Abstract
Although recognized as effective measures to curb the spread of the COVID19 outbreak, social distancing and home confinement have generated a mental health burden with older adults who are considered to be more vulnerable to psychosocial strains. To date, the application of digital technologies in response to COVID-19 pandemic has been narrowed to public-health needs related to containment and mitigation. However, information and communications technology (ICT)-based initiatives directed toward prediction and prevention of psychosocial support are still limited. Given the power of digital health solutions to allow easy and accurate characterization and intervention for health and disease, as well as to flatten the COVID19 incidence curves in many countries, our ECLB-COVID19 consortium is highlighting the importance of providing innovative ICT-based solutions (ICT-COVID-Companion) to improve elderly physical and mental health, thereby preventing/dampening psychosocial strain during pandemics. Based on innovative approaches (e.g., emotional/social computing, open social platform, interactive coaching, gamification, fitness-tracker, internet of things) and smart digital solutions (smartwatch/smartphone), smart companions must provide safe personalised physical, mental and psychosocial health surveillance. Additionally, by delivering personalised multi-dimension crisis-oriented health recommendations, such innovative crisis-oriented solutions would help (i) facilitate a user’s adherence to active and healthy confinement lifestyle (AHCL), (ii) achieve a rapid psychosocial recovery in case of depression issues and (iii) enhance preparedness for eventual future pandemics.
Keywords: SARS-CoV-2, Information and communications, technology (ICT), Digital health, Physical activity, Mental health, Home confinement, Psychosocial strain, Seniors
BACKGROUND
On December 31, 2019 the first case of a new coronavirus (SARS-CoV-2) detected in Wuhan (China) was reported to the World Health Organisation (WHO) country office in China. The disease called “COVID-19”, was declared by the WHO as global pandemic on March 11th, 2020, and presented a serious challenge facing all societies. The virus has rapidly spread around the world, with the number of infected pneumonia patients far exceeding that of SARS (severe acute respiratory syndrome) in 2003.
In only 9 months, COVID19 affected nearly 30 million people (up to September 30, 2020), including more than 1 million deaths [1]. Due to the ever-growing number of confirmed cases and in order to decelerate the rapid overwhelming of health systems, lockdowns with home-confinement and social distancing measures were implemented by public health authorities around the world [2]. Home confinement has been utilised previously to combat infectious diseases (e.g., cholera, SARS, Ebola) and, along with hygiene care, has been identified as the best non-pharmacological prevention solution. However, the level of confinement applied to the global population during COVID19 is considered to be the most severe in history and has disrupted normal lifestyles, generating psychosocial strain throughout the population [3,4].
Psychosocial consequences of the COVID-19 pandemic for the public
A recent report highlighted the urgent need for research to help improve our understanding of the pandemic’s mental health consequences on the general public [5]. In order to help characterise the psychosocial effects of the COVID19 crisis as well as the moderators of these effects, our ECLB-COVID19 research group (a consortium including over 60 scientists worldwide) launched a multi-language, multi-centre anonymous online survey to assess the “Effects of home Confinement on psychosocial health status and multiple Lifestyle Behaviors” during the COVID-19 outbreak. Preliminary findings from this project revealed that the COVID19 home confinement resulted in significant negative effects on mental wellbeing and emotional status, with more people experiencing psychosocial and emotional distress compared to before the pandemic [6,7]. Additionally, unhealthy lifestyle behaviors were significantly associated with these psychosocial tolls. Our data have shown an increased number of individuals that are: (i) physically (+15.2%) [8] and socially (71.2%) [9] inactive, (ii) experiencing poor sleep quality (12.8%) [6], (iii) exhibiting unhealthy dietary behaviors (10%) [7], and (iv) dealing with unemployment (6%) [6]. In addition, participants have demonstrated a higher acceptance rate (15%) toward the use of technology-based solutions during this same period [6].
Taking together, these preliminary findings suggest that COVID19-related confinement effects are having a vast negative impact on mood-state, well-being and lifestyle behaviors of the general population [6]. As a result, mitigation strategies are important and should be addressed by all stakeholders. Our research group recently suggested that engaging in indoor and/or outdoor physical activity, whilst conforming with distancing and hygiene recommendations, may be a preliminary measure for promoting physical and mental benefits [7]. Moreover, as participants in our previous studies showed higher acceptance rates toward the use of technology during this confinement period, promoting healthy lifestyle behaviors (i.e., physical and social activity, healthy diet and good sleep quality) through Information and Communication Technologies (ICT)-based solutions may be an efficient approach to foster an Active and Healthy Confinement Lifestyle (AHCL) [6,7].
Physical inactivity is well recognised as a modifiable risk factor for several chronic diseases [10]. A previous large-scale global investigation reported that physical inactivity causes 9% of premature mortality and 6–10% of the major non-communicable diseases (i.e., 5.8% of coronary heart disease, 7.2% of type 2 diabetes, 10.1% of breast and 9.4% of colon cancers) [11]. Additionally, physical inactivity is suggested to contribute to one third of global Alzheimer’s disease cases [12]. Similarly, social inactivity relates to higher rates of mortality, morbidity, and lower quality of life [13]. Fortunately, physical activity and/or exercise is a low-cost intervention for the prevention of numerous chronic diseases [14], while participating in personal leisure activities (a form of social participation) is of high importance for physical health, mental health, and improved quality of life [15]. Furthermore, physical exercise exerts anti-inflammatory effects [16] and may be beneficial against viral diseases such as COVID19 [17]. A recent report indicates that physical exercise helped promote mental wellbeing [18] while reducing the severity of acute respiratory infection symptoms and the number of symptom days (-2.24 days) during the follow-up period [19]. In light of these data, we recently recommend the inclusion of home-based physical activity and online social interactions, among other intervention domains (e.g, recommending healthy diet and cognitive training and improving sleep quality) as part of a multidimension crisis-oriented mitigation strategy to counteract psychosocial strain caused by the COVID19 pandemic [20–22]. Furthermore, our own systematic reviews revealed that reduced physical activity levels and social participation are serious concerns during home confinement in pandemic times and we further recommended gamification strategies in order to combine social belonging elements, cognitive training, and home-based physical activity programs to improve AHCL during pandemics.
The strengths of our preliminary studies are that the cross-disciplinary survey was (i) fully anonymous, (ii) provided in multiple languages, and (iii) widely distributed in several continents, thus enabling the ability to collect the data very quickly. Over 60 international scientists from different disciplines cooperated to make this possible. However, it should be acknowledged that there were limitations of this strategy in that it did not allow for narrow targeting of specific groups with defined inclusion and exclusion criteria. Additionally, the moderation effects of demographic and cultural variables have not been studied and there was no age-criteria-based sub-samples analysis. Consequently, risk-factors relating to psychosocial toll during the COVID19 outbreak among more vulnerable populations, such as older-adults, is still not well understood. As a result, our preliminary recommendations to maintain AHCL during times of pandemic mainly target the general population, with no specific consideration for more vulnerable populations.
Caring for the physical and psycho-social health of seniors during pandemics
COVID19 has been documented to cause respiratory infection with clinical symptoms of viral pneumonia and acute respiratory distress syndrome in some patients [23]. In addition to respiratory symptoms, the disease can cause inflammation with associated multiorgan damage, coagulation abnormalities, acute kidney injury, acute heart failure, and rhabdomyolysis [23]. Furthermore, COVID-19 is associated with several neurological manifestations, including stroke, headache, and impaired consciousness [24]. Aging, a highly complex biological process, is inexorably associated with health declines and frailty, affecting several aspects of cognitive and motor functioning. Aging is also related to increased vulnerability to non-communicable diseases and rates of social exclusion [25]. Therefore, elderly are considered at high risk of developing severe illness from COVID19 [26]. Indeed, a recent report indicated that the number of hospitalized cases per 10,000 people was between 199 and 513 for elderly aged over 65 years old, while this number only ranged between 27 and 136 for young and middle-aged adults [26]. Being aware that they are increasingly vulnerable to develop severe illness from COVID19, older adults have also developed the greatest levels of stress, anxiety, and depression during the home confinement, leading to increased levels of loneliness and social isolation [27].
Consequently, the WHO recommends that particular attention be given to alleviate risk factors associated with the negative mental health symptoms experienced by older adults during times of pandemics. However, the available recommendations provided by our preliminary work, as well as by many international organisations (e.g., WHO, the American Heart Association, or the American College of Sports Medicine), mainly target the general population. Therefore, the development of a personalized multidimension intervention for use in times of crisis is urgently needed for vulnerable sub-groups to prevent this psychosocial toll and augment governmental efforts to provide support for older adults. Additionally, given that policies are different across regions and countries, the categorization of recommendations for elderly populations, according to different social-distancing scenarios, is required. By capturing a more holistic view of behavioral changes and the associated consequences on mental health among older adults from different regions during the COVID19 home confinement, such interventions would provide personalised recommendations covering the majority of psychosocial risk factors. Thus, effectively responding to the need for a multi-dimensional crisis-oriented approach assessing a range of essential lifestyle metrics (e.g., physical, cognitive and social activities, diet and sleep behaviors, and emotional aspects) is warranted in older adults.
As such an intervention requires accurate user profiling and must provide personalised multidomain recommendations to be delivered to end-users via multimodal techniques (e.g., multilanguage vocal and chats interaction, interactive coaching), this intervention strategy is only feasible if integrated in an innovative solution based on ICTs.
Information and Communication Technologies to support the crisis-oriented intervention
ICTs provide a range of technologies for gathering, storing, retrieving, processing, analysing, transmitting, and receiving data and information. With the widespread availability of smart solutions, wireless internet, digitalization, and sensors, ICTs have become an integral part of daily life and present an opportunity to facilitate the delivery of health services and enhance accessibility to personalised prevention and intervention programs [28–30]. Being aware of the potential impact that ICT could have on health-care delivery, the WHO has established the Global Observatory for e-Health (GOH) with the objective of improving the evidence base and guiding policies for integrating e-Health into health systems.
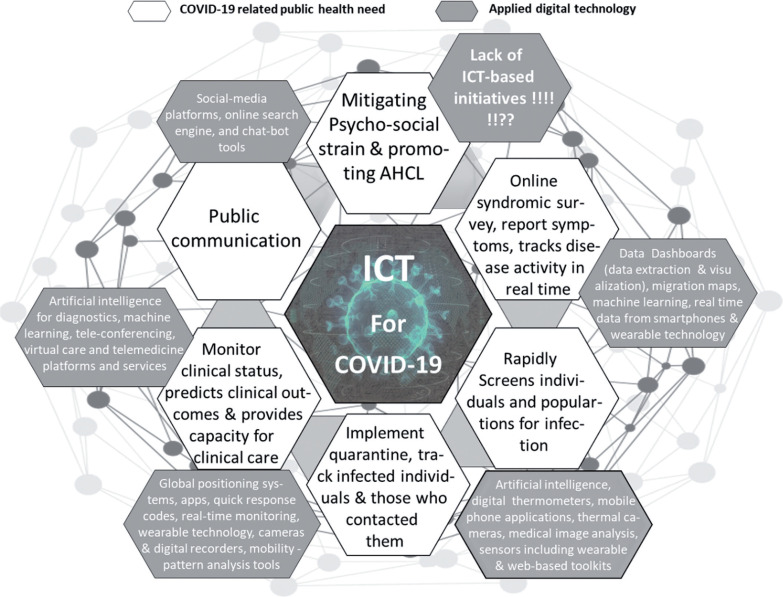
In accordance with this perspective, and due to the lack of an effective vaccine or therapy against the COVID-19 global pandemic so far, digital health technology is suggested as an effective solution to facilitate pandemic strategy management based on containment and mitigation [31–33]. Coordinated global government efforts have worked to develop strategies which include early surveillance, contact tracing, testing, interruption of community transmission, rapid identification of cases, strict quarantine, and clinical care. The scale of coordination and data management currently relies on digital technology adoption and policy/ healthcare integration [31–33]. Examples of these utilizations are below (Figure 1):
FIG. 1.
COVID-19 related public health need and the applied digital technology.
Note: ICT: Information and Communication Technology; AHCL: Active and Healthy Confinement Lifestyle.
Data dashboards (i.e., visualization, data extraction), machine learning, real-time smartphone data, migration maps, and wearable technology that can be used to report symptoms, complete online syndromic surveys, and track real time disease activity.
Digital thermometers, medical image analysis, artificial intelligence, thermal cameras, mobile phone applications, and sensors (wearable, web-based toolkits) used to screen individuals and populations rapidly to detect infection.
Quick response codes, global positioning systems, real-time monitoring of mobile devices, mobile phone applications, digital recorders/cameras, and wearable technology with the mobility-pattern tools for quarantine implementation and for the identification and tracking of infected individuals as well as those who may have come into close contact.
Artificial intelligence for machine learning, diagnostics, tele-conferencing, telemedicine and virtual care platforms/services for the monitoring of clinical status, prediction of clinical outcomes, and increase capacity in clinical care.
Social-media, search engines, and chat-bots have use for public communication.
Additionally, in non-crisis times, advances in biotechnology (e.g., wearable and environmental sensors), as well as remote health assessment, are widely applied to promote healthy lifestyle, reduce health services utilization, and decrease costs by identifying changes in health that can inform early diagnosis, timeliness of care, enhance treatment adherence and improve health outcomes [28–30]. However, unhealthy lifestyle (e.g., social isolation, loneliness, physical inactivity, poor sleep habits) and the resulting psychosocial strain among the general population [6–9, 34], as well as in older adults, are considered a global challenge in the context of COVID19 [27]. The application of digital technologies during the COVID19 pandemic management and response was primarily limited to containment and mitigation processes while, to the best of the author’s knowledge, use of ICT-based initiatives directed toward public-health psychosocial support have been sparse. The use of digital tools to increase healthy behaviors has been already implemented in smart tools (mhealth apps, nutrition apps, fitness track, smart watch, etc.); however, these solutions generally deal with each component individually (physical activity, diet, mood, social participation, chat-bot etc.) and to date, no solution is able to provide a personalised crisis-oriented healthy behavior accompaniment.
Taking into-consideration the emerging evidence for digital health solutions to potentially allow easy and accurate prediction and intervention in health and disease [35], as well as to flatten the COVID19 incidence curves in many countries [31–33], it appears appropriate that, in times of pandemic crisis, applying digital technology in a mental health dimension may help prevent the psychosocial strain and related risk factors in older adults. Based on innovative approaches (e.g., emotional/social computing, open social platform, interactive coaching, gamification, fitness-tracker, internet of things etc.) and via smart digital solutions (smartwatch/smartphone), we recommend the development of an ICT-based companion for older-adults. Such device would be highly beneficial in normal times, but especially during pandemic times. In compliance with data privacy regulation, this smart companion should provide safe personalised physical, mental and psychosocial health surveillance, as well as helping facilitate a user’s adherence to AHCL by delivering personalised multi-dimension crisis-oriented health recommendations (adapted to end-user’s environment and specific needs) based on cross-disciplinary expert-knowledge (Figure 2). Besides the beneficial effect on an end-user’s behaviors and psychosocial-health, we believe that such smart recommender/assistant system may also minimize unprecedented pressure on helpline centers during crisis-periods.
FIG. 2.
ICT-COVID-Companion concept.
Note: ICT: Information and Communication Technology; AI: Artificial Intelligence; GUI: Grafic user interface; VUI: Voice User Interface; IoT: Internet of Things.
CONCLUSIONS
Previous reports detailed that the highest risk of psychosocial strain during the COVID-19 home confinement period is found in older adults and these reports also provide a clear remit for the need of urgent implementation of technology-based intervention. Providing an affordable user-friendly ICT-based companion for pandemics lockdown could (i) identify the psychosocial and behavioural disorders and risk factors in the target population, (ii) deliver personalised recommendations, and thereby (iii) hopefully prevent/dampen psychosocial strain in older adults.
Conflicts of Interest
The authors declare no conflict of interest.
Details of funding
The author received no specific funding for this work.
REFERENCES
- 1.WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (assessed on 28 June 2020)
- 2.Jiang X, Niu Y, Li X, Li L, Cai W, Chen Y, Liao B, Wang E. Is a 14-day quarantine period optimal for effectively controlling coronavirus disease 2019 (COVID19)? medRxiv preprint. 2020:1–12. doi: 10.1101/2020.03.15.20036533. [DOI] [Google Scholar]
- 3.WHO . Mental health and psychosocial considerations during the COVID-19 outbreak. World Health Organization; https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf. Retrieved 18 Aout 2020. [Google Scholar]
- 4.Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. 2020. Available at SSRN 3561265. [DOI] [PMC free article] [PubMed]
- 5.Mahase E. Covid-19: Mental health consequences of pandemic need urgent research, paper advises. BMJ. 2020 doi: 10.1136/bmj.m1515. [DOI] [PubMed] [Google Scholar]
- 6.Ammar A, Trabelsi K, Brach M, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insight from the ECLB-COVID19 multicenter study. Biol Sport. 2021;38(1):9–21. doi: 10.5114/biolsport.2020.96857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Brach M, et al. Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PLOS one. 2020 doi: 10.1371/journal.pone.0240204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Bentlage E, et al. on behalf of the ECLB-COVID19 Consortium Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;2(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Bentlage E, et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicentre study. Int J Env Res Pub Health. 2020;17(17):6237. doi: 10.3390/ijerph17176237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee I.-M, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hermansen R, Jacobsen BK, Lochen ML, Morseth B. Leisure time and occupational physical activity, resting heart rate and mortality in the Arctic region of Norway: the Finnmark Study. Eur J Prev Cardiol. 2019;26(15):1636–1644. doi: 10.1177/2047487319848205. [DOI] [PubMed] [Google Scholar]
- 12.Kivipelto M, Mangialasche F, Ngandu T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat Rev Neurol. 2018;14:653–666. doi: 10.1038/s41582-018-0070-3. [DOI] [PubMed] [Google Scholar]
- 13.Levasseur M, Richard L, Gauvin L, Raymond É. Inventory and analysis of definitions of social participation found in the aging literature: Proposed taxonomy of social activities. Soc Sci Med. 2010;71(12):2141–2149. doi: 10.1016/j.socscimed.2010.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Litwin H, Shiovitz-Ezra S. The association between activity and wellbeing in later life: What really matters? Ageing Soc. 2006;26(2):225–243. [Google Scholar]
- 16.Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11:607–615. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 17.Amatriain-Fernández S, Gronwald T, Murillo-Rodríguez E, Imperatori C, Solano AF, Latini A, Budde H. Physical Exercise Potentials Against Viral Diseases Like COVID-19 in the Elderly. Front Med (Lausanne) 2020;7:379. doi: 10.3389/fmed.2020.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callow DD, Arnold-Nedimala NA, Jordan LS, et al. The Mental Health Benefits of Physical Activity in Older Adults Survive the COVID-19 Pandemic. Am J Geriatr Psychiatry. 2020:1046–1057. doi: 10.1016/j.jagp.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grande AJ, Keogh J, Silva V, Scott AM. Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections. Cochrane Database Syst Rev. 2020;4:1–66. doi: 10.1002/14651858.CD010596.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chtourou H, Trabelsi K, H, mida C, Boukhris O, Brach M, Bentlage E, et al. Staying physically active during the quarantine and self-isolation period for controlling and mitigating the COVID-19 pandemics: A systematic overview of the literature. Front Psycho. 2020 doi: 10.3389/fpsyg.2020.01708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bentlage E, Ammar A, How D, Ahmed M, Trabelsi K, Chtourou H, et al. Practical recommendations for maintaining active lifestyle during the COVID-19 pandemic: A systematic literature review. Int J Environ Res Public Health. 2020;17(17):6265. doi: 10.3390/ijerph17176265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yousfi N, Bragazzi N, Briki W, Zmijewski P, Chamari K. The COVID-19 pandemic: how to maintain a healthy immune system during the lockdown –a multidisciplinary approach with special focus on athletes. Biol Sport. 2020;37(3):211–216. doi: 10.5114/biolsport.2020.95125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niazkar HR, Zibaee B, Nasimi A, Bahri N. The neurological manifestations of COVID-19: a review article. Neurol Sci. 2020;41:1667–1671. doi: 10.1007/s10072-020-04486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stöckel T, Wunsch K, Hughes CML. Age-Related Decline in Anticipatory Motor Planning and Its Relation to Cognitive and Motor Skill Proficiency. Front Aging Neurosci. 2017;9:283. doi: 10.3389/fnagi.2017.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CDC june 2020 (Center for sisease control and prevention: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html#:~:text = As%20you%20get%20older%2C%20your,than%20people%20in%20their%2050s. Accessed Aout 18, 2020.
- 27.Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob health res policy. 2020;5:27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haluza D, Jungwirth D. ICT and the future of health care: aspects of health promotion. Int J Med Inform. 2015;84(1):48–57. doi: 10.1016/j.ijmedinf.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Barrett M, Boyne J, Brandts J, et al. Artificial intelligence supported patient self-care in chronic heart failure: a paradigm shift from reactive to predictive, preventive and personalised care. EPMA J. 2019;10:445–464. doi: 10.1007/s13167-019-00188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berliner L, Lemke HU, vanSonnenberg E, et al. Model-guided therapy for hepatocellular carcinoma: a role for information technology in predictive, preventive and personalized medicine. EPMA J. 2014;5:16. doi: 10.1186/1878-5085-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Radanliev P, De Roure D, Walton R, et al. COVID-19 what have we learned? The rise of social machines and connected devices in pandemic management following the concepts of predictive, preventive and personalized medicine. EPMA J. 2020;11:311–332. doi: 10.1007/s13167-020-00218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitelaw S, Mamas MA, Topol E, Van Spall H. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digital technology. 2020;2(8) doi: 10.1016/S2589-7500(20)30142-4. E435-E440.S2589-7500(20)30142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Budd J, Miller BS, Manning EM, et al. Digital technologies in the public-health response to COVID-19. Nat Med. 2020;26:1183–1192. doi: 10.1038/s41591-020-1011-4. [DOI] [PubMed] [Google Scholar]
- 34.Bisciotti G, Eirale C, Corsini A, Baudot C, Saillant G, Chalabi H. Return to football training and competition after lockdown caused by the COVID-19 pandemic: medical recommendations. Biol Sport. 2020;37(3):313–319. doi: 10.5114/biolsport.2020.96652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barker R, Donnelly T. Transforming Healthcare Through Technology. Health Pap. 2017;16(3):27–33. doi: 10.12927/hcpap.2017.25083. [DOI] [PubMed] [Google Scholar]