Abstract
BACKGROUND
Most clinical trials of contrast-rebalanced binocular amblyopia treatment used a contrast increment protocol of 10% daily with successful play. Paired with a definition of success requiring only 15–30 min/day of gameplay, this increment protocol could allow children to reach 100% fellow eye contrast in 3–9 hours; however, this may not provide adequate therapeutic time with reduced fellow eye contrast. The purpose of this study was to compare the original protocol against three alternative contrast increment protocols designed to increase the number of treatment hours.
METHODS
In this prospective study, 63 amblyopic children (4–10 years; amblyopic eye visual acuity, 20/40-125) were randomly assigned one of four daily contrast increment protocols for 4 weeks, all starting with 20% fellow eye contrast: 10%, 5%, 0%, or 10% for first 4 weeks then reset to 20% and repeat 10% increment for the final 4 weeks. Children played contrast-rebalanced games for 1 hour/day, 5 days/week. Best-corrected visual acuity, stereoacuity, and suppression were assessed at baseline and every 2 weeks until the 8-week outcome visit.
RESULTS
At baseline, mean amblyopic eye best-corrected visual acuity was 0.47 ± 0.14 logMAR (20/60), improving overall 0.14 ± 0.08 logMAR (1.4 lines; P < 0.0001) at 8 weeks. All four protocols resulted in similar improvement in visual acuity (0.13–0.16 logMAR; all Ps < 0.0002). Stereoacuity and suppression also improved (all Ps < 0.05).
CONCLUSIONS
None of the new protocols resulted in less improvement than the original 10% contrast increment protocol. Contrast-rebalanced binocular games yielded significant improvements in visual acuity, stereoacuity, and suppression with or without daily contrast increments.
Amblyopia is the most common cause of monocular visual impairment, affecting 2%−4% of children.1,2 Though traditionally viewed as a monocular disorder, it typically arises as a result of binocularly discordant visual experience in the presence of strabismus or anisometropia during childhood. Patching and atropine are mainstays of amblyopia treatment, but not all children achieve long-term normal visual acuity.3–6 Our understanding of the role of interocular suppression as the primary factor interfering with normal visual development in amblyopia7,8 has led to the development of binocular amblyopia treatments that alleviate interocular suppression and restore binocular combination.
Binocular experience with at-home dichoptic tablet games, enhanced by decreasing fellow eye contrast to reduce interocular suppression, can effectively treat amblyopia, especially in children <7 years.9–11 Contrast rebalancing, that is, reducing fellow eye contrast to decrease its signal strength and reduce suppression of the amblyopic eye, allows the child to experience binocular vision while playing games.9–12 Previous randomized clinical trials have reported that contrast-rebalanced binocular gameplay yielded significant improvement in visual acuity; one study showed significantly more improvement than patching.10,13
Previous clinical trials of contrast-rebalanced games8–15 all used the same 10% per day fellow eye contrast increment protocol, that is, if gameplay was successful, the starting fellow eye contrast of 20% was incremented to 22%, 24%, 26%, 29%, and so forth. The 10% daily contrast- increment was first used in an attempt to progressively normalize binocular vision with repeated binocular game play.16 Although there is a clear rationale for reducing fellow eye contrast to minimize suppression, there is no scientific evidence that a contrast increment is necessary. In addition, the 10% contrast increment protocol results in equal contrast for both eyes after only 18 days of successful gameplay; that is, contrast-rebalancing is no longer present. This protocol, paired with a definition of success that required a minimum game score paired with only 15–30 minutes daily game play. In one study that started fellow eye contrast at >20%,17 children could reach 100% fellow eye contrast with as little as 3–9 hours of gameplay.4,9–17 Data from feline and murine models of amblyopia suggest that a long period of decreased activity followed by a period where presynaptic activity of both eyes is correlated with postsynaptic activity is needed to effect a strong and permanent rebalancing of ocular dominance.18–20
Although 35%−40% of children in previous studies achieved normal visual acuity after playing the binocular action game Dig Rush for 4 weeks,10,11 60%−65% of children remained amblyopic. Barriers to continuing contrast-rebalanced binocular treatment beyond 4 weeks exist. For many children, contrast rebalancing was no longer present by 4 weeks with the 10% daily contrast increment protocol. Also, compliance with a single game drops after 4 weeks of playing the same game. Thus, there is a need to examine alternate contrast increment protocols that, if effective, could prolong the duration of contrast-rebalanced binocular treatment, as well as a need for additional games to enhance compliance.
We investigated whether the contrast increment is necessary by determining whether a constant fellow eye contrast of 20% (0% daily contrast increment) is effective in promoting visual acuity recovery, and whether the amount of visual acuity improvement is significantly less than that obtained with the 10% per day contrast increment protocol. Also, we evaluated two new daily contrast increment protocols designed to extend the contrast-balanced treatment duration: 5% and 10% with a reset of fellow eye contrast to 20% at the end of the initial 4-week period.
Subjects and Methods
The research protocol adhered to the tenets of the Declaration of Helsinki, was approved by the the University of Texas Southwestern Medical Center Institutional Review Board, and conformed to requirements of the US Health Insurance Portability and Accountability Act of 1996. Written informed consent was obtained from parents or legal guardians; assent was obtained for children 10 years of age.
Eligible participants were children 4–10 years of age who were diagnosed with amblyopia due to strabismus, anisometropia, or both and referred to the Retina Foundation by pediatric eye specialists in the Dallas area. Medical records were obtained from referring ophthalmologists to extract diagnoses, alignment, and prior treatment. Children with strabismic or combined mechanism amblyopia were eligible to participate only after correction of residual strabismus to <5Δ. Eligible children had to have been wearing their current spectacle correction for at least 8 weeks. See eSupplement 1 (available at jaapos.org) for inclusion and exclusion criteria.
This study was a randomized clinical trial. At the baseline visit, eligibility was ascertained and vision assessments were conducted. Children 4 to<7.5 years of age (younger) and 7.5 to 10.9 years of age (older) were randomized separately to one of four daily fellow eye contrast increment protocols for the 8-week treatment (Figure 1). Investigators had access to the randomization assignment only after the child was enrolled. Children had follow-up visits every 2 weeks (14 ± 3 days).
FIG 1.

Consort diagram showing the number of completed and missed visits during the 8-week study period. There were 5 missed follow-up examinations among the 63 children who completed 8-week visit. There were 5 children, excluded from analysis, lost to follow-up between the baseline visit and the 8-week final examination.
Binocular Games
Children were loaned an Android OS tablet computer with a previously studied action-oriented dichoptic game, Dig Rush, for the first 4 weeks.10,11 At the 4-week visit, children were given a second action-oriented dichoptic game, Monster Burner, for the final 4 weeks. Both games were designed using the same contrast-rebalancing principle; that is, suppression of the amblyopic eye can be reduced or eliminated by reducing fellow eye contrast. Children wore anaglyphic glasses so that reduced-contrast elements were seen by the fellow eye, and high-contrast elements were seen by the amblyopic eye; some background elements were seen by both eyes. For successful gameplay, both eyes must see their respective game elements.
During the baseline visit, children were familiarized with the games, and they demonstrated their ability to see both the high-contrast and low-contrast game elements while wearing anaglyphic glasses. Children practiced using the games until one of the authors (RMJ) was confident in their ability to understand and play. Children were asked to play games at home for 1 hour/day, 5 days/week for 8 weeks (40 hours total).
Fellow Eye Contrast-increment Protocols
Amblyopic eye contrast was fixed at 100% contrast. Fellow eye contrast was initially 20% for all four contrast-increment protocols evaluated in this 8-week study. See Table 1 and Figure 2. Fellow eye contrast was incremented using one of 4 protocols on the day following a session of successful gameplay, defined as >30 minutes gameplay with at least one star earned:
10%: fellow eye contrast incremented 10% each day with game success over 8 weeks
5%: fellow eye contrast incremented 5% each day with game success over 8 weeks
0%: no fellow eye contrast increment; fellow eye contrast remains at 20%
10% + reset: fellow eye contrast incremented 10% each day with game success for the first 4 weeks, then reset to 20% fellow eye contrast and repeat 10% contrast increment for the final 4 weeks
Table 1.
Contrast increment protocols
| Contrast increment protocol | Initial FE contrast | Daily increment, weeks 0–4 | 4-week contrast (%), mean ± SD | No. at 100% contrast | Daily increment, weeks 4–8 | 8-week contrast (%), mean ± SD | No. at 100% contrast |
|---|---|---|---|---|---|---|---|
| 10% | 20% | 10% | 89 ± 21 | 12 (71%) | Continue 10% | 95 ± 19 | 16 (94%) |
| 5% | 20% | 5% | 42 ± 17 | 0 (0%) | Continue 5% | 73 ± 33 | 9 (56%) |
| 0% | 20% | 0% | 20 ± 0 | 0 (0%) | Continue 0% | 20 ± 0 | 0 (0%) |
| 10% + reset | 20% | 10% | 78 ± 26 | 8 (50%) | Reset FE to 20%, continue 10% | 80 ± 31 | 11 (65%) |
FE, fellow eye; SD, standard deviation.
FIG 2.
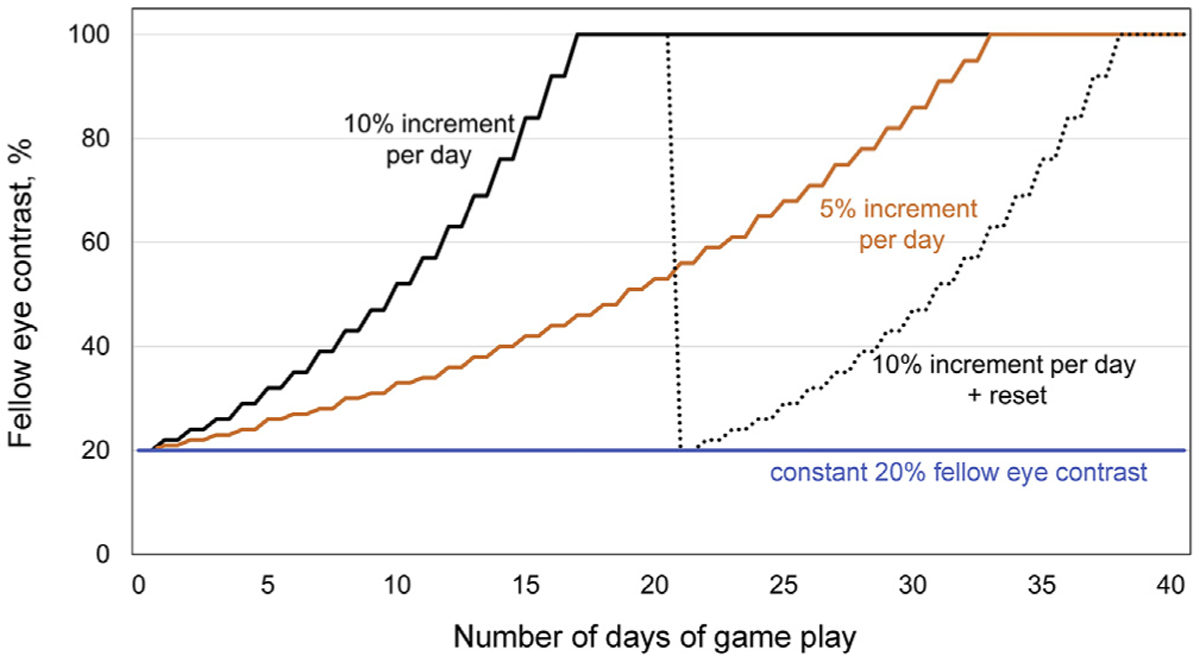
Illustration of hypothetical fellow eye contrast percentage for the four contrast increment protocols over the 8-week study.
If game play was unsuccessful for 30 minutes (no star earned), fellow eye contrast was decremented by 5% the following day. A tablet log file recorded the minutes played and fellow eye contrast for each session.
Vision Assessment
Vision assessments were conducted at baseline, 2 weeks, 4 weeks, 6 weeks, and 8 weeks and included the following: (1) crowded monocular best-corrected visual acuity using the electronic Early Treatment Diabetic Retinopathy Study protocol21,22 (ages 7–10 years) or the Amblyopia Treatment Study HOTV protocol23,24 (ages 4–6.9 years); (2) Stereoacuity (Randot Preschool Stereoacuity and Stereo Butterfly Tests [Stereo Optical Inc, Chicago, IL]); (3) extent of suppression scotoma using the Worth 4-Dot test at 7 distances25,26; and (4) depth of suppression using a dichoptic eye chart that determines the contrast balance index (CBI) at which the child can overcome suppression.26,27
Sample Size and Statistical Analysis
Based on a recent study using the contrast-rebalanced Dig Rush game showing 0.17 logMAR change in 4 weeks and 35%−39% achieving 0.2 logMAR or better visual acuity,10,11 we anticipated the 10% contrast protocol for 8 weeks would result in 0.17 ± 0.09 logMAR improvement in BCVA, with >30% of children achieving 0.2 logMAR or better visual acuity. For α = 0.05 and 1 − β = 0.80, the required sample size is 13 per group. We enrolled 68 children (17 per group) to account for potential loss to follow-up.
The primary outcome was change in amblyopic eye best-corrected visual acuity at 8 weeks’ follow-up examination. The analysis was conducted with a modified intent-to-treat approach, limited to participants who completed the 8-week visit within the prespecified analysis windows (53–59 days after randomization) and no imputation for missing data. A one-way analysis of variance compared visual acuity change (baseline to 8 weeks) in the four groups. Three secondary analyses of visual acuity outcomes were conducted: (1) one sample t tests to determine whether amblyopic eye visual acuity at 8 weeks differed significantly from baseline per group (Bonferroni-corrected P = 0.0125); (2) change in visual acuity at the 2-, 4-, 6-, and 8-week visits using one-sample t tests to determine whether it differed significantly from baseline for the overall group; (3) differences in the proportion of children with visual acuity of 20/32 or better at 8 weeks in the original 10% protocol and the other protocols using a χ2 test.
Additional secondary analyses were conducted to examine changes in stereoacuity and suppression. Stereoacuity was converted to log arcsec for analyses; nil stereoacuity was arbitrarily assigned a value of 4.0. Using the Worth 4-Dot test, the farthest distance at which the child reported 4 dots was converted into size of suppression scotoma in degrees for extent of suppression. The depth of suppression test determined the CBI at which the amblyopic eye was not suppressed. Overall group change in stereoacuity, extent of suppression, and depth of suppression at 8 weeks (Wilcoxon signed-rank test) and change in visual acuity for younger versus older (independent t test) and no prior treatment versus prior treatment (Mann-Whitney U test) were also evaluated.
Results
Between July 24, 2017, and May 23, 2019, 68 eligible children were enrolled. Of the 68 participants, 5 left the study prior to the 8-week outcome visit (3 were too young or immature to play the games; 2 were lost to follow-up), and 63 completed the study (Figure 1). Baseline characteristics for the included children are listed in Table 2.
Table 2.
Baseline characteristics
| Characteristic | Total (N = 63) |
10% (n = 17) |
5% (n = 16) |
0% (n = 14) |
10% + reset (n = 16) |
|---|---|---|---|---|---|
| Female, no. (%) | 33 (52) | 11 (65) | 7 (44) | 5 (36) | 10 (63) |
| Age group, years, no. (%) | |||||
| 4.0–7.4 | 30 (48) | 9 (53) | 8 (50) | 7 (50) | 6 (38) |
| 7.5–10.9 | 33 (52) | 8 (47) | 8 (50) | 7 (50) | 10 (62) |
| Mean ± SD | 7.6 ± 1.6 | 7.4 ± 1.4 | 7.5 ± 1.4 | 7.6 ± 1.9 | 8.1 ± 1.9 |
| Prior treatment | |||||
| Patching/atropine, no. (%) | 57 (90) | 16 (94) | 15 (94) | 14 (100) | 12 (75) |
| Binocular treatmenta | 5 (8) | 2 (12) | 2 (13) | 1 (7) | 0 (0) |
| Weeks in glasses at enrollment, no. (%) | |||||
| 8–13 | 2 (3) | 0 (0) | 0 (0) | 0 (0) | 2 (12) |
| 14–26 | 1 (2) | 0 (0) | 0 (0) | 1 (7) | 0 (0) |
| >26 | 60 (95) | 17 (100) | 16 (100) | 13 (93) | 14 (88) |
| Amblyogenic factor, no. (%) | |||||
| Strabismus | 16 (25) | 4 (24) | 6 (38) | 3 (21) | 3 (19) |
| Anisometropia | 28 (44) | 8 (47) | 4 (25) | 7 (50) | 9 (56) |
| Combined | 19 (30) | 5 (29) | 6 (38) | 4 (29) | 4 (25) |
| Amblyopic eye BCVA, logMAR, no. (%) | |||||
| 0.3–0.6 | 57 (90) | 14 (82) | 14 (88) | 14 (100) | 15 (94) |
| 0.7–0.8 | 6 (10) | 3 (18) | 2 (12) | 0 (0) | 1 (6) |
| Mean ± SD | 0.47 ± 0.14 | 0.50 ± 0.16 | 0.47 ± 0.16 | 0.46 ± 0.12 | 0.46 ± 0.14 |
| Fellow eye BCVA, logMAR, no. (%) | |||||
| −0.1 | 19 (30) | 6 (35) | 4 (25) | 4 (29) | 5 (31) |
| 0.0 | 29 (46) | 6 (35) | 8 (50) | 8 (57) | 7 (44) |
| 0.1 | 13 (21) | 5 (29) | 3 (19) | 1 (7) | 4 (25) |
| 0.2 | 2 (3) | 0 (0) | 1 (6) | 1 (7) | 0 (0) |
| Mean ± SD | 0.00 ± 0.09 | 0.01 ± 0.09 | −0.01 ± 0.09 | −0.01 ± 0.08 | −0.01 ± 0.08 |
Adherence to Protocol
For the first 4 weeks, with Dig Rush, children completed a mean of 17.4 hours (87% adherence). For the second 4 weeks, with Monster Burner, children completed a mean of 15.2 hours (76% adherence). Four children (6%) played ≤25% of prescribed treatment for the 8 weeks. As expected, most children in the 10% and 10% + reset contrast increment groups reached 100% fellow eye contrast by 4 weeks (Table 1). All but 5 of the 33 children (85%) in the two groups reached 100% fellow eye contrast by 8 weeks, but only 30% of children in the 5% and 0% contrast increment groups did.
Outcomes
Each protocol resulted in significant improvement in best-corrected visual acuity at 8 weeks (all Ps < 0.0002; Table 3). Combining data for all four groups, the mean (with standard deviation) amblyopic eye visual acuity improvement was 0.14 ± 0.08 logMAR (1.4 ± 0.8 lines; 95% CI, 0.12–0.16 logMAR).
Table 3.
Mean improvement at 8 weeks
| AE BCVA, logMARa | RDS, log arcseca | Extent of suppression scotoma, log degreesa | Depth of suppression, CBIa | |
|---|---|---|---|---|
| Total (N = 63) | 0.14 ± 0.08b | 0.16 ± 0.39b | 0.19 ± 0.49b | 0.61 ± 3.07b |
| Contrast increment protocol | ||||
| 10% (n = 17) | 0.14 ± 0.07b | 0.14 ± 0.30 | 0.19 ± 0.46 | 0.79 ± 3.39 |
| 5% (n = 16) | 0.14 ± 0.09b | 0.12 ± 0.45 | 0.15 ± 0.38 | 0.65 ± 3.06 |
| 0% (n = 14) | 0.13 ± 0.09b | 0.16 ± 0.32 | 0.24 ± 0.64b | −0.76 ± 3.17 |
| 10% + reset (n = 16) | 0.16 ± 0.09b | 0.22 ± 0.49 | 0.18 ± 0.35 | 1.49 ± 2.49b |
| Age group | ||||
| 4.0–7.4 years | 0.17 ± 0.08b | 0.19 ± 0.43 | 0.23 ± 0.38b | 0.43 ± 3.05b |
| 7.5–10.9 years | 0.12 ± 0.08b | 0.13 ± 0.37 | 0.15 ± 0.57b | 0.75 ± 3.09 |
AE BCVA, amblyopic eye best-corrected visual acuity; CBI, contrast balance index; logMAR, logarithm of the minimum angle of resolution; RDS, random dot stereoacuity.
Results presented as mean and standard deviation.
Significant improvement from baseline.
At the 8-week primary outcome visit, all four contrast increment protocols yielded similar amblyopic eye visual acuity improvements (F3,59 = 0.44; P = 0.73): 10%, 0.14 ± 0.07 logMAR (1.4 ± 0.7 lines); 5%, 0.14 ± 0.09 logMAR (1.4 ± 0.9 lines); 0%, 0.13 ± 0.09 logMAR (1.3 ± 0.9 lines); 10% + reset, 0.16 ± 0.09 logMAR (1.6 ± 0.9 lines). Significant amblyopic eye improvements were seen at 2 weeks, 4 weeks, 6 weeks, and 8 weeks (all Ps < 0.001; Figure 3). As shown in Figure 4, change in visual acuity ranged from −0.1 to 0.3 logMAR (−1 to 3 lines): 1 child (2%) regressed 0.1 logMAR (−1 line), 4 children (6%) did not improve, 32 children (51%) improved 0.1 logMAR (1 line), 19 children (30%) improved 0.2 logMAR (2 lines), and 7 children (11%) improved 0.3 logMAR (3 lines).
FIG 3.
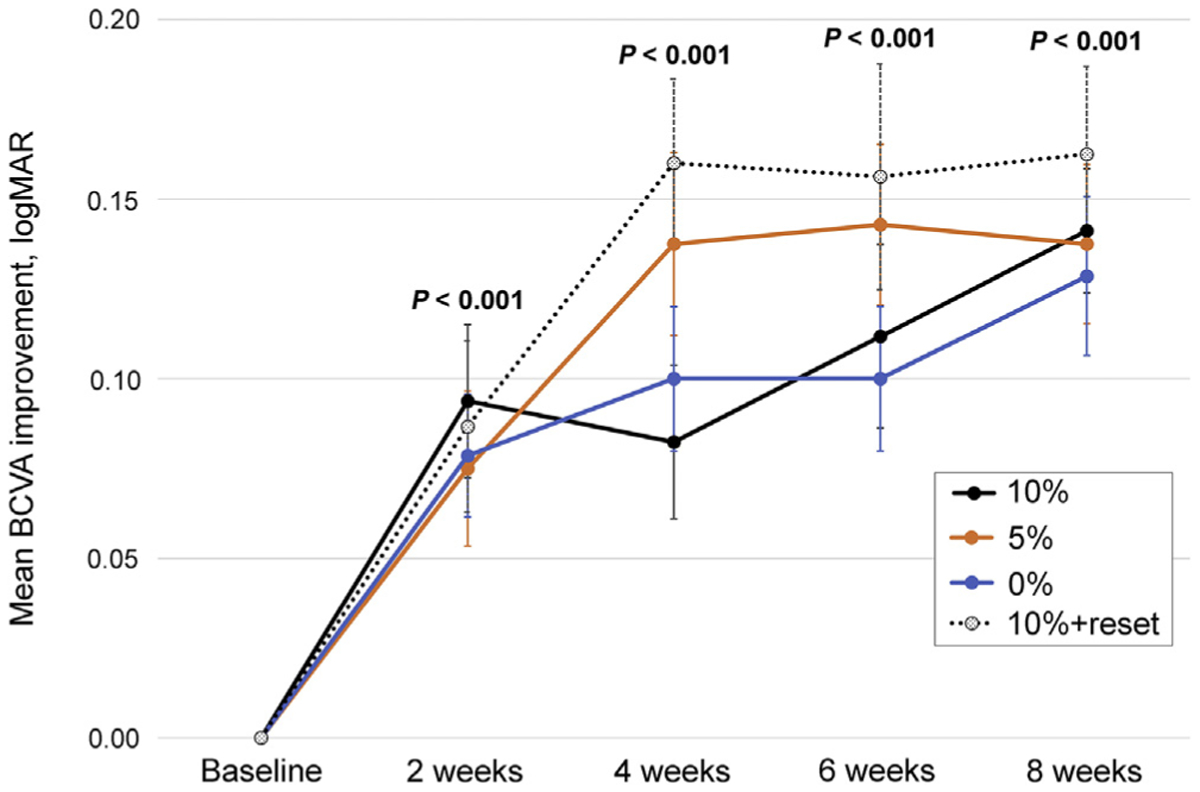
Amblyopic eye best-corrected visual acuity (BCVA) improvement at baseline, 2 weeks, 4 weeks, 6 weeks, and 8 weeks. Error bars represent ± standard error. P values are group differences from baseline.
FIG 4.

Amblyopic eye best-corrected visual acuity (BCVA) at the baseline and 8 weeks for children with 10% contrast increment, 5%, 0%, and 10% + reset. Data points above the line indicate improvement. Overlapping symbols are slightly shifted for clarity.
The proportion of children achieving visual acuity of 0.2 logMAR (20/32) or better increased at each visit: 23% at 2 weeks, 29% at 4 weeks, 33% at 6 weeks, and 40% at 8 weeks. Compared with the original 10% protocol, in which 7 of 17 children (41%) reached 0.2 logMAR (20/32) or better at 8 weeks, there was not a significant difference for the 5% protocol (8/16 [50%] children; χ2 = 0.26; P = 0.61; 95% CI, −23% to 38%), the 0% protocol (3/14 [21%] children; χ2 = 1.37; P = 0.24; 95% CI, −13% to 47%), or the 10% + reset protocol (40% of 16 children; χ2 < 0.00; P = 0.95; 95% CI, −30% to 31%).
At the 8 weeks, younger children had a larger mean improvement in visual acuity than older children (younger, 0.17 ± 0.08 logMAR [1.7 ± 0.8 lines]; older, 0.12 ± 0.08 logMAR [1.2 ± 0.8 lines]; t61 = 2.22; P = 0.015) The 6 children with no prior amblyopia treatment improved more than the 57 children who had prior amblyopia treatment (no prior, 0.22 logMAR [2.2 lines]; prior, 0.14 logMAR [1.4 lines]; U = 80.5; P = 0.03).
At 8 weeks, overall random dot stereoacuity improved by a mean of 0.16 ± 0.39 log arcsec (z = 2.84; P = 0.045; 95% CI, 0.06–0.26). The extent of suppression scotoma (Worth 4-Dot) improved by 0.19 ± 0.45 log degrees (z = 3.53; P = 0.0004; 95% CI, 0.07–0.30). Depth of suppression by CBI improved by 0.61 ± 3.07 (z = 2.05; P = 0.04; 95% CI, −0.15 to 1.37).
Discussion
Binocular game treatment with the addition of a second game and new contrast increment protocols designed to extend the treatment period to 8 weeks was successful. An overall mean visual acuity improvement of 0.14 logMAR (1.4 lines) was achieved, and 40% of the children achieved visual acuity of at least 0.2 logMAR (20/32) at 8 weeks. Children were enrolled only after they had stable visual acuity in glasses on multiple visits prior to baseline. There was no significant difference between the four contrast increment protocols in the amount of visual acuity improvement at 8 weeks, ranging from 0.13 to 0.16 logMAR (1.3–1.6 lines). Extending the treatment period with fellow eye contrast increments of 5%, 0%, or resetting it back to the initial 20% was just as effective as the original 10% per day contrast increment, at least over 8 weeks. Both the 0% contrast increment protocol and the 10% + reset protocol have the potential advantage of indefinitely extending treatment, if needed.
The mean visual acuity improvement achieved progressively diminished as the study progressed. This was an expected result of the increasing number of children whose amblyopic eye achieved normal visual acuity at each visit. As more children recover normal visual acuity, a ceiling effect limits group mean visual acuity improvement. The proportion of children achieving age-normal visual acuity nearly doubled from 23% to 40% between the 2-week and 8-week visits, but the ceiling effect resulted in only a modest change in mean visual acuity.
Younger children improved more than older children (0.17 vs 0.12 logMAR). This echoes the mounting evidence10,13,28 that binocular treatment is more effective in younger than in older children. Though only a small sample, the 6 children with no prior amblyopia treatment improved significantly more than the rest of the cohort, suggesting that binocular amblyopia treatment, like patching, is more effective as an initial treatment than as a treatment for residual amblyopia.
Our finding of improvement by 1.4 lines after 8 weeks of binocular game treatment is similar to our previous studies using Tetris and Pong9 (0.9 line after 4 weeks), Dig Rush10 (1.7 lines after 4 weeks), and dichoptic movie treatment28 (1.5 lines after 2 weeks). Compliance with the prescribed binocular treatment appears to be vital in maximizing amblyopic visual acuity.11 This is the first study to use two games and contrast increment protocols specifically designed for 8 or more weeks rather than 4 weeks9–16 of binocular treatment.
We observed modest improvements in binocular vision in random dot stereoacuity, extent of suppression, and depth of suppression at 8 weeks. Overall, 30% of children had improved stereoacuity, 57% had reduced extent of suppression, and 60% had reduced depth of suppression. These are similar to an earlier report of binocular treatment outcomes with a contrast-rebalanced game or movies (20%, 49%, and 63%, resp.).29 There has been a focus on interocular suppression in the etiology of amblyopia,7,8 and alleviating suppression with binocular treatment may be the key to treatment.
One limitation of the current study was the absence of long-term follow-up. Although 92% of children had improved visual acuity at 8 weeks, 60% remained amblyopic and returned to patching. Thus, we were unable to determine the lasting effects of binocular treatment. However, two prior studies of binocular game treatment, using the same contrast-rebalanced design principle, reported that gains in visual acuity were stable for 6–12 months.30,31 A second limitation was that visual acuity examiners were not masked to assignment at the primary outcome visit. However, visual acuity was tested using the EVA system with the ATS-HOTV (for children <7 years of age) or E-ETDRS (for children 7–10 years of age) protocols. This equipment and software, commonly used in multi-center clinical trials, offer standardized optotypes, luminance, and testing procedures, ensuring objective visual acuity measurement.
Binocular treatment for amblyopia is novel and many questions remain. It needs to be determined how to convert binocular games to prolong amblyopia treatment beyond 8 weeks (eg, development of a variety of engaging games, adjustment of contrast levels, and maintenance treatment). Although 40% of children achieved normal visual acuity within 8 weeks, the remaining 60% may have benefited from additional binocular treatment. Our finding that children improved with multiple contrast increment protocols using two separate binocular games over 8 weeks suggests future investigation of long-term binocular treatment is warranted, especially in younger children.
Supplementary Material
Acknowledgments
Supported by a grant from the National Eye Institute (EY022313). The tablets and games were loaned to the Retina Foundation of the Southwest for the duration of the study by Amblyotech Inc, Atlanta, Georgia.
Footnotes
References
- 1.Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months the Baltimore Pediatric Eye Disease Study. Ophthalmology 2009;116:2128–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Multi-Ethnic Pediatric Eye Disease Study. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology 2008;115:1229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Repka MX, Wallace DK, Beck RW, et al. , Pediatric Eye Disease Investigator Group. Two-year follow-up of a 6-month randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol 2005;123:149–57. [DOI] [PubMed] [Google Scholar]
- 4.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol 2003;121:603–11. [DOI] [PubMed] [Google Scholar]
- 5.Stewart CE, Moseley MJ, Stephens DA, Fielder AR. Treatment dose-response in amblyopia therapy: the Monitored Occlusion Treatment of Amblyopia Study (MOTAS). Invest Ophthalmol Vis Sci 2004;45: 3048–54. [DOI] [PubMed] [Google Scholar]
- 6.Wallace DK, Edwards AR, Cotter SA, et al. , Pediatric Eye Disease Investigator Group. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology 2006;113:904–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birch EE. Amblyopia and binocular vision. Prog Retin Eye Res 2013; 33:67–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hess RF, Thompson B. Amblyopia and the binocular approach to its therapy. Vision Res 2015;114:4–16. [DOI] [PubMed] [Google Scholar]
- 9.Birch EE, Li SL, Jost RM, et al. Binocular iPad treatment for amblyopia in preschool children. J AAPOS 2015;19:6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly KR, Jost RM, Dao L, Beauchamp CL, Leffler JN, Birch EE. Binocular iPad game vs patching for treatment of amblyopia in children: a randomized clinical trial. JAMA Ophthalmol 2016;134: 1402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birch EE, Jost RM, Kelly KR, Leffler JN, Dao L, Beauchamp CL. Baseline and clinical factors associated with response to amblyopia treatment in a randomized clinical trial. Optom Vis Sci 2020;97: 316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knox PJ, Simmers AJ, Gray LS, Cleary M. An exploratory study: prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol Vis Sci 2012;53:817–24. [DOI] [PubMed] [Google Scholar]
- 13.Holmes JM, Manh VM, Lazar EL, et al. , Pediatric Eye Disease Investigator Group. Effect of a binocular iPad game vs part-time patching in children aged 5 to 12 years with amblyopia: a randomized clinical trial. JAMA Ophthalmol 2016;134:1391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manh VM, Holmes JM, Lazar EL, et al. , Pediatric Eye Disease Investigator Group. A randomized trial of a binocular iPad game versus part-time patching in children aged 13 to 16 years with amblyopia. Am J Ophthalmol 2018;186:104–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group, Holmes JM, Manny RE, Lazar EL, et al. A randomized trial of binocular Dig Rush game treatment for amblyopia in children aged 7 to 12 years of age. Ophthalmology 2019;126:456–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.To L, Thompson B, Blum JR, Maehara G, Hess RF, Cooperstock JR. A game platform for treatment of amblyopia. IEEE Trans Neur Sys Rehab Eng 2011;19:280–89. [DOI] [PubMed] [Google Scholar]
- 17.Gao TY, Guo CX, Babu RJ, et al. , BRAVO Study Team. Effectiveness of a binocular video game vs placebo video game for improving visual functions in older children, teenagers, and adults with amblyopia: a randomized clinical trial. JAMA Ophthalmol 2018; 136:172–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell DE, Aronitz E, Bobbie-Ansah P, Crowder N, Duffy KR. Fast recovery of the amblyopic eye acuity of kittens following brief exposure to total darkness depends on the fellow eye. Neural Plast 2019;2019:7624837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell DE, Crowder NA, Duffy KR. The critical period for darkness-induced recovery of the vision of the amblyopic eye following early monocular deprivation. J Vis 2019;19:25. [DOI] [PubMed] [Google Scholar]
- 20.Mower GD, Christen WG. Evidence for an enhanced role of GABA inhibition in visual cortical ocular dominance of cats reared with abnormal monocular experience. Brain Res Dev Brain Res 1989;45: 211–18. [DOI] [PubMed] [Google Scholar]
- 21.Beck R, Moke P, Turpin A, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol 2003;135: 194–205. [DOI] [PubMed] [Google Scholar]
- 22.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the electronic early treatment diabetic retinopathy study testing protocol in children 7 to < 13 years old. Am J Ophthalmol 2003;136: 655–61. [DOI] [PubMed] [Google Scholar]
- 23.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol 2001;119:1345–53. [DOI] [PubMed] [Google Scholar]
- 24.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol 2001;132:903–9. [DOI] [PubMed] [Google Scholar]
- 25.Rosenbaum AL, Santiago AP. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia: Saunders; 1999. [Google Scholar]
- 26.Webber AL, Wood JM, Thompson B, Birch EE. From suppression to stereoacuity: a composite binocular function score for clinical research. Ophthalmic Physiol Opt 2019;39:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Birch EE, Morale SE, Jost RM, et al. Assessing suppression in amblyopic children with a dichoptic eye chart. Invest Ophthalmol Vis Sci 2016;57:5649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Birch E, Jost R, De La Cruz A, et al. Binocular amblyopia treatment with contrast re-balanced movies. J AAPOS 2019;23:160. e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelly KR, Jost RM, Wang YZ, et al. Improved binocular outcomes following binocular treatment for childhood amblyopia. Invest Ophthalmol Vis Sci 2018;59:1221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li SL, Jost RM, Morale SE, et al. Binocular iPad treatment of amblyopia for lasting improvement of visual acuity. JAMA Ophthalmol 2015;133:479–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mansouri B, Singh P, Globa A, Pearson P. Binocular training reduces amblyopic visual acuity impairment. Strabismus 2014;22:1–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


