Abstract
The COVID-19 pandemic represents a collective trauma that may have enduring stress effects during sensitive periods, such as pregnancy. Prenatal stress may result in epigenetic signatures of stress-related genes (e.g., the serotonin transporter gene, SLC6A4) that may in turn influence infants’ behavioral development. In April 2020, we launched a longitudinal cohort study to assess the behavioral and epigenetic vestiges of COVID-19-related prenatal stress exposure in mothers and infants. COVID-19-related prenatal stress was retrospectively assessed at birth. SLC6A4 methylation was assessed in thirteen CpG sites in mothers and infants’ buccal cells. Infants’ temperament was assessed at 3-month-age. Complete data were available from 108 mother-infant dyads. Greater COVID-19-related prenatal stress was significantly associated with higher infants’ SLC6A4 methylation in seven CpG sites. SLC6A4 methylation at these sites predicted infants’ temperament at 3 months.
Subject terms: DNA methylation, Human behaviour, Paediatrics
Introduction
Northern Italy was hit dramatically by the first COVID-19 wave during the first months of 20201. With the exponential increase in the number of patients requiring intensive care and the mortality rate associated with this clinical condition, the COVID-19 pandemic is an unprecedented healthcare emergency that also emerges as a potential collective trauma2,3. The detrimental effects of COVID-19-related stress have been highlighted for healthcare professionals at the forefront of the emergency4 as well as for the general population5. Fragile individuals and those who are exposed to the pandemic during a period of heightened neuroplasticity may be especially at risk for the consequences of COVID-19-related stress6–8. Pregnancy is such a sensitive period for the embedding of environmental exposures—for bad and for good—in the developmental phenotype of infants9. Previous research suggested that the prenatal exposure to maternal stress may impact different domains of infant behavioral, affective, and socio-cognitive development10–12. Maternal stress during pregnancy may be specifically linked with alterations of the temperamental profile of the infant13–15. Previous studies reported that higher levels of prenatal stress were significantly associated with infants’ higher negative affectivity, lower expression of intense pleasure and difficulties in the regulatory functioning during the first months of life15,16. As temperament is involved in setting thresholds of reactivity to environmental stimuli17, understanding how adverse prenatal conditions may affect temperamental traits is crucial.
The influence of prenatal stress on later infants’ developmental outcomes may be at least partially mediated by epigenetic mechanisms18. DNA methylation is by far the most studied mechanism at the interface between environmental exposures and phenotype in human infants. This epigenetic mechanism mainly occurs among DNA sites rich in cytosine and guanine (i.e., CpG sites), it is involved in the regulation of genes’ expression and may contribute to gene silencing in a way that is highly susceptible to environmental stimuli19,20. DNA methylation is of specific concern when it occurs at the level of stress-related genomic portions, such as the serotonin transporter gene (SLC6A4)21. Previous research reported heightened CpG-specific SLC6A4 methylation in infants exposed to prenatal maternal depression22 and stress as well as to postnatal adverse exposurs23. A recent systematic review reported that heightened SLC6A4 methylation may be considered as a potential biomarker of early adverse experiences21. The study of the epigenetic vestiges of collective trauma has been useful to elucidate biomarkers of stress in previous large-scale events such as the Canadian Ice Storm in 199924 or the World Trade Center terroristic attack in 200125. Nonetheless, we do not know how a global pandemic may be harmful during pregnancy by increasing the exposure to stress and producing indirect behavioral effects on infants’ temperament. As such, in April 2020 we launched the Measuring the Outcomes of Maternal COVID-19-related Prenatal Exposure—i.e., MOM-COPE26—research project to assess the epigenetic and behavioral consequences of COVID-19-related prenatal stress on maternal well-being and infants’ development from birth to 12 months. In the present paper, we report on (1) the effects of COVID-19-related prenatal stress on maternal and infants’ SLC6A4 methylation and (2) the association between infants’ SLC6A4 methylation and temperament assessed at 3 months of age.
Methods
Participants and procedures
The MOM-COPE is a longitudinal and multi-centric cohort study that involves ten neonatal units in Northern Italy. The fully detailed description of this project is reported elsewhere26. Here we report on a sample of 108 (62%) mother-infant dyads who provided complete data for prenatal (T0), neonatal (T1) and 3-month (T2) assessments by February 2021 (Fig. 1). Mothers were included if at least 18-year-old, in the absence of prenatal and perinatal diseases or injuries, if they delivered at term (i.e., from 37 + 0 to 41 + 6 weeks of gestation), and if they were negative for COVID-19 at delivery. Mothers were first contacted at antepartum classes or immediately following the postpartum period. Socio-demographic and neonatal data were obtained from medical records. Within 48 h from delivery, the mothers filled in a first set of questionnaires to provide retrospective quantitative measures of prenatal COVID-19-related stress. Between 6 and 24 h, buccal cells were obtained from mothers and infants using DNA Genotek Oragene OC-175, according to manufacturer guidelines. When infants were approaching 3-month-age, mothers filled-in a questionnaire on infants’ temperament. The study was approved by the Ethics Committees of the project lead institution (IRCCS Mondino Foundation, Pavia, Italy) and the participating hospitals. All the procedures were performed in accordance with the 2018 Declaration of Helsinki for studies conducted with human participants. All mothers provided informed consent to participate to the study.
Figure 1.
Overview of the study.
Measures
Mothers self-reported on socio-demographic (i.e., age, educational level, occupational status). At delivery mothers retrospectively reported on their prenatal COVID-19-related stress during the last trimester of pregnancy through an ad-hoc questionnaire (Supplementary File S1). A mean COVID-19-related prenatal stress score was obtained, ranging from 1 (low) to 5 (high). Neonatal characteristics (i.e., gestational age, birth weight, head circumference, neonatal length, Apgar at minute 1, breastfeeding at birth, and mode of delivery) were collected from medical records. The saliva was collected from both mothers and infants using the OraCollect for Pediatrics kit OC-175 (DNA Genotek, Ottawa, Canada) between 6 and 24 h from delivery. Methylation assessment was conducted according to previous validated procedures from this lab27,28. The genomic DNA was extracted following manufacturer’s protocols and its quality was assessed using a Qubit fluorometer Invitrogen, Thermo Fisher Scientific, Waltham, Massachusetts, USA). The methylation status of the SLC6A4 gene’s region (chr17:28562750–28562958, 13 CpGs) was assessed by PCR amplification of bisulfite-treated DNA followed by Next Generation Sequencing (NGS) on a NEXTSeq-500 (Illumina, San Diego, California, USA). At infants’ 3-month-age, infants’ temperament was assessed with the short form version of the Infant Behaviour Questionnaire-Revised, IBQ-R29. The IBQ-R includes 91 items that are rated on a 7-point and summarized into 14 scales and 3 main factors: surgency (i.e., activity level and expression of pleasure), negative affectivity (i.e., distress, sadness and fear) and regulatory capacity (i.e., cuddliness, soothability and orienting).
Plan of analysis
Descriptive statistics were computed for socio-demographic characteristics and for all the variables reported in the “Measures” section. Parametric indexes (i.e., mean, standard deviation, and range) were obtained for continuous variables, whereas frequencies and percentages were obtained for categorical variables. Normal distribution was checked for all variables of interest and normalization occurred by means of natural log (ln) adjustment. Bivariate Pearson’s correlation coefficients were computed to assess the association among COVID-19-related prenatal stress and both infants and mothers’ methylation status of SLC6A4 CpG sites. Multiple-comparison bias was checked using the Benjamini–Hochberg procedure, q < 0.10. A principal component analysis (PCA) was used to reduce the number of methylation items; a single principal component (PC1) accounted for 35% of the total variance in SLC6A4 methylation and it was used in further analyses. Bivariate correlations were carried to test for the potential association of neonatal and socio-demographic variables with both SLC6A4 PC1 methylation and infants’ surgency at 3 months. A linear general model was used to estimate the association between COVID-19-related prenatal stress and infants SLC6A4 PC1 methylation (ln). A linear general model was used to estimate the association between infants SLC6A4 PC1 methylation and 3-month surgency score. Analyses were carried using R and IBM SPSS 26 for Windows, with p < 0.05.
Results
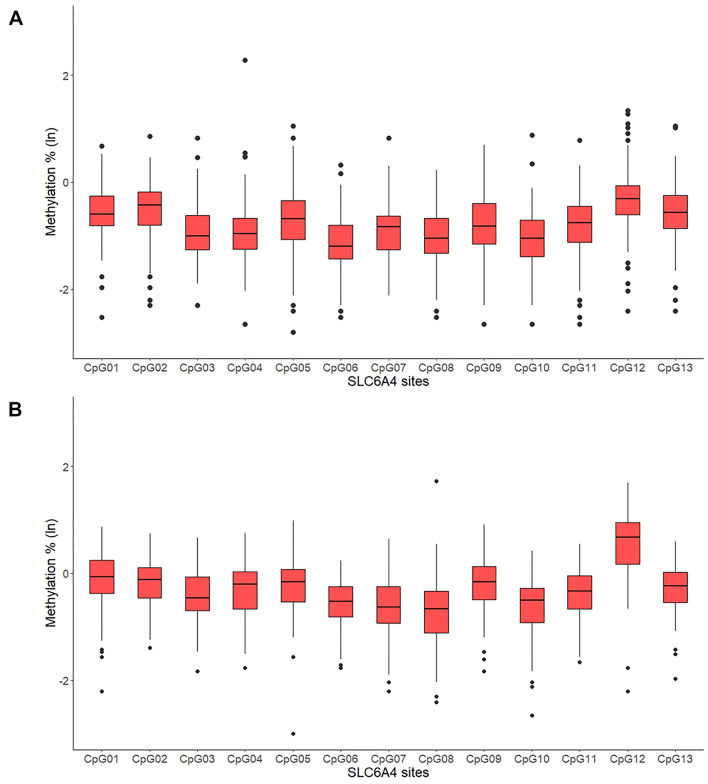
Descriptive statistics are reported in Table 1. Figure 2 reports infants and mothers’ CpG-specific SLC6A4 methylation estimates.
Table 1.
Descriptive statistics.
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| Gestational age (weeks) | 37.00 | 42.00 | 39.71 | 1.05 |
| Birth weight (g) | 2430.00 | 4345.00 | 3342.88 | 413.82 |
| Head circumference (cm) | 30.00 | 39.00 | 34.33 | 1.27 |
| Neonatal length (cm) | 46.00 | 56.00 | 50.64 | 1.95 |
| Apgar at minute 1 | 6.00 | 10.00 | 9.18 | 0.69 |
| Maternal educational level (years of study) | 5.00 | 23.00 | 14.44 | 3.57 |
| Infants’ surgency | 2.37 | 6.31 | 4.07 | 0.89 |
| Infants’ negative affectivity | 1.30 | 5.65 | 3.10 | 0.81 |
| Infants’ regulatory capacity | 3.52 | 6.81 | 5.15 | 0.76 |
| N | % | |||
|---|---|---|---|---|
| Maternal occupational status (employed) | 95 | 88.0 | ||
| Delivery (eutocic) | 69 | 63.9 | ||
| Infant's sex (females) | 55 | 50.9 | ||
| Breastfeeding at birth (maternal milk) | 71 | 65.7 | ||
Figure 2.
SLC6A4 methylation in infants (A) and mothers (B). Note. Bars represent standard errors.
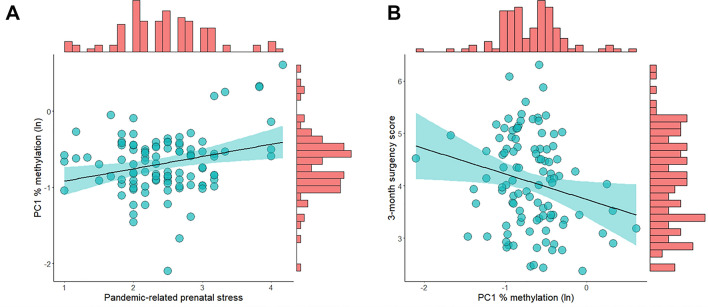
Bivariate correlations between COVID-19-related prenatal stress and both infants and mothers’ CpG-specific SLC6A4 methylation are reported in Fig. 3. For infants, SLC6A4 methylation was positively and significantly associated with COVID-19-related prenatal stress at seven CpG sites (i.e., 1, 2, 6, 8, 9, 10, and 12). All significant correlations survived to Benjamini–Hochberg test. No significant correlations emerged for mothers’ SLC6A4 methylation.
Figure 3.
Heat map of the bivariate correlations between COVID-19-related prenatal stress and both infants and mothers’ SLC6A4 methylation.
The PCA results are reported in Table 2. The infants’ CpG sites whose methylation levels were significantly correlated with prenatal stress loaded on PC1, accounting for 35% of total variance in infants’ SLC6A4 methylation.
Table 2.
Principal component analysis (PCA) on infants’ SLC6A4 methylation conducted among the 13 CpG sites.
| SLC6A4 site | Principal components | ||
|---|---|---|---|
| PC1 | PC2 | PC3 | |
| CpG 1 | 0.704 | ||
| CpG 2 | 0.735 | ||
| CpG 3 | 0.512 | 0.653 | |
| CpG 4 | |||
| CpG 5 | 0.614 | ||
| CpG 6 | 0.691 | ||
| CpG 7 | 0.577 | ||
| CpG 8 | 0.635 | ||
| CpG 9 | 0.776 | ||
| CpG 10 | 0.618 | ||
| CpG 11 | 0.502 | ||
| CpG 12 | 0.849 | ||
| CpG 13 | 0.793 | ||
Loadings on the respective principal components (PC) are reported in bold. Loadings < 0.500 are not reported.
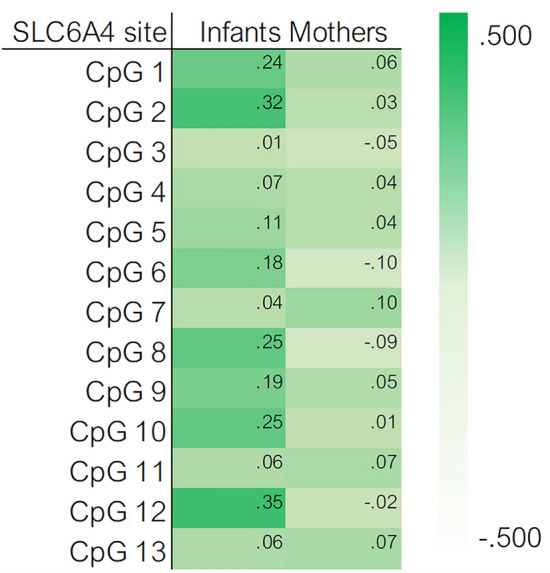
PC1 showed non-Gaussian distribution and it was normalized by means of ln transformation. No significant correlations emerged for neonatal and socio-demographic variables with heightened PC1% methylation (ln) and infants’ 3-month temperament. COVID-19-related prenatal stress was significantly and positively associated with infants’ PC1% methylation (ln), R2 = 0.07, F = 7.71, p = 0.007, B = 0.16 [95% CI 0.05:0.29] (Fig. 4A). Infants’ PC1% methylation (ln) was significantly and associated with 3-month surgency score, R2 = 0.05, F = 5.05, p = 0.027, B = − 0.45 [95% CI − 0.92:− 0.06] (Fig. 4B): infants who showed higher levels of SLC6A4 gene methylation in the selected region were rated by their parents as exhibiting greater surgency. No significant associations emerged for infants’ negative affectivity and regulatory capacity.
Figure 4.
Association between (A) COVID-19-related prenatal stress and infants’ SLC6A4 PC1 methylation; (B) infants’ SLC6A4 PC1 methylation and 3-month surgency score.
Discussion
Pregnant women experiencing prenatal stress during the COVID-19 pandemic may give birth to infants who present heightened SLC6A4 methylation levels and early dysregulations in the temperament profile at 3 months. These findings are consistent with previous literature that highlighted how precocious stress-related epigenetic signatures may represent a biomarker of early adversity exposures21.
Notably, in the present study, a significant effect of COVID-19-related prenatal stress emerged for infants’ SLC6A4 methylation, but not for mothers. This result may be interpreted in the light of the conflict perspective in fetal programming by maternal stress30. Literature about maternal prenatal stress showed that it may act not only as a risk factor on fetal development31, but it may also lead to a fetus adaptive response, increasing his organism’s defensive processes32. Additionally, prenatal stress may represent a scenario of mother-fetus conflictual exchanges. Genetic interests of parents and offspring are only partially overlapping and—during critical conditions—the maternal biology may manipulate the fetal environment in order to promote its own biological interest30. From this perspective, it should be highlighted that maternal prenatal stress has been found to increase the risk of inflammations which, in turn, may further exposure the fetal compartment to stress hormones. One can speculate that, during the COVID-19 pandemic, the maternal biological functioning may have opted for the activation of protective mechanisms—such as cortisol production to reduce stress-induced inflammatory processes—that may have resulted in a heightened exposure of the fetus to stress hormones33. Unfortunately, in the present cohort study we did not collect placental tissues and the assessment of biomarkers of stress-related inflammations are not available.
In our sample, the SLC6A4 methylation was significantly and negatively associated with infants’ temperament, in particular with the infants’ positive affect at 3 months. In a recent study, Gartstein and colleagues34 showed that the SLC6A4 methylation was associated with soothability at 3 months in infants prenatally exposed to antidepressant medication, while Montirosso and colleagues35 found a significant impact on preterm infants’ duration of orienting and approach to novelty. However, these two studies did not document similar effects for control groups of healthy age-matched counterparts. In the present study, we enrolled only healthy full-term infants and mothers with no documented psychiatric conditions. As such, it can be hypothesized that the epigenetic effect observed at the level of the SLC6A4 gene may be ascribed to the prenatal exposure to pandemic-related stress. In other words, although the present study lacks a control group of non-exposed age-matched mother-infant dyads, there is indirect support that the stress due to being exposed to a global healthcare emergency during pregnancy may contribute to the epigenetic regulation of the serotonin transporter gene in young infants.
Limitations
First, we originally planned to have a control group enrolment between April and December 2021; nonetheless, due to the ongoing nature of the COVID-19 emergency in Italy, it was not possible to enroll non-exposed age-matched controls and this research project qualifies as a longitudinal cohort study. Second, the unprecedented nature of this healthcare emergency required to develop ad-hoc instruments to detect pandemic-related prenatal stress. Consistently, in our study, the prenatal stress was retrospectively assessed using an ad-hoc self-report measure. Although this measure was developed according to previous literature26, it provides an estimate of maternal stress during pregnancy that can be only partially compared to previous studies that included standardized measures. Third, SLC6A4 methylation was peripherally assessed in buccal cells. The association between peripheral SLC6A4 methylation and actual serotonin transporter expression has received partial confirmation in animal model research and cross-tissue concordance remains an open question20. Recently, Booij and colleagues reported on a significant association between SLC6A4 methylation in buccal tissue and brain response to negative emotionality stimuli36, suggesting that peripheral markers of serotonin epigenetic regulation should be considered the closest reliable source of functionally relevant DNA methylation in human subjects. Finally, a single-gene approach to the study of the epigenetic correlates of early stress exposure in infants was made possible here by the availability of a well-documented rationale for the SLC6A4 gene20. Nonetheless, it should be highlighted that multiple loci in different genomic regions may be potential targets of environmentally driven epigenetic regulation and other genes—e.g., NR3C137, BDNF38—should be also involved.
Conclusion
In a general population of healthy mother-infant dyads, pandemic-related prenatal stress emerged as a risk factor for infants’ development. In more specific terms, pregnant women experiencing greater COVID-19-related prenatal stress may give birth to infants who present higher levels of SLC6A4 methylation and temperament dysregulation at 3 months. In this scenario, the consequences of COVID-19-related stress experienced during pregnancy risk to result in a “hidden pandemic” that may affect the early developmental trajectories of infants, even in absence of severe medical risk conditions. Appropriate actions are needed from clinicians and policymakers to timely provide families with appropriate and efficient preventive strategies during and after the healthcare emergency.
Supplementary Information
Acknowledgements
The authors are thankful to the following colleagues of the MOM-COPE study: Lilia Altieri, Giulia Bensi, Elisa Bettiga, Renza Bonini, Anna Cavallini, Giovanna Centinaio, Elisa Fazzi, Anna Freddi, Roberta Giacchero, Andrea Gritti, Paola Guerini, Gaia Kullmann, Maria Luisa Magnani, Laura Malerba, Mario Motta, Dario Pantaleo, Benedetta C. Pietra, Laura Riva, Maria Valentina Spartà, Arsenio Spinillo, Pierangelo Veggiotti, Patrizia Vergani, Marzo Zecca. Beril Calgan, Eleonora Fullone, Vanessa Manfredini, Francesca Masoni, Giada Pettenati, Elisa Rinaldi, and Luisa Vercellino were trainees in psychology in the Child Neurology and Psychiatry Unit of the IRCCS Mondino Foundation (Pavia, Italy) at the time of study and they provided critical help with data collection. Cinzia Fattore provided key support with administrative issues and IRB procedures during the delicate time of the COVID-19 outbreak in Italy. The authors are thankful to all the families who participated in this study.
Author contributions
L.P. conceptualized and designed the study, coordinated the research actions, contributed to statistical data analyses, and drafted the initial manuscript. F.M., M.V., A.C., R.G. were responsible for epigenetic data analysis and they critically reviewed the manuscript. E.B., G.B., L.D., R.F., B.G., M.R.L., R.N., C.P., F.P., and B.S. coordinated/performed participants’ enrollment and data collection in the neonatal units involved in the project, they reviewed the manuscript. S.G. contributed to the study conceptualization, to the statistical data analyses. S.O. and R.B. critically reviewed the manuscript for intellectual content and supervised the study procedures. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This study is supported by funds from the Italian Ministry of Health (Cinque per Mille 2017) and from Roche Italia to author LP.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-95053-z.
References
- 1.Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R. The response of Milan's Emergency Medical System to the COVID-19 outbreak in Italy. Lancet. 2020;395(10227):e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D'Agostino A, Demartini B, Cavallotti S, Gambini O. Mental health services in Italy during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(5):385–387. doi: 10.1016/S2215-0366(20)30133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masiero M, Mazzocco K, Harnois C, Cropley M, Pravettoni G. From individual to social trauma: Sources of everyday trauma in Italy, the US and UK during the COVID-19 pandemic. J. Trauma Dissoc. 2020;21:1–7. doi: 10.1080/15299732.2020.1787296. [DOI] [PubMed] [Google Scholar]
- 4.Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Provenzi L, Grumi S, Borgatti R. Alone with the kids: Tele-medicine for children with special healthcare needs during COVID-19 emergency. Front. Psychol. 2020;11:2193. doi: 10.3389/fpsyg.2020.02193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis EP, Narayan AJ. Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Dev. Psychopathol. 2020;32(5):1625–1639. doi: 10.1017/S0954579420001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buitelaar JK, Huizink AC, Mulder EJ, de Medina PGR, Visser GH. Prenatal stress and cognitive development and temperament in infants. Neurobiol. Aging. 2003;24:S53–S60. doi: 10.1016/S0197-4580(03)00050-2. [DOI] [PubMed] [Google Scholar]
- 11.Hartman S, Freeman SM, Bales KL, Belsky J. Prenatal stress as a risk—and an opportunity—factor. Psychol. Sci. 2018;29(4):572–580. doi: 10.1177/0956797617739983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graignic-Philippe R, Dayan J, Chokron S, Jacquet AY, Tordjman S. Effects of prenatal stress on fetal and child development: A critical literature review. Neurosci. Biobehav. Rev. 2014;43:137–162. doi: 10.1016/j.neubiorev.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Huizink AC, De Medina PGR, Mulder EJ, Visser GH, Buitelaar JK. Psychological measures of prenatal stress as predictors of infant temperament. J. Am. Acad. Child Adolesc. Psychiatry. 2002;41(9):1078–1085. doi: 10.1097/00004583-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Gutteling BM, de Weerth C, Willemsen-Swinkels SH, Huizink AC, Mulder EJ, Visser GH, Buitelaar JK. The effects of prenatal stress on temperament and problem behavior of 27-month-old toddlers. Eur. Child Adolesc. Psychiatry. 2005;14(1):41–51. doi: 10.1007/s00787-005-0435-1. [DOI] [PubMed] [Google Scholar]
- 15.Nolvi S, Karlsson L, Bridgett DJ, Korja R, Huizink AC, Kataja EL, Karlsson H. Maternal prenatal stress and infant emotional reactivity six months postpartum. J. Affect. Disord. 2016;199:163–170. doi: 10.1016/j.jad.2016.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Howland MA, Sandman CA, Davis EP, Glynn LM. Prenatal maternal psychological distress and fetal developmental trajectories: Associations with infant temperament. Dev. Psychopathol. 2020;32(5):1685–1695. doi: 10.1017/S095457942000142X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ellis BJ, Boyce WT, Belsky J, Bakermans-Kranenburg MJ, Van IJzendoorn MH. Differential susceptibility to the environment: An evolutionary–neurodevelopmental theory. Dev. Psychopathol. 2011;23(1):7–28. doi: 10.1017/S0954579410000611. [DOI] [PubMed] [Google Scholar]
- 18.Cao-Lei L, Laplante DP, King S. Prenatal maternal stress and epigenetics: Review of the human research. Curr. Mol. Biol. Rep. 2016;2(1):16–25. doi: 10.1007/s40610-016-0030-x. [DOI] [Google Scholar]
- 19.Weaver IC, Cervoni N, Champagne FA, D'Alessio AC, Sharma S, Seckl JR, Dymov S, Szyf M, Meaney MJ. Epigenetic programming by maternal behavior. Nat. Neurosci. 2004;7(8):847–854. doi: 10.1038/nn1276. [DOI] [PubMed] [Google Scholar]
- 20.Provenzi L, Brambilla M, Scotto di Minico G, Montirosso R, Borgatti R. Maternal caregiving and DNA methylation in human infants and children: Systematic review. Genes Brain Behav. 2020;19(3):e12616. doi: 10.1111/gbb.12616. [DOI] [PubMed] [Google Scholar]
- 21.Provenzi L, Giorda R, Beri S, Montirosso R. SLC6A4 methylation as an epigenetic marker of life adversity exposures in humans: A systematic review of literature. Neurosci. Biobehav. Rev. 2016;71:7–20. doi: 10.1016/j.neubiorev.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 22.Devlin AM, Brain U, Austin J, Oberlander TF. Prenatal exposure to maternal depressed mood and the MTHFR C677T variant affect SLC6A4 methylation in infants at birth. PLoS One. 2010;5(8):e12201. doi: 10.1371/journal.pone.0012201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fumagalli M, Provenzi L, De Carli P, Dessimone F, Sirgiovanni I, Giorda R, Cinnante C, Squarcina L, Medea E, Pozzoli U, Medea E, Triulzi F, Brambilla P, Borgatti R, Mosca F, Montirosso R. From early stress to 12-month development in very preterm infants: Preliminary findings on epigenetic mechanisms and brain growth. PLoS One. 2018;13(1):e0190602. doi: 10.1371/journal.pone.0190602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cao-Lei L, Massart R, Suderman MJ, Machnes Z, Elgbeili G, Laplante DP, Szyf M, King S. DNA methylation signatures triggered by prenatal maternal stress exposure to a natural disaster: Project Ice Storm. PLoS One. 2014;9(9):e107653. doi: 10.1371/journal.pone.0107653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuan PF, Waszczuk MA, Kotov R, Marsit CJ, Guffanti G, Gonzalez A, Yang X, Koenen K, Bromet E, Luft BJ. An epigenome-wide DNA methylation study of PTSD and depression in World Trade Center responders. Transl. Psychiatry. 2017;7(6):e1158. doi: 10.1038/tp.2017.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Provenzi L, Grumi S, Giorda R, Biasucci G, Bonini R, Cavallini A, Decembrino L, Drera B, Falcone R, Fazzi E, Gardella B, Giacchero R, Nacinovich R, Pisoni C, Prefumo F, Scelsa B, Spartà MV, Veggiotti P, Orcesi S, Borgatti R. Measuring the Outcomes of Maternal COVID-19-related Prenatal Exposure (MOM-COPE): Study protocol for a multicentric longitudinal project. BMJ Open. 2020;10(12):e044585. doi: 10.1136/bmjopen-2020-044585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Provenzi L, Fumagalli M, Scotto di Minico G, Giorda R, Morandi F, Sirgiovanni I, Schiavolin P, Mosca F, Borgatti R, Montirosso R. Pain-related increase in serotonin transporter gene methylation associates with emotional regulation in 4.5-year-old preterm-born children. Acta Paediatr. 2020;109(6):1166–1174. doi: 10.1111/apa.15077. [DOI] [PubMed] [Google Scholar]
- 28.Provenzi L, Fumagalli M, Sirgiovanni I, et al. Pain-related stress during the Neonatal Intensive Care Unit stay and SLC6A4 methylation in very preterm infants. Front. Behav. Neurosci. 2015;9:99. doi: 10.3389/fnbeh.2015.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gartstein MA, Rothbart MK. Studying infant temperament via the revised infant behavior questionnaire. Infant Behav. Dev. 2003;26(1):64–86. doi: 10.1016/S0163-6383(02)00169-8. [DOI] [Google Scholar]
- 30.Del Giudice M. Fetal programming by maternal stress: Insights from a conflict perspective. Psychoneuroendocrinology. 2012;37(10):1614–1629. doi: 10.1016/j.psyneuen.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 31.Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav. Rev. 2005;29(2):237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 32.Kaiser S, Norbert S. Effects of prenatal social stress on offspring development: Pathology or adaptation? Curr. Dir. Psychol. Sci. 2009;18(2):118–121. doi: 10.1111/j.1467-8721.2009.01620.x. [DOI] [Google Scholar]
- 33.Osborne S, Biaggi A, Chua TE, et al. Antenatal depression programs cortisol stress reactivity in offspring through increased maternal inflammation and cortisol in pregnancy: The Psychiatry Research and Motherhood - Depression (PRAM-D) Study [published correction appears in Psychoneuroendocrinology. 2020 Sep; 119:104795] Psychoneuroendocrinology. 2018;98:211–221. doi: 10.1016/j.psyneuen.2018.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gartstein MA, Hookenson KV, Brain U, Devlin AM, Grunau RE, Oberlander TF. Sculpting infant soothability: The role of prenatal SSRI antidepressant exposure and neonatal SLC6A4 methylation status. Dev. Psychobiol. 2016;58(6):745–758. doi: 10.1002/dev.21414. [DOI] [PubMed] [Google Scholar]
- 35.Montirosso R, Provenzi L, Fumagalli M, et al. Serotonin transporter gene (SLC6A4) methylation associates with neonatal intensive care unit stay and 3-month-old temperament in preterm infants. Child Dev. 2016;87(1):38–48. doi: 10.1111/cdev.12492. [DOI] [PubMed] [Google Scholar]
- 36.Ismaylova E, Lévesque ML, Pomares FB, et al. Serotonin transporter promoter methylation in peripheral cells and neural responses to negative stimuli: A study of adolescent monozygotic twins. Transl. Psychiatry. 2018;8(1):147. doi: 10.1038/s41398-018-0195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berretta E, Guida E, Forni D, Provenzi L. Glucocorticoid receptor gene (NR3C1) methylation during the first thousand days: Environmental exposures and developmental outcomes. Neurosci. Biobehav. Rev. 2021;125:493–502. doi: 10.1016/j.neubiorev.2021.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Fumagalli M, Provenzi L, De Carli P, et al. From early stress to 12-month development in very preterm infants: Preliminary findings on epigenetic mechanisms and brain growth. PLoS One. 2018;13(1):e0190602. doi: 10.1371/journal.pone.0190602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Provenzi L, et al. Prenatal maternal stress during the COVID-19 pandemic and infant regulatory capacity at 3 months: A longitudinal study. Dev. Psychopathol. 2021 doi: 10.1017/S0954579421000766. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.