Abstract
The members of the Tumor Necrosis Factor (TNF) superfamily, the ligand lymphotoxin α1β2 (LTα1β2) and its unique receptor lymphotoxin β receptor (LTβR), play a pivotal role in the establishment and regulation of the immune system by allowing a tight communication between lymphocytes and stromal cells. Recent advances using transgenic mice harboring a specific deletion of the Ltbr gene in distinct stromal cells have revealed important roles for LTβR signaling in the thymic function that ensures the generation of a diverse and self-tolerant T-cell repertoire. In this review, we summarize our current knowledge on this signaling axis in the thymic homing of lymphoid progenitors and peripheral antigen-presenting cells, the trafficking and egress of thymocytes, the differentiation of medullary thymic epithelial cells, and the establishment of central tolerance. We also highlight the importance of LTα1β2/LTβR axis in controlling the recovery of the thymic function after myeloablative conditioning regimen, opening novel perspectives in regenerative medicine.
Subject terms: Immune cell death, T cells
Facts
Immunological tolerance is established in the thymus through the elimination of autoreactive T cells and the selection of Foxp3+ regulatory T cells.
LTα1β2/LTβR interactions act as a communication signal between developing lymphocytes and thymic stromal cells.
The lymphotoxin axis controls the cell trafficking, the differentiation of stromal cells and the death of autoreactive T cells.
LTα1β2/LTβR axis controls the regeneration of thymus by boosting the recovery of stromal niches and the homing of T-cell progenitors.
Open Questions
Given the recent identification of TEC heterogeneity, what is the implication of the LTα1β2/LTβR axis in the development of each TEC subset?
What are the target genes of LTβR signaling in each thymic stromal cell subset?
What is the impact of the LTα1β2/LTβR axis on T-cell selection and prevention of autoimmunity?
To what extent does the LTα1β2/LTβR axis regulate chemokines in the thymic stroma?
What is the impact of the LTα1β2/LTβR axis in the thymic regeneration in humans?
Introduction
Lymphotoxin α (LTα), also known as TNFβ, has been originally described in the 1960s as a cytotoxic factor produced by activated lymphocytes that could kill transformed cell lines [1, 2]. LTα forms a soluble homotrimer (LTα3), which binds to Tumor Necrosis Factor Receptor 1 (TNFR1), TNFR2 and to the herpes virus entry mediator (HVEM) [3, 4]. When co-expressed with lymphotoxin β (LTβ) that possesses a transmembrane domain, LTα forms a cell surface-bound heterotrimer (LTα1β2) that exclusively binds to the LTβ receptor (LTβR) [5–7]. LTβR has a second ligand, LIGHT that also binds to HVEM. LTα1β2 is expressed by lymphoid cells such as activated T lymphocytes, B cells, natural killer cells (NK), and type 3 innate lymphoid cells (ILC3). LTβR is expressed mainly by stromal cells including endothelial, mesenchymal, and epithelial cells and by myeloid cells such as dendritic cells (DC) and macrophages [8–10]. This specific expression pattern implies that LTα1β2/LTβR interactions act as a communication signal between lymphocytes and stromal cells. A seminal study based on the generation of Lta-deficient mice has revealed the critical role of LTα in the development of lymph nodes (LN) and Peyer’s patches [11]. These mice also show abnormal splenic architecture with defective segregation of B and T cells. Mice harboring a point mutation induced by N-ethyl-N-nitrosourea (ENU) in the Lta gene also lack LN and Peyer’s patches and display disorganized splenic architecture [12]. Similarly Ltb- and Ltbr-deficient mice lack LN and Peyer’s patches and have disrupted splenic organization [13, 14]. Nevertheless, unlike Lta-deficient mice, Ltb-deficient mice have cervical and mesenteric LN, indicating that LTα3 is implicated in the development of these secondary lymphoid structures. Accordingly, the inhibition of LTβR signaling in pregnant mice at 9 days of gestation with the LTβR-Ig fusion protein blocks the development of all lymph nodes, except cervical and mesenteric LN, and disrupts splenic architecture [15, 16]. These observations further highlight a dominant role of LTα1β2 in lymphoid organ development with the potential for LTα3 in promoting cervical and mesenteric LN [17].
Beyond lymphoid organogenesis, subsequent studies have revealed that lymphotoxin members control the development and/or homeostasis of distinct immune cells as well as numerous aspects of the immune response (reviewed in [10, 18, 19]. For example, LTβR promotes NK and NKT cell development [20] and the homeostasis of CD8α- DC in lymphoid tissues [9, 21]. LTα1β2/LTβR interactions between helper CD4+ T cells and DC are necessary for CD8+ T-cell expansion [22]. LTα1β2/LTβR interactions between B cells and follicular DC allow the recruitment of DC and CD4+ T cells that promotes helper T-cell responses [23]. LT members are critical for the formation of germinal centers and humoral immunity [24, 25]. LTβR signaling also controls the production of type I interferons in stromal cells and macrophages of lymphoid organs upon virus infections [18]. LTα1β2 expressed by ILC3 drives IL-22 production required for mucosal pathogen clearance [26, 27]. Furthermore, LTα3 secreted by ILC controls T-cell homing in the gut and thus T-cell-dependent IgA induction, whereas LTα1β2 expressed by ILC controls T-cell-independent IgA induction [28].
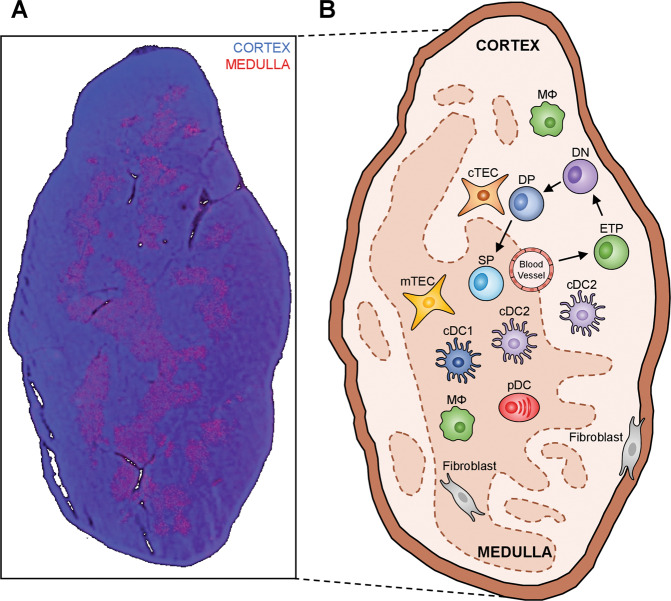
In contrast to the complete absence of LN and Peyer’s patches, the thymus develops in Lta-, Ltb-, and Ltbr-deficient mice [11, 13, 14]. This primary lymphoid organ, organized into an outer cortical region and an inner medullary region, ensures the production of self-tolerant naïve T cells (Fig. 1A). The cortex supports early stages of T-cell development such as the proliferation and survival of T-cell progenitors, the development of double positive (DP) thymocytes into CD4+ and CD8+ single positive (SP) thymocytes and the deletion of DP thymocytes bearing T-cell receptors (TCR) specific for ubiquitous self-antigens. In contrast, the medulla sustains the induction of central tolerance, characterized mainly by the clonal deletion of autoreactive SP thymocytes and the production of Foxp3+ regulatory T cells (Treg). The cortex and the medulla contain a large variety of stromal cells including cortical and medullary thymic epithelial cells (cTEC and mTEC, respectively), DC, macrophages and fibroblasts that participate in T-cell development and selection (Fig. 1B). LTα1β2 expression is mainly restricted to SP thymocytes and a subset of ILC3 while LTβR is expressed by TEC, DC, endothelial cells and fibroblasts [29–33]. This large expression pattern of LTβR explains why LTβR signaling has a pleiotropic role in the thymic activity. In this review, we discuss recent advances that have unraveled novel roles of the LTα1β2/LTβR axis in distinct aspects of the thymic function.
Fig. 1. Cortico-medullary organization and cellular composition of the thymus.
A Representative image of a wild-type thymic section stained with the mTEC-specific marker keratin-14 (red) and counterstained with DAPI (blue). B Major thymocyte and APC subsets of the cortex and medulla are depicted. cDC conventional dendritic cells, cTEC cortical thymic epithelial cells, DN double negative thymocytes, DP double positive thymocytes, ETP early thymic progenitors, mTEC medullary thymic epithelial cells, MФ macrophages, pDC plasmacytoid dendritic cells, SP single positive thymocytes.
LTβR controls the thymic homing of lymphoid progenitors and thymocyte egress
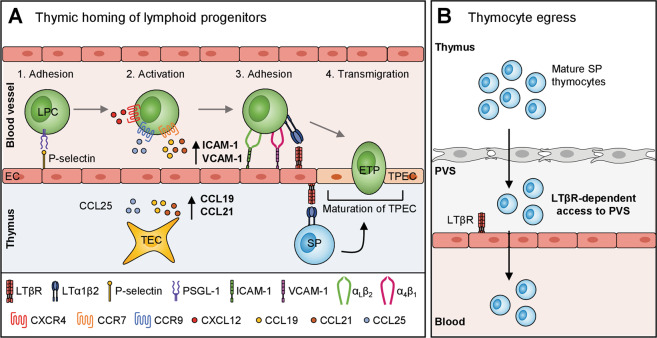
Normal T-cell development requires a continuous homing of lymphoid progenitor cells (LPC) derived from the bone marrow (BM) into the thymus via blood vessels localized at the cortico-medullary junction [34]. This colonization relies on a multi-step process involving P-selectin, ICAM-1, and VCAM-1 adhesion molecules, expressed by endothelial cells, and CCL19, CCL21, CCL25, and CXCL12 chemokines expressed by both endothelial cells and TEC (Fig. 2A). These adhesion molecules allow the attachment of LPC to the endothelium whereas the chemokines direct their migration into the thymus via CCR7, CCR9, and CXCR4 chemokine receptors [35–39]. Disruption of these molecules alone or in combination leads to altered thymus homing.
Fig. 2. LTβR signaling controls the homing of LPC and the egress of mature thymocytes.
A LTβR expression in endothelial cells is required for the homing of lymphoid progenitor cells (LPC) into the thymus by regulating Ccl19, Ccl21, Icam1, and Vcam1 expression. LTα1β2-delivered by SP thymocytes also controls the development and homeostasis of thymic portal endothelial cells (TPEC). B LTβR expression in endothelial cells is required for the thymic egress of mature SP thymocytes by driving their entry into the perivascular space (PVS).
Recent studies have demonstrated the involvement of LTβR signaling in the homing of LPC into the thymus (Table 1). Lin−CD4−CD8−CD44+CD25−c-Kit+ cells, which represent the early thymic progenitors (ETP), are drastically reduced in Ltbr−/− mice [40, 41]. LTβR expression in endothelial cells controls the numbers of ETP as shown by reciprocal BM chimeras and Ltbr deletion specifically in endothelial cells with the endothelial-specific receptor tyrosine kinase (Tek) promoter [40]. Short-term homing assays using BM transfer in Ltbr−/− and Ltbrfl/fl × TekCre recipients have demonstrated that LTβR is required for the homing of LPC. Given that LTβR signaling can be triggered by either LTα1β2 or LIGHT, the implication of both ligands has been studied. ETP are normal in Light−/− mice and slightly altered in Lta−/− mice. Interestingly, they are substantially reduced in Lta−/− × Light−/− double-deficient mice, to a similar degree to Ltbr−/− mice, indicating that LTα1β2 and LIGHT act in cooperation for ETP colonization [40].
Table 1.
Thymic phenotypes of mice deficient for the lymphotoxin signaling.
| Biological processes | Mouse models | Phenotype | References |
|---|---|---|---|
|
Lymphoid progenitor homing |
Ltbr−/− mice |
Reduced Vcam1 and Icam1 in endothelial cells Drastic reduction of ETP |
[40, 41] |
| Lta−/− mice | Reduction of ETP | [40] | |
| Lta−/− × Light−/− mice | Drastic reduction of ETP | [40] | |
| TekCre × Ltbrfl/fl | Drastic reduction of ETP | [40] | |
| Migration of SP thymocytes into the medulla | Ltbr−/− mice | Reduced Ccl19 and Ccl21 in mTEC | [44] |
| Lta−/− mice | Reduced Ccl19 in mTEC | [32] | |
| Ltb−/− mice | Reduced Ccl19 in mTEC | [32] | |
| Egress of mature T cells | Ltbr−/− mice | Augmentation of RTE | [29] |
| Ltbr−/− × Rag2GFP mice | Defective emigration of mature SP thymocytes | [51] | |
| Recruitment of peripheral APC | Foxn1Cre × Ltbrfl/fl mice | Increased thymic cDC2 | [69] |
| Lta−/− mice |
Enhanced recruitment of peripheral cDC2, pDC and MΦ |
[67] | |
| Medullary architecture | Ltbr−/− mice |
Smaller medullary islets Loss of UEA-1+ mTEC homogeneous distribution Reduced ICAM-1hiVCAM-1+ mesenchymal cells |
[29, 82, 83, 94] |
| Lta−/− mice |
Smaller medullary islets Disrupted 3D medulla organization |
[76, 82, 83] | |
| Ltb−/− mice |
Loss of UEA-1+ mTEC homogeneous distribution |
[29] | |
| Light−/− mice | No major alteration | [82] | |
| Lta−/− × Light−/− mice | Smaller medullary islets | [82] | |
| Ltb−/− × Light−/− mice |
Loss of UEA-1+ mTEC homogeneous distribution |
[29] | |
| Foxn1Cre × Ltbrfl/fl mice | Smaller medullary islets | [69] | |
| K14Cre × Ltbrfl/fl mice | Smaller medullary islets | [86] | |
| mTEC composition | Ltbr−/− mice |
Reduced UEA-1+, Aire+, CCL21+ and post-Aire mTEC |
[29, 44, 46], [83, 84] |
| Foxn1Cre × Ltbrfl/fl mice |
Reduced mTEClo, mTEChi, Aire+ and CCL21+ mTEC Loss of thymic tuft cells |
[69, 85] | |
| Lta−/− mice | Not affected | [31, 83, 88] | |
| K14Cre × Ltbrfl/fl mice | Reduced mTEC progenitors | [86] | |
| Aire-independent TRA expression | Ltbr−/− mice | Reduced TRA expression | [32, 92, 93] |
| Twist2Cre × Ltbrfl/fl mice | Reduced self-antigens expression | [33] | |
| Clonal deletion | Lta−/− mice | Enhanced | [67] |
| OTII-Rag2−/− × Lta−/− mice | Enhanced | [67] | |
| OT-I/Rip-mOVA × Ltbr−/− mice | Reduced | [44] | |
| OT-II/Rip-mOVA × Ltbr−/− mice | Not affected | [83] | |
| TAG-I/TRAMP × Lta−/− mice | Reduced | [91] | |
|
LTβR-Ig blockade in TGB/TRAMP mice |
Reduced | [91] |
APC antigen-presenting cell, cDC2 type 2 conventional dendritic cell, ETP early thymic progenitor, mTEC medullary thymic epithelial cell, MФ macrophage, pDC plasmacytoid dendritic cell, RTE recent thymic emigrant, SP single positive thymocytes, TRA tissue restricted self-antigen.
Mechanistically, during the development of LN, LTβR signaling induces the expression of Vcam-1, Ccl19 and Ccl21, which are also implicated in the thymic homing of LPC [42, 43]. It has been reported that the expression of Vcam-1 and Icam-1 is likely reduced in thymic endothelial and mesenchymal cells of Ltbr−/− mice whereas Selp expression is normal [41]. However, another study found normal levels of Icam-1, Vcam-1 and Selp in endothelial cells from Ltbr−/− mice [40]. Thus, the implication of LTβR in the regulation of adhesion molecules in the thymus remains unclear. Moreover, reduced expression of Ccl19 and Ccl21 has been reported in mTEC of Ltbr−/− mice, whereas only Ccl19 was reduced in mTEC of Lta−/− and Ltb−/− mice [32, 44]. Accordingly, the stimulation of fetal thymic stroma with anti-LTβR agonist antibody upregulates Ccl19 [45]. Furthermore, LTβR was shown to regulate the development of CCL21+ mTEC [46]. Thus, it seems that LTβR controls LPC homing by regulating the expression of adhesion molecules and chemokines implicated in this process (Fig. 2A).
Recently, another interesting hypothesis emerged indicating that LTβR promotes the homing of LPC by inducing the differentiation of functional endothelial cells [40]. Several studies have shown that LTβR signaling in endothelial cells, stimulated by LTα1β2-expressing DC, promotes the development and maintenance of high endothelial venules that are responsible for T-cell entry into LN [47]. The direct role of LTβR signaling in the development of functional high endothelial venules was demonstrated by the selective deletion of Ltbr gene in endothelial cells [48]. In the thymus, CD31+Ly6C-Selp+ endothelial cells, termed thymic portal endothelial cells (TPEC), have been proposed to correspond to a specialized population implicated in LPC homing. Interestingly, Ltbr−/− mice have reduced frequency of TPEC. Moreover, in vivo treatment with agonistic LTβR antibody increases TPEC, whereas LTβR-Ig blockade decreases TPEC. These observations indicate that LTβR signaling controls the development of TPEC. Furthermore, Tcra−/− and Zap70−/− mice, which both lack SP thymocytes due to an arrest at the DP stage, have reduced ETP [40, 49]. Accordingly, Tcra−/− mice exhibit diminished numbers of TPEC, suggesting that SP thymocytes regulate their development. This is consistent with the fact that the LTβR ligand, LTα1β2, is mainly provided by SP thymocytes [29, 50]. Thus, a model emerged in which SP thymocytes, through the LTα1β2/LTβR axis, induce the development of TPEC, responsible for LPC homing. Taken together, these studies have revealed that LTβR signaling controls the homing of LPC into the thymus via the regulation of chemokines and adhesion molecules as well as the development of functional TPEC (Fig. 2A).
The LTα1β2/LTβR axis is also implicated in the egress of mature SP thymocytes. Ltbr−/− mice show increased mature SP thymocytes with a phenotype of recent thymic emigrants [29]. The normal proliferation of these over-represented cells in Ltbr−/− mice suggested that LTβR might control their egress. Given that mature SP thymocytes egress involves their migration across the endothelial barrier that expresses LTβR, unsurprisingly LTβR on endothelial cells regulates this process [51, 52] (Table 1). LTβR controls the access of the most mature SP thymocytes to the perivascular space, where they induce the development of TPEC (Fig. 2B). During their egress, mature SP thymocytes seem to regulate the homing of LPC by providing instructive signals to endothelial cells via LTα1β2/LTβR interactions. Thus, this feedback loop could allow the thymus to tightly control T-cell production. While further investigations are required, TPEC likely act as gatekeepers of thymus entry and exit.
LTα1β2/LTβR axis regulates the trafficking of thymocytes and peripheral antigen-presenting cells
The migration of SP thymocytes from the cortex into the medulla is essential for the negative selection of autoreactive T cells and the generation of Foxp3+ Treg. This migration mediated by the chemokine receptor CCR7, expressed by positively-selected SP thymocytes, allows them to be exposed to tissue restricted self-antigens (TRA) in the medulla. In mice deficient for Ccr7 or its two ligands Ccl19 and Ccl21, predominantly expressed by mTEC, SP thymocytes are arrested in the cortex and fail to accumulate in the medulla [53]. This impaired migration in Ccr7- or Ccr7 ligand-deficient mice causes defective medullary size and tissue-specific autoimmunity due to impaired negative selection [54–56]. Conversely, premature expression of CCR7 leads to abnormal migration of DP thymocytes into the medulla [57]. Ccl21a and Ccl21b/Ccl21c genes encode for CCL21Ser and CCL21Leu proteins, respectively [58]. Interestingly, CCL21Ser plays a non-redundant role in the migration of SP thymocytes into the medulla [56]. Moreover, Ccl19-deficient mice exhibit normal medulla architecture, suggesting that CCL19 alone is dispensable for the medullary migration of SP thymocytes [59]. Similarly, whereas Ccl19−/− × Ccl21−/− mice lack segregation of B- and T-cell areas, Ccl19−/− mice do not show any defect, indicating that CCL21 alone is sufficient for maintaining normal architecture of peripheral lymphoid organs [59].
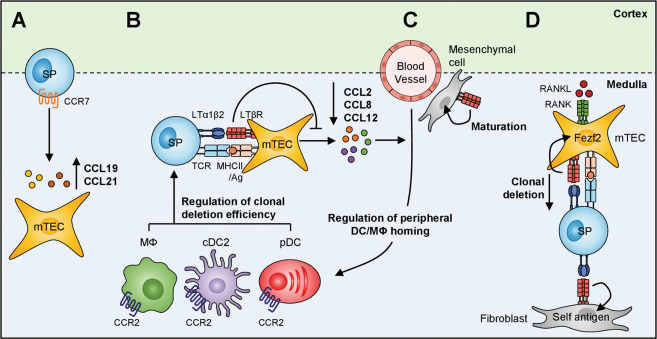
In the thymus, LTβR is required for the migration of SP thymocytes into the medulla. Abnormal migration of SP thymocytes in Ltbr−/− mice was initially attributed to a reduced expression of Ccl19 and Ccl21 in mTEC [44]. Intriguingly, only Ccl19, that is unlikely implicated in this process, was reduced in mTEC of Lta−/− and Ltb−/− mice [32]. The expression of Ccl19 and Ccl21 was also diminished in mice deficient for the Autoimmune regulator (Aire) [60]. Aire+ and CCL21+ mTEC seem to correspond to two distinct populations, although their developmental relationship remains unclear. CCL21+ mTEC development was proposed to be regulated by LTβR and to a lesser extent by Aire, which could explain the reduction of Ccl21 observed in both Ltbr−/− and Aire−/− mice [46]. Therefore, defective migration of SP thymocytes into the medulla of Ltbr−/− mice may be attributed to altered development of CCL21+ mTEC. Nevertheless, since CCL21 protein detection was used to identify CCL21-expressing mTEC, it remains unclear whether LTβR regulates the development of these cells or alternatively controls Ccl21 gene expression. The identification of specific markers of CCL21+ mTEC as well as biochemical approaches aimed at deciphering Ccl21 gene regulation in mTEC are needed to clarify both possibilities. This clarification appears important because Ccl21 expression was reported to be regulated by IKKα and NIK, upstream kinases of the non-canonical NFκB pathway, activated by LTβR stimulation [42, 61]. Regardless the underlying mechanisms, LTβR is implicated in the migration of SP thymocytes into the medulla (Fig. 3A and Table 1).
Fig. 3. The LTα1β2-LTβR axis regulates the cell trafficking into the thymus and clonal deletion.
A The LTα1β2-LTβR axis regulates the migration of SP thymocytes into the medulla by regulating Ccl19 and Ccl21 expression in mTEC. B LTα1β2-delivered signal by SP thymocytes upon antigen (Ag)-specific interactions with mTEC negatively controls the expression of CCR2 ligands, thereby regulating the homing of CCR2-expressing peripheral DC and macrophages (MФ). Thus, the LTα1β2-LTβR axis regulates the efficiency of clonal deletion by controlling the recruitment of peripheral APC into the thymus. C LTβR signaling is also required for the maturation of thymic mesenchymal cells, characterized by the co-expression of ICAM-1 and VCAM-1. D Moreover, the LTβR signaling is implicated in thymocyte selection by regulating Fezf2 expression in mTEC and inducing the expression of self-antigens in medullary fibroblasts.
The induction of central tolerance requires the recruitment of DC that transport and display innocuous self-antigens captured in the periphery [62–65]. Two main DC subsets, type 2 conventional DC (cDC2; CD11chiPDCA-1loCD8αloSirpα+) and plasmacytoid DC (pDC; CD11cint PDCA-1hi) have the ability to home into the thymus [66]. Our group recently identified that LTα1β2/LTβR interactions between CD4+ SP thymocytes and mTEC regulate the recruitment of peripheral DC into the thymus (Fig. 3B and Table 1) [67]. The expression of LTα is induced in CD4+ SP thymocytes upon antigen-specific interactions with mTEC. In contrast to OTII-Rag2−/− mice, LTα expression is upregulated in CD4+ SP thymocytes of OTII-Rag2−/− mice carrying a RIP-mOVA transgene driving the synthesis of membrane-bound OVA in mTEC [68]. This upregulation was also recapitulated in vitro by co-culturing OVA323-339-loaded purified mTEC with OTII CD4+ SP thymocytes [67]. Interestingly, Lta−/− mice contain increased numbers of cDC2 and pDC as well as F4/80+CD11b+ macrophages in their thymus. In line with these observations, a TEC-specific deletion of Ltbr also leads to increased thymic numbers of cDC2 [69] (Table 1). The adoptive transfer of blood-derived donor cells in Lta−/− recipients demonstrated that this phenotype was due to an increased recruitment of these cells, revealing that LTα acts as a repressor of peripheral antigen-presenting cell (APC) entry into the thymus [67]. Mechanistically, LTα1β2/LTβR interactions with CD4+ SP thymocytes negatively regulate in mTEC the production of CCL2, CCL8 and CCL12. mTEC of Lta−/− mice overexpress these chemokines and blocking LTα1β2/LTβR interactions with the LTβR-Fc soluble receptor in an antigen-specific co-culture of mTEC and CD4+ SP thymocytes also results in the upregulation of these chemokines. CCR2 and its ligand, CCL2, were previously reported to control the thymic representation of cDC2 and pDC [64, 70]. The generation of BM chimeras with Ccr2−/− BM-derived cells revealed that CCR2 also controls the numbers of F4/80+CD11b+ macrophages in the thymus [67]. CCL8, a ligand for CCR1 and CCR5, is also overexpressed in mTEC from Lta−/− mice. BM chimeras with Ccr1−/− or Ccr5−/− BM-derived cells showed that these two chemokine receptors participate in the thymic composition of cDC2, pDC and F4/80+CD11b+ macrophages, but to a lesser extent than CCR2. The adoptive transfer of Ccr2−/− blood-derived donor cells in Lta−/− recipients demonstrated that LTα controls APC thymic homing in a CCR2-dependent manner. Given that LTα1β2/LTβR signaling could regulate other chemokines in the thymic stroma [45], future investigations are needed to reveal a broader implication in the intrathymic cell trafficking.
LTα1β2/LTβR axis controls medulla organization and central tolerance induction
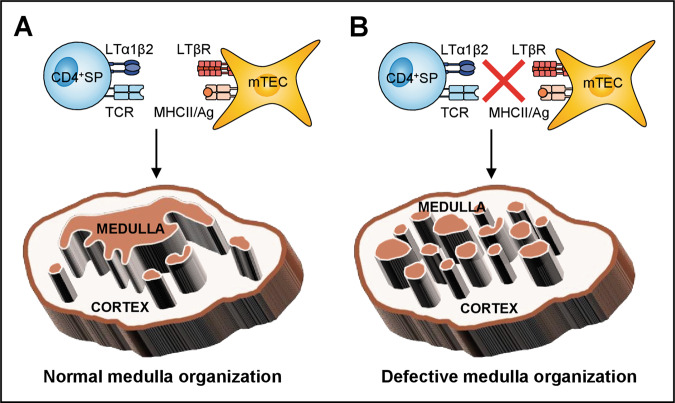
The medulla constitutes a privileged microenvironment for the negative selection that consists in the deletion of SP thymocytes bearing TCR with a high affinity for self-antigen/MHC complexes [71]. This specialized niche is also the main site for the generation of Foxp3+ Treg [72]. mTEC largely contribute in both processes through their unique ability to express thousands of TRA [73]. In turn, mTEC differentiation and organization require signals from developing T cells. This bi-directional relationship is called “thymic crosstalk” [74, 75]. The 3D reconstruction of wild-type mouse thymic lobes unraveled a complex medulla organization with a large central compartment surrounded by ~200 medullary islets (Fig. 4A) [76, 77]. Furthermore, the medulla topology exhibits a highly convoluted shape, controlled by SP thymocytes. Tcra−/− and Zap70−/− mice lacking SP thymocytes have a well-developed cortex but a severely reduced medulla [50, 78–80]. Similarly, Rag2−/− mice showing an early block at the DN3 stage exhibit only ~20 small unconnected medullary islets [76]. This complex organization depends preferentially on CD4+ SP thymocytes. Whereas β2m−/− mice, lacking CD8+ SP thymocytes, have medullary regions closely resembling to those of WT mice, H2-Aa−/− mice show underdeveloped medulla characterized by small individual islets [68]. CD4+ SP thymocytes induce the development of the medulla upon TCR reactivity with TRA expressed by mTEC. Compared to OTII-Rag2−/− mice that do not express the cognate antigen, RIP-mOVA × OTII-Rag2−/− mice, in which antigen-specific interactions can occur, exhibit enlarged medulla. In agreement with TCR reactivity, the CD28-CD80/86 and CD40-CD40L costimulatory axes are also required for normal medulla development [76, 81].
Fig. 4. The LTα1β2-LTβR axis controls the 3D organization of the thymus.
A Upon Ag-specific interactions with mTEC, CD4+ SP thymocytes upregulate the expression of LTα1β2. In turn, the LTα1β2-LTβR axis controls the 3D organization of the medulla, characterized by a central compartment surrounded by small isolated islets. B When the LTα1β2-LTβR axis is defective or when TCR-MHCII interactions are disrupted, the medulla organization is altered, lacking the central compartment and showing only several small isolated islets.
Antigen-specific interactions with mTEC induce in CD4+ SP thymocytes the upregulation of LTα, expressed as a membrane-bound heterotrimer LTα1β2 [29, 68]. The LTα1β2/LTβR signal delivered in the context of these interactions controls medulla organization (Table 1). The 3D reconstruction of thymic lobes of Lta−/− mice showed that the medulla is composed of small islets with no apparent central compartment [76]. Ltb−/− mice also show disrupted medulla organization, whereas no major alterations were observed in Light−/− mice [29, 82]. No additional defects were found between Ltb−/− and Ltb−/− × Light−/− mice [29]. In contrast, double-deficiency for Lta and Light induces a more profound defect in medulla architecture than in single Lta−/− mice, suggesting that LTα and LIGHT cooperatively drive medulla development [82]. Furthermore, the small remaining medullary islets observed in Lta−/− × Light−/− mice are also found in Ltbr−/− mice [29, 82, 83]. Thus, the lymphotoxin axis crucially controls the 3D organization of the thymic medulla (Fig. 4B).
Ltbr−/− mice display abnormal mTEC development characterized by reduced numbers of MHCIIloCD80lo and MHCIIhiCD80hi mTEC, known as mTEClo and mTEChi, respectively. A further characterization of mTEC subsets in these mice showed a reduction in Aire+ mTEChi, CCL21+ mTEClo, DCLK1+ tuft-like and terminally differentiated involucrin+ mTEC [46, 82–85]. In line with these observations, the treatment of fetal thymic lobes with an agonistic anti-LTβR antibody increases mTEC numbers [68]. In contrast, Lta deficiency alone does not affect mTEC development and cellularity but rather their spatial organization [31, 83]. Nevertheless, the composition of mTEC subsets remains to be determined in Lta−/− × Light−/− and Lta−/− × Ltb−/− mice. Interestingly, a TEC-specific deletion of Ltbr using Ltbrfl/fl × Foxn1Cre mice recapitulates the medullary disorganization and altered mTEC composition observed in Ltbr−/− mice, indicating that the LTβR signaling in TEC controls medulla organization and mTEC development [69]. The use of Ltbrfl/fl × K14Cre mice also showed that TEC-intrinsic LTβR controls medulla organization and mTEC from their progenitor stage [86]. Therefore, LTβR signaling in mTEC not only drives the 3D organization of the medulla but also its mTEC composition (Table 1).
Both Ltbr−/− and Lta−/− mice show signs of autoimmunity characterized by inflammatory infiltration of peripheral organs and serum autoantibodies, suggesting that the LTβR signaling is required for the establishment of central tolerance [29, 87, 88]. Although the medulla constitutes a specialized niche for the generation of Foxp3+ Treg, Ltbr−/− mice do not show major defect in Treg development although further investigations are required considering that these cells are heterogeneous in the thymus [44, 87, 89]. To define the role of LTβR in the negative selection, several MHCI-restricted TCR transgenic models have been used such as RIP-mOVA × OTI, TAG-I × TRAMP and TGB × TRAMP mice (Table 1) [90]. In these models, the LTα1β2/LTβR axis seems to be implicated in the negative selection since Ltbr or Lta deficiency prevents clonal deletion of TCR clones [44, 91]. Nevertheless, the degree of the involvement of lymphotoxin varies according to the MHCI-restricted TCR transgenic system used. Furthermore, in the MHCII-restricted TCR transgenic model, Rip-mOVA × OT-II mice, this axis has little influence on clonal deletion [83]. Although further investigations are required, these observations suggest a differential role for the lymphotoxin pathway in CD8 versus CD4 clonal deletion (Table 1). Mechanistically, the involvement of this pathway in clonal deletion could be explained by the fact that it is suspected to be involved in the regulation of Aire-independent TRA [32, 92]. In line with this hypothesis, LTβR was reported to induce the expression of Fezf2 transcription factor, which controls the expression of a set of Aire-independent TRA [93]. Furthermore, the lymphotoxin pathway is involved in the migration of SP thymocytes into the medulla, which could also explain in part its role in clonal deletion. Surprisingly, the specific deletion of LTβR in TEC results in a milder autoimmune phenotype than in Ltbr−/− mice [33, 69].
Interestingly, LTβR signaling is required for the maintenance and maturation of thymic mesenchymal cells, characterized by the co-expression of ICAM-1 and VCAM-1 [94] (Fig. 3C and Table 1). A recent study also indicates that the deletion of LTβR in fibroblasts, using Ltbrfl/fl × Twist2Cre mice, causes a marked autoimmune phenotype characterized by the production of autoantibodies against lung, pancreas, salivary glands and liver accompanied by T-cell infiltrates [33]. LTβR signaling in fibroblasts controls the expression of a unique set of self-antigens that seems to contribute to central tolerance. Nevertheless, Ltbr deficiency in fibroblasts results not only in impaired development and/or maintenance of medullary fibroblasts but also in Aire+ mTEC. Thus, LTβR is likely required for central tolerance through the regulation of fibroblast-specific antigens or indirectly by regulating the overall pool of Aire+ mTEC (Fig. 3D). Our group also recently reported that the thymic entry of peripheral DC and macrophages is regulated by LTα, which substantially impinges clonal deletion [67]. Similarly to Lta−/− mice, OTII-Rag2−/− × Lta−/− mice show an increased expression of CCR2 ligands in mTEC and consequently an enhanced recruitment of cDC2, pDC and macrophages compared to OTII-Rag2−/− mice. Interestingly, OTII-Rag2−/− × Lta−/− recipients adoptively transferred with OVA323-339-loaded DC and macrophage-enriched cells show an augmented deletion of OTII DP and Vα2+Vβ5+CD4+ SP thymocytes, demonstrating that LTα-regulated APC thymic entry controls the clonal deletion of autoreactive thymocytes (Fig. 3B and Table 1).
Besides its role in the selection of conventional αβ T cells, LTβR by controlling the development of mTEClo subsets also regulates the generation of invariant natural killer T (iNKT) cells. Mice with a TEC-specific deletion of Ltbr show a reduction in Tbet+ NKT1, PLZFhi NKT2 and RORγt+ NKT17 differentiated subsets [85]. Nevertheless, since all iNKT subsets are affected, it remains unclear whether TEC expression of LTβR influences the iNKT development from a common progenitor stage.
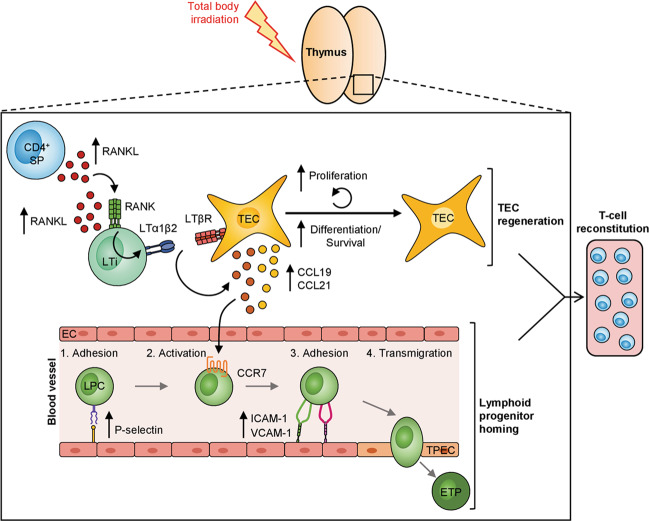
LTα1β2/LTβR axis controls thymic regeneration
The thymus is highly sensitive to cytoablative treatments such as radiation or chemotherapy, used to prepare patients to hematopoietic stem cell or bone marrow transplantation (BMT). Thymic damages engendered by the conditioning regimen result in delayed T‐cell reconstitution that could lead to serious clinical complications such as opportunistic infections, autoimmunity, tumor relapse or secondary malignancies. Interestingly, LTα expression is upregulated in radio-resistant CD4+ SP thymocytes and host-derived lymphoid tissue inducer cells (LTi) during the early phase of thymus recovery after total body irradiation and BMT [31]. LTi cells, which belong to the ILC3 subset, have been identified as important actors of thymic regeneration [95]. LTα upregulation by LTi cells during the early phase of thymus recovery suggests that LTα is implicated in thymic repair. Short-term homing assays in irradiated Lta−/− recipients revealed that LTα controls the homing of LPC into the thymus [31]. Accordingly, LTα controls the expression of Icam-1, Vcam-1, and Selp adhesion molecules in endothelial cells and Ccl19 and Ccl21 chemokines in TEC, all implicated in LPC homing [35, 36, 39]. Similarly to Lta−/− mice, Ltbr−/− recipients show an altered recruitment of LPC after irradiation [40]. Furthermore in vivo treatment with agonistic anti-LTβR antibodies after BMT enhances LPC homing [41].
Mechanistically, LTα upregulation in LTi cells depends on RANK signaling induced by RANK ligand (RANKL) stimulation (Fig. 5). In vivo administration of RANKL recombinant protein after sublethal total body irradiation upregulates LTα selectively in LTi cells, whereas the administration of a neutralizing anti-RANKL antibody prevents this upregulation [31, 96]. LTα protein is expressed as a membrane-bound heterotrimer LTα1β2, which is upregulated in a radiation dose-dependent manner in this cell type. Interestingly, total body irradiation also induces the upregulation of LTβR in both cTEC and mTEC, as well as in a TEC population described to be enriched in thymic epithelial progenitor cells (TEPC), defined as α6-integrinhiSca-1hi in the TEClo (MHCIIloUEA-1lo) subset.
Fig. 5. LTα1β2-LTβR axis controls thymic regeneration.
Total body irradiation induces the production of RANKL by radioresistant CD4+ SP thymocytes and LTi cells, which triggers the upregulation of LTα1β2 expression, mostly on LTi cells. Total body irradiation also enhances LTβR expression on all TEC subsets. LTα1β2-LTβR axis favors thymic regeneration and thereby enhances T-cell reconstitution trough (i) TEC recovery by stimulating their proliferation, differentiation and survival and (ii) the homing of lymphoid progenitor cells (LPC) by increasing the expression of CCL19 and CCL21 chemokines in TEC and P-selectin, ICAM-1 and VCAM-1 adhesion molecules on endothelial cells.
Whereas LTα is dispensable for TEC cellularity in the steady state [31, 83], this cytokine has a unique role in TEC regeneration since the recovery of cTEC, mTEClo, Aire− mTEChi, Aire+ mTEChi and TEPC-enriched cells is defective in BM-transplanted Lta−/− recipients [31]. The LTα1β2/LTβR axis therefore controls both the thymic homing of LPC and the recovery of TEC, which constitutes two important aspects of thymic regeneration (Fig. 5). Consequently, T-cell reconstitution from the DN to the SP stage is impaired in BM-transplanted Lta−/− recipients. The stimulation of the LTα1β2/LTβR axis constitutes an interesting potential immunotherapeutic target to boost T-cell recovery not only after BMT but also in the elderly in which the thymic activity is severely altered [97, 98]. It is worth mentioning that LTβR is also required for spleen and liver regeneration, indicative of a conserved repair mechanism in other tissues [99–101].
Concluding remarks
The lymphotoxin pathway was initially described to regulate medulla organization and the trafficking of thymocytes. However, given that LTβR is expressed by distinct stromal cells, this pathway plays a broader role in several aspects of the thymic function. In particular, transgenic mice with a conditional deletion of Ltbr in specific stromal cells have recently ameliorated our understanding of the implication of this pathway in the thymus. These recent discoveries have highlighted novel roles including in the homing of LPC, thymocyte egress, the recruitment of peripheral DC, mTEC composition and clonal deletion (Table 1). A particular focus on the embryonic versus postnatal stage is nevertheless expected to unravel specific functions of this pathway at different stages of life. Additional studies are also needed to identify the downstream target genes induced by LTβR activation in the distinct thymic stromal cells such as cTEC, mTEC, endothelial cells, fibroblasts and dendritic cells. The LTα1β2/LTβR axis controlling two important facets of thymic regeneration, i.e. LPC homing and TEC recovery, the stimulation of this axis could constitute an interesting therapeutic target to ameliorate de novo thymopoiesis in patients in which the thymic activity is compromised. In conclusion, improving our knowledge on the lymphotoxin axis in the thymus is expected to pave the way toward preclinical studies in both autoimmunity and regenerative medicine.
Acknowledgements
We thank Lena Alexopoulou (CIML, Marseille) and Arnauld Sergé (LAI, Marseille) for critical reading of the manuscript. The M.I. laboratory at CIML received funding from Excellence Initiative of Aix-Marseille University-A*Midex, a French “Investissements d’avenir” program (LTalpha-Treg to MI) and from the Agence Nationale de la Recherche (grant ANR-19-CE18-0021-01, RANKLthym to MI). This work was also supported by institutional grants from Institut National de la Santé et de la Recherche Médicale, Centre National de la Recherche Scientifique and Aix-Marseille Université. AB is supported by a PhD fellowship from the Ministère de l’Enseignement Supérieur et de la Recherche.
Author contributions
MI and AB contributed equally in the literature search, writing, design of the figures, edition and proofreading of the manuscript.
Funding
Funding for this work is mentioned in the acknowledgements.
Ethics statment
This review did not require ethical approval.
Competing interests
The authors declare no competing interests.
Footnotes
Edited by S. Nagata
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williams TW, Granger GA. Lymphocyte in vitro cytotoxicity: lymphotoxins of several mammalian species. Nature. 1968;219:1076–7. doi: 10.1038/2191076a0. [DOI] [PubMed] [Google Scholar]
- 2.Ruddle NH. Lymphotoxin and TNF: how it all began-a tribute to the travelers. Cytokine Growth Factor Rev. 2014;25:83–9. doi: 10.1016/j.cytogfr.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mauri DN, Ebner R, Montgomery RI, Kochel KD, Cheung TC, Yu GL, et al. LIGHT, a new member of the TNF superfamily, and lymphotoxin alpha are ligands for herpesvirus entry mediator. Immunity. 1998;8:21–30. doi: 10.1016/S1074-7613(00)80455-0. [DOI] [PubMed] [Google Scholar]
- 4.Ware CF. Network communications: lymphotoxins, LIGHT, and TNF. Annu Rev Immunol. 2005;23:787–819. doi: 10.1146/annurev.immunol.23.021704.115719. [DOI] [PubMed] [Google Scholar]
- 5.Crowe PD, VanArsdale TL, Walter BN, Ware CF, Hession C, Ehrenfels B, et al. A lymphotoxin-beta-specific receptor. Science. 1994;264:707–10. doi: 10.1126/science.8171323. [DOI] [PubMed] [Google Scholar]
- 6.Androlewicz MJ, Browning JL, Ware CF. Lymphotoxin is expressed as a heteromeric complex with a distinct 33-kDa glycoprotein on the surface of an activated human T cell hybridoma. J Biol Chem. 1992;267:2542–7. doi: 10.1016/S0021-9258(18)45914-5. [DOI] [PubMed] [Google Scholar]
- 7.Browning JL, Ngam-ek A, Lawton P, DeMarinis J, Tizard R, Chow EP, et al. Lymphotoxin beta, a novel member of the TNF family that forms a heteromeric complex with lymphotoxin on the cell surface. Cell. 1993;72:847–56. doi: 10.1016/0092-8674(93)90574-A. [DOI] [PubMed] [Google Scholar]
- 8.Browning JL, Sizing ID, Lawton P, Bourdon PR, Rennert PD, Majeau GR, et al. Characterization of lymphotoxin-alpha beta complexes on the surface of mouse lymphocytes. J Immunol. 1997;159:3288–98. [PubMed] [Google Scholar]
- 9.Kabashima K, Banks TA, Ansel KM, Lu TT, Ware CF, Cyster JG. Intrinsic lymphotoxin-beta receptor requirement for homeostasis of lymphoid tissue dendritic cells. Immunity. 2005;22:439–50. doi: 10.1016/j.immuni.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Upadhyay V, Fu YX. Lymphotoxin signalling in immune homeostasis and the control of microorganisms. Nat Rev Immunol. 2013;13:270–9. doi: 10.1038/nri3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Togni P, Goellner J, Ruddle NH, Streeter PR, Fick A, Mariathasan S, et al. Abnormal development of peripheral lymphoid organs in mice deficient in lymphotoxin. Science. 1994;264:703–7. doi: 10.1126/science.8171322. [DOI] [PubMed] [Google Scholar]
- 12.Wang H, Feng J, Qi C, Morse HC., 3rd An ENU-induced mutation in the lymphotoxin alpha gene impairs organogenesis of lymphoid tissues in C57BL/6 mice. Biochem Biophys Res Commun. 2008;370:461–7. doi: 10.1016/j.bbrc.2008.03.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Futterer A, Mink K, Luz A, Kosco-Vilbois MH, Pfeffer K. The lymphotoxin beta receptor controls organogenesis and affinity maturation in peripheral lymphoid tissues. Immunity. 1998;9:59–70. doi: 10.1016/S1074-7613(00)80588-9. [DOI] [PubMed] [Google Scholar]
- 14.Koni PA, Sacca R, Lawton P, Browning JL, Ruddle NH, Flavell RA. Distinct roles in lymphoid organogenesis for lymphotoxins alpha and beta revealed in lymphotoxin beta-deficient mice. Immunity. 1997;6:491–500. doi: 10.1016/S1074-7613(00)80292-7. [DOI] [PubMed] [Google Scholar]
- 15.Rennert PD, Browning JL, Mebius R, Mackay F, Hochman PS. Surface lymphotoxin alpha/beta complex is required for the development of peripheral lymphoid organs. J Exp Med. 1996;184:1999–2006. doi: 10.1084/jem.184.5.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rennert PD, Browning JL, Hochman PS. Selective disruption of lymphotoxin ligands reveals a novel set of mucosal lymph nodes and unique effects on lymph node cellular organization. Int Immunol. 1997;9:1627–39. doi: 10.1093/intimm/9.11.1627. [DOI] [PubMed] [Google Scholar]
- 17.Cyster JG. Blown away: the unexpected role of lymphotoxin in lymphoid organ development. J Immunol. 2014;192:2007–9. doi: 10.4049/jimmunol.1400059. [DOI] [PubMed] [Google Scholar]
- 18.Gommerman JL, Browning JL, Ware CF. The Lymphotoxin Network: orchestrating a type I interferon response to optimize adaptive immunity. Cytokine growth factor Rev. 2014;25:139–45. doi: 10.1016/j.cytogfr.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koroleva EP, Fu YX, Tumanov AV. Lymphotoxin in physiology of lymphoid tissues - Implication for antiviral defense. Cytokine. 2018;101:39–47. doi: 10.1016/j.cyto.2016.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iizuka K, Chaplin DD, Wang Y, Wu Q, Pegg LE, Yokoyama WM, et al. Requirement for membrane lymphotoxin in natural killer cell development. Proc Natl Acad Sci USA. 1999;96:6336–40. doi: 10.1073/pnas.96.11.6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Q, Wang Y, Wang J, Hedgeman EO, Browning JL, Fu YX. The requirement of membrane lymphotoxin for the presence of dendritic cells in lymphoid tissues. J Exp Med. 1999;190:629–38. doi: 10.1084/jem.190.5.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Summers deLuca L, Ng D, Gao Y, Wortzman ME, Watts TH, Gommerman JL. LTbetaR signaling in dendritic cells induces a type I IFN response that is required for optimal clonal expansion of CD8+ T cells. Proc Natl Acad Sci USA. 2011;108:2046–51. doi: 10.1073/pnas.1014188108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leon B, Ballesteros-Tato A, Browning JL, Dunn R, Randall TD, Lund FE. Regulation of T(H)2 development by CXCR5+ dendritic cells and lymphotoxin-expressing B cells. Nat Immunol. 2012;13:681–90. doi: 10.1038/ni.2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matsumoto M, Lo SF, Carruthers CJ, Min J, Mariathasan S, Huang G, et al. Affinity maturation without germinal centres in lymphotoxin-alpha-deficient mice. Nature. 1996;382:462–6. doi: 10.1038/382462a0. [DOI] [PubMed] [Google Scholar]
- 25.Vu F, Dianzani U, Ware CF, Mak T, Gommerman JLICOS. CD40, and lymphotoxin beta receptors signal sequentially and interdependently to initiate a germinal center reaction. J Immunol. 2008;180:2284–93. doi: 10.4049/jimmunol.180.4.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tumanov AV, Koroleva EP, Guo X, Wang Y, Kruglov A, Nedospasov S, et al. Lymphotoxin controls the IL-22 protection pathway in gut innate lymphoid cells during mucosal pathogen challenge. Cell Host Microbe. 2011;10:44–53. doi: 10.1016/j.chom.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Y, Koroleva EP, Kruglov AA, Kuprash DV, Nedospasov SA, Fu YX, et al. Lymphotoxin beta receptor signaling in intestinal epithelial cells orchestrates innate immune responses against mucosal bacterial infection. Immunity. 2010;32:403–13. doi: 10.1016/j.immuni.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kruglov AA, Grivennikov SI, Kuprash DV, Winsauer C, Prepens S, Seleznik GM, et al. Nonredundant function of soluble LTα3 produced by innate lymphoid cells in intestinal homeostasis. Science. 2013;342:1243–6. doi: 10.1126/science.1243364. [DOI] [PubMed] [Google Scholar]
- 29.Boehm T, Scheu S, Pfeffer K, Bleul CC. Thymic medullary epithelial cell differentiation, thymocyte emigration, and the control of autoimmunity require lympho-epithelial cross talk via LTbetaR. J Exp Med. 2003;198:757–69. doi: 10.1084/jem.20030794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hikosaka Y, Nitta T, Ohigashi I, Yano K, Ishimaru N, Hayashi Y, et al. The cytokine RANKL produced by positively selected thymocytes fosters medullary thymic epithelial cells that express autoimmune regulator. Immunity. 2008;29:438–50. doi: 10.1016/j.immuni.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 31.Lopes N, Vachon H, Marie J, Irla M. Administration of RANKL boosts thymic regeneration upon bone marrow transplantation. EMBO Mol Med. 2017; 9:835–51. [DOI] [PMC free article] [PubMed]
- 32.Seach N, Ueno T, Fletcher AL, Lowen T, Mattesich M, Engwerda CR, et al. The lymphotoxin pathway regulates Aire-independent expression of ectopic genes and chemokines in thymic stromal cells. J Immunol. 2008;180:5384–92. doi: 10.4049/jimmunol.180.8.5384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nitta T, Tsutsumi M, Nitta S, Muro R, Suzuki EC, Nakano K, et al. Fibroblasts as a source of self-antigens for central immune tolerance. Nat Immunol. 2020;21:1172–80. [DOI] [PubMed]
- 34.Lind EF, Prockop SE, Porritt HE, Petrie HT. Mapping precursor movement through the postnatal thymus reveals specific microenvironments supporting defined stages of early lymphoid development. J Exp Med. 2001;194:127–34. doi: 10.1084/jem.194.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scimone ML, Aifantis I, Apostolou I, von Boehmer H, von Andrian UH. A multistep adhesion cascade for lymphoid progenitor cell homing to the thymus. Proc Natl Acad Sci USA. 2006;103:7006–11. doi: 10.1073/pnas.0602024103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krueger A, Willenzon S, Lyszkiewicz M, Kremmer E, Forster RCC. chemokine receptor 7 and 9 double-deficient hematopoietic progenitors are severely impaired in seeding the adult thymus. Blood. 2010;115:1906–12. doi: 10.1182/blood-2009-07-235721. [DOI] [PubMed] [Google Scholar]
- 37.Rossi FM, Corbel SY, Merzaban JS, Carlow DA, Gossens K, Duenas J, et al. Recruitment of adult thymic progenitors is regulated by P-selectin and its ligand PSGL-1. Nat Immunol. 2005;6:626–34. doi: 10.1038/ni1203. [DOI] [PubMed] [Google Scholar]
- 38.Plotkin J, Prockop SE, Lepique A, Petrie HT. Critical role for CXCR4 signaling in progenitor localization and T cell differentiation in the postnatal thymus. J Immunol. 2003;171:4521–7. doi: 10.4049/jimmunol.171.9.4521. [DOI] [PubMed] [Google Scholar]
- 39.Zlotoff DA, Sambandam A, Logan TD, Bell JJ, Schwarz BA, Bhandoola ACCR7. and CCR9 together recruit hematopoietic progenitors to the adult thymus. Blood. 2010;115:1897–905. doi: 10.1182/blood-2009-08-237784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shi Y, Wu W, Chai Q, Li Q, Hou Y, Xia H, et al. LTbetaR controls thymic portal endothelial cells for haematopoietic progenitor cell homing and T-cell regeneration. Nat Commun. 2016;7:12369. doi: 10.1038/ncomms12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lucas B, James KD, Cosway EJ, Parnell SM, Tumanov AV, Ware CF, et al. Lymphotoxin beta receptor controls T cell progenitor entry to the thymus. J Immunol. 2016;197:2665–72. [DOI] [PMC free article] [PubMed]
- 42.Dejardin E, Droin NM, Delhase M, Haas E, Cao Y, Makris C, et al. The lymphotoxin-beta receptor induces different patterns of gene expression via two NF-kappaB pathways. Immunity. 2002;17:525–35. doi: 10.1016/S1074-7613(02)00423-5. [DOI] [PubMed] [Google Scholar]
- 43.Schneider K, Potter KG, Ware CF. Lymphotoxin and LIGHT signaling pathways and target genes. Immunological Rev. 2004;202:49–66. doi: 10.1111/j.0105-2896.2004.00206.x. [DOI] [PubMed] [Google Scholar]
- 44.Zhu M, Chin RK, Tumanov AV, Liu X, Fu YX. Lymphotoxin beta receptor is required for the migration and selection of autoreactive T cells in thymic medulla. J Immunol. 2007;179:8069–75. doi: 10.4049/jimmunol.179.12.8069. [DOI] [PubMed] [Google Scholar]
- 45.Bichele R, Kisand K, Peterson P, Laan M. TNF superfamily members play distinct roles in shaping the thymic stromal microenvironment. Mol Immunol. 2016;72:92–102. doi: 10.1016/j.molimm.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 46.Lkhagvasuren E, Sakata M, Ohigashi I, Takahama Y. Lymphotoxin beta receptor regulates the development of CCL21-expressing subset of postnatal medullary thymic epithelial cells. J Immunol. 2013;190:5110–7. doi: 10.4049/jimmunol.1203203. [DOI] [PubMed] [Google Scholar]
- 47.Lu TT, Browning JL. Role of the lymphotoxin/LIGHT system in the development and maintenance of reticular networks and vasculature in lymphoid tissues. Front Immunol. 2014;5:47. doi: 10.3389/fimmu.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onder L, Danuser R, Scandella E, Firner S, Chai Q, Hehlgans T, et al. Endothelial cell-specific lymphotoxin-beta receptor signaling is critical for lymph node and high endothelial venule formation. J Exp Med. 2013;210:465–73. doi: 10.1084/jem.20121462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vicente R, Adjali O, Jacquet C, Zimmermann VS, Taylor N. Intrathymic transplantation of bone marrow-derived progenitors provides long-term thymopoiesis. Blood. 2010;115:1913–20. doi: 10.1182/blood-2009-06-229724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irla M, Hugues S, Gill J, Nitta T, Hikosaka Y, Williams IR, et al. Autoantigen-specific interactions with CD4+ thymocytes control mature medullary thymic epithelial cell cellularity. Immunity. 2008;29:451–63. doi: 10.1016/j.immuni.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 51.James KD, Cosway EJ, Lucas B, White AJ, Parnell SM, Carvalho-Gaspar M, et al. Endothelial cells act as gatekeepers for LTbetaR-dependent thymocyte emigration. J Exp Med. 2018;215:2984–93. doi: 10.1084/jem.20181345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zachariah MA, Cyster JG. Neural crest-derived pericytes promote egress of mature thymocytes at the corticomedullary junction. Science. 2010;328:1129–35. doi: 10.1126/science.1188222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ueno T, Saito F, Gray DH, Kuse S, Hieshima K, Nakano H, et al. CCR7 signals are essential for cortex-medulla migration of developing thymocytes. J Exp Med. 2004;200:493–505. doi: 10.1084/jem.20040643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kurobe H, Liu C, Ueno T, Saito F, Ohigashi I, Seach N, et al. CCR7-dependent cortex-to-medulla migration of positively selected thymocytes is essential for establishing central tolerance. Immunity. 2006;24:165–77. doi: 10.1016/j.immuni.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Nitta T, Nitta S, Lei Y, Lipp M, Takahama Y. CCR7-mediated migration of developing thymocytes to the medulla is essential for negative selection to tissue-restricted antigens. Proc Natl Acad Sci USA. 2009;106:17129–33. doi: 10.1073/pnas.0906956106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kozai M, Kubo Y, Katakai T, Kondo H, Kiyonari H, Schaeuble K, et al. Essential role of CCL21 in establishment of central self-tolerance in T cells. J Exp Med. 2017;214:1925–35. doi: 10.1084/jem.20161864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kwan J, Killeen N. CCR7 directs the migration of thymocytes into the thymic medulla. J Immunol. 2004;172:3999–4007. doi: 10.4049/jimmunol.172.7.3999. [DOI] [PubMed] [Google Scholar]
- 58.Lo JC, Chin RK, Lee Y, Kang HS, Wang Y, Weinstock JV, et al. Differential regulation of CCL21 in lymphoid/nonlymphoid tissues for effectively attracting T cells to peripheral tissues. J Clin Invest. 2003;112:1495–505. doi: 10.1172/JCI19188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Link A, Vogt TK, Favre S, Britschgi MR, Acha-Orbea H, Hinz B, et al. Fibroblastic reticular cells in lymph nodes regulate the homeostasis of naive T cells. Nat Immunol. 2007;8:1255–65. doi: 10.1038/ni1513. [DOI] [PubMed] [Google Scholar]
- 60.Laan M, Kisand K, Kont V, Moll K, Tserel L, Scott HS, et al. Autoimmune regulator deficiency results in decreased expression of CCR4 and CCR7 ligands and in delayed migration of CD4+ thymocytes. J Immunol. 2009;183:7682–91. doi: 10.4049/jimmunol.0804133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Valino-Rivas L, Gonzalez-Lafuente L, Sanz AB, Ruiz-Ortega M, Ortiz A, Sanchez-Nino MD. Non-canonical NFkappaB activation promotes chemokine expression in podocytes. Sci Rep. 2016;6:28857. doi: 10.1038/srep28857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bonasio R, Scimone ML, Schaerli P, Grabie N, Lichtman AH, von Andrian UH. Clonal deletion of thymocytes by circulating dendritic cells homing to the thymus. Nat Immunol. 2006;7:1092–100. doi: 10.1038/ni1385. [DOI] [PubMed] [Google Scholar]
- 63.Hadeiba H, Lahl K, Edalati A, Oderup C, Habtezion A, Pachynski R, et al. Plasmacytoid dendritic cells transport peripheral antigens to the thymus to promote central tolerance. Immunity. 2012;36:438–50. doi: 10.1016/j.immuni.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baba T, Nakamoto Y, Mukaida N. Crucial contribution of thymic Sirp alpha+ conventional dendritic cells to central tolerance against blood-borne antigens in a CCR2-dependent manner. J Immunol. 2009;183:3053–63. doi: 10.4049/jimmunol.0900438. [DOI] [PubMed] [Google Scholar]
- 65.Proietto AI, van Dommelen S, Zhou P, Rizzitelli A, D’Amico A, Steptoe RJ, et al. Dendritic cells in the thymus contribute to T-regulatory cell induction. Proc Natl Acad Sci USA. 2008;105:19869–74. doi: 10.1073/pnas.0810268105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li J, Park J, Foss D, Goldschneider I. Thymus-homing peripheral dendritic cells constitute two of the three major subsets of dendritic cells in the steady-state thymus. J Exp Med. 2009;206:607–22. doi: 10.1084/jem.20082232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lopes N, Charaix J, Cedile O, Serge A, Irla M. Lymphotoxin alpha fine-tunes T cell clonal deletion by regulating thymic entry of antigen-presenting cells. Nat Commun. 2018;9:1262. doi: 10.1038/s41467-018-03619-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Irla M, Guerri L, Guenot J, Serge A, Lantz O, Liston A, et al. Antigen recognition by autoreactive cd4(+) thymocytes drives homeostasis of the thymic medulla. PLoS ONE. 2012;7:e52591. doi: 10.1371/journal.pone.0052591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cosway EJ, Lucas B, James KD, Parnell SM, Carvalho-Gaspar M, White AJ, et al. Redefining thymus medulla specialization for central tolerance. J Exp Med. 2017;214:3183–95. doi: 10.1084/jem.20171000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cedile O, Lobner M, Toft-Hansen H, Frank I, Wlodarczyk A, Irla M, et al. Thymic CCL2 influences induction of T-cell tolerance. J Autoimmun. 2014;55:73–85. doi: 10.1016/j.jaut.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 71.Klein L, Kyewski B, Allen PM, Hogquist KA. Positive and negative selection of the T cell repertoire: what thymocytes see (and don’t see) Nat Rev Immunol. 2014;14:377–91. doi: 10.1038/nri3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cowan JE, Parnell SM, Nakamura K, Caamano JH, Lane PJ, Jenkinson EJ, et al. The thymic medulla is required for Foxp3+ regulatory but not conventional CD4+ thymocyte development. J Exp Med. 2013;210:675–81. doi: 10.1084/jem.20122070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sansom SN, Shikama-Dorn N, Zhanybekova S, Nusspaumer G, Macaulay IC, Deadman ME, et al. Population and single-cell genomics reveal the aire dependency, relief from Polycomb silencing, and distribution of self-antigen expression in thymic epithelia. Genome Res. 2014;24:1918–31. [DOI] [PMC free article] [PubMed]
- 74.Lopes N, Serge A, Ferrier P, Irla M. Thymic crosstalk coordinates medulla organization and T-Cell tolerance induction. Front Immunol. 2015;6:365. doi: 10.3389/fimmu.2015.00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.van Ewijk W, Shores EW, Singer A. Crosstalk in the mouse thymus. Immunol Today. 1994;15:214–7. doi: 10.1016/0167-5699(94)90246-1. [DOI] [PubMed] [Google Scholar]
- 76.Irla M, Guenot J, Sealy G, Reith W, Imhof BA, Serge A. Three-dimensional visualization of the mouse thymus organization in health and immunodeficiency. J Immunol. 2013;190:586–96. doi: 10.4049/jimmunol.1200119. [DOI] [PubMed] [Google Scholar]
- 77.Serge A, Bailly AL, Aurrand-Lions M, Imhof BA, Irla M. For3D: Full Organ Reconstruction in 3D, an automatized tool for deciphering the complexity of lymphoid organs. J Immunol Meth. 2015;424:32–42. [DOI] [PubMed]
- 78.Negishi I, Motoyama N, Nakayama K, Nakayama K, Senju S, Hatakeyama S, et al. Essential role for ZAP-70 in both positive and negative selection of thymocytes. Nature. 1995;376:435–8. doi: 10.1038/376435a0. [DOI] [PubMed] [Google Scholar]
- 79.Palmer DB, Viney JL, Ritter MA, Hayday AC, Owen MJ. Expression of the alpha beta T-cell receptor is necessary for the generation of the thymic medulla. Dev Immunol. 1993;3:175–9. doi: 10.1155/1993/56290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pouzolles M, Machado A, Guilbaud M, Irla M, Gailhac S, Barennes P, et al. Intrathymic adeno-associated virus gene transfer rapidly restores thymic function and long-term persistence of gene-corrected T cells. J Allergy Clin Immunol. 2020;145:679–97 e5. doi: 10.1016/j.jaci.2019.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Williams JA, Zhang J, Jeon H, Nitta T, Ohigashi I, Klug D, et al. Thymic medullary epithelium and thymocyte self-tolerance require cooperation between CD28-CD80/86 and CD40-CD40L costimulatory pathways. J Immunol. 2014;192:630–40. doi: 10.4049/jimmunol.1302550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mouri Y, Yano M, Shinzawa M, Shimo Y, Hirota F, Nishikawa Y, et al. Lymphotoxin signal promotes thymic organogenesis by eliciting RANK expression in the embryonic thymic stroma. J Immunol. 2011;186:5047–57. [DOI] [PubMed]
- 83.Venanzi ES, Gray DH, Benoist C, Mathis D. Lymphotoxin pathway and Aire influences on thymic medullary epithelial cells are unconnected. J Immunol. 2007;179:5693–700. doi: 10.4049/jimmunol.179.9.5693. [DOI] [PubMed] [Google Scholar]
- 84.White AJ, Nakamura K, Jenkinson WE, Saini M, Sinclair C, Seddon B, et al. Lymphotoxin signals from positively selected thymocytes regulate the terminal differentiation of medullary thymic epithelial cells. J Immunol. 2010;185:4769–76. doi: 10.4049/jimmunol.1002151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lucas B, White AJ, Cosway EJ, Parnell SM, James KD, Jones ND, et al. Diversity in medullary thymic epithelial cells controls the activity and availability of iNKT cells. Nat Commun. 2020;11:2198. doi: 10.1038/s41467-020-16041-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wu W, Shi Y, Xia H, Chai Q, Jin C, Ren B, et al. Epithelial LTbetaR signaling controls the population size of the progenitors of medullary thymic epithelial cells in neonatal mice. Sci Rep. 2017;7:44481. doi: 10.1038/srep44481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Martins VC, Boehm T, Bleul CC. Ltbetar signaling does not regulate Aire-dependent transcripts in medullary thymic epithelial cells. J Immunol. 2008;181:400–7. doi: 10.4049/jimmunol.181.1.400. [DOI] [PubMed] [Google Scholar]
- 88.Chin RK, Lo JC, Kim O, Blink SE, Christiansen PA, Peterson P, et al. Lymphotoxin pathway directs thymic aire expression. Nat Immunol. 2003;4:1121–7. doi: 10.1038/ni982. [DOI] [PubMed] [Google Scholar]
- 89.Santamaria JC, Borelli A, Irla M. Regulatory T cell heterogeneity in the thymus: impact on their functional activities. Front Immunol. 2021;12:643153. doi: 10.3389/fimmu.2021.643153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu M, Brown NK, Fu YX. Direct and indirect roles of the LTbetaR pathway in central tolerance induction. Trends Immunol. 2010;31:325–31. doi: 10.1016/j.it.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhou P, Fang X, McNally BA, Yu P, Zhu M, Fu YX, et al. Targeting lymphotoxin-mediated negative selection to prevent prostate cancer in mice with genetic predisposition. Proc Natl Acad Sci USA. 2009;106:17134–9. doi: 10.1073/pnas.0905707106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chin RK, Zhu M, Christiansen PA, Liu W, Ware C, Peltonen L, et al. Lymphotoxin pathway-directed, autoimmune regulator-independent central tolerance to arthritogenic collagen. J Immunol. 2006;177:290–7. doi: 10.4049/jimmunol.177.1.290. [DOI] [PubMed] [Google Scholar]
- 93.Takaba H, Morishita Y, Tomofuji Y, Danks L, Nitta T, Komatsu N, et al. Fezf2 orchestrates a thymic program of self-antigen expression for immune tolerance. Cell. 2015;163:975–87. doi: 10.1016/j.cell.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 94.Sitnik KM, Wendland K, Weishaupt H, Uronen-Hansson H, White AJ, Anderson G, et al. Context-dependent development of lymphoid stroma from adult CD34(+) adventitial progenitors. Cell Rep. 2016;14:2375–88. doi: 10.1016/j.celrep.2016.02.033. [DOI] [PubMed] [Google Scholar]
- 95.Dudakov JA, Mertelsmann AM, O’Connor MH, Jenq RR, Velardi E, Young LF, et al. Loss of thymic innate lymphoid cells leads to impaired thymopoiesis in experimental graft-versus-host disease. Blood. 2017;130:933–42. doi: 10.1182/blood-2017-01-762658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Irla M. RANK signaling in the differentiation and regeneration of thymic epithelial cells. Front Immunol. 2020;11:623265. doi: 10.3389/fimmu.2020.623265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Palmer DB. The effect of age on thymic function. Front Immunol. 2013;4:316. doi: 10.3389/fimmu.2013.00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cowan JE, Takahama Y, Bhandoola A, Ohigashi I. Postnatal involution and counter-involution of the thymus. Front Immunol. 2020;11:897. doi: 10.3389/fimmu.2020.00897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tan JK, Watanabe T. Murine spleen tissue regeneration from neonatal spleen capsule requires lymphotoxin priming of stromal cells. J Immunol. 2014;193:1194–203. doi: 10.4049/jimmunol.1302115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Anders RA, Subudhi SK, Wang J, Pfeffer K, Fu YX. Contribution of the lymphotoxin beta receptor to liver regeneration. J Immunol. 2005;175:1295–300. doi: 10.4049/jimmunol.175.2.1295. [DOI] [PubMed] [Google Scholar]
- 101.Sorg UR, Behnke K, Degrandi D, Reich M, Keitel V, Herebian D, et al. Cooperative role of lymphotoxin beta receptor and tumor necrosis factor receptor p55 in murine liver regeneration. J Hepatol. 2016;64:1108–17. doi: 10.1016/j.jhep.2015.12.006. [DOI] [PubMed] [Google Scholar]