Abstract
Objective:
We and others have found that couples’ sleep is a shared and dyadic process. Couples’ sleep-wake concordance (whether couples are awake or asleep at the same time) is associated with couples’ relationship factors; however, we know little of the temporal associations between concordance and daily relationship characteristics. The purpose of this study was to examine daily positive and negative interpersonal interactions to determine how they predict, and are predicted by, nightly sleep-wake concordance.
Method:
Participants were 48 heterosexual couples between 18–45 years of age who shared a bed with their spouse. Couples completed questionnaires and daily assessments of positive and negative interactions. Each member of the dyad wore wrist actigraphs for 10 days. Sleep-wake concordance was calculated as the percentage of time couples were awake or asleep throughout the night at one-minute intervals. Multilevel modeling with lagged effects determined bidirectional and lagged associations between concordance and couples’ daily interactions.
Results:
Couples had more negative interactions than their usual following nights with higher concordance than their usual (but not vice versa) and this was more pronounced for well-adjusted couples. In contrast, across all couples, more positive interactions and perceived warmth and support from partners was associated with higher concordance.
Conclusions:
Our findings demonstrate that the valence of sleep-wake concordance depends on relationship quality characteristics (e.g., marital adjustment). Future research on relationships, sleep, and health should consider couples’ shared sleep behaviors as one mechanism by which relationships are associated with long-term health outcomes.
Keywords: couples, sleep, daily interactions, health, coregulation, actigraphy
Social relationships are strongly linked to health (1). Marital relationships likely have an even greater impact on health because they are a primary and daily source of positive (i.e., supportive) and negative (i.e., conflict) interpersonal interactions (2). The subsequent psychophysiological and behavioral responses that accompany those interactions (3) can have long-term downstream consequences (4). Couples’ relationships are also uniquely poised to influence health as a function of attachment to one another. That is, due to their shared, emotional bond, couples exhibit co-regulated physiological processes in biological systems such as within the cardiovascular and endocrine systems (5, 6). We, and others, posit that sleep systems may also be co-regulated (6) and that one way to quantify this is by observing the degree to which couples are awake and asleep at the same time (i.e., sleep-wake concordance; 7). However, it is not yet known whether daily marital functioning influences, and is influenced by, sleep-wake concordance. Determining whether and how marital functioning contributes to sleep coregulation is an important next step to understanding how relationships contribute to health outcomes.
Sleep is often studied as an individual phenomenon; however, survey data suggests that nearly 90% of partnered individuals share a bed (8). More recent evidence suggests that in addition to being a shared behavior, assessments of sleep at the dyadic level demonstrate co-regulatory patterns (6). For example, couples’ diary-assessed sleep duration covaried across eight nights; when women’s sleep duration was longer or shorter than their usual, so was their male partners (9). Likewise, self-reported sleep quality ratings covaried across days between partners (9). Actigraphic evidence also indicates that sleep in one partner is related to sleep in the other partner (10) and that couples’ sleep is concordant in minute-to-minute epochs throughout the night, more so than would be expected by chance (7).
It is currently unknown whether higher levels of sleep-wake concordance are indicative of “healthy” relationship functioning or portend health benefits more broadly, as current data are somewhat mixed. For example, sleep-wake concordance was linked to more attachment anxiety in the context of low marital satisfaction (7). This suggests that higher sleep-wake concordance can be a negative indication of the couples’ emotional bond. However, recent evidence suggests that there are positive associations with couples’ concordance; more sleep-wake concordance was linked to lower c-reactive protein in men and women and lower nighttime blood pressure in women (11). In one of the only prospective studies of couples’ concordance in sleep timing, for women, lower concordance in sleep onset (whether assessed by diary or actigraphy) predicted negative marital interactions the following day (12).
The ambiguities of co-regulation are not unique to sleep processes. Co-regulated heart-rate variability, an index of emotion regulation (13), predicted higher inflammation and more negative affect during conflict in couples (14); however, emotional synchrony in other non-stressful contexts could be related to greater partner attunement (e.g., responsiveness to other person; 5). In their review, Timmons and colleagues report that coregulation varies across systems and that whether coregulation is “good” or “bad” likely depends on several contextual factors including emotional context (negative, positive, or neutral interactions) and the degree of relationship satisfaction (5). Thus, expanding on the current literature to explore positive and negative marital interactions in more detail could provide more clarity on the valence of sleep-wake concordance.
To that end, greater specificity in how couples’ day-to-day relationship experiences track with night-to-night sleep-wake concordance facilitates understanding of how dynamic relationship processes are linked to sleep. Limited findings on associations between individually-assessed sleep and couples’ relationship characteristics suggest that sleep at the level of the dyad would also influence, and be influenced by, relationship characteristics. Sleep influences cognitive processing and could increase emotional reactivity (15). Thus, individuals in relationships may be more prone to more relationship difficulties following a poor night of sleep (16). On the other hand, sleep may be sensitive to disruptions in interpersonal security (17, 18). Indeed, conflict between partners predicted elevated anxiety and less time asleep in bed (19).
The purpose of the current study is to extend upon theories of coregulation in couples (6), and in particular, to test how couples’ shared sleep experience is associated with changes in interpersonal context (5). In this study, coregulation is operationalized as actigraphy-assessed night-to-night sleep-wake concordance. The couples’ interpersonal context is captured via 10 daily ratings of positive and negative interactions. Daily ratings reflect day-to-day fluctuations that might not be apparent in aggregate measures of positive and negative relationship characteristics (e.g., (14)). Bidirectional associations between sleep-wake concordance and positive and marital interactions are expected because individually-assessed sleep parameters predict, and are predicted by relationship characteristics (e.g., 16, 19). However, given that the valence of sleep-wake concordance is unclear (e.g., 7, 11, 12), there is no a priori hypothesis regarding directionality or strength of associations (e.g., that positive marital interactions would more strongly predict more sleep-wake concordance). Similar associations are expected among concordance and couples’ positive and negative marital interactions, on average, across days (between couples’ level).
In addition to the above, we test global relationship characteristics and sleep parameters that could influence associations between sleep-wake concordance and daily positive and negative experiences. For example, the effects of negative interactions may be mitigated in well-adjusted and secure couples. In addition, concordant couples who report poor sleep quality or wakefulness may be more likely to have negative interactions due to insufficient or poor sleep that is shared by the couple. Finally, women and men may differ in reporting negative marital interactions and how they are affected by sleep concordance (e.g., 11, 12). We therefore test whether gender moderates significant bidirectional and lagged associations. Based on previous findings (12), we predict that associations between negative and positive marital interactions and sleep-wake concordance would be stronger for women than men.
Methods
Participants
The University of Pittsburgh Biomedical Institutional Review Board approved this study. All participants provided written, informed consent. Participants were 48 heterosexual couples from a study focused on sleep and relationship characteristics and cardiovascular health (HL093220). Healthy, married individuals were recruited from the community via flyers and advertisements. Participants were between 18–45 years of age and shared a bed with their spouse at least four nights a week. They underwent a diagnostic interview and an in-home, screening night using a two-channel apnea screening device (ApneaLink 2™; ResMed Corporation, Poway, California) to rule out Obstructive Sleep Apnea (OSA). Participants with an Apnea-Hypopnea Index (AHI) > 10 were excluded. Additional exclusionary criteria were having a current sleep disorder, night-shift work, current psychiatric illness, pregnancy, substance dependence, cardiovascular or renal disease. Participants were also excluded if they took prescription medications known to affect sleep or the autonomic nervous system.
Procedure
Each member of the couple completed questionnaires about their relationship at the initial visit and answered daily questions about positive and negative marital interactions via an electronic diary for 10 days. Each participant also wore a wrist actigraph for 10 days. They were instructed to press a marker on the watch to indicate when they were getting into bed and attempting to sleep and when they were getting out of bed and no longer attempting to sleep. Couples also maintained separate daily sleep diaries to track bedtime, wake time, wake after sleep onset, naps, etc.
Measures
Actigraphy
Participants wore actiwatches (Actiwatch 64, Philips Respironics, Bend, OR) which include an accelerometer that records movement. Sleep was determined in 60-second epochs using the scoring algorithm in Actiware Version 5.70.1, Philips Respironics, Bend, OR). The threshold for movement counts for this study was set at a “medium” sensitivity of 40 (i.e., if movement counts are <40, the epoch is labeled sleep). Sleep onset is determined by 10 consecutive epochs of sleep during a set rest interval. Sleep offset is determined by 10 consecutive epochs of wake during the rest interval. Rest intervals were determined by a scorer via event markers. Event markers were set by the participants to denote when they were in bed and attempting to sleep and when they were out of bed upon awakening. If the event marker was not pressed or was inaccurate (which occurred <1% of the time), diary entries were used to set the rest interval.
To ensure synchronized timing, watches were programmed on the same computer at the start of the study. Sleep-wake concordance was calculated from the actigraphy data and has been described in detail in two previous studies (7, 11). Briefly, sleep-wake concordance is the percentage of time that couples are both awake or asleep throughout the night at one-minute intervals. The percentage is calculated by dividing the number of concordant epochs by the total number of epochs for that night [(concordant epochs/total epochs)*100]. Concordance was evaluated based on the earliest bedtime and the latest wake time within the dyad. Over the 10 days, concordance ranged from 54% to 88% (M = 74.8, SD – 7.22). On average, concordance for sleep represents 66% of concordant epochs.
Marital interactions
Positive and negative ratings of marital interactions were rated once daily on a scale from 0 (very little) to 100 (very much). Positive ratings of interactions included four items such as, “During today’s interactions with your spouse to what extent did you feel valued by your spouse” and “During today’s interactions with your spouse to what extent did you feel close to your spouse”. Cronbach’s alpha for the positive interaction scale was .86. Negative ratings included four items such as “During today’s interactions with your spouse, to what extent did you feel criticized” and “During today’s interactions with your spouse, to what extent did you feel dismissed.” Cronbach’s alpha for the negative interactions scale was also .86. Positive and negative items were each summed and divided by the number of items in that scale to create daily positive and negative composite scores that ranged from 0 to 100. Higher scores on each composite score indicate more negative or positive evaluations of the interactions. On average couples reported more positive than negative interactions (Table 1).
Table 1.
Means and Standard Deviations of Descriptives and Study Variables
| Women | Men | |
|---|---|---|
| Age | 30.55 (6.07) | 31.33 (5.83) |
| BMI | 24.00 (5.51) | 26.38 (6.65) |
| Daily positive interactions | 69.50 (20.98) | 70.60 (20.10) |
| Daily negative interactions | 14.72 (16.51) | 16.16 (16.59) |
| Support and affection toward partner | 61.11 (19.78) | 61.66 (17.56) |
| Support and affection from partner | 62.92 (17.46) | 59.74 (18.00) |
| Daily diary sleep quality | 64.18 (21.65) | 66.62 (20.46) |
| Daily Actigraphy Assessed WASO (minutes) | 58.24 (39.08) | 59.33 (43.70) |
| Marital Adjustment* | 121.81 (12.15) | 121.40 (10.91) |
| Anxious Attachment* | 2.98 (1.02) | 2.68 (0.92) |
| Avoidant Attachment* | 1.68 (.83) | 1.74 (.74) |
Previously reported; Values represent means (standard deviations); BMI = body mass index; WASO = Wake after sleep onset; Daily positive and negative interactions were rated on a scale of 0 – 100 where higher numbers indicate more positive and negative ratings, respectively; Daily diary sleep quality were rated on 0–100 scale where higher ratings indicate better sleep quality; Anxious and avoidant attachment scores were averaged and rated on a 7-point scale, higher scores indicate more anxious and avoidant attachment, respectively.
Partners also rated three items to determine how much tangible support and affection they provided to their spouse overall? (e.g., Did you express affection towards your spouse?) and three items to determine tangible support and affection they received from their spouse (e.g., Did your spouse do you a favor?). Each item was rated from 0 (very little) to 100 (very much) and averaged to yield a composite evaluation of support and affection to and from the spouse (Table 1). Cronbach’s alphas for support to spouse and support from spouse were .77 and .79, respectfully.
Moderators
Relationship characteristics.
As previously reported (7, 11), couples in this study also rated their individual attachment style and marital quality. Anxious and Avoidant attachment styles were assessed with the Experiences in Close Relationships (ECR) inventory (20). It is a 36-item scale with 18 items that assess avoidance and anxiety in close relationships. Items are rated from 1 (strongly agree) to 7 (strongly disagree). Each subscale is averaged and higher scores indicate a tendency towards more anxious or avoidant styles. Marital Quality was assessed with the Dyadic Adjustment Scale (21). Higher scores on this scale indicate couples are highly adjusted and have cohesion and consensus on important matters in the relationship. As previously reported (7, 11), all relationship measures had good internal reliability in this sample (α’s ≥ .86).
Sleep measures.
Each individual in the study rated his or her sleep quality from 0 (very bad) to 100 (very good) each morning in response to the item, “The quality of my sleep last night was…” Each individual’s wake after sleep onset (WASO) was calculated as the total number of minutes awake after sleep onset and before final wake time as assessed by actigraphy.
Covariates
Sociodemographic characteristics that are associated with individual sleep characteristics and marital interactions were entered as covariates in all models. Specifically, age (in years), body mass index (BMI), gender (1=male, vs. 0=female), race (1=nonwhite, vs. 0=white), education (1=less than high school, 2=high school graduate, 3=technical school, 4=some college, 5=college degree, 6=some post-graduate work, 7=post-graduate degree), years married (1= < 1year, 2= 1–4 years, 3= 5–10 years, 4= 11–14 years, 5= 15+ years), and whether children lived at home (yes/no) were all included. In addition, individuals’ average sleep quality as well as nightly sleep quality were included. We also controlled for previous day’s marital interactions in models predicting next day marital interactions (or previous night’s sleep concordance in models predicting tonight’s sleep concordance). All continuous covariates were centered at the sample means.
Statistical Analyses
We used multilevel modeling with lagged effects in SAS version 9.4 to take into account clustered data structure, such that a total of 960 daily observations were clustered around 96 partnered individuals (48 couples × 2 individuals × 10 days). We used only daily observations when individuals indicated that they shared a bed with their spouse; this resulted in 820 daily observations in models examining previous night’s sleep concordance → next-day marital interactions and 880 daily observations in models examining today’s marital interactions → same night sleep concordance. Since the use of lagged variables excludes the first day’s observation, a total of 730–746 daily observations were used in the analyses.
Sleep-wake concordance is a between-couples predictor (individuals in a dyad had the same value each night), which precludes use of dyadic modeling to account for potential interdependence in the data. However, the risk of committing a Type I error increases significantly when correlations within dyads are about .45 (22, 23). Intraclass correlations for all four daily marital interactions variables ranged from .20 to .43. Thus, to test our hypotheses about the temporal association between nightly sleep-wake concordance and daily marital interactions, variances for key measures were decomposed to level-1 (daily) and level-2 (person) levels. Because all participants were couples and the main variables of interest (i.e., sleep-wake concordance and marital interactions) reflect couple-level behaviors, we interchangeably used “persons” and “couples” for easier interpretation. Level-1 variables were centered at the person mean, such that positive values indicate scores higher than the participant’s own cross-day average. Level-2 variables were centered at the sample mean, such that positive values indicate higher scores than others in the sample.
Results
Descriptive Results
About 20% of couples were married less than one year; 45% of couples were married between one and four years; 17% were married between 5 and 10 years and 14% of couples were married more than 10 years. Most of the sample self-identified as White (79.3%). About 90% of the sample had some college education or beyond. The remainder of the sample had technical training and/or completed high school. Most of the couples did not have children (62%) and the remainder had between one and four children. Additional relevant descriptives are in Table 1.
The Effects of Sleep-Wake Concordance on Daily Marital Interactions
Table 2 presents results from multilevel models of four marital interactions predicted by sleep-wake concordance. A significant temporal association was found in the sleep concordance—negative marital interaction relationship. Greater sleep-wake concordance on the previous night was associated with higher negative marital interactions the following day. This effect was evident after controlling for the effects of previous day’s negative marital interactions and sociodemographic covariates (none of them were significant at p < .05) as well as significant effects of previous night’s and average sleep quality (better sleep quality predicted fewer negative interactions). Average sleep-wake concordance across days was not associated with average negative marital interactions.
Table 2.
Sleep-wake concordance predicting marital interactions
| Negative interactions | Positive interactions | Support and affection toward partner | Support and affection from partner | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | B | SE | p | |
| Fixed Effects | ||||||||||||
| Sleep-wake concordance | ||||||||||||
| Previous night’s | .16 | .07 | .013 | −.03 | .07 | .71 | .002 | .08 | .98 | −.07 | .09 | .49 |
| Average | −.09 | .18 | .60 | .42 | .24 | *.077 | .34 | .31 | .27 | .55 | .30 | *.069 |
| Random Effects | ||||||||||||
| Intercept | 92.42 | 18.31 | <.001 | 181.38 | 32.71 | <.001 | 318.77 | 55.59 | <.001 | 271.99 | 50.44 | <.001 |
| Residual | 173.28 | 9.61 | <.001 | 189.96 | 10.54 | <.001 | 257.73 | 14.29 | <.001 | 361.48 | 20.24 | <.001 |
Note. Bold = p < .05,
= p < .10; All models adjusted for individuals’ age, gender, race, education, years married, whether children lived at home, previous day’s marital interaction, and previous night’s and average sleep quality. Models included bed sharing nights only.
There were no temporal associations of sleep-wake concordance with positive interactions, or support and affection to the partner. However, average sleep-wake concordance was marginally associated with more overall positive interactions and with receiving more support and affection from the partner (p = .077, p = .069, respectively). Average sleep-wake concordance was not associated with overall support and affection towards the partner.
The Effects of Daily Marital Interactions on Sleep-Wake Concordance
Table 3 shows results from multilevel models of the reverse direction. There was no significant temporal association between today’s marital interactions, support and affection between partners, and sleep concordance on the same night. However, across days, positive marital interactions, and receiving more support and affection from the partner were associated with higher sleep wake concordance on average (p = .015, p = .009, respectively). That is, couples who reported more positive interactions with their partner and providing more affection and support to and from one’s partner had higher sleep-wake concordance overall. Higher average support and affection towards the partner was also marginally associated with higher sleep-wake concordance overall (p = .061). Negative marital interactions overall were not predictive of sleep-wake concordance overall (Table 3).
Table 3.
Marital interactions predicting sleep-wake concordance
| Sleep-wake concordance | |||
|---|---|---|---|
| B | SE | p | |
| Fixed Effects | |||
| Negative interactions | |||
| Today’s | −.02 | .02 | .29 |
| Average | −.03 | .07 | .66 |
| Random Effects | |||
| Intercept | 33.12 | 6.46 | <.001 |
| Residual | 60.73 | 3.38 | <.001 |
| Fixed Effects | |||
| Positive interactions | |||
| Today’s | .01 | .02 | .64 |
| Average | .12 | .05 | .015 |
| Random Effects | |||
| Intercept | 30.66 | 6.07 | <.001 |
| Residual | 60.40 | 3.34 | <.001 |
| Fixed Effects | |||
| Support and affection toward partner | |||
| Today’s | .02 | .02 | .20 |
| Average | .07 | .04 | *.061 |
| Random Effects | |||
| Intercept | 32.36 | 6.29 | <.001 |
| Residual | 60.19 | 3.33 | <.001 |
| Fixed Effects | |||
| Support and affection from partner | |||
| Today’s | .0004 | .02 | .98 |
| Average | .10 | .04 | .009 |
| Random Effects | |||
| Intercept | 30.00 | 5.96 | <.001 |
| Residual | 60.80 | 3.38 | <.001 |
Note. Bold = p < .05
= p < .10; All models adjusted for individuals’ age, gender, race, education, years married, whether children lived at home, previous night’s sleep concordance level, and previous night’s and average sleep quality. Models included bed sharing nights only.
Post-hoc analyses
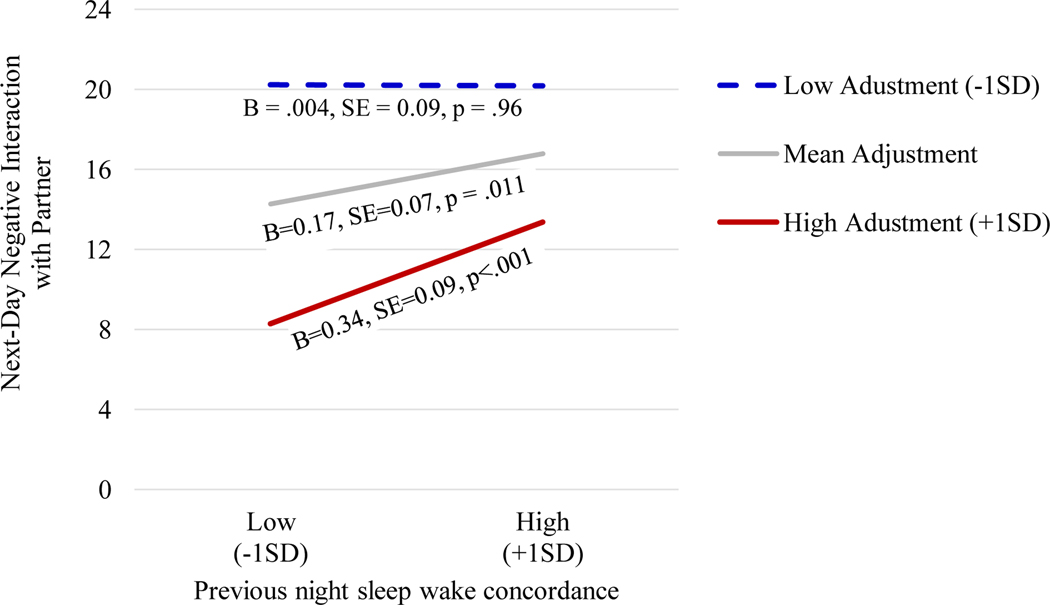
Moderation of significant effects were tested in in post-hoc analyses. There was a significant interaction between previous night’s sleep concordance and marital adjustment predicting next-day negative marital interactions (B = .01, SE = .01, p = .005). As demonstrated in Figure 1, when couples had higher sleep-wake concordance than was typical for them, they had more negative interactions the following day (B = .17, SE = .07, p = .011). This effect was stronger in highly adjusted couples (1 SD above from the mean; see black line, Figure 1) than in couples with low adjustment ratings (1 SD below from the mean; see dashed line, Figure 1). The slope for highly adjusted couples was significant (B = .34, SE = .09, p < .001), but the slope for low adjustment couples was not significant (B = .004, SE = .09, p = .96). There was no significant moderation by attachment styles. We also tested potential differences by gender, previous night’s self-reported sleep quality or WASO but these were not significant moderators.
Figure 1.
Interaction between sleep-wake concordance and adjustment on next-day negative interactions. Note. The interaction between previous night’s sleep concordance and marital adjustment predicting next-day negative marital interactions (B = .01, SE = .01, p = .005). The model adjusted for individuals’ age, gender, race, education, years married, whether children lived at home, previous night’s sleep concordance level, previous night’s and average sleep quality, and the main effect of marital adjustment (B = −.35, SE = .10, p < .001). Model included bed sharing nights only.
Discussion
To our knowledge, this is the first study to examine couples’ day-to-day marital interactions and their association with sleep at a dyadic level. Temporal findings of sleep-wake concordance and daily marital interactions add specificity to the current literature on marital relationships, co-regulation, and health. In particular, we found that previous night’s sleep-wake concordance predicted more negative marital interactions the following day (but not vice versa). This effect was more pronounced for couples with better marital quality (more highly adjusted) couples. Bidirectional findings emerged when examining average interactions and sleep-wake concordance across days. Couples with more positive interactions, or those who experienced more warmth and affection from their partner, had higher sleep-wake concordance overall. There was also a trend for higher sleep-wake concordance when partners had more warmth and affection toward their partner overall. When examining the reverse direction, higher sleep wake concordance predicted positive interactions and receiving more affection and support from the partner. Thus, findings on nightly sleep-wake concordance and daily positive and negative interactions varied when looking within couples versus between couples over 10 days’ time.
This study reveals that the valence of sleep-wake concordance and its association with couple relationship functioning can be both positive and negative. On average, positive interactions and receiving more support and affection from partners significantly predicted higher sleep-wake concordance. The reverse pattern (higher sleep-wake concordance predicting more positive interactions and support and affection) emerged, albeit at a trend level. This suggests that better relationship functioning more strongly predicts higher sleep-wake concordance than the reverse. However, at the within-person level, higher sleep-wake concordance was associated with more negative interactions the following day. It is possible that couples may attempt to exert control over their own and their partner’s bedtime and wake time when they have stressful events scheduled on the next day (e.g., 24). As stressful days usually involve more negative couple interactions, this may explain the higher sleep-wake concordance and more negative interactions found in this study. Over time, the accumulation of day-to-day sleep-wake concordance and negative interactions may contribute to building high intimacy, more support exchanges, and strong relationships (25).
To that end, we also found that the link between higher sleep-wake concordance and more negative marital interactions the next day was more pronounced for highly adjusted couples. That is, when highly adjusted couples had higher concordance than their average, they had more than their average number of negative interactions the following day. This finding was not explained by poor sleep quality ratings or wake after sleep onset, and thus, does not appear to be due to concordance on a night of poor sleep. In their review of couples’ coregulation (“physiological linkage”) of other biological systems (e.g., hypothalamic-pituitary adrenal axis and sympathetic nervous system), Timmons and colleagues suggest that the valence of coregulation can vary (5). For example, coregulation of stress response systems (e.g., HPA) could be indicative of negative relationship characteristics and too much coregulation could escalate conflict (5). This is because coregulation is a reciprocal process for maintaining psychophysiological homeostasis (6). Our findings suggest that when well-adjusted couples have more concordance than is typical, they may be more negatively attuned the following day. However, it is important to examine other contextual factors (e.g., budding conflict within couples, time pressure, work schedules, differing circadian preferences) and how couples jointly negotiate nightly sleep behaviors that influence concordance (e.g., bedtime, light out, wake time, etc.). For example, couples in high quality relationships may be better able to engage in approach tactics, as opposed to avoidance tactics, and, as mentioned above, coordinate their sleep timing in anticipation of challenging days (24). It is also possible that when couples have higher than their usual sleep-wake concordance, it is because of higher than usual social control from one partner. Negative social control can lead to negative affective responses in the other partner (26), which could, in turn, lead to more negative marital interactions the following day. It will be important to continue to explore within-couple fluctuations via daily diaries and ecological momentary assessments to better understand instances in which higher sleep-wake concordance lead to more negative interactions the following day.
Associations between marital interactions and concordance should be considered in light of methodological limitations. The relatively small sample of dyads in the current study comprised male-female partners who were satisfied in their marriages. Moreover, self-rated attachment and avoidance anxiety was low for most individuals in the study. Same-sex relationships, insecure attachment, and low relationship satisfaction could demonstratively weaken or strengthen associations between daily relationship characteristics and concordance. For example, insecurely attached individuals who are unsatisfied in their relationship could have even more negative interactions following concordant sleep, but not have the benefit of resolution and intimacy. Couples in this study were also free from sleep disorders that negatively affect cohabitating relationships (e.g., shiftwork disorder, sleep apnea) and influence bedsharing habits. It is likely that bedsharing is influenced by daily interactions; and vice-versa however, this study recruited couples who routinely share a bed and analyses included bedsharing nights only. In future studies it will be important to recruit more couples who also have diverse bed-sharing practices due to children, disturbed sleep, work schedules, or travel. For example, recent findings on minute-to-minute awakenings throughout the night suggest that chronotype (“owl” versus “lark”) could influence the degree to which couples are concordant for sleep (27).
Future studies on sleep in couples will also want to consider methodological approaches to account for inherent interdependence within dyads. Intraclass correlations were within recommended ranges to conduct analyzes at the person level. We additionally conducted analyses stratified by gender to account for interdependence, which resulted in loss of power (S1). When dyads have unique concordance values (e.g., Walters et al., (27)), it is possible to employ alternative statistical approaches that have more power than stratified models (e.g., Actor Partner Interdependence Modeling). With APIM, one can examine, for example, the extent to which one’s unique sleep concordance value influences his/her own and the other partner’s reports of marital interaction.
An additional methodological consideration in dyadic sleep research is the possibility that associations between concordance and marital functioning vary by workdays versus free days. The current study was limited to 10 days which was insufficient for examining lagged associations on non-workdays. Moreover, participants were not instructed to specify whether it was indeed a workday. Future studies would benefit from 14 or greater days of data collection and greater specificity of workday activities. Indeed, a prolonged and continued focus on dyadic sleep behaviors in the context of day-to-day, and night-to-night living will provide further insight into couples’ relationships and health.
Conclusion
We extend previous cross-sectional work in couples’ sleep by examining whether sleep-wake concordance (as one measure of coregulation) predicted, and was predicted by, daily positive and negative interactions. An examination of daily sleep-wake concordance and marital interactions allowed for assessments of within-couple variation in concordance and positive and negative interactions in addition to patterns over a 10-day period. This study contributes to the larger literature on couple-level coregulation in emotions and stress physiology (28, 29). We found that sleep-wake concordance is both positively and negatively associated with couples’ daily interactions. Similar to other findings on coregulation in couples (see 5 for review), our findings demonstrate that the valence of coregulatory processes likely depends on other nuances in the relationship context (e.g., degree of marital adjustment/quality). Findings also strengthen existing theory (30, 31) that sleep, especially when examined at the dyadic level, can be both a barometer of couples’ relationship functioning and an influencer of couples’ relationship functioning. Thus, our findings, along with the growing literature on couples’ relationships and sleep, support further research into sleep as a mechanism by which couples’ relationships are associated with health outcomes.
Supplementary Material
Acknowledgement
The authors wish to thank Mary Fletcher and Jean Miewald for their assistance with data management.
Grant support:
Funding for the current study was provided by National Heart Lung and Blood Institute K23HL093220 (PI: Wendy M. Troxel). Support for Dr. Gunn was provided by National Heart and Blood Institute T32 HL082610 (PI: Daniel J. Buysse). Support for Dr. Troxel was also provided by National Heart Lung and Blood Institute HL122460 (PI: Wendy. M. Troxel).
Footnotes
Conflicts of Interest
Outside of the current work, Orfeu M. Buxton discloses that, in the last 3 years, he received subcontract grants to Penn State from Proactive Life LLC (formerly Mobile Sleep Technologies) doing business as SoundScape (NSF/STTR #1622766, NIH/NIA SBIR R43-AG056250, R44-AG056250), received honoraria/travel support for lectures from Boston University, Boston College, Tufts School of Dental Medicine, New York University and Allstate, and receives an honorarium for his role as the Editor in Chief of Sleep Health (sleephealthjournal.org).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. PLOS Medicine. 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robles TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. Physiol Behav. 2003;79(3):409–16. [DOI] [PubMed] [Google Scholar]
- 3.Pietromonaco PR, Collins NL. Interpersonal mechanisms linking close relationships to health. Am Psychol. 2017;72(6):531–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital Quality and Health: A Meta-Analytic Review. Psychological Bulletin. 2014;140(1):140–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timmons AC, Margolin G, Saxbe DE. Physiological linkage in couples and its implications for individual and interpersonal functioning: A literature review. J Fam Psychol. 2015;29(5):720–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sbarra DA, Hazan C. Coregulation, dysregulation, self-regulation: an integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Pers Soc Psychol Rev. 2008;12(2):141–67. [DOI] [PubMed] [Google Scholar]
- 7.Gunn HE, Buysse DJ, Hasler BP, Begley A, Troxel WM. Sleep Concordance in Couples is Associated with Relationship Characteristics. Sleep. 2015;38(6):933–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Sleep Foundation. Sleep in America Bedroom Poll. www.sleepfoundation.org 2011. [Google Scholar]
- 9.Lee S, Martire LM, Damaske SA, Mogle JA, Zhaoyang R, Almeida DM, et al. Covariation in couples’ nightly sleep and gender differences. Sleep Health. 2018;4(2):201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pankhurst FP, Horne JA. The influence of bed partners on movement during sleep. Sleep. 1994;17(4):308–15. [DOI] [PubMed] [Google Scholar]
- 11.Gunn HE, Buysse DJ, Matthews KA, Kline CE, Cribbet MR, Troxel WM. Sleep-Wake Concordance in Couples Is Inversely Associated With Cardiovascular Disease Risk Markers. Sleep. 2017;40(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasler BP, Troxel WM. Couples’ nighttime sleep efficiency and concordance: evidence for bidirectional associations with daytime relationship functioning. Psychosom Med. 2010;72(8):794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–16. [DOI] [PubMed] [Google Scholar]
- 14.Wilson SJ, Bailey BE, Jaremka LM, Fagundes CP, Andridge R, Malarkey WB, et al. When couples’ hearts beat together: Synchrony in heart rate variability during conflict predicts heightened inflammation throughout the day. Psychoneuroendocrinology. 2018;93:107–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tempesta D, Socci V, De Gennaro L, Ferrara M. Sleep and emotional processing. Sleep Medicine Reviews. 2018;40:183–95. [DOI] [PubMed] [Google Scholar]
- 16.Gordon AM, Chen S. The Role of Sleep in Interpersonal Conflict: Do Sleepless Nights Mean Worse Fights? Social Psychological and Personality Science. 2014;5(2):168–75. [Google Scholar]
- 17.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–84. [DOI] [PubMed] [Google Scholar]
- 18.Worthman CM, Melby MK. Toward a comparative developmental ecology of human sleep. Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. 2002:69–117. [Google Scholar]
- 19.El-Sheikh M, Kelly R, Rauer A. Quick to berate, slow to sleep: interpartner psychological conflict, mental health, and sleep. Health Psychol. 2013;32(10):1057–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350–65. [DOI] [PubMed] [Google Scholar]
- 21.Spanier GB. Measuring Dyadic Adjustment - New Scales for Assessing Quality of Marriage and Similar Dyads. Journal of Marriage and the Family. 1976;38(1):15–28. [Google Scholar]
- 22.Kenny DK D; Bolger N. Data analysis in social psychology. In: Gilbert DF S; Lindsey G, editor. Handbook of social psychology. New York: McGraw-Hill; 1998. p. 233–65. [Google Scholar]
- 23.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. xix, 458 p. p. [Google Scholar]
- 24.Lee S, Crain TL, McHale SM, Almeida DM, Buxton OM. Daily antecedents and consequences of nightly sleep. J Sleep Res. 2017;26(4):498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Milek A, Butler EA, Bodenmann G. The interplay of couple’s shared time, women’s intimacy, and intradyadic stress. J Fam Psychol. 2015;29(6):831–42. [DOI] [PubMed] [Google Scholar]
- 26.Tucker JS, Anders SL. Social control of health behaviors in marriage. Journal of Applied Social Psychology. 2001;31(3):467–85. [Google Scholar]
- 27.Walters EM, Phillips AJK, Mellor A, Hamill K, Jenkins MM, Norton PJ, et al. Sleep and wake are shared and transmitted between individuals with insomnia and their bed-sharing partners. SLEEP. 2020;43:1r+. [DOI] [PubMed] [Google Scholar]
- 28.Butler EA, Randall AK. Emotional Coregulation in Close Relationships. Emotion Review. 2013;5(2):202–10. [Google Scholar]
- 29.Saxbe D, Repetti RL. For better or worse? Coregulation of couples’ cortisol levels and mood states. J Pers Soc Psychol. 2010;98(1):92–103. [DOI] [PubMed] [Google Scholar]
- 30.Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: examining the covariation between relationship quality and sleep. Sleep Med Rev. 2007;11(5):389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Troxel WM. It’s more than sex: exploring the dyadic nature of sleep and implications for health. Psychosom Med. 2010;72(6):578–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang FL. Multilevel modeling myths. 2018;33:492–9. [DOI] [PubMed] [Google Scholar]
- 33.Musca S, Kamiejski R, Nugier A, Méot A, Er-rafiy A, Brauer M. Data with Hierarchical Structure: Impact of Intraclass Correlation and Sample Size on Type-I Error. Frontiers in Psychology. 2011;2(74). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.