Key Points
Question
Is very preterm birth or very low birth weight vs term birth associated with intelligence in adulthood?
Findings
In this meta-analysis of individual participant data from 8 cohorts comprising 2135 adults with and without very preterm birth or very low birth weight in 7 countries, IQ was significantly lower among adults who were born very preterm or with very low birth weight compared with adults who were born at term, with a mean between-group difference of approximately 12 IQ points. Lower gestational age, lower birth weight z scores, the presence of neonatal bronchopulmonary dysplasia or intraventricular hemorrhage, and lower maternal educational levels were significantly associated with lower IQ among adults born very preterm or with very low birth weight.
Meaning
This individual patient data meta-analysis suggests that very preterm birth or very low birth weight may be associated with a clinically relevant difference in IQ, relative to term birth, in adulthood.
Abstract
Importance
Birth before 32 weeks’ gestation (very preterm [VPT]) and birth weight below 1500 g (very low birth weight [VLBW]) have been associated with lower cognitive performance in childhood. However, there are few investigations of the association of neonatal morbidities and maternal educational levels with the adult cognitive performance of individuals born VPT or VLBW (VPT/VLBW).
Objective
To assess differences in adult IQ between VPT/VLBW and term-born individuals and to examine the association of adult IQ with cohort factors, neonatal morbidities, and maternal educational level among VPT/VLBW participants.
Data Sources
Systematic review of published data from PubMed and meta-analysis of individual participant data (IPD) of cohorts from 2 consortia (Research on European Children and Adults Born Preterm [RECAP] and Adults Born Preterm International Collaboration [APIC]).
Study Selection
The meta-analysis included prospective longitudinal cohort studies that assessed the full-scale IQ of adults born VPT or VLBW and respective control groups comprising term-born adults.
Data Extraction and Synthesis
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline for analyses of individual participant data and identified 8 studies that provided data from 2135 adults (1068 VPT/VLBW and 1067 term-born participants) born between 1978 and 1995. Meta-analyses of IPD were performed using a 1-stage approach, treating VPT birth or VLBW and cohort as random effects.
Main Outcomes and Measures
Full-scale IQ scores were converted to z scores within each cohort using the combined SD of VPT/VLBW participants and a control group of term-born participants, with scores centered on the mean of the control group.
Results
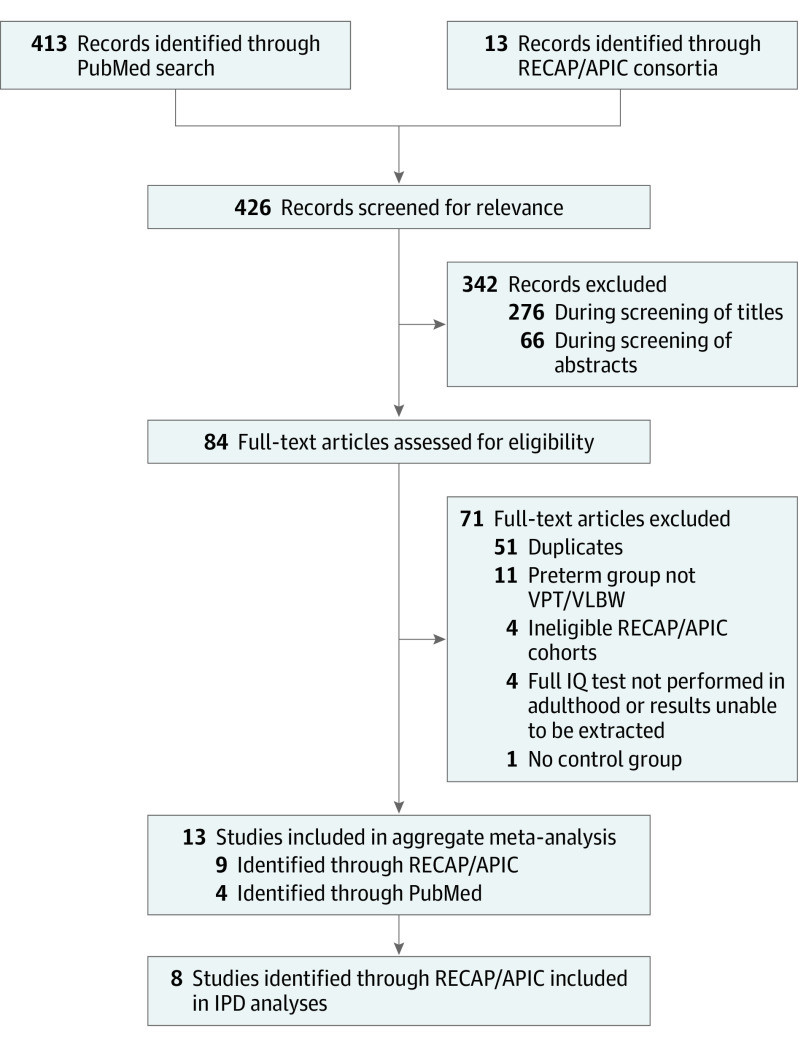
A total of 426 records were identified and screened. After exclusions, 13 studies were included in the aggregate meta-analysis. The IPD meta-analysis included 8 of the 9 RECAP and APIC cohorts with adult IQ data. The mean (SD) age among the 8 IPD cohorts was 24.6 (4.3) years, and 1163 participants (54.5%) were women. In unadjusted analyses, VPT/VLBW participants had mean adult IQ scores that were 0.78 SD (95% CI, −0.90 to −0.66 SD) lower than term-born participants, equivalent to a difference of 12 IQ points. Among VPT/VLBW participants, lower gestational age (score difference per week of gestation, 0.11; 95% CI, 0.07-0.14), lower birth weight z scores (score difference per 1.0 SD, 0.21; 95% CI, 0.14-0.28), the presence of neonatal bronchopulmonary dysplasia (score difference, −0.16; 95% CI, −0.30 to −0.02) or any grade of intraventricular hemorrhage (score difference, −0.19; 95% CI, −0.33 to −0.05), and lower maternal educational level (score difference, 0.26; 95% CI, 0.17-0.35) were all significantly associated with lower IQ scores in adulthood.
Conclusions and Relevance
In this IPD meta-analysis, lower gestational age, lower weight for gestational age, neonatal morbidities, and lower maternal educational levels were all important risk factors associated with lower IQ among young adults born VPT or VLBW.
This meta-analysis of individual participant data uses data from cohort studies to examine the association of very preterm birth or very low birth weight with intelligence in adulthood.
Introduction
An important life outcome after very preterm (VPT) birth (<32 weeks’ gestation) or very low birth weight (VLBW; <1500 g) is intelligence, defined as “the capacity to learn from experience, using metacognitive processes to enhance learning and adapt to the surrounding environment.”1(p751) Standardized intelligence tests in the general population provide an IQ score with a normative mean (SD) of 100 (15) points. An individual’s IQ is associated with a range of life course outcomes, including physical health, premature death, educational attainment, and socioeconomic success.2,3,4,5 Thus, adult IQ is a global factor associated with long-term outcomes among individuals born VPT or VLBW (VPT/VLBW).
While individual studies typically indicate that VPT/VLBW individuals have lower IQ in adulthood than term-born individuals,6,7,8 to our knowledge, no specific meta-analysis of adult IQ among VPT/VLBW individuals has been published. Meta-analyses of childhood IQ have reported that the scores of VPT/VLBW children are approximately 11 to 13 IQ points lower on tests than term-born children.9,10,11,12 Sustained differences into adulthood cannot be assumed, as indicated by the smaller IQ differences in adulthood that have been reported among individuals with normal vs low birth weight.13 Furthermore, considerable variation across VPT/VLBW cohorts has been found, which is potentially explained by factors such as gestational age or birth weight inclusion criteria and later selective attrition.11 Variation in IQ may be associated with individual-level neonatal or demographic factors, such as sex, low birth weight for gestational age, neonatal morbidities, or maternal educational level.14,15,16,17
To investigate cohort- and individual-level factors, meta-analyses of individual participant data (IPD) have been proposed as superior to traditional meta-analyses of aggregated data.18 Meta-analysis of IPD allows for accurate harmonization of data across cohorts and increased statistical power for detecting individual-level risk factors.19 Furthermore, the associations of cohort-specific factors, such as rates of attrition, can be investigated.
We performed an IPD meta-analysis of IQ in adulthood with 3 objectives. The first was to compare the difference in adult IQ among VPT/VLBW participants vs a control group of term-born participants, the second was to examine cohort- and individual-level factors associated with adult IQ among VPT/VLBW participants, and the third was to conduct a sensitivity analysis assessing whether adult IQ scores from the IPD cohorts were representative of all cohorts of VPT/VLBW individuals.
Methods
Protocol and Registration
This study was conducted as part of the Research on European Children and Adults Born Preterm (RECAP) Consortium.20 Along with 7 adult RECAP cohorts, 6 non-European cohorts from the Adults Born Preterm International Collaboration (APIC) Consortium21 were invited to participate. All studies had received country-specific ethical reviews, with participants providing written informed consent, and all adhered to the Declaration of Helsinki.22 This IPD meta-analysis was registered with the International Prospective Register of Systematic Reviews (PROSPERO; registration number CRD42020162043) and followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline for analyses of individual participant data.
Eligibility Criteria and Search Strategy
Prospective longitudinal cohort studies of VPT/VLBW adult participants who had completed a standardized IQ test at a mean age of 17 years or older were eligible for inclusion. All cohort studies were required to include a control group of term-born participants to allow for computation of harmonized and comparable IQ z scores, which minimized bias owing to different versions of tests or secular trends (ie, the Flynn effect).23
To assess whether the cohorts from RECAP and APIC were representative of all VPT/VLBW participants reported in the literature, we performed a PubMed search using the search string (intelligence OR IQ OR cognition OR cognitive) AND (adult OR adulthood OR late adolescence) AND (preterm OR gestation OR birthweight OR birth weight). The last search was performed on July 9, 2020.
Study Selection, Data Collection, and Data Harmonization
Eligibility for inclusion was assessed by 2 authors (R.E. and Y.N.). Any disagreements regarding eligibility were resolved by discussion.
After initial data scoping, encrypted data from each cohort were transferred to the University of Warwick. Data including IQ scores, neonatal variables, maternal educational levels, the presence of neurosensory impairment (NSI) in childhood, and attrition rates were collected for all cohorts. All data were only accessible to authorized personnel from the RECAP Consortium.
To harmonize results, IQ scores were converted to z scores within each cohort using the combined SD of both groups (VPT/VLBW and control), with scores centered on the mean of the control group. Neonatal data included gestational age at birth, sex, birth weight, presence of bronchopulmonary dysplasia (BPD), presence of intraventricular hemorrhage (IVH), and multiple birth. The definitions of BPD varied, with some studies defining BPD as oxygen dependency at 36 weeks’ postmenstrual age and some defining it as oxygen dependency more than 28 days after birth. For each definition, separate subanalyses were performed to assess each criterion’s independent association with IQ. The definition of IVH was classified according to criteria provided by Papile et al24 (ie, IVH is categorized from grades 1-4, with 1 indicating hemorrhage limited to germinal matrix, 2 indicating blood noted within the ventricular system but not distending it, 3 indicating blood in the ventricles with distension of the ventricles, and 4 indicating intraventricular hemorrhage with parenchymal extension); however, some cohorts provided either IVH grades 3 and 4 or IVH grades 2 and 3 combined. Thus, IVH was harmonized into no IVH vs any IVH (grades 1-4), and a subanalysis was performed to compare no IVH or IVH grades 1 to 2 with IVH grades 3 to 4 among cohorts for which analysis was possible. Multiple birth was classified as a binary variable, with 0 indicating singleton birth and 1 indicating multiple birth. Birth weight z scores were determined using the Fenton international growth chart for preterm infants.25
Maternal educational level was harmonized according to the International Standard Classification of Education (ISCED) into low (ISCED levels 0-2), medium (ISCED levels 3-5), and high (ISCED levels 6-8).26 Evidence of childhood NSI was collated from data indicating severe visual impairment (blind in both eyes), hearing impairment (uncorrected by assistive devices), nonambulatory cerebral palsy, or childhood cognitive impairment (IQ <70 points). If data regarding a certain NSI variable were missing for a participant, the individual was categorized as having no evidence of the presence of that impairment. Data indicating the presence of NSI were combined into a binary childhood NSI variable (any evidence of impairment vs no evidence of impairment) (eTable 1 in the Supplement). In addition, 4 cohort-level factors were assessed. For each cohort, the percentage of eligible VPT/VLBW participants who did not have adult IQ scores was calculated (ie, the percentage of attrition among VPT/VLBW participants). To focus on selective attrition, the percentage of VPT/VLBW participants with diagnoses of childhood NSI who did not have adult IQ scores was also calculated (ie, the percentage of attrition among VPT/VLBW participants with childhood NSI). Data on year of birth and mean age at assessment among VPT/VLBW participants in each cohort were also recorded.
IPD Integrity, Risk of Bias, and Outcome Measures
Data were assessed for consistency with previous studies of the included cohorts, with any discrepancies resolved by communication with the respective study investigators. Two authors (R.E. and Y.N.) assessed cohort quality and comparability using the Newcastle-Ottawa Scale27 (score range of 0-9, with higher scores indicating higher quality) (eTable 2 in the Supplement). The primary outcome of interest was the full-scale IQ z score of VPT/VLBW participants compared with term-born participants.
Synthesis Methods
All participants with adult IQ scores were included. Missing neonatal data were imputed solely for VPT/VLBW participants, and missing data on maternal educational levels were imputed for both VPT/VLBW and term-born participants using multiple imputation by chained equations (mice),28 which resulted in less than 5% of the data being imputed (Table 1).7,8,29,30,31,32,33,34 In the first analysis, a simple comparison of IQ scores between VPT/VLBW and term-born participants was conducted using a 1-stage linear mixed model. We analyzed the association of VPT birth or VLBW with IQ using a random-intercept model for each cohort and a random slope for the association of VPT birth or VLBW with IQ by cohort, which was estimated using maximum likelihood via the lme4 package, version 1.1-21, in R software, version 3.6.1 (R Foundation for Statistical Computing).35 The association between VPT birth or VLBW and IQ was then examined after adjusting for sex and maternal educational level and after removing VPT/VLBW participants with childhood NSI or differentiating between VPT/VLBW participants with and without neonatal morbidities (ie, IVH and BPD). All analyses used a 1-stage approach with random intercepts and slopes.
Table 1. Summary of Studies Included in Individual Participant Data Meta-analysis.
| Source | Study name | Country | Participant birth year | Mean age at IQ assessment, y | IQ test administered | Initial eligibility criteria | Initial VPT/VLBW participants surviving to discharge, No. | Eligible VPT/VLBW adults, No. | Attrition among VPT/VLBW participants, No./total No. (%) | Attrition among VPT/ VLBW participants with childhood NSI, No./total No. (%) | VPT/ VLBW participants with adult IQ scores, No. | Term-born participants in control group, No. (age range at recruitment) | Harmonization issues | Neonatal/maternal educational data imputed for VPT/VLBW participants, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heinonen et al,29 2018 | Arvo Ylppo Longitudinal Study (AYLS) | Finland | 1985-1986 | 26 | WAIS-III | GA <37 wk (reduced to VPT/VLBW for this analysis) | 108 | 68 | 40/68 (58.8) | 12/15 (80.0) | 28 | 303 (infancy) | None | 0 |
| Madzwamuse et al,8 2015 | Bavarian Longitudinal Study (BLS) | Germany | 1985-1986 | 26 | WAIS-III | VPT/VLBW (GA <32 wk or BW <1500 g) | 510 | 411 | 208/411 (50.6) | 69/91 (75.8) | 203 | 192 (infancy) | None | <1 |
| Linsell et al,7 2018 | EPICure | United Kingdom and Ireland | 1995 | 19 | WAIS-II | EPT (GA <26 wk) | 315 | 306 | 182/306 (59.5) | 41/55 (74.5) | 124 | 64 (6 or 11 y) | None | 1 |
| Pyhala et al,30 2011 | Helsinki Study of Very Low Birth Weight Adults (HESVA) | Finland | 1978-1985 | 25 | WAIS-III | VLBW (<1500 g) | 334 | 254 | 145/254 (57.1) | 11/16 (68.8) | 109 | 98 (adulthood) | Maternal educational level measured in adulthood; NSI did not include IQ <70 and could not differentiate ambulatory/nonambulatory cerebral palsy | 4 |
| Lærum et al,31 2019 | Norwegian University of Science and Technology (NTNU) study | Norway | 1986-1988 | 26 | WASI | VLBW (<1500 g) | 86 | 82 | 31/82 (37.8) | 6/10 (60.0) | 51 | 75 (infancy) | Maternal educational level measured at 14 y | 6 |
| Darlow et al,32 2020 | New Zealand Very Low Birth Weight (NZ-VLBW) study | New Zealand | 1986 | 28 | WASI-II | VLBW (<1500 g) | 338 | 323 | 98/323 (30.3) | 16/25 (64.0) | 225 | 100 (adulthood) | None | 1 |
| Kroll et al,33 2017 | University College London Hospitals (UCLH) study | United Kingdom | 1979-1984 | 30 | WAIS-II | VPT (GA <33 wk, reduced to VPT/VLBW for this analysis) | 302a | 220a | 98/220 (44.5) | 11/13 (84.6) | 104 | 89 (adulthood) | BPD not available so was fully imputed; maternal educational level reported by participant in adulthood; NSI solely based on IQ <70 at 8 y | 21 |
| Doyle et al,34 2015 | Victorian Infant Collaborative Study (VICS) | Australia | 1991-1992 | 18b | WAIS-II | EPT/ELBW (GA <28 wk or BW <1000 g) | 299 | 277 | 53/277 (19.1) | 16/43 (37.2) | 224 | 146 (infancy) | None | 6 |
Abbreviations: BPD, bronchopulmonary dysplasia; BW, birth weight; EPT/ELBW, extremely preterm or extremely low birth weight; GA, gestational age; NSI, neurosensory impairment; VPT/VLBW, very preterm or very low birth weight; WAIS-II, Wechsler Adult Intelligence Scale, Second Edition (1981); WAIS-III, Wechsler Adult Intelligence Scale, Third Edition (1997); WASI, Wechsler Abbreviated Scale of Intelligence (1999); WASI-II, Wechsler Abbreviated Scale of Intelligence, Second Edition (2011).
Cohort information regarding attrition, eligible adult sample, and initial sample from the Kroll et al UCLH study33 was based on the <33 weeks’ gestational age criteria rather than the VPT/VLBW criteria (gestational age <32 weeks or birth weight <1500 g) that was used in subsequent studies. Although 122 individuals who were born preterm (<33 weeks’ gestation) participated in the study in adulthood, only 104 adults were VPT/VLBW and included in the present meta-analysis.
This study only used data from the follow-up at age 18 years. Not all participants were strictly aged 18 years; therefore, the mean age was used.
Additional Analyses
To explore antecedents of IQ scores among VPT/VLBW participants, a 1-stage IPD analysis was performed. Cohort factors (age at IQ assessment, birth year, percentage of attrition among VPT/VLBW participants, and percentage of attrition among VPT/VLBW participants with childhood NSI) were added as fixed effects. Individual-level neonatal factors and maternal educational levels were then also added as fixed effects. Beta estimates from all factors were reported for both the univariable and multivariable analyses to assess their independent and combined associations. Statistical significance was set at P < .05.
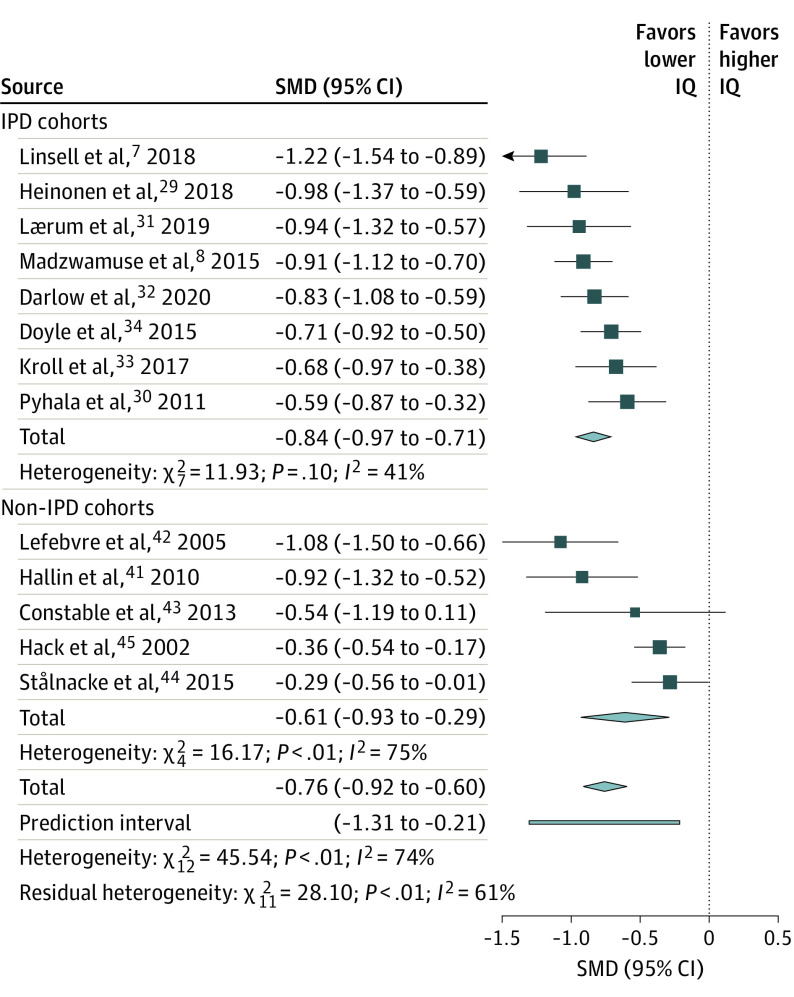
A sensitivity meta-analysis using aggregate data was performed by combining all cohorts used in the IPD analyses, summary data from the Hack study,6 and additional cohorts identified through the PubMed search for whom IPD were not requested. The standardized mean difference (SMD) in IQ scores between VPT/VLBW and term-born participants in each cohort were pooled using a random-effects meta-analysis via the meta package, version 4.9-7, in R software.36 Heterogeneity across cohorts was assessed using Cochran Q and I2 statistics, and a subgroup analysis was performed to differentiate between IPD and non-IPD cohorts to test for selection bias.
Results
Study Selection and Participant Characteristics
A total of 426 records were identified and screened; of those, 413 records were identified through a PubMed search, and 13 records were known studies conducted by the RECAP and APIC consortia. Overall, 342 records were excluded based on titles and abstracts, and 84 full-text articles were assessed for eligibility (Figure 1). Of 7 potential RECAP cohort studies of adults,7,8,29,30,31,37,38 2 were excluded: the Suikkanen et al study,37 which did not perform a full-scale IQ test, and the Weisglas-Kuperus et al study,38 which did not include a control group. Among 6 potential APIC cohort studies,6,32,33,34,39,40 3 were excluded: the Saigal et al39 and Doyle et al40 studies, which did not assess adult IQ, and the Hack study,6 for which only summary data were available. After exclusions, 13 studies (9 RECAP or APIC cohorts and 4 cohorts identified through PubMed) were included in the aggregate meta-analysis. The IPD meta-analysis included 87,8,29,30,31,32,33,34 of the 9 RECAP and APIC cohorts with adult IQ data, comprising a total of 2135 adults (1068 VPT/VLBW participants and 1067 term-born participants). The mean (SD) age among the 8 IPD cohorts was 24.6 (4.3) years, and 1163 participants (54.5%) were women. Summary data for each cohort included in the IPD analyses are shown in Table 1.
Figure 1. Flowchart of Studies Included in the Independent Participant Data (IPD) and Aggregate Meta-analyses.
APIC indicates Adults Born Preterm International Collaboration; RECAP, Research on European Children and Adults Born Preterm; and VPT/VLBW, very preterm or very low birth weight.
The 8 IPD cohorts were from 7 high-income countries (Australia,34 Finland,29,30 Germany,8 Ireland,7 New Zealand,32 Norway,31 and the United Kingdom7,33); 6 of the studies were regional,8,29,30,31,33,34 and 2 were national.7,32 The mean (SD) gestational age at birth was 28.3 (2.8) weeks among VPT/VLBW participants and (mean [SD] gestational age was not available for term-born participants because some participants were recruited in childhood or adulthood), and birth years ranged from 1978 to 1995. The mean (SD) age at IQ assessment was 24.4 (4.6) years among VPT/VLBW participants and 24.8 (4.3) years among term-born participants. Among VPT/VLBW participants, more recent birth year (post-1978) was associated with lower gestational age (difference per year, −0.32 weeks; 95% CI, −0.60 to −0.04 weeks) and lower birth weight (difference, −29.85 g; 95% CI, −58.78 to −0.91 g) (eTable 3 and eTable 4 in the Supplement). In total, 557 VPT/VLBW participants (52.2%) and 606 term-born participants (56.8%) were women (eTable 5 and eTable 6 in the Supplement).
Integrity and Risk of Bias
Based on the Newcastle-Ottawa Scale27 (eTable 2 in the Supplement), the mean (SD) study quality score was 7.9 (0.6), and studies were rated highly with regard to representativeness, ascertainment of exposure, and assessment of outcomes. However, studies differed in inclusion criteria and attrition rates among VPT/VLBW participants, which were higher than 50% in 47,8,29,30 of 8 cohorts (Table 1).
Results of Syntheses
IPD Meta-analysis of All Participants
The analysis of all participants from IPD cohorts7,8,29,30,31,32,33,34 indicated that mean IQ z scores among VPT/VLBW participants were 0.78 SD (95% CI, −0.90 to −0.66 SD) lower than those of term-born participants. When sex and maternal educational level were included, the estimate of the association of VPT birth or VLBW with IQ scores was minimally reduced, from a difference of −0.78 SD to a difference of −0.74 SD (95% CI, −0.85 to −0.63 SD). Excluding participants with childhood NSI reduced the IQ difference from −0.78 SD to −0.65 SD (95% CI, −0.76 to −0.55 SD). With regard to neonatal morbidities, the presence of any grade of IVH among VPT/VLBW participants was associated with a larger difference in IQ scores than no IVH (−0.99 SD [95% CI, −1.19 to −0.79 SD] vs −0.70 SD [95% CI, −0.84 to −0.57 SD], respectively). A similar difference among VPT/VLBW participants with and without neonatal BPD was also found (−0.93 SD [95% CI, −1.10 to −0.76] vs −0.67 SD [95% CI, −0.80 to −0.55], respectively).
IPD Analysis of Antecedent Risk Factors
Table 2 shows the results of the IPD meta-analysis examining the association of neonatal factors, maternal educational level, and cohort factors with IQ scores among VPT/VLBW participants. Significant associations with IQ z scores in the multivariable analysis were gestational age (score difference per week of gestation, 0.11; 95% CI, 0.07-0.14), birth weight z score (score difference per 1.0 SD, 0.21; 95% CI, 0.14-0.28), the presence of neonatal BPD (score difference, −0.16; 95% CI, −0.30 to −0.02) or any grade of IVH (score difference, −0.19; 95% CI, −0.33 to −0.05), and maternal educational level (score difference, 0.26; 95% CI, 0.17-0.35) (Table 2). These findings indicated, for example, that among VPT/VLBW participants, each extra week of gestation was associated with an increase in IQ z score of 0.11, which was equivalent to 1.65 IQ points. In contrast, neither sex nor singleton or multiple birth significantly altered adult IQ scores among VPT/VLBW participants. In addition, none of the cohort-level factors were significant in the multivariable analysis. The association with birth year was significant in the univariable analysis (score difference, −0.02; 95% CI, −0.03 to 0), which suggested that more recent birth year was associated with lower IQ in adulthood.
Table 2. Univariable and Multivariable Analyses of Association of Individual- and Cohort-Level Factors With IQ z Scores Among Adults With Very Preterm Birth or Very Low Birth Weight (N = 1068).
| Factor | 1-Stage univariable analysis | 1-Stage multivariable analysis | ||
|---|---|---|---|---|
| IQ z score estimate (95% CI) | P value | IQ z score estimate (95% CI) | P value | |
| Individual-level | ||||
| Gestational age, wk | 0.04 (0.02 to 0.06) | <.001 | 0.11 (0.07 to 0.14) | <.001 |
| Male sex | 0.07 (−0.05 to 0.20) | .26 | 0.09 (−0.03 to 0.20) | .16 |
| Birth weight z score per 1 SD | 0.05 (−0.01 to 0.11) | .08 | 0.21 (0.14 to 0.28) | <.001 |
| Maternal educational levela | 0.25 (0.17 to 0.34) | <.001 | 0.26 (0.17 to 0.35) | <.001 |
| Presence of neonatal BPDb | −0.37 (−0.51 to −0.23) | <.001 | −0.16 (−0.30 to −0.02) | .02 |
| BPD defined as oxygen after 28 d postbirthc | −0.34 (−0.56 to −0.12) | .003 | NA | NA |
| BPD defined as oxygen after 36 wk postmenstrual agec | −0.40 (−0.56 to −0.23) | <.001 | NA | NA |
| Presence of neonatal IVH | ||||
| Any graded | −0.27 (−0.40 to −0.13) | <.001 | −0.19 (−0.33 to −0.05) | .007 |
| Grade 3 or 4e | −0.66 (−0.92 to −0.41) | <.001 | NA | NA |
| Multiple birthf | 0.01 (−0.13 to 0.15) | .86 | 0.00 (−0.13 to 0.14) | .95 |
| Cohort-level | ||||
| Attrition, % | ||||
| VPT/VLBW participants | 0 (−0.01 to 0) | .08 | −0.02 (−0.06 to 0.02) | .32 |
| VPT/VLBW participants with childhood NSI | 0 (−0.01 to 0) | .25 | 0.02 (−0.03 to 0.08) | .39 |
| Mean cohort age at IQ assessment, y | 0 (−0.01 to 0.02) | .60 | −0.10 (−0.26 to 0.06) | .28 |
| Year of birth | −0.02 (−0.03 to 0) | .02 | −0.03 (−0.11 to 0.05) | .48 |
Abbreviations: BPD, bronchopulmonary dysplasia; IVH, intraventricular hemorrhage; NA, not applicable; NSI, neurosensory impairment; VPT/VLBW, very preterm or very low birth weight.
Level 1 indicates low, 2 indicates medium, and 3 indicates high.
Compared with participants with no BPD. Participants from the Kroll et al33 cohort were not included in the univariable estimate, but their BPD values were imputed for the multivariable estimate.
The Heinonen et al,29 Madzwamuse et al,8 Pyhala et al,30 and Lærum et al31 studies used the criterion of 28 days’ after birth. The Linsell et al,7 Darlow et al,32 and Doyle et al34 studies used the criterion of 36 weeks’ postmenstrual age.
Compared with participants with no neonatal IVH.
Compared with all other grades. Participants in the Darlow et al study32 could not have IVH harmonized into grade 3 or 4 and were therefore not included in the subanalysis.
Compared with singleton birth.
Sensitivity Meta-analysis
The PubMed search of 413 records identified 4 additional non-RECAP and non-APIC cohorts41,42,43,44,45 with extractable adult IQ data. Adding the summary data from the Hack study45 produced 5 non-IPD cohorts and 8 IPD cohorts (Figure 1). Characteristics of the non-IPD cohorts are shown in eTable 7 in the Supplement.
Using aggregate data, the SMD between VPT/VLBW and term-born participants was −0.61 (95% CI, −0.93 to −0.29) in non-IPD cohorts41,42,43,44,45 and −0.84 (95% CI, −0.97 to −0.71) in IPD cohorts7,8,29,30,31,32,33,34 (Figure 2). According to the results of the Cochran Q test, this finding suggested no significant differences between the IPD and non-IPD cohorts (Q = 1.80; P = .18). However, the heterogeneity was larger among non-IPD cohorts (I2 = 75%) compared with IPD cohorts (I2 = 41%).
Figure 2. Aggregate Meta-analysis Comparing IQ Performance in Independent Participant Data (IPD) vs Non-IPD Cohorts of Adults Who Were Born Very Preterm or With Very Low Birth Weight.
Diamonds represent pooled estimates from either the IPD or non-IPD subgroup analysis or from all cohorts; diamond size indicates the 95% CI for the pooled estimate. The arrow indicates that the lower 95% CI (1.54) for the Linsell et al EPICure study7 is further than the axis limit of 1.5. Horizontal lines represent the 95% CIs of the estimates for each cohort. Box size represents the weighting given to the study. SMD indicates standardized mean difference.
Discussion
Summary of Evidence
This IPD meta-analysis examined the association between VPT birth or VLBW and adult IQ. Among 8 cohorts contributing IPD,7,8,29,30,31,32,33,34 VPT/VLBW participants scored 0.78 SD lower in IQ score than term-born participants, which is equivalent to a between-group difference of approximately 12 IQ points. This substantial difference was marginally reduced after adjustment for sex and maternal educational level. Even when participants with childhood NSI were excluded (which also removed those with low childhood IQ), the IQ score difference between VPT/VLBW and term-born participants was 0.65 SD (equivalent to 9.8 IQ points). The addition of cohorts for which IPD were not available41,42,43,44,45 did not substantially alter the findings. Among VPT/VLBW participants, individual-level factors associated with lower IQ were earlier gestational age, lower birth weight z score, the presence of neonatal BPD or IVH, and lower maternal educational level.
The IQ score difference of −0.78 SD between VPT/VLBW and term-born participants is a larger standardized difference than that reported for other functional outcomes, such as mental and physical health and social functioning.46 The IQ differences between VPT/VLBW and term-born adults found in this study are also similar to those previously reported in studies of childhood IQ.9,10,11,12 Three prospective studies found moderate to high stability in IQ scores from childhood to adulthood among VPT/VLBW individuals.7,32,47 The adult cohorts in the present IPD analysis were followed up for decades, producing a higher risk of selective attrition over a long period. Individuals who are more socially disadvantaged or who have NSI are more frequently lost to follow-up,48 which may be associated with the smaller difference in IQ between VPT/VLBW and term-born participants.49 However, the cohort differences in rates of attrition among all VPT/VLBW participants or among VPT/VLBW participants who specifically had childhood NSI were not associated with IQ, nor was the age at IQ assessment. Furthermore, the association between IQ and birth year was not significant after including individual-level factors in the multivariable analysis. This finding suggests little change in mean adult IQ scores among VPT/VLBW individuals born between 1978 and 1995 after adjustment for the lower birth weights and gestational ages among individuals born more recently. In more recent VPT/VLBW cohorts, no improvements in childhood IQ by birth year have been reported.12 Improvements in IQ have also not been observed in successive cohorts of children born extremely preterm from the same regions.50,51 Thus, given the stability of IQ over time among these cohorts, changes in neonatal care and reduced mortality52 do not appear to have translated into long-term improvements in IQ among VPT/VLBW individuals during this period.
For individual-level factors (Table 2), even when adjusting for other neonatal factors and maternal educational levels, a dose-response association was found between gestational age and IQ, replicating individual study findings.53,54 The association of neonatal IVH and BPD with lower IQ is also consistent with previous meta-analyses of IQ in childhood and individual studies of IQ in adulthood.12,55 After other factors were controlled for, neonatal BPD was associated with a mean reduction in IQ of 2.4 points (95% CI, −4.5 to −0.3 points; difference in z score, −0.16), and the presence of any grade of IVH was associated with a mean reduction in IQ of 2.9 points (95% CI, −5.0 to −0.8 points; difference in z score, −0.19) (Table 2). Severe IVH (grades 3-4) was only investigated in a univariable analysis that did not include all cohorts; however, severe IVH was associated with a mean decrease in IQ of 9.9 points (95% CI, −13.8 to −6.2 points; difference in z score, −0.66). However, this finding warrants cautious interpretation because other neonatal factors and maternal educational levels were not controlled for. Birth weight z scores had a significant association with IQ after other factors were controlled for. Results from the multivariable model suggest that a birth weight of −2 SD for gestational age is associated with a decrease of 6.3 IQ points (95% CI, −8.4 to −4.2 points) compared with a birth weight that is appropriate for gestational age. This finding provides additional support for the association between low birth weight for gestational age and lower IQ in adulthood among VPT/VLBW individuals.56
In contrast to neonatal factors, maternal educational levels and similar factors have been largely overlooked in research on VPT birth or VLBW and outcomes.17 Compared with low maternal educational level, VPT/VLBW participants who had mothers with medium or high educational levels had IQ scores that were generally 0.26 SD and 0.52 SD (3.9 and 7.8 IQ points) higher, respectively. These associations are equivalent in extent to those associated with serious neonatal complications (ie, BPD and IVH). The association of maternal educational level with adult IQ may reflect an amalgam of different factors. These factors may include genetic traits,57 maternal smoking,58 breastfeeding rates,59 and parental behaviors.55 Some factors could be modified postnatally and have been reported to have implications for academic achievement and development among both the general population and VPT/VLBW groups.60,61
Strengths and Limitations
This study has several strengths. The harmonization and use of IPD to assess neonatal factors and maternal educational levels, the presence of childhood NSI, and adult IQ scores for 8 cohorts of VPT/VLBW participants allowed for reliable comparison across cohorts. In addition, we tested a range of specific cohort factors, which is a challenging task in an aggregate meta-analysis because these details are rarely available in published studies.
The study also has limitations. These include the differences in cohorts with regard to eligibility criteria, such as the stricter inclusion criterion of less than 26 weeks’ gestational age in the Linsell et al study,7 the use of maternal educational level rather than broader factors (such as socioeconomic status or combined parental educational level), and the different methods used for recruiting participants for the control groups. Individuals in the control groups were typically recruited in infancy; however, in some cohorts, recruitment occurred in childhood or adulthood, and neonatal data were unavailable. Thus, we could not evaluate whether factors such as birth weight z scores are similarly associated with IQ among term-born participants. Given that the mean age at assessment was 24.6 years, the findings of the present study reflect IQ in young adulthood only.
Conclusions
Adults who were born VPT/VLBW had IQ scores that were a mean of 12 points lower than adults who were term born. This finding is similar to those reported in meta-analyses of IQ in childhood7,9,10,11,12,47 despite the present study’s greater risk of selective attrition owing to a longer follow-up period. The provision of antenatal and neonatal care that is associated with reductions in BPD and IVH62,63 and parenting or educational interventions that help to decrease the social disparities associated with maternal educational levels61 may improve cognitive outcomes among adults who were VPT or VLBW.
eTable 1. Childhood Neurosensory Impairment in VPT/VLBW Participants From Each IPD Cohort
eTable 2. Newcastle Ottawa Criteria and Ratings for Each IPD Cohort
eTable 3. Linear Mixed Model Demonstrating Reducing Gestational Age by Birth Year Among VPT/VLBW Participants
eTable 4. Linear Mixed Model Demonstrating Reducing Birth Weight by Birth Year Among VPT/VLBW Participants
eTable 5. IQ and Demographic Information of All Participants From Each IPD Cohort
eTable 6. Neonatal and Demographic Data for VPT/VLBW Participants From Each IPD Cohort
eTable 7. Study Characteristics of VPT/VLBW Cohorts Not Included in the IPD Meta-analysis
eReferences
References
- 1.Sternberg RJ. Intelligence. In: Holyoak KJ, Morrison RG, eds. The Cambridge Handbook of Thinking and Reasoning. Cambridge University Press; 2005:751-773. [Google Scholar]
- 2.Deary IJ, Whiteman MC, Starr JM, Whalley LJ, Fox HC. The impact of childhood intelligence on later life: following up the Scottish mental surveys of 1932 and 1947. J Pers Soc Psychol. 2004;86(1):130-147. doi: 10.1037/0022-3514.86.1.130 [DOI] [PubMed] [Google Scholar]
- 3.Basten M, Jaekel J, Johnson S, Gilmore C, Wolke D. Preterm birth and adult wealth: mathematics skills count. Psychol Sci. 2015;26(10):1608-1619. doi: 10.1177/0956797615596230 [DOI] [PubMed] [Google Scholar]
- 4.Hegelund ER, Flensborg-Madsen T, Dammeyer J, Mortensen EL. Low IQ as a predictor of unsuccessful educational and occupational achievement: a register-based study of 1,098,742 men in Denmark 1968–2016. Intelligence. 2018;71:46-53. doi: 10.1016/j.intell.2018.10.002 [DOI] [Google Scholar]
- 5.Strenze T. Intelligence and socioeconomic success: a meta-analytic review of longitudinal research. Intelligence. 2007;35(5):401-426. doi: 10.1016/j.intell.2006.09.004 [DOI] [Google Scholar]
- 6.Hack M. Young adult outcomes of very–low-birth-weight children. Semin Fetal Neonatal Med. 2006;11(2):127-137. doi: 10.1016/j.siny.2005.11.007 [DOI] [PubMed] [Google Scholar]
- 7.Linsell L, Johnson S, Wolke D, et al. Cognitive trajectories from infancy to early adulthood following birth before 26 weeks of gestation: a prospective, population-based cohort study. Arch Dis Child. 2018;103(4):363-370. doi: 10.1136/archdischild-2017-313414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madzwamuse SE, Baumann N, Jaekel J, Bartmann P, Wolke D. Neuro-cognitive performance of very preterm or very low birth weight adults at 26 years. J Child Psychol Psychiatry. 2015;56(8):857-864. doi: 10.1111/jcpp.12358 [DOI] [PubMed] [Google Scholar]
- 9.Allotey J, Zamora J, Cheong-See F, et al. Cognitive, motor, behavioural and academic performances of children born preterm: a meta-analysis and systematic review involving 64 061 children. BJOG. 2018;125(1):16-25. doi: 10.1111/1471-0528.14832 [DOI] [PubMed] [Google Scholar]
- 10.Brydges CR, Landes JK, Reid CL, Campbell C, French N, Anderson M. Cognitive outcomes in children and adolescents born very preterm: a meta-analysis. Dev Med Child Neurol. 2018;60(5):452-468. doi: 10.1111/dmcn.13685 [DOI] [PubMed] [Google Scholar]
- 11.Sentenac M, Boutron I, Draper ES, et al. Defining very preterm populations for systematic reviews with meta-analyses. JAMA Pediatr. 2020;174(10):997-999. doi: 10.1001/jamapediatrics.2020.0956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Twilhaar ES, Wade RM, de Kieviet JF, van Goudoever JB, Elburg RM, Oosterlaan J. Cognitive outcomes of children born extremely or very preterm since the 1990s and associated risk factors: a meta-analysis and meta-regression. JAMA Pediatr. 2018;172(4):361-367. doi: 10.1001/jamapediatrics.2017.5323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kormos CE, Wilkinson AJ, Davey CJ, Cunningham AJ. Low birth weight and intelligence in adolescence and early adulthood: a meta-analysis. J Public Health (Oxf). 2014;36(2):213-224. doi: 10.1093/pubmed/fdt071 [DOI] [PubMed] [Google Scholar]
- 14.Benavente-Fernandez I, Synnes A, Grunau RE, et al. Association of socioeconomic status and brain injury with neurodevelopmental outcomes of very preterm children. JAMA Netw Open. 2019;2(5):e192914. doi: 10.1001/jamanetworkopen.2019.2914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linsell L, Malouf R, Morris J, Kurinczuk JJ, Marlow N. Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight: a systematic review. JAMA Pediatr. 2015;169(12):1162-1172. doi: 10.1001/jamapediatrics.2015.2175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah P, Kingdom J. Long-term neurocognitive outcomes of SGA/IUGR infants. Obstet Gynaecol Reprod Med. 2011;21(5):142-146. doi: 10.1016/j.ogrm.2011.02.004 [DOI] [Google Scholar]
- 17.Wolke D. Is social inequality in cognitive outcomes increased by preterm birth–related complications? JAMA Netw Open. 2019;2(5):e192902. doi: 10.1001/jamanetworkopen.2019.2902 [DOI] [PubMed] [Google Scholar]
- 18.Lambert PC, Sutton AJ, Abrams KR, Jones DR. A comparison of summary patient-level covariates in meta-regression with individual patient data meta-analysis. J Clin Epidemiol. 2002;55(1):86-94. doi: 10.1016/S0895-4356(01)00414-0 [DOI] [PubMed] [Google Scholar]
- 19.Tierney JF, Vale C, Riley R, et al. Individual participant data (IPD) meta-analyses of randomised controlled trials: guidance on their use. PLoS Med. 2015;12(7):e1001855. doi: 10.1371/journal.pmed.1001855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Research on European Children and Adults Born Preterm website. RECAP Preterm; 2021 Accessed July 9, 2020. https://recap-preterm.eu
- 21.APIC: Adults Born Preterm International Collaboration website. APIC; 2021. Accessed July 9, 2020. https://www.apic-preterm.org
- 22.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 23.Trahan LH, Stuebing KK, Fletcher JM, Hiscock M. The Flynn effect: a meta-analysis. Psychol Bull. 2014;140(5):1332-1360. doi: 10.1037/a0037173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529-534. doi: 10.1016/S0022-3476(78)80282-0 [DOI] [PubMed] [Google Scholar]
- 25.Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59. doi: 10.1186/1471-2431-13-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.UNESCO Institute of Statistics . International Standard Classification of Education: ISCED 2011. UNESCO Institute of Statistics; 2012. [Google Scholar]
- 27.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Hospital Research Institute; 2012. Accessed September 1, 2020. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 28.van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 29.Heinonen K, Lahti J, Sammallahti S, et al. Neurocognitive outcome in young adults born late-preterm. Dev Med Child Neurol. 2018;60(3):267-274. doi: 10.1111/dmcn.13616 [DOI] [PubMed] [Google Scholar]
- 30.Pyhala R, Lahti J, Heinonen K, et al. Neurocognitive abilities in young adults with very low birth weight. Neurology. 2011;77(23):2052-2060. doi: 10.1212/WNL.0b013e31823b473e [DOI] [PubMed] [Google Scholar]
- 31.Lærum AMW, Reitan SK, Evensen KAI, et al. Psychiatric symptoms and risk factors in adults born preterm with very low birthweight or born small for gestational age at term. BMC Psychiatry. 2019;19(1):223. doi: 10.1186/s12888-019-2202-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Darlow BA, Woodward LJ, Levin KJ, Melzer T, Horwood LJ. Perinatal and childhood predictors of general cognitive outcome at 28 years in a very–low-birthweight national cohort. Dev Med Child Neurol. 2020;62(12):1423-1428. doi: 10.1111/dmcn.14649 [DOI] [PubMed] [Google Scholar]
- 33.Kroll J, Karolis V, Brittain PJ, et al. Real-life impact of executive function impairments in adults who were born very preterm. J Int Neuropsychol Soc. 2017;23(5):381-389. doi: 10.1017/S1355617717000169 [DOI] [PubMed] [Google Scholar]
- 34.Doyle LW, Cheong JLY, Burnett A, Roberts G, Lee KJ, Anderson PJ; Victorian Infant Collaborative Study Group . Biological and social influences on outcomes of extreme-preterm/low–birth weight adolescents. Pediatrics. 2015;136(6):e1513-e1520. doi: 10.1542/peds.2015-2006 [DOI] [PubMed] [Google Scholar]
- 35.Bates D, Machler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1-48. doi: 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 36.Balduzzi S, Rucker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153-160. doi: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suikkanen J, Miettola S, Heinonen K, et al. Reaction times, learning, and executive functioning in adults born preterm. Pediatr Res. 2021;89(1):198-204. doi: 10.1038/s41390-020-0851-4 [DOI] [PubMed] [Google Scholar]
- 38.Weisglas-Kuperus N, Hille ETM, Duivenvoorden HJ, et al. ; Dutch POPS-19 Collaborative Study Group . Intelligence of very preterm or very low birthweight infants in young adulthood. Arch Dis Child Fetal Neonatal Ed. 2009;94(3):F196-F200. doi: 10.1136/adc.2007.135095 [DOI] [PubMed] [Google Scholar]
- 39.Saigal S, Ferro MA, Van Lieshout RJ, Schmidt LA, Morrison KM, Boyle MH. Health-related quality of life trajectories of extremely low birth weight survivors into adulthood. J Pediatr. 2016;179:68-73. doi: 10.1016/j.jpeds.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 40.Doyle LW, Faber B, Callanan C, Morley R. Blood pressure in late adolescence and very low birth weight. Pediatrics. 2003;111(2):252-257. doi: 10.1542/peds.111.2.252 [DOI] [PubMed] [Google Scholar]
- 41.Hallin AL, Hellstrom-Westas L, Stjernqvist K. Follow-up of adolescents born extremely preterm: cognitive function and health at 18 years of age. Acta Paediatr. 2010;99(9):1401-1406. doi: 10.1111/j.1651-2227.2010.01850.x [DOI] [PubMed] [Google Scholar]
- 42.Lefebvre F, Mazurier E, Tessier R. Cognitive and educational outcomes in early adulthood for infants weighing 1000 grams or less at birth. Acta Paediatr. 2005;94(6):733-740. doi: 10.1111/j.1651-2227.2005.tb01973.x [DOI] [PubMed] [Google Scholar]
- 43.Constable RT, Vohr BR, Scheinost D, et al. A left cerebellar pathway mediates language in prematurely-born young adults. Neuroimage. 2013;64:371-378. doi: 10.1016/j.neuroimage.2012.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stålnacke J, Lundequist A, Böhm B, Forssberg H, Smedler AC. Individual cognitive patterns and developmental trajectories after preterm birth. Child Neuropsychol. 2015;21(5):648-667. doi: 10.1080/09297049.2014.958071 [DOI] [PubMed] [Google Scholar]
- 45.Hack M, Flannery DJ, Schluchter M, Cartar L, Borawski E, Klein N. Outcomes in young adulthood for very–low-birth-weight infants. N Engl J Med. 2002;346(3):149-157. doi: 10.1056/NEJMoa010856 [DOI] [PubMed] [Google Scholar]
- 46.Wolke D, Johnson S, Mendonca M. The life course consequences of very preterm birth. Annu Rev Dev Psychol. 2019;1:69-92. doi: 10.1146/annurev-devpsych-121318-084804 [DOI] [Google Scholar]
- 47.Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Preterm cognitive function into adulthood. Pediatrics. 2015;136(3):415-423. doi: 10.1542/peds.2015-0608 [DOI] [PubMed] [Google Scholar]
- 48.Wolke D, Sohne B, Ohrt B, Riegel K. Follow-up of preterm children: important to document dropouts. Lancet. 1995;345(8947):447. doi: 10.1016/S0140-6736(95)90425-5 [DOI] [PubMed] [Google Scholar]
- 49.Howe LD, Tilling K, Galobardes B, Lawlor DA. Loss to follow-up in cohort studies: bias in estimates of socioeconomic inequalities. Epidemiology. 2013;24(1):1-9. doi: 10.1097/EDE.0b013e31827623b1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheong JLY, Anderson PJ, Burnett AC, et al. ; Victorian Infant Collaborative Study Group . Changing neurodevelopment at 8 years in children born extremely preterm since the 1990s. Pediatrics. 2017;139(6):e20164086. doi: 10.1542/peds.2016-4086 [DOI] [PubMed] [Google Scholar]
- 51.Marlow N, Ni Y, Lancaster R, et al. No change in neurodevelopment at 11 years after extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. Published online February 17, 2021. doi: 10.1136/archdischild-2020-320650 [DOI] [PubMed] [Google Scholar]
- 52.Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Analg. 2015;120(6):1337-1351. doi: 10.1213/ANE.0000000000000705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wolke D, Strauss VYC, Johnson S, Gilmore C, Marlow N, Jaekel J. Universal gestational age effects on cognitive and basic mathematic processing: 2 cohorts in 2 countries. J Pediatr. 2015;166(6):1410-1416. doi: 10.1016/j.jpeds.2015.02.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kroll J, Karolis V, Brittain PJ, et al. Systematic assessment of perinatal and socio-demographic factors associated with IQ from childhood to adult life following very preterm birth. Intelligence. 2019;77:101401. doi: 10.1016/j.intell.2019.101401 [DOI] [Google Scholar]
- 55.Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Neonatal predictors of cognitive ability in adults born very preterm: a prospective cohort study. Dev Med Child Neurol. 2017;59(5):477-483. doi: 10.1111/dmcn.13380 [DOI] [PubMed] [Google Scholar]
- 56.Eves R, Mendonça M, Bartmann P, Wolke D. Small for gestational age–cognitive performance from infancy to adulthood: an observational study. BJOG. 2020;127(13):1598-1606. doi: 10.1111/1471-0528.16341 [DOI] [PubMed] [Google Scholar]
- 57.Torres DD. Understanding how family socioeconomic status mediates the maternal intelligence–child cognitive outcomes relationship: a moderated mediation analysis. Biodemography Soc Biol. 2013;59(2):157-177. doi: 10.1080/19485565.2013.833804 [DOI] [PubMed] [Google Scholar]
- 58.Rahu K, Rahu M, Pullmann H, Allik J. Effect of birth weight, maternal education and prenatal smoking on offspring intelligence at school age. Early Hum Dev. 2010;86(8):493-497. doi: 10.1016/j.earlhumdev.2010.06.010 [DOI] [PubMed] [Google Scholar]
- 59.Brion MJA, Lawlor DA, Matijasevich A, et al. What are the causal effects of breastfeeding on IQ, obesity and blood pressure? evidence from comparing high-income with middle-income cohorts. Int J Epidemiol. 2011;40(3):670-680. doi: 10.1093/ije/dyr020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolke D, Jaekel J, Hall J, Baumann N. Effects of sensitive parenting on the academic resilience of very preterm and very low birth weight adolescents. J Adolesc Health. 2013;53(5):642-647. doi: 10.1016/j.jadohealth.2013.06.014 [DOI] [PubMed] [Google Scholar]
- 61.Shah R, Kennedy S, Clark MD, Bauer SC, Schwartz A. Primary care–based interventions to promote positive parenting behaviors: a meta-analysis. Pediatrics. 2016;137(5):e20153393. doi: 10.1542/peds.2015-3393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taylor LK, Lee YYC, Lim K, Simpson JM, Roberts CL, Morris J. Potential prevention of small for gestational age in Australia: a population-based linkage study. BMC Pregnancy Childbirth. 2013;13:210. doi: 10.1186/1471-2393-13-210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gien J, Kinsella JP. Pathogenesis and treatment of bronchopulmonary dysplasia. Curr Opin Pediatr. 2011;23(3):305-313. doi: 10.1097/MOP.0b013e328346577f [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Childhood Neurosensory Impairment in VPT/VLBW Participants From Each IPD Cohort
eTable 2. Newcastle Ottawa Criteria and Ratings for Each IPD Cohort
eTable 3. Linear Mixed Model Demonstrating Reducing Gestational Age by Birth Year Among VPT/VLBW Participants
eTable 4. Linear Mixed Model Demonstrating Reducing Birth Weight by Birth Year Among VPT/VLBW Participants
eTable 5. IQ and Demographic Information of All Participants From Each IPD Cohort
eTable 6. Neonatal and Demographic Data for VPT/VLBW Participants From Each IPD Cohort
eTable 7. Study Characteristics of VPT/VLBW Cohorts Not Included in the IPD Meta-analysis
eReferences