Abstract
Over half of the world’s population is estimated to be infected with Helicobacter pylori. Chronic infection with this microbial class I carcinogen is considered the most important risk factor for developing gastric cancer. The increasing antimicrobial resistance to first-line antibiotics mainly causes the failure of current eradication therapies, inducing refractory infections. The alarming increase in multidrug resistance in H. pylori isolates worldwide is already beginning to limit the efficacy of existing treatments. Consequently, the World Health Organization (WHO) has included H. pylori in its list of “priority pathogens” for which new antibiotics are urgently needed. Novel strategies must be followed to fight this antibiotic crisis, including properly exploiting the proven therapeutic potential of medicinal plants and plant-derived phytochemicals. In this mini-review, we overview the impressive properties of naturally occurring flavonoids as effective antimicrobial agents against H. pylori, which support the use of these plant-derived bioactive compounds as promising drug candidates for inclusion in novel and personalized combinatory therapies against H. pylori infection.
Keywords: Helicobacter pylori, flavonoids, plant-derived antimicrobials, antibiotic resistance, natural products
Introduction
Helicobacter pylori inhabits the gastric mucosa of almost 4.4 billion people worldwide (Hooi et al., 2017). Without effective eradication therapy, infection usually persists lifelong, causing gastric mucosal inflammation, which may gradually progress to peptic ulcer disease, gastric adenocarcinoma, and mucosa-associated lymphoid-tissue (MALT) lymphoma (Kusters et al., 2006; Yamaoka, 2010). Presently, the efficacy of one-week standard triple therapy containing clarithromycin (CLR) and either metronidazole (MTZ) or amoxicillin (AMX) combined with a proton-pump inhibitor (PPI) has dramatically dropped, showing eradication rates as low as 50% to 70% (Fallone et al., 2016). CLR-containing regimens are no longer suitable for unconditional empiric use because of commonly high levels of antimicrobial resistance and inadequate eradication rates, while the efficacy of the other alternative treatments varies greatly, which usually causes refractory infections. Given the rate at which clinically relevant pathogens, such as H. pylori, are acquiring multidrug resistance, the feared possibility that we cannot effectively treat these human bacterial infections is becoming a reality (Boyanova et al., 2016). In 2017, the World Health Organization (WHO) included H. pylori in its first list of antibiotic-resistant “priority pathogens”, a catalogue of 12 families of bacteria that presently pose the greatest threat to human health (Tacconelli et al., 2018). Nowadays, effective novel therapy against H. pylori is mandatory to increase eradication rates and minimize both antimicrobial resistance and side effects on normal microbiota.
Long before H. pylori infection was recognized as causing chronic gastritis and peptic ulcers in 1982 (Marshall and Warren, 1984), natural products have been used by physicians and healers to combat these illnesses based on empirical knowledge (Yesilada et al., 1997). Today, over 240 plant species have demonstrated anti-H. pylori activity (Salehi et al., 2018; Baker, 2020). With the pressing need for novel therapeutic options to face the current antibiotic crisis, the scientific community’s interest in traditional medicine and the use of natural products as sources of novel antibacterial drugs have been reinforced (Cheesman et al., 2017; Anand et al., 2019). In this mini-review, we overview the impressive findings obtained due to various studies that focused on the anti-H. pylori properties of flavonoids. We also discuss the promising roles of these natural products as potential drug candidates. Finally, we revise the current strategies to improve the bioavailability and efficacy of these phytochemicals.
Flavonoids: A Large Family of Naturally Occurring Bioactive Compounds
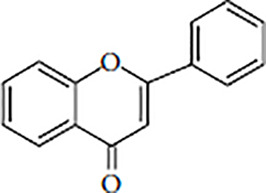
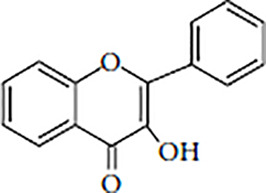
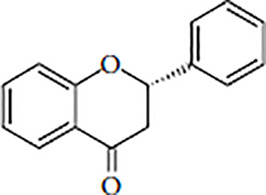
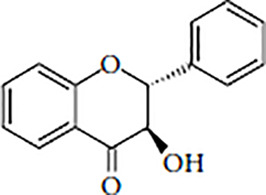
Flavonoids are polyphenolic, low-molecular-weight bioactive compounds ubiquitous in plants (Buer et al., 2010). The flavonoid family comprises over 9,000 species of molecules, which mostly share a chemical structure based on a fifteen-carbon (C6-C3-C6) skeleton comprising two benzene rings denoted as A and B, linked through a heterocyclic pyran ring referred to as ring C. The C6-C3-C6 skeleton is often hydroxylated in positions 2, 3, 5, 7, 3´, 4´, and 5´. Methyl ethers and acetyl esters of the alcohol groups are frequent, although a plethora of other derivative groups, including different alkyls, isoprenoids, and carboxylic groups, also contribute to the vast diversity of these compounds (Kumar and Pandey, 2013). Based on the oxidation state of the central pyran ring, its degree of hydroxylation, and the connection position of benzene ring B, flavonoids could be divided into seven major classes: flavones, flavonols, flavanones, flavanonols, flavanols (also known as flavan-3-ols), anthocyanidins, and isoflavones ( Table 1 ).
Table 1.
Flavonoid classes and their major natural sources.
| Flavonoid class | Structure backbone | Examples | Major natural sources |
|---|---|---|---|
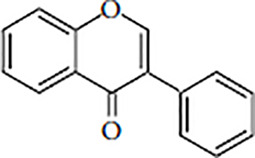
| Flavones |
|
Apigenin Chrysin Luteolin Tangeritin |
Celery, parsley, red peppers, chamomile, mint, ginkgo biloba |
| Flavonols |
|
Kaempferol Quercetin Myricetin Fisetin |
Onions, kale, lettuce, tomatoes, apples, grapes, berries, tea, red wine |
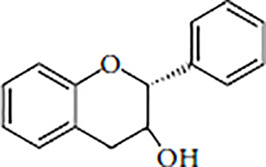
| Flavanones |
|
Hesperetin Naringenin Eriodictyol Butin |
Citrus fruits, grapes, rice |
| Flavanonols |
|
Taxifolin Aromadedrin Engeletin Astilbin |
Citrus fruits, tea, rice |
| Flavanols (Flavan-3-ols) |
|
Catechin Epicatechin Gallocatechin Proanthocyanidins |
Tea, cocoa, bananas, apples, blueberries, peaches, pears, grapes, red wine |
| Anthocyanidins |
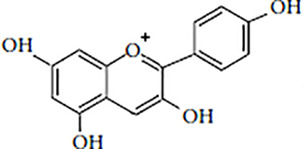
|
Malvidin Cyanidin Delphinidin Petunidin |
Berries, black currants, red grapes, merlot grapes |
| Isoflavones |
|
Daidzein Genistein Glycitein Formononetin |
Legumes |
Flavonoids are synthesized as secondary metabolites by all plant organs. These natural polyphenols are critical in plants’ interaction with other organisms, such as microorganisms, animals, and other plants, but they also participate in responding to different abiotic stresses, including UV radiation, extreme temperatures, heavy metals, and droughts (Mierziak et al., 2014). A major role of flavonoids in plants is their function as a second line of defense against oxidative stress. Flavonoids can inhibit the generation of reactive oxygen species (ROS) by several mechanisms (Kumar and Pandey, 2013), but they also quench ROS once they are produced. Some environmental stresses, such as drought, salinity, extreme temperatures, and nutrient scarcity, may significantly reduce the activity of ROS-detoxifying enzymes in chloroplasts. As an adaptive response, plants upregulate the biosynthesis of ROS-scavenging flavonoids. These polyphenols will not only absorb the most energetic solar wavelengths (i.e., UV-B and UV-A) but will also scavenge free metal ions, peroxyl, superoxide, and peroxynitrite radicals, thereby avoiding lipid peroxidation and oxidative damage to other biomolecules (Kumar and Pandey, 2013; Del Valle et al., 2020).
Mechanisms of Antimicrobial Action—A Close Relationship Between Structure and Activity
As with other phytochemicals, the antimicrobial activity of flavonoids appears multifactorial while acting against different molecular targets in the pathogen instead of having one specific action site. However, the presence of certain structural features in the flavonoid molecule enhances its pharmacological effects, reinforcing one or another action mechanism, suggesting a relationship between the flavonoid structure and its antiviral and/or antimicrobial activities (Cushnie and Lamb, 2005; Kumar and Pandey, 2013; Wang et al., 2018; Farhadi et al., 2019; Górniak et al., 2019). Thus, while a greater abundance in hydroxyl groups increases the antioxidant effects of flavonoids due to a higher number of functional sites for scavenging free radicals and chelating metal ions, this high degree of hydroxylation diminishes simultaneously with flavonoid lipophilicity, thereby limiting the influx of these molecules across the pathogen cell membranes. Hence, lipophilic flavonoids, such as herperetin, naringenin, sophoraflavanone G, and catechins with gallate groups, could penetrate the lipid bilayer membrane up to the zone under phosphate groups and laterally diffuse into the bilayer plane, causing alterations in membrane fluidity and permeability (Tsuchiya and Iinuma, 2000; Tarahovsky et al., 2014). Other flavonoids such as quercetin cause a decrease in the proton-motive force impairing the production of adenosine triphosphate (ATP), while apigenin and morin induce destabilization of the membrane structure by the disordering and disorientation of membrane lipids (Górniak et al., 2019).
Also, hydrophilic flavonoids could interact at the membrane surface and/or in the cytosol with proteins involved in different essential functions, including adhesins, cell envelope transporters, transcriptional regulators, enzymes, and toxins, inactivating these biomolecules by forming flavonoid-protein complexes through hydrophobic interactions, hydrogen, and/or covalent bonds (Kumar and Pandey, 2013; Górniak et al., 2019). Notably, little difference in the molecular structure of two flavonoids could be responsible for different effectivities in their capability to inhibit the biological activity of the same protein target. For instance, both apigenin and quercetin inhibited the function of D-alanine:D-alanine ligase (Ddl) using the same inhibition mechanism as competing with the substrate ATP (Wu D. et al., 2008). Although these two flavonoids only differ in the two additional hydroxyl groups that quercetin possesses at positions 3 and 3´, this little difference induces a substantial increase in the affinity of quercetin by the active site of the enzyme, resulting in at least a three-fold increase in its inhibitory activity against Ddl regarding apigenin. However, quercetin exhibited lower antibacterial activity than apigenin, which could be a consequence of poorer transport across cell membranes due to lower lipophilicity (Wu D. et al., 2008).
Natural Flavonoids Against Helicobacter pylori Infection
Although many published studies have described the therapeutic potential of different plant extracts and other flavonoid-rich natural products (Ankolekar et al., 2011; Njume et al., 2011; Takeuchi et al., 2014; Wang, 2014; Boyanova et al., 2015; Salehi et al., 2018; Baker, 2020; Mendonca et al., 2020), we focused this mini-review on the advances in the knowledge of the antimicrobial activities of natural purified flavonoids against H. pylori ( Table 2 ). Notably, several flavonoids have exhibited potent antimicrobial activities (MIC ≤ 8 µg/mL) against H. pylori. These in vitro antimicrobial potencies are comparable with those exhibited by some conventional antibiotics traditionally used in anti-H. pylori therapies, such as metronidazole, against sensitive strains (Loo et al., 1997). Although the anti-H. pylori activity exhibited by these flavonoids is probably multifactorial, an increasing number of studies have successfully identified specific molecular targets of these bioactive compounds in H. pylori, unravelling both antimicrobial and antivirulence mechanisms. Thus, several bactericidal flavonoids noticeably inhibited the essential function of HsrA (González et al., 2019), an OmpR-like orphan response regulator (Lee et al., 2006), which acts as a global homeostatic regulator synchronizing metabolic functions and virulence with the availability of nutrients and cell division, also mediating the response to oxidative stress (Olekhnovich et al., 2013; Olekhnovich et al., 2014; Pelliciari et al., 2017). Isothermal titration calorimetry studies indicated that chrysin, apigenin, kaempferol, and hesperetin bind to HsrA with dissociation constants in the micromolar range, showing a 1:1 stoichiometry. Molecular docking analyses suggest that interactions between these flavonoids and HsrA preferably occur by the C-terminal effector domain of the response regulator, thereby blocking its interaction with DNA (González et al., 2019). Notably, apigenin, kaempferol, and hesperetin also affected other recognized molecular targets in H. pylori, including enzymes (Wu D. et al., 2008; Zhang et al., 2008), secretion systems (Yeon et al., 2019), and cell membranes (Moon et al., 2013).
Table 2.
Natural flavonoids with antimicrobial activities against H. pylori.
1FabZ, β-hydroxyacyl-acyl carrier-protein dehydratase; Ddl, D-Alanine:D-alanine ligase; NAT, N-acetyltransferase; PDF, Peptide deformylase. T4SS and T5SS: bacterial type IV and type V secretion systems.
2Additive or synergistic effect according to the checkerboard assay (White et al., 1996). CLR, clarithromycin; MTZ, metronidazole; TET, tetracycline; AMX, amoxicillin; LVX, levofloxacin.
Many naturally occurring flavonoids exhibit anti-urease activity ( Table 2 ). Molecular docking studies and structure–activity relationship analyses proved that 3-OH, 5-OH, and 3′,4′-dihydroxyl groups of quercetin generate hydrogen bonds with amino acid residues of H. pylori urease, which appear essential for the inhibitory activity exerted by this flavonoid. Removing or substituting any of these functional hydroxyl groups from the quercetin structure significantly decreases its urease inhibitory activity (Xiao et al., 2012). The critical impact of OH groups on the affinity and half maximal inhibitory concentration (IC50) of flavonoids against H. pylori enzymes has also been demonstrated in other studies (Wu D. et al., 2008; Yu et al., 2015). Flavonoids’ value as effective anti-H. pylori therapeutic drugs is not only supported by their proven bactericidal effect but also due to their antivirulence actions, which in many cases reduce damage to the host and alleviate associated diseases. Some H. pylori virulence factors, including cytotoxin-associated gene A (CagA) and vacuolating cytotoxin A (VacA), are critical in the inflammation process associated with infection with this pathogen. Cytotoxin CagA (Ansari and Yamaoka, 2020), encoded by the cag pathogenicity island, is translocated to host cells via the type IV secretion system (T4SS), a sophisticated transmembrane protein complex that directly injects the toxin into gastric epithelial cells (Backert et al., 2017). Once into the target cells, CagA activates NF-κB, a master regulator of immune and inflammatory responses that modulates the gene expression of pro-inflammatory cytokines, such as IL-8, TNF-α, and IL-1β (Lamb and Chen, 2013). Additionally, the cytotoxin VacA (Palframan et al., 2012), which is secreted from H. pylori via the type V secretion system (T5SS), acts on the host cell, inducing vacuolation and apoptosis, and also increases IL-8 production by activating the p38 MAPK via intracellular Ca2+ release, thereby activating the transcription factors, ATF-2, CREB, and NF-κB (Hisatsune et al., 2008). Several flavonoids, including apigenin (Wang and Huang, 2013), kaempferol (Yeon et al., 2019), quercetin (Gonzalez-Segovia et al., 2008; Zhang et al., 2017), nobiletin (Ouyang et al., 2020), baicalin, baicalein (Chen et al., 2018), galangin (Skiba et al., 2016), and genistein (Siriviriyakul et al., 2020) have shown protection against gastric inflammation associated with H. pylori infection by reducing pro-inflammatory cytokine expression. Thus, kaempferol decreased the mRNA levels of IL-8, TNF-α, and IL-1β in gastric adenocarcinoma cells infected with H. pylori by inhibiting vacA expression and suppressing CagA and VacA translocation to target cells by inhibiting the expression of several T4SS and T5SS components (Yeon et al., 2019). Quercetin significantly reduced in vivo gastric inflammation in H. pylori-infected mice by reducing IL-8 secretion and downregulating the p38 MAPK signaling pathway (Zhang et al., 2017). Apigenin decreased the levels of IL-8 by inhibiting the activation of NF-κB (Wang and Huang, 2013). Adding to their anti-inflammatory actions, several flavonoids have been demonstrated to protect against vacuolation, apoptosis, and lipid peroxidation induced by H. pylori in gastric mucosa (Shin et al., 2005; Gonzalez-Segovia et al., 2008; Zhang et al., 2017).
A further benefit of flavonoids as antimicrobials against H. pylori infections lies in their capacity for synergism combined with anti-H. pylori first-line antibiotics, including CLR, MTZ, or AMX ( Table 2 ). Notably, chrysin induced an eight-fold decrease in the MIC value of CLR (FIC = 0.125), and caused a 16-fold decrease in the MIC value of MTZ (FIC = 0.0625) (González et al., 2019). Likewise, hesperetin led to a 4-fold increase in the inhibitory activity of MTZ and a two-fold increase in the CLR anti-H. pylori in vitro activity (González et al., 2019). Although the molecular mechanisms by which flavonoids enhance the antimicrobial activities of conventional antibiotics remain poorly understood, some experimental evidence unravels putative synergistic interactions. Thus, the increased inhibitory activities of AMX and TET in multidrug-resistant strains of H. pylori after baicalin action appeared to be associated with a decrease in the expression of the efflux pump gene hefA (Huang et al., 2015). hefA encodes a TolC-like outer membrane channel tunnel protein that interacts with different inner-membrane translocases to form efflux systems involved in drug resistance (Liu et al., 2008). Myricetin strongly inhibited the expression of genes involved in the morphological transition of H. pylori from spiral to coccoid forms, thereby avoiding the increase in antimicrobial resistance associated with cell shape transformation, which has been observed in this pathogen. Consequently, myricetin induced a 4–16-fold reduction in the MIC values of CLR, MTZ, LVX, TET, and AMX (Krzyzek et al., 2021). In addition, several authors suggest that the proven damage triggered by certain flavonoids in the cytoplasmic membrane and/or cell wall could enhance the susceptibility of bacterial pathogens to the action of antibiotics (Amin et al., 2015; Sanhueza et al., 2017).
Challenges and Perspectives in Using Flavonoids as Antimicrobials
Low solubility, poor permeability, relative chemical instability, rapid release, and susceptibility to environmental influences, but mainly low bioavailability, contribute to the fact that the in vivo exposure levels of flavonoids are usually inconsistent and much below the effective concentrations observed in the in vitro studies. Most flavonoids undergo sulfation, methylation, and glucuronidation in the small intestine and liver due to phase 2 metabolism reactions, resulting in more hydrophilic conjugated metabolites, which show reduced bioactivity compared to parent compounds (D’Archivio et al., 2010; Thilakarathna and Rupasinghe, 2013; Hu et al., 2017; Yang et al., 2020).
In recent years, many advanced nanoparticles have been developed not only to improve polyphenol bioavailability but also to control/target their release. Liposomes, phospholipid complexes, niosomes, protein-based nanoparticles, micelles, emulsions, and metal nanoparticles have been demonstrated to significantly increase bioavailability and improve the pharmacokinetics of polyphenols, becoming promising options for flavonoid delivery systems (Chen et al., 2020; Riaz et al., 2020; Yang et al., 2020). Another approach to improving the bioavailability of flavonoids is the rational modification of their molecular structures to bypass phase 2 metabolism during absorption. Some chemical modifications of bioactive molecules generate inactive forms, known as prodrugs, which can usually be transformed into their active forms by a single-step reaction after ingestion. Designing different synthetic prodrugs of polyphenols by capping phenolic hydroxyls with different protecting groups could increase bioavailability and reinforce the therapeutic properties of these bioactive compounds (Biasutto and Zoratti, 2014; Biasutto et al., 2017). Finally, phyto-phospholipid complexes have emerged as a promising strategy for enhancing the bioavailability of bioactive polyphenols. Phytosomes are obtained by complexing phytochemicals with phospholipids at defined molar ratios and under certain conditions. The resulting complexes are more readily absorbed and exhibit higher bioavailability than free bioactive compounds (Lu et al., 2019; Riva et al., 2019).
Discussion
Antibiotic resistance is among the greatest threats to global health in this century. An impressive accumulation of antibiotic resistance genes by clinically relevant bacterial pathogens, jointly with the present slowdown in developing new antibiotics, is inducing untreatable infections worldwide. H. pylori is a carcinogenic bacterium that infects over half of the global population, causing chronic progressive gastric inflammation and various diseases, including gastric and duodenal ulcers and gastric cancer. This malignancy constitutes the fifth most common cancer and the third leading cause of cancer-related mortality globally, representing 9% of all cancer-related deaths worldwide. Although the eradication of H. pylori infection has been proven to significantly reduce gastric cancer incidence, the efficacy of current eradication therapies has dramatically decreased, mainly because of an increasing development of antibiotic resistance. In this context, different R&D strategies must be urgently considered to fast-track novel, effective therapeutic options against H. pylori infection. Hence, validating novel therapeutic targets, repurposing the existing drugs, using synergistic combinatory therapies, and properly exploiting the proven therapeutic potential of medicinal plants and other natural products could accelerate the delivery of new antimicrobials and the design of novel and personalized treatments against H. pylori refractory infections.
Since most of the currently prescribed antibiotics have been obtained from microbial sources or derivatives thereof, using bioactive phytochemicals to develop new antibiotics could overcome the circulating resistome and slowdown the emergence and dissemination of novel antibiotic resistance mechanisms. Among these naturally occurring substances, flavonoids stand out for their multiple and remarkable beneficial effects on human health. Several flavonoids have revealed potent antimicrobial activities against H. pylori, in some cases, at the level achieved by first-line antibiotics, such as metronidazole. In addition, some of these polyphenolic molecules exhibited synergistic effects combined with conventional antibiotics, thereby reverting antibiotic resistant phenotypes. Furthermore, the antivirulence actions of these compounds against H. pylori contribute to protecting against gastric inflammation, vacuolation, apoptosis, and lipid peroxidation, reducing the damage exerted by the pathogen to the host cells, and decreasing the progression of associated diseases. Although low bioavailability contributes to decreasing the in vivo effectivity of natural flavonoids, the current development of novel delivery systems, such as prodrugs, phytosomes, and several nanotechnology approaches, enables the inclusion of flavonoids as novel therapeutic tools against H. pylori infection.
Author Contributions
AG, JC, and ÁL wrote the review. All authors contributed to the article and approved the submitted version.
Funding
This work has been supported by the Government of Aragon, Spain (B25_17R) and University of Zaragoza (2018/0420).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Amin M. U., Khurram M., Khattak B., Khan J. (2015). Antibiotic Additive and Synergistic Action of Rutin, Morin and Quercetin Against Methicillin Resistant Staphylococcus aureus . BMC Complement Altern. Med. 15, 59. 10.1186/s12906-015-0580-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand U., Jacobo-Herrera N., Altemimi A., Lakhssassi N. (2019). A Comprehensive Review on Medicinal Plants as Antimicrobial Therapeutics: Potential Avenues of Biocompatible Drug Discovery. Metabolites 9 (11), 258. 10.3390/metabo9110258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankolekar C., Johnson D., Pinto Mda S., Johnson K., Labbe R., Shetty K. (2011). Inhibitory Potential of Tea Polyphenolics and Influence of Extraction Time Against Helicobacter pylori and Lack of Inhibition of Beneficial Lactic Acid Bacteria. J. Med. Food 14 (11), 1321–1329. 10.1089/jmf.2010.0237 [DOI] [PubMed] [Google Scholar]
- Ansari S., Yamaoka Y. (2020). Helicobacter pylori Virulence Factor Cytotoxin-Associated Gene A (CagA)-Mediated Gastric Pathogenicity. Int. J. Mol. Sci. 21 (19), 7430. 10.3390/ijms21197430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backert S., Haas R., Gerhard M., Naumann M. (2017). The Helicobacter pylori Type IV Secretion System Encoded by the Cag Pathogenicity Island: Architecture, Function, and Signaling. Curr. Top. Microbiol. Immunol. 413, 187–220. 10.1007/978-3-319-75241-9_8 [DOI] [PubMed] [Google Scholar]
- Baker D. A. (2020). Plants Against Helicobacter pylori to Combat Resistance: An Ethnopharmacological Review. Biotechnol. Rep. (Amst.) 26, e00470. 10.1016/j.btre.2020.e00470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biasutto L., Mattarei A., Azzolini M., La Spina M., Sassi N., Romio M., et al. (2017). Resveratrol Derivatives as a Pharmacological Tool. Ann. N. Y. Acad. Sci. 1403 (1), 27–37. 10.1111/nyas.13401 [DOI] [PubMed] [Google Scholar]
- Biasutto L., Zoratti M. (2014). Prodrugs of Quercetin and Resveratrol: A Strategy Under Development. Curr. Drug Metab. 15 (1), 77–95. 10.2174/1389200214666131211160005 [DOI] [PubMed] [Google Scholar]
- Bisignano C., Filocamo A., La Camera E., Zummo S., Fera M. T., Mandalari G. (2013). Antibacterial Activities of Almond Skins on cagA-Positive and-Negative Clinical Isolates of Helicobacter pylori . BMC Microbiol. 13, 103. 10.1186/1471-2180-13-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyanova L., Evstatiev I., Yordanov D., Markovska R., Mitov I. (2016). Three Unsuccessful Treatments of Helicobacter pylori Infection by a Highly Virulent Strain With Quadruple Antibiotic Resistance. Folia Microbiol. (Praha) 61 (4), 307–310. 10.1007/s12223-015-0439-2 [DOI] [PubMed] [Google Scholar]
- Boyanova L., Ilieva J., Gergova G., Vladimirov B., Nikolov R., Mitov I. (2015). Honey and Green/Black Tea Consumption may Reduce the Risk of Helicobacter pylori Infection. Diagn. Microbiol. Infect. Dis. 82 (1), 85–86. 10.1016/j.diagmicrobio.2015.03.001 [DOI] [PubMed] [Google Scholar]
- Brown J. C., Jiang X. (2013). Activities of Muscadine Grape Skin and Polyphenolic Constituents Against Helicobacter pylori . J. Appl. Microbiol. 114 (4), 982–991. 10.1111/jam.12129 [DOI] [PubMed] [Google Scholar]
- Brown J. C., Wang J., Kasman L., Jiang X., Haley-Zitlin V. (2011). Activities of Muscadine Grape Skin and Quercetin Against Helicobacter pylori Infection in Mice. J. Appl. Microbiol. 110 (1), 139–146. 10.1111/j.1365-2672.2010.04870.x [DOI] [PubMed] [Google Scholar]
- Buer C. S., Imin N., Djordjevic M. A. (2010). Flavonoids: New Roles for Old Molecules. J. Integr. Plant Biol. 52 (1), 98–111. 10.1111/j.1744-7909.2010.00905.x [DOI] [PubMed] [Google Scholar]
- Cheesman M. J., Ilanko A., Blonk B., Cock I. E. (2017). Developing New Antimicrobial Therapies: Are Synergistic Combinations of Plant Extracts/Compounds With Conventional Antibiotics the Solution? Pharmacogn. Rev. 11 (22), 57–72. 10.4103/phrev.phrev_21_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K. T. J., Anantha M., Leung A. W. Y., Kulkarni J. A., Militao G. G. C., Wehbe M., et al. (2020). Characterization of a Liposomal Copper(II)-Quercetin Formulation Suitable for Parenteral Use. Drug Delivery Transl. Res. 10 (1), 202–215. 10.1007/s13346-019-00674-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M. E., Su C. H., Yang J. S., Lu C. C., Hou Y. C., Wu J. B., et al. (2018). Baicalin, Baicalein, and Lactobacillus Rhamnosus JB3 Alleviated Helicobacter pylori Infections In Vitro and In Vivo . J. Food Sci. 83 (12), 3118–3125. 10.1111/1750-3841.14372 [DOI] [PubMed] [Google Scholar]
- Chledzik S., Strawa J., Matuszek K., Nazaruk J. (2018). Pharmacological Effects of Scutellarin, an Active Component of Genus Scutellaria and Erigeron: A Systematic Review. Am. J. Chin. Med. 46 (2), 319–337. 10.1142/S0192415X18500167 [DOI] [PubMed] [Google Scholar]
- Chung J. G., Hsia T. C., Kuo H. M., Li Y. C., Lee Y. M., Lin S. S., et al. (2001). Inhibitory Actions of Luteolin on the Growth and Arylamine N-Acetyltransferase Activity in Strains of Helicobacter pylori From Ulcer Patients. Toxicol. In Vitro 15 (3), 191–198. 10.1016/S0887-2333(01)00015-7 [DOI] [PubMed] [Google Scholar]
- Cushnie T. P., Lamb A. J. (2005). Antimicrobial Activity of Flavonoids. Int. J. Antimicrob. Agents 26 (5), 343–356. 10.1016/j.ijantimicag.2005.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Archivio M., Filesi C., Vari R., Scazzocchio B., Masella R. (2010). Bioavailability of the Polyphenols: Status and Controversies. Int. J. Mol. Sci. 11 (4), 1321–1342. 10.3390/ijms11041321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Valle J. C., Buide M. L., Whittall J. B., Valladares F., Narbona E. (2020). UV Radiation Increases Phenolic Compound Protection But Decreases Reproduction in Silene littorea . PloS One 15 (6), e0231611. 10.1371/journal.pone.0231611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallone C. A., Chiba N., van Zanten S. V., Fischbach L., Gisbert J. P., Hunt R. H., et al. (2016). The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology 151 (1), 51–69.e14. 10.1053/j.gastro.2016.04.006 [DOI] [PubMed] [Google Scholar]
- Farhadi F., Khameneh B., Iranshahi M., Iranshahy M. (2019). Antibacterial Activity of Flavonoids and Their Structure-Activity Relationship: An Update Review. Phytother. Res. 33 (1), 13–40. 10.1002/ptr.6208 [DOI] [PubMed] [Google Scholar]
- Fong P., Hao C. H., Io C. C., Sin P. I., Meng L. R. (2019). In Silico and In Vitro Anti-Helicobacter pylori Effects of Combinations of Phytochemicals and Antibiotics. Molecules 24 (19), 3608. 10.3390/molecules24193608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Chang E., Uribe-Estanislao G. V., Martinez-Martinez M., Galvez-Mariscal A., Romero I. (2018). Anti-Helicobacter pylori Potential of Three Edible Plants Known as Quelites in Mexico. J. Med. Food 21 (11), 1150–1157. 10.1089/jmf.2017.0137 [DOI] [PubMed] [Google Scholar]
- González A., Salillas S., Velázquez-Campoy A., Espinosa Angarica V., Fillat M. F., Sancho J., et al. (2019). Identifying Potential Novel Drugs Against Helicobacter pylori by Targeting the Essential Response Regulator HsrA. Sci. Rep. 9 (1), 11294. 10.1038/s41598-019-47746-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Segovia R., Quintanar J. L., Salinas E., Ceballos-Salazar R., Aviles-Jimenez F., Torres-Lopez J. (2008). Effect of the Flavonoid Quercetin on Inflammation and Lipid Peroxidation Induced by Helicobacter pylori in Gastric Mucosa of Guinea Pig. J. Gastroenterol. 43 (6), 441–447. 10.1007/s00535-008-2184-7 [DOI] [PubMed] [Google Scholar]
- Górniak I., Bartoszewski R., Króliczewski J. (2019). Comprehensive Review of Antimicrobial Activities of Plant Flavonoids. Phytochem. Rev. 18 (1), 241–272. 10.1007/s11101-018-9591-z [DOI] [Google Scholar]
- Haghi A., Azimi H., Rahimi R. (2017). A Comprehensive Review on Pharmacotherapeutics of Three Phytochemicals, Curcumin, Quercetin, and Allicin, in the Treatment of Gastric Cancer. J. Gastrointest. Cancer 48 (4), 314–320. 10.1007/s12029-017-9997-7 [DOI] [PubMed] [Google Scholar]
- Hisatsune J., Nakayama M., Isomoto H., Kurazono H., Mukaida N., Mukhopadhyay A. K., et al. (2008). Molecular Characterization of Helicobacter pylori VacA Induction of IL-8 in U937 Cells Reveals a Prominent Role for p38MAPK in Activating Transcription Factor-2, cAMP Response Element Binding Protein, and NF-kappaB Activation. J. Immunol. 180 (7), 5017–5027. 10.4049/jimmunol.180.7.5017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooi J. K. Y., Lai W. Y., Ng W. K., Suen M. M. Y., Underwood F. E., Tanyingoh D., et al. (2017). Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 153 (2), 420–429. 10.1053/j.gastro.2017.04.022 [DOI] [PubMed] [Google Scholar]
- Hribova P., Khazneh E., Zemlicka M., Svajdlenka E., Ghoneim M. M., Elokely K. M., et al. (2014). Antiurease Activity of Plants Growing in the Czech Republic. Nat. Prod. Res. 28 (12), 868–873. 10.1080/14786419.2014.888553 [DOI] [PubMed] [Google Scholar]
- Huang Y. Q., Huang G. R., Wu M. H., Tang H. Y., Huang Z. S., Zhou X. H., et al. (2015). Inhibitory Effects of Emodin, Baicalin, Schizandrin and Berberine on hefA Gene: Treatment of Helicobacter pylori-Induced Multidrug Resistance. World J. Gastroenterol. 21 (14), 4225–4231. 10.3748/wjg.v21.i14.4225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu M., Wu B., Liu Z. (2017). Bioavailability of Polyphenols and Flavonoids in the Era of Precision Medicine. Mol. Pharm. 14 (9), 2861–2863. 10.1021/acs.molpharmaceut.7b00545 [DOI] [PubMed] [Google Scholar]
- Isobe T., Doe M., Morimoto Y., Nagata K., Ohsaki A. (2006). The Anti-Helicobacter pylori Flavones in a Brazilian Plant, Hyptis Fasciculata, and the Activity of Methoxyflavones. Biol. Pharm. Bull. 29 (5), 1039–1041. 10.1248/bpb.29.1039 [DOI] [PubMed] [Google Scholar]
- Kataria R., Khatkar A. (2019. a). In-Silico Designing, ADMET Analysis, Synthesis and Biological Evaluation of Novel Derivatives of Diosmin Against Urease Protein and Helicobacter pylori Bacterium. Curr. Top. Med. Chem. 19 (29), 2658–2675. 10.2174/1568026619666191114123452 [DOI] [PubMed] [Google Scholar]
- Kataria R., Khatkar A. (2019. b). Molecular Docking, Synthesis, Kinetics Study, Structure-Activity Relationship and ADMET Analysis of Morin Analogous as Helicobacter pylori Urease Inhibitors. BMC Chem. 13 (1), 45. 10.1186/s13065-019-0562-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. H., Lee M. H., Park M., Woo H. J., Kim Y. S., Tharmalingam N., et al. (2018). Regulatory Effects of Black Rice Extract on Helicobacter pylori Infection-Induced Apoptosis. Mol. Nutr. Food Res. 62 (3), 1700586. 10.1002/mnfr.201700586 [DOI] [PubMed] [Google Scholar]
- Kim S. H., Park M., Woo H., Tharmalingam N., Lee G., Rhee K. J., et al. (2012). Inhibitory Effects of Anthocyanins on Secretion of Helicobacter pylori CagA and VacA Toxins. Int. J. Med. Sci. 9 (10), 838–842. 10.7150/ijms.5094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. H., Woo H., Park M., Rhee K. J., Moon C., Lee D., et al. (2014). Cyanidin 3-O-Glucoside Reduces Helicobacter pylori VacA-Induced Cell Death of Gastric KATO III Cells Through Inhibition of the SecA Pathway. Int. J. Med. Sci. 11 (7), 742–747. 10.7150/ijms.7167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzyzek P., Migdal P., Paluch E., Karwanska M., Wieliczko A., Gosciniak G. (2021). Myricetin as an Antivirulence Compound Interfering With a Morphological Transformation Into Coccoid Forms and Potentiating Activity of Antibiotics Against Helicobacter pylori . Int. J. Mol. Sci. 22 (5), 2695. 10.3390/ijms22052695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Pandey A. K. (2013). Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013:162750. 10.1155/2013/162750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo C. H., Weng B. C., Wu C. C., Yang S. F., Wu D. C., Wang Y. C. (2014). Apigenin has Anti-Atrophic Gastritis and Anti-Gastric Cancer Progression Effects in Helicobacter pylori-Infected Mongolian Gerbils. J. Ethnopharmacol. 151 (3), 1031–1039. 10.1016/j.jep.2013.11.040 [DOI] [PubMed] [Google Scholar]
- Kusters J. G., van Vliet A. H., Kuipers E. J. (2006). Pathogenesis of Helicobacter pylori Infection. Clin. Microbiol. Rev. 19 (3), 449–490. 10.1128/CMR.00054-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb A., Chen L. F. (2013). Role of the Helicobacter pylori-Induced Inflammatory Response in the Development of Gastric Cancer. J. Cell Biochem. 114 (3), 491–497. 10.1002/jcb.24389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H. M., Hong E., Jeon B. Y., Kim D. U., Byun J. S., Lee W., et al. (2006). Crystallization and Preliminary X-Ray Crystallographic Study of HP1043, a Helicobacter pylori Orphan Response Regulator. Biochim. Biophys. Acta 1764 (5), 989–991. 10.1016/j.bbapap.2005.10.024 [DOI] [PubMed] [Google Scholar]
- Lee Y. S., Huh J. Y., Nam S. H., Moon S. K., Lee S. B. (2012). Enzymatic Bioconversion of Citrus Hesperidin by Aspergillus Sojae Naringinase: Enhanced Solubility of Hesperetin-7-O-Glucoside With In Vitro Inhibition of Human Intestinal Maltase, HMG-CoA Reductase, and Growth of Helicobacter pylori . Food Chem. 135 (4), 2253–2259. 10.1016/j.foodchem.2012.07.007 [DOI] [PubMed] [Google Scholar]
- Liu Z. Q., Zheng P. Y., Yang P. C. (2008). Efflux Pump Gene hefA of Helicobacter pylori Plays an Important Role in Multidrug Resistance. World J. Gastroenterol. 14 (33), 5217–5222. 10.3748/wjg.14.5217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo V. G., Fallone C. A., De Souza E., Lavallee J., Barkun A. N. (1997). In-Vitro Susceptibility of Helicobacter pylori to Ampicillin, Clarithromycin, Metronidazole and Omeprazole. J. Antimicrob. Chemother. 40 (6), 881–883. 10.1093/jac/40.6.881 [DOI] [PubMed] [Google Scholar]
- Lu M., Qiu Q., Luo X., Liu X., Sun J., Wang C., et al. (2019). Phyto-Phospholipid Complexes (Phytosomes): A Novel Strategy to Improve the Bioavailability of Active Constituents. Asian J. Pharm. Sci. 14 (3), 265–274. 10.1016/j.ajps.2018.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macomber L., Minkara M. S., Hausinger R. P., Merz K. M., Jr. (2015). Reduction of Urease Activity by Interaction With the Flap Covering the Active Site. J. Chem. Inf. Model 55 (2), 354–361. 10.1021/ci500562t [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall B. J., Warren J. R. (1984). Unidentified Curved Bacilli in the Stomach of Patients With Gastritis and Peptic Ulceration. Lancet 1 (8390), 1311–1315. 10.1016/s0140-6736(84)91816-6 [DOI] [PubMed] [Google Scholar]
- Martini S., D’Addario C., Colacevich A., Focardi S., Borghini F., Santucci A., et al. (2009). Antimicrobial Activity Against Helicobacter pylori Strains and Antioxidant Properties of Blackberry Leaves (Rubus ulmifolius) and Isolated Compounds. Int. J. Antimicrob. Agents 34 (1), 50–59. 10.1016/j.ijantimicag.2009.01.010 [DOI] [PubMed] [Google Scholar]
- Matsumoto T., Takahashi T., Yamada H. (2008). A Novel Approach for Screening of New Anti-Helicobacter pylori Substances. Biol. Pharm. Bull. 31 (1), 143–145. 10.1248/bpb.31.143 [DOI] [PubMed] [Google Scholar]
- Mendonca M. A. A., Ribeiro A. R. S., Lima A. K., Bezerra G. B., Pinheiro M. S., Albuquerque-Junior R. L. C., et al. (2020). Red Propolis and its Dyslipidemic Regulator Formononetin: Evaluation of Antioxidant Activity and Gastroprotective Effects in Rat Model of Gastric Ulcer. Nutrients 12 (10), 2951. 10.3390/nu12102951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mierziak J., Kostyn K., Kulma A. (2014). Flavonoids as Important Molecules of Plant Interactions With the Environment. Molecules 19 (10), 16240–16265. 10.3390/molecules191016240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon S. H., Lee J. H., Kim K. T., Park Y. S., Nah S. Y., Ahn D. U., et al. (2013). Antimicrobial Effect of 7-O-Butylnaringenin, a Novel Flavonoid, and Various Natural Flavonoids Against Helicobacter pylori Strains. Int. J. Environ. Res. Public Health 10 (11), 5459–5469. 10.3390/ijerph10115459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa H., Takaishi Y., Tanaka N., Tsuchiya K., Shibata H., Higuti T. (2006). Chemical Constituents From the Peels of Citrus sudachi . J. Nat. Prod. 69 (8), 1177–1179. 10.1021/np060217s [DOI] [PubMed] [Google Scholar]
- Ndemangou B., Sielinou V. T., Vardamides J. C., Ali M. S., Lateef M., Iqbal L., et al. (2013). Urease Inhibitory Isoflavonoids From Different Parts of Calopogonium Mucunoides (Fabaceae). J. Enzyme Inhib. Med. Chem. 28 (6), 1156–1161. 10.3109/14756366.2012.719025 [DOI] [PubMed] [Google Scholar]
- Njume C., Jide A. A., Ndip R. N. (2011). Aqueous and Organic Solvent-Extracts of Selected South African Medicinal Plants Possess Antimicrobial Activity Against Drug-Resistant Strains of Helicobacter pylori: Inhibitory and Bactericidal Potential. Int. J. Mol. Sci. 12 (9), 5652–5665. 10.3390/ijms12095652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olekhnovich I. N., Vitko S., Chertihin O., Hontecillas R., Viladomiu M., Bassaganya-Riera J., et al. (2013). Mutations to Essential Orphan Response Regulator HP1043 of Helicobacter pylori Result in Growth-Stage Regulatory Defects. Infect. Immun. 81 (5), 1439–1449. 10.1128/IAI.01193-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olekhnovich I. N., Vitko S., Valliere M., Hoffman P. S. (2014). Response to Metronidazole and Oxidative Stress Is Mediated Through Homeostatic Regulator HsrA (HP1043) in Helicobacter pylori . J. Bacteriol. 196 (4), 729–739. 10.1128/JB.01047-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang Y., Li L., Ling P. (2020). Nobiletin Inhibits Helicobacterium Pylori Infection-Induced Gastric Carcinogenic Signaling by Blocking Inflammation, Apoptosis, and Mitogen-Activated Protein Kinase Events in Gastric Epithelial-1 Cells. J. Environ. Pathol. Toxicol. Oncol. 39 (1), 77–88. 10.1615/JEnvironPatholToxicolOncol.2020031272 [DOI] [PubMed] [Google Scholar]
- Palframan S. L., Kwok T., Gabriel K. (2012). Vacuolating Cytotoxin A (VacA), a Key Toxin for Helicobacter pylori Pathogenesis. Front. Cell Infect. Microbiol. 2, 92. 10.3389/fcimb.2012.00092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastene E., Parada V., Avello M., Ruiz A., Garcia A. (2014). Catechin-Based Procyanidins From Peumus boldus Mol. Aqueous Extract Inhibit Helicobacter pylori Urease and Adherence to Adenocarcinoma Gastric Cells. Phytother. Res. 28 (11), 1637–1645. 10.1002/ptr.5176 [DOI] [PubMed] [Google Scholar]
- Pelliciari S., Pinatel E., Vannini A., Peano C., Puccio S., De Bellis G., et al. (2017). Insight Into the Essential Role of the Helicobacter pylori HP1043 Orphan Response Regulator: Genome-Wide Identification and Characterization of the DNA-Binding Sites. Sci. Rep. 7, 41063. 10.1038/srep41063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajesh K. P., Manjunatha H., Bharath B. R. (2013). Simulated Screening of Flavonoids as Probable Anti-Helicobacter pylori Drug. Med. Chem. Res. 22, 4537–4546. 10.1007/s00044-012-0426-y [DOI] [Google Scholar]
- Riaz S., Fatima Rana N., Hussain I., Tanweer T., Nawaz A., Menaa F., et al. (2020). Effect of Flavonoid-Coated Gold Nanoparticles on Bacterial Colonization in Mice Organs. Nanomaterials (Basel) 10 (9), 1769. 10.3390/nano10091769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva A., Ronchi M., Petrangolini G., Bosisio S., Allegrini P. (2019). Improved Oral Absorption of Quercetin From Quercetin Phytosome™, a New Delivery System Based on Food Grade Lecithin. Eur. J. Drug Metab. Pharmacokinet. 44 (2), 169–177. 10.1007/s13318-018-0517-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi B., Sharopov F., Martorell M., Rajkovic J., Ademiluyi A. O., Sharifi-Rad M., et al. (2018). Phytochemicals in Helicobacter pylori Infections: What Are We Doing Now? Int. J. Mol. Sci. 19 (8), 2361. 10.3390/ijms19082361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanhueza L., Melo R., Montero R., Maisey K., Mendoza L., Wilkens M. (2017). Synergistic Interactions Between Phenolic Compounds Identified in Grape Pomace Extract With Antibiotics of Different Classes Against Staphylococcus Aureus and Escherichia Coli . PloS One 12 (2), e0172273. 10.1371/journal.pone.0172273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. E., Kim J. M., Bae E. A., Hyun Y. J., Kim D. H. (2005). In Vitro Inhibitory Effect of Flavonoids on Growth, Infection and Vacuolation of Helicobacter pylori . Planta Med. 71 (3), 197–201. 10.1055/s-2005-837816 [DOI] [PubMed] [Google Scholar]
- Silvan J. M., Gutierrez-Docio A., Moreno-Fernandez S., Alarcon-Cavero T., Prodanov M., Martinez-Rodriguez A. J. (2020). Procyanidin-Rich Extract From Grape Seeds as a Putative Tool Against Helicobacter pylori . Foods 9 (10), 1370. 10.3390/foods9101370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siriviriyakul P., Werawatganon D., Phetnoo N., Somanawat K., Chatsuwan T., Klaikeaw N., et al. (2020). Genistein Attenuated Gastric Inflammation and Apoptosis in Helicobacter pylori-Induced Gastropathy in Rats. BMC Gastroenterol. 20 (1), 410. 10.1186/s12876-020-01555-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skiba M. A., Szendzielorz K., Mazur B., Krol W. (2016). The Inhibitory Effect of Flavonoids on Interleukin-8 Release by Human Gastric Adenocarcinoma (AGS) Cells Infected With cag PAI (+) Helicobacter pylori . Cent. Eur. J. Immunol. 41 (3), 229–235. 10.5114/ceji.2016.63119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stompor M. (2020). A Review on Sources and Pharmacological Aspects of Sakuranetin. Nutrients 12 (2), 513. 10.3390/nu12020513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D. L., et al. (2018). Discovery, Research, and Development of New Antibiotics: The WHO Priority List of Antibiotic-Resistant Bacteria and Tuberculosis. Lancet Infect. Dis. 18 (3), 318–327. 10.1016/S1473-3099(17)30753-3 [DOI] [PubMed] [Google Scholar]
- Takeuchi H., Trang V. T., Morimoto N., Nishida Y., Matsumura Y., Sugiura T. (2014). Natural Products and Food Components With Anti-Helicobacter pylori Activities. World J. Gastroenterol. 20 (27), 8971–8978. 10.3748/wjg.v20.i27.8971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarahovsky Y. S., Kim Y. A., Yagolnik E. A., Muzafarov E. N. (2014). Flavonoid-Membrane Interactions: Involvement of Flavonoid-Metal Complexes in Raft Signaling. Biochim. Biophys. Acta 1838 (5), 1235–1246. 10.1016/j.bbamem.2014.01.021 [DOI] [PubMed] [Google Scholar]
- The European Committee on Antimicrobial Susceptibility Testing . (2020). Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 10.0. Available at: http://www.eucast.org.
- Thilakarathna S. H., Rupasinghe H. P. (2013). Flavonoid Bioavailability and Attempts for Bioavailability Enhancement. Nutrients 5 (9), 3367–3387. 10.3390/nu5093367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran Trung H., Truong Thi Huynh H., Nguyen Thi Thuy L., Nguyen Van Minh H., Thi Nguyen M. N., Luong Thi M. N. (2020). Growth-Inhibiting, Bactericidal, Antibiofilm, and Urease Inhibitory Activities of Hibiscus rosa sinensis L. Flower Constituents Toward Antibiotic Sensitive- and Resistant-Strains of Helicobacter pylori . ACS Omega 5 (32), 20080–20089. 10.1021/acsomega.0c01640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuchiya H., Iinuma M. (2000). Reduction of Membrane Fluidity by Antibacterial Sophoraflavanone G Isolated From Sophora exigua . Phytomedicine 7 (2), 161–165. 10.1016/S0944-7113(00)80089-6 [DOI] [PubMed] [Google Scholar]
- Ustun O., Ozcelik B., Akyon Y., Abbasoglu U., Yesilada E. (2006). Flavonoids With Anti-Helicobacter pylori Activity From Cistus laurifolius Leaves. J. Ethnopharmacol. 108 (3), 457–461. 10.1016/j.jep.2006.06.001 [DOI] [PubMed] [Google Scholar]
- Wang Y. C. (2014). Medicinal Plant Activity on Helicobacter pylori Related Diseases. World J. Gastroenterol. 20 (30), 10368–10382. 10.3748/wjg.v20.i30.10368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. C., Huang K. M. (2013). In Vitro Anti-Inflammatory Effect of Apigenin in the Helicobacter pylori-Infected Gastric Adenocarcinoma Cells. Food Chem. Toxicol. 53, 376–383. 10.1016/j.fct.2012.12.018 [DOI] [PubMed] [Google Scholar]
- Wang T., Li Q., Bi K. (2018). Bioactive Flavonoids in Medicinal Plants: Structure, Activity and Biological Fate. Asian J. Pharm. Sci. 13 (1), 12–23. 10.1016/j.ajps.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White R. L., Burgess D. S., Manduru M., Bosso J. A. (1996). Comparison of Three Different In Vitro Methods of Detecting Synergy: Time-Kill, Checkerboard, and E Test. Antimicrob. Agents Chemother. 40 (8), 1914–1918. 10.1128/AAC.40.8.1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittschier N., Lengsfeld C., Vorthems S., Stratmann U., Ernst J. F., Verspohl E. J., et al. (2007). Large Molecules as Anti-Adhesive Compounds Against Pathogens. J. Pharm. Pharmacol. 59 (6), 777–786. 10.1211/jpp.59.6.0004 [DOI] [PubMed] [Google Scholar]
- Wu J., Hu D., Wang K. X. (2008). Study of Scutellaria baicalensis and Baicalin Against Antimicrobial Susceptibility of Helicobacter pylori Strains In Vitro . Zhong Yao Cai 31 (5), 707–710. [PubMed] [Google Scholar]
- Wu D., Kong Y., Han C., Chen J., Hu L., Jiang H., et al. (2008). D-Alanine:D-Alanine Ligase as a New Target for the Flavonoids Quercetin and Apigenin. Int. J. Antimicrob. Agents 32 (5), 421–426. 10.1016/j.ijantimicag.2008.06.010 [DOI] [PubMed] [Google Scholar]
- Xiao Z. P., Wang X. D., Peng Z. Y., Huang S., Yang P., Li Q. S., et al. (2012). Molecular Docking, Kinetics Study, and Structure-Activity Relationship Analysis of Quercetin and Its Analogous as Helicobacter pylori Urease Inhibitors. J. Agric. Food Chem. 60 (42), 10572–10577. 10.1021/jf303393n [DOI] [PubMed] [Google Scholar]
- Yamaoka Y. (2010). Mechanisms of Disease: Helicobacter pylori Virulence Factors. Nat. Rev. Gastroenterol. Hepatol. 7 (11), 629–641. 10.1038/nrgastro.2010.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang B., Dong Y., Wang F., Zhang Y. (2020). Nanoformulations to Enhance the Bioavailability and Physiological Functions of Polyphenols. Molecules 25 (20), 4613. 10.3390/molecules25204613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeon M. J., Lee M. H., Kim D. H., Yang J. Y., Woo H. J., Kwon H. J., et al. (2019). Anti-Inflammatory Effects of Kaempferol on Helicobacter pylori-Induced Inflammation. Biosci. Biotechnol. Biochem. 83 (1), 166–173. 10.1080/09168451.2018.1528140 [DOI] [PubMed] [Google Scholar]
- Yesilada E., Gurbuz I., Ergun E. (1997). Effects of Cistus Laurifolius L. Flowers on Gastric and Duodenal Lesions. J. Ethnopharmacol. 55 (3), 201–211. 10.1016/s0378-8741(96)01502-4 [DOI] [PubMed] [Google Scholar]
- Yuan L., Li X., He S., Gao C., Wang C., Shao Y. (2018). Effects of Natural Flavonoid Isoorientin on Growth Performance and Gut Microbiota of Mice. J. Agric. Food Chem. 66 (37), 9777–9784. 10.1021/acs.jafc.8b03568 [DOI] [PubMed] [Google Scholar]
- Yu X. D., Zheng R. B., Xie J. H., Su J. Y., Huang X. Q., Wang Y. H., et al. (2015). Biological Evaluation and Molecular Docking of Baicalin and Scutellarin as Helicobacter pylori Urease Inhibitors. J. Ethnopharmacol. 162, 69–78. 10.1016/j.jep.2014.12.041 [DOI] [PubMed] [Google Scholar]
- Zhang S., Huang J., Xie X., He Y., Mo F., Luo Z. (2017). Quercetin From Polygonum capitatum Protects Against Gastric Inflammation and Apoptosis Associated With Helicobacter pylori Infection by Affecting the Levels of P38mapk, BCL-2 and BAX. Molecules 22 (5), 744. 10.3390/molecules22050744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Kong Y., Wu D., Zhang H., Wu J., Chen J., et al. (2008). Three Flavonoids Targeting the Beta-Hydroxyacyl-Acyl Carrier Protein Dehydratase From Helicobacter pylori: Crystal Structure Characterization With Enzymatic Inhibition Assay. Protein Sci. 17 (11), 1971–1978. 10.1110/ps.036186.108 [DOI] [PMC free article] [PubMed] [Google Scholar]


