Abstract
Objective
The purpose of this study was to systematically evaluate the efficacy and safety of acupuncture combined with the WHO three-step analgesic drug ladder for cancer pain.
Methods
The Cochrane Library, PubMed, and CNKI Database of Systematic Reviews were searched. Using the Cochrane Register for Randomized Controlled Trials, the quality of the included literature was evaluated, and the meta-analysis was carried out with RevMan 5.3 software.
Results
Compared with three-step analgesia alone, acupuncture combined with three-step analgesia for cancer pain increased pain relief response rates (RR = 1.12, 95% CI: 1.08∼1.17, P < 0.00001), reduced NRS score (SMD = −1.10, 95% CI: −1.86∼−0.35, P=0.004), reduced the rate of side effects (RR = 0.45, 95% CI: 0.38∼0.53, P < 0.00001), including nausea (P < 0.00001), vomiting (P=0.008), constipation (P < 0.00001), and dizziness (P=0.010), reduced the burst pain rate (SMD = −1.38; 95% CI: −2.44∼−0.32, P=0.01), shortened analgesia effect onset time (P=0.004), and extended the duration of response (P < 0.0001).
Conclusion
For the treatment of cancer pain, acupuncture combined with three-step analgesic drugs is better than using only three-step analgesic drugs.
1. Introduction
Pain is one of the most debilitating symptoms experienced by patients with advanced cancer. According to WHO statistics, 70% of cancer patients worldwide have some degree of pain in the advanced stages of cancer [1]. Because the pain is intense and easily aggravated, it directly affects the appetite, sleep, psychological status, and treatment effect of patients, reduces their quality of life, and increases their psychological stress [2, 3]. Cancer pain has become a medical, psychological, and social issue of great concern. At present, the treatment of cancer pain mostly utilizes the three-step “ladder” treatment principle proposed by the WHO, where mild, moderate, and severe pain are treated with nonsteroidal anti-inflammatory drugs (NSAIDs), weak opioids, and strong opioids, respectively [4]. Although the analgesic effect of three-step drugs is good, their side effects, such as liver and kidney function damage, risk of dependency and addiction, respiratory inhibition, and gastrointestinal side effects, limit their clinical application [5]. One primary reason why cancer pain is difficult to control is because cancer pain patients cannot tolerate the side effects of analgesics. Therefore, there is a consensus to seek other effective and safe analgesic methods [6]. Acupuncture is an important part of TCM. Acupuncture is to insert a needle at one of the patient's acupoints and use a specific manipulation to stimulate the patient's acupoints to achieve an effect (DE QI). Acupuncture has outstanding performance in the treatment of all kinds of pain through its principle of moving qi, dredging qi channels and collaterals, and activating blood. Various acupuncture treatments can be combined, with no risk of addiction, no side effects, convenient application and at a low cost, demonstrating the unique advantages of TCM in the treatment of cancer pain [7]. In the last 20 years, there have been many clinical reports on the utility and safety of acupuncture for the treatment of cancer pain, and acupuncture therapy is a widely recognised alternative measure for the treatment of cancer pain. Therefore, it is necessary to use a systematic evaluation method to rigorously evaluate the randomised controlled study of acupuncture combined with three-step analgesic drugs to treat cancer pain, to assess its exact effect in the treatment of cancer pain.
2. Methods
2.1. Data Sources
The following databases were searched from their inception to January 10, 2021: the Cochrane Library, PubMed, Embase, CNKI, China Biology Medicine disc (CBMdisc), Chinese Journal of Science and Technology database (VIP), and Wanfang database. We searched MeSH (Medical Subject Headings) term trees for “acupuncture” and “pain” in PubMed, and the keywords searched included “acupuncture”, “needling”, “tumour”, “cancer”, “neoplasm”, “ache”, “pain”, and “randomised controlled trial”. The keywords were translated into Chinese and searched in the above-mentioned Chinese databases. Search terms were combined with the Boolean “AND” and “OR” terms in search strategies, for example, (“acupuncture” OR “needling”) AND (“cancer” OR “tumour” OR “neoplasm” OR “ache” OR “pain”) AND (“randomised controlled trial”). Comprehensive retrieval was carried out according to the characteristics of different databases. Then, the literature mentioning “randomised controlled” and “randomised grouped” was screened. In addition, we manually searched our own personal literature files. After reading the full text of the included literature and related articles, we collected the documents together in hard copy format for preservation.
2.2. Inclusion Criteria
2.2.1. Types of Studies
The included studies were all randomised controlled clinical trials. The published experiments included were mainly in the form of theses and abstracts. There were no restrictions on the language of publication.
2.2.2. Types of Participants
The subjects were patients with malignant tumours confirmed by cytology or histopathology, and all patients had cancer pain. There were no limits on age, gender, race, and nationality of the patients; however, patients had to be able to clearly describe their pain to medical staff.
2.2.3. Types of Interventions
In the literature, the intervention treatment group was treated with acupuncture augmented by three-step analgesia, including traditional acupuncture or other acupuncture methods, such as ear acupuncture and electroacupuncture. Acupuncture points included traditional acupuncture points and pain points. The control groups only received three-step analgesic treatment.
2.2.4. Types of Outcome Evaluations
The included materials had a clear evaluation standard for curative effects and at least one clinical index related to cancer pain, including the effective rate of pain relief after treatment, quality of life score, side effect rates, burst pain rate, onset time to analgesic effect, and duration of response.
2.3. Exclusion Criteria
The exclusion criteria were as follows: if patients had one or more other type(s) of pain in addition to cancer pain; if the study used moxibustion, percutaneous electrical stimulation of nerves, acupoint injection, laser irradiation, cupping, massage, herbal medicines, or other intervention measures; if the experiments were carried out on patients during or a few days after surgical therapy, radiotherapy, chemotherapy, or hyperthermia-therapy on their malignant tumours; if the trial design was not rigorous; if inappropriate statistical methods were used; if the paper was only an abstract, review, or summary of previously published literature; if the study has no result indicators; if the experimental design was unreasonable; or if the literature could not be obtained by contacting the author.
2.4. Data Extraction and Bias Risk Assessment
Two researchers independently evaluated the quality of each study meeting the inclusion criteria and extracted the data, including the baseline situation, intervention measures, and efficacy results, and cross-checked the data. Any disagreements were resolved through discussion or assessment by a third researcher. We used a “Modification of Cochrane Tool to assess the risk of bias in randomised trials,” where a decision regarding bias must be made, categorised into “probably no” or “probably yes,” for items that are thought to be of unclear risk [8]. We judged trials with more than 2 and more than 4 high-risk components as moderate risk and high risk, respectively [9]. The following criteria were used to assess the risk of bias: whether the study was randomised; how allocation concealment was conducted; whether the study was double-blind or triple-blind; whether the results data were complete; and whether there was selective reporting or other types of bias. The authors categorised studies into “low risk,” “unclear risk,” and “high risk” categories. For dropout patients, we contacted the authors of the studies twice over four weeks via e-mail for missing or unclear data. If missing data could not be found, they were recorded as high risk; if no response was received, the data were marked as unclear risk. All authors reached a consensus on the results of bias risk assessment.
2.5. Data Synthesis
The effect of acupuncture combined with three-step analgesic drug therapy for treatment of cancer pain was analyzed in terms of response rate, numerical rating scale (NRS), side effect rates, times of burst pain, onset time, and duration of response (DOR). If the information included in the study was insufficient, we communicated with the main author to obtain accurate data. RevMan 5.3 software provided by the Cochrane Collaboration Network was used for the meta-analysis. The relative risk (RR) was used for the enumeration data, the mean difference (MD) was used for the measurement data, and the 95% confidence interval (CI) was used for each effect quantity. When the heterogeneity of test results was not statistically significant (P > 0.05), a fixed effects model was selected; when the heterogeneity of test results was statistically significant (P < 0.05), a random effects model was selected. A funnel plot was used to analyse and detect publication bias.
3. Results
3.1. Study Description
The first search found 115 potentially relevant articles. After reading and screening, 19 articles met our inclusion criteria (Figure 1). The critical data from all the included RCTs are shown in Table 1 [10–28]. In total, 1502 cancer pain cases were included. The numbers of cases of acupuncture combined with three-step analgesic drug therapy (treatment group) and three-step analgesic drug therapy (control group) were 751 and 751, respectively. All patients' cancers were confirmed by cell histology or pathology, and pain was their main symptom. The baseline was comparable between the two groups. Almost all of the research was on the use of manual acupuncture (AT), which is guided by the theory of TCM for acupuncture interventions. Two studies used electroacupuncture (EA) [11, 28]. One study used floating acupuncture (FA) [12]. Two studies used fire needle (FN) [13, 14]. Three studies used wrist-ankle acupuncture (WA) [17–19]. Among them, the two acupuncture methods were all included in Fu Yang et al.'s report [17], in which morphine hydrochloride sustained-release tablets and acupuncture or wrist-ankle acupuncture were used in the treatment of cancer pain. All studies provided patients with a semistandardised acupuncture programme, that is, the use of a predefined set of acupoints combined with a set of acupoints according to the location of the tumour. The Ashi point, Zusanli (ST36), Hegu (LI4), Sanyinjiao (SP6), and Taichong (LR3) points were most frequently used. For most studies, patients received acupuncture treatment for 1 to 3 weeks, for durations of 20 to 60 min per session. The evaluation criteria for the curative effect were similar across studies. The objective outcome measures were treatment response rate, NRS, side effect rates (nausea, vomiting, constipation, hiccups, dizziness, itching, palpitation, and abdominal distention), times of burst pain, onset time to analgesic effect (min), DOR (h), quality of life (QOL), Karnofsky performance status (KPS), and quality of life questionnaires (QLQ-C30). The minimal important difference (MID) refers to the change in the score of the smallest efficacy evaluation questionnaire recognised by the patient. MID indicates an important improvement in symptoms and signs; the intervention has achieved the minimal important difference.
Figure 1.

Flowchart of the literature review and selection process.
Table 1.
Summary of randomised clinical studies of acupuncture combined with three-step analgesic drug therapy for the treatment of cancer pain.
| Study (year) | Type of cancer | Sample sizes | Interventions | Acupuncture point selection | Session frequency and duration | Main outcomes and assessment of pain | ||
|---|---|---|---|---|---|---|---|---|
| T | C | T | C | |||||
| Wang (2018) [10] | Various | 35 | 35 | AT + C | Drug (three-step analgesic ladder) | LI4, LR3, and Ashi point | 30 min qd 6 weeks | Response rate, NRS, and side effect rate |
|
| ||||||||
| Wang (2016) [11] | Lung cancer | 30 | 30 | EA + C | Oxycodone sustained-release tablets | LI4, PC6, ST36, and SP6 | 30 min qd 14 days | Response rate, NRS, side effect rate, burst pain, onset time, and DOR |
|
| ||||||||
| Zhong (2016) [12] | Various | 30 | 30 | FA + C | Morphine sulfate sustained-release tablets | Ashi point | Once a day 14 days | Response rate, QOL, and burst pain |
|
| ||||||||
| Mi (2010) [13] | Gastric cancer | 32 | 30 | FN + AT + C | Drug (three-step analgesic ladder) | FN: BL21, BL18, and BL17. AT: CV12, ST25, and St36 | 30 min qod 4 weeks | Response rate and side effect rate |
|
| ||||||||
| Bai (2019) [14] | Various | 50 | 50 | FN + C | Drug (three-step analgesic ladder) | Ashi point, ST36, and SP6 | qod 14 days | Response rate, NRS, and side effect rate |
|
| ||||||||
| Liu (2018) [15] | Various | 72 | 75 | TEAS + C | Drug (three-step analgesic ladder) | LI4, PC6, ST36, and SP6 | 30 min bid 3 weeks | Response rate, BPI-S, KPS, and side effect rate |
|
| ||||||||
| Liu (2011) [16] | Liver cancer | 30 | 30 | AT + C | Tramadol hydrochloride sustained-release tablets | SP4, PC6, GB41, TE5, SI3, BL62, LU7, KI6, LR3, and LR14 | qd 14 days | Response rate, NRS, QOL, side effect rate, onset time, and DOR |
|
| ||||||||
| Fu (2019) [17] | Various | 16/16 | 16 | AT + C | Morphine hydrochloride sustained-release tablets | PC6 and SP6 | 1 h qd | Response rate, NRS, KPS, side effect rate, burst pain, onset time, and DOR |
| WA + C | ||||||||
|
| ||||||||
| Wu (2019) [18] | Various | 30 | 30 | WA + C | Drug (three-step analgesic ladder) | Based on syndrome differentiation and disease differentiation | 12 h qd 10 days | Response rate, VAS, burst pain, and side effect rate |
|
| ||||||||
| Dong (2018) [19] | Various | 60 | 60 | WA + C | Drug (three-step analgesic ladder) | Based on syndrome differentiation and disease differentiation | 10–12 h qd 7 days | Response rate, NRS, QLQ-C30, and side effect rate |
|
| ||||||||
| Sun (2016) [20] | Various | 30 | 30 | AT + C | Oxycodone | LI4, PC6, ST36, SP6, Ashi point, and others | 30 min qd 14 days | Response rate, NRS, KPS, QOL, and side effect rate |
|
| ||||||||
| Zhang (2014) [21] | Various | 30 | 30 | AT + C | Drug (three-step analgesic ladder) | LI4 and ST36. Lung cancer: PC6 and LU6. Liver cancer: GB34, LR6, and LR3. Colorectal cancer: PC6, CV12, and TE6 | 30 min qd 7 days | Response rate, QOL, side effect rate, onset time, and DOR |
|
| ||||||||
| Hui (2019) [22] | Various | 40 | 40 | AT + C | Drug (three-step analgesic ladder) | Ashi point, LI4, GV14, BL11, GB34, and LR3 | 30 min qd 14 days | Response rate, side effect rate, onset time, and DOR |
|
| ||||||||
| Tan (2012) [23] | Various | 106 | 101 | AT + C | Drug (three-step analgesic ladder) | LI4 and PC6. Lung cancer: LU6. Liver cancer: GB34 and LR6. Colorectal cancer: CV12, ST36, and TE6 | 0.5–1 h qd 3 weeks | Response rate and side effect rate |
|
| ||||||||
| Fan (2017) [24] | Lung cancer | 35 | 34 | AT + C | Drug (three-step analgesic ladder) | PC6, LI4, ST36, GB34, and SP6 | 20 min qd 20 days | Response rate, NRS, onset time, and DOR |
|
| ||||||||
| Jiang (2016) [25] | Various | 25 | 25 | AT + C | Drug (three-step analgesic ladder) | Ashi point, LR3, and LI4 | 30 min qd 7 days | Response rate and NRS |
|
| ||||||||
| Li (2017) [26] | Gastric cancer | 30 | 30 | AT + C | Drug (three-step analgesic ladder) | ST36, LR3, and LI4 | 30 min qd 7 days | Response rate, NRS, QOL, and side effect rate |
|
| ||||||||
| Huang (2018) [27] | Various | 31 | 31 | AT + C | Drug (three-step analgesic ladder) | PC6. Lung cancer: LI4, LU4, LU6, and ST36. Liver cancer: GB34 and LR3. Breast cancer: LI4, STI8, and CV9. Gastric cancer: CV12, ST36, and TE6 | 30 min qd 7 days | Response rate |
|
| ||||||||
| Peng (2012) [28] | Various | 23 | 24 | EA + C | Drug (three-step analgesic ladder) | LI4, PC6, ST36, and SP6 | 30 min qd 7 days | Response rate, onset time, and DOR |
T: treatment group, C: control group, AT: acupuncture, EA: electroacupuncture, FA: floating acupuncture, FN: fire needle, WA: wrist-ankle acupuncture, DOR: duration of response, NRS: numerical rating scale, BPI-S: brief pain inventory-severity, QOL: quality of life, and KPS: Karnofsky performance status.
3.2. Risk of Bias
Most included RCTs had a high risk of bias. Nineteen RCTs [10–28] described their randomisation methods. Among them, 9 RCTs [10, 12–14, 16–18, 22, 24] used a random number table, 1 study [15] used a computer-generated random number sequence for randomisation, and 3 RCTs [20, 21, 26] randomly numbered cases according to the order of hospitalization. Three RCTs [10, 15, 17] described incomplete outcome methods, and these three studies had cases of dropouts. Two studies reported details about allocation concealment [15, 16]. Fourteen RCTs described adverse events from acupuncture combined with three-step analgesic drugs [10, 11, 13–23, 26]. Table 2 presents the Cochrane risk of bias assessment of the included articles. There were 2 trials with high risks of bias [10, 17], 5 trials with moderate risk of bias [12, 15, 18, 23, 25], and 12 trials with low risk of bias [11, 13, 14, 16, 19–22, 24, 26–28]. A high risk of bias resulted from lack of blinding of participants and personnel and lack of blinding among outcome assessors. A moderate risk resulted from selective reporting bias and incomplete outcome data, and a low risk of bias resulted from randomisation sequence generation and allocation concealment (see Figure 2).
Table 2.
Risk of bias for the 19 included studies using a modified approach to the Cochrane risk of bias tool.
| Risk of bias | Trial characteristics | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Source | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Infrequent loss to follow-up | Free of selective outcome reporting | Free of other types of bias | Statistical analysis (per protocol, intention to treat, etc.) | How is loss to follow-up handled? | Adverse event |
| Wang (2018) [10] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely no | Definitely no | Definitely no | Not mentioned | Ignored | Yes |
|
| ||||||||||
| Wang (2016) [11] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Zhong (2016) [12] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely no | Probably yes | Per protocol | Not mentioned | No |
|
| ||||||||||
| Mi (2010) [13] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Bai (2019) [14] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Liu (2018) [15] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely no | Definitely yes | Probably yes | Not mentioned | Ignored | Yes |
|
| ||||||||||
| Liu (2011) [16] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Fu (2019) [17] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely no | Definitely no | Definitely no | Per protocol | Ignored | Yes |
|
| ||||||||||
| Wu (2019) [18] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely no | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Dong (2018) [19] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Sun (2016) [20] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Zhang (2014) [21] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Per protocol | Not mentioned | Yes |
|
| ||||||||||
| Hui (2019) [22] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Tan (2012) [23] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely no | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Fan (2017) [24] | Definitely yes | Definitely yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Per protocol | Not mentioned | No |
|
| ||||||||||
| Jiang (2016) [25] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely no | Probably yes | Per protocol | Not mentioned | No |
|
| ||||||||||
| Li (2017) [26] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | Yes |
|
| ||||||||||
| Huang (2018) [27] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Not mentioned | Not mentioned | No |
|
| ||||||||||
| Peng (2012) [28] | Probably yes | Probably yes | Probably no | Probably no | Definitely yes | Definitely yes | Probably yes | Per protocol | Not mentioned | No |
Figure 2.

Cochrane risk of bias by trial.
3.3. Response Rates
Eighteen studies reported the response rates to pain relief after treatment [10–14, 16–28]. In the treatment group, 621 out of the 679 cases had effective responses; in the control group, among the 672 cases, 548 had effective responses. The heterogeneity test in the meta-analysis showed that χ2 = 22.19, P=0.22, I2 = 19%, and there was no significant difference between the studies, so a fixed effects model was used. The total response rate of the treatment group was better than that of the control group, and the difference was statistically significant (n = 1351, RR = 1.12; 95% CI: 1.08∼1.17, P < 0.00001; see Figure 3).
Figure 3.

Forest plot of the total response rates of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
3.4. NRS Score
Seven studies reported NRS scores after treatment [10, 11, 14, 17, 19, 22, 24]. Overall, 282 cases were in the treatment group, and 281 were in the control group. The heterogeneity test of the meta-analysis showed that χ2 = 158.90, P < 0.00001, I2 = 96%, and the differences between the studies were statistically significant, so a random effects model was used. The NRS score of the treatment group was lower than that of the control group, and the difference was statistically significant (n = 563, SMD = −1.10, 95% CI: −1.86∼−0.35, Z = 2.87, P=0.004; see Figure 4).
Figure 4.
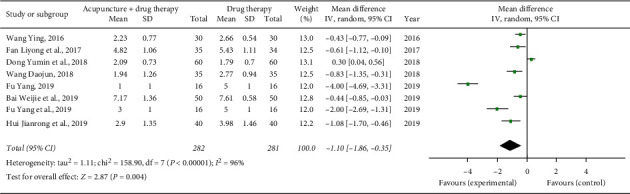
Forest plot of NRS score of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
3.5. Side Effect Rates
Side effects mainly included nausea, vomiting, constipation, and dizziness. Eight studies reported the number of cases of nausea [10, 13, 16, 18, 21–23, 26], 7 studies reported the number of cases of vomiting [10, 13, 16, 18, 21, 22, 26], 11 studies reported the number of cases of constipation [10, 11, 13, 16–18, 20–23, 26], and 5 studies reported the number of cases of dizziness [11, 13, 17, 20, 22]. The consolidated statistics results demonstrated that, compared to the control group, in the treatment group, the incidence of nausea (n = 659, RR = 0.48, 95% CI: 0.34∼0.66, P < 0.00001), vomiting (n = 452, RR = 0.56, 95% CI: 0.37∼0.86, P=0.008), constipation (n = 843, RR = 0.38, 95% CI: 0.29∼0.49, P < 0.00001), and dizziness (n = 326, RR = 0.53, 95% CI: 0.33∼0.86, P=0.010) decreased (see Figure 5).
Figure 5.

Forest plot of side effect rates of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
3.6. Burst Pain
Four studies reported the mean number of burst pain events [11, 12, 17, 18]. The heterogeneity test in the meta-analysis showed that χ2 = 78.30, P < 0.00001, I2 = 95%, and the differences between the studies were statistically significant, so a random effects model was used. The combined statistical results showed that the incidence of burst pain in the treatment group was lower than that in the control group (n = 244, SMD = −1.38, 95% CI: −2.44∼−0.32, P=0.01; see Figure 6).
Figure 6.

Forest plot of times of burst pain of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
3.7. Onset Time to Analgesic Effect and Duration of Response
Five studies reported the mean onset time [11, 17, 19, 24, 28]. The combined statistical results showed that the onset time in the treatment group was shorter than that in the control group (n = 360, SMD = −20.11, 95% CI: −33.90∼−6.33, P=0.004). Six studies reported the mean duration of response [11, 17, 19, 22, 24, 28]. The combined statistical results showed that the duration of response in the treatment group was longer than that in the control group (n = 440, SMD = 3.22, 95% CI: 1.63∼4.80, P < 0.0001); see Figures 7 and 8.
Figure 7.
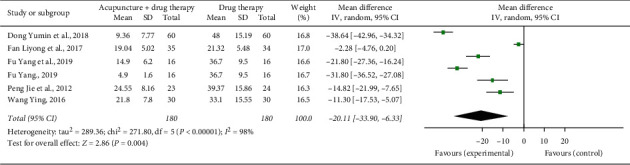
Forest plot of the onset time of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
Figure 8.

Forest plot of the duration of response of acupuncture combined with three-step analgesic drugs versus three-step analgesic drugs alone for cancer pain.
3.8. Publication Bias
Publication bias, which has always been a problem in meta-analysis, refers to the fact that research with positive results is easier to publish than research with negative results. The funnel chart analysis results of the main outcome indicators of the response rates of pain relief suggested that publication bias might exist and exaggerate the efficacy of acupuncture combined with three-step analgesic drugs in the treatment of cancer pain; see Figure 9.
Figure 9.

Total efficiency funnel.
4. Discussion
Cancer is a significant global public health issue, and the disease burden is growing. Globally, there are 18.1 million new cancer cases and 9.6 million cancer deaths each year; cancer deaths are expected to exceed 13 million by 2030, and 70% of cancer deaths globally occur in low-income and middle-income countries. In China in 2018, nearly 24% (4.3 million) of global new cases and 30% (2.9 million) of deaths occurred [29, 30]. China is the largest developing country. Chinese doctors need to pay attention to promoting cancer prevention for people and treating cancer patients. Cancer pain is severe, intolerable, and intractable pain, and such pain is a main symptom in the advanced stages of malignant tumours. When the tumour body markedly enlarges, tissue necrosis, erosion, and so on result in severe compression of, damage to, and irritation of the nerve sheath, nerve fibres, and blood vessels. Although there are many ways to treat cancer pain, many years of clinical experience at home and abroad indicate that providers believe that drug therapy is still the most common and effective way to control cancer pain. The WHO three-step cancer pain treatment programme has become an internationally accepted cancer pain drug treatment method that can control most cancer pain; however, three-step pain drugs, especially opioids, are often accompanied by side effects such as nausea, vomiting, constipation, drowsiness, dizziness, and respiratory depression [31].
There are many ways to treat cancer, but in recent years, TCM has played an increasingly important role in cancer prevention and treatment. As an integral part of TCM, acupuncture has been used to treat pain for thousands of years. The complications of acupuncture in the treatment of pain diseases are fewer than those of drug treatment [32]. Wang Limei et al. reported that [33] complications such as pneumothorax, dizziness, pain, needle syncope, infection, and visceral puncture can occur due to improper acupuncture manipulation; however, when doctors master anatomical knowledge, perform acupuncture correctly, and sterilise needles strictly, complications are further reduced. Modern research shows that the mechanism of acupuncture analgesia may be related to regulating the self-healing of the body, changing patients' perceptions of pain, and affecting the conduction of the central nervous system [34]. Another possible acupuncture mechanism is stimulation/excitation of the endogenous pain modulation system, which induces the secretion of endogenous opioids, blocks the transmission of neurotransmitters, and regulates the perception of pain to achieve analgesia [35]. A third possibility is that the pain signals from acupuncture are modulated in the pain receptor areas, and the dorsal root ganglion cells of the outgoing primary neurons transmit the signal to the near end of the secondary neurons. The pain signal produced by acupuncture may then induce the secretion of endogenous opioids and analgesia in the periaqueductal grey matter of the midbrain, or it may induce the penetration of electric ions, stimulate neurons, and exert an inhibitory effect in the intercellular area of the periaqueductal grey matter of the midbrain [36]. The exact mechanism of acupuncture's analgesic effect has not yet been elucidated. However, this review of acupuncture treatment of cancer pain with a large number of RCT experiments demonstrated that acupuncture treatment of cancer has fewer adverse reactions such as nausea and vomiting than analgesic drug treatment alone. Acupuncture treatment for cancer pain is considered to have sufficient evidence to determine its effectiveness [37]; these results are encouraging and support further research on acupuncture treatment for cancer.
5. Conclusion
Based on the meta-analysis of 19 studies, compared with the treatment of cancer pain with three-step analgesic drug treatment alone, the response rates of pain relief from acupuncture combined with three-step analgesic drug treatment were higher, the NRS scores were lower, the incidence of adverse reactions such as nausea and vomiting was less frequent, the incidence of times of burst pain was also less frequent, the onset time to analgesic effect was shorter, and the duration of pain response was longer.
There were several limitations in this study. The lack of high-quality studies in the literature may limit the validity of the results. Meta-analyses generally face methodological challenges such as insufficient literature retrieval, potential selection bias for which studies are included, and inappropriate evaluation of the quality of the original research. This study only included published literature and did not search for unpublished literature; in addition, there may be publication bias in the literature.
In conclusion, this study shows that acupuncture combined with three-step analgesic drugs has specific advantages over three-step analgesic drugs alone in the treatment of cancer pain. It is hoped that, in the future, rigorous randomised controlled trials will be carried out with multicentre and large-sample studies to determine acupuncture's exact curative effect and further demonstrate the superiority of acupuncture combined with three-step analgesic drugs over the use of such drugs alone to treat cancer pain.
Acknowledgments
This research was supported by the National Natural Science Foundation of China (Grant no. 81603412); Key R&D Projects of Hebei Province (Grant no. 18277731D); Scientific Research Project of Hebei Administration of Traditional Chinese Medicine (Grants nos. 2017163, 2019008, and 2020014); General Projects for Improving Scientific Research Capacity of Hebei College of Traditional Chinese Medicine (Grant no. KTY2019009); Hebei Key Laboratory of Chinese Medicine Research on Cardio-Cerebrovascular Disease; Key Laboratory of Integrated Traditional Chinese and Western Medicine Hepatonephrosis in Hebei Province (Grant no. A201902); and Hebei Province “Three Three Three Talent Project” funded project (Grant no. A202002008).
Data Availability
The data can be obtained from the author upon reasonable request.
Conflicts of Interest
All the authors declare no conflicts of interest.
Authors' Contributions
De-hui Li conceived and designed the study, analysed and interpreted the data, and drafted the manuscript. Yi-fan Su and Na Guo contributed to the literature searches, study selection, data extraction, and data synthesis. Huan-fang Fan and Chun-xia Sun assisted in the development of search strategies and critically reviewed the manuscript. All the authors read and approved the final version of the manuscript.
References
- 1.Bouhassira D., Luporsi E., Krakowski I. Prevalence and incidence of chronic pain with or without neuropathic characteristics in patients with cancer. Pain. 2017;158(6):1118–1125. doi: 10.1097/j.pain.0000000000000895. [DOI] [PubMed] [Google Scholar]
- 2.Tang F. P., Ding L. P., Qin Y., et al. A bibliometric-based analysis of cancer pain care research hotspots in China and abroad. Journal of Guangxi Medical University. 2020;37(9):1716–1720. [Google Scholar]
- 3.Ding C., Li B., Wu X. M., et al. A clinical study of simple implantable epidural infusion system in the treatment of regional intractable cancer pain. Chinese Journal of Pain Medicine. 2015;21(8):626–629. [Google Scholar]
- 4.Li W. J., Liu J. Y., Si Q., et al. Development and change of the vision of drug treatment for cancer pain. Herald of Medicine. 2021;40(1):45–51. doi: 10.1016/j.accpm.2021.100902. [DOI] [Google Scholar]
- 5.Bu L. J., An C., Bao W. Q., et al. Prof. Wang Pei’s experience in treating cancer pain. Modern Chinese Clinical Medicine. 2021;28(1):22–26. [Google Scholar]
- 6.Zhong A. H., Xie Q., Chen Q., et al. Comparison of clinical effects of oxycontin and methadone in the treatment of severe cancer pain. Chinese Journal of Clinical Oncology and Rehabilitation. 2015;22(1):112–115. [Google Scholar]
- 7.Chen X. X., YAO M. H., Sai J. T., et al. The study of the analgesic effect of acupuncture in cancer pain. World Chinese Medicine. 2020;15(15):2346–2353. [Google Scholar]
- 8.Guyatt G. H., Busse J. W. Modification of Cochrane Tool to Assess Risk of Bias in Randomized Trials. 2011, http://distillercer.com/resources/ [Google Scholar]
- 9.Fallah A., Akl E. A., Ebrahim S., et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS One. 2012;7(8):p. e43407. doi: 10.1371/journal.pone.0043407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D. J. Clinical Research on Acupuncture Manipulation of “Reinforcing in the Upper and Reducing in the Lower” for Cancer Pain. Hangzhou, China: Zhejiang Chinese Medical University; 2018. [Google Scholar]
- 11.Wang Y. The Clinical Research of Electro-Acupuncture Therapy Combined with Oxycontin to Treat the Pain of Advanced Non-small Cell Lungcancer. Hangzhou, China: Zhejiang Chinese Medical University; 2016. [Google Scholar]
- 12.Zhong H. Clinical effective observation of floating-needle assisted therapy for moderate cancer pain of patients. Chinese Journal of Acupuncture and Moxibustion (Electronic Edition) 2016;5(4):148–151. [Google Scholar]
- 13.Mi J. P., Deng T. W., Zhou D. J. Clinical observation on the treatment of pain in gastric cancer by fire acupuncture combined with three steps analgesic method. Liaoning Journal of Traditional Chinese Medicine. 2010;37(10):2018–2019. [Google Scholar]
- 14.Bai W. J., Liu E. M., Fang C. T., et al. A clinical study on the treatment of cancer pain by needling with milli fire needle based on the theory of “fire is smooth, general principle is not painful”. Chinese Manipulation & Rehabilitation Medicine. 2019;10(15):14–17. [Google Scholar]
- 15.Liu Y. Effect Analysis and Safety Evaluation of Three Ladder Analgesic Method Combined with TEAS in the Treatment of Moderate and Severe Cancer Pain. Hangzhou, China: Zhejiang Chinese Medical University; 2018. [Google Scholar]
- 16.Liu J. Clinic Research on Hepatic Carcinoma Pain Relived by Needling with Eight Methods of Intelligent Turtle and Western Medicine. Guangzhou, China: Guangzhou University of Chinese Medicine; 2011. [Google Scholar]
- 17.Fu Y., Hu M. Y., Wang X. Y., et al. Clinical observation on wrist-ankle acupuncture combined with morphine in the treatment of 16 cases of refractory cancer pain. Journal of Traditional Chinese Medicine. 2019;60(9):768–772. [Google Scholar]
- 18.Wu Q. L., Cao W., Wang W., et al. Wrist-ankle needle combined with opioid drugs on refractory cancer pain: a randomized controlled trial. Chinese Acupuncture & Moxibustion. 2019;39(10):1051–1054. doi: 10.13703/j.0255-2930.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Dong S. M., Yang Y., Jia Y. Y., et al. The role of wrist ankle acupuncture in the treatment of cancer pain in community cancer patients. Journal of Clinic Nursing’s Practicality. 2018;3(11):99–100. [Google Scholar]
- 20.Sun R. R. The Clinical Research on Acupuncture Combined with Opioids in the Treatment of Cancer Pain. Hefei, China: Anhui University of Chinese Medicine; 2016. [Google Scholar]
- 21.Zhang J. W. Acupuncture Combined with Level Three Ladder Analgesic Clinical Study in the Treatment of Severe Cancer Pain. Nanjing, China: Nanjing University of Chinese Medicine; 2014. [Google Scholar]
- 22.Hui J. R., Zhang N., Li M., et al. Clinical observation on acupuncture combined with three-step analgesic therapy in the treatment of 40 cases of cancer pain. Journal of Traditional Chinese Medicine. 2019;60(2):146–149. [Google Scholar]
- 23.Tan G. S., Lin Z. T., Wang Q., et al. Clinical observation on analgesia effect in cancer pain treated with acu-puncture and western medicine. World Journal of Integrated Traditional and Western Medicine. 2012;7(2):147–149. [Google Scholar]
- 24.Fan L. Y., Gao S. L., Wang Y. Q., et al. Clinical observation of acupuncture combined with western medicine in treatment of advanced lung cancer pain. Medical Journal of Chinese People’s Health. 2017;29(11):36–38. [Google Scholar]
- 25.Jiang B., Chen F., Deng S., et al. 25 cases of cancer pain treated by acupuncture at Taichong Hegu. Zhejiang Journal of Traditional Chinese Medicine. 2016;51(4):p. 270. [Google Scholar]
- 26.Li D. H., Sun C. X., Fan H. F., et al. Clinical study on acupuncture at Zusanli, Taichong and Hegu points combined with three-step analgesic ladder for treatment of gastric cancer pain. Journal of Guangzhou University of Traditional Chinese Medicine. 2017;34(3):344–347. [Google Scholar]
- 27.Huang Y. Observation on the curative effect of acupuncture combined with three steps medicine in the treatment of moderate and severe cancer pain. Inner Mongolia Journal of Traditional Chinese Medicine. 2018;37(5):58–59. [Google Scholar]
- 28.Peng J., Wang W. H., Zhou R. Y., et al. Clinical study on integrated acupuncture and medication in treating moderate and severe cancer pain. Shanghai Journal of Acupuncture and Moxibustion. 2012;31(4):236–238. [Google Scholar]
- 29.Feng R. M., Zong Y. N., Cao S. M., Xu R. H. Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics? Cancer Communications. 2019;39(1):p. 22. doi: 10.1186/s40880-019-0368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Middletion D. R. S., McCormack V. A., Watts M. J., et al. Environmental geochemistry and cancer: a pertinent global health problem requiring interdisciplinary collaboration. Environmental Geochemistry and Health. 2020;42(4):1047–1056. doi: 10.1007/s10653-019-00303-9. [DOI] [PubMed] [Google Scholar]
- 31.Brigitte G., Christian M., Gilles A., et al. Opioids in cancer-related pain: current situation and outlook. Official Journal of the Multinational Association of Supportive Care in Cancer. 2019;27(8):3105–3188. doi: 10.1007/s00520-019-04828-8. [DOI] [PubMed] [Google Scholar]
- 32.He Y. H., May B. H., Zhang A. L., et al. Acupuncture for cancer pain: protocol for a pilot pragmatic randomised controlled trial. BMJ Open. 2019;9(7):p. e025564. doi: 10.1136/bmjopen-2018-025564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang L. M., Du Y. J. Re-realization of adverse reactions to acupuncture and moxibustion. Shanghai Journal of Acupuncture and Moxibustion. 2013;32(11):964–967. [Google Scholar]
- 34.Hou X. R., Cai X. H., Wu S. B., Zhang R. J., Zhang L. D., Song X. G. Mechanism of acupuncture on anti-neuronal apoptosis and the regulation of PI3K/AKT signaling pathway in heroin relapse rats. World Journal of Acupuncture-Moxibustion. 2019;29(4):285–289. doi: 10.1016/j.wjam.2019.12.005. [DOI] [Google Scholar]
- 35.Usman A., Evhy A., Zaeem A. M., et al. Acupuncture/electroacupuncture as an alternative in current opioid crisis. Chinese Journal of Integrative Medicine. 2020;26(9):643–647. doi: 10.1007/s11655-019-3175-7. [DOI] [PubMed] [Google Scholar]
- 36.Zivaljevic A., Shi B., Tam E. M. S., et al. Treatment of visceral pain associated with irritable bowel syndrome using acupuncture: mechanism of action. World Journal of Traditional Chinese Medicine. 2019;5(4):181–186. [Google Scholar]
- 37.Paiey C. A., Johnson M. I. Acupuncture for the relief of chronic pain: a synthesis of systematic reviews. Medicina (Kaunas, Lithuania) 2019;56(1):p. 6. doi: 10.3390/medicina56010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data can be obtained from the author upon reasonable request.


