Abstract
Objective:
The purpose of this longitudinal study was to identify associations of drinking intensity at age 29/30 with symptoms of alcohol use disorder (AUD) at age 35.
Method:
Analyses used national longitudinal data from 1,253 individuals (53.5% female) participating in the Monitoring the Future study. Age 29/30 data were collected from 2005 to 2013; age 35 data were collected from 2010 to 2018. Multivariable models regressed age 35 past-5-year AUD symptoms (vs. nondisordered drinking/abstinence) on age 29/30 past-2-week drinking intensity (no/low [0–4] drinking, binge [5–9] drinking, high-intensity [10+] drinking), with key covariates being controlled for.
Results:
At age 35, 32.6% (SE = 1.50) of respondents reported AUD symptoms. AUD symptoms at age 35 were reported by 77.5% (SE = 4.79) of participants who reported age 29/30 high-intensity drinking and 60.6% (SE = 3.95) of participants who reported age 29/30 binge drinking. Age 35 past-5-year abstinence was reported by almost no respondents reporting age 29/30 binge drinking or high-intensity drinking. AUD symptoms at age 35 were significantly more likely for those who reported binge (adjusted multivariable odds ratio [AOR] = 5.61, 95% CI [3.79, 8.30], p < .001) or high-intensity (AOR = 12.26, 95% CI [6.70, 22.41], p < .001) drinking versus no/low drinking at age 29/30. The likelihood of having AUD symptoms was significantly higher for high-intensity than for binge drinkers (AOR = 2.18, 95% CI [1.14, 4.19], p = .019).
Conclusions:
Nearly 80% of those young adults who reported engaging in high-intensity drinking (10+ drinks in a row) at age 29/30 later reported AUD symptoms at age 35. High-intensity drinking appears to be a strong prospective marker of risk for AUD symptoms among adults in the United States.
Alcohol use disorder (aud) is linked to a range of adverse outcomes, including mortality, disability, accidents, and violence (Room et al., 2005; Samokhvalov al., 2010; Stahre et al., 2014). Worldwide, more than 2.5 million deaths are attributable to AUD on an annual basis (World Health Organization, 2014). Approximately 5.8% of the U.S. adult population age 18 and older—roughly 14.4 million adults—met criteria for AUD in 2018 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2019). Annually in the United States, excessive alcohol use and AUD are responsible for 90,000 premature deaths and cost more than $225 billion (Bouchery et al., 2011; Centers for Disease Control and Prevention, 2019). Reducing AUD risk and prevalence is a central public health priority.
The number of drinks consumed at a single occasion is a key measure of alcohol risk and has been associated with AUD (e.g., Linden-Carmichael et al., 2017). Heavy episodic or “binge” drinking—defined as 5+ drinks using a universal threshold or 4+ drinks for women/5+ drinks for men—is associated with AUD among adolescents and young adults in cross-sectional studies and controlled experiments (Addolorato et al., 2018; Gowin et al., 2017; Grant et al., 2003). Yet, the average number of drinks consumed during a binge is significantly higher than the 4+/5+ threshold (Naimi et al., 2010). Reliance on the binge indicator alone may obscure higher-risk populations (Patrick, 2016). High-intensity drinking (HID) is defined as 10+ drinks using a universal threshold or sex-specific cutoffs of 8+ for women/10+ for men (Hingson et al., 2017; Linden-Carmichael et al., 2017; Patrick, 2016). Cross-sectionally, individuals who engage in HID report binge drinking more frequently than non-HID binge drinkers (Patrick et al., 2016), and they are at higher risk for alcohol-related problems, including AUD, compared with individuals who engage in binge but not high intensity drinking (Linden-Carmichael et al., 2017). Both binge drinking and HID are cross-sectionally associated with AUD across adulthood; however, HID is a stronger correlate of AUD than binge drinking (Linden-Carmichael et al., 2017). Prospective risk from HID to later AUD symptoms has not been previously examined.
Key gaps in longitudinal research focused on AUD remain, including long-term associations between alcohol use and AUD among national samples in the United States (King et al., 2014; McCambridge et al., 2011; Seeley et al., 2019; Zucker et al., 2006). In general, there is a dearth of research on AUD from young adulthood to later adulthood (35+; King et al., 2014; Newton-Howes et al., 2019). AUD typically emerges in adolescence, peaks in the mid or late 20s, and thereafter declines as alcohol misuse becomes less socially acceptable and prevalent, potentially resulting from social role changes (Evans-Polce et al., 2020a, 2020b; King et al., 2014; Newton-Howes et al., 2019; Pardini et al., 2007; SAMHSA, 2019). Yet AUD can persist into adulthood (i.e., age 30), resulting in increased risk for more severe consequences from alcohol misuse (Grant et al., 2006; Jennison, 2004; Linden-Carmichael et al., 2017).
Available longitudinal research on AUD has primarily focused on binge drinking among adolescents or young adults (King et al., 2014; Newton-Howes et al., 2019). Binge drinking in early adolescence is associated with AUD in young adulthood (Foster et al., 2015; Grant et al., 2006; Mc-Cambridge et al., 2011; Riala et al., 2004), and after age 30 (Newton-Howes, 2019; Schulenberg et al., 2003; Seeley et al., 2019; Zucker et al., 2006). To our knowledge, prospective research on associations between HID and AUD is not available. In particular, it is not known if HID is a particular marker for AUD risk above and beyond binge drinking. More detailed information on markers for future AUD risk spanning from early to later adulthood is key to identifying patterns and prevention targets to reduce later AUD onset as well as persistent and increased risk in later adulthood (King et al., 2014; Zucker et al., 2006).
Current study
The current study examined prospective associations between drinking intensity and AUD symptoms using longitudinal data from a national sample aged 29/30 to 35. Specifically, analyses modeled associations between past-2-week drinking intensity level (<5 drinks per occasion, 5–9 drinks, or 10+ drinks) at age 29/30 and abstinence, nondisordered drinking, or AUD symptoms at age 35.
Method
Sample
Data were obtained from the Monitoring the Future study (Schulenberg et al., 2018). Monitoring the Future comprises annual, nationally representative samples of approximately 15,000 U.S. 12th grade students (modal age 18) in roughly 130 schools. Each year, a sample of 2,400 12th graders is selected for longitudinal follow-up (drug users are oversampled; analytic weights account for such oversampling). Data collection involves mailed questionnaires; a random half of the follow-up sample begins follow-up 1 year after 12th grade (modal age 19) and is surveyed biennially through modal age 29; the other half begins follow-up 2 years after 12th grade (modal age 20) and is surveyed biennially through modal age 30. Additional follow-up surveys are collected every 5 years beginning at modal age 35 (hereafter, modal age is referred to simply as “age”). A University of Michigan Behavioral Sciences Institutional Review Board approved the study.
HID measures were first introduced in 2005 on one of the six randomly distributed Monitoring the Future questionnaire forms used at ages 18 to 29/30. Age 29/30 data collection occurred from 2005 to 2013 (involving 12th grade cohorts from 1993 to 2001); age 35 data from these individuals were collected from 2010 to 2018. A total of 3,359 individuals who responded to the relevant questionnaire form were selected for follow-up; 1,314 (39.1%) responded to the age 35 survey. Sixty-one respondents (4.6% of 1,314) had missing data on AUD symptoms at age 35, leaving 1,253 cases for analysis (95.4% of 1,314). Weights were used to adjust for attrition (see Analysis).
Measures
Age 35 AUD symptoms. Respondents were asked if they had used any alcohol in the past 5 years. If yes, they were asked, “Think back over the last 5 years. Did your use of alcohol cause you any of the following problems?” Items addressing all 11 of the criteria for substance use disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association, 2013), were listed (response options: “no,” “a little,” “some,” “a lot”) (see Supplemental Table 1). (Supplemental material appears as an online-only addendum to this article on the journal's website.) Respondents were coded as exhibiting each criterion if they responded other than “no” to any item; the 11 dichotomous indicators were then summed to calculate the total number of criteria endorsed. Following recommended practice (American Psychiatric Association, 2013; Goldstein et al., 2015; Grant et al., 2015), AUD symptoms were indicated by meeting two or more criteria. Respondents were coded as past-5-year abstainers, nondisordered drinkers (endorsed 0 or 1 criteria), or having AUD symptoms (endorsed 2+ criteria) (Bray et al., 2019; Jang et al., 2018, 2019; Patrick et al., 2011; Schulenberg et al., 2016). Although the resulting measure does not reflect a clinical AUD diagnosis, the approach is fairly consistent with that used in other large surveys (Evans-Polce et al., 2020a, 2020b; Harford & Muthén, 2001; Muthén, 1996; Nelson et al., 1998) and has been used with Monitoring the Future data in prior studies examining symptoms of substance use disorder (Patrick et al., 2011, 2016; Schulenberg et al., 2016). AUD symptoms were further differentiated into mild (2–3 criteria), moderate (4–5 criteria), and severe (6+ criteria) categories.
Age 29/30 drinking intensity. Respondents were asked to report the number of occasions during the last 2 weeks in which they had (a) 5 or more, and (b) 10 or more drinks in a row. Responses were combined to make a mutually exclusive three-category variable reflecting the maximum number of drinks consumed in a row in the past 2 weeks: no/low drinking (0–4 drinks), binge but not HID (5–9 drinks; hereafter referred to simply as binge drinking), and HID (10+ drinks).
Covariates. At age 18 (12th grade survey), respondents reported sex (male/female), race (White/non-White), and if at least one parent had obtained a college degree (yes/no, as a measure of socioeconomic status; Patrick et al., 2012). At age 29/30, respondents reported if they had graduated from a 4-year college program (yes/no), were married (yes/no), had any children (yes/no), and were employed during the first full week of March (yes [having two or more jobs/one full-time job/one part-time job] vs. no [full-time homemaker/laid off or waiting to start a job/no paid employment at all]). Age 35 data collection year was coded using dichotomous indicators comprising 3-year groupings to account for possible nonlinear time associations: 2010–2012, 2013–2015, and 2016–2018.
Analysis
Analyses used survey procedures in SAS v.9.4 (SAS Institute Inc., Cary NC) for descriptive analyses. Logistic regression and ordinal logistic regression models were fit using Mplus v.7.4 specifying MLR and Monte Carlo integration; missing data on covariates were addressed using full information maximum likelihood. All analyses were weighted using attrition weights, calculated as the inverse of the probability of responding at age 35 based on covariates measured at age 18 (sex, race/ethnicity, college plans, high school grades, number of parents in the home, religiosity, parental education, alcohol use, cigarette use, marijuana use, region of country, cohort, and sampling weight correcting for oversampling of age 18 substance users).
Results
Sample description
The sample was 46.5% (SE = 1.63) male and 70.0% (1.71) White; at age 18, 51.7% (1.61) reported having at least one parent with a college degree. At age 29/30, 56.5% (1.75) reported being a college graduate, 53.3% (1.71) were married, 46.8% (1.72) had children, and 87.3% (1.15) were employed. Past-2-week drinking intensity at age 29/30 was 75.8% (1.44) no/low drinking, 16.0% (1.21) binge drinking, and 8.2% (0.95) HID. Regarding past-5-year alcohol use at age 35, 9.9% of respondents were classified as abstainers, 57.5% as nondisordered drinkers, and 32.6% as having AUD symptoms. Almost none of those reporting binge or HID at age 29/30 were categorized as past-5-year abstainers at age 35. Therefore, to estimate associations between age 29/30 drinking intensity and past-5-year AUD symptoms at age 35, the categories of abstainer and nondisordered were combined, resulting in 67.4% (1.50) abstainer/nondisordered drinkers and 32.6% (1.50) with AUD symptoms for further analyses.
Associations between drinking intensity and AUD symptoms
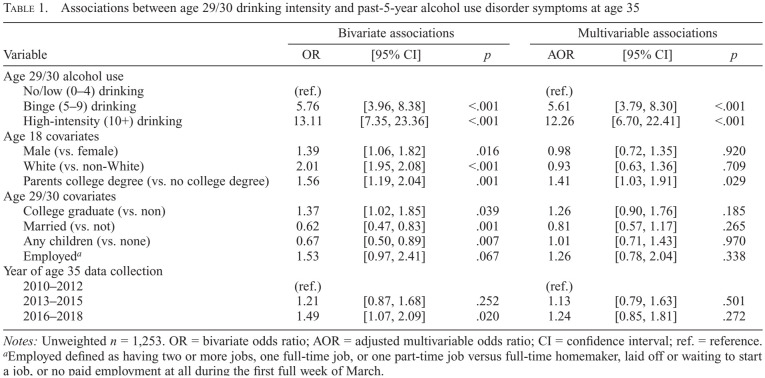
Table 1 reports bivariate and multivariable associations between age 29/30 drinking intensity and past-5-year AUD symptoms at age 35. In bivariate models using no/low drinking as the referent category, the odds of AUD symptoms were five times higher (bivariate odds ratio [OR] = 5.76) for those reporting binge drinking and more than double that (OR = 13.11) for those reporting HID. Only 21.1% (SE = 1.57) of those who reported no/low drinking met criteria for AUD symptoms compared with 60.6% (3.95) of those reporting binge drinking and 77.5% (4.79) of those reporting HID. An additional bivariate model (not shown) indicated that the likelihood of AUD symptoms was more than twice as high for those reporting HID versus binge drinking (OR = 2.26, 95% CI [1.19, 4.30], p = .012).
Table 1.
Associations between age 29/30 drinking intensity and past-5-year alcohol use disorder symptoms at age 35
| Variable | Bivariate associations | Multivariable associations | ||||
|---|---|---|---|---|---|---|
| OR | [95% CI] | p | AOR | [95% CI] | p | |
| Age 29/30 alcohol use | ||||||
| No/low (0–4) drinking | (ref.) | (ref.) | ||||
| Binge (5–9) drinking | 5.76 | [3.96, 8.38] | <.001 | 5.61 | [3.79, 8.30] | <.001 |
| High-intensity (10+) drinking | 13.11 | [7.35, 23.36] | <.001 | 12.26 | [6.70, 22.41] | <.001 |
| Age 18 covariates | ||||||
| Male (vs. female) | 1.39 | [1.06, 1.82] | .016 | 0.98 | [0.72, 1.35] | .920 |
| White (vs. non-White) | 2.01 | [1.95, 2.08] | <.001 | 0.93 | [0.63, 1.36] | .709 |
| Parents college degree (vs. no college degree) | 1.56 | [1.19, 2.04] | .001 | 1.41 | [1.03, 1.91] | .029 |
| Age 29/30 covariates | ||||||
| College graduate (vs. non) | 1.37 | [1.02, 1.85] | .039 | 1.26 | [0.90, 1.76] | .185 |
| Married (vs. not) | 0.62 | [0.47, 0.83] | .001 | 0.81 | [0.57, 1.17] | .265 |
| Any children (vs. none) | 0.67 | [0.50, 0.89] | .007 | 1.01 | [0.71, 1.43] | .970 |
| Employeda | 1.53 | [0.97, 2.41] | .067 | 1.26 | [0.78, 2.04] | .338 |
| Year of age 35 data collection | ||||||
| 2010–2012 | (ref.) | (ref.) | ||||
| 2013–2015 | 1.21 | [0.87, 1.68] | .252 | 1.13 | [0.79, 1.63] | .501 |
| 2016–2018 | 1.49 | [1.07, 2.09] | .020 | 1.24 | [0.85, 1.81] | .272 |
Notes: Unweighted n = 1,253. OR = bivariate odds ratio; AOR = adjusted multivariable odds ratio; CI = confidence interval; ref. = reference.
Employed defined as having two or more jobs, one full-time job, or one part-time job versus full-time homemaker, laid off or waiting to start a job, or no paid employment at all during the first full week of March.
As shown in Table 1, the strength of these associations was attenuated only slightly after covariates were controlled for. In the multivariable model, the adjusted odds of past-5-year AUD symptoms at age 35 remained five times higher (adjusted multivariable OR [AOR] = 5.61) for those reporting age 29/30 binge drinking versus no/low drinking, and more than twice that (AOR = 12.26) for those reporting HID. In an additional multivariable model (not shown), the likelihood of AUD symptoms at age 35 remained more than twice as likely for those reporting HID versus binge drinking (AOR = 2.18, 95% CI [1.14, 4.19], p = .019).
AUD symptom severity
In additional analyses (not tabled), AUD symptoms were modeled as a five-level ordinal outcome (0 = abstainer, 1 = nondisordered, 2 = mild [2–3 criteria], 3 = moderate [4–5 criteria], or 4 = severe [6+ criteria]). In multivariable models using moderate drinking as the referent, higher AUD severity was associated with binge drinking (5–9 drinks; AOR = 5.82, 95% CI [4.13, 8.20], p < .001) and high-intensity drinking (10+ drinks; AOR = 12.49, 95% CI [7.73, 20.19], p < .001). In an additional model using binge drinking as the referent, high-intensity drinking was associated with significantly higher AUD symptom severity (AOR = 2.14, 95% CI [1.32, 3.49], p = .002).
Discussion
In this national longitudinal study, involvement in binge drinking or HID at age 29/30 was associated with a greater likelihood of AUD symptoms at age 35. Although binge drinking (5–9 drinks) was associated with higher risk of AUD symptoms than no/low drinking (0–4 drinks), those who reported HID (10+ drinks) at age 29/30 had significantly higher odds of AUD symptoms at age 35 than either those reporting binge or no/low drinking. HID at the end of young adulthood is a strong risk factor for subsequent symptoms of AUD.
The current study found that approximately one third of age 35 respondents reported AUD symptoms in the past 5 years. These estimates are in line with those obtained from other studies investigating nationally representative samples of U.S. adult alcohol users. Data from the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions–III found that among those ages 30–44, 34.4% reported any lifetime AUD (Grant et al., 2015). Only among those ages 18–29 was lifetime AUD prevalence higher, at 37.0% (Grant et al., 2015).
It was remarkable that almost no respondents who reported binge drinking or HID at age 29/30 went on to report past-5-year abstinence from alcohol use at age 35. This finding speaks to the stability of continued alcohol use among those who engage in binge drinking and HID. Prior research found that individuals were unlikely to start HID after high school (Terry-McElrath & Patrick, 2016), and those who reported HID in 12th grade continued to have high probabilities of participating in HID in 2-year follow-ups throughout their mid-20s (Patrick et al., 2017). Findings from the current study indicate that both binge drinking and HID are markers for sustained risky alcohol use that extends across periods of years. Among adolescents who drink at high-intensity levels, alcohol appears to serve a larger number of functions (i.e., use for more reasons and in more contexts) than for adolescents who report binge drinking or no/low drinking (Terry-McElrath et al., 2017). Such increased reliance on drinking to address daily events and situations may help to perpetuate HID across age and highlights the need for treatment evaluation and support to help reduce drinking intensity among those who engage in HID. Further longitudinal research is needed to examine the extent to which HID persists into midand late adulthood, and the extent to which the additional risks associated with HID continue to be observed.
The current study's results indicated that almost 80% of those who reported HID at age 29/30 also reported past-5-year AUD symptoms at age 35. Although binge drinking was associated with increased risk, HID was a clearer marker for later AUD symptoms. Given the high morbidity and mortality associated with excessive alcohol use and AUD (Bouchery et al., 2011; Centers for Disease Control and Prevention, 2019), identification of specific factors that can help health professionals quickly and effectively assess risk for symptoms of AUD is a priority. The results of the current study indicate that HID may function as one such particular risk factor. Health professionals should consider screening for this extreme drinking behavior. Quick assessments asking individuals about the maximum number of drinks they have consumed within the past 2 weeks may provide a concise and simple way for health care providers to identify individuals who may benefit from more detailed screening tools and/or treatment referrals.
Limitations
The current study's results are subject to limitations. The sample was based on 12th grade students; dropout before 12th grade is associated with increased alcohol use (Tice et al., 2017). Although some bias in study results may have resulted from attrition, use of attrition weights resulted in recapturing baseline sample characteristics on key measures. Monitoring the Future items on binge drinking and HID reflect recent (past-2-week) drinking intensity only and were included in the survey from 2005 onward just for those ages 18–30 (and thus not asked at age 35). Further, symptoms of AUD are first asked at age 35. These factors result in an inability to examine associations between HID and AUD before 2005 or before age 35. These limitations notwithstanding, the current analysis provides data from a national sample of adults to examine associations between drinking intensity—including HID—and later AUD symptoms during mid-adulthood.
Conclusion
This study is one of the first to use HID (compared with binge drinking) as a prospective predictor of AUD symptoms. The majority of prior research focused on the first few years after high school (e.g., among college students); this study clarifies that HID continues throughout the late 20s and is indicative of subsequent problematic drinking. In fact, almost 80% of those reporting HID at age 29/30 later reported AUD symptoms at age 35. High-intensity (10+ drinks) drinkers had significantly greater risk than either binge (5–9 drinks) drinkers or no/low (0–4 drinks) drinkers for AUD symptoms at age 35. Future research that examines additional and longer-term mental and physical health consequences would further enhance our understanding of the impact of HID.
Footnotes
This study was supported by research grant R01AA023504 from the National Institute on Alcohol Abuse and Alcoholism. Data collection and manuscript preparation were supported by research grants R01DA001411 and R01DA016575 from the National Institute on Drug Abuse. The study sponsors had no role in the study design, collection, analysis, or interpretation of the data; writing of the manuscript; or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsors.
References
- Addolorato G., Vassallo G. A., Antonelli G., Antonelli M., Tarli C., Mirijello A., Gasbarrini A. Binge drinking among adolescents is related to the development of alcohol use disorders: Results from a cross-sectional study. Scientific Reports. 2018;12624 doi: 10.1038/s41598-018-29311-y. doi:10.1038/s41598-018-29311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (5th ed.). Arlington, VA: Author; 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Bouchery E. E., Harwood H. J., Sacks J. J., Simon C. J., Brewer R. D. Economic costs of excessive alcohol consumption in the US, 2006. American Journal of Preventive Medicine. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. doi:10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Bray B. C., Dziak J. J., Patrick M. E., Lanza S. T. Inverse propensity score weighting with a latent class exposure: Estimating the causal effect of reported reasons for alcohol use on problem alcohol use 16 years later. Prevention Science. 2019;20:394–406. doi: 10.1007/s11121-018-0883-8. doi:10.1007/s11121-018-0883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention(2019Alcohol-Related Disease Impact (ARDI) application Atlanta, GA: Author; Retrieved from https://www.cdc.gov/alcohol/ARDI/announcement.html [Google Scholar]
- Evans-Polce R. J., Jang B. J., Maggs J. L., Patrick M. E. Gender and age differences in the associations between family social roles and excessive alcohol use. Social Science & Medicine. 2020a;244:112664. doi: 10.1016/j.socscimed.2019.112664. doi:10.1016/j.socscimed.2019.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce R. J., Veliz P. T., Boyd C. J., Hughes T. L., McCabe S. E. Associations between sexual orientation discrimination and substance use disorders: Differences by age in US adults. Social Psychiatry and Psychiatric Epidemiology. 2020b;55:101–110. doi: 10.1007/s00127-019-01694-x. doi:10.1007/s00127-019-01694-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster K. T., Hicks B. M., Iacono W. G., McGue M. Gender differences in the structure of risk for alcohol use disorder in adolescence and young adulthood. Psychological Medicine. 2015;45:3047. doi: 10.1017/S0033291715001014. doi:10.1017/S0033291715001014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein R. B., Chou S. P., Smith S. M., Jung J., Zhang H., Saha T. D., Grant B. F. Nosologic comparisons of DSM-IV and DSM-5 alcohol and drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Journal of Studies on Alcohol and Drugs. 2015;76:378–388. doi: 10.15288/jsad.2015.76.378. doi:10.15288/jsad.2015.76.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowin J. L., Sloan M. E., Stangl B. L., Vatsalya V., Ramchandani V. A. Vulnerability for alcohol use disorder and rate of alcohol consumption. American Journal of Psychiatry. 2017;174:1094–1101. doi: 10.1176/appi.ajp.2017.16101180. doi:10.1176/appi.ajp.2017.16101180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Dawson D. A., Stinson F. S., Chou P. S., Kay W., Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. doi:10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Saha T. D., Chou S. P., Jung J., Zhang H., Hasin D. S. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. doi:10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J. D., Scherrer J. F., Lynskey M. T., Lyons M. J., Eisen S. A., Tsuang M. T., Bucholz K. K. Adolescent alcohol use is a risk factor for adult alcohol and drug dependence: Evidence from a twin design. Psychological Medicine. 2006;36:109–118. doi: 10.1017/S0033291705006045. doi:10.1017/S0033291705006045. [DOI] [PubMed] [Google Scholar]
- Harford T. C., Muthén B. O. The dimensionality of alcohol abuse and dependence: A multivariate analysis of DSM-IV symptom items in the National Longitudinal Survey of Youth. Journal of Studies on Alcohol. 2001;62:150–157. doi: 10.15288/jsa.2001.62.150. doi:10.15288/jsa.2001.62.150. [DOI] [PubMed] [Google Scholar]
- Hingson R. W., Zha W., White A. M. Drinking beyond the binge threshold: predictors, consequences, and changes in the US. American Journal of Preventive Medicine. 2017;52:717–727. doi: 10.1016/j.amepre.2017.02.014. doi:10.1016/j.amepre.2017.02.014. [DOI] [PubMed] [Google Scholar]
- Jang B. J., Schuler M. S., Evans-Polce R. J., Patrick M. E. Marital status as a partial mediator of the associations between young adult substance use and subsequent substance use disorder: Application of causal inference methods. Journal of Studies on Alcohol and Drugs. 2018;79:567–577. doi: 10.15288/jsad.2018.79.567. doi:10.15288/jsad.2018.79.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang J. B., Schuler M. S., Evans-Polce R. J., Patrick M. E. College attendance type and subsequent alcohol and marijuana use in the U.S. Drug and Alcohol Dependence. 2019;204:107580. doi: 10.1016/j.drugalcdep.2019.107580. doi:10.1016/j.drugalcdep.2019.107580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennison K. M. The short term effects and unintended long term consequences of binge drinking in college: a 10 year follow up study. American Journal of Drug and Alcohol Abuse. 2004;30:659–684. doi: 10.1081/ada-200032331. doi:10.1081/ada-200032331. [DOI] [PubMed] [Google Scholar]
- King A. C., McNamara P. J., Hasin D. S., Cao D. Alcohol challenge responses predict future alcohol use disorder symptoms: A 6-year prospective study. Biological Psychiatry. 2014;75:798–806. doi: 10.1016/j.biopsych.2013.08.001. doi:10.1016/j.biopsych.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael A. N., Vasilenko S. A., Lanza S. T., Maggs J. L. High-intensity drinking versus heavy episodic drinking: Prevalence rates and relative odds of alcohol use disorder across adulthood. Alcoholism: Clinical and Experimental Research. 2017;41:1754–1759. doi: 10.1111/acer.13475. doi:10.1111/acer.13475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCambridge J., McAlaney J., Rowe R.2011Adult consequences of late adolescent alcohol consumption: A systematic review of cohort studies PLoS Medicine 8, e1000413.doi:10.1371/journal.pmed.1000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. O. Psychometric evaluation of diagnostic criteria: Application to a two-dimensional model of alcohol abuse and dependence. Drug and Alcohol Dependence. 1996;41:101–112. doi: 10.1016/0376-8716(96)01226-4. doi:10.1016/0376-8716(96)01226-4. [DOI] [PubMed] [Google Scholar]
- Naimi T. S., Nelson D. E., Brewer R. D. The intensity of binge alcohol consumption among U.S. adults. American Journal of Preventive Medicine. 2010;38:201–207. doi: 10.1016/j.amepre.2009.09.039. doi:10.1016/j.amepre.2009.09.039. [DOI] [PubMed] [Google Scholar]
- Nelson C. B., Heath A. C., Kessler R. C. Temporal progression of alcohol dependence symptoms in the U.S. household population: Results from the National Comorbidity Survey. Journal of Consulting and Clinical Psychology. 1998;66:474–483. doi: 10.1037//0022-006x.66.3.474. doi:10.1037/0022-006X.66.3.474. [DOI] [PubMed] [Google Scholar]
- Newton-Howes G., Cook S., Martin G., Foulds J. A., Boden J. M. Comparison of age of first drink and age of first intoxication as predictors of substance use and mental health problems in adulthood. Drug and Alcohol Dependence. 2019;194:238–243. doi: 10.1016/j.drugalcdep.2018.10.012. doi:10.1016/j.drugalcdep.2018.10.012. [DOI] [PubMed] [Google Scholar]
- Pardini D., White H. R., Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and Alcohol Dependence. 2007;88:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. doi:10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M.E. A call for research on high-intensity alcohol use. Alcoholism: Clinical and Experimental Research. 2016;40:256–259. doi: 10.1111/acer.12945. doi:10.1111/acer.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M. E., Bray B. C., Berglund P. A. Reasons for marijuana use among young adults and long-term associations with marijuana use and problems. Journal of Studies on Alcohol and Drugs. 2016;77:881–888. doi: 10.15288/jsad.2016.77.881. doi:10.15288/jsad.2016.77.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M. E., Schulenberg J. E., O’Malley P. M., Johnston L. D., Bachman J. G. Adolescents’ reported reasons for alcohol and marijuana use as predictors of substance use and problems in adulthood. Journal of Studies on Alcohol and Drugs. 2011;72:106–116. doi: 10.15288/jsad.2011.72.106. doi:10.15288/jsad.2011.72.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M. E., Terry-McElrath Y. M., Schulenberg J. E., Bray B. C. Patterns of high-intensity drinking among young adults in the United States: A repeated measures latent class analysis. Addictive Behaviors. 2017;74:134–139. doi: 10.1016/j.addbeh.2017.06.004. doi:10.1016/j.addbeh.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M. E., Wightman P., Schoeni R. F., Schulenberg J. E. Socioeconomic status and substance use among young adults: A comparison across constructs and drugs. Journal of Studies on Alcohol and Drugs. 2012;73:772–782. doi: 10.15288/jsad.2012.73.772. doi:10.15288/jsad.2012.73.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riala K., Hakko H., Isohanni M., Järvelin M. R., Räsänen P. Teenage smoking and substance use as predictors of severe alcohol problems in late adolescence and in young adulthood. Journal of Adolescent Health. 2004;35:245–254. doi: 10.1016/j.jadohealth.2003.08.016. doi:10.1016/j.jadohealth.2003.08.016. [DOI] [PubMed] [Google Scholar]
- Room R., Babor T., Rehm J. Alcohol and public health. The Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. doi:10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- Samokhvalov A. V., Popova S., Room R., Ramonas M., Rehm J. Disability associated with alcohol abuse and dependence. Alcoholism: Clinical and Experimental Research. 2010;34:1871–1878. doi: 10.1111/j.1530-0277.2010.01275.x. doi:10.1111/j.1530-0277.2010.01275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J. E., Johnston L. D., O’Malley P. M., Bachman J. G., Miech R. A., Patrick M. E.2018Monitoring the Future national survey results on drug use 1975–2017. Volume IICollege students and adults ages 19–55.Ann Arbor, MI: Institute for Social Research, The University of Michigan; Retrieved from http://monitoringthefuture.org/pubs.html#monographs [Google Scholar]
- Schulenberg J. E., Maggs J. M., O’Mally P. M.2003How and why the understanding of developmental continuity and discontinuity is important: The sample case of long-term consequences of adolescent substance use In Mortimer J. T., Shanahan M. J.Eds.), Handbook of the life coursepp. 413–436New York: Plenum Publishers [Google Scholar]
- Schulenberg J. E., Patrick M. E., Kloska D. D., Maslowsky J., Maggs J. L., O’Malley P. M.2016Substance use disorder in early midlife: A national prospective study on health and well-being correlates and long-term predictors Substance Abuse: Research and Treatment 9, Supplement 141–57.doi:10.4137/SART.S31437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley J. R., Farmer R. F., Kosty D. B., Gau J. M. Prevalence, incidence, recovery, and recurrence of alcohol use disorders from childhood to age 30. Drug and Alcohol Dependence. 2019;194:45–50. doi: 10.1016/j.drugalcdep.2018.09.012. doi:10.1016/j.drugalcdep.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahre M., Roeber J., Kanny D., Brewer R. D., Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing Chronic Disease. 2014;11:E109. doi: 10.5888/pcd11.130293. doi:10.5888/pcd11.130293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2019Results from the 2018 National Survey on Drug Use and Health: Detailed tables Rockville, MD: Author; Retrieved from https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2018R2/NSDUHDetailedTabs2018.pdf [Google Scholar]
- Terry-McElrath Y. M., Patrick M. E. Intoxication and binge and high-intensity drinking among US young adults in their mid-20s. Substance Abuse. 2016;37:597–605. doi: 10.1080/08897077.2016.1178681. doi:10.1080/08897077.2016.1178681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath Y. M., Stern S. A., Patrick M. E. Do alcohol use reasons and contexts differentiate adolescent high-intensity drinking? Data from U.S. high school seniors, 2005-2016. Psychology of Addictive Behaviors. 2017;31:775–785. doi: 10.1037/adb0000314. doi:10.1037/adb0000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tice P., Lipari R. N., Van Horn S. L. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. Substance use among 12th grade aged youths, by dropout status. The CBHSQ Report: August 15, 2017. Retrieved from https://www.samhsa.gov/data/sites/default/files/report_3196/ShortReport-3196.html. [PubMed] [Google Scholar]
- World Health Organization 2014Global status report on alcohol and health 2014 Poznyak V., Rekve D.Eds.). Geneva: Author; Retrieved from https://www.who.int/substance_abuse/publications/alcohol_2014/en/ [Google Scholar]
- Zucker R. A., Wong M. M., Clark D. B., Leonard K. E., Schulenberg J. E., Cornelius J. R., Puttler L. I. Predicting risky drinking outcomes longitudinally: what kind of advance notice can we get? Alcoholism: Clinical and Experimental Research. 2006;30:243–252. doi: 10.1111/j.1530-0277.2006.00033.x. doi:10.1111/j.1530-0277.2006.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]