Abstract
Objective: Therapeutic options for lumbar disc surgery (LDH) have been rapidly evolved worldwide. Conventional pair meta-analysis has shown inconsistent results of the safety of different surgical interventions for LDH. A network pooling evaluation of randomized controlled trials (RCT) was conducted to compare eight surgical interventions on complications for patients with LDH.
Methods: PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched for RCT from inception to June 2020, with registration in PROSPERO (CRD42020176821). This study is conducted in accordance with Cochrane guidelines. Primary outcomes include intraoperative, post-operative, and overall complications, reoperation, operation time, and blood loss.
Results: A total of 27 RCT with 2,948 participants and eight interventions, including automated percutaneous lumbar discectomy (APLD), chemonucleolysis (CN), microdiscectomy (MD), micro-endoscopic discectomy (MED), open discectomy (OD), percutaneous endoscopic lumbar discectomy (PELD), percutaneous laser disc decompression (PLDD), and tubular discectomy (TD) were enrolled. The pooling results suggested that PELD and PLDD are with lower intraoperative and post-operative complication rates, respectively. TD, PELD, PLDD, and MED were the safest procedures for LDH according to complications, reoperation, operation time, and blood loss.
Conclusion: The results of this study provided evidence that PELD and PLDD were with lower intraoperative and post-operative complication rates, respectively. TD, PELD, PLDD, and MED were the safest procedures for LDH according to complications, reoperation, operation time, and blood loss.
Systematic Review Registration: PROSPERO, identifier CRD42020176821.
Keywords: lumbar disc herniation, minimally invasive surgery, network meta-analysis, reoperation, complication
Introduction
Lumbar disc herniation (LDH) is highly associated with inflammation in the context of low back pain (1). It is a common disease in spine surgery and a primary cause of sciatica, which affects 1–2% of the general population in the USA annually (2, 3). Approximately, 5% of men and 2.5% of women will experience sciatica at some point in their lives (4). Many cases of acute sciatica can be treated conservatively with satisfactory results (5). Conservative treatment as a first-line treatment can benefit most patients with LDH (6–8). However, surgical treatment is considered a more effective way for rapid pain relief and nerve decompression (5, 9). Surgical methods including traditional discectomy and minimally invasive techniques have become more popular in recent years (10, 11).
Open discectomy (OD) has been considered the standard surgical treatment for lumbar disc herniation since 1929 (12). Currently, microdiscectomy (MD) displayed by microscope was introduced in 1976 and is identified as the gold standard procedure for treating LDH with better visualization (13). Automated percutaneous lumbar discectomy (APLD) was reported in 1985 using a new aspiration probe (14). Micro-endoscopic discectomy (MED) technology, introduced by Foley in 1997, is displayed by microendoscope performing by a transmuscular approach and has less damage to soft tissues and muscles than MD (15). With the advancement of spine endoscopy, minimally invasive surgery for symptomatic LDH (16) has been further developed to allow patients to suffer smaller surgical trauma and thereby recover faster, such as percutaneous laser disc decompression (PLDD) with laser energy delivered to the nucleus pulposus by means of fiber (17), and percutaneous endoscopic lumbar discectomy (PELD) including introduced percutaneous endoscopic interlaminar discectomy and percutaneous endoscopic transforaminal discectomy (18). Chemonucleolysis (CN), introduced in 1964, is the injection of proteolytic enzymes into the disc cavity to dissolve displaced disc material (19). The tubular discectomy (TD) system is a muscular split tubular approach that was proposed in 1997 (20). It allows surgeons to work with two hands through a small-diameter, operating table-mounted tubular retractor.
A novel surgical approach has brought some complications while benefiting patients with LDH. However, the current studies have not yet compared all interventions and analyzed their advantages and disadvantages (12, 21, 22). We use a network meta-analysis (NMA) of multiple treatments to provide a clinically useful conclusion based on the results of NMA, which can be used to guide treatment decisions.
Materials and Methods
Search Strategy
This study was registered in PROSPERO (CRD42020176821). We searched the PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) based on the preferred reporting information for systematic reviews and meta-analyses (PRISMA) guidelines to identify all relevant studies published until June 2020 (23–25). Keywords and mesh terms for the searching strategy include “lumbar disc herniation,” “open discectomy,” “intervertebral discectomy,” “microdiscectomy,” “minimally invasive surgery,” “percutaneous disc Resection,” and “laser.” Articles written only in English were included in this study.
Enrolled Criteria
Please refer to Supplementary Table 1.
Study Selection
The two authors of the review team (Wei and Li) independently reviewed all titles and abstracts found in the database during the initial online search and excluded papers that were not relevant to the subject. The full-text articles of all relevant abstracts were further reviewed. In the research selection process, disagreements between reviewers can be resolved by third-party reviewers (Zhu).
Data Extraction
A standard “characteristics of included studies” table from the Cochrane Handbook (26), was piloted in parallel with the development of the search strategy and modified to match the needs of this review. Data extraction was performed independently by two reviewers (Wei and Du). A third reviewer (Gao) checked the accuracy of the extracted data. If the data needed was missing from the paper, the study authors who participated in the review was contacted. The extracted data included study design, sample size, inclusion and exclusion criteria, study time, mean follow-up time, number of participants, age, gender, interventions, and outcomes (operation time, blood loss, number of complications, and reoperations).
Risk of Bias Within Individual Studies
This study used 13 criteria recommended in the Cochrane Back and Neck Group guidelines (27) to assess the risk of bias (Supplementary Table 2).
Summary Measures and Synthesis of Results
Pairwise meta-analyses for studies that directly compared different interventions were imported by RevMan 5.3 (Nordic Cochrane Center, Copenhagen, Denmark). NMA plots depicting were completed with statistical analysis software STATA 14.0 (StataCorp LLC, TX, USA). The NMA was performed by WinBUGS 1.4.3 (MRC Biostatistics Unit, Cambridge, UK) by a random effects model (REM) (28). Results obtained using the Markov Chain Monte Carlo (MCMC) method are reported as the median of the posterior distribution with 95% CI. Non-informative prior distributions and overdispersed initial values (with a scaling of five) were used in models in two chains to fit the model (29, 30), yielding 100,000 iterations (including 50,000 tuning iterations) and a thinning interval of 10 for each chain. Treatment inconsistency evaluation is an important aspect of NMA. It judges whether the treatment effect is consistent through direct evidence and indirect evidence. The results of node-splitting are used to evaluate the consistency of the direct and indirect comparisons; P < 0.05 indicated significant inconsistency. If there is significant heterogeneity, a random effects model was used. Otherwise, we use a fixed effects model.
Evaluating the Quality of Evidence
Two reviewers (Wei and Zhou) independently assessed the quality of the evidence for each study by using the Cochrane Collaboration tool to assess the risk of bias (31). The quality of evidence was reported using the GRADE criteria (32, 33).
Results
Literature Search and Network Structure
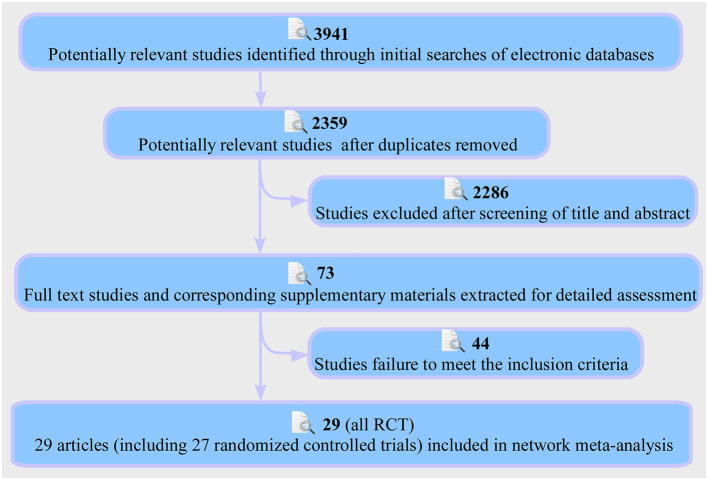
The PRISMA flow chart of the selection process for the study was shown in Figure 1. This retrieved 3,941 results, and after filtering by title, 1,582 irrelevant papers or duplicates were deleted (Wei). The title and abstract of the remaining 2,359 studies were then screened, and the remaining 73 papers were assessed for full text (Wei, Yang). Finally, 29 published articles were eligible for inclusion in the study to perform a multi-therapy meta-analysis (Figure 2) (20, 34–61). The baseline characteristics of the 27 studies (27 RCT) with 2,948 participants are shown in Supplementary Table 3 (20, 34–59).
Figure 1.
Flowchart of study selection and design.
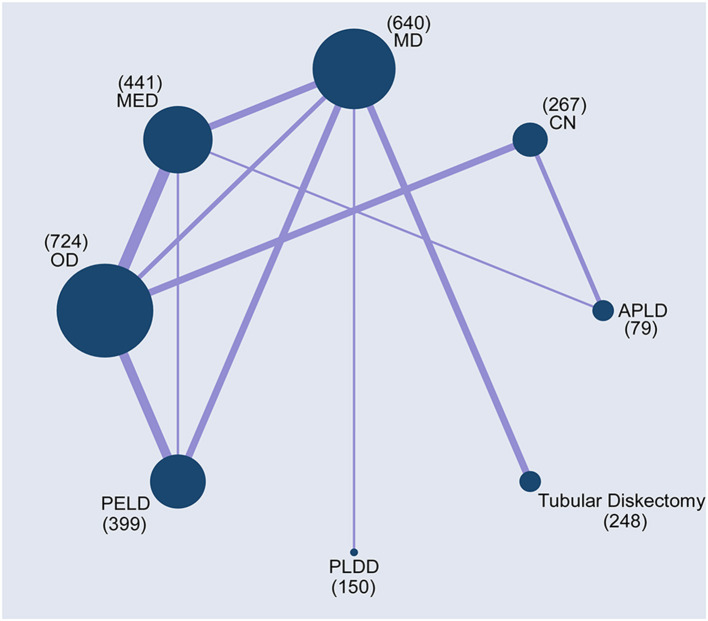
Figure 2.
Network plots of comparisons based on network meta-analysis (NMA). Each circular node represented a type of treatment. The circle size is proportional to the total number of patients. The width of lines was proportional to the number of studies performing head-to-head comparisons in the same study.
Risk of Bias in Included Studies
The risk of selection bias for each study was described according to the Cochrane Back and Neck Group guidelines (27). Supplementary Figures 1, 2 showed a summary of the risk of bias assessment. Six studies were evaluated as high risk of selection bias (35, 41, 46, 47, 52, 53). Regarding the blinding method, 11 studies were considered as high risk (20, 35, 50, 51, 58, 59). No study had been evaluated as high risk of reporting bias. One study was assessed as having a high risk of outcome detection bias (56). In addition, no studies had been evaluated as high-risk of selective reports and other potential biases.
Complication
Complication Based NMA
About 24 studies reported complications for statistical analysis (20, 34, 36, 37, 39–50, 52–59). Compared with other interventions, whether it was intraoperative, post-operative, or overall complications, PELD had a lower incidence of complications. However, the differences were not statistically significant (Figures 3A, 4A). The results obtained by the consistency model were in accordance with the results obtained by the inconsistency model, and there was no obvious inconsistency in the node split analysis (all P > 0.05, Supplementary Figure 3 and Supplementary Table 4).
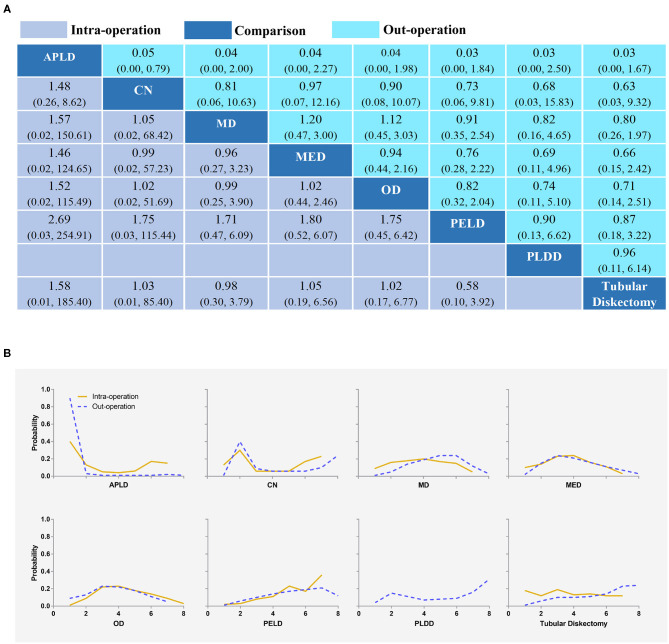
Figure 3.
Intra-complication and out-complication (A) and the rank possibility of intra-complication and out-complication (B) based NMA in the consistency model. Each cell of the profile contained the pooled odds ratio (OR) and 95% credibility intervals for disability change; significant results were in bold. APLD, Automated percutaneous lumbar discectomy; CN, Chemonucleolysis; MD, Microdiscectomy; MED, Micro-endoscopic discectomy; OD, Open discectomy; PELD, Percutaneous endoscopic lumbar discectomy; PLDD, Percutaneous laser disc decompression.
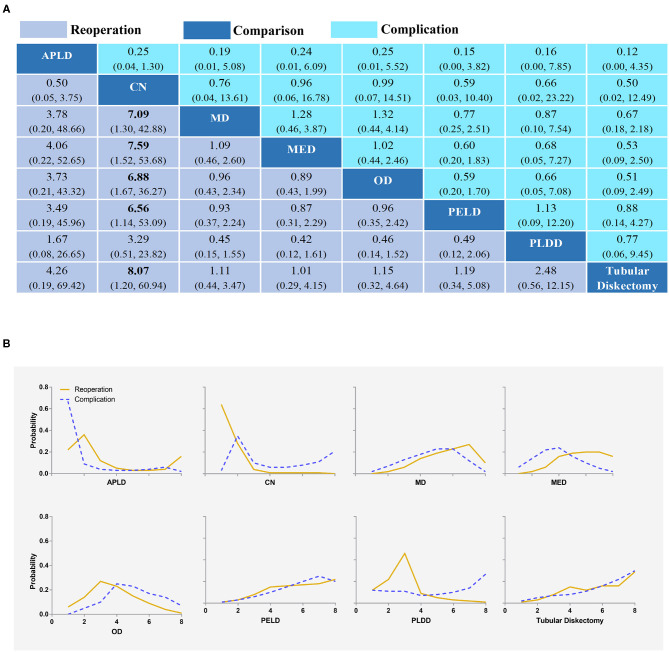
Figure 4.
Overall complication and reoperation (A) and the rank possibility of overall complication and reoperation (B) based NMA in the consistency model. Each cell of the profile contained the pooled OR and 95% credibility intervals for disability change; significant results were in bold. APLD, Automated percutaneous lumbar discectomy; CN, Chemonucleolysis; MD, Microdiscectomy; MED, Micro-endoscopic discectomy; OD, Open discectomy; PELD, Percutaneous endoscopic lumbar discectomy; PLDD, Percutaneous laser disc decompression.
The Rank Possibility of Complication Based NMA Inconsistency Model
The distribution of probabilities about the complication rate of each intervention being ranked at each of the possible eight positions is shown in Figures 3B, 4B. PELD was with the lowest intraoperative complication rate (Figure 3B). The cumulative probabilities of being among the lowest intraoperative complication rates were: PELD (36%), CN (23%), APLD (15%), TD (14%), MD (5%), OD (5%), and MED (3%). PLDD was with the lowest post-operative complication rate (Figure 3B). The cumulative probabilities of being among the lowest post-operative complication rates were: PLDD (31%), TD (24%), CN (24%), PELD (12%), MED (3%), MD (3%), OD (3%), and APLD (15%). In addition, TD, PLDD, CN, and PELD were with the lowest overall complication rates (Figure 4B). The cumulative probabilities of being among the lowest overall complication rates were: TD (29%), PLDD (26%), CN (20%), PELD (18%), MED (2%), MD (2%), APLD (1%), and OD (1%) and the probabilities were detailed in the Supplementary Table 5.
Reoperation
Reoperation Based NMA
All 27 studies reported reoperations for statistical analysis (20, 34–59). TD had a lower incidence of reoperation. However, except that CN had higher reoperation rates than MD, MED, OD, PLED, and TD with statistical significance, there were no statistically significant differences in other comparisons (Figure 4A). The results obtained by the consistency model were in accordance with the results obtained by the inconsistency model, and there was no obvious inconsistency in the node split analysis (all P > 0.05, Supplementary Figure 4 and Supplementary Table 6).
The Rank Possibility of Reoperation Based NMA Inconsistency Model
The distribution of probabilities about reoperation rates of each intervention being ranked at each of the possible eight positions is shown in Figure 4B. TD was with the lowest reoperation rate (Figure 4B). The cumulative probabilities of being among the lowest reoperation rates were: TD (29%), MED (21%), PELD (15%), OD (11%), APLD (10%), MD (9%), PLDD (2%), and CN (0%). The probabilities were detailed in the Supplementary Table 7.
Blood Loss
Blood Loss Based NMA
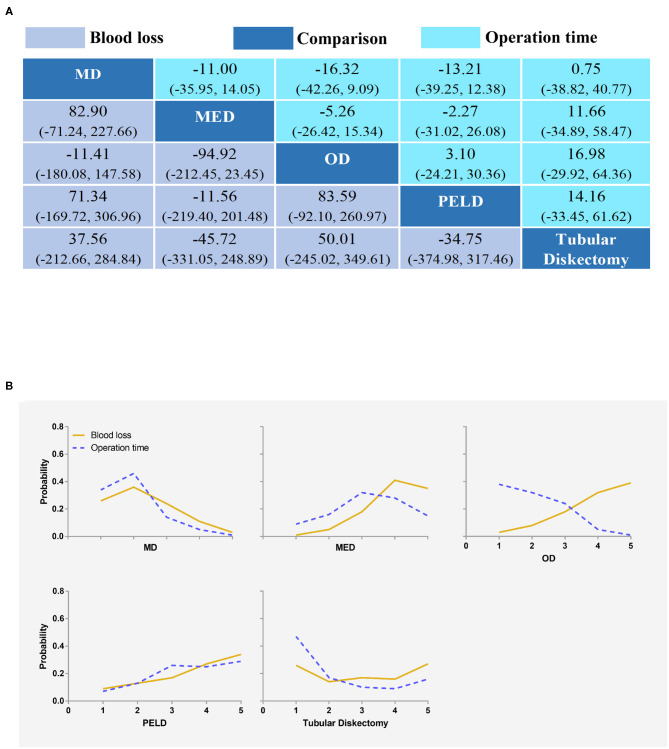
Ten studies reported blood loss for statistical analysis (34, 36, 43, 46, 47, 49, 54–57). MED had the least amount of blood loss. However, there was no statistically significant difference between any two interventions (Figure 5A). The results obtained by the consistency model were in accordance with the results obtained by the inconsistency model, and there was no obvious inconsistency in the node split analysis (all P > 0.05, Supplementary Figure 5 and Supplementary Table 8).
Figure 5.
Blood loss and operation time (A) and the rank possibility of blood loss and operation time (B) based on NMA in the consistency model. Each cell of the profile contained the pooled mean difference and 95% credibility intervals for disability change; significant results are in bold. MD, Microdiscectomy; MED, Micro-endoscopic discectomy; OD, Open discectomy; PELD, Percutaneous endoscopic lumbar discectomy.
The Rank Possibility of Blood Loss Based NMA Inconsistency Model
The distribution of probabilities about blood loss of each intervention being ranked at each of the possible five positions is shown in Figure 5B. The cumulative probabilities of being among the least blood loss were: MED (35%), PELD (34%), TD (27%), MD (3%), and OD (1%). The probabilities were detailed in the Supplementary Table 9.
Operation Time
Operation Time-Based NMA
Seventeen studies reported operation time for statistical analysis (20, 34, 36, 39, 42, 44, 46, 47, 49, 52–59). OD took the shortest time. However, there was no statistically significant difference between any two interventions (Figure 5A). The results obtained by the consistency model were in accordance with the results obtained by the inconsistency model, and there was no obvious inconsistency in the node split analysis (all P > 0.05, Supplementary Figure 5 and Supplementary Table 10).
The Rank Possibility of Operation Time-Based NMA Inconsistency Model
The distribution of probabilities about the operation time of each intervention being ranked at each of the possible five positions is shown in Figure 5B. The cumulative probabilities of being among the shortest operation time were: OD (39%), PELD (29%), TD (16%), MED (15%), and MD (1%). The probabilities were detailed in the Supplementary Table 11.
Discussion
This NMA provided a hierarchical ranking of intraoperative, post-operative, and overall complications, reoperations, blood loss, and operation time for eight different interventions for LDH patients. In recent years, minimally invasive technologies have developed rapidly, including PELD, TD, MED, and MD. A total of 27 clinical RCT were included in this study. This study confirmed that they were all safe surgeries and had lower complication rates than traditional open surgery.
Compared with other interventions, whether it was intraoperative, post-operative, or total complications, APLD was with a higher incidence of complications. PELD was with the lowest intro-complication rate, which was consistent with prior studies (12, 62). PLDD was with the lowest out-complication rates. TD has the lowest complication rates, which was somewhat different from previous meta-analyses (21, 22). The previous studies believed that the overall complication rate was the lowest in PELD, and this study still had a low but not lowest complication rate in PELD. The reason for this result might be that all interventions were included reducing the incidence of bias. In addition, TD, PELD, and MED were good interventions for LDH. Their biggest advantage is that they do less damage to the spinal muscle and soft tissue, and better visualization, which makes the incidence of complications lower.
This study showed that the reoperation rate of CN was higher than MED and OD, which was statistically significant. And the result was consistent with the prior study (21). TD with the lowest reoperation rate was inconsistent with prior studies (12). This difference was due to the reason that previous studies were traditional paired meta-analyses and the number of studies included was small.
Blood loss and operation time are important indicators for evaluating surgical risks. MED surgery had the least blood loss, which was inconsistent with prior studies (63). Previous studies suggested that PELD had less blood loss than MED (63). This result might be because previous studies included many non-RCT and the quality of the included studies was not high. OD took the shortest operation time, but the difference was not statistically significant. However, previous studies have suggested that OD took a longer time than PELD (18). The reason for this result might be that this meta-analysis included some dated studies when the technology was not yet mature. With the advancement of PELD technology, the operation time is gradually shortened.
Limitation
Although this study was somewhat different from previous studies, in general, the main results in this NMA were consistent with most previous reports. Previous studies without all interventions may be an important reason for this difference. Although the NMA incorporates all intervention methods and the results were relatively comprehensive, this study still had certain limitations. First, the size of the direct comparison and the sample size of many studies was small, which increases the instability of the statistical results. Second, because the prognostic indicators were reported at different time points, there was great heterogeneity. In addition, different standards of complications reported by different researchers may cause heterogeneity. So, there is an urgent need to further study and formulate a standard complication evaluation scheme for LDH discectomy. Whether PELD is better than TD and PLDD still needs to be confirmed in head-to-head randomized trials.
In conclusion, the results of this NMA provided evidence that PELD and PLDD were the safest procedures for LDH with minimal intraoperative and post-operative complications, respectively. TD, PELD, PLDD, and MED were the safest procedures for LDH according to complications, reoperation, operation time, and blood loss. The importance of this study can be used to guide treatment decisions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
All authors contributed substantially to the conception and design of the work, acquisition and interpretation of data, and the drafted work. F-LW, J-XQ, C-PZ, TL, and Q-YG contributed to the revised the work critically. All authors have approved the final version to be published and have agreed to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the National Natural Science Foundation of China for making this research possible.
Footnotes
Funding. This study was supported by grants from the National Natural Science Foundation of China (No. 81871818). The funding body had no role in the design of the study, data collection, analysis, interpretation, and in writing the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.679142/full#supplementary-material
References
- 1.Cunha C, Silva AJ, Pereira P, Vaz R, Gonçalves RM, Barbosa MA. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. (2018) 20:251. 10.1186/s13075-018-1743-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A. Current concepts for lumbar disc herniation. Int Orthop. (2019) 43:841–51. 10.1007/s00264-018-4247-6 [DOI] [PubMed] [Google Scholar]
- 3.Wei FL, Li T, Song Y, Bai LY, Yuan Y, Zhou C, et al. Sciatic herpes zoster suspected of lumbar disc herniation: an infrequent case report and literature review. Front Surg. (2021) 8:663740. 10.3389/fsurg.2021.663740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine. (2008) 33:2464–72. 10.1097/BRS.0b013e318183a4a2 [DOI] [PubMed] [Google Scholar]
- 5.Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine. (2007) 32:1735–47. 10.1097/BRS.0b013e3180bc2431 [DOI] [PubMed] [Google Scholar]
- 6.Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. (2011) 20:513–22. 10.1007/s00586-010-1603-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. (2017) 10:507–16. 10.1007/s12178-017-9441-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li T, Jiang S, Lu C, Yang W, Yang Z, Hu W, et al. Melatonin: another avenue for treating osteoporosis? J Pineal Res. (2019) 66:e12548. 10.1111/jpi.12548 [DOI] [PubMed] [Google Scholar]
- 9.Hägg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. (2003) 12:12–20. 10.1007/s00586-002-0464-0 [DOI] [PubMed] [Google Scholar]
- 10.Blamoutier A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. (2013) 99:S187–96. 10.1016/j.otsr.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 11.Wei FL, Gao H, Yan X, Yuan Y, Qian S, Gao Q, et al. Comparison of postoperative outcomes between patients with positive and negative straight leg raising tests who underwent full-endoscopic transforaminal lumbar discectomy. Sci Rep. (2020) 10:16516. 10.1038/s41598-020-73357-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alvi MA, Kerezoudis P, Wahood W, Goyal A, Bydon M. Operative approaches for lumbar disc herniation: a systematic review and multiple treatment meta-analysis of conventional and minimally invasive surgeries. World Neurosurg. (2018) 114:391–407.e2. 10.1016/j.wneu.2018.02.156 [DOI] [PubMed] [Google Scholar]
- 13.Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. (2014) 14:180–91. 10.1016/j.spinee.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 14.Onik G, Helms CA, Ginsburg L, Hoaglund FT, Morris J. Percutaneous lumbar diskectomy using a new aspiration probe. AJR Am J Roentgenol. (1985) 144:1137–40. 10.2214/ajr.144.6.1137 [DOI] [PubMed] [Google Scholar]
- 15.Smith N, Masters J, Jensen C, Khan A, Sprowson A. Systematic review of microendoscopic discectomy for lumbar disc herniation. Eur Spine J. (2013) 22:2458–65. 10.1007/s00586-013-2848-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. (2014) 9:CD010328. 10.1002/14651858.CD010328.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goupille P, Mulleman D, Mammou S, Griffoul I, Valat JP. Percutaneous laser disc decompression for the treatment of lumbar disc herniation: a review. Semin Arthritis Rheum. (2007) 37:20–30. 10.1016/j.semarthrit.2007.01.006 [DOI] [PubMed] [Google Scholar]
- 18.Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta- analysis. Int J Surg. (2016) 31:86–92. 10.1016/j.ijsu.2016.05.061 [DOI] [PubMed] [Google Scholar]
- 19.Smith L. Enzyme dissolution of the nucleus pulposus in humans. JAMA. (1964) 187:137–40. 10.1001/jama.1964.03060150061016 [DOI] [PubMed] [Google Scholar]
- 20.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan WF, et al. Tubular diskectomy vs. conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. (2011) 69:135–44; discussion 44. 10.1227/NEU.0b013e318214a98c [DOI] [PubMed] [Google Scholar]
- 21.Feng F, Xu Q, Yan F, Xie Y, Cai L. Comparison of 7 surgical interventions for lumbar disc herniation: a network meta-analysis. Pain Phys. (2017) 20:E863–71. 10.36076/ppj.20.5.E863 [DOI] [PubMed] [Google Scholar]
- 22.Chen X, Chamoli U, Lapkin S, Castillo JV, Diwan AD. Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: a network meta- analysis. Eur Spine J. (2019) 28:2588–601. 10.1007/s00586-019-06142-7 [DOI] [PubMed] [Google Scholar]
- 23.Wei FL, Liu Y, Zhou CP, Sun SG, Zhu KL, Du MR, et al. Management for lumbar spinal stenosis: protocol for a network meta-analysis and systematic review. J Orthop Surg (Hong Kong). (2020) 28:2309499020975212. 10.1177/2309499020975212 [DOI] [PubMed] [Google Scholar]
- 24.Li T, Jiang S, Han M, Yang Z, Lv J, Deng C, et al. Exogenous melatonin as a treatment for secondary sleep disorders: a systematic review and meta-analysis. Front Neuroendocrinol. (2019) 52:22–8. 10.1016/j.yfrne.2018.06.004 [DOI] [PubMed] [Google Scholar]
- 25.Li T, Providencia R, Mu N, Yin Y, Chen M, Wang Y, et al. Association of metformin monotherapy or combined therapy with cardiovascular risks in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. (2021) 20:30. 10.1186/s12933-020-01202-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Furlan AD, Pennick V, Bombardier C, van Tulder M. Updated method guidelines for systematic reviews in the cochrane back review group. Spine. (2009) 34:1929–41. 10.1097/BRS.0b013e3181b1c99f [DOI] [PubMed] [Google Scholar]
- 27.Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, et al. Updated method guideline for systematic reviews in the cochrane back and neck group. Spine. (2015) 40:1660–73. 10.1097/BRS.0000000000001061 [DOI] [PubMed] [Google Scholar]
- 28.Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS ONE. (2013) 8:e76654. 10.1371/journal.pone.0076654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sutton AJ, Abrams KR. Bayesian methods in meta-analysis and evidence synthesis. Stat Methods Med Res. (2001) 10:277–303. 10.1177/096228020101000404 [DOI] [PubMed] [Google Scholar]
- 30.Wei FL, Zhou CP, Liu R, Zhu KL, Du MR, Gao HR, et al. Management for lumbar spinal stenosis: a network meta-analysis and systematic review. Int J Surg. (2021) 85:19–28. 10.1016/j.ijsu.2020.11.014 [DOI] [PubMed] [Google Scholar]
- 31.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. (2014) 349:g5630. 10.1136/bmj.g5630 [DOI] [PubMed] [Google Scholar]
- 33.Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 34.Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong). (2011) 19:30–4. 10.1177/230949901101900107 [DOI] [PubMed] [Google Scholar]
- 35.Crawshaw C, Frazer AM, Merriam WF, Mulholland RC, Webb JK. A comparison of surgery and chemonucleolysis in the treatment of sciatica. A prospective randomized trial. Spine. (1984) 9:195–8. 10.1097/00007632-198403000-00010 [DOI] [PubMed] [Google Scholar]
- 36.Thomé C, Barth M, Scharf J, Schmiedek P. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine. (2005) 2:271–8. 10.3171/spi.2005.2.3.0271 [DOI] [PubMed] [Google Scholar]
- 37.Wardlaw D, Rithchie IK, Sabboubeh AF, Vavdha M, Downing M, Eastmond CJ. Prospective randomized trial of chemonucleolysis compared with surgery for soft disc herniation with 1-year, intermediate, and long-term outcome: part II: the radiological outcome. Spine. (2013) 38:E1058–64. 10.1097/BRS.0b013e3182996301 [DOI] [PubMed] [Google Scholar]
- 38.Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. (1999) 81:958–65. 10.2106/00004623-199907000-00008 [DOI] [PubMed] [Google Scholar]
- 39.Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. (1993) 78:216–25. 10.3171/jns.1993.78.2.0216 [DOI] [PubMed] [Google Scholar]
- 40.Krugluger J, Knahr K. Chemonucleolysis and automated percutaneous discectomy–a prospective randomized comparison. Int Orthop. (2000) 24:167–9. 10.1007/s002640000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Franke J, Greiner-Perth R, Boehm H, Mahlfeld K, Grasshoff H, Allam Y, Awiszus F. Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J. (2009) 18:992–1000. 10.1007/s00586-009-0964-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gibson JNA, Subramanian AS, Scott CEH. A randomised controlled trial of transforaminal endoscopic discectomy vs. microdiscectomy. Eur Spine J. (2017) 26:847–56. 10.1007/s00586-016-4885-6 [DOI] [PubMed] [Google Scholar]
- 43.Pan L, Zhang P, Yin Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg. (2014) 12:534–7. 10.1016/j.ijsu.2014.02.015 [DOI] [PubMed] [Google Scholar]
- 44.Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. (2010) 19:443–50. 10.1007/s00586-010-1290-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Revel M, Payan C, Vallee C, Laredo JD, Lassale B, Roux C, et al. Automated percutaneous lumbar discectomy versus chemonucleolysis in the treatment of sciatica. A randomized multicenter trial. Spine. (1993) 18:1–7. 10.1097/00007632-199301000-00001 [DOI] [PubMed] [Google Scholar]
- 46.Hussein M, Abdeldayem A, Mattar MMM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. (2014) 23:1992–9. 10.1007/s00586-014-3296-9 [DOI] [PubMed] [Google Scholar]
- 47.Hussein M. Minimal incision, multifidus-sparing microendoscopic diskectomy versus conventional microdiskectomy for highly migrated intracanal lumbar disk herniations. J Am Acad Orthop Surg. (2016) 24:805–13. 10.5435/JAAOS-D-15-00588 [DOI] [PubMed] [Google Scholar]
- 48.Muralikuttan KP, Hamilton A, Kernohan WG, Mollan RA, Adair IV. A prospective randomized trial of chemonucleolysis and conventional disc surgery in single level lumbar disc herniation. Spine. (1992) 17:381–7. 10.1097/00007632-199204000-00001 [DOI] [PubMed] [Google Scholar]
- 49.Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. (2007) 61:545–9; discussion 9. 10.1227/01.NEU.0000290901.00320.F5 [DOI] [PubMed] [Google Scholar]
- 50.Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WC, Schenk B, van den Berg-Huijsmans AA, et al. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: two-year results of a randomised controlled trial. Interv Neuroradiol. (2017) 23:313–24. 10.1177/1591019917699981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abrishamkar S, Kouchakzadeh M, Mirhosseini A, Tabesh H, Rezvani M, Moayednia A, et al. Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci. (2015) 20:1133–7. 10.4103/1735-1995.172979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. (2008) 33:931–9. 10.1097/BRS.0b013e31816c8af7 [DOI] [PubMed] [Google Scholar]
- 53.Ruetten S, Komp M, Merk H, Godolias G. Recurrent lumbar disc herniation after conventional discectomy: a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech. (2009) 22:122–9. 10.1097/BSD.0b013e318175ddb4 [DOI] [PubMed] [Google Scholar]
- 54.Tullberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniationlead to better results than the standard procedure? Results of a one-year randomized study. Spine. (1993) 18:24–7. 10.1097/00007632-199301000-00005 [DOI] [PubMed] [Google Scholar]
- 55.Huang T-J, Hsu RW-W, Li Y-Y, Cheng C-C. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res. (2005) 23:406–11. 10.1016/j.orthres.2004.08.010 [DOI] [PubMed] [Google Scholar]
- 56.Ryang Y-M, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery. (2008) 62:174–81. 10.1227/01.NEU.0000311075.56486.C5 [DOI] [PubMed] [Google Scholar]
- 57.Pan Z, Ha Y, Yi S, Cao K. Efficacy of transforaminal endoscopic spine system (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit. (2016) 22:530–9. 10.12659/MSM.894870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen Z, Zhang L, Dong J, Xie P, Liu B, Wang Q, et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine. (2018) 28:300–10. 10.3171/2017.7.SPINE161434 [DOI] [PubMed] [Google Scholar]
- 59.Ding ZM, Tao YQ. Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Int Transl Med. (2017) 005:29–33. 10.11910/2227-6394.2017.05.01.06 [DOI] [Google Scholar]
- 60.Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RHMA, Peul WC. Tubular diskectomy vs. conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA. (2009) 302:149–58. 10.1001/jama.2009.972 [DOI] [PubMed] [Google Scholar]
- 61.Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WCH, Schenk B, van den Berg- Huijsmans AA, et al. Percutaneous laser disc decompression versus conventional microdiscectomy in sciatica: a randomized controlled trial. Spine J. (2015) 15:857–65. 10.1016/j.spinee.2015.01.020 [DOI] [PubMed] [Google Scholar]
- 62.Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ. A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: a meta-analysis. Biomed Res Int. (2018) 2018:9073460. 10.1155/2018/9073460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shi R, Wang F, Hong X, Wang YT, Bao JP, Liu L, et al. Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: a meta-analysis. Int Orthop. (2019) 43:923–37. 10.1007/s00264-018-4253-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.