, although the proportion of uninsured patients in Connecticut declined throughout the study period,29 LTFU rates in this study did not significantly decrease over time. It is possible that after the Affordable Care Act’s Medicaid expansion, uninsured patients became newly covered by Medicaid but experienced difficulties in understanding their health plan’s coverage, as has been reported in other states.30 This may partly contribute to a greater likelihood of LTFU among patients with Medicaid observed in this study. Furthermore, ophthalmologist appointments may be perceived as specialist care with potentially higher cost-sharing burdens among socioeconomically disadvantaged populations.31 Indeed, recent studies utilizing real-world data have found that deprivation, a metric encompassing many socioeconomic factors, is significantly associated with lower adherence to first-time DR screening and more severe symptoms of DR at the time of first presentation.32,33
Patients who had an appointment scheduled for more than 5 days after ED discharge were more likely to be LTFU, a finding consistent with prior literature.27 While longer lag time between ED discharge and follow-up may increase the likelihood that symptoms will self-resolve, patients with an appointment more than 5 days after discharge remained nearly 3 times more likely to be LTFU even after controlling for the urgency of the condition. This suggests that longer wait times may be a deterrent irrespective of the presenting condition.
Although the likelihood of LTFU was not significantly different between English and non-English speaking patients, the presence of an interpreter significantly increased the odds of follow-up for non-English speaking patients, corroborating previous work.34,35 Interpreters likely contributed to greater patient understanding of their condition and the importance of follow-up care. Patients for whom an ophthalmic condition was not the primary diagnosis upon ED presentation and those who had additional non-ophthalmic follow-up referrals to schedule at discharge were more likely to be LTFU. This may reflect the burden of care in the presence of multiple comorbidities. Clinically, patients with an urgent ocular condition or worse BCVA were less likely to be LTFU, which is unsurprising and suggest that the impact of a condition on a patient’s daily functioning strongly influences their motivation to seek care.
Younger males, those with visual acuity of 20/40 or better and uninsured males had a significantly higher risk of being LTFU while females in these categories did not. These results are suggestive of gender differences in the perceived necessity of follow-up. Indeed, a prior study utilizing real-world data found that men were more likely to present to an ophthalmologist for the first time with late glaucomatous disease compared to women, supporting the theory that gender differences in ocular care adherence may exist.36 Greater LTFU among men has also been reported in the context of other conditions.37 Of note, the interaction term between gender and non-ophthalmic referrals was significant, with females being more likely to be LTFU if provided with multiple other referrals. Future studies should continue to be aware of gender differences in barriers to access and uptake of health services that may be obscured in combined analysis.
In contrast to prior studies, we did not find that having an appointment scheduled prior to ED discharge was significantly associated with follow-up completion. It is possible that because appointments were provided by ED physicians or ophthalmologists, they may not have best represented patient availability. A Canadian study reported ophthalmology follow-up rates of 98% after the implementation of a streamlined scheduling system that allowed patients to personally schedule an appointment while still in the ED.27 Additionally, because all patients included in our study had scheduled appointments, patients who did not receive an appointment at discharge made their own appointments, likely reflecting motivation to seek follow-up care. This study’s results do not preclude the possibility that scheduling appointments prior to ED discharge is valuable for patients and follow-up attendance.
Our study estimated an overall 4-month revisit rate of 2.2% for ophthalmic conditions. While this revisit rate is lower than previous reports of ED revisit rates,3 we included only those patients re-presenting with the same diagnosis as recorded on the index ED visit who revisited after the date of their original scheduled follow-up appointment. Furthermore, it is possible that individuals may have revisited EDs outside of the YNHH system, although we would not expect this to have occurred at a different rate among those who completed follow-up compared to those LTFU. Therefore, our methodology likely underestimates true revisit rates. Importantly, those who were LTFU were at a significantly higher risk for a revisit compared to those who completed follow-up care. It is plausible that patients with ophthalmic follow-up were more likely to receive a correct diagnosis and appropriate treatment. Indeed, in a study of patients presenting to the ED with chest pain, follow-up with a cardiologist was associated with decreased subsequent hospitalizations.38 Our findings suggest that interventions to reduce LTFU after an ED encounter for an ophthalmic condition may also impact ED revisit frequency.
Identification of factors associated with LTFU can inform the development of targeted interventions to reduce the burden and frequency of LTFU. For instance, navigation services for patients who are uninsured, presenting with a non-ophthalmic primary diagnosis or have numerous follow-up appointments, all of which were associated with LTFU in this study, could be utilized to help reinforce patients’ ability to access follow-up care.39 Discharge documentation could also provide clear instructions for transportation options to access the clinic. Our study found that patients without previous appointments within our system were more likely to be LTFU and physical access to clinics has previously been reported to be a barrier to accessing eye care.31
Additionally, we identified a cutoff time of 5 days from a patient’s ED discharge to their date of follow-up appointment after which a patient’s odds of LTFU increased most significantly. While modification of appointment availability to prioritize ED follow-up patients can be a complex and unfeasible task for clinics, a patient-driven scheduling system may aid patients in establishing earlier appointments. For example, the implementation of a system that allows patients to identify their preferred follow-up appointment time prior to discharge from the ED would likely increase access to earlier appointments and or appointments that are more compatible with patients’ schedules. This is particularly important in ED settings where providers may lack access to outpatient scheduling and patients are often seen after outpatient clinic operating hours. Previous studies examining LTFU for chronic ophthalmic care have also suggested the utilization of monitoring systems.40 In the setting of ED follow-ups, a list of patients who have missed appointments and or have not yet completed follow-up within their recommended follow-up window could be collated into a list for automated or individualized telephone reminders. Clinically, more extensive counseling and education efforts could be provided to patients with visual acuity of 20/40 or better, to emphasize that their visual acuity may not be representative of the severity of their condition and their need to follow-up. This counseling could be provided by ophthalmologists as well as ED physicians in discharge conversations and documentation. Future work should assess how visual and health outcomes are impacted by LTFU after ED discharge. For example, studies could assess differences in treatment failure rates and visual acuity decline between patients LTFU and those who followed-up. Results from this research could help identify patients who may benefit the most from ophthalmic follow-up care after an ED visit.
There are several limitations to this study. First, encounters were limited to a single academic institution which may limit this study’s generalizability. However, the YNHH system is the dominant healthcare organization in the New Haven metropolitan area and New Haven has previously been reported as one of the most demographically representative cities in the United States.41,42 Furthermore, this study serves as an initial step for future multi-institutional or national studies to examine an important, previously un-investigated topic in the field of ophthalmology. A second limitation of this study is the categorization of primary diagnoses into urgent and non-urgent categories, which may over-generalize presenting ophthalmic conditions and is also subject to provider variation in knowledge and coding preferences. Third, in our efforts to exclude patients who might have followed-up with an ophthalmologist outside the YNHH system, we may have excluded patients who were instructed to follow-up but ultimately did not call to schedule an appointment. Future studies should consider utilizing claims-based databases to gather more comprehensive follow-up information for patients seeking care across multiple health system. Fourth, this study is limited in its retrospective nature of examination predicated largely on clinical records. Future prospective studies should examine the impact of other factors, which have been shown to impact follow-up adherence after ED visits as well as routine ophthalmic care, including patient knowledge of their condition, access to transportation, and occupational status.43 Finally, there may still have been a small subset of patients who followed-up with an unidentified outside ophthalmologist and were misclassified as LTFU.
In this study of a single academic institution, over a quarter of patients seen in the emergency department who were scheduled for follow-up ophthalmic care were LTFU. Patients who were younger, had Medicaid insurance or were uninsured, had additional non-ophthalmic referrals on discharge, a non-urgent ophthalmic condition, a primary diagnosis that was not an ophthalmic condition, better visual acuity in the ED and a longer period of time between the ED visit and the follow-up appointment were more likely to be LTFU, independent of the urgency of the presenting ophthalmic condition. Additionally, patients who were LTFU were significantly more likely to revisit the ED for the same condition within 4 months of the index visit compared to individuals who completed follow-up. Overall, our findings indicate that targeted interventions for high risk populations and modified referral practices may be needed to improve ED follow-up attendance. Reduction of LTFU rates for ophthalmic care may subsequently reduce the frequency of ED revisits and improve clinical outcomes for patients.
Supplementary Material
Highlights.
One quarter of patients were lost to follow-up after an eye-related ED visit
Several patient and ED factors were associated with loss to follow-up care
ED revisit rates were significantly higher among patients lost to follow-up
ACKNOWLEDGEMENTS/DISCLOSURES
a. Funding/Support: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number T35AG049685 and the Yale School of Medicine James G. Hirsch Endowed Medical Student Research Fellowship (Recipient: EC). The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental Material available at AJO.com
Financial Disclosures: No financial disclosures.
REFERENCES
- 1.Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of Eye-Related Emergency Department Visits. JAMA Ophthalmol. 2016;134(3):312–319. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. [DOI] [PubMed] [Google Scholar]
- 3.Duseja R, Bardach NS, Lin GA, et al. Revisit rates and associated costs after an emergency department encounter: a multistate analysis. Ann Intern Med. 2015;162(11):750–756. [DOI] [PubMed] [Google Scholar]
- 4.Alangh M, Chaudhary V, McLaughlin C, Chan B, Mullen SJ, Barbosa J. Ophthalmic referrals from emergency wards-a study of cases referred for urgent eye care (The R.E.S.C.U.E Study). Can J Ophthalmol. 2016;51(3):174–179. [DOI] [PubMed] [Google Scholar]
- 5.Yip H, Crock C, Chan E. Diagnostic error in an ophthalmic emergency department. Diagnosis (Berl). 2019. [DOI] [PubMed] [Google Scholar]
- 6.Obeid A, Su D, Patel SN, et al. Outcomes of Eyes Lost to Follow-up with Proliferative Diabetic Retinopathy That Received Panretinal Photocoagulation versus Intravitreal Anti-Vascular Endothelial Growth Factor. Ophthalmology. 2019;126(3):407–413. [DOI] [PubMed] [Google Scholar]
- 7.Elliott K, J WK, Basu A, Sabbatini AK. Transitional care clinics for follow-up and primary care linkage for patients discharged from the ED. Am J Emerg Med. 2016;34(7):1230–1235. [DOI] [PubMed] [Google Scholar]
- 8.Luckenbaugh AN, Yan PL, Dauw CA, Ghani KR, Hollenbeck BK, Hollingsworth JM. Followup Care after Emergency Department Visits for Kidney Stones: A Missed Opportunity. Urol Pract. 2019;6(1):24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magnusson AR, Hedges JR, Vanko M, McCarten K, Moorhead JC. Follow-up compliance after emergency department evaluation. Ann Emerg Med. 1993;22(3):560–567. [DOI] [PubMed] [Google Scholar]
- 10.Bizrah M, Yusuf A, Ahmad S. Adherence to Treatment and Follow-Up in Patients with Severe Chemical Eye Burns. Ophthalmol Ther. 2019;8(2):251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rizzuti AE, Vastardi M, Hajee M, Lazzaro DR. Scope of resident ophthalmology consultation service and patient follow-up rates at a level 1 trauma center in Brooklyn, New York. Clin Ophthalmol. 2013;7:643–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epic. Organizations on the Care Everywhere Network. Epic. https://www.epic.com/careeverywhere/. Published 2019. Accessed December 8, 2019.
- 13.Stagg BC, Shah MM, Talwar N, Padovani-Claudio DA, Woodward MA, Stein JD. Factors Affecting Visits to the Emergency Department for Urgent and Nonurgent Ocular Conditions. Ophthalmology. 2017;124(5):720–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keenum Z, McGwin G Jr., Witherspoon CD, Haller JA, Clark ME, Owsley C. Patients’ Adherence to Recommended Follow-up Eye Care After Diabetic Retinopathy Screening in a Publicly Funded County Clinic and Factors Associated With Follow-up Eye Care Use. JAMA Ophthalmol. 2016;134(11):1221–1228. [DOI] [PubMed] [Google Scholar]
- 15.Giraud T, Cura R, Viry M Interface Between R and the OpenStreetMap-Based Routing Service OSRM. CRAN. https://cran.r-project.org/web/packages/osrm/osrm.pdf. Published 2019. Accessed December 2, 2019. [Google Scholar]
- 16.OpenStreetMap Foundation. OpenStreetMap. OSMF. https://www.openstreetmap.org. Published 2019. Accessed December 2, 2019. [Google Scholar]
- 17.Berg KM, Demas PA, Howard AA, Schoenbaum EE, Gourevitch MN, Arnsten JH. Gender differences in factors associated with adherence to antiretroviral therapy. J Gen Intern Med. 2004; 19(11):1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daien V, Peres K, Villain M, Colvez A, Carriere I, Delcourt C. Visual acuity thresholds associated with activity limitations in the elderly. The Pathologies Oculaires Liees a l’Age study. Acta Ophthalmol. 2014;92(7):e500–506. [DOI] [PubMed] [Google Scholar]
- 19.Zou HL, Wang Y, Gang Q, Zhang Y, Sun Y. Plasma level of miR-93 is associated with higher risk to develop type 2 diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2017;255(6):1159–1166. [DOI] [PubMed] [Google Scholar]
- 20.Barlas D, Homan CS, Rakowski J, Houck M, Thode HC Jr. How well do patients obtain short-term follow-up after discharge from the emergency department? Ann Emerg Med. 1999;34(5):610–614. [DOI] [PubMed] [Google Scholar]
- 21.Kyriacou DN, Handel D, Stein AC, Nelson RR. BRIEF REPORT: Factors affecting outpatient follow-up compliance of emergency department patients. J Gen Intern Med. 2005;20(10):938–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naderi S, Barnett B, Hoffman RS, et al. Factors associated with failure to follow-up at a medical clinic after an ED visit. Am J Emerg Med. 2012;30(2):347–351. [DOI] [PubMed] [Google Scholar]
- 23.Welp A, Woodbury RB, McCoy MA, et al. Making Eye Health a Population Health Imperative: Vision for Tomorrow. In: (US) NAP, ed. Washington DC: National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Public Health Approaches to Reduce Vision Impairment and Promote Eye Health; 2016: https://www.ncbi.nlm.nih.gov/books/NBK402367/. [PubMed] [Google Scholar]
- 24.Eppley SE, Mansberger SL, Ramanathan S, Lowry EA. Characteristics Associated with Adherence to Annual Dilated Eye Examinations among US Patients with Diagnosed Diabetes. Ophthalmology. 2019;126(11):1492–1499. [DOI] [PubMed] [Google Scholar]
- 25.Asplin BR, Rhodes KV, Levy H, et al. Insurance status and access to urgent ambulatory care follow-up appointments. JAMA. 2005;294(10):1248–1254. [DOI] [PubMed] [Google Scholar]
- 26.Blanchard J, Ogle K, Thomas O, Lung D, Asplin B, Lurie N. Access to appointments based on insurance status in Washington, D.C. J Health Care Poor Underserved. 2008;19(3):687–696. [DOI] [PubMed] [Google Scholar]
- 27.Messina FC, McDaniel MA, Trammel AC, Ervin DR, Kozak MA, Weaver CS. Improving specialty care follow-up after an ED visit using a unique referral system. Am J Emerg Med. 2013;31(10):1495–1500. [DOI] [PubMed] [Google Scholar]
- 28.Cunningham PJ, Hadley J, Kenney G, Davidoff AJ. Identifying affordable sources of medical care among uninsured persons. Health Serv Res. 2007;42(1 Pt 1):265–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaiser Family Foundation. Connecticut: Health Coverage & Uninsured. KFF. https://www.kff.org/state-category/health-coverage-uninsured/?state=CT. Published 2020. Accessed January 2, 2020. [Google Scholar]
- 30.Nardin R, Zallman L, Sayah A, McCormick D. Experiences applying for and understanding health insurance under Massachusetts health care reform. Int J Equity Health. 2016;15(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Owsley C, McGwin G, Scilley K, Girkin CA, Phillips JM, Searcey K. Perceived barriers to care and attitudes about vision and eye care: focus groups with older African Americans and eye care providers. Investigative ophthalmology & visual science. 2006;47(7):2797–2802. [DOI] [PubMed] [Google Scholar]
- 32.Yusuf R, Chen EM, Nwanyanwu K, Richards B. Neighborhood Deprivation and Adherence to Initial Diabetic Retinopathy Screening. Ophthalmology Retina. 2020;4(5):550–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Denniston AK, Lee AY, Lee CS, et al. United Kingdom Diabetic Retinopathy Electronic Medical Record (UK DR EMR) Users Group: report 4, real-world data on the impact of deprivation on the presentation of diabetic eye disease at hospital services. The British journal of ophthalmology. 2019;103(6):837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernstein J, Bernstein E, Dave A, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J Immigr Health. 2002;4(4):171–176. [DOI] [PubMed] [Google Scholar]
- 35.Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med. 2000;15(4):256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crabb DP, Saunders LJ, Edwards LA. Cases of advanced visual field loss at referral to glaucoma clinics - more men than women? Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017;37(1):82–87. [DOI] [PubMed] [Google Scholar]
- 37.Edwards P, Fernandes J, Roberts I, Kuppermann N. Young men were at risk of becoming lost to follow-up in a cohort of head-injured adults. Journal of clinical epidemiology. 2007;60(4):417–424. [DOI] [PubMed] [Google Scholar]
- 38.Czarnecki A, Chong A, Lee DS, et al. Association between physician follow-up and outcomes of care after chest pain assessment in high-risk patients. Circulation. 2013;127(13):1386–1394. [DOI] [PubMed] [Google Scholar]
- 39.Horwitz SM, Busch SH, Balestracci KM, Ellingson KD, Rawlings J. Intensive intervention improves primary care follow-up for uninsured emergency department patients. Acad Emerg Med. 2005;12(7):647–652. [DOI] [PubMed] [Google Scholar]
- 40.Davis A, Baldwin A, Hingorani M, Dwyer A, Flanagan D. A review of 145 234 ophthalmic patient episodes lost to follow-up. Eye (London, England). 2017;31(3):422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The Impact of Yale-New Haven Health System’s Expansion. 2015. [Google Scholar]
- 42.Kolko J ‘Normal America’ Is Not A Small Town Of White People. FiveThirtyEight. https://fivethirtyeight.com/features/normal-america-is-not-a-small-town-of-white-people/. Published 2016. Accessed January 7, 2019.
- 43.Thompson AC, Thompson MO, Young DL, et al. Barriers to Follow-Up and Strategies to Improve Adherence to Appointments for Care of Chronic Eye Diseases. Investigative ophthalmology & visual science. 2015;56(8):4324–4331. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


