Abstract
目的
探讨冠状动脉计算机断层扫描造影(CCTA)指标与冠周脂肪CT衰减指数(FAI)在预测冠脉血流动力学异常方面的联合价值。
方法
回顾性纳入2017~2019年于解放军总医院接受CCTA检查,并于1月内行有创血流储备分数(FFR)检查的患者。从血管水平检测CCTA指标,包括斑块分布、冠脉血管钙化积分、病变长度、最大直径狭窄率、最大面积狭窄率(MAS)、总斑块负荷,并测量冠周FAI和基于机器学习的CT-FFR。有创FFR≤0.8被认为存在病变特异性的血流动力学异常。
结果
回顾性入组99例患者,共计血管124支。从血管水平,FFR≤0.8组的冠脉血管钙化积分,最大直径狭窄率、MAS和总斑块负荷均显著高于FFR>0.8组,冠周FAI(P < 0.01)和CT-FFR(P < 0.01)差异也存在统计学意义。诊断试验显示,MAS联合冠周FAI的AUC达到0.818,与CT-FFR相比差异无统计学意义(P=0.076)。
结论
MAS与冠周FAI联合应用对鉴别血流动力学意义的冠脉狭窄具有较高的诊断价值,与CT-FFR技术相类似。
Keywords: 冠状动脉最大面积狭窄率, CT造影, 血流储备分数, 脂肪组织, 脂肪CT衰减指数
Abstract
Objective
To investigate the combined value of coronary computed tomography angiography (CCTA) indicators and perivascular fat attenuation index (FAI) in predicting hemodynamically significant coronary artery disease.
Methods
We retrospectively analyzed the data of patients undergoing CCTA in Chinese PLA General Hospital from 2017 to 2019, who were also examined for fractional flow reserve (FFR) with invasive coronary angiography within one month before inclusion. The CCTA indicators at the vascular level were measured, including plaque distribution, coronary artery calcification score, lesion length, maximum diameter stenosis, maximum area stenosis (MAS), total plaque burden (TPB), perivascular FAI, and CT-FFR based on machine learning. Lesion-specific hemodynamically significant coronary artery disease was diagnosed for an invasive FFR≤0.8.
Results
A total of 99 patients with 124 involved coronary arteries were included in this analysis. At the vascular level, according to the results of invasive FFR, coronary artery calcification score, maximum diameter stenosis, MAS and the total plaque burden were significantly higher in patents with a FFR≤0.8 than in those with a FFR>0.8; the perivascular FAI (P < 0.01) and CT-FFR (P < 0.01) also differed significantly between the two groups. The AUC of MAS combined with perivascular FAI was 0.818, which was not significantly different from that of CT-FFR (P=0.076).
Conclusion
The combination of MAS and perivascular FAI has good diagnostic performance in predicting hemodynamically significant coronary stenosis, which is comparable with that of CT-FFR.
Keywords: maximum area stenosis, CT angiography, fractional flow reserve, adipose tissue, fat attenuation index
冠心病(CAD)是威胁公众健康的重大慢性疾病,其诊断治疗和预后管理至关重要[1]。冠状动脉CT成像检查(CCTA)作为目前临床上CAD一线检查手段,已经凸显其良好的诊断和预后价值[2-4]。基于CCTA技术发展而来的CT血流储备分数(CT-FFR),可通过模拟有创FFR检查的原理和流程,得到与有创FFR高度一致的结果。CT-FFR检查相较于CCTA,在预测血流动力学异常方面,可以提供更高的诊断价值[5-8]。
近年来,有研究者发现,冠脉周围脂肪组织CT衰减指数(FAI)可以作为一种新颖的无创影像学指标,用以呈现冠周脂肪组织的水相改变和冠状动脉血管的炎症状态[9-11]。通过CCTA检测的升高的冠周FAI,可能与升高的心脏死亡风险和较差的临床预后相关[12]。冠周FAI联合总的斑块负荷、最大直径狭窄率等指标可以预测冠脉狭窄的血流动力学异常,具有较高的诊断准确率[13]。然而,据前期研究发现,在评估血流动力学异常方面,最大面积狭窄率(MAS)的价值要高于最大直径狭窄率(MDS)和总斑块负荷(TPB)[14]。相较MDS,MAS可能为诊断提供更全面的管腔信息。但是,MAS联合冠周FAI能否带来更优的诊断效能尚不清楚。因此,本研究的主要目的是探讨MAS联合冠周FAI对于预测血流动力学异常CAD的价值,并将这种诊断效能与CT-FFR技术进行对比。
1. 资料和方法
1.1. 研究对象
回顾性纳入2017~2019年于解放军总医院行CCTA检查,并于1月内行有创冠脉造影(ICA)检查和有创FFR检查的患者。所有患者均具有胸痛、胸闷等疑似冠心病症状。入组标准:胸痛、胸闷等疑似冠心病症状;CCTA发现主支冠脉狭窄程度在50%以上;ICA和FFR在CCTA后的1月内进行。排除标准:既往的经皮冠状动脉介入术和冠脉旁路移植手术病史;CCTA图像质量影响进一步CT-FFR或者冠脉影像学指标测量;患者同时合并有心肌病、严重的心律失常、瓣膜病等;ICA和FFR在CCTA的1月后实施。回顾性研究无需患者签署知情同意书,该研究获得解放军总医院伦理委员会批准。
1.2. CCTA扫描流程
CCTA图像采用西门子双源螺旋CT机(Somatom Definition Flash, Germany)扫描获取。检查过程中对患者的心律进行实时监控,当心率监测超过70/分时,给予静脉注射50~100 mg艾司洛尔。所有接受检查的患者如无禁忌在检查前均舌下含服硝酸甘油用以扩张冠脉。根据患者的心律情况采用不同的扫描模式,如当患者心率≥70/分时,采用回顾性心电门控扫描获取图像,反之,采用前瞻性心电门控扫描方案。扫描参数如下:准直器2×128×0.6 mm,管电流290~560 mAs,管电压80~120 kV(取决于BMI),旋转时间0.28 s。
1.3. 冠脉影像特征分析
所有扫描数据传输至专用的冠脉影像分析平台(SynoMultiModality Workplace, SyngoMMWPVE40A, Siemens, Germany),进行血管狭窄和斑块特征测量。冠脉病变长度、MDS、MAS和TPB等指标测量的节段取决于FFR检查报告中冠脉病变节段位置。MDS定义为管腔最狭窄处的直径/参考血管直径×100%,MAS定义为管腔最狭窄处的面积/参考血管面积×100%,TPB定义为病变斑块的总体积/病变节段血管总体积× 100%。所有纳入分析的血管均依据Agatston法进行冠脉钙化积分(CACS)测量[15]。
1.4. ICA和FFR检查
ICA采用标准流程经股动脉或者桡动脉入路进行,冠脉狭窄由两名有经验的心内科造影医师判定。FFR检查主要在狭窄程度在30~90%的主支冠脉中实施,测量采用压力导丝(PressureWireCertus, St. Jude Medical)经由6F导管至冠脉中操作测量。冠脉内以140~180 μg/(kg·min)速率给予注射三磷酸腺苷以达到最大充血状态。在注射三磷酸腺苷数值稳定后分别记录病变远端及回撤病变前的记录数值,FFR值定义为冠脉病变远端压力与近端压力之比,FFR≤0.8认为存在病变特异性的血流动力学异常。
1.5. 冠周FAI分析测量
在行有创FFR检查的对应冠脉上,采用专用软件进行冠周FAI的测量(Anythink CT, Coronary Artery Analysis, version 1.01,CREALIFE, China),冠周脂肪组织的分离和冠周FAI测量采用前述方法[9]。冠周脂肪组织定义为离冠状动脉外壁径向距离等于节段直径的一层脂肪组织,其测量长度与冠脉病变长度相一致,左主干部位因长度和脂肪分布变异较大而未进行冠周FAI测量[9]。脂肪的CT值设定为-190~-30 HU,当CT阈值和测量范围参数定义完毕后,后台在图像上自动分割测算。当两名研究者测量数据存在差异时,对测量方法和测量位置进行协商。观察者间和观察者内测量冠周FAI的相关系数较高(Pearson相关系数分别为0.96和0.97)。
1.6. CT-FFR分析测量
在实施有创FFR检查的冠脉对应的CCTA图像中进行CT-FFR的测量,测量的方法和软件主要基于机器学习的无创FFR测量技术(DeepFFR V1.0.0, Beijing CuraCloud Technology Co., Ltd., Beijing, China),测算无创CCTA影像上的模拟FFR值,即CT-FFR。DeepFFR技术机器学习算法模型是基于既往回顾性血流动力学样本数据库建立,其有效性已得到验证。测算过程包括:在该软件平台上,导入CCTA图像上并提取整个冠脉树模型,并采用最小路径法提取确定冠脉中心线和血管边缘,如果与实际不符则需要进行手动校正。将目标冠脉树模型代入神经网络进行深度学习测算,从而可以得到整支冠脉树任意一点的CT-FFR值,病变特异性CT-FFR值的测算位置为目标病变后10~20 mm的距离[16]。
1.7. 统计分析
所有数据的分析均基于血管水平进行。连续变量表示为均数±标准差或中位数(四分位数),组间比较采用Student t检验(正态分布)或Mann-Whitney U检验(非正态分布)。分类变量表示为例数和百分比,组间比较采用卡方检验或Fisher精确概率。为寻找能够预测冠脉血流动力学异常的影像学指标,采用单因素和多因素的logistic回归分析各指标与血流动力学异常的关联。为进一步评估各指标诊断效能,绘制受试者工作特征曲线(ROC)用以描述各指标在诊断预测冠脉血流动力学异常方面的效能,并计算曲线下面积(AUC)和95%置信区间(CI)、诊断的准确率、特异性、敏感性、阳性预测值(PPV)和阴性预测值(NPV)。最佳的截断值通过约登指数获得,即在该截断值的诊断下,该技术具有最大的诊断特异性与敏感性之和。ROC曲线之间的比较采用DeLong等[17]的方法。所有统计学分析采用SPSS(22.0; IBM Corporation, Armonk, NY, USA)和MedCalc(Version 15.2.2; MedCalc Software, Mariakerke, Belgium)完成,统计分析采取双尾,P < 0.05被认为差异有统计学意义。
2. 结果
2.1. 患者和血管纳入情况
经过入选排除,共有126名患者于此时间内进行了CCTA、ICA和FFR检查。其中,19名患者由于FFR与CCTA检查之间间隔超过1月而被排除,8名患者由于行FFR检查的血管对应的CCTA图像质量欠佳,不足以满足CT-FFR和冠周FAI的测量而被排除。最终99名患者的124支冠脉血管纳入进一步分析。患者,年龄61.6±5.5岁,男性占比65.7%。高血压、糖尿病、高脂血症、吸烟等危险因素比例分别为63.6%、34.3%、44.4%和29.3%。血清学相关指标中,总胆固醇为4.2 mmol/L,低密度脂蛋白为2.01 mmol/L。所有患者平均的总CACS为97.0(14.5,151.7)(表 1)。
1.
患者一般资料
General information of the patients
| Characteristics | Value |
| HDL-C:High-density lipoprotein; LDL-C: Low-density lipoprotein; CACS: Coronary artery calcification score. | |
| Patients | 99 |
| Age (years) | 61.6±5.5 |
| Gender (n,%) | 65 (65.7) |
| BMI (kg/m2) | 25.4±3.2 |
| Risk factor | |
| Hypertension | 63 (63.6) |
| Diabetes | 34 (34.3) |
| Hyperlipidemia | 44 (44.4) |
| Current smoking | 29 (29.3) |
| Serum index | |
| Total cholesterol (mmol/L) | 4.2±0.8 |
| Triglyceride (mmol/L) | 0.94 (0.81, 2.52) |
| HDL-C (mmol/L) | 1.1±0.3 |
| LDL-C (mmol/L) | 2.01 (1.60, 3.16) |
| Lipoprotein a (mmol/L) | 15.2(10.0, 37.7) |
| CRP (mg/L) | 0.38±0.28 |
| Homocysteine (μmol/L) | 16.7±7.6 |
| Glucose (mmol/L) | 6.5±2.6 |
| Glycosylated hemoglobin (%) | 5.8 (5.6, 6.3) |
| Total CACS | 97.0(14.5, 151.7) |
2.2. 血管纳入情况
从血管水平,共有89支左前降支(71.8%)、10支回旋支(8.1%)和25支右冠状动脉(20.2%)接受了有创FFR检查。依据血管FFR是否存在血流动力学异常,将纳入的血管分为FFR≤0.8(37例)和FFR>0.8(87例)组。从冠脉影像学特征上进行分析发现,FFR≤0.8组的CACS、MDS、MAS和TPB显著高于FFR>0.8组(P < 0.01)。冠周FAI在FFR≤0.8组要高于FFR>0.8组(P < 0.01),CT-FFR在FFR≤0.8组要低于FFR>0.8组(P < 0.01),而两组间病变长度无显著统计学性差异(P=0.075,表 2)。
2.
血管水平影像学特征
Imaging characteristics at the vascular level
| Characteristics | Overall (n=124) | FFR在0.8(n=37) | FFR > 0.8 (n=87) | P |
| LAD: Left anterior descending; LCX: Left circumflex artery; RCA: Right coronary artery; MDS: Maximum diameter stenosis; MAS: Maximum area stenosis; TPB: Total plaque burden; FAI: Fat attenuation index; CT-FFR: Fractional flow reserve. | ||||
| Lesions distribution (n, %) | ||||
| LAD | 89(71.8) | 32 (86.5) | 57 (65.5) | 0.018 |
| LCX | 10(8.1) | 1 (2.7) | 9 (10.3) | 0.279 |
| RCA | 25 (20.2) | 4 (10.8) | 21 (24.1) | 0.091 |
| CACS/vessel | 43.3 (2.4, 168.2) | 85.8 (6.8, 234.1) | 42.5 (0.6, 110.2) | 0.024 |
| Lesion length (mm) | 24.8±10.7 | 27.8±12.8 | 23.5±9.5 | 0.075 |
| MDS (%) | 59.6±10.0 | 63.8±9.9 | 57.6±9.5 | 0.003 |
| MAS (%) | 67.9±9.5 | 73.3±9.4 | 65.5±8.7 | 0.000 |
| TPB (%) | 54.7±12.3 | 58.2±11.3 | 53.1±12.5 | 0.042 |
| Perivascular FAI(HU) | -78.4±8.8 | -73.3±9.5 | -80.6±7.5 | 0.000 |
| CT-FFR | 0.83±0.06 | 0.77±0.04 | 0.86±0.04 | 0.000 |
| Invasive FFR | 0.83±0.10 | 0.71±0.09 | 0.87±0.04 | 0.000 |
在单因素logistic回归中,对应血管的CACS、MAS、TPB和冠周FAI等指标,与血流动力学异常存在关联;多因素logistic回归显示,MAS(OR: 1.130,1.035~ 1.233,P=0.006)和冠周FAI(OR: 1.152,1.075~1.235,P < 0.01)是血流动力学异常的独立预测因素(表 3)。
3.
单因素和多因素logistic回归分析血流动力学异常的预测因素
Univariate and multivariate logistic regression analysis of the predictors of hemodynamic abnormality
| Indicators | Univariable | Multivariable | |||||
| OR | 95% CI | P | OR | 95% CI | P | ||
| CACS/vessel | 1.003 | 1.001-1.006 | 0.013* | 1.003 | 0.999-1.007 | 0.110 | |
| MAS | 1.1.6 | 1.051-1.163 | 0.000* | 1.130 | 1.063-1.201 | 0.000 | |
| TPB | 1.037 | 1.001-1.074 | 0.045* | 1.040 | 0.990-1.093 | 0.117 | |
| Perivascular FAI | 1.112 | 1.055-1.171 | 0.000* | 1.142 | 1.065-1.226 | 0.000 | |
2.3. 各冠脉斑块影像学指标在血流动力学异常方面的诊断效能
CT-FFR具有最高的诊断效能,AUC达到0.909(0.844~0.953),而MAS和冠周FAI次之,分别为0.764(0.679~0.835)和0.723(0.636~0.800)(表 4)。多种指标绘制的ROC曲线(图 1)显示两种具有最大AUC的指标——MAS和冠周FAI两者之间的诊断效能无显著统计学差异(AUC: 0.764 vs. 0.723,P=0.797)。MAS联合冠周FAI可得到较为肯定的诊断效能,AUC达到0.818(0.738~0.881),联合指标诊断的准确率、敏感性、特异性、PPV、NPV分别为81.45%、75.68%、83.91%、66.7% 和89.0%。将此联合指标与CT-FFR同时绘制ROC曲线进行对比,二者之间无显著统计学差异(P=0.076,图 2)。MAS联合冠周FAI预测冠脉血流动力学异常的示例(图 3)。
4.
冠脉影像学指标在血流动力学异常方面的诊断效能
Diagnostic performance of coronary imaging indicators for hemodynamic abnormality
| Indicators | Accuracy | Sensitivity | Specitivity | PPV | NPV | Cut-off | AUC (95% CI) |
| CACS/vessel | 69.35 | 48.65 | 78.16 | 48.6 | 78.2 | 111.4 | 0.628 (0.537-0.713) |
| Lesion length | 70.16 | 29.73 | 87.36 | 50.0 | 74.5 | 34.56 | 0.588 (0.496-0.676) |
| MDS | 66.13 | 79.41 | 56.76 | 45.8 | 85.7 | 59.18 | 0.675 (0.578-0.762) |
| MAS | 77.42 | 72.97 | 79.31 | 60.0 | 87.3 | 69.23 | 0.764 (0.679-0.835) |
| TPB | 67.74 | 50.00 | 72.37 | 43.2 | 77.5 | 58.56 | 0.601 (0.503-0.694) |
| Perivascular FAI | 73.39 | 59.46 | 80.46 | 56.4 | 82.4 | -74.26 | 0.723 (0.636-0.800) |
| CT-FFR | 81.45 | 97.30 | 74.71 | 62.1 | 98.5 | 0.83 | 0.909 (0.844-0.953) |
| MAS+Perivascular FAI | 81.45 | 75.68 | 83.91 | 66.7 | 89.0 | 0.32 | 0.818 (0.738-0.881) |
1.
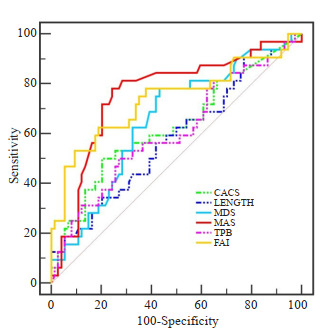
冠周FAI与CCTA影像学指标在血流动力学异常方面的诊断效能对比
Comparison of diagnostic performance of CCTA indicators and perivascular FAI for hemodynamic abnormality. MAS vs. perivascular FAI.
2.
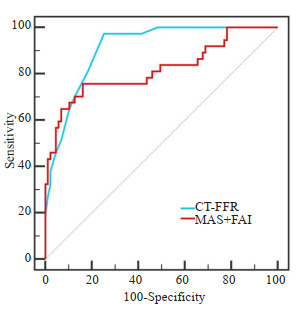
MAS联合冠周FAI与基于机器学习的CT-FFR在血流动力学异常方面的诊断效能对比
Comparison of MAS combined with perivascular FAI with CT-FFR based on machine learning in the diagnosis of hemodynamic abnormality.
3.
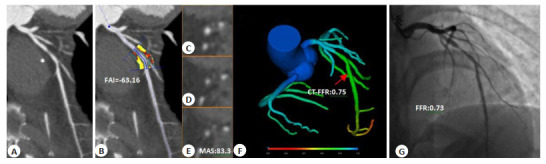
CCTA指标预测冠脉血流动力学异常示意图
A representative case showing the prediction of coronary hemodynamic abnormality using CCTA indicators. A: A 70-year-old female patient presented with severe stenosis of the proximal LAD segment (CAD-RADS: 4A). B: The FAI value was -63.16 HU based on CCTAimages. C-E: The MAS was 83.3%. F: CT-FFR of the distal stenosis was 0.75. G: The invasive FFR was 0.73.
3. 讨论
本研究发现在诊断预测冠脉病变特异性血流动力学异常方面,MAS和冠周FAI均具有较高的诊断效能;联合两指标的诊断效能具有增量价值,与CT-FFR的对比无显著统计学差异,表明这两种指标联合在诊断冠脉病变特异性缺血异常方面具有较好的临床价值。
冠周FAI是近年发现的反映血管活动性炎症状态的新型CCTA影像学指标,冠周FAI的升高与冠脉的炎症密切相关[9, 11, 12]。一方面,炎性信号可以抑制血管外脂肪的蓄积,抑制脂肪细胞的分化、成熟和脂肪化;另一方面,血管的炎症与内皮功能的紊乱存在密切关联[18]。当冠脉血管存在异常的动脉粥样硬化斑块导致的狭窄时,可能借由炎症信号,导致血管外的脂肪发生病理改变,这就能够解释为何升高的冠周FAI可能与FFR的降低有关。血管炎症反应导致了血管周围脂肪组织产生了从脂肪相到水相的变化,这种组织差异可以通过CCTA的CT值检测到[9]。既往研究发现,冠周FAI联合直径狭窄率、总斑块体积,可以较好地预测有临床意义的冠脉狭窄,具有较高的诊断准确率[13]。这与我们的研究结果一致,在应用冠周FAI进行血流动力学异常的诊断时,此指标具备了良好的诊断效能,AUC达到0.723;不同的是,虽然诊断特异性达到了80.46%,但敏感性仅有59.46%,与前述研究相反,这可能是由于本研究样本量小、研究人群是行ICA和有创FFR的CAD高危人群等原因导致。
冠脉解剖学狭窄与血流动力学异常之间存在一定的关联,但结果并不完全吻合[19],功能学异常受到较多因素的影响,如病变弥漫程度、斑块内部成分、内皮功能情况、冠脉痉挛和微循环障碍等,而非仅有管腔狭窄[14, 20-23]。FAME研究发现,即使达到中度以上狭窄,仍有65%的患者并不存在病变特异性的血流动力学异常[24],因此在解剖学发现的中度狭窄的患者中,预测功能学异常是当前研究者重点关注的问题,决定着后续临床决策和患者远期预后。在预测血流动力学异常方面,传统的冠脉狭窄指标可以得到较高的准确率,如直径狭窄率、面积狭窄率和斑块体积等[25, 26]。在本研究中,MAS的诊断效能优于MDS和TPB,可能在于MAS较MDS能够提供更多的血管特征信息,MDS只能反映目标病变横断面最严重的直径狭窄信息,对于部分弥漫、分叉、偏心和重度钙化病变评估方面存在局限,与既往研究结果相似[26];而另一方面,TPB虽然是斑块的三维立体结构的反映,但在测量上受影响因素较多,如血管的体积、图像的伪影、斑块内部成分非均质性等,均有可能对测量带来潜在影响,测量流程较为繁琐,应用价值也不高。由此来看,MAS在预测血流动力学异常方面更加准确,而且测量稳定可靠,同时在实际临床应用中较为简便,具备一定的应用优势。
本研究中,我们发现了冠周FAI与MAS是诊断效能最高的两种CCTA影像学指标,因此探索性的将两种指标结合,对比联合指标与CT-FFR的诊断效能。结果显示,联合指标与CT-FFR的诊断效能无显著统计学差异,这表明了即使是单纯的影像学表现也可在一定程度上综合反映冠脉压力阶差变化。由于冠脉狭窄容易受到CCTA图像质量和钙化容积效应的影响,易高估病变[4],而冠周FAI不受钙化斑块影响,可间接反映血管炎症状态,测量结果相对稳定,因此血管内外两种指标的联合可能带来更好的诊断预测效能。在既往研究中已经发现CT-FFR在冠脉血流动力学异常方面具有较高的诊断准确率,与有创FFR结果高度一致[5-8],因此,与之基本等效的联合指标也可被认为是一种较为理想、可信的诊断指标。更为重要的是,虽然CT-FFR的准确性和可行性已经被大量临床注册研究所证实,但其推广应用仍然存在局限,测量需要专用软件平台、测量时间仍然较长、费用较高[16, 27]。简单、便捷、易于获取和理解的影像学指标在应用上具有更多的潜在价值。
我们通过单因素分析也比较了部分CCTA影像指标,发现对应血管CACS在血流动力学异常组明显较高,这与前述研究相一致[28, 29]。冠脉钙化从形态上,可以分为大钙化与小钙化,小钙化与冠脉斑块的易损性相关,预示着斑块内部存在活动性炎症和坏死核心等,而大钙化则多数与后期病变趋于稳定有关联[30, 31],这也就可以解释为何在多因素分析中,笼统的CACS并不能发现与血流动力学异常之间的关联。此外,在单因素分析中,血流动力学异常组的病变长度均值虽然高于正常组,但两组并无统计学差异,这反映了单独病变弥漫程度不能预测功能学异常与否,符合我们的临床认知。然而,即使此结果也不能完全否认这些影像学指标在诊断血流动力学异常方面的重要性,对于冠心病中低危人群,这些指标与狭窄程度存在关联,并且与患者的心血管预后直接相关,如MESA研究发现,钙化积分可以在传统心血管危险因素基础上,提高对缺血事件的预测价值[32]。对这些指标的充分探索和应用,还需要建立在更大样本量的前瞻性研究的基础之上。
Biography
单冬凯,博士,主治医师,E-mail: shandongkai1234@163.com
Funding Statement
国家重点研发计划(2016YFC1300304),北京市科技新星计划(Z181100006218055),北京力生心血管健康基金会领航基金重点项目
Contributor Information
单 冬凯 (Dongkai SHAN), Email: shandongkai1234@163.com.
杨 俊杰 (Junjie CHEN), Email: fearlessyang@126.com.
References
- 1.Timmis A, Townsend N, Gale C, et al. European society of cardiology: cardiovascular disease statistics 2017. Eur Heart J. 2018;39(7):508–79. doi: 10.1093/eurheartj/ehx628. [Timmis A, Townsend N, Gale C, et al. European society of cardiology: cardiovascular disease statistics 2017[J]. Eur Heart J, 2018, 39(7): 508-79.] [DOI] [PubMed] [Google Scholar]
- 2.Task Force Members, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the european society of cardiology. Eur Heart J. 2013;34(38):2949–3003. doi: 10.1093/eurheartj/eht296. [Task Force Members, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the european society of cardiology[J]. Eur Heart J, 2013, 34(38): 2949-3003.] [DOI] [PubMed] [Google Scholar]
- 3.Chen YD, Fang WY, Chen JY, et al. Chinese expert consensus on the non-invasive imaging examination pathways of stable coronary artery disease. http://www.ixueshu.com/api/search/info/a1a89c49bc6bff804cd947eba48d91c7318947a18e7f9386.html. J Geriatr Cardiol. 2018;15(1):30–40. doi: 10.11909/j.issn.1671-5411.2018.01.012. [Chen YD, Fang WY, Chen JY, et al. Chinese expert consensus on the non-invasive imaging examination pathways of stable coronary artery disease[J]. J Geriatr Cardiol, 2018, 15(1): 30-40.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmermund A, Eckert J, Schmidt M, et al. Coronary computed tomography angiography: a method coming of age. http://europepmc.org/abstract/MED/29974195. Clin Res Cardiol. 2018;107(Suppl 2):40–8. doi: 10.1007/s00392-018-1320-5. [Schmermund A, Eckert J, Schmidt M, et al. Coronary computed tomography angiography: a method coming of age[J]. Clin Res Cardiol, 2018, 107(Suppl 2): 40-8.] [DOI] [PubMed] [Google Scholar]
- 5.Douglas PS, de Bruyne B, Pontone G, et al. 1-year outcomes of FFRCT-guided care in patients with suspected coronary disease: the PLATFORM study. JAm Coll Cardiol. 2016;68(5):435–45. doi: 10.1016/j.jacc.2016.05.057. [Douglas PS, de Bruyne B, Pontone G, et al. 1-year outcomes of FFRCT-guided care in patients with suspected coronary disease: the PLATFORM study[J]. J Am Coll Cardiol, 2016, 68(5): 435-45.] [DOI] [PubMed] [Google Scholar]
- 6.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of ischemia-causing stenoses obtained via noninvasive fractional flow reserve) study. J Am Coll Cardiol. 2011;58(19):1989–97. doi: 10.1016/j.jacc.2011.06.066. [Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of ischemia-causing stenoses obtained via noninvasive fractional flow reserve) study[J]. J Am Coll Cardiol, 2011, 58(19): 1989-97.] [DOI] [PubMed] [Google Scholar]
- 7.Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308(12):1237–45. doi: 10.1001/2012.jama.11274. [Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography[J]. JAMA, 2012, 308(12): 1237-45.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: Next Steps) J Am Coll Cardiol. 2014;63(12):1145–55. doi: 10.1016/j.jacc.2013.11.043. [Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: Next Steps) [J]. J Am Coll Cardiol, 2014, 63(12): 1145-55.] [DOI] [PubMed] [Google Scholar]
- 9.Antonopoulos AS, Sanna F, Sabharwal N, et al. Detecting human coronary inflammation by imaging perivascular fat. Sci Transl Med. 2017;9(398):eaal2658. doi: 10.1126/scitranslmed.aal2658. [Antonopoulos AS, Sanna F, Sabharwal N, et al. Detecting human coronary inflammation by imaging perivascular fat[J]. Sci Transl Med, 2017, 9(398): eaal2658.] [DOI] [PubMed] [Google Scholar]
- 10.Elnabawi YA, Oikonomou EK, Dey AK, et al. Association of biologic therapy with coronary inflammation in patients with psoriasis as assessed by perivascular fat attenuation index. JAMA Cardiol. 2019;4(9):885–91. doi: 10.1001/jamacardio.2019.2589. [Elnabawi YA, Oikonomou EK, Dey AK, et al. Association of biologic therapy with coronary inflammation in patients with psoriasis as assessed by perivascular fat attenuation index[J]. JAMA Cardiol, 2019, 4(9): 885-91.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai X, Deng JH, Yu MM, et al. Perivascular fat attenuation index and high-risk plaque features evaluated by coronary CT angiography: relationship with serum inflammatory marker level. Int J Cardiovasc Imaging. 2020;36(4):723–30. doi: 10.1007/s10554-019-01758-8. [Dai X, Deng JH, Yu MM, et al. Perivascular fat attenuation index and high-risk plaque features evaluated by coronary CT angiography: relationship with serum inflammatory marker level[J]. Int J Cardiovasc Imaging, 2020, 36(4): 723-30.] [DOI] [PubMed] [Google Scholar]
- 12.Oikonomou EK, Marwan M, Desai MY, et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet. 2018;392(10151):929–39. doi: 10.1016/S0140-6736(18)31114-0. [Oikonomou EK, Marwan M, Desai MY, et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data[J]. Lancet, 2018, 392(10151): 929-39.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu MM, Dai X, Deng JH, et al. Diagnostic performance of perivascular fat attenuation index to predict hemodynamic significance of coronary stenosis: a preliminary coronary computed tomography angiography study. Eur Radiol. 2020;30(2):673–81. doi: 10.1007/s00330-019-06400-8. [Yu MM, Dai X, Deng JH, et al. Diagnostic performance of perivascular fat attenuation index to predict hemodynamic significance of coronary stenosis: a preliminary coronary computed tomography angiography study[J]. Eur Radiol, 2020, 30(2): 673-81.] [DOI] [PubMed] [Google Scholar]
- 14.Yin PY, Dou GH, Yang X, et al. Noninvasive quantitative plaque analysis identifies hemodynamically significant coronary arteries disease. http://journals.lww.com/thoracicimaging/Abstract/2021/03000/Noninvasive_Quantitative_Plaque_Analysis.5.aspx. J Thorac Imaging. 2020:10. doi: 10.1097/RTI.0000000000000494. [Yin PY, Dou GH, Yang X, et al. Noninvasive quantitative plaque analysis identifies hemodynamically significant coronary arteries disease[J]. J Thorac Imaging, 2020: 10.1097/RTI. 0000000000000494.] [DOI] [PubMed] [Google Scholar]
- 15.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32. doi: 10.1016/0735-1097(90)90282-T. [Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography[J]. J Am Coll Cardiol, 1990, 15(4): 827-32.] [DOI] [PubMed] [Google Scholar]
- 16.Yang JJ, Shan DK, Dong M, et al. The effect of on-site CT-derived fractional flow reserve on the management of decision making for patients with stable chest pain (TARGET trial): objective, rationale, and design. Trials. 2020;21(1):728. doi: 10.1186/s13063-020-04649-9. [Yang JJ, Shan DK, Dong M, et al. The effect of on-site CT-derived fractional flow reserve on the management of decision making for patients with stable chest pain (TARGET trial): objective, rationale, and design[J]. Trials, 2020, 21(1): 728.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45. doi: 10.2307/2531595. [DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach[J]. Biometrics, 1988, 44(3): 837-45.] [DOI] [PubMed] [Google Scholar]
- 18.Grant RW, Stephens JM. Fat in flames: influence of cytokines and pattern recognition receptors on adipocyte lipolysis. http://www.ncbi.nlm.nih.gov/pubmed/26058863. Am J Physiol Endocrinol Metab. 2015;309(3):E205-13. doi: 10.1152/ajpendo.00053.2015. [Grant RW, Stephens JM. Fat in flames: influence of cytokines and pattern recognition receptors on adipocyte lipolysis[J]. Am J Physiol Endocrinol Metab, 2015, 309(3): E205-13.] [DOI] [PubMed] [Google Scholar]
- 19.Tonino PA, de Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213–24. doi: 10.1056/NEJMoa0807611. [Tonino PA, de Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention [J]. N Engl J Med, 2009, 360(3): 213-24.] [DOI] [PubMed] [Google Scholar]
- 20.Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131(10):861–70. doi: 10.1161/CIRCULATIONAHA.114.011201. [Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries [J]. Circulation, 2015, 131(10): 861-70.] [DOI] [PubMed] [Google Scholar]
- 21.Eftekhari A, Min J, Achenbach S, et al. Fractional flow reserve derived from coronary computed tomography angiography: diagnostic performance in hypertensive and diabetic patients. Eur Heart J Cardiovasc Imaging. 2017;18(12):1351–60. doi: 10.1093/ehjci/jew209. [Eftekhari A, Min J, Achenbach S, et al. Fractional flow reserve derived from coronary computed tomography angiography: diagnostic performance in hypertensive and diabetic patients[J]. Eur Heart J Cardiovasc Imaging, 2017, 18(12): 1351-60.] [DOI] [PubMed] [Google Scholar]
- 22.Doris MK, Otaki Y, Arnson Y, et al. Non-invasive fractional flow reserve in vessels without severe obstructive Stenosis is associated with coronary plaque burden. J Cardiovasc Comput Tomogr. 2018;12(5):379–84. doi: 10.1016/j.jcct.2018.05.003. [Doris MK, Otaki Y, Arnson Y, et al. Non-invasive fractional flow reserve in vessels without severe obstructive Stenosis is associated with coronary plaque burden[J]. J Cardiovasc Comput Tomogr, 2018, 12(5): 379-84.] [DOI] [PubMed] [Google Scholar]
- 23.Ahmadi N, Ruiz-Garcia J, Hajsadeghi F, et al. Impaired coronary artery distensibility is an endothelium-dependent process and is associated with vulnerable plaque composition. Clin Physiol Funct Imaging. 2016;36(4):261–8. doi: 10.1111/cpf.12220. [Ahmadi N, Ruiz-Garcia J, Hajsadeghi F, et al. Impaired coronary artery distensibility is an endothelium-dependent process and is associated with vulnerable plaque composition[J]. Clin Physiol Funct Imaging, 2016, 36(4): 261-8.] [DOI] [PubMed] [Google Scholar]
- 24.Tonino PA, Fearon WF, de Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. JAm Coll Cardiol. 2010;55(25):2816–21. doi: 10.1016/j.jacc.2009.11.096. [Tonino PA, Fearon WF, de Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation [J]. J Am Coll Cardiol, 2010, 55(25): 2816-21.] [DOI] [PubMed] [Google Scholar]
- 25.Nakazato R, Shalev A, Doh JH, et al. Aggregate plaque volume by coronary computed tomography angiography is superior and incremental to luminal narrowing for diagnosis of ischemic lesions of intermediate Stenosis severity. J Am Coll Cardiol. 2013;62(5):460–7. doi: 10.1016/j.jacc.2013.04.062. [Nakazato R, Shalev A, Doh JH, et al. Aggregate plaque volume by coronary computed tomography angiography is superior and incremental to luminal narrowing for diagnosis of ischemic lesions of intermediate Stenosis severity[J]. J Am Coll Cardiol, 2013, 62(5): 460-7.] [DOI] [PubMed] [Google Scholar]
- 26.Chung WY, Choi BJ, Lim SH, et al. Three dimensional quantitative coronary angiography can detect reliably ischemic coronary lesions based on fractional flow reserve. J Korean Med Sci. 2015;30(6):716–24. doi: 10.3346/jkms.2015.30.6.716. [Chung WY, Choi BJ, Lim SH, et al. Three dimensional quantitative coronary angiography can detect reliably ischemic coronary lesions based on fractional flow reserve[J]. J Korean Med Sci, 2015, 30(6): 716-24.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fairbairn TA, Nieman K, Akasaka T, et al. Real-world clinical utility and impact on clinical decision-making of coronary computed tomography angiography-derived fractional flow reserve: lessons from the ADVANCE Registry. Eur Heart J. 2018;39(41):3701–11. doi: 10.1093/eurheartj/ehy530. [Fairbairn TA, Nieman K, Akasaka T, et al. Real-world clinical utility and impact on clinical decision-making of coronary computed tomography angiography-derived fractional flow reserve: lessons from the ADVANCE Registry[J]. Eur Heart J, 2018, 39(41): 3701-11.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease: a substudy of the NXT trial. JACC Cardiovasc Imaging. 2015;8(9):1045–55. doi: 10.1016/j.jcmg.2015.06.003. [Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease: a substudy of the NXT trial [J]. JACC Cardiovasc Imaging, 2015, 8(9): 1045-55.] [DOI] [PubMed] [Google Scholar]
- 29.Jiang M, Zhang XL, Liu H, et al. The effect of coronary calcification on diagnostic performance of machine learning-based CT-FFR: a Chinese multicenter study. Eur Radiol. 2021;31(3):1482–93. doi: 10.1007/s00330-020-07261-2. [Jiang M, Zhang XL, Liu H, et al. The effect of coronary calcification on diagnostic performance of machine learning-based CT-FFR: a Chinese multicenter study[J]. Eur Radiol, 2021, 31(3): 1482-93.] [DOI] [PubMed] [Google Scholar]
- 30.Shioi A, Ikari Y. Plaque calcification during atherosclerosis progression and regression. J Atheroscler Thromb. 2018;25(4):294–303. doi: 10.5551/jat.RV17020. [Shioi A, Ikari Y. Plaque calcification during atherosclerosis progression and regression[J]. J Atheroscler Thromb, 2018, 25(4): 294-303.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.陈 彦汝, 言 述, 修 志刚, et al. 同步12导联动态心电图联合螺旋CT可提高对冠脉血管病变程度的诊断效能. http://www.j-fzyx.com/article/doi/10.12122/j.issn.1674-4500.2021.01.15. 分子影像学杂志. 2021;44(1):78–82. [陈彦汝, 言述, 修志刚, 等. 同步12导联动态心电图联合螺旋CT可提高对冠脉血管病变程度的诊断效能[J]. 分子影像学杂志, 2021, 44(1): 78-82.] [Google Scholar]
- 32.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–45. doi: 10.1056/NEJMoa072100. [Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups[J]. N Engl J Med, 2008, 358(13): 1336-45.] [DOI] [PubMed] [Google Scholar]


