Abstract
OBJECTIVES:
Hypertension increases the risk of developing Alzheimer’s disease or related dementias. This pilot study’s purpose was to examine the feasibility and acceptability of a novel intervention, Mindfulness in Motion (MIM) and Dietary Approaches to Stop Hypertension DASH [MIM DASH]), to improve diet, mindfulness, stress, and systolic blood pressure (BP) in older African Americans with mild cognitive impairment (MCI) and hypertension.
DESIGN:
Cluster randomized controlled trial.
SETTING:
Intergenerational community center in a large metropolitan area.
PARTICIPANTS:
African Americans with MCI and hypertension. Participants were divided into six groups randomized 1:1:1 to the MIM DASH group, attention only (non-hypertensive education) group, or true control group. The MIM DASH and attention only interventions were delivered in 8-weekly 2 hour group sessions. MIM included mindful movements from chair/standing, breathing exercises, and guided meditation. The DASH component used a critical thinking approach of problem solving, goal setting, reflection, and self-efficacy. The true control group received a DASH pamphlet at the end.
MEASUREMENTS:
Feasibility was tracked through enrollment and attendance records; acceptability was assessed through interviews. Blood pressure was measured using the Omron HEM-907XL Monitor. Dietary intake was measured by DASH-Q. Mindfulness was measured by the Cognitive and Affective Mindfulness Scale. Stress was measured by the Perceived Stress Scale. MCI was determined using the Self-Administered Gerocognitive Examination. Data were collected at baseline and 3-months.
RESULTS:
Median session attendance was 6 for the MIM DASH group and 7 for the attention only group. There were no changes in diet, mindfulness, or stress. There was a clinically significant reduction in systolic BP in the MIM DASH group (−7.2mm Hg) relative to the attention only group (−.7), and no change between the MIM DASH and true control groups.
CONCLUSION:
Results indicate that the MIM DASH intervention was feasible and culturally acceptable in African Americans with hypertension and MCI.
Keywords: African Americans/Blacks, systolic blood pressure, non-pharmacological, mindfulness, diet
INTRODUCTION
African Americans have a greater risk of late-life cognitive decline and essential hypertension compared to non-Hispanic Whites. There is a threefold increase of developing Alzheimer’s disease and other dementias among African Amerians.1 African Americans are also at greater risk for essential hypertension, with studies linking facets of heart health such as systolic blood pressure to and cognitive decline in African Americans.2,3 Several qualitative studies have shown the benefits of mindfulness in African Americans to improve depressive symptoms, prediabetes, stress, and blood pressure (BP).4–6 While these studies have added to the extant literature, there is a need for quantitative studies to further inform the field.7–9 The purpose of this pilot study was to examine the feasibility and acceptability to deliver a novel Mindfulness in Motion10,11 plus DASH (MIM DASH) intervention to improve diet, mindfulness, and reduce stress and systolic blood pressure in African American older adults with mild cognitive impairment (MCI) and hypertension. Our hypothesis was that MIM DASH would be feasible and acceptable and compared to the control groups (attention only and true control), participants in MIM DASH would have improved systolic BP, diet, mindfulness affect and stress.
METHODS
Study Design and Participants
This was a cluster randomized controlled trial of community-dwelling African American older adults from a Midwestern urban setting. Participants were divided into 6 groups (6–7 participants/group). Groups, as the units of randomization, were randomized 1:1:1 to one of three arms: MIM DASH (n=2 groups), non-hypertensive education attention only (n=2 groups), or true control (2 groups). Inclusion criteria were (1) diagnosis of hypertension and (2) MCI indicated by a score of 10–17 on the Self-Administered Gerocognitive Examination (SAGE),12 specifically designed to screen for MCI and early dementia. SAGE covers cognitive domains of orientation, language, memory, executive function, calculations, abstraction, and visuospatial abilities. The psychometric properties have been well validated with a 0.84 Spearman rank correlation between SAGE and a 1-day neuropsychiatric battery.12 This study was approved by the Institutional Review Board at a large Midwestern U.S. academic medical center prior to enrollment of study participants.
Intervention group
The MIM DASH intervention was delivered by the investigators (KDW, MK, IA) in a group format of 8-weekly sessions lasting 2 hours each. Weekly group sessions included a didactic presentation on stress, mindfulness, and the somatic mind/body connection (Figure 1). Each participant received a compact disk player with mindfulness recordings as well as a weekly diary to document study activities. Participants were instructed to perform daily 20 minute individual sessions at least 5 times a week. Each participant was asked to track his/her daily meditation practice in their diary.
Figure 1.
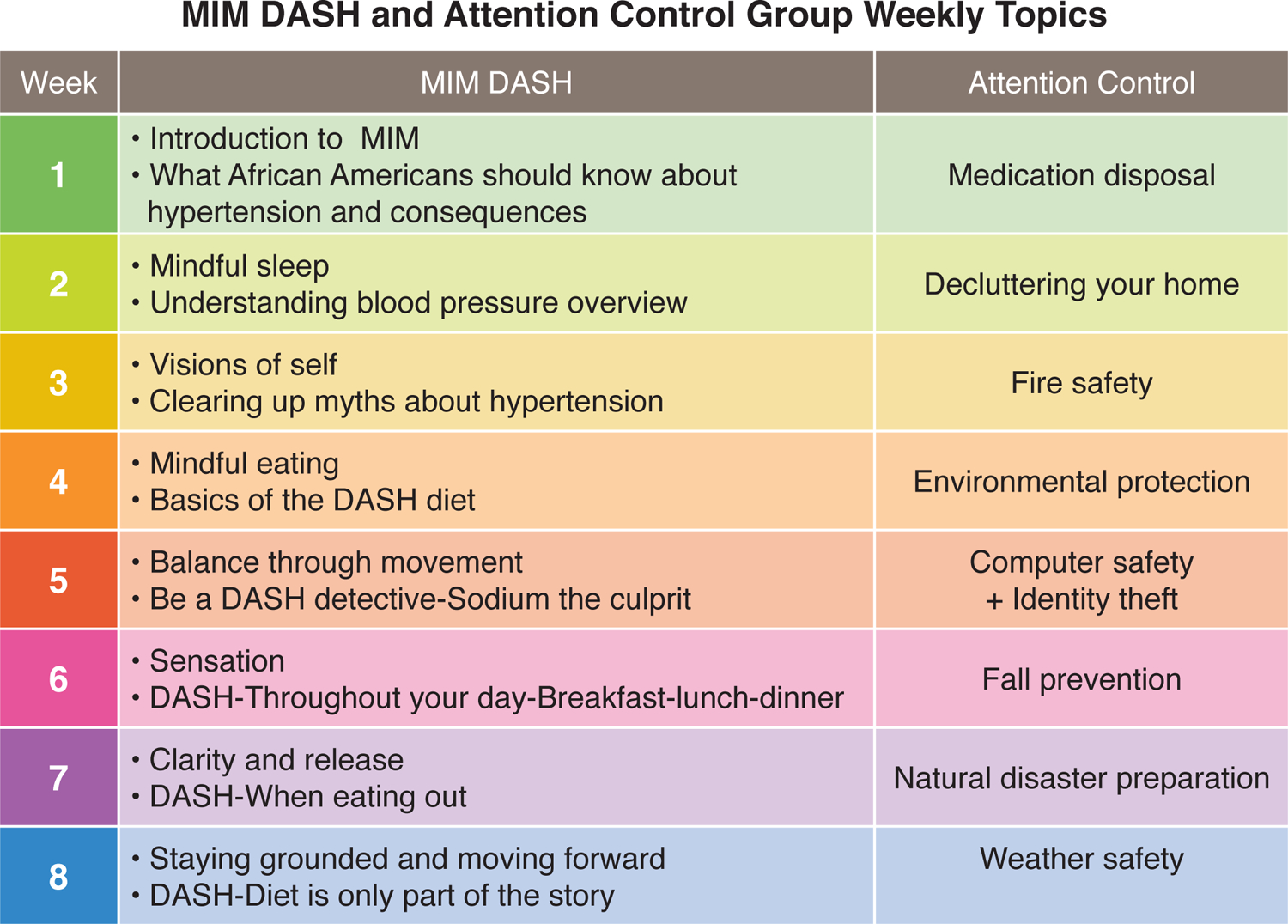
Provides is an Infographic of the weekly topics for the Mindfulness in Motion (MIM) plus the Dietary Approaches to Stop Hypertension (MIM DASH) intervention and the attention only groups.
The DASH portion of MIM DASH focused on education to limit sodium, sweets, sugary beverages, and red meats in preference for foods that were low in saturated fats, and rich in potassium, calcium, magnesium, fiber, and protein. Education included taking traditional “Soul” food dishes and adapted the recipes to meet the DASH dietary guidelines. A combination of didactic and experiential activities were utilized with the participants and included sampling foods, such as quinoa and tofu, that were not traditionally part of the “Soul” food diet. Participants were encouraged to complete a weekly homework assignment to practice the DASH diet in daily life. They also received an individual MyPlate13 displaying serving sizes and food groups comprising a balanced meal. Repetition of key concepts were embedded throughout the sessions to increase critical thinking and problem solving.
Attention only group
The attention only group met for eight, 2-hour sessions that covered non-hypertensive topics such as personal safety and fire prevention (Figure 1). The attention only and the MIM DASH groups were given healthy snacks and water at each meeting. Transportation and free parking were provided. All sessions were held in the community room of an intergenerational care center.
True control group
The true control group received no information between baseline and study measurements. At the conclusion of the study intervention, participants received a DASH pamphlet.
Measurements
All primary and secondary measures were collected by trained research assistants (separate from the attention only group research assistants) at baseline and 3 months. Prior to the 3 month follow-up, up to three phone calls were made to schedule the date, time, and place (home, clinic, or library) for data collection.
Primary outcomes
Feasibility was measured by enrollment rates, weekly session attendance rates, and retention rates.14 Interviews using open-ended questions were used to determine acceptability: (1) how well does the intervention fit within your routine and culture (2) what did you like the best about the sessions, and (3) what did you like least about the sessions.
Secondary outcomes
The secondary outcome measures were systolic (BP), dietary adherence, mindfulness affect, and perceived stress. Blood pressure was taken using an OMRON Hem 907XL IntelliSense Professional Digital Blood Pressure Monitor per protocol.15 The average of three BP results was recorded.
The DASH Questionnaire (DASH Q)16 has 11 items focused on the consumption of DASH foods (e.g., fruits, nuts, and vegetables) in the past seven days (Cronbach α = .83). The reference range for the DASH Q was 0–105 with higher scores indicating greater adherence to DASH diet. The Cognitive and Affective Mindfulness Scale (Cronbach α=.77)17 has 12 questions (reference range 0–48, higher scores indicate greater mindfulness affect) on a Likert scale regarding daily experiences such as “I rush through activities without being really attentive to them.” The Perceived Stress Scale has 10-items reference range 0–30 regarding stress over the past month (Cronbach α = 0.83).18 The cut point for moderate to high stress is ≥12 for persons age 65 and older.
Statistical Analysis
The feasibility data were analyzed using descriptive statistics to measure attendance per group. Descriptive statistics were used to examine the secondary outcomes (systolic BP, diet adherence, mindfulness affect, and perceived stress) among the intervention and attention control groups over time (baseline and 3 months). Next, mixed-effects linear modeling was used to estimate the between-group difference in each outcome. From the mixed-effects modeling, we derived estimates of the within-group difference of 3-months versus baseline measures and between-group (MIM DASH vs. attention only) difference in the change from baseline, adjusting for clustering from cluster randomization and repeated measures.
Since this was primarily a feasibility study, the sample size from this pilot study (13 per arm) did not have sufficient power to detect small-to-medium effect sizes for between-group difference (e.g., 34% power to detect a Cohen’s d of 0.5 with a two-sided significance level of 0.05). Therefore, we did not rely on statistical significance. Rather, we were interested whether the intervention could achieve a clinically meaningful significant reduction in systolic BP defined as ≥ 5mm Hg.19
RESULTS
Feasibility and Acceptability
The enrollment rate was 54% (Supplemental Figure S1); the majority were women (82%) and most had some college education (Table 1). There were no significant statistical differences between the groups per ANOVA. Median session attendance was 6 (M= 4.6, SD= 3.1) for the MIM DASH group and 7 for the attention only group (M= 6, SD= 1.9). The MIM DASH participants reported that the intervention was culturally acceptable and that the group practice of newly learned skills was beneficial. “I liked the whole thing.” “[I] Threw salt out of house.” The MIM DASH intervention was thought be beneficial to others. “[I] believe that this would gel with others and the plate [MyPlate13] should be given to kids too.” Three participants did not attend any MIM DASH sessions due to scheduling conflicts or reluctance to be in a group. Some participants disliked the small class size, limited number of men, and timing of sessions (Friday afternoons). All participants in the attention only group attended at least one session. We incorporated a reminder call system for the second true control group which improved retention for 3-month data collection (100%).
Table 1.
Participant characteristics at baseline for Mindfulness in Motion plus Dietary Approaches to Stop Hypertension (MIM DASH), Attention Only, and True Control groups.
| MIM DASH (n=13) |
Attention Control (n=13) |
True Control (n=12) |
|
|---|---|---|---|
| Demographics | |||
| Age in Years, mean (SD) |
74.0 (5.9) | 71.9 (3.9) | 70.8 (5.5) |
| Sex | |||
| Female | 12 (32.0%) | 9 (23.0%) | 10 (26.6%) |
| Male | 1 (3.0%) | 4 (9.4%) | 2 (6.0%) |
| Education | |||
| Below 12th grade | 4 (30.7%) | 2 (15.3%) | 0 (0.0%) |
| High school graduate/GED | 2 (15.3%) | 3 (23.3%) | 2 (16.6%) |
| Some college | 2 (15.3%) | 4 (30.7%) | 3 (25.1%) |
| Associate degree or higher | 5 (38.5%) | 4 (30.7%) | 7 (58.3%) |
| Monthly Income (U.S. dollars), mean (SD) |
1996.3 (1478.1) | 1588.3 (870.7) | 1596.1 (426.5) |
| Self-Administered Gerocognitive Examination (SAGE) Mean (Standard deviation) |
13.3 (3.5) | 14.1 (2.6) | 13.4 (3.8) |
| Number of chronic conditions, mean (SD) |
5 (1.3) | 4.5 (1.8) | 4.1(0.9) |
| Number of hypertension medications, mean (SD) | 2.1 (0.9) | 1.9 (1.2) | 1.8(1.0) |
| Systolic BP, mean (SD) | 133.6 (14.4) | 140.4 (28.3) | 139.6 (12.8) |
| Diastolic BP, mean (SD) | 75.6 (9.6) | 78.3 (12.1) | 76.3(13.3) |
Secondary outcomes
There were no statistically or clinically significant reductions or changes in secondary outcomes between MIM DASH and true control participants. There was a clinically significant reduction in systolic BP in the MIM DASH group as compared to the attention only group (−7.2 mm Hg versus −.7 mm Hg 95% CI 2.2 to 17.7). The reduction in diastolic blood pressure was not significant. The range of scores for the DASH-Q, perceived stress, and mindfulness were average to above average for these participants and none were significant post-intervention (Table 2).
Table 2.
Difference in Secondary Outcomes (systolic blood pressure, Dietary Approaches to Stop Hypertension [DASH] diet, mindfulness, and stress) in Mindfulness in Motion plus DASH (MIM DASH), Attention Control, and True Control Groups.
| MIM DASH Group, Mean (SD) | |||||
|---|---|---|---|---|---|
| Variable | Baseline (N=13) | 3 month (N=12) | Difference | ||
| Systolic BP | 133.6 (14.5) | 123.2 (14.5) | −10.4 (13.3) | ||
| Diastolic BP | 75.6 (9.7) | 71.5 (9.5) | −4.1 (7.9) | ||
| DASH-Q | 70.0 (12.0) | 68.4 (16.5) | −1.6 (10.8) | ||
| Mindful Affect | 32.1 (5.9) | 29.0 (9.1) | −3.1 (9.1) | ||
| Perceived Stress | 10.5 (7.1) | 11.7 (7.6) | +1.2 (4.9) | ||
| Attention Control Group, Mean (SD) | |||||
| Variable | Baseline (N=13) | 3 month (N=13) | Difference | ||
| Systolic BP | 140.4 (28.3) | 137.2 (25.3) | −3.2 (17.4) | ||
| Diastolic BP | 78.3 (12.1) | 75.5 (10.0) | −3.4 (8.5) | ||
| DASH-Q | 58.1 (11.1) | 58.3 (9.5) | 0.2 (4.2) | ||
| Mindful Affect | 33.7 (6.3) | 31.6 (3.8) | −2.1 (5.8) | ||
| Perceived Stress | 9.7 (6.1) | 10.5 (3.8) | 0.8 (7.4) | ||
| True Control Group, Mean (SD) | |||||
| Variable | Baseline (N=12) | 3 month (N=6) | Difference | ||
| Systolic BP | 139.6 (12.8) | 125.8 (11.9) | −13.8 (9.9) | ||
| Diastolic BP | 76.3(13.3) | 70.6 (17.2) | −5.7 (6.1) | ||
| DASH-Q | 69.1 (8.3) | 63.1 (65.5) | −6 (9.3) | ||
| Mindful Affect | 31.2 (6.0) | 35.1 (4.3) | 3.9 (5.7) | ||
| Perceived Stress | 16.1 (10.1) | 10.2 (8.0) | −5.9 (3.1) | ||
| MIM DASH versus Attention Only Group | |||||
| Variable | Difference-Difference Mean (95% CI) |
P = Value | |||
| Systolic BP | −7.2 (17.7, 2.2) | .12 | |||
| Diastolic BP | −.7 (−7.3, 4.3) | .60 | |||
| DASH-Q | 1.4 (−9.2, 5.2) | .57 | |||
| Mindful Affect | 1 (−6.4, 5.1) | .81 | |||
| Perceived Stress | .4 (−4.9, 3.2) | .68 | |||
| MIM DASH versus True Control | |||||
| Variable | Difference-Difference Mean (95% CI) |
P = Value | |||
| Systolic BP | 3.4 (−33.4, 17.9) | .29 | |||
| Diastolic BP | 2.3 (−7.6, 4.6 ) | .62 | |||
| DASH-Q | 4.3 (−9.5, 5.6) | .59 | |||
| Mindful Affect | −1.8 (−6.7, 5.4) | .82 | |||
| Perceived Stress | 4.7 (−5.1, 3.4) | .69 | |||
DISCUSSION
This pilot study was designed to examine the feasibility and acceptability of engaging African Americans who have hypertension and evidence of MCI in clinical research. Findings support that among this vulnerable group that the intervention is not only feasible and acceptable but also resulted in a clinically meaningful decrease in systolic BP. Similar to other studies of mindfulness interventions for African Americans, the intervention occurred in a familiar location, connected mindfulness with the concept of self, and used culturally familiar language.4,8,20 Median attendance rates for participants in the current pilot study was slightly lower than Palta7 and colleagues’ study of older hypertensive African Americans, but similar to the recommended target attendance of at least 6 sessions by Woods-Giscombe and colleagues’ study of prediabetic African Americans.8 The mindfulness intervention in Palta’s et. al., study took place in a group room on the first floor of the senior housing facility and travel was not required which may have increased Palta’s attendance rates.
A clinically meaningful reduction in systolic BP was observed in the current pilot study among the MIM DASH participants. This reduction was not as great as Palta’s et al study (−16.7 mmHg). However, those participants had a higher baseline systolic BP (148.5 mmHg) than the older adults in the current pilot study (133.6 mmHg).
MIM DASH did not improve diet, mindfulness affect, or perceived stress. Because diagnosis of hypertension was an inclusion criteria, the participants’ knowledge of their heart disease may have exerted a moderating effect on their self-efficacy to make dietary changes, as is reported in a study of African Americans who participated in a cardiovascular health promotion study.21 Participants in our study reported low stress and above average mindfulness affect at baseline. African Americans, who experience less stress, are more likely to engage in health promoting behaviors to reduce their risk of cardiovascular disease.22 Participants with low stress and above average mindfulness affect at baseline may have resulted in sample bias contributing to few significant findings in the current study. Moreover, the participants in the current pilot study were highly educated and this may also have contributed to their reappraisal of stress and mindfulness affect. Increasing education is associated with many mental and physical health benefits for African Americans.23
Findings of the current pilot study should be considered in the context of small randomized controlled trials. Limitations of this study included a small sample size of primarily highly educated women and reliance upon self-reported diet data. However, recruitment of African American men is a common challenge in intervention research that has been attributed to medical mistrust.24 Using small groups to deliver this intervention is appropriate and acceptable to African Americans and will need to be addressed as scalability of this intervention is considered. Future studies should include tailoring to recruit African American men, and those with lower education, as well as a longer follow up to measure sustainability of the intervention. Additional studies may also need to account for the moderating effect of self-efficacy to change dietary habits in persons with known heart disease. The use of a true control group was not feasible; only half of those enrolled completed 3 month data collection. The lack of contact may have led to the reduced completion rates in the true control group. Thus, in future studies, limiting control trials to having two-arms with an intervention group and attention only group would be a more efficient study design.
In summary, the current pilot study contributes important knowledge because few studies have focused on mindfulness plus diet education in African American older adults with MCI and hypertension.
Supplementary Material
Supplemental Figure S1. Mindfulness in Motion (MIM) plus the Dietary Approaches to Stop Hypertension (DASH) CONSORT diagram provides the data regarding enrollment, allocation, follow-up and analysis for this pilot study. Participants were divided into six groups randomized 1:1:1 to the MIM DASH group, attention only (non-hypertensive education) group, or true control group. The group number (1–6) is provided next to each condition (MIM DASH, attention only, or true control).
ACKNOWLEDGEMENTS
The Discovery Themes-Chronic Brain Injury Initiative, The Ohio State University. https://discovery.osu.edu/chronic-brain-injury. 190 N. Oval Mall, Columbus, OH 43210 Office: 614–292-9023. Funded in part by The Ohio State University Center for Clinical and Translational Science grant support (National Center for Advancing Translational Sciences, Grant UL1TR002733). The Ohio State University Health Sciences Library Medical Visuals.
Sponsor’s Role.
The sponsor had no role in the data collection and analysis or writing the article
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
Trial registration: 2018H0136, NCT03736434. Registered 07 November 2018-Retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT03736434
REFERENCES
- 1.Association As. Alzheimer’s disease facts and figures in Alzheimer’s dementia. 2020:321–387.
- 2.Lefferts WK, Heffernan KS, Barreira TV. Association between pulsatile blood pressure and cognitive performance among older adults: Insight from the National Health and Nutrition Examination Survey 1999–2002. Int J Cardiol. 2016;223:981–984. [DOI] [PubMed] [Google Scholar]
- 3.Laditka JN, Laditka SB, Cornman CB, Porter CN, Davis DR, Mintzer J. Notably higher rates of vascular risk factors and dementia among African Americans in South Carolina: opportunities for public health intervention. J S C Med Assoc. 2008;104(7):219–222. [PubMed] [Google Scholar]
- 4.Watson-Singleton NN, Black AR, Spivey BN. Recommendations for a culturally-responsive mindfulness-based intervention for African Americans. Complement Ther Clin Pract. 2019;34:132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parra DC, Wetherell JL, Van Zandt A, Brownson RC, Abhishek J, Lenze EJ. A qualitative study of older adults’ perspectives on initiating exercise and mindfulness practice. BMC Geriatr. 2019;19(1):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tenfelde SM, Hatchett L, Saban KL. “Maybe black girls do yoga”: A focus group study with predominantly low-income African-American women. Complement Ther Med. 2018;40:230–235. [DOI] [PubMed] [Google Scholar]
- 7.Palta P, Page G, Piferi RL, et al. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. J Urban Health. 2012;89(2):308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woods-Giscombe CL, Gaylord SA, Li Y, et al. A Mixed-Methods, Randomized Clinical Trial to Examine Feasibility of a Mindfulness-Based Stress Management and Diabetes Risk Reduction Intervention for African Americans with Prediabetes. Evid Based Complement Alternat Med. 2019;2019:3962623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woods-Giscombe CL, Gaylord SA. The Cultural Relevance of Mindfulness Meditation as a Health Intervention for African Americans: Implications for Reducing Stress-Related Health Disparities. J Holist Nurs. 2014;32(3):147–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gilbertson RM, Klatt MD. Mindfulness in Motion for People with Multiple Sclerosis: A Feasibility Study. Int J MS Care. 2017;19(5):225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klatt M, Steinberg B, Duchemin AM. Mindfulness in Motion (MIM): An Onsite Mindfulness Based Intervention (MBI) for Chronically High Stress Work Environments to Increase Resiliency and Work Engagement. J Vis Exp. 2015(101):e52359. [DOI] [PMC free article] [PubMed]
- 12.Scharre DW, Chang SI, Murden RA, et al. Self-administered Gerocognitive Examination (SAGE): a brief cognitive assessment Instrument for mild cognitive impairment (MCI) and early dementia. Alzheimer Dis Assoc Disord. 2010;24(1):64–71. [DOI] [PubMed] [Google Scholar]
- 13.Chang S, Koegel K. Back to Basics: All About MyPlate Food Groups. J Acad Nutr Diet. 2017;117(9):1351–1353. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Complementary and Intigrative Health. Pilot studies: Common uses and misuses. National Institutes of Health. October 21, 2020. Accecced October 21, 2020. https://www.nccih.nih.gov/grants/pilot-studies-common-uses-and-misuses
- 15.Johnson KC, Whelton PK, Cushman WC, et al. Blood Pressure Measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2018;71(5):848–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warren-Findlow J, Reeve CL, Racine EF. Psychometric Validation of a Brief Self-report Measure of Diet Quality: The DASH-Q. J Nutr Educ Behav. 2017;49(2):92–99 e91. [DOI] [PubMed] [Google Scholar]
- 17.Feldman GC, Hayes AM, Kumar SM, Greeson JG, &Laurenceau JP Mindfulness and emotion regulation: the development and initial validation of the Cognitive andAffective Mindfulness Scale-Revised (CAMS-R). Journal of Psychopathology and Behavioral Assessment. 2007;29:177–190. [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 19.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. [DOI] [PubMed] [Google Scholar]
- 20.Burnett-Zeigler I, Satyshur MD, Hong S, Wisner KL, Moskowitz J. Acceptability of a mindfulness intervention for depressive symptoms among African-American women in a community health center: A qualitative study. Complement Ther Med. 2019;45:19–24. [DOI] [PubMed] [Google Scholar]
- 21.Abbott L, Schluck G, Graven L, & Martorella G. (2018). Exploring the intervention effect moderators of a cardiovascular health promotion study in rural African Americans. Public Health Nursing, 35: 126–134. DOI: 10.1111/phn.12377 [DOI] [PubMed] [Google Scholar]
- 22.Brewer LC, Redmond N, Slusser JP, et al. Stress and Achievement of Cardiovascular Health Metrics: The American Heart Association Life’s Simple 7 in Blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGilton KS, Vellani S, Yeung L, et al. Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: a scoping review. BMC Geriatr. 2018;18(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powell W, Richmond J, Mohottige D, Yen I, Joslyn A, Corbie-Smith G. Medical Mistrust, Racism, and Delays in Preventive Health Screening Among African-American Men. Behav Med. 2019;45(2):102–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1. Mindfulness in Motion (MIM) plus the Dietary Approaches to Stop Hypertension (DASH) CONSORT diagram provides the data regarding enrollment, allocation, follow-up and analysis for this pilot study. Participants were divided into six groups randomized 1:1:1 to the MIM DASH group, attention only (non-hypertensive education) group, or true control group. The group number (1–6) is provided next to each condition (MIM DASH, attention only, or true control).


