Generating neurons from human induced pluripotent stem cells (hiPSCs) overcomes the limited access to human brain tissues and greatly facilitates the research in neuroscience (Karagiannis et al., 2019). However, it is still a big challenge to obtain a particular neuronal subtype with high purity and yield to conduct certain studies, such as determining the pathogenesis of diseased neurons using biochemical approaches. Motor neurons (MNs) are a specialized neuronal subtype responsible for innervating musculature in the periphery and governing both autonomic and volitional movements. Dysfunctions in MNs are implicated in a variety of movement diseases, such as amyotrophic lateral sclerosis (ALS), progressive muscular atrophy, and dystonia (Sances et al., 2016; Ding et al., 2020b). ALS belongs to MN diseases, which are caused by gradual degeneration and death of MNs in the brain (upper MNs) and/or in the spinal cord (lower MNs). Several pathogenic mechanisms are involved in ALS, including glutamate excitotoxicity, dysregulated interactions between neurons and glial cells, intracytoplasmic and intranuclear aggregation of certain proteins and RNAs, impaired nucleocytoplasmic transport, and changes in the axon terminals and neuromuscular junctions (NMJs) (Sances et al., 2016). So far, there are no specific treatments available to cure these diseases due to unclear pathophysiological mechanisms. Generation of patient-specific MNs will provide valuable in vitro model systems in deciphering the pathogenesis of these diseases. Recently, we have developed an approach by which functional MNs could be generated from hiPSCs via lentiviral delivery of three transcription factors (Figure 1). These MNs robustly expressed generic neuronal markers, MN-specific markers, and showed electrical maturation and firing of action potentials within 3 weeks (Sepehrimanesh and Ding, 2020). Compared to previous methods (Tang et al., 2017), this approach significantly improved the neuronal survival, purity, and yield, making it feasible to obtain abundant patient-specific MNs for biochemical studies in modeling movement diseases.
Figure 1.
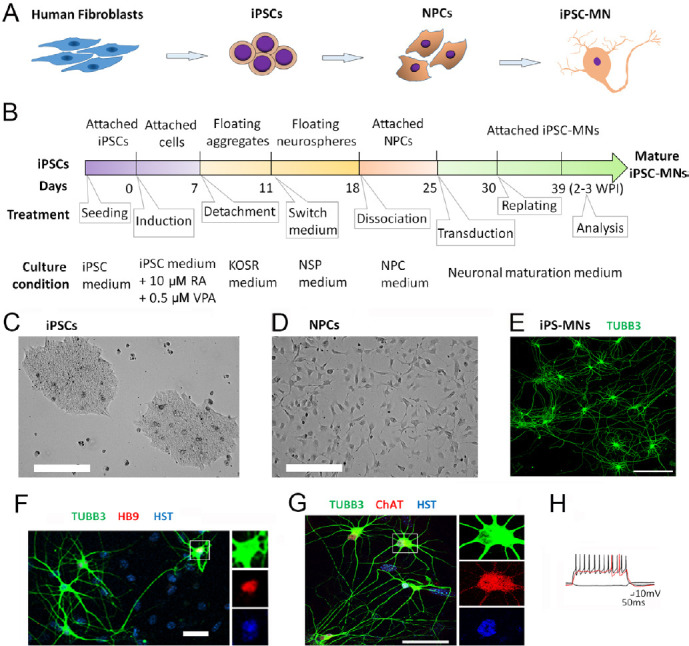
Generation of motor neurons (MNs) from human induced pluripotent stem cells (hiPSCs).
(A) A schematic shows the process of the generation of human MNs from iPSCs. (B) The detailed process of generating iPSC-MNs. The starting induction time was set as day 0. The age of iPSC-MNs was counted from lentiviral transduction. (C) A representative phase contrast micrograph of human iPSCs. Scale bar: 200 µm. (D) A representative phase contrast micrograph of NPCs at lentiviral transduction. Scale bar: 200 µm. (E) A representative fluorescence micrograph of iPSC-MNs induced by three transcription factors (NEUROG2, ISL1 and LHX3) at 3 WPI with immunostaining of TUBB3. Scale bar: 100 μm. (F) A confocal micrograph of iPSC-MNs at 1.5 WPI. Neuronal marker TUBB3 shows the soma and neuron processes, Hoechst 33342 (HST) stained nuclei, and nuclear HB9 was used as the early MN marker. The rectangle highlighted MN was also shown at a large magnification with separated channels. Scale bar: 50 μm. (G) A confocal micrograph of MNs at 2 WPI. Choline acetyltransferase (ChAT) was used as a mature MN marker. The rectangle highlighted MN was also shown at a large magnification with separated channels. Scale bar: 50 μm. (H) Repetitive action potential (AP) waveforms recorded under current-clamp mode of iPSC-MNs at 3 WPI. HB9: MNX1 for motor neuron and pancreas homeobox 1; iPSC-MN: iPSC-derived MN; KOSR: knockout serum replacement; NPCs: neuronal progenitor cells; NSP: neurosphere; RA: retinoic acid; TUBB3: tubulin beta 3 class III; VPA: valproic acid; WPI: weeks post-viral infection. Adapted from Sepehrimanesh and Ding (2020).
Patient-derived MNs could be generated by two kinds of approaches. One is the direct conversion from adult fibroblasts (Ding et al., 2020a). The other approach is hiPSC-based induction and differentiation. However, the relatively low purity and poor yield of directly converted MNs severely limit the studies that require highly pure and large amount of cells, such as gene expression analysis by next-generation sequencing, and protein co-immunoprecipitation and mass spectrometry analysis. An iPSC-based approach will overcome these limitations. iPSCs could be prepared from a variety of readily available tissues such as skin fibroblasts with Yamanaka factors (Takahashi and Yamanaka, 2006) or obtained from international stem cell banks (Kim et al., 2017). These induced neurons retain the specific mutations that are derived from patient donors or engineered by CRISPR makes it possible to directly evaluate the impact of disease-relevant mutations. Most importantly, iPSCs possess almost unlimited expansion capability and are suitable for preparing large amount of materials. These unique features make iPSC-based method a very powerful tool in neuroscience research. iPSC-derived human neurons have been extensively used in understanding of regulatory mechanisms in neuronal development, determining the pathogenesis of neurological diseases, identifying molecular targets for therapeutic interventions, and screening drugs in a more human neuron-specific manner (Karagiannis et al., 2019).
In order to acquire more reproducible and disease-relevant findings in modeling diseases, at least the following four criteria should be considered in evaluation of the cellular system (Sepehrimanesh and Ding, 2020). First, generation of specific neuronal subtype that is particularly affected in the disease. For example, patient-derived MNs are the best neuronal subtype in modeling neurological diseases that target MNs, such as ALS. Second, neurons are able to achieve functional maturation. Some disease-related phenotypes may not be noticed until the diseased neurons reach the late mature stages, especially for modeling aging-dependent neurodegenerative diseases. Examinations of synaptic proteins, neurotransmitter-related enzymes, neurotransmitter release, and electrophysiological activities are good measures to evaluate the maturation and functions. Third, the purity and the yield should be good enough for performing the analysis. Generally, immunostaining of specific markers could be able to distinguish the target neurons from other types of co-cultured cells. However, to biochemically identify dysregulated factors in diseased neurons, large amounts of specific neurons with high purity and yield are required. Lastly, we need to culture the neurons more physiologically and maximize the relevance to in vivo conditions. Using extracellular matrix proteins coated culture vessels, supplemented with neurotrophic factors in culture medium, and co-culture with glia cells could be necessary to make the culture more physiological and improve the neuronal survival. Even though these criteria will be strictly followed, researchers still need to be cautious to interpret the significance of the results in understanding the pathogenesis of diseases.
Currently, several approaches are being used to generate MNs from hiPSCs. Small molecules such as growth factors and chemicals together with transcription factors are widely used for neuronal induction. These factors either directly regulate genes or target signaling pathways that play critical roles in neurogenesis and differentiation. For example, GSK3β inhibitors (such as CHIR99021) combined with the dual Sma and Mad proteins inhibitors (such as SB 431542, and LDN) induce iPSCs into neural progenitor cells (NPCs) (Fujimori et al., 2018). Additionally, other small molecules such as bone morphogenetic protein inhibitors, γ-secretase inhibitors, all-trans-retinoic acid (RA), antioxidants and insulin-like growth factor 1 or insulin have important effects on NPC proliferation and changing into choline acetyltransferase-positive MNs. The presence of brain-derived neurotrophic factor (BDNF), glial cell-derived neurotrophic factor (GDNF), ciliary neurotrophic factor, or neurotrophin-3 (NT-3) in the culture medium is necessary to maintain the neuronal survival and promote neuronal maturation (Ding et al., 2018; Karagiannis et al., 2019). Regardless of the extensive use of these small molecules, these methods have poor efficiency, and produce clear heterogeneity in neuronal subtypes. Therefore, new methods of creating iPSC-MNs are being developed.
In our protocol (Sepehrimanesh and Ding, 2020), hiMNs were first induced into NPCs by addition of RA and valproic acid in mTeSR1 culture medium (Figure 1A–D). Large amount of NPCs could be prepared and frozen for a long-term storage. To efficiently induce NPCs into MNs, transduction of proper amount of lentivirus expressing transcription factors is critical. Because non-infected NPCs could spontaneously differentiate into non-MNs in neuronal maturation medium, generation of higher purity of MNs requires higher transduction efficiency (Sepehrimanesh and Ding, 2020). This could be achieved by preparation of high quality lentivirus. On the other hand, a higher dosage of lentivirus would cause more cell death and lead to low yield. In our practice, we routinely test the titer of active virus in each preparation and use a proper virus dosage to infect NPCs (Ding and Kilpatrick, 2013). Thereby the transduction efficiency and neuronal survival could be balanced well based on titers of active virus. Compare to the previous approach in which NPCs were infected by two lentiviruses expressing four transcription factors, neurogenin-2 (NEUROG2), Insulin gene enhancer 1 (ISL1), LIM/homeobox 3 (LHX3), and SRY-Box Transcription Factor 11 (Sox11; Tang et al., 2017), and the optimized protocol used a single virus co-expressing three essential and sufficient factors (NEUROG2, ISL1 and LHX3). This improvement further maximizes the transduction efficiency and simultaneously minimizes the virus dosage at transduction, resulting in less cell death and a higher yield. These iPSC-MNs robustly expressed generic neuronal markers such as microtubule-associated protein 2 and tubulin beta 3 class III, and early MN marker of nuclear HB9 (also known as MNX1 for motor neuron and pancreas homeobox 1) and the late marker of choline acetyltransferase (Figure 1E–G). Within 3 weeks post-viral infection, action potentials could be detected by whole-cell patch-clamp recordings (Figure 1H), suggesting that these iPSC-MNs achieved electrical maturation and functions (Sepehrimanesh and Ding, 2020).
Besides the purity and yield of iPSC-derived neurons, another big challenge in modeling neurological diseases is how to culture neurons more physiologically, especially for long-term cultures. Chemical or physical modifications of the cell culture plates, such as coating with extracellular matrix proteins, have demonstrated to be an efficient method to better mimic in vivo cell behavior. Neuroglia co-culture is required for modeling certain diseases, exploring neuroglia interactions, and for a long-term survival (Nadadhur et al., 2019). In our studies, we cultured iPSCs, NPCs, and MNs on Matrigel-coated plates. For long-term cultures (more than 2 weeks), iPSC-MNs were seeded onto culture plates coated with a monolayer of astrocytes. Meanwhile, neurotrophic factors (BDNF, GDNF and NT-3) were routinely added in neuronal maturation medium. These measures make the culture more physiological, promote neuronal maturation and survival, and maximize the relevance to in vivo conditions.
Compare to other chemical-based approaches, iPSC-MNs induced by lentiviral delivery of transcription factors possess unique features, such as high purity (> 90%) and fully functional maturity (Ding et al., 2020b; Sepehrimanesh and Ding, 2020). These unique features make iPSC-derived MNs become excellent research materials in determining the pathogenesis of MN-related diseases. However, lentiviral vectors are derived from the human immunodeficiency virus. They have the potential risks for generation of replication-component lentivirus and could randomly integrate virial DNA into host genome. Thus, the lentiviral vector-based gene delivery limits the clinical applications for intervention therapy. Because of the superior biosafety and the mild immune response in humans, Adeno-associated virus (AAV) is widely used as a vector for human gene therapy. Therefore, another research emphasis in neural regeneration field would be generating highly pure MNs for clinical applications using recombinant AAV-based approaches. The major drawback of AAV vector is its limited cloning capacity. In the future, using CRISPR engineering to generate paired patient-specific iPSC lines and isogenic controls, or tagged with fluorescent or reporters will enable researchers to examine the specific subcellular compartments and the activation of specific genes or pathways under physiological and pathological conditions. The growing of “mini brains” (organoids) from hiPSCs will provide a novel research system to model neurological diseases and test therapies.
This work was supported by the National Institute of Neurological Diseases and Stroke, No. NINDS R21NS112910 (to BD) and Department of Defense (DoD) Peer Reviewed Medical Research Program (PRMRP), No. W81XWH2010186 (to BD).
Footnotes
Copyright license agreement: The Copyright License Agreement has been signed by the author before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
C-Editors: Zhao M, Wang L; T-Editor: Jia Y
References
- 1.Ding B, Akter M, Zhang CL. Differential influence of sample sex and neuronal maturation on mRNA and protein transport in induced human neurons. Front Mol Neurosci. 2020a;13:46. doi: 10.3389/fnmol.2020.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ding B, Dobner PR, Mullikin-Kilpatrick D, Wang W, Zhu H, Chow CW, Cave JW, Gronostajski RM, Kilpatrick DL. BDNF activates an NFI-dependent neurodevelopmental timing program by sequestering NFATc4. Mol Biol Cell. 2018;29:975–987. doi: 10.1091/mbc.E16-08-0595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ding B, Kilpatrick DL. Lentiviral vector production, titration, and transduction of primary neurons. Methods Mol Biol. 2013;1018:119–131. doi: 10.1007/978-1-62703-444-9_12. [DOI] [PubMed] [Google Scholar]
- 4.Ding B, Tang Y, Ma S, Akter M, Liu ML, Zang T, Zhang CL. Disease modeling with human neurons reveals LMNB1 dysregulation underlying DYT1 dystonia. bioRxiv. 2020b doi: 10.1523/JNEUROSCI.2507-20.2020. 20200811246371. doi: https://doiorg/101101/20200811246371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujimori K, Ishikawa M, Otomo A, Atsuta N, Nakamura R, Akiyama T, Hadano S, Aoki M, Saya H, Sobue G, Okano H. Modeling sporadic ALS in iPSC-derived motor neurons identifies a potential therapeutic agent. Nat Med. 2018;24:1579–1589. doi: 10.1038/s41591-018-0140-5. [DOI] [PubMed] [Google Scholar]
- 6.Karagiannis P, Takahashi K, Saito M, Yoshida Y, Okita K, Watanabe A, Inoue H, Yamashita JK, Todani M, Nakagawa M, Osawa M, Yashiro Y, Yamanaka S, Osafune K. Induced Pluripotent stem cells and their use in human models of disease and development. Physiol Rev. 2019;99:79–114. doi: 10.1152/physrev.00039.2017. [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, Kurtz A, Yuan BZ, Zeng F, Lomax G, Loring JF, Crook J, Ju JH, Clarke L, Inamdar MS, Pera M, Firpo MT, Sheldon M, Rahman N, O’Shea O, Pranke P, Zhou Q, Isasi R, Rungsiwiwut R, Kawamata S, et al. Report of the international stem cell banking initiative workshop activity: current hurdles and progress in seed-stock banking of human pluripotent stem cells. Stem Cells Transl Med. 2017;6:1956–1962. doi: 10.1002/sctm.17-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nadadhur AG, Alsaqati M, Gasparotto L, Cornelissen-Steijger P, van Hugte E, Dooves S, Harwood AJ, Heine VM. Neuron-glia interactions increase neuronal phenotypes in tuberous sclerosis complex patient iPSC-derived models. Stem Cell Reports. 2019;12:42–56. doi: 10.1016/j.stemcr.2018.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sances S, Bruijn LI, Chandran S, Eggan K, Ho R, Klim JR, Livesey MR, Lowry E, Macklis JD, Rushton D, Sadegh C, Sareen D, Wichterle H, Zhang SC, Svendsen CN. Modeling ALS with motor neurons derived from human induced pluripotent stem cells. Nat Neurosci. 2016;19:542–553. doi: 10.1038/nn.4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sepehrimanesh M, Ding B. Generation and optimization of highly pure motor neurons from human induced pluripotent stem cells via lentiviral delivery of transcription factors. Am J Physiol Cell Physiol. 2020;319:C771–780. doi: 10.1152/ajpcell.00279.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 12.Tang Y, Liu ML, Zang T, Zhang CL. Direct reprogramming rather than iPSC-Based reprogramming maintains aging hallmarks in human motor neurons. Front Mol Neurosci. 2017;10:359. doi: 10.3389/fnmol.2017.00359. [DOI] [PMC free article] [PubMed] [Google Scholar]


