Abstract
Objectives:
Roughly 10% of occupational injuries result in permanent impairment and a permanent partial disability (PPD) award. After initial return to work (RTW) following a work injury, many workers with permanent impairment face RTW interruption (breaks in ongoing employment due to reinjury, poor health, disability, lay-off, etc.). Most RTW and reinjury research has focused on worker-level risk factors, and less is known about contextual factors that may be amenable to workplace or workers’ compensation (WC)-based interventions. The aim of this study was to identify modifiable organizational and psychosocial workplace factors associated with (1) RTW interruption and (2) reinjury among workers with a permanent impairment.
Methods:
This retrospective cohort study included WC claims data and survey data for 567 injured workers who RTW at least briefly after a work-related injury that resulted in permanent impairment. Workers were interviewed once by phone, 11 to 15 months after WC claim closure with a PPD award. Logistic regression models were used to estimate associations between each workplace factor of interest and each outcome, controlling for whole body impairment percentage, gender, age, nativity, educational level, State Fund vs. self-insured WC coverage, employer size, union membership, industry sector, and employment duration of current/most recent job.
Results:
12% of workers had been reinjured in their current or most recent job, 12% of workers were no longer working at the time of interview, and <1% of workers reported both outcomes. The most frequently reported reason for RTW interruption was impairment, disability, and/or pain from the previous work injury. Lower reported levels of safety climate, supervisor support, and ability to take time off work for personal/family matters were significantly associated with both RTW interruption and reinjury. Inadequate employer/health care provider communication, perceived stigmatization from supervisors and/or coworkers, and lower levels of coworker support were significantly associated with RTW interruption but not with reinjury. Discomfort with reporting an unsafe situation at work, absence of a health and safety committee, and higher job strain were significantly associated with reinjury, but not with RTW interruption. Inadequate safety training and lack of needed job accommodations were not significantly associated with either outcome. There were no notable or statistically significant interactions between workplace factors and degree of impairment, and no consistent direction of association.
Conclusions:
This study provides evidence that several potentially modifiable organizational and psychosocial factors are associated with safe and sustained RTW among injured workers with work-related permanent impairment. The lack of interaction between any of these workplace factors and degree of impairment suggests that these findings may be generalizable to all workers, and further suggests that workplace interventions based on these findings might be useful for both primary and secondary prevention. Though primary prevention is key, secondary prevention efforts to sustain RTW and prevent reinjury may reduce the considerable health, economic, and social burden of occupational injury and illness.
Keywords: workers’ compensation, permanent partial disability, workplace, safety management, safety climate, social support, job strain, stigma
INTRODUCTION
About 300,000 U.S. workers per year incur serious work injuries resulting in a permanent partial disability (PPD) award; this represents roughly 10% of injured workers with workers’ compensation (WC) claims (Weiss et al., 2019). WC-based PPD awards are intended to compensate injured workers for permanent impairment resulting from work injuries or illnesses (e.g., vision or hearing loss, amputation, spinal impairment) that prevent working at full physical capacity, but do not preclude return to work (RTW).
After RTW following a work injury, many workers with permanent impairment face RTW interruption (breaks in employment), potentially due to reinjury, poor health, disability, or negative treatment by managers and coworkers (Butler et al., 1995; Bultmann et al., 2007; Young, 2010b; MacEachen et al., 2012; Price et al., 2012; de Jong et al., 2015; Casey and Ballantyne, 2017; Schur et al., 2017). In a survey of Washington State workers with permanent impairment, 47% of workers who had RTW reported that permanent impairment made it difficult to get a job, and 58% reported that permanent impairment made it difficult to keep their job (Sears et al., 2020). In the same study, when comparing current to pre-injury work status, workers with a higher degree of permanent impairment more frequently reported working fewer hours, earning less, and having less job security (Sears et al., 2020).
As many as half of all injured workers are reinjured (Cherry et al., 2010; Ruseckaite and Collie, 2011; Berecki-Gisolf et al., 2012; Keeney et al., 2013), and repeat work injuries are more severe and more costly than initial injuries (Ruseckaite and Collie, 2011, 2013). Risk of reinjury among permanently impaired workers is of particular concern given evidence that occupational injuries are more common, more severe, and more costly among workers with persistent disabilities (Zwerling et al., 1996; Zwerling et al., 1998a; Zwerling et al., 1998b; Price et al., 2012; Shi et al., 2015a; Shi et al., 2015b). In a recent study (Sears et al., 2020), more than half of Washington State workers surveyed thought their permanent impairment put them at higher risk of being reinjured at work, compared to before their injury (65%), or compared to coworkers in the same job (54%). After adjusting for working time at risk, workers with at least 10% permanent impairment had a 34% higher risk of reinjury relative to workers with no permanent impairment (Sears et al., In press.).
Much RTW and reinjury research has been focused on worker-level risk factors (e.g., age, health status, health behaviors, depression, catastrophizing, fear avoidance). Less is known about workplace-level factors, which may be amenable to workplace or WC system-based interventions—thereby having potentially broader impact (Midtsundstad and Nielsen, 2016; Spector and Reul, 2017). Moreover, most studies of workplace accommodations have focused on assistive technology and specialized equipment, rather than on policy-related solutions (e.g., flexible work schedules, telework) or workplace culture (Sundar, 2017). Yet, modifiable workplace or system-level factors were the most commonly described employment barriers in a study of RTW experiences among 150 injured workers who had used vocational rehabilitation services (Young, 2009). Further, a recent study ranked organizational and psychosocial exposures as among the most prevalent workplace exposures in the northwest region of the U.S. (Doubleday et al., 2019). Although few studies have focused specifically on permanently impaired workers, there is accumulating evidence that modifiable workplace organizational and psychosocial factors (e.g., job accommodation, safety climate, job strain, social support) can impact successful RTW, injury/reinjury, and work absence (Franche et al., 2005; Smith and DeJoy, 2012; White et al., 2013; Baidwan et al., 2019; White et al., 2019).
The aim of this study was to identify potentially modifiable workplace organizational and psychosocial factors associated with RTW interruption and/or reinjury, among workers who had RTW at least briefly after a work-related injury that resulted in permanent impairment. We interviewed injured workers regarding their exposure to a number of workplace factors that we hypothesized would be associated with RTW interruption and/or reinjury, and that might be modifiable via workplace or WC system-level interventions designed to support safe and sustained RTW. We assessed associations between (1) worker-reported exposure to each workplace factor and (2) RTW interruption and reinjury outcomes. For each workplace factor, we also assessed effect modification by degree of permanent impairment.
METHODS
Study design and data sources
We surveyed a retrospective cohort of Washington State workers with a work-related permanent impairment, who had RTW at least briefly. The survey was conducted about a year after PPD rating and claim closure. In order to assess workplace factors most proximate and relevant to current employment status, and to minimize recall bias, we focused on characteristics and outcomes of the current or most recent job.
The Washington State Department of Labor and Industries (L&I) administers the WC system, which includes the State Fund, covering about 70% of workers, and self-insured employers, covering the remaining 30%. Private WC insurers do not operate in Washington State. Several months before the survey, we obtained L&I administrative data and contact information associated with closed claims for potentially eligible workers.
Washington State workers were potentially eligible for this study if they met inclusion criteria by having an accepted State Fund or self-insured WC claim that closed with a PPD award between January 1, 2018 and April 30, 2018. Prior to delivering data to the research team, L&I staff applied six exclusion criteria: (1) no valid phone number on record; (2) under age 18 when injured; (3) fatal or total permanent disability claims; (4) residence outside Washington State; (5) L&I employees and other confidentiality exclusions imposed by L&I; and (6) deceased workers. L&I staff identified 2,541 workers who were potentially eligible for the survey. Two additional exclusion criteria were applied by interviewers during eligibility screening: (1) language or comprehension barrier; and (2) no RTW, as determined by a worker’s response to the question, “Have you returned to work since the injury that caused your impairment or disability, even if only very briefly?”
Workers were interviewed between February 6 and April 20, 2019, using Computer Assisted Telephone Interviewing technology. Interviews were conducted 11 to 15 months after claim closure (mean: 12.8 months). In total, 582 complete and 17 partial interviews were conducted, with a response rate of 53.8%. Respondents did not notably differ from nonrespondents with regard to age at injury, gender, State Fund vs. self-insured WC coverage, or closed claim being their first Washington State WC claim. Further details regarding survey development, survey administration, numbers of ineligible workers excluded for specific criteria, response rate calculation, and response bias assessment are available elsewhere (Sears et al., 2020). All survey participants gave informed consent. This study was approved by the University of Washington Human Subjects Division.
Worker outcomes
The two outcomes of interest for this study were: (1) RTW interruption, defined as no longer working when interviewed; and (2) reinjury, defined as any work injury that resulted in at least one missed day of work. Both outcomes were ascertained via self-report, specifically with respect to the worker’s current job when interviewed, or—if no longer working when interviewed—with respect to their most recent job. Workers who had more than one current/most recent job were asked to answer all outcome and workplace questions with respect to the job they considered to be their primary job. For descriptive purposes, the subset of workers who were no longer working were asked, “What is the primary reason you are no longer working at this job?” Several response categories were pre-specified, but workers could also respond “other reason” and provide a brief alternative response.
Selection and measurement of workplace factors
The following set of workplace factors was identified as potentially important based on prior research and stakeholder input: job accommodations, employer/health care provider communication, safety training, presence of a health and safety committee, comfort reporting an unsafe work situation, safety climate, stigmatization, job strain, social support (supervisor, coworker, and combined), and ability to take time off work for personal/family matters. All workplace factors were ascertained via self-report. Survey questions were drawn from existing instruments or previous surveys, where feasible (Sears et al., 2020). A brief summary of relevant literature and the measurement approach for this study are provided below for each workplace factor.
There is substantial evidence that job accommodation facilitates RTW (Krause et al., 1998; Franche et al., 2005; Carroll et al., 2010; McLaren et al., 2017; Villotti et al., 2020), and is economically advantageous (Tompa et al., 2008). In a study of 40 self-insured California employers, job accommodation was associated with significant reductions in both time loss duration and sustained RTW; reductions were particularly large for workers with a permanent disability (McLaren et al., 2017). Job accommodation reduced the number of subsequent work absences among permanently impaired Canadian workers by about 12% to 14% (Campolieti, 2002). We used a two-part question to assess job accommodation. First, workers were asked whether, in their current/most recent job, the worker or employer had made changes to the job, work environment, or work hours, to help them RTW. If the answer was no, workers were asked whether any such changes were needed to help them work at their best. These two questions were recoded into one three-category variable (needed and provided, needed but not provided, not needed).
There is substantial evidence that adequate employer/health care provider communication facilitates RTW (Franche et al., 2005; Carroll et al., 2010), and is economically advantageous (Tompa et al., 2008). We assessed employer/health care provider communication using a binary choice question: “During the past year, did you feel there was adequate communication between your health care provider(s) and your employer(s) to assist you in staying at work?”
Some evidence suggests that adequate safety training protects against injury (Zierold, 2016; Teufer et al., 2019). Health and safety committee presence may reduce injury rates, but evidence is mixed, and committee effectiveness may be more important (Yassi et al., 2013). In a Canadian survey, worker empowerment (including comfort reporting unsafe work situations) was found protective against injury (Lay et al., 2017). We used three binary choice questions to assess these aspects of the safety environment: (1) “In your current/most recent job, did you receive adequate training to perform your job safely?” (2) “Is there a Health and Safety Committee at your current/most recent workplace?” and (3) “If you were aware of an unsafe situation at work, would you be comfortable reporting it to your supervisor or employer?”
Safety climate has been found protective with respect to safety behavior and safety outcomes, including injury (Smith and DeJoy, 2012; Huang et al., 2013a; Huang et al., 2013b; Huang et al., 2017b). Safety climate is also associated with lower turnover, mediated by job satisfaction (Huang et al., 2016), as well as with worker well-being and productivity (Katz et al., 2019). We assessed safety climate at both the organization level (top management) and group level (direct supervisor), using the validated Safety Climate Short Scales (Huang et al., 2017a). To be scored, workers must have responded to at least three of the four items per scale.
The workplace stigmatization studies we identified were conceptual or qualitative, but suggested that experiencing stigma could be associated with worker health and well-being (Lippel, 2007), underemployment (Stuart, 2004), and connection with work (Kirsh et al., 2012). One study found that nonsexual workplace harassment was associated with increased likelihood of occupational injury (Yu et al., 2018). For our study, workers were first asked, “Are any of your supervisors aware of your work-related impairment or disability?” If yes, they were asked about agreement with the statement “Supervisors think less of me because of my work-related disability or impairment.” Agreement was classified as presence of stigmatization; disagreement or supervisors being unaware was classified as absence of stigmatization. The same set of questions was asked with respect to coworkers.
Lower job strain is associated with decreased injury risk (Kraatz et al., 2013; Lee et al., 2015; Baidwan et al., 2019), RTW (Haveraaen et al., 2016; Haveraaen et al., 2017; Villotti et al., 2020), and less workplace absence (White et al., 2013). We used the validated Work History Questionnaire (WHQ) to assess job strain (Landsbergis et al., 2002). High job strain was defined as scoring above the sample median (6) on job demands (two items), in conjunction with scoring below the sample median (7) on decision latitude (two items).
Workplace social support is associated with decreased injury risk (Kraatz et al., 2013; Reme et al., 2014; Tveito et al., 2014; Baidwan et al., 2019), RTW (Haveraaen et al., 2016; Villotti et al., 2020), sustained RTW (Jetha et al., 2018; Etuknwa et al., 2019; White et al., 2019), and less workplace absence (White et al., 2013). Among permanently impaired Massachusetts workers who RTW after WC-related vocational rehabilitation, supportive workplace relationships—and specifically worker-supervisor relationships—contributed to sustained RTW (Young, 2010b, 2010a). A related concept, better treatment by management and coworkers, predicted lower turnover intention and higher job satisfaction (Schur et al., 2017). We used two WHQ items to assess supervisor support, coworker support, and the combined social support concept (Landsbergis et al., 2002). We conducted sensitivity analyses using eight social support items from the validated Job Content Questionnaire (JCQ)—four items each for supervisor support and coworker support (Karasek et al., 1998; Landsbergis et al., 2002).
Work-family interference has been identified as a reinjury risk factor (Smith and DeJoy, 2012). Further, a study of permanently impaired Canadian workers found that disability management strategies that include flexible schedules may be especially effective in reducing reinjury (Campolieti, 2002). We asked a work-family interference question (“How difficult is it to take time off during your work to take care of personal or family matters?”) from the Quality of Worklife module developed for the 2002 General Social Survey (National Institute for Occupational Safety and Health, 2013), using a scale from 1 (not at all difficult) to 5 (extremely difficult).
Covariates
Covariates obtained or constructed from administrative data included gender, age when interviewed, WC coverage (State Fund versus self-insured employer), and whole body impairment (WBI) percentage. In Washington State, impairment is defined as permanent anatomic or functional abnormality or loss of function, once maximum medical improvement has been achieved (Washington State Department of Labor and Industries, 2019). If, after completing treatment, workers have suffered permanent loss of function but are able to work, their degree of impairment may be rated for a PPD award. We constructed a WBI measure representing a conservative estimate of WBI percentage, based on permanent impairment rating at claim closure. This measure essentially produced a lower bound estimate of WBI, as it was based on the single largest contribution from the single impaired body part contributing most to WBI. WBI percentage was then classified into two mutually exclusive groups, WBI <10% and WBI ≥10%. An earlier publication (Sears et al., 2020) provides more detail about how WBI was constructed and classified.
Covariates obtained from the survey included educational level, whether born in the U.S., and union membership, as well as several characteristics pertaining to the worker’s current/most recent job: industry sector, time working in the same job, and employer size. Large (vs. small) employer was based on the worker reporting 50 or more (vs. fewer than 50) employees at their specific workplace.
Data analysis
Missing data was negligible. We excluded the 15 cases (2.6% of the 582 completed interviews) with missing data for either outcome or for any of the 10 covariates, which allowed us to assess the association of each workplace factor with each outcome, using the same sample. However, workplace factor questions had varying numbers of “don’t know” or “declined to answer” responses, and some questions were not applicable to certain workers; thus, the number of included cases varied by workplace factor.
To simplify interpretation of results, coding of all workplace factor variables was aligned so that higher values always referred to the condition hypothesized to be more desirable. Workplace factors that were measured as scales used several different ranges and scoring methods, and some involved multiple items. To enhance comparability of effect sizes, we standardized scale scores to have a mean of zero and a standard deviation of one. We presented means for the original variables to enable comparison to other published data, but used standardized scores in logistic regression models.
Bivariate associations between each outcome and the workplace factors and covariates were tested using Pearson’s chi-squared test (binary or categorical variables), Wilcoxon rank-sum (Mann-Whitney) test (ordinal variables), or unequal variances t-test (ordinal scales or continuous variables). Logistic regression models were used to estimate associations between each workplace factor and each outcome in turn, controlling for gender, age, educational level, nativity, WBI category, State Fund vs. self-insured WC coverage, union membership, employer size, industry sector, and years in the same job. We also tested for interactions between each workplace factor and WBI category. Level of significance was set at P<0.05. All analyses were conducted using Stata/MP 15.1 for Windows (StataCorp, 2017).
RESULTS
Of 567 workers interviewed, 70 (12.35%) were no longer working in their most recent job when interviewed (RTW interruption), and 70 (12.35%) had been reinjured in their current/most recent job. Despite prevalence similarity, there was little overlap between groups—only five workers (0.88%) reported both outcomes. Injury year ranged from 1991 to 2018; 3.70% were injured before 2010. Years from injury to interview ranged from 1.10 to 27.33, with a mean of 3.45 (SD 2.60), and median of 2.55.
Among the 70 workers no longer working in their most recent job, the most frequently reported reason for RTW interruption was impairment, disability, and/or pain from the previous work injury (28.57%; n=20). Other reasons included (in descending frequency): retired (27.14%; n=19); laid off or on work furlough (18.57%; n=13); some other health condition or injury (17.14%; n=12); something about the most recent job/workplace made it hard to keep working (14.29%; n=10); logistical barriers such as transportation, childcare, or family needs (7.14%; n=5); or got a new job, but not yet working (2.86%; n=2). These categories were not mutually exclusive; there were 81 responses from 70 workers.
There were few significant or substantial associations between covariates and either outcome (Table 1). The most striking (and predictable) association was that nearly a third of workers 65 and older were no longer working when interviewed, compared to less than a sixth of workers in all other age categories. At the time of interview, 42.50% of respondents reported being a union member. Union membership was significantly associated with less RTW interruption, but was also strongly associated with reinjury; 18.26% of union members reported reinjury, compared to 7.98% of other workers (P<0.0005).
Table 1.
Worker, injury, and employment characteristics included in the basic model, by whether no longer working at interview (RTW interruption), and by whether reinjured in the current/most recent job (N=567).
| Characteristic | N (Column %) | RTW interrupted | Reinjured | ||
|---|---|---|---|---|---|
| Row % | P | Row % | P | ||
| Overall | 567 (100) | 12.35 | N/A | 12.35 | N/A |
| Gender | 567 (100) | 0.37a | 0.46a | ||
| Male | 383 (67.55) | 11.49 | 13.05 | ||
| Female | 184 (32.45) | 14.13 | 10.87 | ||
| Age when interviewed | 567 (100) | 0.02b | 0.41b | ||
| 18-34 | 72 (12.70) | 11.11 | 11.11 | ||
| 35-44 | 112 (19.75) | 8.04 | 11.61 | ||
| 45-54 | 152 (26.81) | 11.18 | 12.50 | ||
| 55-64 | 198 (34.92) | 13.13 | 11.11 | ||
| 65+ | 33 (5.82) | 30.30 | 24.24 | ||
| Educational level | 567 (100) | 0.57b | 0.15b | ||
| <High school graduation | 22 (3.88) | 18.18 | 4.55 | ||
| High school graduation or GED | 136 (23.99) | 12.50 | 17.65 | ||
| Some college | 294 (51.85) | 12.24 | 11.56 | ||
| College graduation | 115 (20.28) | 11.30 | 9.57 | ||
| Born in U.S. | 567 (100) | 0.38a | 0.35a | ||
| No | 49 (8.64) | 16.33 | 8.16 | ||
| Yes | 518 (91.36) | 11.97 | 12.74 | ||
| Whole body impairment | 567 (100) | 0.69a | 0.69a | ||
| <10% | 440(77.60) | 12.05 | 12.05 | ||
| ≥10% | 127 (22.40) | 13.39 | 13.39 | ||
| Workers’ compensation coverage | 567 (100) | 0.42a | 0.19a | ||
| State Fund | 356 (62.79) | 13.20 | 10.96 | ||
| Self-insured | 211 (37.21) | 10.90 | 14.69 | ||
| Union member | 567 (100) | 0.045a | <0.0005a | ||
| No | 326 (57.50) | 14.72 | 7.98 | ||
| Yes | 241 (42.50) | 9.13 | 18.26 | ||
| Large employer | 567 (100) | 0.56a | 0.27a | ||
| No | 334 (58.91) | 11.68 | 11.08 | ||
| Yes | 233 (41.09) | 13.30 | 14.16 | ||
| Industry sector | 567 (100) | 0.42a | 0.48a | ||
| Construction/utilities/mining/agriculture/forestry | 104 (18.34) | 13.46 | 8.65 | ||
| Manufacturing | 74 (13.05) | 5.41 | 14.86 | ||
| Retail/wholesale trade | 55 (9.70) | 16.36 | 10.91 | ||
| Transportation/warehousing | 68 (11.99) | 14.71 | 11.76 | ||
| Finance/insurance/real estate/professional/technical | 36 (6.35) | 16.67 | 16.67 | ||
| Administrative services/public services | 91 (16.05) | 15.38 | 17.58 | ||
| Education/health care/social services | 106 (18.69) | 9.43 | 8.49 | ||
| Arts/entertainment/hospitality | 33 (5.82) | 9.09 | 15.15 | ||
N/A, not applicable; RTW, return to work.
Pearson’s chi-squared test.
Wilcoxon rank-sum (Mann-Whitney) test.
Note: Column percentages do not always sum to exactly 100% due to rounding.
Time spent working in the same job averaged 9.19 years (SD 10.39). This did not differ significantly by RTW interruption status (mean difference: −0.99; 95% CI: −3.95, 1.97), but did differ by reinjury status. Workers who were reinjured during the past year in their current/most recent job had been working in the same job an average of 12.65 years (SD 10.73), compared to 8.70 years (SD 10.26) for those not reinjured (mean difference: −3.95; 95% CI: −6.65, −1.24).
Table 2 presents bivariate associations between binary/categorical workplace factors and the two outcomes. For each workplace factor, the condition hypothesized as less desirable is shown on the upper line. With two exceptions, the direction of each unadjusted bivariate association was as hypothesized. Both exceptions involved the reinjury outcome, and neither was statistically significant: (1) adequate employer/health care provider communication, and (2) stigmatized for PPD by coworkers. The prevalence of the more desirable condition was above 70% for all workplace factors; over 95% were comfortable reporting an unsafe situation at work.
Table 2.
Distribution of self-reported workplace factors (categorical or binary), by whether no longer working at interview (RTW interruption), and by whether reinjured in the current/most recent job (N=567).
| Workplace factor (binary) | N (Column %) | RTW interrupted | Reinjured | ||
|---|---|---|---|---|---|
| Row % | Pa | Row % | Pa | ||
| Job accommodations | 558 (100) | 0.07 | 0.13 | ||
| Needed but not provided | 71 (12.72) | 18.31 | 18.31 | ||
| Needed and provided | 249 (44.62) | 13.25 | 13.25 | ||
| Not needed | 238 (42.65) | 8.82 | 9.66 | ||
| Adequate employer/health care provider communication | 484 (100) | <0.0005 | 0.20 | ||
| No | 131 (27.07) | 20.61 | 10.69 | ||
| Yes | 353 (72.93) | 8.78 | 15.30 | ||
| Adequate training to do job safely | 561 (100) | 0.10 | 0.38 | ||
| No | 70 (12.48) | 18.57 | 15.71 | ||
| Yes | 491 (87.52) | 11.61 | 12.02 | ||
| Presence of health and safety committee | 525 (100) | 0.42 | 0.42 | ||
| No | 126 (24.00) | 15.08 | 15.08 | ||
| Yes | 399 (76.00) | 12.28 | 12.28 | ||
| Comfortable reporting unsafe situation at work | 565 (100) | 0.20 | 0.01 | ||
| No | 24 (4.25) | 20.83 | 29.17 | ||
| Yes | 541 (95.75) | 12.01 | 11.65 | ||
| Stigmatized for PPD by supervisor | 565 (100) | <0.0005 | 0.06 | ||
| Yes | 60 (10.62) | 28.33 | 20.00 | ||
| No | 505 (89.38) | 10.50 | 11.49 | ||
| Stigmatized for PPD by coworkers | 567 (100) | 0.005 | 0.56 | ||
| Yes | 42 (7.41) | 26.19 | 9.52 | ||
| No | 525 (92.59) | 11.24 | 12.57 | ||
| Job strain | 544 (100) | 0.29 | 0.03 | ||
| High | 81 (14.89) | 14.81 | 19.75 | ||
| Low | 463 (85.11) | 10.80 | 11.02 | ||
PPD, permanent partial disability; RTW, return to work.
Pearson’s chi-squared test.
Note: Column percentages do not always sum to exactly 100% due to rounding.
Table 3 presents bivariate associations between ordinal/continuous workplace factors and the two outcomes. For each workplace factor, higher values indicate the hypothesized desirable condition. In every case, the direction of each unadjusted bivariate association was as hypothesized. Data for the WHQ versions of the social support, supervisor support, and coworker support variables are reported in Table 3. Findings based on the JCQ versions of these three variables were substantially similar (see data in Supplementary Table S1, available at Annals of Work Exposures and Health online).
Table 3.
Distribution of self-reported workplace factors (scales), by whether no longer working at interview (RTW interruption), and by whether reinjured in the current/most recent job (N=567).
| Workplace factor | N items |
Possible range |
N | Overall mean (SD) |
RTW interrupted | Reinjured | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| No Mean (SD) |
Yes Mean (SD) |
Pa | No Mean (SD) |
Yes Mean (SD) |
Pa | |||||
| Organization-level safety climate | 4 (mean) |
1-5 | 546 | 4.00 (1.17) |
4.06 (1.14) |
3.55 (1.27) |
0.003 | 4.07 (1.14) |
3.51 (1.29) |
0.001 |
| Group-level safety climate | 4 (mean) |
1-5 | 551 | 3.91 (1.27) |
4.01 (1.22) |
3.25 (1.39) |
0.0001 | 3.97 (1.25) |
3.55 (1.35) |
0.02 |
| Supervisor support | 1 | 1-4 | 551 | 3.35 (0.95) |
3.43 (0.90) |
2.79 (1.09) |
<0.0001 | 3.40 (0.91) |
3.00 (1.08) |
0.005 |
| Coworker support | 1 | 1-4 | 546 | 3.48 (0 .70) |
3.51 (0.66) |
3.25 (0.90) |
0.03 | 3.48 (0.70) |
3.43 (0.70) |
0.60 |
| Social support | 2 (sum) |
2-8 | 541 | 6.84 (1.34) |
6.94 (1.27) |
6.08 (1.65) |
0.0001 | 6.89 (1.31) |
6.46 (1.50) |
0.03 |
| Able to take time off work for personal/family matters | 1 | 1-5 | 559 | 3.99 (1.29) |
4.02 (1.27) |
3.72 (1.39) |
0.09 | 4.01 (1.31) |
3.82 (1.17) |
0.22 |
RTW, return to work; SD, standard deviation.
Unequal variances t-test.
Table 4 presents the results of the basic regression models for each outcome. Each of these models included all covariates, but excluded the workplace factors of interest. Results were generally in line with unadjusted associations reported in Table 1: (1) workers ages 65 and older had over three times the odds of RTW interruption, compared to workers ages 18 to 34; and (2) union members had nearly three times the odds of reinjury, compared to other workers.
Table 4.
Logistic regression results for the two basic outcome models: whether no longer working at interview (RTW interruption), and whether reinjured in the current/most recent job (N=567).
| Characteristic | RTW interrupted | Reinjured | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Gender | 0.30 | 0.95 | ||||
| Male | ref | ref | ||||
| Female | 1.38 | 0.75, 2.56 | 0.98 | 0.54, 1.78 | ||
| Age when interviewed | 0.04 | 0.30 | ||||
| 18-34 | ref | ref | ||||
| 35-44 | 0.62 | 0.22, 1.77 | 0.99 | 0.38, 2.59 | ||
| 45-54 | 0.91 | 0.36, 2.28 | 0.98 | 0.38, 2.55 | ||
| 55-64 | 1.15 | 0.46, 2.83 | 0.83 | 0.32, 2.14 | ||
| 65+ | 3.26 | 1.05, 10.15 | 2.78 | 0.74, 10.41 | ||
| Educational level | 0.61 | 0.09 | ||||
| <High school graduation | ref | ref | ||||
| High school graduation or GED | 0.52 | 0.16, 1.68 | 3.33 | 0.41, 27.06 | ||
| Some college | 0.50 | 0.17, 1.52 | 1.81 | 0.22, 14.85 | ||
| College graduation | 0.43 | 0.13, 1.50 | 1.38 | 0.15, 12.67 | ||
| Born in U.S. | 0.15 | 0.43 | ||||
| No | ref | ref | ||||
| Yes | 0.54 | 0.23, 1.24 | 1.55 | 0.52, 4.59 | ||
| Whole body impairment | 0.91 | 0.69 | ||||
| <10% | ref | ref | ||||
| ≥10% | 1.03 | 0.58, 1.86 | 1.13 | 0.62, 2.09 | ||
| Workers’ compensation coverage | 0.53 | 0.69 | ||||
| State Fund | ref | ref | ||||
| Self-insured | 0.82 | 0.44, 1.53 | 0.89 | 0.50, 1.59 | ||
| Union member | 0.14 | 0.001 | ||||
| No | ref | ref | ||||
| Yes | 0.60 | 0.30, 1.18 | 2.81 | 1.52, 5.19 | ||
| Large employer | 0.16 | 0.76 | ||||
| No | ref | ref | ||||
| Yes | 1.48 | 0.86, 2.55 | 1.09 | 0.62, 1.91 | ||
| Industry sector | 0.35 | 0.39 | ||||
| Construction/utilities/mining/agriculture/forestry | ref | ref | ||||
| Manufacturing | 0.35 | 0.11, 1.09 | 1.78 | 0.66, 4.81 | ||
| Retail/wholesale trade | 0.84 | 0.31, 2.30 | 1.69 | 0.50, 5.66 | ||
| Transportation/warehousing | 1.00 | 0.39, 2.55 | 1.44 | 0.52, 4.03 | ||
| Finance/insurance/real estate/professional/technical | 1.00 | 0.32, 3.10 | 3.75 | 1.13, 12.40 | ||
| Administrative services/public services | 1.17 | 0.49, 2.77 | 2.20 | 0.87, 5.57 | ||
| Education/health care/social services | 0.50 | 0.18, 1.41 | 1.27 | 0.44, 3.73 | ||
| Arts/entertainment/hospitality | 0.50 | 0.13, 1.95 | 2.92 | 0.82, 10.33 | ||
| Years in same job | 1.01 | 0.98, 1.04 | 0.59 | 1.01 | 0.98, 1.04 | 0.45 |
CI, confidence interval; OR, odds ratio; RTW, return to work.
Table 5 presents results of the adjusted logistic regression models for each outcome, assessing each workplace factor in turn. Each of these models included all covariates, along with one of the workplace factors of interest. With two exceptions, the direction of association was as hypothesized, i.e., the presence of the hypothetically more protective condition of each workplace factor was at least suggestive of a lower odds of both RTW interruption and reinjury. As was the case for the unadjusted bivariate associations (Table 2), both exceptions involved the reinjury outcome, and neither was statistically significant: (1) adequate employer/health care provider communication, and (2) not stigmatized for PPD by coworkers. Despite alignment with the hypothesized direction of association, two of the workplace factors—provision of needed job accommodations and adequate safety training—were not significantly associated with either outcome. Figure 1 depicts the statistically significant associations presented in Table 5.
Table 5.
Logistic regression results, adding each workplace factor in turn to the two basic outcome models: whether no longer working at interview (RTW interruption), and whether reinjured in the current/most recent job (N=567).
| Workplace factor | Variable type | N | RTW interrupted | Reinjured | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |||
| Job accommodations | Categorical | 558 | ||||||
| Needed but not provided | ref | ref | ref | ref | ref | ref | ||
| Needed and provided | 0.74 | 0.36, 1.50 | 0.40 | 0.64 | 0.29, 1.38 | 0.26 | ||
| Not needed | 0.46 | 0.21, 1.02 | 0.06 | 0.44 | 0.20, 0.96 | 0.04 | ||
| Adequate employer/health care provider communication | Binary | 484 | 0.35 | 0.19, 0.64 | 0.001 | 1.12 | 0.57, 2.22 | 0.74 |
| Adequate training to do job safely | Binary | 561 | 0.56 | 0.27, 1.15 | 0.11 | 0.60 | 0.28, 1.26 | 0.18 |
| Presence of health and safety committee | Binary | 525 | 0.85 | 0.42, 1.73 | 0.66 | 0.46 | 0.23, 0.95 | 0.04 |
| Comfortable reporting unsafe situation at work | Binary | 565 | 0.38 | 0.13, 1.07 | 0.07 | 0.29 | 0.11, 0.77 | 0.01 |
| Not stigmatized for PPD by supervisor | Binary | 565 | 0.25 | 0.13, 0.49 | <0.001 | 0.49 | 0.24, 1.04 | 0.06 |
| Not stigmatized for PPD by coworkers | Binary | 567 | 0.26 | 0.12, 0.58 | 0.001 | 1.51 | 0.54, 4.22 | 0.43 |
| Low job strain | Binary | 544 | 0.68 | 0.34, 1.40 | 0.30 | 0.49 | 0.24, 0.98 | 0.04 |
| Organization-level safety climate | Standardized | 546 | 0.64 | 0.51, 0.81 | <0.001 | 0.64 | 0.50, 0.82 | <0.001 |
| Group-level safety climate | Standardized | 551 | 0.56 | 0.45, 0.71 | <0.001 | 0.69 | 0.54, 0.89 | 0.004 |
| Supervisor support | Standardized | 551 | 0.50 | 0.40, 0.63 | <0.001 | 0.68 | 0.53, 0.86 | 0.001 |
| Coworker support | Standardized | 546 | 0.70 | 0.55, 0.90 | 0.006 | 0.92 | 0.71, 1.19 | 0.51 |
| Social support | Standardized | 541 | 0.53 | 0.41, 0.67 | <0.001 | 0.73 | 0.56, 0.94 | 0.02 |
| Able to take time off work for personal/family matters | Standardized | 559 | 0.75 | 0.57, 0.97 | 0.03 | 0.79 | 0.62, 0.99 | 0.046 |
CI, confidence interval; OR, odds ratio; PPD, permanent partial disability; RTW, return to work.
Figure 1.
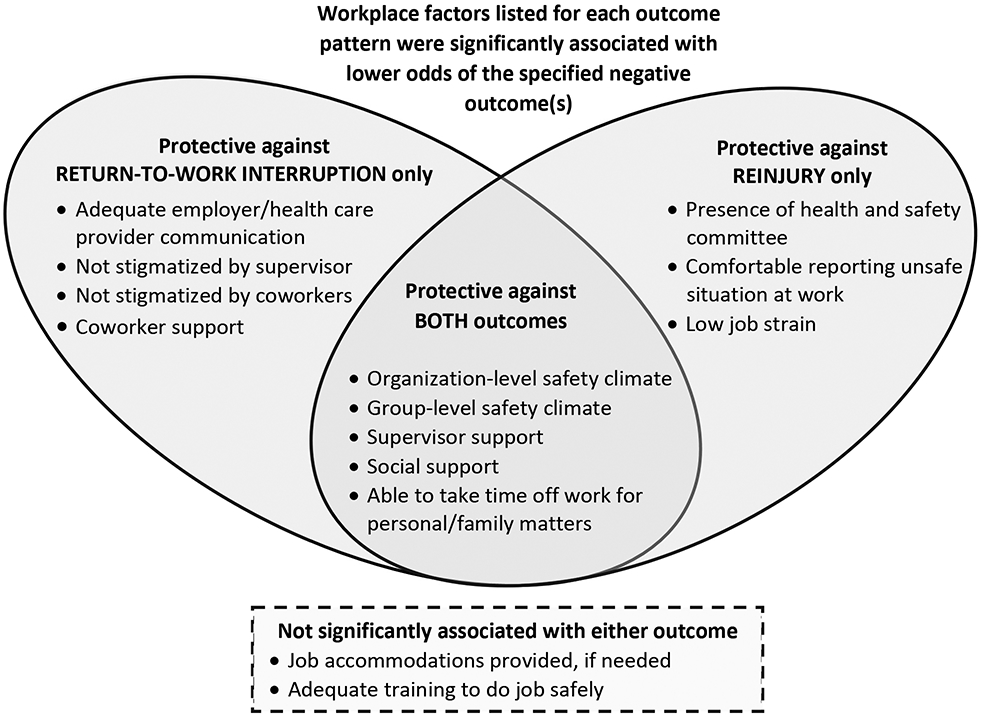
Workplace factors: Patterns of association with study outcomes.
Odds ratios for the binary variables in Table 5 represent effect sizes based on presence or absence of the hypothetically more protective condition, while odds ratios for the standardized variables represent effect sizes based on one standard deviation of difference; hence effect sizes cannot be directly compared across variable type. With respect to RTW interruption, absence of stigmatization by supervisors or by coworkers had the largest effect sizes among binary variables. Supervisor support had the largest effect size among standardized variables; social support was a close second, driven by the supervisor support component. With respect to reinjury, comfort reporting an unsafe work situation had the largest effect size among binary variables. Organization-level safety climate had the largest effect size among standardized variables, nearly matched by group-level safety climate and supervisor support (again, social support closely followed supervisor support).
Testing for interactions between each workplace factor and degree of impairment revealed no notable or statistically significant findings, and no consistent direction of association; therefore, the interaction term was dropped from all regression models. Data for the WHQ versions of the social support, supervisor support, and coworker support variables are reported in Table 5. Findings based on the JCQ versions of these three variables were substantially similar (see data in Supplementary Table S2, available at Annals of Work Exposures and Health online).
DISCUSSION
Lower reported levels of safety climate, supervisor support, and ability to take time off work for personal/family matters were significantly associated with both RTW interruption and reinjury. Inadequate employer/health care provider communication, perceived stigmatization from supervisors and/or coworkers, and lower levels of coworker support were significantly associated with RTW interruption but not with reinjury. Discomfort with reporting an unsafe situation at work, absence of a health and safety committee, and higher job strain were significantly associated with reinjury, but not with RTW interruption. However, inadequate safety training and lack of needed job accommodations were not significantly associated with either outcome. Despite null findings, we are not suggesting that job accommodation and adequate safety training are unimportant. As described earlier, there is strong evidence for the importance of job accommodations, but they may be most important for initial RTW. All workers interviewed for our study had RTW, and only 13% had not obtained needed job accommodations.
To effectively promote safe and sustained RTW, our findings support expanding the focus of prevention efforts to include organizational and psychosocial factors, such as safety climate, supervisor support, and flexible time off work. Factors we found protective for either negative outcome may be as important as those that were protective for both, depending on workplace characteristics and WC system goals. The lack of interaction between any of these workplace factors and degree of impairment suggests that these findings may be generalizable to all workers, and further, that workplace interventions based on these findings may be useful for both primary and secondary prevention.
The most frequently reported reason for RTW interruption was impairment, disability, and/or pain from the previous work injury. Workers ages 65 and older (compared to ages 18 to 34) had over three times the odds of RTW interruption. Early retirement due to a work injury is associated with more severe injuries, as well as with potentially modifiable factors, such as a less supportive workplace (Pransky et al., 2005).
In our study, supervisor support and coworker support had differing associations with outcomes; thus, consolidating the two as social support—as is often done—may result in less informative findings. Using only a single item for each construct resulted in decidedly similar findings compared to using four items, which should facilitate inclusion of both constructs in future surveys.
For all workplace factors in this study, the prevalence of the more desirable condition was above 70%, and over 95% were comfortable reporting an unsafe situation at work. This may have implications for interpretation of our findings, since these factors can interact in complex ways. For example, in a Canadian study, workers who reported no supervisor support in conjunction with any type of occupational health and safety vulnerability (including discomfort reporting unsafe conditions) were significantly more likely to experience workplace injuries (Yanar et al., 2019). Yet, a recent study of workplace exposures ranked ergonomic and work organization/psychosocial exposures as the most prevalent exposures in the northwest U.S. workforce (Doubleday et al., 2019).
Another notable characteristic of our sample was the high prevalence of union membership (42.5%)—more than double the estimated 19.8% of Washington State employed workers who were union members in 2018, and more than quadruple the estimated 10.5% for the U.S. overall [42]. Union membership may be associated with better safety climate (Gillen et al., 2002), and possibly accounts in part for the observed prevalence of these workplace factors. In future research, we plan to assess this issue further. Because we don’t have union membership status for survey non-respondents, we cannot be certain whether response bias affected the prevalence of union membership in our sample; however, we did not observe any noteworthy differences in many other characteristics used to assess response bias (Sears et al., 2020). Though speculative, there are several possible mechanisms that would tend to select union members into our sampling frame. First, if union members tend to be in riskier jobs, they might more often be injured—and union members in this survey did have higher rates of self-reported reinjury. Second, union members may feel safer reporting an injury and filing a WC claim. Third, union members may have better access to legal resources, which may be more likely to result in a PPD award. Finally, union members may be more likely to RTW after a PPD award, which would have made them more likely eligible for this survey.
Numerous studies have supported the need for research-driven prevention programs designed to reduce reinjury risk and sustain RTW (Lipscomb et al., 2008; Cherry et al., 2010; Young, 2010b, 2010a; Ruseckaite and Collie, 2011; Berecki-Gisolf et al., 2012; MacEachen et al., 2012; Keeney et al., 2013; Kosny et al., 2013; Landsbergis et al., 2014; Nevala et al., 2015; Midtsundstad and Nielsen, 2016; Spector and Reul, 2017). This study provides evidence to support prioritizing several modifiable organizational and psychosocial factors for future intervention development. Systemic support from WC agencies/insurers may be needed to develop and test efficient large-scale WC system-level interventions (e.g., management training, educational campaigns, subsidies/incentives), and encourage uptake. Individual employers, particularly small employers, may not have the resources or motivation to implement interventions targeting these workplace factors. However, it may be feasible to develop and offer trainings to educate employers about key workplace organizational and psychosocial factors, perhaps in-hand with financial support for supervisor training or structural changes. Supervisor training programs can improve safety climate and confidence managing successful RTW (Spector and Reul, 2017; Schwatka et al., 2019). Further, systematic reviews have documented that interventions designed to promote workplace social support, job control, and job demands can positively impact absenteeism, productivity and financial outcomes (Wagner et al., 2015; Williams-Whitt et al., 2015). As a WC system-level example, Stay at Work is an L&I program designed to reduce temporary total disability. Employers are reimbursed for certain costs of offering light-duty jobs to injured workers (e.g., wage subsidies, training, tools). Since 2012, more than 4,500 employers have used this program to assist more than 20,000 injured workers. Potential savings are not trivial—L&I estimated saving $700 million in work disability and medical costs from Stay at Work and other RTW initiatives (Washington State Department of Labor and Industries, 2016).
Strengths and limitations
Our survey of workers with permanent impairment was population-based. Many studies have focused on initial RTW after occupational injury; however, relatively few have examined modifiable workplace factors associated with sustained RTW, RTW interruption, and reinjury, particularly among permanently impaired workers. Our inclusion of workers with any type and degree of permanent impairment enhances generalizability to a broad range of injuries and conditions. The survey was focused on characteristics and outcomes of the current or most recent job, in order to assess the most proximate workplace factors, and to minimize recall barriers. Though representative, the survey was cross-sectional and relatively small-scale. Recall bias is a potential threat to the validity of our findings, since workplace exposure and worker outcome data were collected simultaneously.
CONCLUSIONS
This study provides evidence that several potentially modifiable organizational and psychosocial factors are associated with safe and sustained RTW among injured workers with work-related permanent impairment, and potentially among all workers. These factors include safety climate, supervisor support, coworker support, absence of stigmatization by supervisors or coworkers, health and safety committees, ability to take time off work for personal or family matters, adequate employer/health care provider communication, comfort reporting unsafe situations at work, and low job strain. Though primary prevention is key, secondary prevention efforts to sustain RTW and prevent reinjury may reduce the considerable health, economic, and social burden of occupational injuries.
Supplementary Material
What's important about this paper.
Employment is a critical social determinant of health, and successful return to work after a work-related injury is important for the health and economic stability of workers and for workplace productivity. This study provides evidence that several potentially modifiable organizational and psychosocial factors are associated with safe and sustained RTW. Although this study focused on injured workers with permanent impairment, the lack of interaction between degree of impairment and any of the workplace factors studied suggests that these findings may be generalizable to all workers, and further, that workplace interventions based on these findings may be useful for both primary and secondary prevention. This study focused on modifiable workplace factors that may be amenable to large-scale workers’ compensation-based interventions, thus laying the groundwork for development and testing of efficient system-level interventions.
Acknowledgements
We thank all survey participants for their time and input. We also thank Lisann Rolle and Sarah West, Research and Data Services, Washington State Department of Labor and Industries, who facilitated access to the necessary administrative data and provided extensive data documentation.
Declaration
Funding for this work was provided by a NIOSH grant (R21OH011355). The authors declare no conflict of interest relating to the material presented in this article. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
REFERENCES
- Baidwan NK, Gerberich SG, Kim H, et al. (2019) A longitudinal study of work-related psychosocial factors and injuries: implications for the aging United States workforce. Am J Ind Med; 62: 212–21. [DOI] [PubMed] [Google Scholar]
- Berecki-Gisolf J, Clay FJ, Collie A, et al. (2012) Predictors of sustained return to work after work-related injury or disease: insights from workers' compensation claims records. J Occup Rehabil; 22: 283–91. [DOI] [PubMed] [Google Scholar]
- Bultmann U, Franche RL, Hogg-Johnson S, et al. (2007) Health status, work limitations, and return-to-work trajectories in injured workers with musculoskeletal disorders. Qual Life Res; 16: 1167–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler R, Johnson W, Baldwin M. (1995) Managing work disability: why first return to work is not a measure of success. Industrial and Labor Relations Review; 48: 452–69. [Google Scholar]
- Campolieti M (2002) The recurrence of occupational injuries: estimates from a zero inflated count model. Applied Economics Letters; 9: 595–600. [Google Scholar]
- Carroll C, Rick J, Pilgrim H, et al. (2010) Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil; 32: 607–21. [DOI] [PubMed] [Google Scholar]
- Casey R, Ballantyne PJ. (2017) Diagnosed chronic health conditions among injured workers with permanent impairments and the general population. J Occup Environ Med; 59: 486–96. [DOI] [PubMed] [Google Scholar]
- Cherry NM, Sithole F, Beach JR, et al. (2010) Second WCB claims: who is at risk? Can J Public Health; 101 Suppl 1: S53–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong M, de Boer AG, Tamminga SJ, et al. (2015) Quality of working life issues of employees with a chronic physical disease: a systematic review. J Occup Rehabil; 25: 182–96. [DOI] [PubMed] [Google Scholar]
- Doubleday A, Baker MG, Lavoue J, et al. (2019) Estimating the population prevalence of traditional and novel occupational exposures in Federal Region X. Am J Ind Med; 62: 111–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etuknwa A, Daniels K, Eib C. (2019) Sustainable return to work: a systematic review focusing on personal and social factors. J Occup Rehabil; 29: 679–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franche RL, Cullen K, Clarke J, et al. (2005) Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil; 15: 607–31. [DOI] [PubMed] [Google Scholar]
- Gillen M, Baltz D, Gassel M, et al. (2002) Perceived safety climate, job demands, and coworker support among union and nonunion injured construction workers. J Safety Res; 33: 33–51. [DOI] [PubMed] [Google Scholar]
- Haveraaen LA, Skarpaas LS, Aas RW. (2017) Job demands and decision control predicted return to work: the rapid-RTW cohort study. BMC Public Health; 17: 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haveraaen LA, Skarpaas LS, Berg JE, et al. (2016) Do psychological job demands, decision control and social support predict return to work three months after a return-to-work (RTW) programme? The rapid-RTW cohort study. Work; 53: 61–71. [DOI] [PubMed] [Google Scholar]
- Huang Y-h, Zohar D, Robertson MM, et al. (2013a) Development and validation of safety climate scales for lone workers using truck drivers as exemplar. Transp Res Part F Traffic Psychol Behav; 17: 5–19. [Google Scholar]
- Huang Y, Lee J, Chen Z, et al. (2017a) An item-response theory approach to safety climate measurement: the Liberty Mutual Safety Climate Short Scales. Accid Anal Prev; 103: 96–104. [DOI] [PubMed] [Google Scholar]
- Huang YH, Lee J, McFadden AC, et al. (2016) Beyond safety outcomes: an investigation of the impact of safety climate on job satisfaction, employee engagement and turnover using social exchange theory as the theoretical framework. Appl Ergon; 55: 248–57. [DOI] [PubMed] [Google Scholar]
- Huang YH, Lee J, McFadden AC, et al. (2017b) Individual employee's perceptions of "Group-level Safety Climate" (supervisor referenced) versus "Organization-level Safety Climate" (top management referenced): associations with safety outcomes for lone workers. Accid Anal Prev; 98: 37–45. [DOI] [PubMed] [Google Scholar]
- Huang YH, Zohar D, Robertson MM, et al. (2013b) Development and validation of safety climate scales for mobile remote workers using utility/electrical workers as exemplar. Accid Anal Prev; 59: 76–86. [DOI] [PubMed] [Google Scholar]
- Jetha A, LaMontagne AD, Lilley R, et al. (2018) Workplace social system and sustained return-to-work: a study of supervisor and co-worker supportiveness and injury reaction. J Occup Rehabil; 28: 486–94. [DOI] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, et al. (1998) The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol; 3: 322–55. [DOI] [PubMed] [Google Scholar]
- Katz AS, Pronk NP, McLellan D, et al. (2019) Perceived workplace health and safety climates: associations with worker outcomes and productivity. Am J Prev Med; 57: 487–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeney BJ, Turner JA, Fulton-Kehoe D, et al. (2013) Early predictors of occupational back reinjury: results from a prospective study of workers in Washington State. Spine (Phila Pa 1976); 38: 178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsh B, Slack T, King CA. (2012) The nature and impact of stigma towards injured workers. J Occup Rehabil; 22: 143–54. [DOI] [PubMed] [Google Scholar]
- Kosny A, Lifshen M, Pugliese D, et al. (2013) Buddies in bad times? The role of co-workers after a work-related injury. J Occup Rehabil; 23: 438–49. [DOI] [PubMed] [Google Scholar]
- Kraatz S, Lang J, Kraus T, et al. (2013) The incremental effect of psychosocial workplace factors on the development of neck and shoulder disorders: a systematic review of longitudinal studies. Int Arch Occup Environ Health; 86: 375–95. [DOI] [PubMed] [Google Scholar]
- Krause N, Dasinger LK, Neuhauser F. (1998) Modified work and return to work: a review of the literature. J Occup Rehabil; 8: 113–39. [Google Scholar]
- Landsbergis PA, Grzywacz JG, LaMontagne AD. (2014) Work organization, job insecurity, and occupational health disparities. Am J Ind Med; 57: 495–515. [DOI] [PubMed] [Google Scholar]
- Landsbergis PA, Schnall PL, Pickering TG, et al. (2002) Validity and reliability of a work history questionnaire derived from the Job Content Questionnaire. J Occup Environ Med; 44: 1037–47. [DOI] [PubMed] [Google Scholar]
- Lay AM, Saunders R, Lifshen M, et al. (2017) The relationship between occupational health and safety vulnerability and workplace injury. Saf. Sci; 94: 85–93. [Google Scholar]
- Lee SJ, You D, Gillen M, et al. (2015) Psychosocial work factors in new or recurrent injuries among hospital workers: a prospective study. Int Arch Occup Environ Health; 88: 1141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippel K (2007) Workers describe the effect of the workers' compensation process on their health: a Quebec study. Int J Law Psychiatry; 30: 427–43. [DOI] [PubMed] [Google Scholar]
- Lipscomb HJ, Cameron W, Silverstein B. (2008) Incident and recurrent back injuries among union carpenters. Occup Environ Med; 65: 827–34. [DOI] [PubMed] [Google Scholar]
- MacEachen E, Kosny A, Ferrier S, et al. (2012) The 'ability' paradigm in vocational rehabilitation: challenges in an Ontario injured worker retraining program. J Occup Rehabil; 22: 105–17. [DOI] [PubMed] [Google Scholar]
- McLaren CF, Reville RT, Seabury SA. (2017) How effective are employer return to work programs? International Review of Law and Economics; 52: 58–73. [Google Scholar]
- Midtsundstad TI, Nielsen RA. (2016) Do workplace interventions reduce disability rates? Occup Med (Lond); 66: 691–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. (2013) Quality of Worklife Questionnaire. Available at http://www.cdc.gov/niosh/topics/stress/qwlquest.html. Accessed July 3, 2020.
- Nevala N, Pehkonen I, Koskela I, et al. (2015) Workplace accommodation among persons with disabilities: a systematic review of its effectiveness and barriers or facilitators. J Occup Rehabil; 25: 432–48. [Google Scholar]
- Pransky GS, Benjamin KL, Savageau JA. (2005) Early retirement due to occupational injury: who is at risk? Am J Ind Med; 47: 285–95. [DOI] [PubMed] [Google Scholar]
- Price J, Shi J, Lu B, et al. (2012) Nonoccupational and occupational injuries to US workers with disabilities. Am J Public Health; 102: e38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reme SE, Shaw WS, Boden LI, et al. (2014) Worker assessments of organizational practices and psychosocial work environment are associated with musculoskeletal injuries in hospital patient care workers. Am J Ind Med; 57: 810–8. [DOI] [PubMed] [Google Scholar]
- Ruseckaite R, Collie A. (2011) Repeat workers' compensation claims: risk factors, costs and work disability. BMC Public Health; 11: 492–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruseckaite R, Collie A. (2013) The incidence and impact of recurrent workplace injury and disease: a cohort study of WorkSafe Victoria, Australia compensation claims. BMJ Open; 3: e002396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schur L, Han K, Kim A, et al. (2017) Disability at work: a look back and forward. J Occup Rehabil; 27: 482–97. [DOI] [PubMed] [Google Scholar]
- Schwatka NV, Goldenhar LM, Johnson SK, et al. (2019) A training intervention to improve frontline construction leaders' safety leadership practices and overall jobsite safety climate. J Safety Res; 70: 253–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears JM, Schulman BA, Fulton-Kehoe D, et al. (2020) Workforce reintegration after work-related permanent impairment: a look at the first year after workers’ compensation claim closure. J Occup Rehabil; Online First: July 10, 2020; doi: 10.1007/s10926-020-09912-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears JM, Schulman BA, Fulton-Kehoe D, et al. (In press.) Estimating time to reinjury among Washington State injured workers by degree of permanent impairment: using state wage data to adjust for time at risk. Am J Ind Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi J, Gardner S, Wheeler KK, et al. (2015a) Characteristics of nonfatal occupational injuries among U.S. workers with and without disabilities. Am J Ind Med; 58: 168–77. [DOI] [PubMed] [Google Scholar]
- Shi J, Wheeler KK, Lu B, et al. (2015b) Medical expenditures associated with nonfatal occupational injuries among U.S. workers reporting persistent disabilities. Disabil Health J; 8: 397–406. [DOI] [PubMed] [Google Scholar]
- Smith TD, DeJoy DM. (2012) Occupational injury in America: an analysis of risk factors using data from the General Social Survey (GSS). J Safety Res; 43: 67–74. [DOI] [PubMed] [Google Scholar]
- Spector JT, Reul NK. (2017) Promoting early, safe return to work in injured employees: a randomized trial of a supervisor training intervention in a healthcare setting. J Occup Rehabil; 27: 70–81. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017) Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- Stuart H (2004) Stigma and work. Healthcare Papers; 5: 100–11. [DOI] [PubMed] [Google Scholar]
- Sundar V (2017) Operationalizing workplace accommodations for individuals with disabilities: a scoping review. Work; 56: 135–55. [DOI] [PubMed] [Google Scholar]
- Teufer B, Ebenberger A, Affengruber L, et al. (2019) Evidence-based occupational health and safety interventions: a comprehensive overview of reviews. BMJ Open; 9: e032528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tompa E, de Oliveira C, Dolinschi R, et al. (2008) A systematic review of disability management interventions with economic evaluations. J Occup Rehabil; 18: 16–26. [DOI] [PubMed] [Google Scholar]
- Tveito TH, Sembajwe G, Boden LI, et al. (2014) Impact of organizational policies and practices on workplace injuries in a hospital setting. J Occup Environ Med; 56: 802–8. [DOI] [PubMed] [Google Scholar]
- Villotti P, Gragnano A, Lariviere C, et al. (2020) Tools appraisal of organizational factors associated with return-to-work in workers on sick leave due to musculoskeletal and common mental disorders: a systematic search and review. J Occup Rehabil; Online First. doi: 10.1007/s10926-020-09902-1. [DOI] [PubMed] [Google Scholar]
- Wagner SL, White MI, Schultz IZ, et al. (2015) Social support and supervisory quality interventions in the workplace: a stakeholder-centered best-evidence synthesis of systematic reviews on work outcomes. Int J Occup Environ Med; 6: 189–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington State Department of Labor and Industries. (2016) L&I's Stay at Work Program hits major milestones — more than 20,000 workers helped. Available at http://lni.wa.gov/News/2016/pr161129a.asp. Accessed May 12, 2017.
- Washington State Department of Labor and Industries. (2019) Medical Examiners' Handbook. Publication F252–001-000.
- Weiss E, Murphy G, Boden LI. (2019) Workers’ Compensation: Benefits, Costs, and Coverage (2017 data). Washington, DC: National Academy of Social Insurance. [Google Scholar]
- White C, Green RA, Ferguson S, et al. (2019) The influence of social support and social integration factors on return to work outcomes for individuals with work-related injuries: a systematic review. J Occup Rehabil; 29: 636–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White M, Wagner S, Schultz IZ, et al. (2013) Modifiable workplace risk factors contributing to workplace absence across health conditions: a stakeholder-centered best-evidence synthesis of systematic reviews. Work; 45: 475–92. [DOI] [PubMed] [Google Scholar]
- Williams-Whitt K, White MI, Wagner SL, et al. (2015) Job demand and control interventions: a stakeholder-centered best-evidence synthesis of systematic reviews on workplace disability. Int J Occup Environ Med; 6: 61–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanar B, Lay M, Smith PM. (2019) The interplay between supervisor safety support and occupational health and safety vulnerability on work injury Saf Health Work; 10: 172–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yassi A, Lockhart K, Sykes M, et al. (2013) Effectiveness of joint health and safety committees: a realist review. Am J Ind Med; 56: 424–38. [DOI] [PubMed] [Google Scholar]
- Young AE. (2009) Return-to-work experiences: prior to receiving vocational services. Disabil Rehabil; 31: 2013–22. [DOI] [PubMed] [Google Scholar]
- Young AE. (2010a) Employment maintenance and the factors that impact it after vocational rehabilitation and return to work. Disabil Rehabil; 32: 1621–32. [DOI] [PubMed] [Google Scholar]
- Young AE. (2010b) Return to work following disabling occupational injury--facilitators of employment continuation. Scand J Work Environ Health; 36: 473–83. [DOI] [PubMed] [Google Scholar]
- Yu Z, Lin H-C, Smith TD, et al. (2018) Association between workplace harassment and occupational injury among adult workers in the United States. Saf. Sci; 110(Part A): 372–79. [Google Scholar]
- Zierold KM. (2016) Perceptions of supervision among injured and non-injured teens working in the retail or service industry. Workplace Health Saf; 64: 152–62. [DOI] [PubMed] [Google Scholar]
- Zwerling C, Sprince NL, Davis CS, et al. (1998a) Occupational injuries among older workers with disabilities: a prospective cohort study of the Health and Retirement Survey, 1992 to 1994. Am J Public Health; 88: 1691–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwerling C, Sprince NL, Wallace RB, et al. (1996) Risk factors for occupational injuries among older workers: an analysis of the Health and Retirement Study. Am J Public Health; 86: 1306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwerling C, Whitten PS, Davis CS, et al. (1998b) Occupational injuries among older workers with visual, auditory, and other impairments. A validation study. J Occup Environ Med; 40: 720–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


