Abstract
Patients with substance use disorder (SUD) rely upon urine drug testing to support treatment adherence and to mitigate relapse. Before the onset of coronavirus 2019 (COVID-19), the logistical challenges of randomized observed collections for urine drug testing for the patient were significant. During COVID-19, these barriers were often insurmountable. Since SUD patients represent a population at a higher risk for complications from COVID-19, an alternative strategy to support COVID-19 testing was urgently needed. We designed and deployed a telehealth-based solution in which patients could use mobile devices to connect with trained collection professionals to perform observed urine collections, often referred to a UA (urinalysis). The solution was designed with patient-centered best practices for telehealth, stigma prevention, trauma-informed, empathy and compassion, and to remove barriers to access to care. This approach demonstrated high patient satisfaction scores thereby proving that it is possible to provide urine collection services in the patient’s home via a telehealth technology, while still upholding SUD testing integrity best practices. This study lays the path for a more patient-centered way to support this population.
Keywords: COVID-19, urine collection, telehealth, mobile device, telecollections, patient experience
Introduction
Telehealth, distanced medical services provided by clinicians and allied services, is a valuable strategy to extend the delivery of services and access to care (1). In recent years, the expansion of telehealth services has accelerated, in part due to the ubiquity of mobile devices and introduction of new teleservices including radiology, telestroke, teletrauma, and telenursing (2).
Prior to coronavirus 2019 (COVID-19), addiction medicine underutilized telemedicine solutions. A 2019 survey of US addiction treatment centers showed the rate of utilization was less than 20% nationwide and less than 7% in Vermont (3). This trend has changed due to the COVID-19 pandemic (4,5), supported in part by the lifting of previous regulatory and reimbursement barriers (6).
Although the COVID-19 pandemic has impacted all individuals, patients with substance use disorder (SUD) have been especially affected, as their substance use history makes them vulnerable to both COVID-19 infections and worsened outcomes, including higher hospitalizations and death rates (7). Further, their mental health needs are highly dependent on the consistent delivery of services and relationship-based connections. As residents were required to shelter in place, patients with SUD voiced anxiety around viral exposure, isolation, and fear that a change in their routine and accountability could impact their outcomes (8). Many providers, who prior to COVID-19 would order in-person observed urine drug testing (urinalysis [UA]) for patients, stopped doing so. At the onset of COVID-19, professional societies recommended (9) SUD providers opt to temporarily decrease or eliminate UAs to limit viral exposure. Since UAs have been well-recognized as a vital component to clinical care, providing objective identification of drug use or treatment nonadherence (10), these changes in practice resulted in a reduction in the standard of care.
Unfortunately, the pandemic has fueled the opioid epidemic. In July 2020, increased opioid-related mortality was identified over 34 states (11), reversing isolated gains in these communities previously (12). In December 2020, the United States experienced the highest number of drug overdose deaths ever recorded in a 12-month period (13).
Given the challenges posed by the COVID-19 pandemic and the complexity often seen in the lives of SUD patients, solutions to serve this patient population must meet patients where they are at emotionally, mentally, and physically. Successful care delivery requires 3 patient-centered considerations: stigma prevention, trauma-informed care, and empathy-compassion health care delivery.
Stigma, a social construct that associates specific behaviors with a negative perception, opinion, judgment, or labeling, has plagued SUD patients nationally, compromising patient experience. Studies have demonstrated stigma’s contributions to isolation, biases, prejudice, and even discrimination by health care providers (14). Provider training on communication, empathy, compassion, and language choices reduces stigma and improves the provider–patient relationship (14 –19).
Patients with substance use are over 7 times more likely to have a history of trauma, an event(s) that reshapes how a person sees themselves, their environment, and interactions, even without posttraumatic stress disorder (20). Patients who use opioids, sedatives, or amphetamines are particularly vulnerable (21). Training in trauma-informed care approaches allows for psychological safety and healing (20,22).
Empathy is directly correlated with improved patient experience surveys (23). Although empathy is conducive to relationship building, a lack thereof promotes negative outcomes for relationship building and patients’ perception of satisfaction. Outcomes are improved with training on empathetic understanding (24). Closely related to empathy, compassion requires not only connecting to another person’s emotional state and suffering but also showing concern, support, and a desire to comfort (25). For patients with challenging behaviors, the art of patient-centered care is remaining compassionate while providing clear boundaries (17).
Combining these 3 patient-centered considerations with best practices for telehealth services, we designed an observed UA telehealth specimen collection strategy that optimized the patient experience and patient access. Through the combined use of telehealth and a specimen shipping solution (hereafter referred to as “telecollections”), we aimed to improve the patient experience and access to care, allowing for the reinstitution of limited UAs. We hypothesize that by providing observed at-home telecollection services with staff trained in patient experience and telehealth best practices, stigma prevention, trauma-informed care, and empathy and compassion, we could remove barriers to care for the vulnerable SUD population during the pandemic and achieve high levels of patient satisfaction. We assessed the patient experience via a structured survey and a free-form feedback question, designed to represent 5 perceptual dimensions of the patient experience: technology ease of use, convenience of performing UA observed collections at home, patient’s perception of comfort and respect, patient’s rating of usefulness of education and appointment preparedness videos, and patient free-form feedback.
Methods
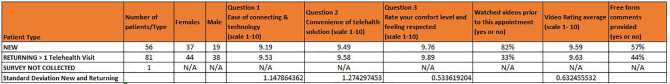
This pilot was performed at Aspenti Health (South Burlington, Vermont), a laboratory centered on care for patients with SUD. It relied on a convenience sample and analyzed for qualitative and quantitative measures of the patient experience during use of telecollection services. The patient samples were composed of new (n = 56) and returning patients (n = 81) to virtual at-home service specimen collection services (Figure 1).
Figure 1.
Telecollection patient satisfaction survey results: This table provides details on patient demographics and patient satisfaction results across 4 domains: usefulness of videos, convenience of solution, patient perception of feeling respected, and ease of technology.
The phases of the study included a business analysis, solution process and technology development, testing of technology, staff training, testing performance, designing and implement patient surveys, and result analysis (Figure 2).
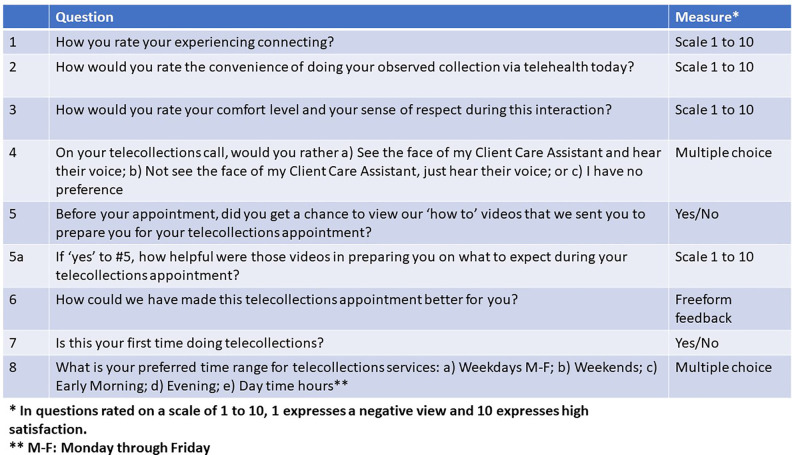
Figure 2.
Telecollections patient experience survey questions: This figure shows the structured survey that all telecollection-patient facing staff was trained to administer. These questions were designed to capture patients’ experience with the technology, the patient–provider interaction, service preferences, and the usefulness of the education material provided to each patient to prepare them for their telecollection appointment.
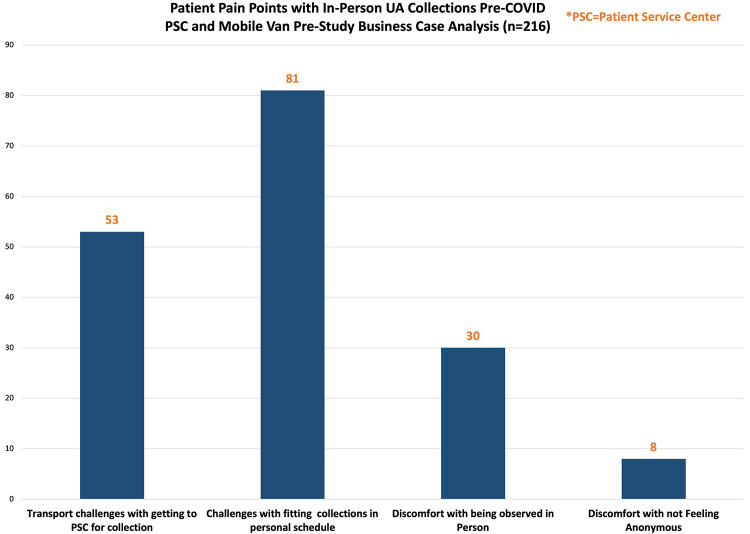
A June 2020 preimplementation business analysis surveyed patients receiving in-person urine collection services at patient service centers or as part of a mobile unit. The survey was designed to identify patients’ needs and preferences in urine collection practices including an evaluation of perceived pain points or barriers to participation in observed UA protocols prior to COVID-19 and to explore the patients’ interest in an at-home telehealth urine collection solution. Survey results pertaining to the mobile unit have been previously published (26).
Through these analyses (Figure 3) and support through the literature (14,16 –18,20 –24,27 –31), we identified 3 patient-centered criteria used in the design of the solution and protocols. First, the technology needed to be easy-to-use and accessible. As part of trauma-informed care, we needed to meet patients where they are at and offer an experience designed to give them a sense of control. Second, patient education for this technology was necessary to prepare them for this new experience. Our team designed patient education delivered via one-on-one patient coaching, one technology ease of use video, and one “what to expect during your telecollection appointment” video. Additionally, a one-page easy to read patient resource with instructions and visuals was created. Third, we incorporated into our procedures the patient-centric principles of care delivery including trauma-informed practices, stigma prevention, and compassion, as previously cited (14,18,20,23,24,28,29,31,32).
Figure 3.
Patients pain points with in-person UA collections pre-COVID: this histogram shows how many patients out of the 216 patients surveyed answered positively when asked about 4 common participation pain points for substance use disorder patients.
A total of 5 staff (3 females, 2 males) were trained to deliver telecollections services. Two female staff members (client care assistants [CCA]) were trained in all-gender UA collections. All CCAs were Caucasian. Team members were highly experienced in in-person collections. The patient-centered trainings were designed using Zoom PowerPoint presentations and developed video modules focused on de-escalation, listening and communication training, understanding our patient population, trauma-informed care, stigma prevention, and telecollections best practices and etiquette. Staff were trained on the process of virtual specimen UA collections, a script on guiding the patients through each step, and how to resolve connectivity issues. Each training was about 1-hour long. Skills were checked via in-person testing, role playing with a supervisor, and skill-check quizzes.
Enrolled patients were sent preassembled kits, including shipping materials. They connected to their appointments and completed their UA collection. Patients shipped back the specimen to the laboratory for testing using the shipping materials provided. Test results were reported via traditional mechanisms. This solution used standard shipping strategies such as UPS and FedEx. Patient shipped specimens at room temperature the same day from their home or at a local drop off site. Routine laboratory validation has demonstrated specimen stability at room temperature for up to 14 days.
Consistent with trauma-informed care best practices, patients selected their preferred CCA gender whenever possible (20,21). When not possible, patients were provided with the choice of an opposite gender CCA or to schedule their appointment at a different time with the same gender CCA. Patients at brick-and-mortar in-person service centers are observed by the same gender only CCAs unless special accommodations are made by their providers.
Although ensuring quality and specimen integrity, telecollections processes differed slightly from in-person processes. The patients were instructed by the CCA to place the mobile device to capture a side-way view of the patient urinating as opposed to a frontal view and where to place their hands, when to hold the cup, and when and how to capture the urine stream. A phone holder was provided to make this process easier for the patient. To uphold patients’ privacy, CCAs were limited to a computer in a lockable private room with no windows for viewing the collection. In addition, telecollections staff members were not allowed to have cell phones while in session and the specimen collection was not recorded.
Since the purpose of this study was to examine the patient experience, we conducted a patient experience survey for all telecollection encounters (n = 138) from August 2020 to December 2020. All telecollection staff were instructed on administering and collecting point-of-care custom-designed patient experience survey questions using a standardized template. Although patient participation in the survey was voluntary, all telecollection participants participated in this exercise, except for one encounter where this step was omitted in error by the CCA. Five patients were excluded from this study due to connectivity issues. The survey consisted of 6 structured questions. Four questions used a scale of 1 to 10 (1 being not satisfied and 10 being very satisfied), 2 yes or no questions, and 1 multiple choice question. A free-form feedback question was also added to gather qualitative data (33). All numerical ratings were assessed using quantitative analysis approach. One investigator applied thematic categorization to the qualitative free-form responses, and no coding or further data abstraction was deployed.
This service was piloted for 100 workdays and followed a trauma-informed care model for assigning patients in partnership between providers and patients. Patients were part of the decision process and had a clear understanding of the process and their role. They were surveyed at each interaction. Following a 10-point scale, survey questions were designed to assess the patient’s experience within 5 dimensions of the patient journey: Ease of use of technology, convenience of performing at-home observed collections, patient perception of comfort and respect during interaction, patient rating of usefulness of education and video resources provided prior to telecollection appointment, and patient free-form feedback (see Figure 4).
Figure 4.
Phases of telecollections PX study: This figure shows the flow of the steps of our study from concept to analysis.
Ethical due diligence was performed, and this work met criteria for operational improvement activities exempt from ethics review, according to the policy defining activities which constitute research at the University of Vermont/University of Vermont Medical Center. Where applicable, statistical evaluation was conducted with the use of an online statistical calculator (34) using a comparison of means t test and a comparison of proportions N-1 chi-square test.
Results
Preliminary business analyses demonstrated patients’ interest and buy-in for an at-home telehealth solution for observed UA collections (n = 216). This preliminary work confirmed perceived barriers to participation in observed UA protocols prior to COVID-19 (Figure 3). Our analysis revealed 96% of our patients surveyed at the time (n = 216) had access to a smartphone and Internet or data plan services; 61% of patients were familiar with telehealth; and 70% of patients surveyed stated that they would either prefer a telehealth visit for their UA collection or were open to any method of specimen collection including an at-home telehealth solution.
Fifty-six participants scheduled visits during the 5-month pilot. All patients participated in the surveys and were willing to score their experience for all encounters (n = 138). Additional, free-form feedback was obtained in only 70 of the 138 encounters. Ninety-two percent of patients demonstrated satisfaction scores of >7 of 10; only 2.2% patients expressed dissatisfaction that was attributable to discomfort with technology. The satisfaction scores averaged 9.5 of 10 across all metrics with the category for perception of comfort and respect exceeding all other variables at 9.8 of 10 (Figure 1).
The role of patient education video in preparing patients was assessed. Eighty-two percent of new participants and 33% of returning patients viewed the patient education videos prior to attending their appointment (Figure 2). 9.6 10 patients stated the videos were instrumental in appointment preparation. Survey responses were comparable across new and returning participants in all response except for video use (P < .0001, N-1 chi-square test).
Free-form feedback provided insights on what patients still struggled with, what they were happy with, and what additional feature they would like added to this new process. Of all the patient encounters (n = 138), 3 individuals provided direct negative feedback: 2 of which were centered around having a telecollection staff of the opposite gender. One patient stated that using a drop box to ship back the specimen to the laboratory was inconvenient. Thirty-three individuals provided positive feedback supporting satisfaction with being able to do an observed UA collection at home, satisfaction with the CCAs, the ease of the solution, and the videos. The remaining patient feedback was categorized as either neutral (n = 6) or additional feature requests (n = 16), including desire for specimen collection hats for female patients (n = 6), same gender staffing (n = 2), oral fluid testing instead of UA testing (n = 2), home pick-ups instead of the drop box process (n = 5), and patient education videos with a male actor (n = 1) as the actor in our videos was a female.
Discussion
Main Findings
Introduction of patient-centered, trauma-informed, compassion-based telecollection services can enhance the overall patient satisfaction and experience. Given the distancing requirements during the pandemic, this solution filled an apparent gap in care at this time. Early during COVID-19, American Society of Addiction Medicine recommended specific guidance on the opportunity to enhance drug testing while allowing patients to stay at home (9). However, many available alternatives posed expensive or technically difficult solutions or potentially deviated from standard best practices. For example, while observed UA remains best practice for many SUD patients, alternative specimen types with known limitations including oral fluid, hair. and sweat samples were considered during this time (35). Our strategy was critically important, given the emergent increase in drug overdose rates since the onset of COVID-19 (13).
Patient experience was central to design this solution. We created, implemented, and trained staff on a Telehealth solution model based on a thorough review of the scientific literature (14,16 –18,20,23,27 –31), addressing possible challenges inherent to the technology and to ensure that patients were prepared.
Lessons Learned
Our results show that patients were satisfied with their telecollection option. Secondary anecdotal feedback through providers supported the high patient satisfaction scores obtained in our surveys. Nonetheless, there were several lessons learned during this process. For example, an early concern that patients would not have access to mobile devices, Internet services, or be able to navigate the steps to connect to their telecollection appointment was not found to be a significant barrier for the vast majority of patients. Isolated connectivity issues were attributable to patients’ subpar Internet or data plan service. Some patients had trouble connecting initially but were able to overcome their challenges with the guidance of our staff. Technical challenges are a documented barrier for telehealth services (36). We found that this challenge can be addressed with proper screening for access to technology and patient education prior the appointment. This approach is supported by the literature and creates a successful telehealth experience for providers and patients (31).
We also found that the patient training via one-on-one phone coaching and quick “how to” videos were valuable to patients navigating this new technology approach. Most patients viewed the videos at least once prior to their encounters. Interestingly, of the small percentage that had difficulty connecting, patients reported they had not clicked on the video links provided, suggesting that the videos may have surmounted some of the technical barriers. The provision of education tools that are easy to navigate, such as videos, for patients participating in a telehealth solution has been recommended previously (27,31).
Finally, we found that analysis through survey questions and free-form feedback allowed us to perform service adjustments to meet our patients’ needs. Without this real-time monitoring, we would have failed to capture what could improve the patient’s experience.
Limitation of the Study and Next Steps
This study had some limitations. First, the study was restricted geographically. Patients were primarily residents of the state of Vermont which offers a lack of racial diversity (37). Second, providers’ clinical approach to the use of UAs in SUD treatment may vary. This variable was not assessed. Future studies could assess the impact of this variable. Finally, due to Health Insurance Portability and Accountability Act (HIPAA) concerns, surveys were administered verbally at the end of each encounter. Although this type of strategy may compromise the patients’ anonymity in this process and secondarily inflate satisfaction scores (8,34,38), provider reporting of patient satisfaction corroborated this study’s findings.
Efforts to remove barriers to access to care for SUD patients resonated with patients. As previously demonstrated through provision of mobile van services (26) and supported in other studies (14,16 –18,20 –24,27 –31), providing an experience that applies stigma prevention, empathy and compassion care delivery, excellent provider–patient communication, and trauma-informed care results in high patient satisfaction scores.
Although the pandemic was the impetus for this innovation, we plan to continue services. Since ongoing feedback is needed to guide improvements, an automated patient survey process will be developed to remove possible analytical biases. We also want to directly capture provider insights as secondary sources of the patients’ experiences. Finally, this work would benefit from geographic expansion to ensure greater racial and socioeconomic diversity.
Conclusions
Even during a pandemic, patient-centered practices can be used to innovate solutions that meet patients where they are at. This telehealth UA collection solution allowed providers to follow best practices for UA collection integrity for SUD treatment. Training centered on empathy, compassion, stigma prevention, de-escalation, and trauma-informed care resulted in high patient experience satisfaction scores. This work is further evidence that organizations should continue to innovate, remove access to care barriers, and strive to provide solutions that are patient-based. This study introduces a more patient-centered way to support this vulnerable patient population.
Supplemental Material
Supplemental Material, sj-docx-1-jpx-10.1177_23743735211033128 for Patient-Centered Telehealth Solution for Observed Urine Collections in Substance Use Disorder Care Delivery During COVID-19 and Beyond by Alexa Brett, Heather Foster, Michael Joseph and Jill S. Warrington in Journal of Patient Experience
Acknowledgments
The authors want to thank their respective institutions championing scholarship. The authors want to acknowledge the excellent professionalism of our telecollection staff and Client Services staff during this study, especially Melissa Schnare, Chad Blair, Kate Greenwood, Christine Ahern, Joel Bissonnette, Jennifer Blades, and Alison Dubuque.
Authors’ Note: Alexa Brett, the corresponding author, drafted the manuscript. Jill S. Warrington, MD, coordinated with the Institutional Review Board at her home institution (the University of Vermont Medical Center) and provided design and editorial guidance on the document for submission. Alexa Brett designed the concept and led the implementation of this project with a special focus on operational protocols, patient experience, staff training, patient education, and patient survey material and analysis. Heather Foster supported this process with a special focus on quality. Michael Joseph contributed to the financial analysis and project management. The data sets generated and/or analyzed during the current study are not publicly available due to the need to support the privacy of patients and providers but are available in an aggregated, deidentified from the corresponding author on reasonable request. According to the policy defining activities which constitute research at the University of Vermont/University of Vermont Medical Center, this work met criteria for operational improvement activities exempt from ethics review.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Alexa Brett and Heather Foster were salaried employees of Aspenti Health at the time of this pilot, a laboratory focused on population health management for substance Use Disorders. Jill S. Warrington carried a nonsalaried position as Chief Medical Officer at Aspenti Health where she held a small portion of stock options (<$1000 in value). She also is a member of the community advisory council at Blue Cross Blue Shield of Vermont. Michael Joseph is an independent consultant from True Vector Management Consulting with over 30 years of healthcare IT experience who was working for Aspenti Health. This study was conducted at Aspenti Health. The University of Vermont is a participating organization of the Project Santa Fe Foundation of which the Clinical Lab 2.0 movement is an initiative.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alexa Brett  https://orcid.org/0000-0002-5161-2766
https://orcid.org/0000-0002-5161-2766
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Open access research telehealth and patient satisfaction. Published June 23, 2017. Accessed May 8, 2021. https://www.researchgate.net/publication/318905550_Telehealth_and_patient_satisfaction_A_systematic_review_and_narrative_analysis/fulltext/59847106458515605844bdae/Telehealth-and-patient-satisfaction-A-systematic-review-and-narrative-analysis.pdf [DOI] [PMC free article] [PubMed]
- 2. Weinstein RS, Lopez AM, Joseph BA, Erps KA, Holcomb M, Barker GP, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med. 2014;127:183–187. doi:10.1016/j.amjmed.2013.09.032 [DOI] [PubMed] [Google Scholar]
- 3. Uscher-Pines L, Cantor J, Huskamp HA, Mehrotra A, Busch A, Barnett M. Adoption of telemedicine services by substance abuse treatment facilities in the U.S. J Subst Abuse Treat. 2020;117:108060. doi:10.1016/j.jsat.2020.108060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blanco C, Compton WM, Volkow ND. Opportunities for research on the treatment of substance use disorders in the context of COVID-19. JAMA Psychiatry. Published online September 01, 2020. doi:10.1001/jamapsychiatry.2020.3177 [DOI] [PubMed] [Google Scholar]
- 5. Kleykamp BA, Guille C, Barth KS, McClure EA. Substance use disorders and COVID-19: the role of telehealth in treatment and research. J Soc Work Pract Addict. 2020;20:248–253. doi:10.1080/1533256X.2020.1793064 [Google Scholar]
- 6. American Telemedicine Association (ATA). Policy update March 17, 2020. Published March 17, 2020. Accessed May 5, 2021. https://info.americantelemed.org/covid-19-cms-hhs-dea-updates-3-17-20
- 7. Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021;26:30–39. doi:10.1038/s41380-020-00880-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krawczyk N, Bunting AM, Frank D, Arshonsky J, Gu Y, Friedman SR, et al. How will I get my next week’s SCRIPT? Reactions of REDDIT OPIOID forum users to changes in treatment access in the early months of the coronavirus pandemic. Published February 06, 2021. Accessed May 8, 2021. https://www.sciencedirect.com/science/article/abs/pii/S0955395921000384 [DOI] [PMC free article] [PubMed]
- 9. American Society of Addiction Medicine [INTERNET]. ASAM. Published July 23, 2020. Accessed May 8, 2021. https://www.asam.org/Quality-Science/covid-19-coronavirus/adjusting-drug-testing-protocols
- 10. Jarvis M, Williams J, Hurford M, Lindsay D, Lincoln P, Giles L, et al. Appropriate use of drug testing in clinical addiction medicine. J Addict Med. 2017;11:163–173. doi:10.1097/ADM.0000000000000323. PMID: 28557958. [DOI] [PubMed] [Google Scholar]
- 11. American Medical Association. PDF [Issue brief: reports of increases in opioid related overdose and other concerns during COVID pandemic]. Published July 20, 2020. Accessed May 9, 2021. https://www.ama-assn.org/system/files/2020-07/issue-brief-increases-in-opioid-related-overdose.pdf
- 12. Wan W, Long H. Washington post. Cries for help: drug overdoses are soaring during the coronavirus pandemic. Published July 09, 2020. Accessed May 9, 2021. https://www.washingtonpost.com/health/2020/07/01/coronavirus-drug-overdose/
- 13. Centers for Disease Control and Prevention [INTERNET]. Overdose deaths accelerating during COVID-19. Published December 18, 2020. Accessed May 9, 2021. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
- 14. Goodyear K, Haass-Koffler CL, Chavanne D. Opioid use and stigma: the role of gender, language and precipitating events. Published April 01, 2018. Accessed May 9, 2021. https://pubmed.ncbi.nlm.nih.gov/29499554/ [DOI] [PMC free article] [PubMed]
- 15. Salamat S, Hegarty P, Patton R. Same clinic, different conceptions: drug users and healthcare professionals perceptions of how stigma may affect clinical care. Published May 24, 2019. Accessed May 9, 2021. https://onlinelibrary.wiley.com/doi/abs/10.1111/jasp.12602
- 16. Paquette CE, Syvertsen JL, Pollini RA. Science direct. Stigma at every turn: health services experiences among people who inject drugs. Published April 30, 2018. Accessed May 9, 2021. https://www.sciencedirect.com/science/article/pii/S0955395918301051 [DOI] [PMC free article] [PubMed]
- 17. Schuermeyer IN, Sieke E, Dickstein L, Falcone T, Franco K. Patients with challenging behaviors: communication strategies. Published July 01, 2017. Accessed May 9, 2021. https://www.ccjm.org/content/84/7/535 [DOI] [PubMed]
- 18. Boissy A. Labels matter: challenging conversations or challenging people? Published July 01, 2017. Accessed May 9, 2021. https://www.ccjm.org/content/84/7/543 [DOI] [PubMed]
- 19. Windover AK, Boissy A, Rice TW, Gilligan T, Velez VJ, Merlino J. The REDE model of healthcare communication: optimizing relationship as a therapeutic agent. J Patient Exp. 2014;1:8–13. doi:10.177/237437431400100103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mills KL. The importance of providing trauma-informed care in alcohol and other drug services. Published May 2015. Accessed May 9, 2021. https://pubmed.ncbi.nlm.nih.gov/25944454/ [DOI] [PubMed]
- 21. Lotzin A, Buth S, Sehner S, Hiller P, Pawils S, Metzner F, et al. Reducing barriers to trauma inquiry in substance use. Published 2019. Accessed May 9, 2021. https://substanceabusepolicy.biomedcentral.com/track/pdf/10.1186/s13011-019-0211-8.pdf [DOI] [PMC free article] [PubMed]
- 22. Killeen TK, Back SE, Brady KT. Implementation of integrated therapies for comorbid post-traumatic stress disorder and substance use disorders in community substance abuse treatment programs. Published March 04, 2015. Accessed May 9, 2021. https://onlinelibrary.wiley.com/doi/pdf/10.1111/dar.12229 [DOI] [PMC free article] [PubMed]
- 23. Chaitoff A, Sun B, Windover A, Bokar D, Featherall J, Rothberg MB, et al. Associations between physician empathy. Acad Med. 2017;92:1464–1471. Accessed May 9, 2021. https://journals.lww.com/academicmedicine/Fulltext/2017/10000/Associations_Between_Physician_Empathy,_Physician.34.aspx [DOI] [PubMed] [Google Scholar]
- 24. Hojat M, DeSantis J, Gonnella J. Patient perceptions of clinician’s empathy: measurement and psychometrics. Published June 2017. Accessed May 9, 2021. https://www.ncbi.nlm.nih.gov/pubmed/28725866 [DOI] [PMC free article] [PubMed]
- 25. Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The role of empathy in health and social care professionals. Published January 30, 2020. Accessed May 10, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151200/ [DOI] [PMC free article] [PubMed]
- 26. Warrington JS, Brett A, Foster H, Brandon J, Francis-Fath S, Joseph M, et al. Driving access to care: use of mobile units for urine specimen collection during the coronavirus disease-19 (COVID-19) pandemic. Acad Pathol. 2020;7. doi:10.1177/2374289520953557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients satisfaction with and preference for telehealth visits. Published 2015. Accessed May 9, 2021. https://pubmed.ncbi.nlm.nih.gov/26269131/ [DOI] [PMC free article] [PubMed]
- 28. Shore JH, Yellowlees P, Caudill R, Johnston B, Turvey C, Mishkind M, et al. Best practices in videoconferencing-based telemental. Published November 2018. Accessed May 10, 2021. https://www.researchgate.net/publication/328524369_Best_Practices_in_Videoconferencing-Based_Telemental_Health_April_2018 [DOI] [PubMed]
- 29. Indovina K, Keniston A, Reid M, Sachs K, Zheng C, Tong A, et al. Real-time patient experience surveys of hospitalized medical patients. J Hosp Med. 2016;11:251–256. doi:10.1002/jhm.2533 [DOI] [PubMed] [Google Scholar]
- 30. Donelan K, Barreto EA, Sossong S, Michael C, Estrada JJ, Cohen AB, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. Accessed May 10, 2021. https://pubmed.ncbi.nlm.nih.gov/30667610/ [PubMed] [Google Scholar]
- 31. Hawley CE, Genovese N, Owsiany MT, Triantafylidis LK, Moo LR, Linsky AM, et al. Rapid integration of home telehealth visits amidst covid-19: what do older adults need to succeed? J Am Geriatr Soc. 2020:68:2431–2439. doi:10.1111/jgs.16845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Langbecker D, Caffery LJ, Gillespie N, Smith AC. Using survey methods in telehealth research: a practical guide. Published 2017. Accessed May 9, 2021. https://journals.sagepub.com/doi/full/10.1177/1357633X17721814 [DOI] [PubMed]
- 33. Brod M, Tesler LE, Christensen TL. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18:1263–1278. doi:10.1007/s11136-009-9540-9 [DOI] [PubMed] [Google Scholar]
- 34. MedCalc. Published 2021. Accessed April 28, 2021. https://www.medcalc.org/calc/comparison_of_proportions.php
- 35. Association for Standardisation of Automation and Measuring Systems. The ASAM appropriate use of drug testing in clinical addiction medicine pocket guide. Published 2017. Accessed May 10, 2021. http://eguideline.guidelinecentral.com/i/840070-drug-testing-pocket-guide/0
- 36. Kemp MT, Williams AM, Sharma SB, Biesterveld BE, Wakam GK, Matusko N, et al. Barriers associated with failed completion of an acute care general surgery telehealth clinic visit. Published August 08, 2020. Accessed May 9, 2021. https://www.sciencedirect.com/science/article/abs/pii/S0039606020304220 [DOI] [PubMed]
- 37. United States Census Bureau. Quickfacts Vermont United States. Published 2019. Accessed May 10, 2021. https://www.census.gov/quickfacts/fact/table/VT,US/PST045219
- 38. Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method. ProQuest Ebook Central; Published 2014. Accessed May 10, 2021. https://ebookcentral.proquest.com [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-jpx-10.1177_23743735211033128 for Patient-Centered Telehealth Solution for Observed Urine Collections in Substance Use Disorder Care Delivery During COVID-19 and Beyond by Alexa Brett, Heather Foster, Michael Joseph and Jill S. Warrington in Journal of Patient Experience