Abstract
Background
Single-legged hop tests are frequently used in substantiating return to sport decisions following lower extremity injury. Evidence for using the non-injured leg as a reference for the injured leg in the return to sport decision-making at the criterion-based point of return to sport following lower extremity injury is lacking.
Purpose
To compare absolute values in single-legged hop tests between the non-injured leg of athletes returning to high-impact sports after lower extremity injury and the matched leg of healthy athletes.
Study Design
Cross-sectional study.
Methods
One hundred and sixty-nine athletes returning to high-impact sports after lower extremity injury and 169 matched healthy athletes executed five single-legged hop tests. Differences between athletes returning to high-impact sports after lower extremity injury and matched healthy athletes on five single-legged hop tests were analyzed using paired t-tests.
Results
There were no statistically significant differences between the non-injured leg of athletes returning to sport and the matched leg of healthy athletes. Effect sizes ranged from 0.05 to 0.14 indicating negligible effects.
Conclusion
Clinicians can use the non-injured leg as a reference for the injured leg in single-legged hop tests for deciding on return to high-impact sports after lower extremity injuries.
Level of Evidence
3b
Keywords: return to sport, lower extremity injuries, hop tests
INTRODUCTION
Lower extremity injuries frequently occur in the athletic population with more than half occurring during high-impact sports.1 For most injured athletes it is important to return to their pre-injury sports level,2 but only 52%-65% actually achieve this.3–5 In addition, athletes returning to sport have up to 25% (re-)injury risk, often at an early stage of the return to sport (RTS) period.6–9 Low rates of returning to pre-injury sports level and high risks of second injury after RTS highlights the importance of accurate RTS decision-making.10,11
In multidimensional RTS decision-making,12,13 hop tests play an important role in measuring functional performance.14,15 Single-legged hop tests assess the performance of the entire lower extremity and athletes’ ability to perform components of sport-specific actions such as hopping.16 It has been suggested that an athlete is ready for RTS when the Limb Symmetry Index (LSI) is ≥90%, implying that performance of the injured leg corresponds to 90% or more with the non-injured leg.15,17–21 However, the LSI is a controversial construct as deficits of the injured leg could be underestimated when using the detrained non-injured leg as a reference standard.11,22–26 In comparison with healthy athletes, strength and performance deficits of both the injured and non-injured leg have been found following anterior cruciate ligament reconstruction (ACLR).11,22–25,27 When clinicians rely on using the possibly detrained non-injured leg as a reference for the injured leg in RTS decision-making following ACLR, athletes could more easily attain an LSI of ≥90%.11,22–25 This may result in premature RTS clearance possibly leading to a higher risk for a (re)injury.28–31
Although the hop tests and the LSI were designed to support RTS decision-making after anterior cruciate ligament injury (ACLI) or ACLR,16,32 these hop tests are also used in clinical practice to make RTS decisions after other lower extremity injuries of the hip,33 ankle,33,34 and the hamstring(s).35 While the studies regarding bilateral deficits after ACLR included athletes at a time-based approach when athletes might not even be ready for RTS,11,14,22–25,27,36 no studies have investigated differences in hop tests in athletes who were, according to their physical therapists, at the criterion-based point of RTS and ready for RTS following different types of lower extremity injuries compared with matched healthy athletes. This may provide clinicians information regarding whether or not the non-injured leg can be used as a reference standard for the injured leg that is essential to substantiate the criterion based RTS decision-making following lower extremity injuries. Therefore, the primary purpose of this study was to compare performance in single-legged hop tests between the non-injured leg of athletes returning to high-impact sports after lower extremity injury (RTS athletes) and the matched leg of healthy athletes. In addition, this study aimed to assess differences in LSI and absolute values for the injured and matched leg between RTS athletes and healthy athletes.
MATERIALS AND METHODS
A cross-sectional study was conducted in primary care physical therapy practices in the Netherlands between April 2018 and November 2018. The study was approved by METC Zuyderland Zuyd Heerlen, the Netherlands (METCZ20180024). Written informed consent was obtained from all athletes.
Participants
Twenty-eight physical therapists, studying for a sports physical therapy master’s degree in the same educational institution, recruited and tested RTS athletes and matched healthy athletes. Each physical therapist included one RTS athlete of each of the six most prevalent lower extremity injury types; conservative treated knee injury, surgically treated knee injury, calf injury, hamstring injury, ankle inversion injury, or adductor injury. RTS athletes were all included at the criterion-based point of RTS. The physical therapists gave clearance for RTS according to the definition by Ardern et al37: “Returning to the defined sport, but not performing at the desired performance level” regardless of whether this was based on objective criteria or not.38,39 In order to have a real-life presentation of RTS-decisions in the usual care of physical therapists, the researchers were not involved in the rehabilitation process and RTS decision-making.40 After RTS clearance, RTS athletes were eligible for participation if they met the following criteria: 18-45 years of age and participating at least twice a week in high-impact sports before the injury. A lower extremity injury was considered as a time-loss injury resulting in the athlete not being able to practice their sport for at least one training or match.41 High-impact sports were defined as sports involving jumping, pivoting, and changes of direction. Athletes were excluded if they had a rheumatic or a neurological disease. For each included RTS athlete, a healthy athlete, practicing sport at the desired performance level without injury, was selected and matched by gender, sport, age (range within five years), height (range within 10 centimeters), and dominant leg (the leg used to kick a ball).18,24 Physical therapists recruited healthy athletes via the network in sport clubs or the team or network of the RTS athlete. Healthy athletes were eligible for participation if they met the same criteria as the RTS athletes with the exception of having suffered a lower extremity injury.
Hop tests
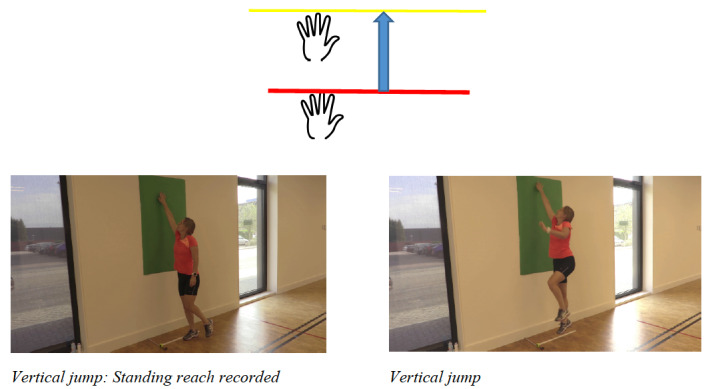
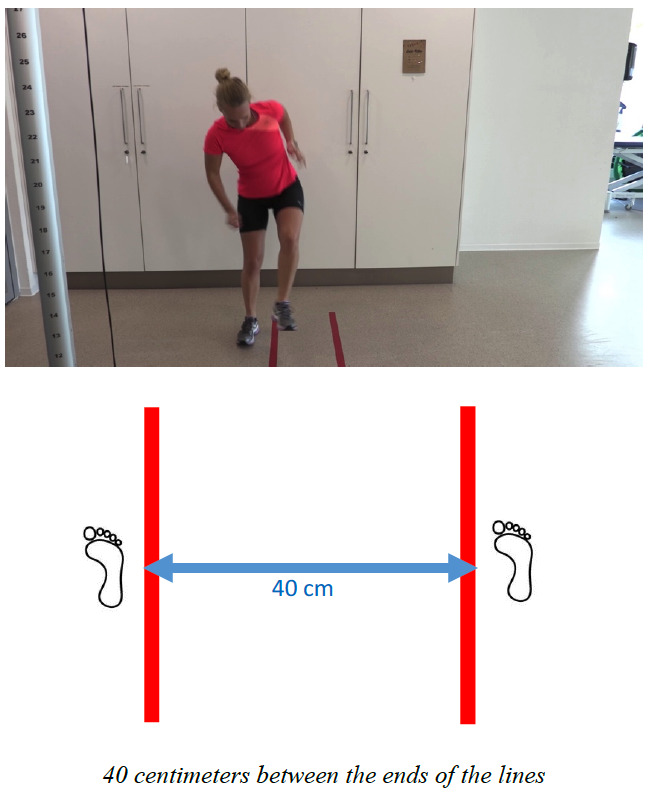
Five single-legged hop tests were executed according to previously described protocols.18,42–45 The hop tests were the single hop,18,43 triple hop,18,43 crossover hop,18,43 vertical jump,42 and 30 seconds side hop.44,45 Athletes were allowed to use arm swings.18,43,46,47 For the single, triple, and crossover hop, athletes were instructed to hop as far as possible for one jump, three jumps, or three diagonal jumps respectively.18,43 The distance was measured from the toe at the starting position to the toe at the landing position using a standard tape measure.43 For the vertical jump, the athlete was instructed to jump as high as possible with chalk on the tip of the middle finger, where the standing reach height was subtracted from the total jump height.42 For the single hop, triple hop, crossover hop, and vertical jump, athletes were asked to maintain a balanced landing for two seconds.18,43 A failed jump involved the loss of balance, touching the floor with the arms or contralateral leg, or using an additional hop on landing.43,44,47 Failure resulted in a disqualified hop.44 For the 30 seconds side hop the athletes were instructed to jump from side to side, over two strips 40 centimeter apart, as many times as possible in 30 seconds.44,45 Number of jumps, without touching the tape or touching the floor with the other foot, was recorded.45 For these hop tests, test-retest reliability ranges from 0.80 to 0.97.18,43–48
Procedures
Physical therapists received written instructions for the test procedures, execution, and scoring of the hop tests. In addition, physical therapists attended a three-hour practice session and received written instructions for the test procedures (Appendix 1). Before testing, athletes filled out a questionnaire regarding personal characteristics, their injury, and sport participation. A warm-up was carried out before the hop tests, during which the athlete ran for five minutes at a comfortable pace. After the therapist explained and demonstrated the hop test, the athlete practiced the test once.43,46,47 Tests were executed three times per leg.44–48 Failure to perform an attempt according to the protocol resulted in a disqualified hop.44 Besides the given instructions, athletes were not verbally encouraged.48 Hop tests were completed wearing sport shoes18,43,44,46,47 on a hard, even, and non-slippery surface.43,47 The order of hop tests and the leg that started were randomized (random.org).44,48 The hop tests were carried out alternately with both legs.45–47 Between the three trials of the 30 seconds side hop, athletes could rest for 30 seconds.18,43,48
Statistical analysis
Leg matching was achieved by matching the injured and non-injured leg of the RTS athlete with the corresponding leg of the healthy athlete. The maximum values for both legs were used.24,44,46 In case of three disqualified hop tests, the maximum value could not be used. The LSI was calculated by dividing the score of the injured leg or matched leg by the score of the non-injured leg or matched leg multiplied by 100%.18,42 Descriptive statistics were calculated to summarize athletes’ characteristics and outcomes of the hop tests. The differences in characteristics between RTS athletes and healthy athletes were analyzed using the McNemar test for dichotomous data and the paired t-test for continuous data.
Test-retest reproducibility using the values of each leg of the hop tests was measured by calculating an Intraclass Correlation Coefficient agreement (ICCa) (two-way random effects model, single measure). An ICC above 0.75 represents excellent reproducibility; 0.60-0.74 good reproducibility; 0.40-0.59 fair reproducibility; and <0.40 low reproducibility.49
Differences in paired data regarding hop test outcomes between RTS athletes and healthy athletes were examined for normal distribution. In case of normal distribution, the paired t-test was used to compare differences in hop tests between RTS athletes and healthy athletes. When data were non-normally distributed, the Wilcoxon signed rank test was used. For sensitivity analysis, the before mentioned differences were also analyzed using the mean score of the hop tests, because the mean is also used in clinical practice.42,43,46–48
The Cohens’ d was used to analyze the magnitude of difference with the effect size. The effect size is an objective, standardized, and easy to interpret measure regarding how big the difference is.50 An effect size of 0.20-0.49 was considered as small; 0.50-0.79 as medium; and ≥ 0.80 as large.50 Statistical significance was set at the p<0.05 level. Statistical Package for the Social Science (IBM SPSS, Chicago, IL, version 25) for Windows was used for statistical analysis. Sample size was calculated using G*Power two-tailed with an alpha of 0.05, a power of 0.95, and a small effect size (0.2), resulting in a required sample size of 327 athletes.
RESULTS
Characteristics of athletes
One hundred ninety-two RTS athletes were eligible for participation, but 23 were excluded. The excluded RTS athletes were not significantly different from included RTS athletes regarding gender, age, weeks since injury occurrence, and weeks in rehabilitation. Also 23 healthy athletes were excluded, who were not significantly different in gender and age compared to included healthy athletes.
Hop tests were completed by 169 RTS athletes and 169 healthy athletes, both aged 25.8 years (± 5.7, 5.6, respectively). Of all participating athletes, 70.4% were male. Among RTS athletes, 28 athletes were surgically treated for knee injuries (16.2%), of which 76% underwent an ACLR. There were 141 athletes conservatively treated, including 29 athletes with knee injuries (17.2%), 28 with calf injuries (16.2%), 28 with hamstring injuries (16.2%), 28 with ankle inversion injuries (16.2%), and 28 with adductor injuries (16.2%). Soccer (61.2%), hockey (10%), handball (7%), and volleyball (6%) were the most prevalent practiced sports. No significant differences were observed between RTS athletes and healthy athletes regarding gender, age, height, dominant leg, number of training sessions, number of matches, minutes training, and minutes matches per week. The percentage of RTS athletes meeting LSI’s ≥90% ranged from 61.5% to 81.7%. In the healthy athletes, the percentage of athletes meeting LSI’s ≥90% ranged from 71.0% to 91.1% (Table 1).
Table 1. Characteristics of RTS athletes and healthy athletes.
| RTS Athletes (n=169) | Healthy athletes (n=169) | p-value | |
|---|---|---|---|
| Males, n (%) | 119 (70.4) | 119 (70.4) | 1.00 |
| Age (yrs.) | 25.8 ± 5.7 | 25.8 ± 5.6 | 0.89 |
| Height (cm) | 180.4 ± 8.2 | 180.5 ± 7.8 | 0.79 |
| Dominant right leg, n (%) | 152 (89.9) | 152 (89.9) | 1.00 |
| Number of training sessions per week | 3.0 ± 1.6 | 2.9 ± 1.6 | 0.80 |
| Minutes training per week | 230.2 ± 119.3 | 233.5 ± 131.0 | 0.76 |
| Number of matches per week | 1.0 ± 0.4 | 1.00 ± 0.4 | 0.96 |
| Minutes matches per week | 79.2 ± 32.9 | 80.7 ± 34.7 | 0.44 |
| Time since injury occurrence (weeks) | 23.2 ± 30.1 | - | - |
| Time in rehabilitation (weeks) | 14.9 ± 20.2 | - | - |
| Single hop LSI ≥90, n (%) | 138 (81.7) (n=167) | 151 (89.3) (n=166) | 0.07 |
| Triple hop LSI ≥90, n (%) | 135 (79.9) (n=168) | 154 (91.1) (n=166) | <0.01* |
| Crossover hop LSI ≥90, n (%) | 134 (79.3) | 148 (87.6) (n=163) | <0.01* |
| Vertical jump LSI ≥90, n (%) | 104 (61.5) (n=158) | 120 (71.0) (n=161) | 0.11 |
| 30 seconds side hop LSI 90, n (%) | 125 (74.0) | 135 (79.9) | 0.22 |
±=standard deviation, cm=centimeter, LSI=Limb Symmetry Index, max=maximum, min=minimum, RTS=Return to Sport, yrs.=years, *=significant difference between athletes returning to sport and matched healthy athletes
Test-retest reproducibility hop tests
Test-retest reproducibility of the hop tests ranged from ICCa 0.87 to ICCa 0.94, indicating excellent reproducibility.
Comparisons between the non-injured leg in RTS athletes and the matched leg in healthy athletes
No significant differences were found between the non-injured leg of RTS athletes and the matched leg of healthy athletes, with effect sizes ranging from 0.05 to 0.14 (Figure 1). On the absolute scores of the non-injured leg, RTS athletes performed worse on all hop tests compared to the healthy athletes (Table 2).
Figure 1. Box plots hop test outcomes non-injured legs RTS athletes and matched legs of healthy athletes.
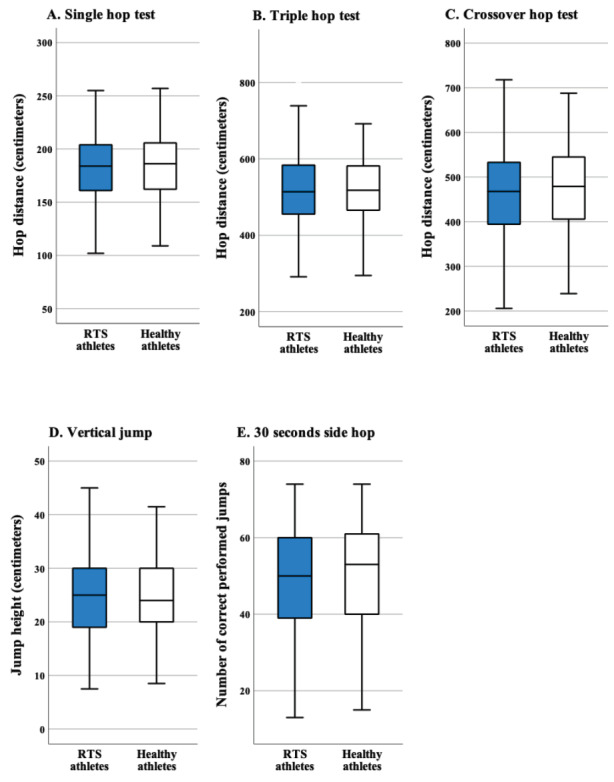
Table 2. Comparison of scores on the hop tests of the injured and non-injured leg between RTS athletes and the matched legs in healthy athletes.
| Hop test | RTS athletes (n=169) | Healthy athletes (n=169) | Mean difference ± SD (95% CI) | p-value |
|---|---|---|---|---|
| Single hop | ||||
| Injured or matched leg (cm) Mean ± SD 4 missing |
176.9 ± 35.3 2 missing |
181.1 ± 31.7 2 missing |
-4.7 ± 35.2 (-10.1 – 0.7) |
0.09 ES 0.13 |
| Non-injured or matched leg (cm) Mean ± SD 1 missing |
181.4 ± 33.3 0 missing |
183.2 ± 31.2 1 missing |
-1.8 ± 32.0 (-6.6 – 3.1) |
0.48 ES 0.06 |
| Triple hop | ||||
| Injured or matched leg (cm) Mean ± SD 2 missing |
500.5 ± 92.0 1 missing |
519.7 ± 87.7 1 missing |
-19.1 ± 82.2 (-31.7 – -6.6)* |
<0.01* ES 0.23 |
| Non-injured or matched leg (cm) Mean ± SD 2 missing |
517.6 ± 88.6 0 missing |
521.5 ± 85.4 2 missing |
-4.1 ± 79.7 (-16.3 – 8.0) |
0.50 ES 0.05 |
| Crossover hop | ||||
| Injured or matched leg (cm) Mean ± SD 2 missing |
451.0 ± 98.0 0 missing |
477.6 ± 92.5 2 missing |
-26.7 ± 95.4 (-41.3 – -12.2)* |
<0.01* ES 0.28 |
| Non-injured or matched leg (cm) Mean ± SD 4 missing |
461.3 ± 98.9 0 missing |
475.1 ± 92.3 4 missing |
-13.3 ± 96.2 (-28.0 – 1.5) |
0.08 ES 0.14 |
| Vertical jump | ||||
| Injured or matched leg (cm) Mean ± SD 12 missing |
23.6 ± 8.0 7 missing |
24.7 ± 7.8 6 missing |
-1.0 ± 8.3 (-2.3 – 0.3) |
0.13 ES 0.12 |
| Non-injured or matched leg (cm) Mean ± SD 8 missing |
24.6 ± 7.8 4 missing |
25.0 ± 7.8 4 missing |
-0.6 ± 8.8 (-1.9 – 0.8) |
0.42 ES 0.07 |
| 30 seconds side hop | ||||
| Injured or matched leg (x) Mean ± SD 0 missing |
47.1 ± 14.6 0 missing |
50.5 ± 14.1 0 missing |
-3.4 ± 13.0 (-5.4 – -1.4)* |
<0.01* ES 0.26 |
| Non-injured or matched leg (x) Mean ± SD 0 missing |
48.8 ± 13.9 0 missing |
50.5 ± 14.4 0 missing |
-1.8 ± 12.7 (-3.7 – 0.2) |
0.08 ES 0.14 |
*=significant difference between athletes returning to sport and matched healthy athletes, cm=centimeter, CI=confidence interval, ES=effect size, RTS=Return to Sport, SD=standard deviation, x=number of correct performed jumps
Comparisons between the injured leg in RTS athletes and the matched leg in healthy athletes
For the triple hop, crossover hop, and 30 seconds side hop, a significant difference was found for the injured leg in RTS athletes compared to matched leg of healthy athletes (p<0.01), with effect sizes ranging from 0.23 to 0.28, indicating small effects. On the absolute scores of the injured leg, RTS athletes performed worse on all hop tests compared to the healthy athletes (Table 2).
Comparisons of LSI’s between RTS athletes and healthy athletes
LSI of RTS athletes was significantly lower for the single hop (p=0.01), triple hop (p=<0.01), and 30 seconds side hop (p=0.02) compared to LSI of healthy athletes, with effect sizes ranging from 0.19 to 0.26. For the crossover hop and vertical jump, RTS athletes scored lower LSI’s compared to healthy athletes, but these differences were not significant (Table 3).
Table 3. Comparison of LSI between RTS athletes and healthy athletes.
| Hop test | RTS athletes | Healthy athletes | Mean difference ± SD (95% CI) | p-value |
|---|---|---|---|---|
|
Single hop LSI (%) ± SD 5 missing |
97.1 ± 10.2 2 missing |
99.5 ± 8.5 3 missing |
-2.5 ± 12.9 (-4.6 – -0.5)* |
0.01* ES 0.19 |
|
Triple hop LSI (%) ± SD 4 missing |
96.9 ± 9.2 1 missing |
99.8 ± 7.2 3 missing |
-2.9 ± 11.2 (-4.6 – -1.5)* |
<0.01* ES 0.26 |
|
Crossover hop LSI (%)± SD 6 missing |
98.6 ± 13.5 0 missing |
100.7 ± 8.9 6 missing |
-1.9 ± 15.8 (-4.3 – 0.6) |
0.14 ES 0.12 |
|
Vertical jump LSI (%)± SD 17 missing |
97.9 ± 20.7 11 missing |
99.9 ± 18.9 8 missing |
-1.8 ± 28.4 (-6.3 – 2.8) |
0.45 ES 0.06 |
|
30 seconds side hop LSI (%) ± SD 0 missing |
97.2 ± 17.4 0 missing |
101.8 ± 17.2 0 missing |
-4.5 ± 24.2 (-8.2 – -0.9)* |
0.02* ES 0.19 |
*=significant difference between athletes returning to sport and matched healthy athletes, CI=confidence interval, ES=effect size, LSI=Limb Symmetry Index, RTS=Return to Sport, SD=standard deviation
Sensitivity analysis
When using the mean outcomes of the hop tests instead of the maximum outcomes, RTS athletes also did not perform significantly differently with their non-injured leg compared to the matched leg of healthy athletes (Table 4). In addition, both the outcomes of the injured leg and the LSI were also lower in RTS athletes compared to the matched leg and the LSI of healthy athletes.
Table 4. Comparison of mean scores on the hop tests between the non-injured leg in RTS athletes and the matched leg in healthy athletes.
| Hop test | RTS athletes (n=169) | Healthy athletes (n=169) | Mean difference ± SD (95% CI) | p-value |
|---|---|---|---|---|
| Single hop | ||||
| Non-injured or matched leg (cm) Mean ± SD |
142.4 ± 49.2 | 143.8 ± 50.5 | -1.4 ± 57.8 (-10.1 – 7.4) |
0.76 ES 0.02 |
| Triple hop | ||||
| Non-injured or matched leg (cm) Mean ± SD |
411.7 ± 136.9 | 390.9 ± 146.2 | 20.8 ± 152.3 (-2.3 – 43.9) |
0.08 ES 0.14 |
| Crossover hop | ||||
| Non-injured or matched leg (cm) Mean ± SD |
351.7 ± 133.3 | 346.0 ± 138.4 | 5.7 ± 152.2 (-17.4 – 28.8) |
0.63 ES 0.04 |
| Vertical jump | ||||
| Non-injured or matched leg (cm) Mean ± SD |
18.2 ± 8.7 | 19.1 ± 9.0 | -0.9 ± 9.3 (-2.3 – 0.5) |
0.20 ES 0.10 |
| 30 seconds side hop | ||||
| Non-injured or matched leg (x) Mean ± SD |
45.2 ± 13.8 | 46.8 ± 14.4 | -1.6 ± 12.7 (-3.6 – 0.2) |
0.10 ES 0.13 |
cm=centimeter, CI=confidence interval, ES=effect size, RTS=Return to Sport, SD=standard deviation, x=number of correct performed jumps
DISCUSSION
This study found no differences between the non-injured leg of RTS athletes after lower extremity injury and the matched leg of healthy athletes. This suggests that the non-injured leg could be used as a reference for the injured leg in athletes when deciding on return to high-impact sports. In addition, although RTS athletes performed consistently lower with their injured leg and had a lower LSI compared to the matched leg and LSI of healthy athletes, differences were negligible to small.
The non-injured leg as a reference for the injured leg in RTS decision-making
Previous authors studying athletes after ACLR found that performance of both the injured and non-injured leg was significantly lower compared to the matched leg of healthy athletes.11,23–25,27 In these time-based studies, athletes were tested six to nine months after ACLR, with the time frame as main criterion to establish whether an athlete was ready to RTS.51 However, RTS clearance might have been premature since it has been advised to delay RTS to at least nine months after ACLR.6,52 The 28 RTS athletes in this study after surgically treated knee injuries were 43 weeks (± 20) in rehabilitation. When comparing the hop test outcomes of the non-injured legs with the matched leg of healthy athletes, no significant differences were found with effect sizes ranging from 0.03 to 0.35. This indicates that also after surgically treated knee injuries at the criterion-based point of RTS the non-injured leg could be used as reference for the surgically treated leg, however, the sample size of 28 is too small to make a substantiated statement.
Although athletes after ACLR were able to achieve LSI’s of ≥90 %, they failed to meet normative or pre-injury performance levels.11,23 This raises concerns regarding the value of the LSI in the RTS decision-making process which may contribute to premature or unsuccessful RTS with an increased risk for a second ACLI.11,19,31 In addition, no association was found between passing RTS hop test criteria on the LSI and RTS21,51,53,54 or between passing RTS hop test criteria on the LSI and the risk of a reinjury.21,51,55 These findings also indicate that there is an urgent need to reconsider the use of the LSI as RTS criterion.55 It is recommended that the non-injured leg is tested immediately after the injury for a more relevant benchmark in the athlete-centered approach or, more preferably, that both legs are tested prior to injury in order to be able to compare with the athletes’ own pre-injury scores and not with matched healthy athletes.51 Since pre-injury scores are often not available in clinical practice, using the non-injured leg as reference standard for the injured leg is an alternative in RTS criterion-based decision-making as this study found that the non-injured leg of RTS is not significantly different from the matched leg of healthy athletes.
Despite RTS clearance was given by the physical therapists in this study, RTS athletes not meeting LSI’s of ≥90% on each of the hop tests ranged from 18.3% to 38.5%. This range at the criterion-based point of RTS is consistent with previous studies where athletes 11-38 months after ACLI or six to seven months after ACLR not meeting LSI’s of ≥90% ranged from 19% to 86%.39,42,44,56–59 Also, 8.9% to 29.0% of healthy athletes in this study did not meet LSI’s of ≥90% on the separate hop tests. Previous findings reported that LSI’s of ≥90% were not achieved in 5% to 20% of the healthy athletes.44,57 For healthy athletes, who have no injured and non-injured leg for calculating the LSI, an LSI below 90% or above 110% can be used for asymmetry.60 When using these cut off scores, asymmetry was present in 16.0% to 51.5% of the healthy athletes in the current study in at least one of the hop tests. This high number of healthy athletes failing to reach the LSI of ≥90% and ≤110% also raises the question regarding the use of the LSI in RTS decision-making if there might be different scores for the dominant or non-dominant leg of ≥10%.21 The use of pre-injury hop scores is again recommended to compare with hop scores at the time of RTS.51 However, the non-injured leg can be used as a reference for the injured leg if pre-injury hop scores are not available.
Using maximum and mean outcomes of hop tests
In this study, failure to perform an attempt according to the protocol resulted in a disqualified hop44 and no repeated attempt was allowed due to the time it takes to execute all hop tests three times per leg. On each attempt, 18.2% of the RTS athletes and 18.5% of the healthy athletes had a disqualified hop. In previous studies, maximum or mean values of three attempts or three successful trials have been used to calculate the LSI.33,61 In most of the studies, an unsuccessful landing resulted in a repeated trial.43–45,62 Sometimes additional trials were allowed when hop test scores increased44,45 or even when the athlete or administrator felt that a better result could be achieved.63 In these previous studies, it is not described how many trials were conducted before there were enough approved trials. In this study, it is possible that repeated trials increased the hop test outcomes of athletes. It could be questionable that RTS athletes resume to training with one fifth disqualified outcomes. However, healthy athletes had the same amount of disqualified outcomes.
The results of the current study suggest that the non-injured leg can be used as a reference standard for the injured leg independent of using the maximum or mean scores. The percentage of RTS athletes meeting LSI’s ≥90% based on mean scores ranged from 54.4% for the vertical jump to 71.6% for the 30 seconds side hop. The percentage of RTS athletes meeting an LSI of ≥90% is significantly higher for maximum scores than for mean scores in all hop tests except the 30 seconds side hop. Clinicians should keep in mind that passing the LSI of ≥90% is achieved more easily using the maximum score with the possible consequence of too early RTS and a higher risk of reinjury.6,7,29
Limitations of this study
This study has three potential limitations. First, there might have been bias in the selection of RTS athletes. Physical therapists were allowed to select athletes, but this was not conducted in a consecutive order or using random sampling.64 Secondly, RTS athletes could have become familiar with the hop tests during rehabilitation or in RTS-decision making,44,47 leading to a possible overestimation of hop test scores for the RTS athletes. Van Melick et al.65 also reported this limitation that is unavoidable when athletes are in rehabilitation to RTS and the physical therapist regularly evaluates the function. On the other hand, in this study the percentage disqualified hop tests was similar in the RTS athletes (18.2%) and healthy athletes (18.5%). And third, athletes performed one practice trial42,43,46,47 and three test trials.44–48 In previous studies, one to ten practice trials were executed because of the possible learning effect where scores might improve across trials.45,48,61 It is therefore possible that after one practice trial and three test trials the scores may have increased. However, one previous study found that results could also have stabilized after three or four trials.18 Although in our study, the maximum score is almost always reached in the third trial, the second trial is not significantly higher than the first trial and the third trial is not significantly higher than the second trial.
Clinical implications and future research
The current findings indicate that the non-injured leg can be used as a reference for the injured leg after lower extremity injury in RTS decision-making. Davies et al.51 advised to use two hop tests in different planes to detect abnormality in hop test function. By testing in different planes of motion, the clinician can more clearly identify movement deficits, and these can be subsequently developed through targeted training.51 However, RTS is complex and influenced by more factors than only single-legged hop tests.12,13 In addition to the role of hop tests in multidimensional RTS decision-making,14,15 psychological factors, sport-specific decision modifiers, and quality of movement are also important.12,13 Measuring and possibly treating psychological responses such as fear is recommended before RTS as negative responses are associated with RTS and (re-)injury.3,53,66,67 The decision for readiness to RTS also depends on type of sport,68 level of play,3,53,68–70 position of play,5,71 and playing experience.70,72,73 Besides hop distance or height, factors related to neuromuscular control should also be assessed.32,51,65,74 For further research is it recommended to measure RTS outcomes such as movement quantity and quality.
CONCLUSION
No differences in single-legged hop tests were observed between the non-injured leg of RTS athletes after lower extremity injury and the matched leg of healthy athletes. Since pre-injury scores are often not available in clinical practice, clinicians can use the score of the non-injured leg as a reference for the score of the injured leg in single-legged hop tests for deciding on return to high-impact sports after lower extremity injuries.
Declaration of Conflict of Interest
All authors declare that they have no conflicts of interest relevant to the content of this manuscript.
Acknowledgments
Acknowledgements
We thank the participating physical therapists for the recruitment of athletes and for collecting the data. We also thank all the athletes who participated in this study.
APPENDIX 1: SINGLE-LEGGED HOP TESTS
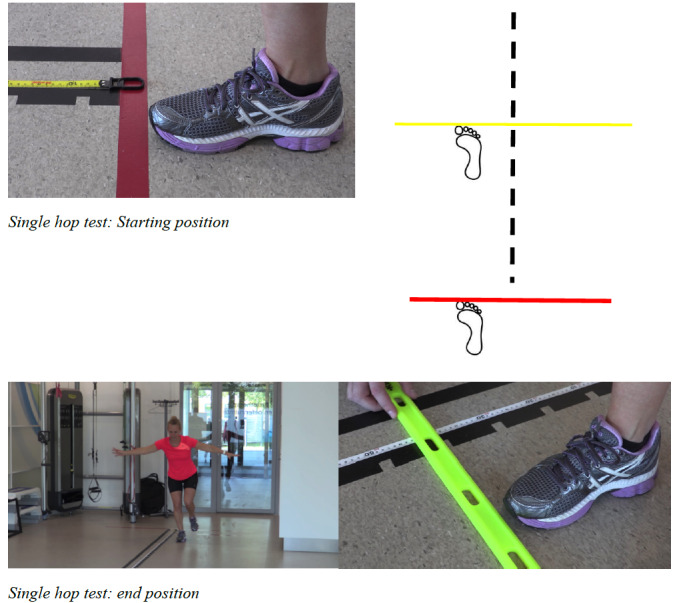
SINGLE HOP TEST
Required material: Standard tape measure and a bar to lay against the toe at the landing position.
Instruction: Stand on one leg with the toe against the starting line. Hop as far as possible for one jump while taking off and landing on the same foot. Maintain a balanced landing for two seconds. No extra hops or touching the floor with the other foot or hand are allowed. You are allowed to use your arms. The test is not accepted if you lose your balance, touch the floor with the arms or other leg, or when you perform and additional hop on landing. A failed jump resulted in a disqualified hop test outcome and no extra trial is allowed.
Measuring the outcome: Measure at the toe at the landing position using a standard tape measure and possibly a bar against the toe, rounded to half a centimeter.
Figure A1. Single hop test.
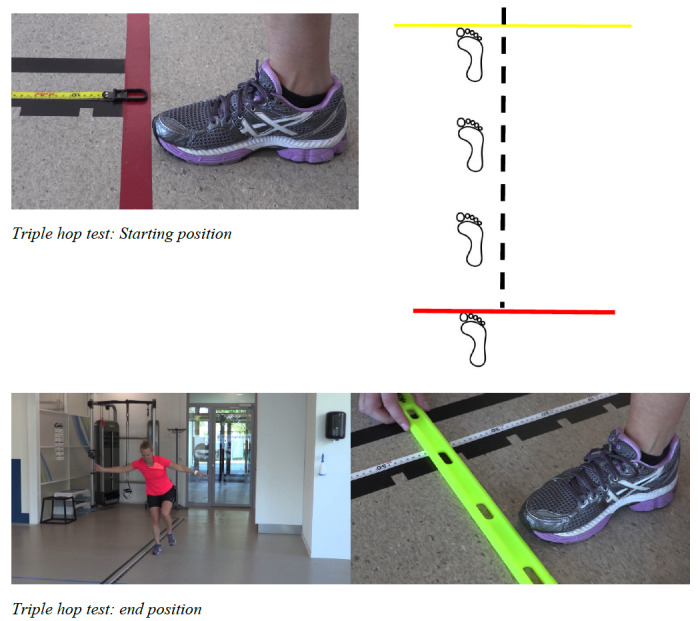
TRIPLE HOP TEST
Required material: Standard tape measure and a bar to lay against the toe at the landing position.
Instruction: Stand on one leg with the toe against the starting line. Hop as far as possible for three jumps in a row while taking off and landing on the same foot. Maintain a balanced landing for two seconds. No extra hops or touching the floor with the other foot or hand are allowed. You are allowed to use your arms. The test is not accepted if you lose your balance, touch the floor with the arms or other leg, or when you perform and additional hop on landing. A failed jump resulted in a disqualified hop test outcome and no extra trial is allowed.
Measuring the outcome: Measure at the toe at the landing position using a standard tape measure and possibly a bar against the toe, rounded to half a centimeter.
Figure A2. Triple hop test.
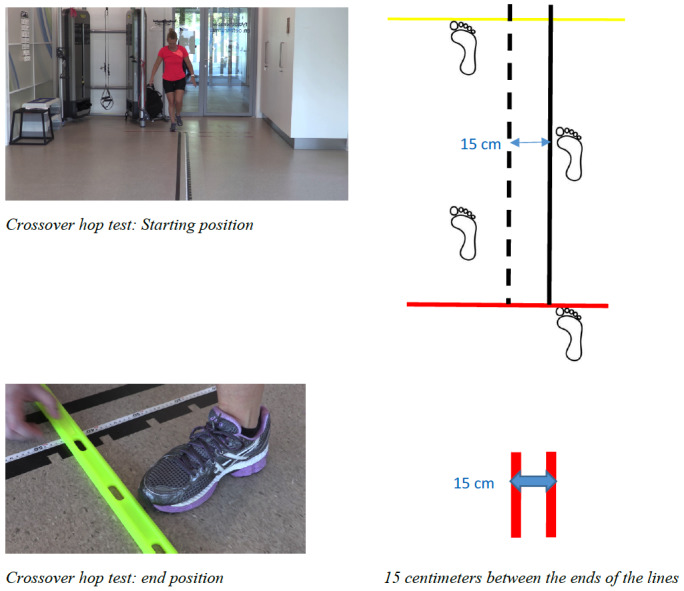
CROSSOVER HOP TEST
Required material: Standard tape measure, a bar to lay against the toe at the landing position, and two lines with 15 centimeters between the ends of the lines.
Instruction: Stand on one leg with the toe against the starting line. When the right leg is tested, you start at the right side of the lines. When the left side is tested, you start at the left sides of the lines. Hop three times as far as possible while executing diagonal hop across a 15-centimeter tape on the floor starting with a medial hop, followed by a lateral hop, and finally medial again. Maintain a balanced landing for two seconds. No extra hops or touching the floor with the other foot or hand are allowed. You are allowed to use your arms. The test is not accepted if you lose your balance, touch the floor with the arms or other leg, or when you perform and additional hop on landing. A failed jump resulted in a disqualified hop test outcome and no extra trial is allowed.
Measuring the outcome: Measure at the toe at the landing position using a standard tape measure and possibly a bar against the toe, rounded to half a centimeter.
Figure A3. Crossover hop test.
VERTICAL JUMP
Required material: Magnesium, dark paper fixed on the wall, standard tape measure.
Beforehand: The standing reach is recorded using magnesium on the tip of the middle finger.
Instruction: Jump as high as possible taking off and landing on the same foot. Maintain a balanced landing for two seconds. No extra hops, touching the floor with the other foot, or touching the wall with the shoulder or hand are allowed. You are allowed to use your arms. The test is not accepted if you lose your balance, touch the floor with the other foot, touch the wall with the shoulder or hand, or when you perform and additional hop on landing. A failed jump resulted in a disqualified hop test outcome and no extra trial is allowed.
Measuring the outcome: The top of the standing reach height subtracting from the top of the total jump height, rounded to half a centimeter.
Figure A4. Vertical jump.
30 SECONDS SIDE HOP
Required material: Stopwatch or timer with 30 seconds and two lines with 40 centimeters between the ends of the lines.
If desired, the trials can be videotaped and viewed after completion.
Instruction: When the right leg is tested, you start at the right side of the lines. When the left side is tested, you start at the left sides of the lines. The physical therapist gives the countdown “3, 2, 1, start”. Jump as many times as possible in 30 seconds from side to side on the same leg between two lines placed 40 centimeters apart. You are allowed to use your arms. The jump does not count when you touch the tape or touch the floor with the other foot.
Measuring the outcome: Number of successful jumps, without touching the tape or touching the floor with the other foot. The failed jumps were also written.
Between the three trials of the 30 seconds side hop, the athlete could rest 30 seconds.
Figure A5. 30 seconds side hop.
References
- Schmikli S. L., Backx F. J., Kemler H. J., van Mechelen W. Clin J Sport Med. 2. Vol. 19. National survey on sports injuries in the Netherlands: target populations for sports injury prevention programs; pp. 101–6. [DOI] [PubMed] [Google Scholar]
- Sonesson S., Kvist J., Ardern C., Österberg A., Silbernagel K. G. Knee Surg Sports Traumatol Arthrosc. 5. Vol. 25. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy; pp. 1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. Br J Sports Med. 21. Vol. 48. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors; pp. 1543–52. [DOI] [PubMed] [Google Scholar]
- Barastegui D., Seijas R., Alvarez-Diaz P., Rivera E., Alentorn-Geli E., Steinbacher G., Cusco X., Cugat R. Knee Surg Sports Traumatol Arthrosc. 3. Vol. 26. Assessing long-term return to play after hip arthroscopy in football players evaluating risk factors for good prognosis; pp. 963–968. [DOI] [PubMed] [Google Scholar]
- Return to play after partial lateral meniscectomy in National Football League athletes. Aune K. T., Andrews J. R., Dugas J. R., Cain E. L., Jr. 2014Am J Sports Med. 42(8):1865–72. doi: 10.1177/0363546514535069. [DOI] [PubMed] [Google Scholar]
- Grindem H., Snyder-Mackler L., Moksnes H., Engebretsen L., Risberg M. A. Br J Sports Med. 13. Vol. 50. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study; pp. 804–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyritsis P., Bahr R., Landreau P., Miladi R., Witvrouw E. Br J Sports Med. 15. Vol. 50. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture; pp. 946–51. [DOI] [PubMed] [Google Scholar]
- Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Paterno M. V., Rauh M. J., Schmitt L. C., Ford K. R., Hewett T. E. 2012Clin J Sport Med. 22(2):116–121. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Walden M., Hagglund M., Ekstrand J. 2006Br J Sports Med. 40(2):158–62. doi: 10.1136/bjsm.2005.021055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederer D., Engeroff T., Wilke J., Vogt L., Banzer W. Scand J Med Sci Sports. 10. Vol. 28. Return to play, performance, and career duration after anterior cruciate ligament rupture: A case-control study in the five biggest football nations in Europe; pp. 2226–2233. [DOI] [PubMed] [Google Scholar]
- Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. Wellsandt E., Failla M. J., Snyder-Mackler L. 2017J Orthop Sports Phys Ther. 47(5):334–338. doi: 10.2519/jospt.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creighton D. W., Shrier I., Shultz R., Meeuwisse W. H., Matheson G. O. Clin J Sport Med. 5. Vol. 20. Return-to-play in sport: a decision-based model; pp. 379–85. [DOI] [PubMed] [Google Scholar]
- Shrier I. Br J Sports Med. 20. Vol. 49. Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making; pp. 1311–5. [DOI] [PubMed] [Google Scholar]
- Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Abrams G. D., Harris J. D., Gupta A. K., McCormick F. M., Bush-Joseph C. A., Verma N. N., Cole B. J., Bach B. R., Jr. 2014Orthop J Sports Med. 2(1):2325967113518305. doi: 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber-Westin S. D., Noyes F. R. Arthroscopy. 12. Vol. 27. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction; pp. 1697–705. [DOI] [PubMed] [Google Scholar]
- Narducci E., Waltz A., Gorski K., Leppla L., Donaldson M. Int J Sports Phys Ther. 4. Vol. 6. The clinical utility of functional performance tests within one-year post-acl reconstruction: a systematic review; pp. 333–42. [PMC free article] [PubMed] [Google Scholar]
- Lynch A. D., Logerstedt D. S., Grindem H., Eitzen I., Hicks G. E., Axe M. J., Engebretsen L., Risberg M. A., Snyder-Mackler L. Br J Sports Med. 5. Vol. 49. Consensus criteria for defining 'successful outcome' after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation; pp. 335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro A. G., Herrington L. C. J Strength Cond Res. 5. Vol. 25. Between-session reliability of four hop tests and the agility T-test; pp. 1470–7. [DOI] [PubMed] [Google Scholar]
- Thomee R., Kaplan Y., Kvist J., Myklebust G., Risberg M. A., Theisen D., Tsepis E., Werner S., Wondrasch B., Witvrouw E. Knee Surg Sports Traumatol Arthrosc. 11. Vol. 19. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction; pp. 1798–805. [DOI] [PubMed] [Google Scholar]
- Thomee R., Neeter C., Gustavsson A., Thomee P., Augustsson J., Eriksson B., Karlsson J. Knee Surg Sports Traumatol Arthrosc. 6. Vol. 20. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction; pp. 1143–51. [DOI] [PubMed] [Google Scholar]
- What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Webster K. E., Hewett T. E. 2019Sports Med. 49(6):917–929. doi: 10.1007/s40279-019-01093-x. [DOI] [PubMed] [Google Scholar]
- Hiemstra L. A., Webber S., MacDonald P. B., Kriellaars D. J. Clin Biomech (Bristol, Avon) 5. Vol. 22. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft; pp. 543–50. [DOI] [PubMed] [Google Scholar]
- A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: A case control study. Gokeler A., Welling W., Benjaminse A., Lemmink K., Seil R., Zaffagnini S. 2017Orthop Traumatol Surg Res. 103(6):947–951. doi: 10.1016/j.otsr.2017.02.015. [DOI] [PubMed] [Google Scholar]
- Larsen J. B., Farup J., Lind M., Dalgas U. Hum Mov Sci. Vol. 39. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes; pp. 73–87. [DOI] [PubMed] [Google Scholar]
- Pairot de Fontenay B., Argaud S., Blache Y., Monteil K. Knee. 4. Vol. 22. Contralateral limb deficit seven months after ACL-reconstruction: an analysis of single-leg hop tests; pp. 309–12. [DOI] [PubMed] [Google Scholar]
- Patterson B. E., Crossley K. M., Perraton L. G., Kumar A. S., King M. G., Heerey J. J., Barton C. J., Culvenor A. G. Phys Ther Sport. Vol. 44. Limb symmetry index on a functional test battery improves between one and five years after anterior cruciate ligament reconstruction, primarily due to worsening contralateral limb function; pp. 67–74. [DOI] [PubMed] [Google Scholar]
- Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament Injury? Two-year follow-up after reconstruction. Chung K. S., Ha J. K., Yeom C. H., Ra H. J., Lim J. W., Kwon M. S., Kim J. G. 2015Am J Sports Med. 43(12):3013–21. doi: 10.1177/0363546515606126. [DOI] [PubMed] [Google Scholar]
- Herbst E., Hoser C., Hildebrandt C., Raschner C., Hepperger C., Pointner H., Fink C. Knee Surg Sports Traumatol Arthrosc. 5. Vol. 23. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery; pp. 1283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laboute E., Savalli L., Puig P., Trouve P., Sabot G., Monnier G., Dubroca B. Ann Phys Rehabil Med. 10. Vol. 53. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople; pp. 598–614. [DOI] [PubMed] [Google Scholar]
- Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Webster K. E., Feller J. A., Leigh W. B., Richmond A. K. 2014Am J Sports Med. 42(3):641–647. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- The utility of limb symmetry indices in return-to-sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Zwolski C., Schmitt L. C., Thomas S., Hewett T. E., Paterno M. V. 2016Am J Sports Med. 44(8):2030–8. doi: 10.1177/0363546516645084. [DOI] [PubMed] [Google Scholar]
- Barber-Westin S. D., Noyes F. R. Phys Sportsmed. 3. Vol. 39. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review; pp. 100–10. [DOI] [PubMed] [Google Scholar]
- Hegedus E. J., McDonough S. M., Bleakley C., Baxter D., Cook C. E. Br J Sports Med. 10. Vol. 49. Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2--the tests for the hip, thigh, foot and ankle including the star excursion balance test; pp. 649–56. [DOI] [PubMed] [Google Scholar]
- Criteria-based return to sport decision-making following lateral ankle sprain injury: a systematic review and narrative synthesis. Tassignon B., Verschueren J., Delahunt E., Smith M., Vicenzino B., Verhagen E., Meeusen R. 2019Sports Med. 49(4):601–619. doi: 10.1007/s40279-019-01071-3. [DOI] [PubMed] [Google Scholar]
- Return to play after hamstring injuries: a qualitative systematic review of definitions and criteria. van der Horst N., van de Hoef S., Reurink G., Huisstede B., Backx F. 2016Sports Med. 46(6):899–912. doi: 10.1007/s40279-015-0468-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbach D., Nebelung W., Becker R., Awiszus F. J Bone Joint Surg Br. 8. Vol. 83. Effects of reconstruction of the anterior cruciate ligament on voluntary activation of quadriceps femoris a prospective twitch interpolation study; pp. 1104–10. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Glasgow P., Schneiders A., Witvrouw E., Clarsen B., Cools A., Gojanovic B., Griffin S., Khan K. M., Moksnes H., Mutch S. A., Phillips N., Reurink G., Sadler R., Silbernagel K. G., Thorborg K., Wangensteen A., Wilk K. E., Bizzini M. Br J Sports Med. 14. Vol. 50. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern; pp. 853–64. [DOI] [PubMed] [Google Scholar]
- van Melick N., Pronk Y., Nijhuis-van der Sanden M., Rutten S., van Tienen T., Hoogeboom T. J Orthop Res. Meeting movement quantity or quality return to sport criteria is associated with reduced second ACL injury rate. [DOI] [PubMed]
- Less than half of ACL-reconstructed athletes are cleared for return to play based on practice guideline criteria: results from a prospective cohort study. van Melick N., Hoogeboom T, Pronk Y., et al. 2020Int J Sports Phys Ther. 15(6):1006–1018. doi: 10.26603/ijspt20201006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? Toole A. R., Ithurburn M. P., Rauh M. J., Hewett T. E., Paterno M. V., Schmitt L. C. 2017J Orthop Sports Phys Ther. 47(11):825–833. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- Fuller C. W., Ekstrand J., Junge A., Andersen T. E., Bahr R., Dvorak J., Hägglund M., McCrory P., Meeuwisse W. H. Br J Sports Med. 3. Vol. 40. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries; pp. 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S. D., Noyes F. R., Mangine R. E., McCloskey J. W., Hartman W. Clin Orthop Relat Res. 255. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees; pp. 204–14. [PubMed]
- Reid A., Birmingham T. B., Stratford P. W., Alcock G. K., Giffin J. R. Phys Ther. 3. Vol. 87. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction; pp. 337–49. [DOI] [PubMed] [Google Scholar]
- Gustavsson A., Neeter C., Thomeé P., Silbernagel K. G., Augustsson J., Thomeé R., Karlsson J. Knee Surg Sports Traumatol Arthrosc. 8. Vol. 14. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction; pp. 778–88. [DOI] [PubMed] [Google Scholar]
- Hop performance and leg muscle power in athletes: reliability of a test battery. Kockum B., Heijne A. I. 2015Phys Ther Sport. 16(3):222–7. doi: 10.1016/j.ptsp.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Ageberg E., Zätterström R., Moritz U. Scand J Med Sci Sports. 4. Vol. 8. Stabilometry and one-leg hop test have high test-retest reliability; pp. 198–202. [DOI] [PubMed] [Google Scholar]
- Brosky J. A., Nitz A. J., Malone T. R., Caborn D. N., Rayens M. K. J Orthop Sports Phys Ther. 1. Vol. 29. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction; pp. 39–48. [DOI] [PubMed] [Google Scholar]
- Bolgla L. A., Keskula D. R. J Orthop Sports Phys Ther. 3. Vol. 26. Reliability of lower extremity functional performance tests; pp. 138–42. [DOI] [PubMed] [Google Scholar]
- Fleiss J L, Levin B, Paik M C. Statistical Methods for Rates and Proportion. John Wiley And Sons Ltd; [Google Scholar]
- Streiner D. L., Norman G. R. Chest. 3. Vol. 141. Mine is bigger than yours: measures of effect size in research; pp. 595–598. [DOI] [PubMed] [Google Scholar]
- Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Davies W. T., Myer G. D., Read P. J. 2020Sports Med. 50(3):485–495. doi: 10.1007/s40279-019-01221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Beischer S., Senorski E. H., Thomee C., Samuelsson K., Thomee R. 2018Knee Surg Sports Traumatol Arthrosc. 26(7):1966–1974. doi: 10.1007/s00167-017-4747-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Webster K. E., McPherson A. L., Hewett T. E., Feller J. A. 2019Am J Sports Med. 47(11):2557–2562. doi: 10.1177/0363546519865537. [DOI] [PubMed] [Google Scholar]
- Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Webster K. E., Feller J. A. 2018Orthop J Sports Med. 6(8) doi: 10.1177/2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. Losciale J. M., Zdeb R. M., Ledbetter L., Reiman M. P., Sell T. C. 2019J Orthop Sports Phys Ther. 49(2):43–54. doi: 10.2519/jospt.2019.8190. [DOI] [PubMed] [Google Scholar]
- Gokeler A., Welling W., Zaffagnini S., Seil R., Padua D. Knee Surg Sports Traumatol Arthrosc. 1. Vol. 25. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction; pp. 192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh H., Kurosaka M., Yoshiya S., Ichihashi N., Mizuno K. Knee Surg Sports Traumatol Arthrosc. 4. Vol. 6. Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency; pp. 241–5. [DOI] [PubMed] [Google Scholar]
- Logerstedt D., Lynch A., Axe M. J., Snyder-Mackler L. Knee Surg Sports Traumatol Arthrosc. 4. Vol. 21. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction; pp. 859–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Sousa P. L., Krych A. J., Cates R. A., Levy B. A., Stuart M. J., Dahm D. L. 2017Knee Surg Sports Traumatol Arthrosc. 25(5):1356–1363. doi: 10.1007/s00167-015-3697-2. [DOI] [PubMed] [Google Scholar]
- Holsgaard-Larsen A., Jensen C., Mortensen N. H., Aagaard P. Knee. 1. Vol. 21. Concurrent assessments of lower limb loading patterns, mechanical muscle strength and functional performance in ACL-patients--a cross-sectional study; pp. 66–73. [DOI] [PubMed] [Google Scholar]
- Hegedus E. J., McDonough S., Bleakley C., Cook C. E., Baxter G. D. Br J Sports Med. 10. Vol. 49. Clinician-friendly lower extremity physical performance measures in athletes: a systematic review of measurement properties and correlation with injury, part 1. The tests for knee function including the hop tests; pp. 642–8. [DOI] [PubMed] [Google Scholar]
- Ageberg E., Thomeé R., Neeter C., Silbernagel K. G., Roos E. M. Arthritis Rheum. 12. Vol. 59. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup; pp. 1773–9. [DOI] [PubMed] [Google Scholar]
- Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Beischer S., Senorski E. Hamrin, Thomee C., Samuelsson K., Thomee R. 2018Knee Surg Sports Traumatol Arthrosc. 26(7):1966–1974. doi: 10.1007/s00167-017-4747-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann C. J. Emerg Med J. 1. Vol. 20. Observational research methods. Research design II: cohort, cross sectional, and case-control studies; pp. 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatigue affects quality of movement more in ACL-reconstructed soccer players than in healthy soccer players. van Melick N., van Rijn L., Nijhuis-van der Sanden M. W. G., Hoogeboom T. J., van Cingel R. E. H. 2019Knee Surg Sports Traumatol Arthrosc. 27(2):549–555. doi: 10.1007/s00167-018-5149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. Br J Sports Med. 17. Vol. 47. A systematic review of the psychological factors associated with returning to sport following injury; pp. 1120–6. [DOI] [PubMed] [Google Scholar]
- Ardern C. L., Österberg A., Tagesson S., Gauffin H., Webster K. E., Kvist J. Br J Sports Med. 22. Vol. 48. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction; pp. 1613–9. [DOI] [PubMed] [Google Scholar]
- Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR) A Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Dunn W. R., Spindler K. P., Consortium M. 2010Am J Sports Med. 38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casartelli N. C., Leunig M., Maffiuletti N. A., Bizzini M. Br J Sports Med. 12. Vol. 49. Return to sport after hip surgery for femoroacetabular impingement: a systematic review; pp. 819–24. [DOI] [PubMed] [Google Scholar]
- Namdari S., Baldwin K., Anakwenze O., Park M. J., Huffman G. R., Sennett B. J. Am J Sports Med. 5. Vol. 37. Results and performance after microfracture in National Basketball Association athletes; pp. 943–8. [DOI] [PubMed] [Google Scholar]
- Femoroacetabular impingement in professional football players: return to play and predictors of career length after hip arthroscopy. Menge T. J., Bhatia S., McNamara S. C., Briggs K. K., Philippon M. J. 2017Am J Sports Med. 45(8):1740–1744. doi: 10.1177/0363546517700118. [DOI] [PubMed] [Google Scholar]
- Fifteen-year audit of anterior cruciate ligament reconstructions in the Australian Football League from 1999 to 2013: return to play and subsequent ACL injury. Lai C. C. H., Feller J. A., Webster K. E. 2018Am J Sports Med. 46(14):3353–3360. doi: 10.1177/0363546518803932. [DOI] [PubMed] [Google Scholar]
- Shah V. M., Andrews J. R., Fleisig G. S., McMichael C. S., Lemak L. J. Am J Sports Med. 11. Vol. 38. Return to play after anterior cruciate ligament reconstruction in National Football League athletes; pp. 2233–9. [DOI] [PubMed] [Google Scholar]
- Kotsifaki A., Korakakis V., Whiteley R., Van Rossom S., Jonkers I. Br J Sports Med. 3. Vol. 54. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: a systematic review and meta-analysis; pp. 139–153. [DOI] [PubMed] [Google Scholar]


