ABSTRACT
A recent report by the Chief Public Health Officer of Canada demonstrates the inferior health status of Indigenous Peoples in Canada when compared to non-Indigenous populations. This scoping review maps out the available literature concerning acute health care for Indigenous Peoples in Canada in order to better understand the health care issues they face. All existing articles concerning health care provided to Indigenous Peoples in Canada in acute settings were included in this review. The targeted studied outcomes were access to care, health care satisfaction, hospital visit rates, mortality, quality of care, length of stay and cost per hospitalisation. 114 articles were identified. The most studied outcomes were hospitalisation rates (58.8%), length of stay (28.0%), mortality (25.4%) and quality of care (24.6%) Frequently studied topics included pulmonary disease, injuries, cardiovascular disease and mental illness. Indigenous Peoples presented lower levels of satisfaction and access to care although they tend to be over-represented in hospitalisation rates for acute care. Greater inclusion of Indigenous Peoples in the health care system and in the training of health care providers is necessary to ensure a better quality of care that is culturally safe for Indigenous Peoples.
KEYWORDS: Indigenous health, acute health care, Canadians’ health, emergency department, hospitalisation
Introduction
In 2016, 1 673,780 Indigenous people were identified in Canada, representing 4.76% of the Canadian population [1]. Indigenous Peoples include three major groups: First Nations (61%), Inuit (4%) and Métis (32%) Peoples [2]. It is important to recognise that within these three groups, there are over fifty different Indigenous nations and over six hundred Indigenous communities, each of them with their own traditions and experiences [3]. Although Indigenous communities are distinct from one another, they share certain common experiences. An example of such experiences is the Residential School Program imposed by the Government of Canada until 1996. This program aimed to assimilate Indigenous Peoples by forcing Indigenous children to attend boarding schools directed by religious authorities and the Canadian government. This program led to significant intergenerational trauma due to the tearing of Indigenous children from their culture and community in addition to the abuse inflicted upon them in these schools [4,5]. The Residential School Program is only one example of many government policies and measures, which aimed to assimilate Indigenous Peoples in Canada. These policies of cultural assimilation are reflected in the current relations between Indigenous Peoples and government institutions such as health care services.
In Canada, the health care of Indigenous Peoples is mainly managed by the federal government since the adoption of the Indian Act in 1985. However, important differences in health care management between Indigenous communities persist. Indigenous communities in the province of Quebec have the authority to manage their own health care services whereas others communities depend on the federal government. The health care coverage and access also differ for Indigenous Peoples living on-reserve and off-reserve and for those who identify as Métis [1]. These differences in health care management have a direct impact on the health care provided to Indigenous Peoples in Canada.
A recent report by the Chief Public Health Officer of Canada establishes that Indigenous Peoples in Canada have a shorter life expectancy at birth than non-Indigenous populations. Indigenous Peoples are also less likely to report a very good or excellent state of health [2]. Additionally, several studies demonstrate significant disparities between Indigenous and non-Indigenous populations in Canada regarding health status [6–9].
The clear health disparities between Indigenous and non-Indigenous populations in Canada raise questions regarding inequalities in access, use and quality of health care. The primary objective of this scoping review is to map out the available literature on acute health care provided to Indigenous Peoples in Canada. In doing so, it aims to better understand the health care issues Indigenous Peoples face and identify areas that have not been fully explored in the current literature. In this study, acute health care refers to emergency department care, intensive unit care or hospitalisation for acute health problems.
Methods
This scoping review aims to identify all available literature regarding acute health care (emergency care, intensive care or hospitalisation for acute health problems) provided to First Nation, Inuit and Métis Peoples of North America in order to better understand the health care issues they face. The studied outcomes are patient satisfaction, access to care, hospitalisation rates and emergency department visit rates, mortality, quality of care, length of stay and cost. To determine these outcomes, a preliminary exploration of the available literature on health care provided to Indigenous Peoples was conducted by two authors in order to identify recurring themes. We searched Medline, Embase, Cochrane Library, Web of science and PsycInfo databases up until 1 February, 2021. These databases were selected in collaboration with librarians to ensure a maximum number of studies were found. An example of the research strategy is presented below. In summary, the research strategy focused on three main concepts: Indigenous Peoples, North America and acute health care. An example of the detailed research strategy is presented in Figure 1.
Figure 1.
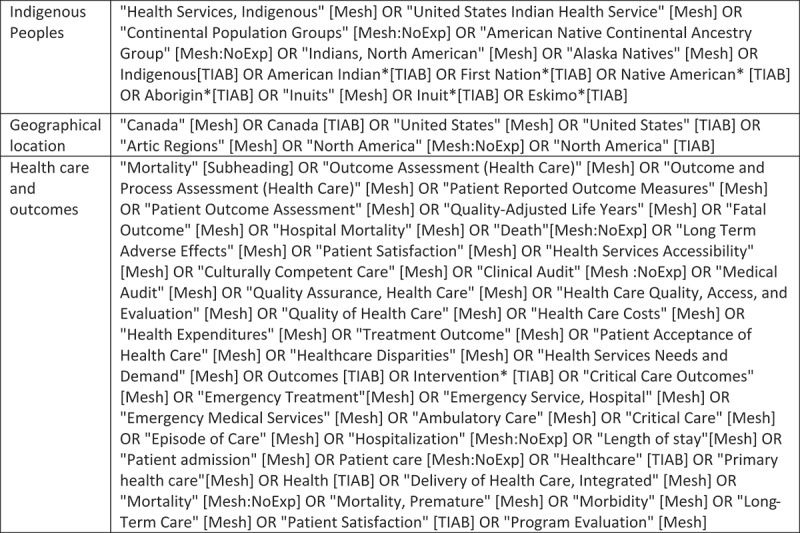
Research strategy for medline
Articles which did not correspond to the objective of the scoping review were excluded from the analysis. This process is described in the flow chart presented below (Figure 2). Articles were excluded based on the fact they did not correspond to the studied population or the type of health care. Articles discussing public health, veterans’ health or paramedical health care were therefore excluded from this analysis. Articles that were not in English or in French were also excluded. The selection of articles was assessed by two independent authors (L.P.V., A.P., E.D., C.S.P). Canadian and American articles were divided into separate groups given the major differences between their health care systems.
Figure 2.
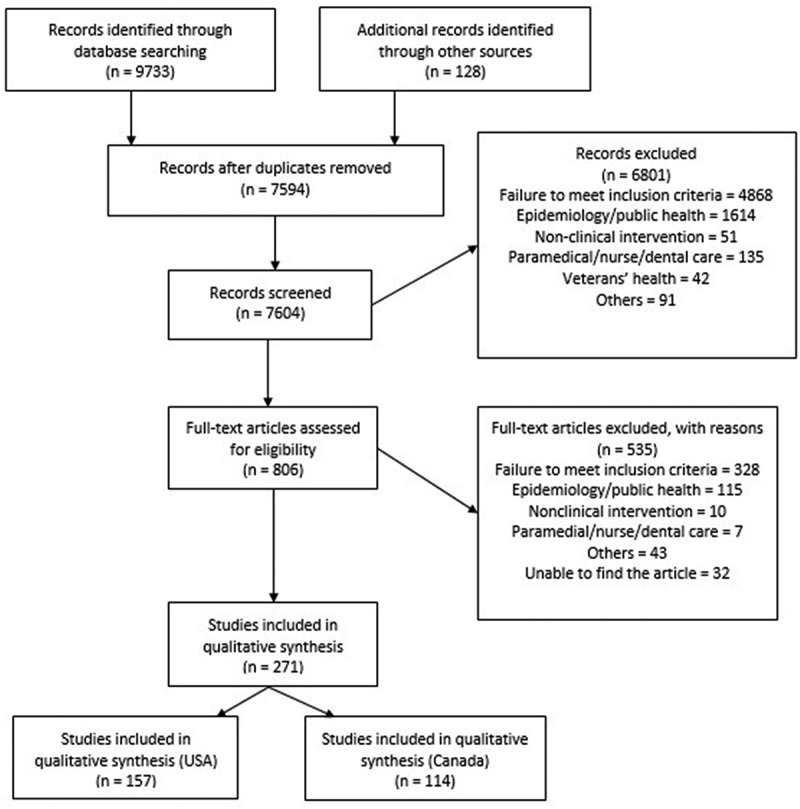
Flow diagram
Data from each article were collected by three independent readers, every article being reviewed by two readers (L.P.V., E.D., C.S.P). The data was entered independently in a data collection form and two readers then discussed the results to ensure an objective data extraction process. To assess the quality of the different articles retrieved, we used the STROBE Statement checklist for cohort studies, cross-sectionals studies and case-control studies [10]. These checklists provide a score based off of a total of 22 items. We also used a STROBE checklist for abstracts [10] which provides a score out of 11. The checklist to assess the quality of qualitative studies [11] provides a score out of 32 and the checklist for case reports provides a score out of 13 [12]. For each of these checklists, a criterion was considered not fulfilled if one of its sub-items was missing. Two independent readers (L.P.V., C.S.P, E.D.) completed the quality analysis for each article.
Results
114 articles studying the Indigenous Peoples in Canada and acute health care were retrieved. Figure 3 presents the distribution of articles according to the studied province although articles often collected data from more than one province or territory. Acute care provided to Indigenous Peoples has been most studied in the provinces of Alberta, Manitoba and Ontario. As indicated in Figure 4, most studies were retrospective (n = 86) and 14 articles were prospective. The rest of the articles were either case reports (n = 4), qualitative (n = 6), descriptive (n = 2), cross-sectional (n = 1) or comparative studies (n = 1).
Figure 3.
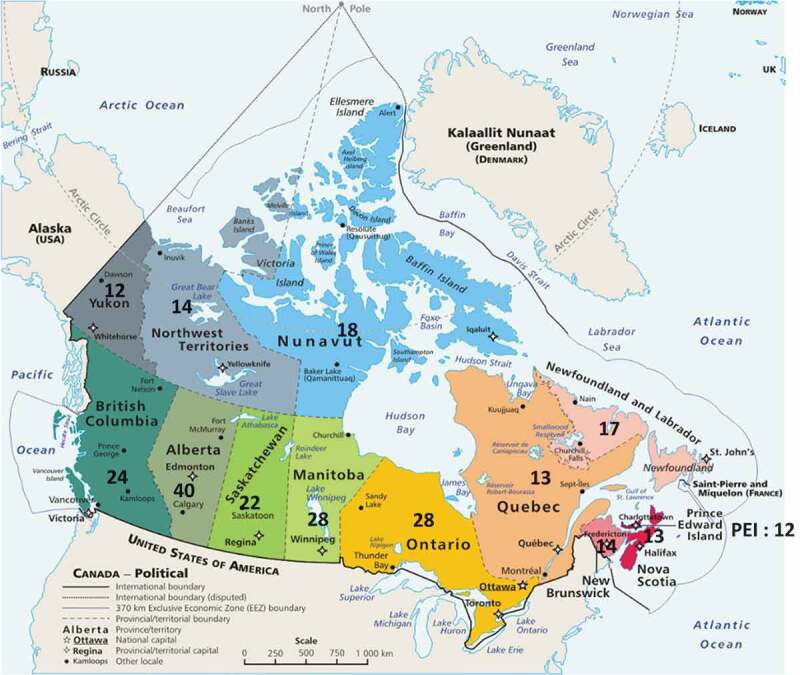
Distribution of articles by province
Figure 4.
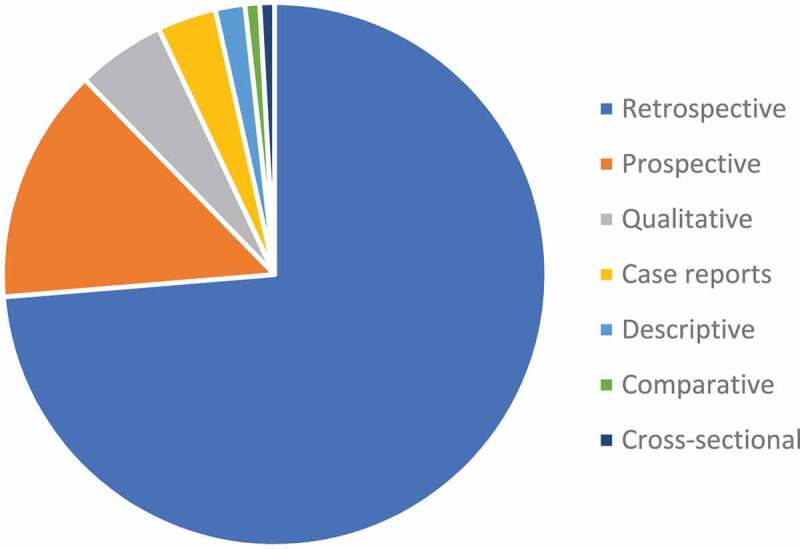
Studies’ design
The general characteristics of the articles are presented in Table 1. Most articles studied hospitalisation (73,7%) and the most frequently studied population were First Nations (47.3%). Figure 5 illustrates the distribution of articles by year of publication. The number of studies discussing acute health care for Indigenous Peoples exponentially increased in the 2000’s as only 17 studies were published before 2000. Table 2 shows the distribution of articles according to their studied outcomes. The most frequently studied outcome was hospitalisation rates (58,8%), followed by length of stay (28.0%), mortality (25.4%) and quality of care (24.6%). The most studied health conditions are pulmonary diseases (n = 27), injuries and poisonings (n = 16), cardiovascular diseases (n = 9) and psychiatric illnesses (n = 8) as presented in Table 3.
Table 1.
Main features of articles
| Indigenous Peoples by group: First Nations Métis Inuit Non specified Indigenous peoples |
54 14 21 45 |
| Age of population cohorts | All ages: 57 Paediatric*: 29 Adults*: 28 |
| Type of acute health care Hospitalisation Emergency department visits Intensive care unit admissions Surgical intervention Other/Non defined |
84 29 8 6 5 |
| Journals which published >1 retrieved articles | Am J Public Health: 4 Am J Resp Crit Care: 2 BMC Public Health: 2 C J Public Health: 4 Can J of Cardiol: 3 Can J of Psychiat: 2 Chest: 2 CJEM: 3 CMAJ: 6 CMAJ Open: 2 Chron Dis Inj Can: 2 Ethnic Health: 2 Health Rep: 4 Int J Infect Dis: 2 Int J Circumpol Heal: 7 J Pediatr: 2 J Rheumatol: 2 Pediatr Infect Dis J: 3 Pediatr Pulm: 2 PLoS One: 3 |
* Given that the age of majority differs between provinces, the distinction between paediatric and adult patients was adjusted according to the province of origin of the studies. The age of majority is 18 years old in Alberta, Prince-Edward-Island, Manitoba, Ontario, Quebec and Saskatchewan and is 19 years old in British Columbia, New-Brunswick, Nova-Scotia, Nunavut, Newfoundland and Labrador, Northwest territory and Yukon.
Figure 5.
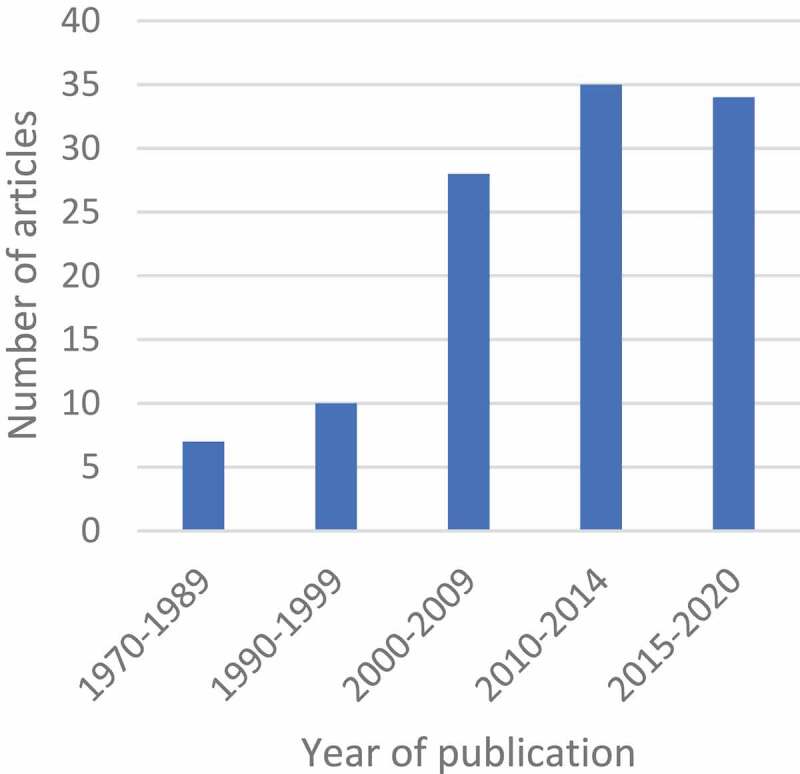
Distribution of articles by year of publication
Table 2.
Distribution of articles by studied outcomes
| Outcomes | Number of articles (%) |
|---|---|
| Health care satisfaction | 9 (7.9%) |
| Access to care | 14 (12.3%) |
| Hospitalisation rate | 67 (58.8%) |
| Emergency department visit rate | 26 (22.8%) |
| Mortality | 29 (25.4%) |
| Quality of care | 28 (24.6%) |
| Length of stay | 32 (28.0%) |
| Cost | 7 (6.1%) |
Table 3.
Studied health conditions
| Illness | Number of articles |
|---|---|
| Pulmonary diseases Injuries and poisonings Cardiovascular diseases Psychiatric diseases Rheumatologic diseases Neurological diseases Endocrine-related conditions Paediatric-related diseases Gastrointestinal diseases Infectiology-related diseases Obstetrical and gynaecological conditions Nephrological-related conditions |
27 16 9 8 5 5 5 5 4 4 4 1 |
The complete tables for each of the 114 studies are presented in Appendix 1. Studies are distributed according to their health condition of interest.
Health care satisfaction
Nine articles collected information concerning Indigenous Peoples’ health care satisfaction. One article reported great satisfaction of Indigenous Peoples while consulting through telemedicine [13]. Another article concluded that the health care satisfaction is inferior for Indigenous patients suffering from mental illness when compared to non-Indigenous patients [14]. The other seven studies reported several cases of stigmatisation and racism in the health care system. Study participants evoked certain barriers in their access to health care such as long wait times, trouble communicating and difficult interactions with health care professionals. Most of these issues were attributed to cultural differences and misinterpretations, often exacerbated in a bustling hospital setting [15,16]. Another important problem reported was the misperception by many health care professionals that Indigenous patients are seeking health care in order to receive drugs [17,18]. Others mentioned that health care providers tend to attribute illnesses to alcohol or drug consumption without completing a thorough history with the patient [17]. An Indigenous patient also stated not always inquiring about illness or treatment options due to communication barriers and subsequent difficulties understanding the information provided [15]. It has also been mentioned that some Indigenous patients are afraid of visiting hospitals and will avoid them by all means [17,19]. Many Indigenous patients felt they were treated differently and appreciated when health care professionals treated them as they would any other patient while also recognising and respecting their Indigenous identity [15,18].
Tang published two articles in which he interviewed health care professionals working in an urban emergency department in Canada as well as Indigenous patients. In his study published in 2008, Indigenous patients expressed often experiencing discrimination in the emergency department setting. Four health care providers were questioned on this subject and presented similar answers. They maintained that they provide the same quality of care to all patients including Indigenous patients, however, certain contradictions were raised in the testimonies of different health professionals. A health care provider said: “As an ED staff person, you tend to have a vision of every Aboriginal person having a drug and alcohol issue […]” [20]. This same provider later admitted to being more guarded when meeting an Indigenous patient. In Tang’s study published in 2015, health care providers were asked to describe their perception of Indigenous patients. A few health care providers provided similar answers which can be summarised by the following statement by health care provider 11: “A lot of them are on welfare or drug pushers […]. They don’t seem to have jobs, not well dressed, dirty, unkempt, using drugs, not taking care of themselves”. [21] Another health care provider explained why, in his opinion, Indigenous patients are dissatisfied with the health care they receive: “We’ll meet all of their needs, and when that doesn’t happen, there is a great deal of frustration of their part which makes it almost confrontational at times, it can be incredibly challenging to remain compassionate and non-judgemental about patients we see, when that kind of situation arises”. [21]
Access to health care
Articles discussing access to care presented data that for the most part cannot be grouped given the great diversity of studied outcomes. Four articles reported an inferior access to care when compared to non-Indigenous Canadians. This decreased access is characterised by a longer time between onset of symptoms and hospital presentation [22,23], a lower proportion of patients with access to prenatal care [24] and a lower satisfaction towards health care in general [16]. Five articles reported no difference in access to care for Indigenous Peoples when compared to other Canadians [25–29]. One study reported that specialist follow-up visits after an episode of arrhythmia occurs approximately 80 days earlier for Indigenous patients [30]. Firestone reported that 60% of questioned Indigenous patients consider their access to care to be excellent or good whereas 11% of them consider it to be poor [31]. A study reported that Indigenous patients mainly use the emergency department to access health care [19]. Another study reported that, for psychiatric patients, hospitalisation rates are higher if the primary source of health care is an hospital rather than a nursing centre [32]. Finally, one study was a case report and no conclusions can therefore be drawn [33].
Hospitalisation rates
67 articles studied hospitalisation rates. 48 studies found higher hospitalisation rates for Indigenous patients. 16 studies mentioned no difference whereas 3 articles mentioned reduced hospitalisation rates for Indigenous patients. 6 articles did not provide any comparison between hospitalisation rates for Indigenous and non-Indigenous patients [34–39]. For articles concerning multiple health issues, 10 articles concluded to higher hospitalisation rates for Indigenous patients [31,40–48]. With regards to pulmonary diseases, seven articles concerning pneumonia [22,49,50], LRTI (lower respiratory tract infection) [51], bronchiolitis [52] or H1N1 Influenza A [23,53] showed increased hospitalisation rates. 4 articles showed no difference in hospitalisation rates for asthma and COPD (chronic obstructive pulmonary disease) [40], LRTI [54,55] and aspiration pneumonia [22]. Senthilselvan’s study on asthma presented increased hospitalisation rates for age groups ranging from 0–4 and 35–64 years old. Meanwhile the group aged from 15 to 34 years old showed no difference in hospitalisation rates and the group aged from 5 to 14 years old had decreased hospitalisation rates [56]. As for unintentional injuries, 8 articles presented higher hospitalisation rates [57–64] whereas two articles mentioned no difference [65,66]. Three articles studied intentional injuries, two of which showed an increased hospitalisation rate for Indigenous patients [64, 67] while the other showed no difference [60]. With regards to poisonings, two articles published in 2007 by Myers mentioned a risk ratio for hospitalisation for acetaminophen overdose of approximately 4 [68,69]. For cardiovascular diseases, three articles provided results of increased hospitalisation rates [70–72] and one article mentioned decreased hospitalisation rates [73]. Atzema reported increased hospitalisation rates related to hypertension and congestive heart failure and found no difference for acute coronary syndromes, strokes and atrial fibrillation [74]. Kapral also found no difference in hospitalisation rates for strokes [75]. Increased hospitalisation rates were reported for pyelonephritis [76], acute complications of dialysis [77], epilepsy [78] and traumatic brain injury [79] and for all types of arthritis except ankylosing spondylitis [80]. One article found no difference in hospitalisation rates for cancer-related complications [81]. For mental health issues, five articles presented increased hospitalisation rates [32,82–85]. Carrière’s article showed increased hospitalisation rates for all mental illnesses except for personality disorders [82] and Soleimani’s article mentioned increased hospitalisation rates for women but decreased rates for men [85]. Articles about paediatric-related illnesses concluded to increased hospitalisation rates for acute otitis media [86], as well as for infections, congenital anomalies, respiratory, cutaneous, neurological and endocrine diseases and found no difference in hospitalisation rates for other health problems [87]. Finally, three articles showed higher hospitalisation rates for diabetes-related complications [88–90] and one article showed no difference between Indigenous and non-Indigenous patients [91].
Emergency department visit rates
26 articles presented results regarding emergency department visit rates. 17 studies found higher emergency department visit rates for Indigenous patients. 6 articles showed increased emergency visit rates for Indigenous patients with asthma or COPD [92–97] while one article reported no difference [40]. Two articles reported higher visit rates for LRTI [98,99]. Ospina’s article showed increased visit rates for all Indigenous communities except for Métis people for whom no difference was reported [92]. In articles discussing multiple acute health conditions, 2 articles found higher visit rates [31,40] while 4 articles reported no difference [26,27,43,100]. Most articles found higher emergency department visit rates for cardiovascular problems [30,70,74] with the exception of Atzema’s study which reported higher visit rates for all illnesses except for hypertension [74]. One article found higher visit rates for epilepsy [78]. For diabetes-related complications, one study found higher emergency department visit rates for all Indigenous patients [88] whereas another study found that only First Nation patients living off-reserve had higher visit rates [101]. Only one study found lower emergency department rates for Indigenous patients [94]. Four studies did not present a comparison with non-Indigenous patients and conclusions could therefore not be drawn [102–105]. Finally, Newton found that Indigenous patients had double the rate of emergency visits for self-harm [106] and for psychiatric illnesses [107] when compared to non-Indigenous patients.
Mortality
Mortality was studied as an outcome in 29 studies. 8 articles reported an increased mortality, 10 articles found no difference in mortality rates and 5 articles reported a decreased mortality for Indigenous patients. 7 articles provided mortality data without providing comparison to non-Indigenous patients and therefore no conclusion can be drawn for these results [105,108–113]. With regards to pulmonary diseases, two articles mentioned increased mortality for Indigenous patients hospitalised for pneumonia [114] and COPD [40], two studies revealed no difference in mortality for H1N1 Influenza A and asthma [40,115] and three studies showed decreased mortality for Indigenous patients hospitalised for pneumonia [22,49,50]. For injuries and poisonings, two studies reported a higher mortality rate for Indigenous patients [57,60] and one study found no significant difference [116]. Studies reported no difference in mortality rates caused by strokes [75] or obstetrical diseases [24]. As for cardiovascular diseases, most articles reported an increased mortality rate for Indigenous patients [70,71,73,117] although some articles did not report any difference in mortality rates [74,118]. For articles discussing multiple health problems, three studies reported increased mortality for Indigenous patients [46,47,119] and one article reported no change in mortality [45]. Finally, Oppenheimer’s study in 2007 found an increased mortality rate for Indigenous patients hospitalised for blastomycosis of joints and bones [28].
Quality of care
A total of 28 studies discussed the quality of care in their results. Quality of care was often studied for cardiovascular diseases. Atzema found no difference between Indigenous and non-Indigenous patients regarding the use of beta-blockers after an acute coronary syndrome or echocardiography in follow-up of atrial fibrillation [74]. Three studies found no difference in the use or percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) [25,71,117] whereas one study found no difference for CABG but a decreased rate of Indigenous patients receiving PCI [72]. Two studies found Indigenous patients less likely to undergo a coronary angiogram [72,117] and one study mentioned that Indigenous patients tend to wait longer before their coronary angiogram [25]. For pulmonary diseases, two studies found no difference in the quality of care for people with lower respiratory tract infections [55,115] and one study concluded that Indigenous patients with asthma or COPD were 55% less likely to see a specialist and 66% less likely to have a spirometry [96]. For injuries, one study found that Indigenous patients wait longer for their follow-up [106], are less likely to opt for palliative health care and undergo more surgeries [116]. Two studies showed a decreased chance for Indigenous patients to consult a specialist for their health problem [48,120]. For neurological illnesses, Indigenous patients tend to have fewer surgeries for spinal cord trauma [121] and longer wait times before follow-up after a traumatic brain injury [122]. As for strokes, the only difference found was that Indigenous patients were less likely to receive thrombolysis [75]. No difference in health care quality was noted for rheumatological diseases [28] or in neonatal intensive care [24]. Two studies by Newton demonstrated that Indigenous patients receive less follow-up after a visit to the emergency department for mental illness [103,107]. A study found that Indigenous patients presenting with appendicitis underwent more open surgeries and waited longer between their time of presentation at hospital and the beginning of their surgery [123]. Rose’s study found that Indigenous patients underwent more forefoot and below the knee amputations and fewer toe or above the knee amputations for diabetes-related complications [90]. Finally, seven articles did not provide any comparison with non-Indigenous patients [33,109–112,124].
Length of stay
For Indigenous patients with pneumonia or COPD, three studies revealed an increased length of hospital stay [55,56,114], two studies found no difference [54,115] and five studies showed decreased length of stay when compared to non-Indigenous patients [22,49,50,92,93]. Two articles mentioned longer hospitalisations for burn injuries [58,116]. For articles discussing multiple acute health problems, two studies showed a longer length of stay for Indigenous patients [42,46], one study reported a shorter length of stay [119] and four studies showed no difference [26,27,45,104]. Although no statistically significant difference was noted, Laupland found that over 17% of Indigenous patients were delayed in their discharge because of transportation issues or lack of resources in their community [45]. For psychiatric diseases, length of stay was found to be longer in one study [14] and shorter in two other studies [32,84]. One article found no difference between the length of stay in the emergency department for Indigenous and non-Indigenous patients [103]. Six studies did not provide any comparison with non-Indigenous patients [33,36,37,52,108,112]. There was no difference in length of stay for Indigenous patients with traumatic brain injury [122], blastomycosis of bones [28] or appendicitis [123]. Finally, Indigenous neonates stayed longer in the intensive care unit when hospitalised [24].
Cost
Seven studies discussed cost of health care for Indigenous patients. Five articles concluded to increased health care cost for Indigenous patients living in remote areas [36,51] as well as for Indigenous patients in general [22,91,125]. One study showed no statistically significant difference in health care cost [126] and one article provided no comparison with non-Indigenous patients [37].
Discussion
In this study, we found 114 articles that studied acute health care provided to Indigenous patients. Most studies presented results for Indigenous patients of all ages, focused on hospitalisation rates and were mainly retrospective. Only six articles out of 114 were qualitative, which is surprising considering the importance of qualitative studies in understanding the perception of health care of Indigenous patients. All provinces and territories of Canada were represented in the retrieved articles. Hospitalisation rates was the most studied outcome as it was analysed in more than half of all articles. 48 articles out of 67 reported higher hospitalisation rates for Indigenous patients when compared to non-Indigenous patients and 17 articles out of 26 found higher emergency department visit rates. Access to care was studied in 14 articles from which four articles noted a decreased access to care, five reported no difference and one reported a better access for Indigenous patients. For mortality, it is difficult to draw conclusions as eight articles reported an increased mortality, 10 articles reported no difference and five articles reported a decreased mortality for Indigenous patients. As for quality of care, care for cardiovascular diseases was similar for major interventions. The main difference in access to care was that Indigenous patients had less follow-up with specialists or longer wait times than non-Indigenous patients [48,96,103,107,120,122]. Studies discussing length of stay provided diverging results and no clear conclusion can be drawn seeing as nine studies showed increased length of stay, nine showed no difference and eight showed a decreased length of stay. Cost for health care seems to be higher for Indigenous patients since out of 6 studies, 5 articles reported higher costs. Finally, nine articles discussed satisfaction with health care. Most of them reported cases of miscommunication and misinterpretation between Indigenous patients and health care professionals that had an impact on satisfaction with care [15,16]. Throughout these studies, Indigenous patients often mentioned not being satisfied with their access to health care and encountering multiple barriers in the health care system. These barriers include long wait times [15,16],, difficulty communicating [15] as well as prejudices and discrimination [17,19–21]. Indigenous patients mentioned simply wanting to be treated like any other patient by practitioners who respect their Indigenous identity [15,18].
According to our research, no previous review has gathered all articles dealing with disparities in health care between Indigenous and non-Indigenous patients all illnesses combined. Our scoping review highlights important disparities between Indigenous and non-Indigenous patients in Canada, especially with regards to access to care, satisfaction with health care and hospitalisation or emergency department visit rates.
A systematic review on the experiences of Indigenous patients during hospitalisation for acute care was published in 2017 [127]. This review found 21 qualitative articles which provided three themes characterising the experience of Indigenous patients. Firstly, Indigenous patients reported feeling like they were going into a foreign land when they were hospitalised as health care practitioners are not always accustomed to their culture and traditions [128,129]. Furthermore, communication difficulties were frequent because of language barriers and/or cultural differences [130–132]. Finally, relationships with practitioners were sometimes difficult because of diverging views of health care and prejudices they may have had. This review is consistent with our findings which tend to confirm that many Indigenous patients have experienced negative encounters with health care professionals. As for access to care, our study did not provide any clear conclusions but some important elements have nonetheless emerged. A study published in 2018 aimed to identify barriers to health care access and presents similar results as our review. In this study, the most important barriers for Indigenous patients were long wait times, substandard quality of care and discrimination. This article provides an interesting perspective, especially regarding long wait times. Indeed, long wait times are experienced by all patients seeking health care in Canada. However, this article underlines the way in which different cultures and past experiences lead to different interpretations of certain events and these differences must be recognised in order to provide culturally safe care [132].
The use of health services by Indigenous Peoples has been studied for various health conditions in Australia over the past years. A review published in 2016 discussed the use of the emergency room by Indigenous Peoples living on Torres Island. Indigenous patients consulted at the emergency department more often than other Australians [133]. An article studying visits to the emergency department by Indigenous patients in 2004–2005 arrived to the same conclusion but also found that Indigenous patients were more likely to leave the emergency department before being seen by a health care practitioner [134]. A study with the same aim has recently been published in Canada and the results are very similar to those found in Australia [135]. Another study published in Australia about intensive care unit admissions also obtained similar results. Indigenous patients were over-represented in the ICU and more frequently required emergency admissions although no difference was found in mortality [136].
Some authors have suggested solutions to improve the quality of health services provided to Indigenous patients. A study in Australia suggested that health care services managed by Indigenous patients are the best way to maximise their access to care [137]. A scoping review published in 2009 grouped articles regarding Indigenous patients’ experience within emergency departments in Canada [138]. The author’s concluded that developing cultural competency is essential in order to upgrade the quality of health care. In order to achieve this, it is necessary to have a shared understanding of Indigenous communities and to collaborate with them. It is also essential to prevent discrimination by providing appropriate training to professionals and by promoting access to health care services [138]. A systematic review published in 2015 obtained the same conclusions. It identified training health care workers and recruiting Indigenous workers as the most effective interventions to improve cultural competency. These interventions improve patient’s satisfaction of care [139]. Another strategy for improving quality of care is integrated care [140]. Health care provided in a multidisciplinary approach, which encompasses all aspects of health can reduce disparities in health care and help communities achieve a better state of health. This approach involves the patient as an active partner in his health care and aims to include psychological and spiritual aspects of health care [140].
Changes in the health care system must be made to improve the quality of health care provided to Indigenous Peoples in Canada. Solutions to reconcile Indigenous cultures with hospital practices to provide health care in a culturally safe organisation should be explored. Future health care workers must be taught about the cultures and traditions of Indigenous Peoples in regard to health care. To increase cultural competency and prevent racism, future health care providers must recognise and understand cultural differences, in order to adapt their practice to each patient. Furthermore, no studies have focused on understanding the fundamental causes behind the differences in the prevalence of health problems disproportionately affecting Indigenous Peoples. Interventions to reduce the disproportionately high prevalence of certain diseases affecting Indigenous Peoples need to be explored. Finally, very few qualitative studies were performed with Indigenous Peoples in Canada. Studies examining ways in which health care could be improved with Indigenous communities would be important. Indeed, it is essential to include Indigenous communities in the discussions about health care to ensure their perspectives and traditions are respected.
Given that our study is a literature review, its quality depends of the quality of the articles included. The articles retrieved are mostly retrospective or prospective cohort studies (median STROBE score = 15/22). The quality scores differ for qualitative studies (median = 21/32), case reports (Median = 7/13) and abstracts (median = 7/11). No randomised control trials have been published about health care issues of Indigenous Peoples in Canada in an acute care setting. 18 articles were published before 2000 and the quality of their evidence may therefore differ from current standards. It is important to mention that although all included Indigenous Peoples live in Canada, important differences exist between each community. Indeed, access to care may vary depending on the location of the community. Furthermore, every community has a unique history and traditions as well as a unique perspective on health care. The health care system in Canada also varies depending on the territory and nation of Indigenous Peoples. This thus limits the generalisation of our results as data retrieved from a specific community may not apply to others. Our study is at risk of a publication bias since articles with positive results are more likely to be published than negative studies. To minimise this bias, incomplete articles were included in the analysis and available data was used. A publication bias would increase the proportion of articles showing disparities between health care provided to Indigenous and non-indigenous Canadians. Studies regarding Indigenous Peoples completed by non-Indigenous authors are at risk of interpretation bias which is difficult to estimate. This review presents the same risk since the authors are non-Indigenous. To diminish the importance of this bias, articles were included with objective inclusion criteria and studied outcomes were clearly defined. Also, subjective data was drawn directly from published data and does not reflect personal opinions. To prevent subjectivity in data interpretation, at least two different authors were involved in the reading of articles and extraction of data. Another limit of this article is the small number of articles that exist relative to certain specific topics such as health care costs making it impossible to draw conclusions about their impact on Indigenous Peoples. Finally, the small number of existing qualitative studies may affect the generalisability of conclusions about satisfaction with health care since only a small proportion of Indigenous patients and communities were questioned on this particular topic.
Conclusion
Indigenous Peoples in Canada still face significant inequalities in their access to health care when compared to non-Indigenous Canadians. They also carry a greater burden of health problems requiring acute health care, particularly in regards to pulmonary, cardiovascular, traumatic and psychiatric illnesses. Furthermore, their satisfaction with health care is lower than that of other Canadians which in turn limits their use of health care services. Given the historical context of colonialism in Canada and the persistence of significant disparities between Indigenous and non-Indigenous populations, it is essential to include Indigenous communities in the organisation of health care. Indigenous Peoples are most well informed of their reality and are best suited to identify their needs. It is essential to ensure that Indigenous Peoples in Canada have access to culturally safe health care, which embraces their unique perspective on health.
Disclosure statement
No potential conflict of interest was reported by the author(s).
| PULMONARY DISEASES (n = 27) | ||||||
|---|---|---|---|---|---|---|
| Main author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Alaghehbandan (2005, Am J of Epidemiology) (49) |
|
Pneumonia Hospitalisation |
|
Hospitalisation rates (/1000) (p < 0.0001) In-hospital mortality Length of stay |
Gr 1: 11.6 (Innu: 16.9; Inuit 8.4); Gr 2: 3.0 Lower for Indigenous Shorter for Indigenous |
7/11 |
| Alaghehbandan (2007, Int J Infect Dis) (50) |
|
Pneumonia Hospitalisation |
|
Standardised hospitalisations rates (/1000) (95% CI) Mortality (p < 0.00001) Median length of stay (days) |
Gr 1: 4.82 (4.21-5.37); Gr 2: 1.03 (0.96-1. Gr 1: 2.1%; Gr 2: 10.1% Gr 1: 3.0; Gr 2: 5.0 |
18/22 |
| Alharbi (2012, BMC Infect Dis) (105) |
|
LRTI ED visits |
|
ED visits rates Mortality |
112/193 (58%) 0% |
15/22 |
| Banerji (2001, CMAJ) (35) |
|
LRTI Hospitalisation |
|
Annualised incidence rate of admission (/1000) | 484 | 12/22 |
| Banerji (2001, Int J Circumpol Heal) (34) |
|
Bronchiolitis Hospitalisation |
|
Rate of hospital admission (/1000) | 306 | 10/22 |
| Banerji, Greenberg et al (2009, Pediatr Infect Dis J) (51) |
|
LRTI Hospitalisation |
|
Odds ratio for hospitalisation (95% CI) Average cost per admission (< 1 year old/ < 6 months old) Annual admission rate/1000 live births without use of Palivizumab (<1 year old/ <6 months old) |
Inuit: 3.8 (1.1-12.8) Gr 1: 19,014$/21,145$; Gr 2: 3915$/ 3621$; Gr 3: 21,345$/23,030$; Gr 4: 20,770$/ 22,673$ Gr 1: 166/245; Gr 2: 63/72; Gr 3: 216/328; Gr 4: 349/512 |
14/22 |
| Banerji (2013, Int J Circumpol Heal) (36) |
|
LRTI Hospitalisation |
|
Hospitalisation rates/1000 live births Median length of stay (days) Cost per admission |
Gr 1: 38; Gr 2: 236; Gr 3: 445 Gr 1: 5; Gr 2: 6; Gr 3: 5 Gr 1: 36,542$; Gr 2: 55,265$; Gr 3: 23,203$ |
14/22 |
| Charland (2011, Epidemiol Infect) (98) |
|
Influenza, Bronchitis, Pneumonia ED visits |
|
Standardised Risk Ratios to visit ED for Mohawks all ages (95% CI) | Influenza: 1.58 (1.49-1.67) Influenza + Pneumonia: 1.51 (1.44-1.58) Influenza + Bronchitis: 1.48 (1.44-1.53) Respiratory infection: 1.21 (1.19-1.23) |
15/22 |
| Creery (2005, Int J Circumpol Heal) (37) |
|
Bronchiolitis Hospitalisation |
|
Annual admission rate of children <1 year old Average length of stay (days) Overall average cost per admission Cost per admission to Baffin Regional Hospital Cost per admission to CHEO |
197/1000 5.7 14,273$ 12,029$ 45,688$ |
17/22 |
| Gershon (2014, PLoS One) (40) |
|
Asthma, COPD Hospitalisation, ED visits |
|
Standardised rates/1000 for people with Asthma (95% CI) Standardised rates /1000 for people with COPD (95% CI) Standardised all-cause mortality/1000 Metis/Ontarians |
All-cause ED visits: Gr 1: 761.7 (729.0-795.8); Gr 2: 563.9 (562.9-565.0) Asthma ED visits: Gr 1: 26.3 (21.2-32.2); Gr 2: 21.5 (21.3-21.7) All-cause hospitalisations: Gr 1: 118.9 (104.5-134.7); Gr 2: 93.1 (92.6-93.5) Asthma hospitalisations: Gr 1: 5.8 (3.2-9.8); Gr 2: 4.7 (4.6-4.8) All-cause ED visits: Gr 1: 910.7 (861.3-962.2); Gr 2: 674.3 (672.5-676.2) COPD ED visits: Gr 1: 26.7 (20.4-34.3); Gr 2: 32.2 (31.9-32.5) All-cause hospitalisations: Gr 1: 176.3 (155.9-198.5); Gr 2: 132.7 (132.0-133.4) COPD hospitalisations: Gr 1: 32.9 (25.1-42.3); Gr 2: 25.0 (24.7-25.3) Asthma: 68.0/65.0 (p = 0.67) COPD: 39.0/29.0 (p = 0.01) |
21/22 |
| Houston (1979, CMAJ) (114) |
|
Pneumonia Hospitalisation |
|
Mortality Average length of stay (days) |
Gr 1: 4/102; Gr 2: 0/64 Whites Gr 1: 26.9; Gr 2: 8.7 |
11/22 |
| Hui (2016, Pediatr Infect Dis J) (54) |
|
LRTI Hospitalisation, ICU admissions |
|
Hazard ratio of hospitalisation (95% CI; p) % of ICU admission (p = 0.334) Mean Length of stay (days) (p = 0.598) |
Gr 1: 1.2 (0.7-2.2; p = 0.383) Gr 1: 17.4%; Gr 2: 21.5% Gr 1: 9.0; Gr 2: 8.3 |
16/22 |
| Jung (2011, Am J Resp Crit Care) (115) |
|
H1N1 Influenza A Hospitalisation ICU admissions |
|
Hospitalised critically ill patients (384 patients) Mortality (p = 0.25) Frequency of reception of antivirals (p = 0.50) Mean ICU length of stay (days) (p = 0.72) Mean hospital length of stay (days) (p = 0.20) |
Gr 1: 16.7% Gr 1: 15.6%; Gr 2: 23.8% Gr 1: 92.2%; Gr 2: 94.4% Gr 1: 17.0; Gr 2: 14.6 Gr 1: 23.2; Gr 2: 24.4 |
9/11 |
| Marrie (2004, Can Respir J) (22) |
|
Pneumonia Hospitalisation |
|
Hospital discharge rate for community acquired pneumonia/1000 (95% CI) Hospital discharge rate for aspiration pneumonia/1000 (95% CI) Mean distance to closest hospital (km) Mortality odds ratio (95% CI) Median length of stay (days) Odds ratio for daily hospital cost higher than the median cost of 722.71$ (95% CI) |
Gr 1: 22.1 (20.7-23.6); Gr 2: 4.4 (4.4-4.5) Gr 1: 1.29 (0.96-1.6); Gr 2: 0.27 (0.26-0.29) Gr 1: 21; Gr 2: 6 Gr 1: 0.49 (0.37-0.66) Gr 1: 6.1; Gr 2: 7.8 Gr 1: 1.25 (1.14-1.36) |
14/22 |
| McCuskee (2014, Pediatr Infect Dis J) (52) |
|
Bronchiolitis, Pneumonia Hospitalisation |
|
Admission rate for < 1 year old (p = 0.011) Admission rate for <6 months old Mean length of stay |
Gr 1: 4.4%; Gr 2: 2.5% Gr 1: 5.6% 3.2 days |
17/22 |
| Morrison (2014, Health Place) (23) |
|
H1N1 Influenza A Hospitalisation |
|
Access to care (p<0.001) Odds ratio for hospitalisation |
On-reserve First Nations have a longer delay between infection and hospitalisation. OR = 2.34 (1.16-4.73) |
18/22 |
| Mostaco-Guidolin (2013, Am J Public Health) (53) |
|
H1N1 Influenza A Hospitalisation |
|
Hospitalisation risk ratio (p < 0.001) | In all First Nations age groups during the first wave, they were significantly higher than those in non-First Nations age groups. | 15/22 |
| Ospina (2015, Am J Resp Crit Care) (92) |
|
COPD Hospitalisation |
|
Risk ratios for hospitalisation for all causes (95% CI) Risk ratios for hospitalisation for AECOPD (95% CI) Median hospital length of stay (days) |
Gr 1: 1.31 (1.24-1.37); Gr 2:1.60 (1.52-1.69); Gr 3: 0.80 (0.72-0.88); Gr 4: 0.71 (0.64-0.79) Gr 2: 1.44 (1.26-1.65); Gr 3: 1.10 (0.89-1.36); Gr 4: 0.67 (0.52-0.86) Gr 2: 5; Gr 3: 5; Gr 4: 4 All shorter than for Non-Aboriginals. |
10/11 |
| Ospina (2016, CJEM) (93) |
|
COPD ED visits |
|
Adjusted Risk Ratio for ED visits rates (95% CI) Median ED length of stay (hours) |
Gr 1: 1.72 (1.67-1.77); Gr 2: 2.02 (1.97-2.08); Gr 3: 1.28 (1.22-1.35); Gr 4: 0.94 (0.90-0.98) Gr 1: 2.8; Gr 2: 2.9; Gr 3: 2.4; Gr 4: 2.2; Gr 5: 3.7 |
16/22 |
| Poling (2014, Can J of rural medicine) (108) |
|
Pneumonia Hospitalisation |
|
% of death resulting from pneumonia Mean length of stay (days) |
3% 5.32 |
15/22 |
| Rosychuk (2010, Pediatr Pulm) (99) |
|
Croup ED visits |
|
ED visit rates/1000 infants for croup (95% CI) | 1999-2000: Gr 1: 28.1 (23.7-32.4); Gr 2: 43.4 (41.8-44.9) 2004-2005: Gr 1: 29.7 (24.9-34.5); Gr 2: 34.1 (32.8-35.4) |
17/22 |
| Rosychuk (2010, Pediatr Pulm) (94) |
|
Asthma ED visits |
|
Directly standardised rates per 1000 for ED visits for asthma (95% CI) | 1999-2000: Gr 1: 28.1 (26.0-30.2); Gr 2: 21.1 (20.5-21.6) 2004-2005: Gr 1: 29.7 (27.5-31.9); Gr 2: 19.8 (19.3-20.2) |
17/22 |
| Rowe (2009, Chest) (95) |
|
Asthma ED visits |
|
ED visits rates (95% CI) | Gr 1: 14.9 (13.2-16.5); Gr 2: 6.8 (6.6-6.9) | 16/22 |
| Senthilselvan (1995, J Clin Epidemiol) (56) |
|
Asthma Hospitalisation |
|
Hospitalisation risk ratios for Gr 1 for 1985-1989 (95% CI) Hospitalisation rates/1000 for Gr 1 in 1989 Average length of stay |
0-4 y.o.: 2.97 (2.75-3.20); 5-14 y.o.: 0.78 (0.67-0.92) 15-34 y.o.: 0.99 (0.81-1.21); 35-64 y.o.: 2.83 (2.42-3.33) 0-4 y.o.: Asthma: 21.73; Bronchitis: 53.47; LRTI: 4.11 35-64 y.o.: Asthma:3.43; Bronchitis: 5.24; LRTI: 3.24 Greater for Indigenous children under 14 years of age |
15/22 |
| Sin (2002, Chest) (96) |
|
Asthma, COPD ED visits |
|
Risk ratio for ED visits for Gr 1 (95% CI) Quality of care |
2.10 (2.01-2.19) Indigenous 55% less likely to see a specialist and 66% less likely to undergo spirometry |
13/22 |
| Sin (2004, Arch Pediat Adol Med) (97) |
|
Asthma ED visits |
|
Risk ratio for ED visits for Gr 1 (95% CI) | 1.20 (1.11-1.29) | 17/22 |
| Wang (1995, J Pediatr) (55) |
|
LRTI ICU admission |
|
Odds ratio for ICU admission (95% CI) 95% CI odds ratio for ventilation Prolonged hospitalisation in days |
Gr 1: 3.1 (1.0-9.2) Gr 1: 0.3-2.3 Gr 1 1.2 (1.1-1.4) |
17/22 |
LRTI: Lower respiratory tract infection, ED: Emergency department, y.o.: years old, F/M: Female/Male, Gr: Group, COPD: Chronic obstructive pulmonary disease, ICU: Intensive care unit, AECOPD: Acute exacerbation of chronic obstructive pulmonary disease
| INJURIES AND POISONINGS (n = 16) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Alaghehbandan (2010, Int J Circumpol Heal) (57) |
|
Unintentional injuries Hospitalisation |
|
Hospitalisation rates/100,000 (95% CI) Risk ratio for hospitalisation for Aboriginals (95% CI) Mortality/100,000 (p <0.001) |
Gr 2: 1329.2 (1008.3-1650.2); Gr 3: 972.1 (731.3-1212.9); Gr 4: 1142.3 (857.3-1427.4); Gr 5: 614.2 (597.1-631.3) 0-4 y.o.: 1.78 (1.30-2.45); 5-9 y.o.: 1.62 (1.18-2.22); 10-14 y.o.: 1.83 (1.38-2.42); 15-19 y.o.: 2.28 (1.76-2.95) Gr 1: 84.3; Gr 5: 10.2 |
18/22 |
| Alaghehbandan (2012, Burns) (58) |
|
Burns Hospitalisation |
|
Hospitalisation rates/100,000 Median length of stay (days) |
Total: (p <0.001)) Gr 1: 20.3/ Gr 2: 51.4 Gr 1: 5.0; Gr 2: 3.0 |
16/22 |
| Anne George (2013, Int J Circumpol Heal) (59) |
|
Injuries Hospitalisation Primary care visits |
|
Standardised risk ratio to be hospitalised Standardised risk ratio to visit primary care |
Gr 1: 1.3-3.7; Gr 2: 0.6-1.9 * RR varies with health service delivery areas Gr 1: 1.2-2.1; Gr 2: 0.8-1.3 |
13/22 |
| Bell (2011, Inj Prev) (60) |
|
Injuries Hospitalisation |
|
Hospitalisation rates/100,000 for Mortality rates/100,000 * p ≤ 0.05 |
Unintentional injuries: Gr 1: 622.2*; Gr 2 322.1 Intentional self harm: Gr 1: 7.5; Gr 2: 8.3 Injuries involving third party: Gr 1: 67.5*; Gr 2: 32.4 Unintentional injuries: Gr 1: 368.1*; Gr 2: 240.4 Intentional self harm: Gr 1: 168.7*; Gr 2: 97.7 Injuries involving third party: Gr 1: 23.0; Gr 2: 14.7 |
18/22 |
| Boeckx (1977, Paediatrics) (109) |
|
Gasoline sniffing and tetraethyl lead poisoning Hospitalisation |
|
Mortality Type of treatment |
1 death/ 2 cases CASE 1: 24h of EDTA and Dimercaprol. Then treatment with penicillamine. Discharge after 4 weeks with continued penicillamine. Returned 3 times to the hospital. The third time: treatment with Phenobarbital and Dilantin failed. He was diagnosed with aspiration pneumonia treated with Cloxacillin and Gentamicin. He died 72h after admission. CASE 2: Multivitamins, IV fluids and glucose. Then 5 days of EDTA twice. Then penicillamine for 4 weeks. He was readmitted and treated again because of gasoline sniffing 6 months later. |
7/13 |
| Bougie (2014, Health Rep) (65) |
|
Unintentional injuries Hospitalisation |
|
Rate ratios for unintentional injury hospitalisations | Gr 1: Females: 1.25; Males: 1.20 Gr 2: Females: 1.20; Males: 1.23 |
17/22 |
| Brussoni (2014, Prev Sci) (66) |
|
Injuries Hospitalisation |
|
Standard relative risk of injury hospitalisation (95% CI) | Gr 1: 1.049 (0.994-1.107) Gr 2: 1.040 (0.984-1.098) |
14/22 |
| Brussoni (2016, BMC Public Health) (62) |
|
Injuries Hospitalisation |
|
Standard relative risk of hospitalisation (95% CI) | Gr 1: 2.61 (2.58-2.64) Gr 2: 2.44 (2.34-2.54) Gr 3: 3.04 (2.98-3.10) Gr 4 1.99 (1.93-2.04) Gr 5: 2.51 (2.46-2.56) Gr 6: 1.0 |
18/22 |
| Brussoni (2018, PLoS One) (63) |
|
Unintentional transport injuries Hospitalisation |
|
Standardised rate ratios (95% CI) | Gr 1, Females: 2.13 (2.03-2.24) Gr 1. Males: 1.69 (1.63-1.75) |
15/22 |
| Callegari (1989, Burns Incl Therm Inj) (116) |
|
Burns Hospitalisation |
|
Deaths % Treatment: Gr 1/ Gr 2 (p <0.05) Number of days in hospital (p <0.05) |
Gr 1: 4.8%; Gr 2: 4.3% Non operative: 34.4%/ 46.9% Surgical with healing: 60.85%/48.85% Surgical with death: 3.2%/1.8% Palliation: 1.6%/2.4% Gr 1: 42.3 days; Gr 2: 25.4 days |
16/22 |
| Finès (2013, Chron Dis Inj Can) (61) |
|
Unintentional injuries Hospitalisation |
|
Age-standardised hospitalisation rate for injuries/10,000 person-years (95% CI) Males/Females | Gr 1: 145.94 (144.13-147.77)/ 103.47 (101.95-105.02) Gr 2: 100.47 (95.14-106.09)/ 86.87 (81.77-92.28) Gr 3: 111.76 (107.71-115.97)/ 73.63 (70.51-76.87) Gr 4: 54.53 (54.36-54.70)/ 37.13 (37.04-37.29) |
16/22 |
| Myers (2007, BMC Public Health (68) |
|
Acetaminophen overdose Hospitalisation |
|
Risk ratio for hospitalisation for acetaminophen overdose for Gr 1 | RR = 4.04 (p < 0.0005) | 16/22 |
| Myers (2007, CJEM) (69) |
|
Acetaminophen overdose Hospitalisation |
|
Risk ratio for hospitalisation for Gr 1 (95% CI) | RR = 4.78 (4.24-5.39) | 17/22 |
| Newton, 2015 (CJEM) (106) |
|
Self harm ED visits |
|
Standardised visit rates/100,000 (95% CI) % of follow up visits for children at 30 days |
2002-2003: Gr 1: 243.5 (194.8-292.1); Gr 2: 101.2 (93.2-109.1) 2010-2011: Gr 1: 201.5 (156.5-246.4); Gr 2: 70.8 (64.4-77.2) Gr 1: 11.6% Families receiving no subsidy: 65.3% Families receiving human services program subsidy: 6.2% Families receiving government-sponsored program subsidy: 16.9% |
17/22 |
| Oliver (2012, Health rep) (64) |
|
Unintentional injuries Hospitalisation |
|
Hospitalisation risk ratio (95% CI) | Gr 1: 2.3 (2.3-2.4); Gr 2: 2.4 (2.2-2.6); Gr 3: 2.2 (2.1-2.4) * RR are higher for Indigenous people for all types of injuries: fall, transportation, struck, poisoning, cut/pierce, fire, environmental, drowning, suffocation. |
16/22 |
| Oliver (2014, Chron Dis Inj Can) (67) |
|
Intentional injuries Hospitalisation |
|
Age-standardised hospitalisation rates per 10,000 person-years for females (95% CI) Age-standardised hospitalisation rates per 10,000 person-years for males (95% CI) |
Total self-inflicted: Gr 1: 28.44 (27.53-29.39); Gr 2: 19.14 (17.37-21.09); Gr 3: 44.04 (40.46-47.95); Gr 4: 6.25 (6.19-6.31) Total self-inflicted: Gr 1: 14.39 (13.75-15.06); Gr 2: 9.56 (8.33-10.96); Gr 3: 21.50 (19.07-24.23); Gr 4: 3.77 (3.73-3.82) |
17/22 |
| MULTIPLE ACUTE HEALTH PROBLEMS (n = 15) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Carrière (2016, Health Rep) (41) |
|
Acute care Hospitalisation |
|
Age-standardised acute care hospitalisation rates/100,000 (95% CI) | Gr 1: 17,042 (16,901-17,183); Gr 2: 11,190 (11,005-11,379); Gr 3: 9535 (9360-9713); Gr 4: 13,227 (12,865-13,598); Gr 5: 6459 (6440-6479) | 17/22 |
| Firestone (2014, BMJ) (31) |
|
ED visits, Hospitalisation |
|
Number (%) of ED visits for acute reason (95% CI) Gr 1/Gr 2 Number (%) of ED visits for non-acute reasons (95% CI) Gr 1/Gr 2 Perception of availability of healthcare among First Nations adults (95% CI) Hospitalisation rates |
None: 50.2% (43.9-57.5)/80.1% 1: 24.7% (18.7-30.1)/13.1% 2-5: 20.7% (15.3-26.1)/6.3% ≥ 6: 4% (1.6-6.9)/0.6% None: 54.3% (47.6-61.2)/81.2% 1: 22.4% (17.3-28.5)/12.2% 2-5: 20.4% (14.5-25.4)/6% ≥ 6: 2.9% (1-5.6)/0.6% Excellent: 16.7% (11.4-22.1); Good: 43.3% (36.1-49.6) Fair: 28.9% (23.3-35.2); Poor: 11.1% (7.9-15.6) Slightly higher among the First Nations population |
18/22 |
| Kashuba (1994, C J Public Health) (42) |
|
Acute diseases Hospitalisation |
|
Hospital separation rate ratio for Gr 1 Patient days rate ratio for Gr 1 Age-adjusted separation rate ratio for Gr 1 |
Males: 2.59; Females: 2.65 Males: 2.18; Females: 2.26 Infectious and parasitic diseases: 4.09 Neoplasms: 0.32 Endocrine, nutritional and metabolic diseases: 7.48 Diseases of blood: 2.09 Mental disorders: 6.81 Diseases of the nervous system: 3.23 Diseases of the circulatory system: 1.58 Diseases of the respiratory system: 2.92 Diseases of the digestive system: 2.43 Diseases of the genitourinary system: 1.66 Diseases of the skin: 5.16 Diseases of the musculoskeletal system: 1.88 Conditions originating in the perinatal period: 1.14 Injury and poisoning: 2.79 |
13/22 |
| Kendall (2016, Harm Reduct J) (43) |
|
ED visits, Hospitalisation for people who use drugs |
|
Risk ratio for Gr 1 to have ≥ 2 ED visits (95% CI) Risk ratio for Gr 1 to have ≥ 1 hospitalisation (95% CI) |
1.58 (0.98-2.55) 2.39 (95% CI 1.38-4.13) |
19/22 |
| Khan (2008, Crit Care Med) (119) |
|
Critical diseases Hospitalisation, ICU admissions |
|
Median hospital length of stay (days) ICU median length of stay (days) ICU mortality, % (95% CI) Adjusted OR for hospital mortality (95% CI) |
Gr 1: 16; Gr 2: 16 Gr 1: 5.7; Gr 2: 8.3 Gr 1: 22.2 (17.4-27.0); Gr 2: 19.0 (18.0-20.1) Gr 1: 1.24 (1.21-1.29) |
19/22 |
| Kliewer (2002, CCM and Manitoba Health) (44) |
|
Hospitalisation |
|
Age-standardised hospitalisation rates/1000 | Gr 1, males: 293.4; Gr 1, females: 454.2 Gr 2, males: 228.6; Gr 2, females: 301.9 |
15/22 |
| Lafond (2016, J Eval Clin Pract) (104) |
|
ED visits, Hospitalisation |
|
Emergency department admissions Adjusted mean length of stay (days) (p=0.064) Delay in discharge for Gr 1 |
Gr 1: 82.8%; Gr 2: 92.5% Gr 1: 12.01; Gr 2: 9.05 17.7% (Delays were related to transportation, bed availability, lack of medical equipment in the community and lack of family support) |
20/22 |
| Laupland (2006, J Crit Care) (45) |
|
Critical illnesses ICU admission |
|
Annual incidence of critical illness/100,000 Annual incidence of critical illness rate ratio (95% CI; p) Odds ratio for in-hospital death for Status-Aboriginals (95% CI; p) Median ICU length of stay (p = 0.9) Overall median length of hospital stay (p <0.1) |
Gr 1: 620.6; Gr 2: 302.6 2.1 (1.78-2.35; p < 0.001) 1.40 (0.88-2.23; p = 0.15) Gr 1: 1.8 days; Gr 2: 1.9 days Gr 1: 9 days; Gr 2: 11 days |
16/22 |
| Martens (2005, C J Public Health) (46) |
|
Hospitalisation |
|
Overall hospitalisation rate per person (p <0.05) Premature mortality rate/1000 (p<0.05) Overall hospital days of care per person (p<0.05) |
Gr 1: 0.35; Gr 2: 0.16 Gr 1: 6.61; Gr 2: 3.30 Gr 1: 1.75; Gr 2: 1.05 |
15/22 |
| Martens (2010, MCHP) (47) |
|
Hospitalisation |
|
Total mortality rates/1000 Premature mortality rates/1000 Hospital separation rates/1000 |
Gr 1: 9.7; Gr 2: 8.4 (RR for Gr 1 = 1.15) Gr 1: 4.0; Gr 2: 3.3 (RR for Gr 1 = 1.21) Gr 1: 194; Gr 2: 154 |
16/22 |
| Rivers (2013, J Adolescent Health) (19) |
|
Health care access |
|
Perception of health care Access to health care |
Most youth had positive experiences with nurses and doctors. They preferred immediate access services (emergency room, clinics). Most youth avoided care until their problem couldn’t be ignored. Marginalised young men were more likely to have accessed emergency room. |
13/22 |
| Shah (2003, Am J Public Health) (48) |
|
Hospital admissions for ambulatory care-sensitive conditions (ACSC) |
|
Risk ratio for admission for ACSC Risk ratio for utilisation of specialist procedures Risk ratio for utilisation of acute care for insensitive conditions |
Gr 1: 2.54 (p <0.001) Gr 1: 0.64 (p <0.001) Gr 1: 1.39 (p <0.001) |
14/22 |
| Stergiopoulos (2016, Psychiatr Serv) (26) |
|
ED visits |
|
Unmet need for health care Adjusted RR for ED visits for Gr 1 (95% CI; p) Adjusted RR for hospital days for Gr 1 (95% CI; p) |
Gr 1: 52%; Gr 2: 50%; Gr 3: 32% 0.85 (0.71-1.01; p = 0.07) 0.91 (0.64-1.29; 0.60) |
14/22 |
| Waldram (1991, Artic Med Res) (27) |
|
ED visits |
|
Time from onset of symptoms to contact with a physician (not statistically significant) % of patients who visited an ED in the past year (not statistically significant) |
Gr 1: 3.8 days Gr 2 5.0 days Gr 1: 51% Gr 2: 47.6% |
11/22 |
| Wen (1996, Ethnic Health) (100) |
|
ED visits |
|
% of people who had an ED visits in the past year Odds ratio for Gr 1 to visit the ED (95% CI) |
Gr 1: 32.2%; Gr 2: 22.6% 1.39 (1.00-1.94) |
17/22 |
| CARDIOVASCULAR DISEASES (n = 9) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Atzema (2015, PLoS One) (74) |
|
ACS, CHF, AF, Stroke, HTN Hospitalisation, ED visits |
|
Age and sex-adjusted rate ratios of one-year disease-specific hospitalisations for Gr 1 (95% CI; p) Age and sex-adjusted all-cause mortality/100 in the year after diagnosis Gr 1/Gr 2 (95% CI) Age and sex-adjusted cardiovascular mortality in the year after diagnosis/100 Gr 1/Gr 2 (95% CI) Frequency of beta-blocker use within 3 months after ACS diagnosis (95% CI) Frequency of outpatient echocardiogram within 6 months after AF diagnosis (95% CI) Rate ratio for ED visits for Gr 1 in the year after diagnosis (95% CI) |
ACS: 1.23 (0.95-1.61; p = 0.12) CHF: 1.93 (1.34-2.78; p <0.001) Stroke: 1.03 (0.54-1.98; p= 0.93) AF: 1.23 (0.73-2.08; p = 0.44) HTN: 2.27 (1.88-2.74; p <0.001) ACS: 11.5 (5.7-17.2)/ 16.2 (16.1-16.4) CHF: 25.2 (13.1-37.3)/ 22.80 (22.5-23.1) Stroke: 20.7 (13.0-28.5)/ 14.8 (14.6-15.0) AF: 16.6 (7.3-25.4)/ 7.8 (7.4-8.1) HTN: 1.8 (0.89-2.6)/ 1.3 (1.2-1.3) ACS: 9.8 (4.7-14.8)/ 11.4 (11.3-11.6) CHF: 13.0 (6.5-19.5)/ 9.3 (9.1-9.5) Stroke: 25.4 (13.4-37.3)/ 21.8 (21.4-22.1) AF: 10.0 (2.4-17.7)/ 4.8 (4.6-5.0) HTN: 0.82 (0.24-1.4)/ 0.54 (0.52-0.56) Gr 1: 77.8% (67.8-85.9); Gr 2: 66.9% (66.6-67.3) Gr 1: 52.9% (38.5-67.1); Gr 2: 42.1% (41.5-42.6) CHF: 2.03 (1.47-2.80) HTN: 1.51 (0.95-2.40) |
19/22 |
| Bresee (2014, CMAJ) (118) |
|
AMI Coronary angiography, PCI, CABG |
|
Adjusted odds ratio of coronary angiography within 1 day after AMI (95% CI) Adjusted hazard ratios for likelihood of PCI after coronary angiography (95% CI) Adjusted hazard ratios for likelihood of CABG after coronary angiography (95% CI) Adjusted hazard ratios for all-cause mortality for Gr 1 after coronary angiography (95% CI) |
Gr 1: 0.73 (0.62-0.87) Gr 1: 0.92 (0.83-1.02) Gr 1: 1.03 (0.85-1.25) Medical management: 1.38 (1.07-1.77) PCI: 1.38 (1.06-1.80); CABG: 0.91 (0.56-1.47) |
19/22 |
| King (2009, Am J Cardiol) (25) |
|
AMI ED visits, PCI, CABG |
|
Time to ED presentation (hours): Gr 1/ Gr 2 (p=0.015) % of patients who saw provider ≤ 72h to ED presentation (p=0.002) Accompanying person fluent in English Time from ED presentation to cardiac catheterisation: Gr 1/Gr 2 (p = 0.001) % of patients who had PCI (p <0.001) % of patients who had CABG (p=0.022) |
<1h: 23%/20%; 1-2 h: 26%/25%; 3-6 h: 11%/27%; 7-12h: 5.7%/1.8%; 13-24h: 34%/27% Gr 1: 21%; Gr 2: 12% Gr 1: 100%; Gr 2: 93% (p=0.940) <3h: 18%/42%; 3-6h: 7.7%/5.1%; 6-24h: 0.0%/9.4%; >24h: 46%/27%; Not done: 28%/16% Gr 1: 62%; Gr 2: 63% Gr 1: 2.6%; Gr 2: 6.0% |
15/22 |
| Lyons (2013, Can J of Cardiol) (70) |
|
Heart failure Hospitalisation, ED visits |
|
Odds ratio of death for Gr 1 (95% CI) Hospitalisations per patient in the year after hospitalisation for HF Gr 1/Gr 2 ED visits per patient in the year after hospitalisation for HF Gr 1/Gr 2 |
1 year: 1.18 (1.02-1.38); 3 years: 1.43 (1.22-1.66); 5 years: 1.39 (1.16-1.67) All causes: 1.68/1.03 (p <0.0001) HF related: 0.21/0.14 (p = 0.004) All causes: 4.95/2.30 (p <0.0001) HF related: 0.32/0.19 (p = 0.0003) |
10/22 |
| Rosychuk (2016, BMC Emerg Med) (30) |
|
AF and flutter ED visits |
|
ED visits Time for specialist follow-up visits |
“First Nations seniors also had approximately three times as many ED presentations as would have been expected by the population proportion”. Gr 1 <65 y.o.: 103 days; Gr 1 >65 y.o.: 182 days |
16/22 |
| Shavadia (2020, Can J of Cardiol) (117) |
|
ACS Hospitalisation |
|
In-hospital mortality (95% CI) | OR = 1.88 (0.63-4.8) | 8/11 |
| Shultz (2018, Can J of Cardiol) (71) |
|
AMI, CHF, IHD, Stroke Hospitalisation, PCI, CABG |
|
AMI group Hazard ratio for mortality for Gr 1 (95% CI) Hazard ratio for hospitalisations for Gr 1 (95% CI) Hazard ratio of revascularization following coronary angiogram for Gr 1 (95% CI) Non-AMI group Hazard ratio for mortality for Gr 1 (95% CI) Hazard ratio for hospitalisations for First Nations (95% CI) Hazard ratio of revascularization following coronary angiogram for Gr 1 (95% CI) |
All-cause: 1.30 (0.96-1.75); Cardiovascular: 1.57 (1.05-2.35) All-causes: 1.35 (1.17-1.55); AMI: 1.30 (0.92-1.85); CHF: 1.54 (1.06-2.24); IHD: 1.46 (1.20-1.78); Stroke: 0.71 (0.33-1.52) PCI: 0.88 (0.75-1.02) CABG: 1.19 (0.94-1.49) All-cause: 1.52 (1.28-1.79); Cardiovascular: 1.50 (1.17-1.94) All-cause: 1.40 (1.29-1.51); AMI: 2.26 (1.79-2.85); CHF: 1.71 (1.38-2.12); IHD: 1.33 (1.17-1.50); Stroke: 1.47 (1.05-2.06) PCI: 0.85 (0.73-0.99) CABG: 1.26 (1.10-1.45) |
19/22 |
| Wei-Randall (2013, Health Rep) (72) |
|
AMI Hospitalisation, PCI, CABG, Coronary angiogram |
|
Age-standardised hospitalised AMI events rates Age-standardised % of patients who had a coronary angiogram (95% CI) Age-standardised % of patients who had revascularization (95% CI) Age-standardised % of patients who had PCI (95% CI) Age-standardised % of patients who had CABG (95% CI) |
Gr 1: 276.8/100,000; Gr 2: 157.1/100,000 (p <0.05) Gr 1: 51.1% (49.9-52.3); Gr 2: 58.1% (57.9-58.3) Gr 1: 39.6% (38.5-40.7); Gr 2: 46.8% (46.6-47.0) Gr 1: 30.7% (29.6-31.8); Gr 2: 38.1% (37.9-38.3) Gr 1: 9.3% (8.6-10.0); Gr 2: 9.2% (9.1-9.3%) |
15/22 |
| Young (1993, Am J Public Health) (73) |
|
Cardiovascular diseases Hospitalisation |
|
Age-standardised mortality rates/100,000 for diseases of the circulatory system (men/women) Hospitalisation rates/100,000 for diseases of the circulatory system Male/Female |
Gr 1: 195/187; Gr 2: 205/149; Gr 3: 349/198 Keewatin Region (90% Inuit): 438/404; Northwest Territory: 891/640; All Canada: 1914/1472 |
15/22 |
ACS: Acute coronary syndrome, CHF: Congestive heart failure, AF: Atrial fibrillation, HTN: Hypertension, AMI: Acute myocardial infarction, PCI: Percutaneous coronary intervention, CABG: Coronary artery bypass grafting, IHD: Ischaemic heart disease
| PSYCHIATRIC DISEASES (n = 8) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Carriere (2018, Statistics Canada) (82) |
|
Mental disorders Hospitalisation |
|
Rate ratios for age-standardised hospitalisation rates/100,000 (95% CI) | Total: Gr 1: 2.4 (2.3-2.5); Gr 2: 2.0 (1.9-2.1) Substance-related: Gr 1: 7.0 (6.6-7.4); Gr 2: 4.3 (3.8-4.8) Mood: Gr 1: 1.2 (1.1-1.3); Gr 2: 1.6 (1.4-1.8) Schizophrenic/Psychotic: Gr 1: 1.8 (1.6-2.0); Gr 2: 1.9 (1.6-2.2) Anxiety: Gr 1: 2.3 (2.0-2.7); Gr 2: 1.7 (1.3-2.3) Organic: Gr 1: 1.1 (0.9-1.3); Gr 2: 1.0 (0.7-1.3) Personality: Gr 1: 1.2 (0.9-1.5); Gr 2: 1.3 (0.9-2.1) Other: Gr 1: 1.7 (1.6-1.9); Gr 2: 1.5 (1.3-1.8) |
15/22 |
| D’Arcy (1979, Can J Psychiat) (83) |
|
Mental illnesses Hospitalisation |
|
Admissions per 10,000 population Gr 1/Gr 2 |
Total: 41/36; Psychoses: 16/19; Psychoneuroses: 12/7; Personality/Behaviour: 9/6; Mental Retardation: 1/0; Other/Unknown: 3/4 | 6/22 |
| Dalrymple (1995, Can J Psychiat) (14) |
|
Mental illnesses Hospitalisation |
|
Consumer satisfaction survey (% Gr 1/% Gr 2) Length of stay in 1991-1992 (days) |
Schizophrenia and other psychoses: 31.5%/37.8%; Mood disorders: 15.7%/21.3%; Substance abuse disorders: 0%/3.8%; Anxiety, Adjustment, Conduct and personality disorders: 0%/2.9%; Other disorders: 42.1%/33.9% Gr 1: 69.5; Gr 2: 32.8 |
14/22 |
| Lavoie (2018, Int J Equity Health) (84) |
|
Mental health related-ambulatory care sensitive conditions Hospitalisation |
|
Access to care Hospitalisation rate for mental health conditions Length of stay |
First Nation communities served by nursing station have the lowest rate of hospitalisation. Communities served by health centres have highest rate of hospitalisation (poorer access to care). First Nations living off-reserve had significantly higher hospitalisation rates People in Gr 2 stay 4-6 days longer than Gr 1 in the hospital. |
17/22 |
| Lavoie (2020, Can J of Pub Health) (32) |
|
Mental illnesses Hospitalisation |
|
Hospitalisation rates/1000 (95% CI; p) Adjusted rate of length of stay |
Gr 1: 26.00 (17.59-38.42; p < 0.0001) Gr 2: 12.55 (12.34-12.75; p = 0.8596) Gr 1: 9.79 (7.08-13.52; p = 0.0466) Gr 2: 23.68 (23.60-23.76; p=0.5596) |
17/22 |
| Newton (2012, CMAJ) (103) |
|
Mental health crisis ED visits |
|
Median length of stay in hours (95% CI) Age and sex-adjusted standardised visit rate/100,000 for Gr 1 (p = 0.004) Age and sex-adjusted standardised visit rate/ 100,000 for Gr 1 of 15-17 y.o. Hazard ratio for time to physician follow-up visit for Gr 1 (95% CI) |
Gr 1: 2h27 (1h05-5h40); Gr 2: 3h (1h30-5h21) 2002-2003: 1368.0 2007-2008: 1664.0 Females: 7047.6 Males: 5787.3 Psychiatrist: 0.47 (0.32-0.70) |
16/22 |
| Newton (2016, Pediatr emerg care) (107) |
|
Anxiety and stress disorders ED visits |
|
ED visit rates/100,000 (95% CI) Follow-up visits |
2002-2003: Gr 1: 263.49 (218.43-308.55); Gr 2: 126.87 (119.16-134.57) 2010-2011: Gr 1: 345.59 (294.18-397.00); Gr 2: 168.95 (160.51-177.39) Gr 1 children had less follow-up visits after discharge. Median time to follow-up visits = 32 days. |
17/22 |
| Soleimani (2016, BMC Psychiatry) (85) |
|
Psychotic symptoms Hospitalisation |
|
Hazard ratio for inpatient hospitalisation within 90 days of first ED visit (95% CI) | Gr 1 females: 4.18 (1.24-14.06) Gr 1 males: 0.57 (0.13-2.49) |
17/22 |
| PERCEPTION OF HEALTH CARE (n = 6) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Baker (2000, Western J Nurs Res) (15) |
|
Satisfaction of cross-cultural hospital care |
|
Patient satisfaction |
Mi’kMaq appreciated when their family were allowed to visit them and when they felt they received the same treatment as anybody else. They also appreciated when caregivers were kind. |
23/32 |
| Cameron (2014, Adv Nurs Sci) (16) |
|
Inequalities in access to health care Emergency care services |
|
Satisfaction of health care Barriers in access to care Access to care % of people who did not receive needed health care in the past year |
Participants reported stories of racism, stigmatisation, language difficulties, intimidation, harassment and fear. They felt that professionals did not always take time to explain things properly or to assess participant’s needs and concerns. Limited access to comprehensive and specialised care, long waiting time, barriers in the communication and understanding of medical jargon, barriers in the interaction with professionals. 35% of Gr 1 felt that their access to health care was worst than Gr 2. Gr 1: 18% Gr 2: 12% |
24/32 |
| Goodman (2017, Soc Sci Med) (17) |
|
ED visits, Hospital visits |
|
Satisfaction of health care | They feel they are treated differently than other patients. Some are scared to go to the hospital. Several reported only seeking healthcare once their illness or symptoms had become severe. The security or staff of the hospital often threatens them. Hospital policies exacerbate cultural barriers. There is facility devoted space for Indigenous, but Indigenous don’t know it exist and when they looked for it, it was not accessible. Presence of stereotypes associating Indigenous to substance use. Because of that, requests for pain medication are often perceived as drug seeking. Health care professionals care more about proving the patient took drug than providing medical care. Lack of empathy, Incompetent addiction medicine training. |
20/32 |
| Hole (2015, Qual Health Res) (18) |
|
Health care at a community hospital |
|
Things appreciated in health care Bad perceptions of health care |
Being recognised as Indigenous, heard and respected. People with lower income wait longer in the waiting room. Professionals think that Indigenous are drunk and treat Indigenous differently than others. It’s hard for the staff to give good care when they are short-staffed and exhausted. It’s when the staff is stressed that all the bad commentaries tend to come out. Hospital rules exclude Indigenous realities. Indigenous staff is not allowed to speak up about the problems. Professionals are too concentrated in having access to the patient to do medical procedures rather than letting the patient have family support. The professionals sometimes hide information from the family. Professionals have access to a lot of pain reliever medication, but they don’t want to give them because they are afraid that the patient will get addicted. |
18/32 |
| Tang (2008, Ethnic Health) (20) |
|
ED visits, hospital visits |
|
Patients’ satisfaction Health care professionals’ perceptions |
Health care professionals often think that the cause of the symptoms is alcohol even when the patient claims he did not drink. Some Indigenous get kicked out of the ED because the security thinks they are drunk or that they aren’t really sick. A lot of Indigenous won’t go to the hospitals unless they are almost dying. Some feel they have to wait longer for getting health care professional’s attention towards an important health problem. Believe they provide the same quality of care to any patients. There is no judgment towards patients of First Nation status. Some professionals think you can give them the best care in the world and they will not be able to access it because they can’t or they do not want to. One ED professional recognised that sometimes health care professionals tend to generalise that all Indigenous have a drinking problem and have a low social economic background. Another said he is more guarded with an Indigenous patient. |
20/32 |
| Tang (2015, Sociol Health Illn) (21) |
|
ED visits |
|
Health care providers opinions towards indigenous people: Indigenous people perception towards health care providers: |
Indigenous have addictions and they present physical signs of their addiction. Many are on welfare and don’t have a job nor take care of themselves. They want to be seen as needy people. They misuse the money from tax payers. Some Indigenous just come to the hospital to have food and drugs. There are other population groups which misuse the health care system and have poverty issues but the stigma is not the same as with Indigenous. When all their requests are not met, they become frustrated and it’s hard to remain compassionate and non-judgemental when those behaviours are seen. Providers always think that you’re a drug addict or a drunk. Sometimes, Indigenous are getting escorted out of the hospital because the staff think they are here just to get drugs or to get free food. |
21/32 |
a All the information from this table comes from the articles directly, it does not represent our opinion
| RHEUMATOLOGIC DISEASES (n = 5) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Barnabe (2016, J Rheumatol) (38) |
|
RA, AS, PsD Hospitalisation |
|
Hospitalised infection rates/1000 for Gr 1 | RA: 29.7; AS: 19.8; PsD: 22.4 | 5/11 |
| Barnabe (2016, J Rheumatol) (126) |
|
RA Hospitalisation ED visits |
|
Cost estimates for Gr 1 patients (95% CI) | Hospital: −5406$ (−11,552 – 470) Emergency room: 660$ (−38 – 1357) |
6/11 |
| Barnabe (2017, Arthrit Care Res) (80) |
|
RA, AS, PsD, CRA Hospitalisation |
|
Crude all-cause hospitalisation rates/100 (95% CI) Arthritis-specific hospitalisation/100 (95% CI) |
RA: Gr 1: 38.9 (38.2-39.7); Gr 2: 25.1 (24.9-25.3) AS: Gr 1: 37.5 (35.8-39.2); Gr 2: 20.2 (19.9-20.6) PsD: Gr 1: 36.8 (34.1-39.7); Gr 2: 17.9 (17.6-18.3) Crystal-related arthritis: Gr 1: 34.1 (32.5-35.7); Gr 2: 23.9 (23.7-24.1) RA: Gr 1: 2.3 (2.1-2.5); Gr 2: 3.4 (3.3-3.4) AS: Gr 1: 1.0 (0.7-1.3); Gr 2: 1.3 (1.2-1.4) PsD: Gr 1: 1.7 (1.2-2.4); Gr 2: 1.4 (1.3-1.5) CRA: Gr 1: 1.6 (1.2-1.9); Gr 2: 1.6 (1.6-1.7) |
17/22 |
| Levy (2013, Arthritis Rheum) (102) |
|
Childhood-onset SLE Hospitalisation ED visits |
|
Distribution of patients ED visit in the first year of diagnosis % of patients hospitalised % of patients who required at least 3 hospitalisations |
Gr 1: 1.3%; Gr 2: 42% Whites; Gr 3: 24%; Gr 4: 15%; Gr 5: 13% 43% 38% 12% |
10/11 |
| Oppenheimer (2007, South med J) (28) |
|
Blastomycosis of bones and joints Hospitalisation, ICU admission |
|
Time from first symptoms to admission (days) Time from admission to diagnosis (days) Duration of hospital stay (days) % of death |
Gr 1: 31 ± 30; Gr 2: 95 ± 150 Gr 1: 10 ± 30; Gr 2: 15 ± 30 Gr 1: 30 ± 20; Gr 2: 22 ± 30 Gr 1: 8%; Gr 2: 3% |
15/22 |
RA: Rheumatoid arthritis, AS: Ankylosis spondylitis, PsD: Psoriatic disease, CRA: Crystal-related arthritis, SLE: Systemic lupus erythematous
| NEUROLOGICAL DISEASES (n = 5) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Ahmed (2020, Can J of Surg) (121) |
|
Traumatic spinal cord injury Hospitalisation |
|
Time from admission to surgery, h, median (p=0.20) Proportion of surgical management (%) |
Gr 1: 20.0 Gr 2: 15.0 Gr 1: 71% Gr 2: 85% |
16/22 |
| Blackmer (1999, Brain injury) (122) |
|
Traumatic brain injury Hospitalisation |
|
Acute care length of stay (days) Time to follow-up (days) (p <0.0001) |
Gr 1: 33.33; Gr 2: 35.23 (p = 0.734) Gr 1: 56.50; Gr 2: 28.10 |
15/22 |
| Jetté (2008, Epilepsia) (78) |
|
Epilepsy Hospitalisation, ED visits |
|
Odds ratio for hospitalisation (95% CI) Odds ratio for ED visits (95% CI) Mean hospital length of stay |
Gr 1: 2.8 (1.49-5.13) Gr 1: 2.3 (1.09-4.98) 2 ± 12 days |
16/22 |
| Kapral (2020, CMAJ Open) (75) |
|
Stroke or transient ischaemic attack Hospitalisation |
|
Rate of hospital admission per 100,000 (95% CI) % of mortality at 7 days (95% CI) % of mortality at 1 year (95% CI) % of patients with neuroimaging (95% CI) % of thrombolysis (95% CI) % of carotid revascularization (95% CI) |
Gr 1: 641.2 (539.8-756.2); Gr 2: 540.2 (527.6-552.9) Gr 1: 12.0 (8.9-15.9); Gr 2: 8.5 (8.0-9.0) Gr 1: 33.8 (28.2-40.2); Gr 2: 28.1 (27.1-29.1) Gr 1: 94.6 (85.9-100.0); Gr 2: 96.0 (94.2-97.9) Gr 1: 6.3 (3.9-9.7); Gr 2: 11.0 (10.3-11.7) Gr 1: 1.4 (0.5-3.0); Gr 2: 2.7 (2.4-3.0) |
20/22 |
| Lasry (2016, Can J Neurol Sci) (79) |
|
Traumatic brain injury Hospitalisation |
|
Rate ratios for hospitalisation (95% CI) | Gr 1: 1.86 (1.56-2.17) | 4/11 |
| ENDOCRINE-RELATED CONDITIONS (n = 5) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Booth (2005, Diabetes Care) (88) |
|
Complications of diabetes ED visits, Hospitalisation |
|
Risk ratio for ED visits or hospital admission for diabetes for Indigenous | 1.8 | 17/22 |
| Campbell (2014, Diabetol Metab Syndr) (89) |
|
Complications of diabetes, Hospitalisation |
|
Adjusted odds ratio for hospitalisation for Gr 1 (95% CI) | 30 y.o.: 3.94 (3.11-4.99) 55 y.o.: 4.75 (3.24-6.97) 80 y.o.: 5.74 (3.36-9.80) |
15/22 |
| Pohar (2007, BMC health serv res) (91) |
|
Diabetic patients Hospitalisation |
|
Odds ratio for hospitalisation for diabetic patients (p <0.05) Age-standardised per capita health care cost for Gr 1 (95% CI) Age-standardised per capita health care cost for Gr 2 (95% CI) |
Gr 1: 2.2; Gr 2: 2.1 Without diabetes: 1 395$ (1 394-1 397) With diabetes: 3 204$ (3 201-3 206) Without diabetes: 875$ (875-875) With diabetes: 2 257$ (2 256- 2 258) |
16/22 |
| Rose (2008, Foot Ankle Surg) (90) |
|
Diabetic ulcers, Hospitalisation |
|
% of patients with amputation Gr 1/Gr 2 |
Toe only: 39%/ 53% Forefoot: 13%/ 7% Below knee: 45%/ 33% Above knee: 3%/ 7% |
17/22 |
| Shah (2020, CMAJ Open) (101) |
|
Diabetes complications Hospitalisation, ED visits |
|
% admitted to hospital for ambulatory-care-sensitive-conditions Emergency department visits for hypo- or hyperglycaemia (%) |
Gr 1: 2.5 (2.1-2.9) Gr 2: 2.4 (2.1-2.7) Gr 3: 1.2 (1.2-1.2) Gr 1: 1.1 (0.9-1.3) Gr 2: 1.8 (1.5-2.0) Gr 3: 0.8 (0.8-0.9) |
18/22 |
| PAEDIATRIC-RELATED DISEASES (n = 5) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| He (2017, CMAJ) (87) |
|
Hospitalisation |
|
Adjusted rate ratios for infant hospitalisation (95% CI) | Any cause: Gr 1: 1.43 (1.37-1.50); Gr 2: 1.37 (1.24-1.52) Infections: Gr 1: 1.66 (1.54-1.78); Gr 2: 1.31 (1.10-1.57) Injuries/accidents: Gr 1: 1.16 (0.97-1.39); Gr 2: 1.36 (0.86-2.15) Congenital anomalies: Gr 1: 1.35 (1.15-1.59); Gr 2: 1.40 (1.01-1.95) Perinatal-originated conditions: Gr 1: 0.95 (0.75-1.19); Gr 2: 0.92 (0.58-1.45) Respiratory system: First Nations: 1.91 (1.80-2.03) Inuit: 1.82 (1.59-2.08) Digestive system: Gr 1: 1.49 (1.31-1.69); Gr 2: 1.01 (0.73-1.39) Nervous system: Gr 1: 1.64 (1.43-1.89); Gr 2: 1.64 (1.20-2.25) Genitourinary system: Gr 1: 1.75 (1.45-2.11); Gr 2: 0.61 (0.32-1.16) Musculoskeletal system: Gr 1: 1.34 (0.60-2.98) Circulatory system: Gr 1: 1.50 (0.86-2.61) Endocrine system: Gr 1: 1.49 (1.29-1.73); Gr 2: 2.61 (1.50-4.53) Skin and subcutaneous tissue: Gr 1: 3.00 (2.58-3.49); Gr 2: 2.86 (1.57-5.23) Blood: Gr 1: 0.96 (0.57-1.60) Mental/neurodevelopmental disorders: Gr 1: 1.20 (0.50-2.95) Neoplasms: Gr 1: 0.91 (0.50-1.71) |
18/22 |
| Reime (2007, Paediatr Perinat Epidemiol) (24) |
|
ICU admissions |
|
No access to prenatal care Mortality (p <0.001) Adjusted odds ratio for Gr 1 for specific treatments (95% CI) Length of stay (days) (p<0.05) |
Gr 1: 7.2%; Gr 2: 1.6% Gr 1: 7.1%; Gr 2: 7.4% Transparenteral nutrition: 0.77 (0.60-1.00) Blood transfusion 1.07 (0.78-1.46) Surfactant 0.78 (0.57-1.06) Assisted ventilation 0.86 (0.67-1.09) Surgery 0.73 (0.54-0.99) Antenatal steroids 1.04 (0.81-1.34) Incubator 0.85 (0.65-1.12) Gr 1: 4.5 days; Gr 2: 2.9 days |
19/22 |
| Stammers (2014, Pediatr Blood Cancer) (81) |
|
Cancer complications Hospitalisation |
|
Risk ratios for hospital admission days for treatment complications for Gr 1 (95% CI; p) | Low risk: 0.853 (0.27-1.55; p= 0.371) Intermediate/High risk: 1.140 (0.52-2.48; p=0.748) |
18/22 |
| Thanh (2015, J Pediatr) (125) |
|
Health care utilisation for low birth-weight population |
|
Health services use cost coefficient | Gr 1: 1560 (1359-1762; p <0.001) | 18/22 |
| Thomson (1994, Can Fam Physician) (86) |
|
Acute otitis media Hospitalisation |
|
Hospitalisation rates/100 for otitis media (Gr 1/Gr 2) Relative risk of hospitalisations for otitis media for Gr 1 (95% CI) Hospitalisation rates/100 for upper respiratory tract infection (Gr 1/Gr 2) Relative risk of hospitalisation for upper respiratory infection for Gr 1 (95% CI) |
Boys 1-4 y.o.: 6.7/1.1; Girls 1-4 y.o.: 5.6/0.8 0-1 y.o.: 2.1/0.3 Boys 1-4 y.o.: 6.1 (5.1-7.3); Girls 1-4 y.o.: 6.7 (5.4-8.2) 0-1 y.o.: 6.1 (0.6-67.0) Boys 1-4 y.o.: 24.7/5.2; Girls 1-4 y.o.: 22.9/3.8 Saskatchewan’s boys 0-1 y.o.: 27.1/4.8 Saskatchewan’s girls 0-1 y.o.: 27.4/3.1 Ontario’s 0-1 y.o.: 5.2/0.7 Boys 1-4 y.o.: 4.7 (4.3-5.1); Girls 1-4 y.o.: 6.1 (5.6-6.7) Saskatchewan’s boys 0-1 y.o.: 5.7 (4.8-6.7) Saskatchewan’s girls 0-1 y.o.: 8.9 (7.4-10.6) Ontario’s 0-1 y.o.: 7.7 (1.5-38.9) |
12/22 |
| GASTROINTESTINAL DISEASES (n = 4) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Beres (2010, J Pediatr Surg) (123) |
|
Appendicitis Hospitalisation, Surgery |
|
Type of appendectomy (%) (p=0.02) Length of stay (days) (p = 0.98) Intervals between arrival and operating room Mean operative time |
Laparoscopic: Gr 1: 57%; Gr 2: 73% Open: Gr 1: 43%; Gr 2: 27% Gr 1: 2.9 ± 2.0; Gr 2: 2.9 ± 3.0 Gr 1: 10.3h; Gr 2: 7.0h (p = 0.0002) Gr 1: 49.0 ± 20.2 min; Gr 2: 54.5 ± 17.6 min |
15/22 |
| Carey (1977, Can Assoc Radiol J) (124) |
|
Lead shot appendicitis Hospitalisation |
|
Type of treatment | CASE 1: Rectal suppositories to clear the lead shot (no effect). Sigmoidoscopy to evacuate the lead shot (no success). Laparotomy to remove the appendix, 3 lead shots, to mobilise lead shots through the rectum. 2 weeks after the surgery, enemas, purgatives and repeated sigmoidoscopy were done to dislodge the lead shots still present (no success). Another surgery was done to remove the rest of the lead shots. CASE 2: Catheterisation of bladder (wrong diagnosis of urinary retention). Sigmoidoscopy (no success). Barium examination of the colon. Open appendicectomy for peritonitis. |
7/13 |
| Cohen (1989, Am J Public Health) (120) |
|
Gall bladder diseases Hospitalisation, Surgery |
F/M |
% of patients who received their operation from a general practitioner | Gr 1: 34.2%; Gr 2: 18% | 14/22 |
| Harper (2015, Int J Circumpol Heal) (29) |
|
Acute gastrointestinal illness Primary care visits |
|
% of patients who visited clinic or hospital (95% CI) Reasons for not seeking care Rigolet/Iqaluit |
Rigolet: 4.8% (1.5-14.4) Iqaluit: 16.9% (11.2-24.7) Illness not serious enough: 82%/50%; Would not make a difference: 2%/10%; Dislikes or distrusts doctors or nurses: 2%/3%; On the land: 5%/1%; Language barriers: 0%/0% |
16/22 |
| INFECTIOLOGY-RELATED DISEASES (n = 4) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Dallaire (2006, C J Public Health) (39) |
|
Acute infections Hospitalisation |
|
Hospitalisation rates/1000 for Inuit (95% CI) 0-11 months old/12-23 months old/2-4 y.o. |
Pneumonia: 198 (145-251)/ 119 (77-160)/ 30 (17-44) Bronchitis/Bronchiolitis: 107 (68-147)/ 23 (5-40)/ 5 (0-10) Upper respiratory tract infections: 28 (8-49)/ 0/ 1 (−1 – 3) Urinary tract infections (female): 17 (−2 – 36)/ 33 (7-60)/ 2 (−2 – 6) Urinary tract infections (male): 18 (−2 – 38)/ 121 (−11 – 35)/ 2 (−2 – 6) Fever NOS: 14 (2-27)/ 3 (−3 – 8)/ 1 (−1 – 3) Acute otitis media: 11 (0-22)/ 3 (−3 – 8)/ 1 (−1 – 3) Pyelonephritis/pyelitis (female): 11 (−6 – 27)/ 6 (−5 – 17)/ 6 (−1 – 12) Cellulitis: 9 (−1 – 18)/ 14 (−1 – 29)/ 8 (1-14) Meningitis: 9 (−1 – 18)/ 6 (−2 – 14)/ 1 (−1 – 3) Laryngitis/Tracheitis: 3 (−3 – 8)/ 9 (−1 – 18)/ 3 (0-6) |
17/22 |
| Landy (2010, Int J Infect Dis) (33) |
|
Gonococcal septic shock, ARDS and Multisystem organ failure Hospitalisation |
|
Time for transfer to tertiary care Type of treatment Length of stay |
13h (because of artic winter and distance) Fluid resuscitation, intubation and vasopressors prior to transfer. Empiric ceftriaxone and vancomycin were administered after blood cultures. Ethanol infusion was started then discontinued when the anion gap became normal. The patient improved with mechanical ventilation, vasopressor support, ceftriaxone, corticosteroids and supportive ICU care. 12 days in ICU, 2 days in general medicine |
7/13 |
| Mashru (2017, J Telemed Telecare) (13) |
|
Infectious diseases Hospitalisation |
|
Patient satisfaction towards telemedicine consultation | Patient understood how the session would run: 98% Help was available if there were problems: 100% Able to hear specialist comfortably: 98%; Satisfied with picture quality: 94%; Privacy was respected: 100%; Would use telemedicine again: 94%; Would recommend to family/friends: 92%; Overall satisfied with appointment: 98% |
15/22 |
| Nicolle (1996, Clin Infect Dis) (76) |
|
Acute pyelonephritis Hospitalisation |
|
Mean hospitalisation rates/10,000 Rate ratios for hospitalisation for Gr 1 patients (95% CI) |
Women: 9.01 ± 0.47; Men: 3.24 ± 0.27 First Nations women: 46.11 ± 4.86 First Nations men: 4.76 ± 1.59 Women: 5.12 (4.23-6.20) Men: 1.47 (0.85-2.53) |
14/22 |
| OBSTETRICAL AND GYNAECOLOGICAL CONDITIONS (n = 4) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Houd (2004, Int J of Circump Health) (110) |
|
Delivery Hospitalisation |
|
Perinatal death rate | 7/1000 | 12/22 |
| Lessard (1987, CMAJ) (111) |
|
Delivery Hospitalisation |
|
Stillbirth rate Medical intervention for nulliparous women Medical interventions for multiparous Primary caesarean sections rates |
9.7/1000 deliveries Induction: 6%; Augmentation: 4%; Analgesia: 17% Induction: 6%; Augmentation: 1%; Analgesia: 3% Nulliparous: 5.6%; Multiparous: 2.5% |
10/22 |
| Oluyomi-Obi (2010, Obstetrics) (112) |
|
H1N1 Influenza A and pregnancy Admission to ICU |
|
Admission to ICU Mortality Quality of care Median length of stay (days) |
6 patients 2 women and 1 baby 3/6 patients intubated ECMO 2/6 patients Emergency caesarian delivery: 3/6 20.5 |
19/22 |
| Van Wagner (2012, Birth) (113) |
|
Delivery Hospitalisation |
|
Mortality Active management of third stage |
1 maternal death, 4 foetal deaths (0.29%), 5 neonatal deaths (0.36%) 49.8% |
21/22 |
| NEPHROLOGICAL CONDITIONS (n = 1) | ||||||
|---|---|---|---|---|---|---|
| Author (year, journal) | Setting | Topic | Populations’ characteristics | Outcomes | Main results | STROBE |
| Molnar (2018, Can J Kidney Health Dis) (77) |
|
Complications in dialysis patients Hospitalisation |
|
Adjusted hazard ratio for all-cause hospitalisations (95% CI) Hazard ratio for infection-related hospitalisations (95% CI) |
Gr 1: 1.20 (1.12-1.28) Gr 1: 1.30 (1.11-1.53) |
18/22 |
References
- [1].Ministère de la santé et des services sociaux . Particularités des services aux Premières Nations et aux Inuits [Internet]. Santé et services sociaux Québec. 2016. [cited 2020 Mar 16]. Available from: https://www.msss.gouv.qc.ca/professionnels/soins-et-services/particularites-des-services-aux-communautes-autochtones [Google Scholar]
- [2].Agence de la santé publique du Canada . État de santé des canadiens 2016: rapport de l’administrateur en chef de la santé publique. Gouvernement du Canada. 2016.
- [3].Government of Canada; Indigenous and Northern Affairs Canada; Communications Branch . Indigenous peoples and communities [Internet]. Government of Canada; Indigenous and Northern Affairs Canada; Communications Branch. 2017. [cited 2021 May 23]. Available from: https://www.rcaanc-cirnac.gc.ca/eng/1100100013785/1529102490303 [Google Scholar]
- [4].Miller JR Residential Schools in Canada [Internet]. The Canadian Encyclopedia. 2020. [cited 2021 May 24]. Available from: https://www.thecanadianencyclopedia.ca/en/article/residential-schools [Google Scholar]
- [5].Menzies P Intergenerational Trauma and Residential Schools [Internet]. Intergenerational Trauma and Residential Schools | The Canadian Encyclopedia. 2020. [cited 2021 May 24]. Available from: https://www.thecanadianencyclopedia.ca/en/article/intergenerational-trauma-and-residential-schools [Google Scholar]
- [6].Adelson N. The Embodiment of Inequity: health Disparities in Aboriginal Canada. Can J Public Health. 2005;96(S2):S45–S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cooke M, Beavon D. Measuring the well-being of aboriginal people: an Application of the United Nations’ Human Development Index to Registered Indians in Canada, 1981-2001. Aboriginal policy research: setting the agenda for change. 2004;1.
- [8].Greenwood M, de Leeuw S, Lindsay N. Challenges in health equity for Indigenous peoples in Canada. Lancet. 2018;391(10131):1645–15. [DOI] [PubMed] [Google Scholar]
- [9].Hajizadeh M, Hu M, Bombay A, et al. Socioeconomic inequalities in health among Indigenous peoples living off-reserve in Canada: trends and determinants. Health Policy. 2018;122(8):854–865. [DOI] [PubMed] [Google Scholar]
- [10].von Elm E, Altman D, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. [DOI] [PubMed] [Google Scholar]
- [11].Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- [12].CARE Case Report Guidelines . 2021. CARE Checklist — CARE Case Report Guidelines. [online] Available at: [cited 2021 Feb 23]. <https://www.care-statement.org/checklist>
- [13].Mashru J, Kirlew M, Saginur R, et al. Management of infectious diseases in remote northwestern Ontario with telemedicine videoconference consultations. J Telemed Telecare. 2016;23(1):83–87. [DOI] [PubMed] [Google Scholar]
- [14].Dalrymple A, O’doherty J, Nietschei K. Comparative analysis of native admissions and registrations to Northwestern Ontario treatment facilities: hospital and community sectors. Can J Psychiatry. 1995;40(8):467–473. [DOI] [PubMed] [Google Scholar]
- [15].Baker C, Daigle M, Biro A, et al. Cross-Cultural Hospital Care as Experienced by Mi’kmaq Clients. West J Nurs Res. 2000;22(1):8–28. [Google Scholar]
- [16].Cameron B, Carmargo Plazas M, Salas A, et al. Understanding Inequalities in access to health care services for aboriginal people. Adv Nurs Sci. 2014;37(3):E1–E16. [DOI] [PubMed] [Google Scholar]
- [17].Goodman A, Fleming K, Markwick N, et al. “They treated me like crap and I know it was because I was Native”: the healthcare experiences of Aboriginal peoples living in Vancouver’s inner city. Soc Sci Med. 2017;178:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hole R, Evans M, Berg L, et al. Visibility and Voice. Qual Health Res. 2015;25(12):1662–1674. [DOI] [PubMed] [Google Scholar]
- [19].Rivers R, Saewyc E, MacKay L, et al. Masculinities and Marginalized Young Men’s Patterns of Accessing Health Care Services. J Adolesc Health. 2013;52(2):S21.23601608 [Google Scholar]
- [20].Tang S, Browne A. ‘Race’ matters: racialization and egalitarian discourses involving Aboriginal people in the Canadian health care context. Ethn Health. 2008;13(2):109–127. [DOI] [PubMed] [Google Scholar]
- [21].Tang S, Browne A, Mussell B, et al. ‘Underclassism’ and access to healthcare in urban centres. Sociol Health Illn. 2015;37(5):698–714. [DOI] [PubMed] [Google Scholar]
- [22].Marrie T, Carriere K, Jin Y, et al. Hospitalization for Community Acquired Pneumonia in Alberta First Nations Aboriginals Compared with Non-First Nations Albertans. Can Respir J. 2004;11(5):336–342. [DOI] [PubMed] [Google Scholar]
- [23].Morrison K, Buckeridge D, Xiao Y, et al. The impact of geographical location of residence on disease outcomes among Canadian First Nations populations during the 2009 influenza A(H1N1) pandemic. Health Place. 2014;26:53–59. [DOI] [PubMed] [Google Scholar]
- [24].Reime B, Tu AW, Lee SK. Treatment differences between Aboriginal and white infants admitted to Canadian neonatal intensive care units. Paediatr Perinat Epidemiol. 2007;21(6):532–540. [DOI] [PubMed] [Google Scholar]
- [25].King K, Khan N, Quan H. Ethnic variation in acute myocardial infarction presentation and access to care. Am J Cardiol. 2009;103(10):1368–1373. [DOI] [PubMed] [Google Scholar]
- [26].Stergiopoulos V, Gozdzik A, Nisenbaum R, et al. Racial-Ethnic differences in health service use in a large sample of homeless adults with mental illness from five Canadian cities. Psychiatric Serv. 2016;67(9):1004–1011. [DOI] [PubMed] [Google Scholar]
- [27].Waldram J Urban native health care in Canada: the relevance of socio-economic status. Arctic medical research. 1991;Suppl:34–36. [PubMed]
- [28].Oppenheimer M, Embil J, Black B, et al. Blastomycosis of Bones and Joints. South Med J. 2007;100(6):570–578. [DOI] [PubMed] [Google Scholar]
- [29].Harper S, Edge V, Ford J, et al. Healthcare use for acute gastrointestinal illness in two Inuit communities: rigolet and Iqaluit, Canada. Int J Circumpolar Health. 2015;74(1):26290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rosychuk R, Graham M, Holroyd B, et al. Emergency department presentations for atrial fibrillation and flutter in Alberta: a large population-based study. BMC Emerg Med. 2016;17(1). DOI: 10.1186/s12873-016-0113-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Firestone M, Smylie J, Maracle S, et al. Unmasking health determinants and health outcomes for urban First Nations using respondent-driven sampling. BMJ Open. 2014;4(7):e004978–e004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lavoie J, Phillips-Beck W, Kinew K, et al. Manitoba First Nation peoples’ use of hospital-based mental health services: trends and solutions. Can J Public Health. 2020; 112(2):231-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Landy J, Djogovic D, Sligl W. Gonococcal septic shock, acute respiratory distress syndrome, and multisystem organ failure: a case report. Inter J Infect Dis. 2010;14:e239–e241. [DOI] [PubMed] [Google Scholar]
- [34].Banerji A. High rates of hospitalisation for bronchiolitis in Inuit children on Baffin Island. Int J Circumpolar Health. 2001;60(3):375–379. [PubMed] [Google Scholar]
- [35].Banerji A, Bell A, Mills E, et al. Lower respiratory tract infections in Inuit infants on Baffin Island. Can Med Assoc J. 2001;164(13):1847–1850. [PMC free article] [PubMed] [Google Scholar]
- [36].Banerji A, Panzov V, Robinson J, et al. The cost of lower respiratory tract infections hospital admissions in the Canadian Arctic. Int J Circumpolar Health. 2013;72(1):21595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Creery D, Iyer P, Samson L, et al. Costs associated with infant bronchiolitis in the Baffin region of Nunavut. Int J Circumpolar Health. 2005;64(1):38–45. [DOI] [PubMed] [Google Scholar]
- [38].Barnabe C, Kaplan G, Avina-Zubieta A, et al. Complications of inflammatory arthritis in first nations and non-first nations populations of Alberta, Canada. J Rheumatol. 2016;43(6):1206. [Google Scholar]
- [39].Dallaire F, Dewailly E, Vézina C, et al. Portrait of outpatient visits and hospitalizations for acute infections in Nunavik preschool children. Can J Public Health. 2006;97(5):362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Gershon A, Khan S, Klein-Geltink J, et al. Asthma and Chronic Obstructive Pulmonary Disease (COPD) prevalence and health services use in Ontario Métis: a population-based cohort study. PLoS ONE. 2014;9(4):e95899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Carrière G, Bougie E, Kohen D, et al. Acute care hospitalization by Aboriginal identity, Canada, 2006 through 2008. Health Rep. 2016;27(8):3–11. [PubMed] [Google Scholar]
- [42].Kashuba S, Flowerdew G, Hessel P, et al. Acute care hospital morbidity in the blood Indian band, 1984-87. Can J Public Health. 1994;85(5):317–321. [PubMed] [Google Scholar]
- [43].Kendall C, Boucher L, Mark A, et al. A cohort study examining emergency department visits and hospital admissions among people who use drugs in Ottawa, Canada. Harm Reduct J. 2017;14(1): 1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kliewer E, Mayer T, Wajda A. The Health of Manitoba’s Métis Population and their Utilization of Medical Services: a Pilot Study. Manitoba: Manitoba Health; 2002. [Google Scholar]
- [45].Laupland K, Karmali S, Kirkpatrick A, et al. Distribution and determinants of critical illness among status Aboriginal Canadians. A population-based assessment. J Crit Care. 2006;21(3):243–247. [DOI] [PubMed] [Google Scholar]
- [46].Martens P, Sanderson D, Jebamani L. Health services use of Manitoba first nations people: is it related to underlying need? Can J Public Health. 2005;96(S1):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Martens P. Profile of Métis health status and healthcare utilization in Manitoba: a population-based study. Winnipeg: Manitoba Centre for Health Policy; 2010. [Google Scholar]
- [48].Shah B, Gunraj N, Hux J. Markers of access to and quality of primary care for aboriginal people in Ontario, Canada. Am J Public Health. 2003;93(5):798–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Alaghehbandan R, MacDonald D, Gates K, et al. 145: hospitalization for Pneumonia among aboriginal compared to non-aboriginal people, newfoundland and labrador. Am J Epidemiol. 2005;161(Supplement_1):S37–S37. [Google Scholar]
- [50].Alaghehbandan R, Gates K, MacDonald D. Hospitalization due to pneumonia among Innu, Inuit and non-Aboriginal communities, newfoundland and Labrador, Canada. Inter J Infect Dis. 2007;11(1):23–28. [DOI] [PubMed] [Google Scholar]
- [51].Banerji A, Lanctôt K, Paes B, et al. Comparison of the cost of hospitalization for respiratory syncytial virus disease versus palivizumab prophylaxis in Canadian Inuit Infants. Pediatr Infect Dis J. 2009;28(8):702–706. [DOI] [PubMed] [Google Scholar]
- [52].McCuskee S, Kirlew M, Kelly L, et al. Bronchiolitis and pneumonia requiring hospitalization in young first nations children in Northern Ontario, Canada. Pediatr Infect Dis J. 2014;33(10):1023–1026. [DOI] [PubMed] [Google Scholar]
- [53].Mostaço-Guidolin L, Towers S, Buckeridge D, et al. Age distribution of infection and hospitalization among Canadian first nations populations during the 2009 H1N1 pandemic. Am J Public Health. 2013;103(2):e39–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Hui C, Paes B, Papenburg J, et al. Palivizumab adherence and outcomes in Canadian aboriginal children. Pediatr Infect Dis J. 2016;35(11):1187–1193. [DOI] [PubMed] [Google Scholar]
- [55].Wang E, Law B, Stephens D. Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr. 1995;126(2):212–219. [DOI] [PubMed] [Google Scholar]
- [56].Senthilselvan A, Habbick B. Increased asthma hospitalizations among registered Indian children and adults in Saskatchewan, 1970–1989. J Clin Epidemiol. 1995;48(10):1277–1283. [DOI] [PubMed] [Google Scholar]
- [57].Alaghehbandan R, Sikdar C, MacDonald D, et al. Unintentional injuries among children and adolescents in Aboriginal and non-Aboriginal communities, newfoundland and Labrador, Canada. Int J Circumpolar Health. 2010;69(1):61–71. [DOI] [PubMed] [Google Scholar]
- [58].Alaghehbandan R, Sikdar K, Gladney N, et al. Epidemiology of severe burn among children in Newfoundland and Labrador, Canada. Burns. 2012;38(1):136–140. [DOI] [PubMed] [Google Scholar]
- [59].Anne George M, McCormick R, Lalonde C, et al. The RISC research project: injury in First Nations communities in British Columbia, Canada. Int J Circumpolar Health. 2013;72(1):21182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Bell N, Schuurman N, Hameed S, et al. Are we homogenising risk factors for public health surveillance? Variability in severe injuries on First Nations reserves in British Columbia, 2001-5. Inj Prev. 2011;17(6):394–400. [DOI] [PubMed] [Google Scholar]
- [61].Finès P, Bougie E, Oliver L, et al. Hospitalizations for unintentional injuries among Canadian adults in areas with a high percentage of Aboriginal-identity residents. Chronic Dis Inj Canada. 2013;33(4):204–217. [PubMed] [Google Scholar]
- [62].Brussoni M, George M, Jin A, et al. Injuries to Aboriginal populations living on- and off-reserve in metropolitan and non-metropolitan areas in British Columbia, Canada: incidence and trends, 1986-2010. BMC Public Health. 2016;16(1). DOI: 10.1186/s12889-016-3078-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Brussoni M, George M, Jin A, et al. Hospitalizations due to unintentional transport injuries among Aboriginal population of British Columbia, Canada: incidence, changes over time and ecological analysis of risk markers. Plos One. 2018;13(1): 1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Oliver L, Kohen D. Unintentional injury hospitalizations among children and youth in areas with a high percentage of Aboriginal identity residents: 2001/2002 to 2005/2006. Health Rep. 2012;23(3):7–15. [PubMed] [Google Scholar]
- [65].Bougie E, Finès P, Oliver L, et al. Unintentional injury hospitalizations and socio-economic status in areas with a high percentage of First Nations identity residents. Health Rep. 2014;25(2):3–12. [PubMed] [Google Scholar]
- [66].Brussoni M, Jin A, George M, et al. Aboriginal community-level predictors of injury-related hospitalizations in British Columbia, Canada. Prevent Sci. 2014;16(4):560–567. [DOI] [PubMed] [Google Scholar]
- [67].Oliver L, Finès P, Bougie E, et al. Intentional injury hospitalizations in geographical areas with a high percentage of Aboriginal-identity residents, 2004/2005 to 2009/2010. Chronic Dis Inj Canada. 2014;34(2–3):82–93. [PubMed] [Google Scholar]
- [68].Myers R, Li B, Fong A, et al. Hospitalizations for acetaminophen overdose: a Canadian population-based study from 1995 to 2004. BMC Public Health. 2007;7(1). DOI: 10.1186/1471-2458-7-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Myers R, Li B, Shaheen A. Emergency department visits for acetaminophen overdose: a Canadian population-based epidemiologic study (1997–2002). CJEM. 2007;9(4):267–274.70. Lyons K, Ezekowitz J, Liu W, McAlister F, Kaul P. Differences in Mortality Outcomes Among Status Aboriginal Patients and Caucasian Patients With Heart Failure. Canadian Journal of Cardiology. 2013;29(10):S196-S197. [DOI] [PubMed] [Google Scholar]
- [70].Lyons K, Ezekowitz J, Liu W, et al. Differences in mortality outcomes among status aboriginal patients and Caucasian patients with heart failure. Can J Cardiol. 2013;29(10):S196–S197. [Google Scholar]
- [71].Schultz A, Dahl L, McGibbon E, et al. Health outcome and follow-up care differences between first nation and non-first nation coronary angiogram patients: a retrospective cohort study. Can J Cardiol. 2018;34(10):1333–1340. [DOI] [PubMed] [Google Scholar]
- [72].Wei-Randall H, Davidson M, Jin J, et al. Acute myocardial infarction hospitalization and treatment: areas with a high percentage of First Nations identity residents. Health Rep. 2013;24(7):3–10. [PubMed] [Google Scholar]
- [73].Young T, Moffatt M, O’Neil J. Cardiovascular diseases in a Canadian Arctic population. Am J Public Health. 1993;83(6):881–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Atzema C, Khan S, Lu H, et al. Cardiovascular Disease Rates, Outcomes, and Quality of Care in Ontario Métis: a Population-Based Cohort Study. PLOS ONE. 2015;10(3):e0121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Kapral M, Shah B, Green M, et al. Hospital admission for stroke or transient ischemic attack among First Nations people with diabetes in Ontario: a population-based cohort study. CMAJ Open. 2020;8(1):E156–E162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Nicolle L, Friesen D, Harding G, et al. Hospitalization for acute pyelonephritis in Manitoba, Canada, during the period from 1989 to 1992: impact of diabetes, pregnancy, and aboriginal origin. Clinl Infect Dis. 1996;22(6):1051–1056. [DOI] [PubMed] [Google Scholar]
- [77].Molnar A, Moist L, Klarenbach S, et al. Hospitalizations in dialysis patients in Canada: a national cohort study. Can J Kidney Health Dis. 2018;5:205435811878037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Jetté N, Quan H, Faris P, et al. Health resource use in epilepsy: significant disparities by age, gender, and aboriginal status. Epilepsia. 2008;49(4):586–593. [DOI] [PubMed] [Google Scholar]
- [79].Lasry O, Dudley R, Fuhrer R, et al. 080 Traumatic brain injury in a rural indigenous population in Canada: a community-based approach to surveillance. Can J Neurol Sci. 2016;43(S2):S39–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Barnabe C, Jones C, Bernatsky S, et al. Inflammatory arthritis prevalence and health services use in the first nations and non–first nations populations of Alberta, Canada. Arthritis Care Res (Hoboken). 2017;69(4):467–474. [DOI] [PubMed] [Google Scholar]
- [81].Stammers D, Israels S, Lambert P, et al. Cancer incidence, morbidity, and survival in Canadian first nation children: a Manitoba population-based study from the cancer in young people in Canada (CYP-C) registry. Pediatr Blood Cancer. 2014;61(12):2164–2169. [DOI] [PubMed] [Google Scholar]
- [82].Carrière G, Bougie E, Kohen D. Acute care hospitalizations for mental and behavioural disorders among First Nations people. Health Rep. 2018;29(6):11–19. [PubMed] [Google Scholar]
- [83].D’Arcy C, Fritz W, Mental Health A. System in Transition: profiles of Change. Can J Psychiatry. 1979;24(2):121–131. [DOI] [PubMed] [Google Scholar]
- [84].Lavoie J, Ward A, Wong S, et al. Hospitalization for mental health related ambulatory care sensitive conditions: what are the trends for First Nations in British Columbia? Int J Equity Health. 2018;17(1). DOI: 10.1186/s12939-018-0860-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Soleimani A, Rosychuk R, Newton A. Predicting time to emergency department re-visits and inpatient hospitalization among adolescents who visited an emergency department for psychotic symptoms: a retrospective cohort study. BMC Psychiatry. 2016;16(1). DOI: 10.1186/s12888-016-1106-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Thomson M. Otitis media. How are first nations children affected? Can Family Physician. 1994;40:1943–1950. [PMC free article] [PubMed] [Google Scholar]
- [87].He H, Xiao L, Torrie J, et al. Disparities in infant hospitalizations in Indigenous and non-Indigenous populations in Quebec, Canada. Can Med Assoc J. 2017;189(21):E739–E746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Booth G, Hux J, Fang J, et al. Time trends and geographic disparities in acute complications of diabetes in Ontario, Canada. Diabetes Care. 2005;28(5):1045–1050. [DOI] [PubMed] [Google Scholar]
- [89].Campbell D, Lacny S, Weaver R, et al. Age modification of diabetes-related hospitalization among first nations adults in Alberta, Canada. Diabetol Metab Syndr. 2014;6(1):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Rose G, Duerksen F, Trepman E, et al. Multidisciplinary treatment of diabetic foot ulcers in Canadian Aboriginal and non-Aboriginal people. Foot Ankle Surg. 2008;14(2):74–81. [DOI] [PubMed] [Google Scholar]
- [91].Pohar S, Johnson J. Health care utilization and costs in Saskatchewan’s registered Indian population with diabetes. BMC Health Serv Res. 2007;7(1). DOI: 10.1186/1472-6963-7-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Ospina M, Voaklander D, Senthilserlvan A, et al. Hospitalizations after diagnosed chronic obstructive pulmonary disease in aboriginal peoples in Alberta, Canada. American Journal of Respiratory and Critical Care Medicine [Internet]. 2015. [cited 2020 Jul 22] A2303–A2303. Available from: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2015.191.1_MeetingAbstracts.A2303
- [93].Ospina M, Rowe B, Voaklander D, et al. Emergency department visits after diagnosed chronic obstructive pulmonary disease in aboriginal people in Alberta, Canada. CJEM. 2016;18(6):420–428. [DOI] [PubMed] [Google Scholar]
- [94].Rosychuk R, Voaklander D, Klassen T, et al. Asthma presentations by children to emergency departments in a Canadian province: a population-based study. Pediatr Pulmonol. 2010;45(10):985–992. [DOI] [PubMed] [Google Scholar]
- [95].Rowe B, Voaklander D, Wang D, et al. Asthma presentations by adults to emergency departments in Alberta, Canada. Chest. 2009;135(1):57–65. [DOI] [PubMed] [Google Scholar]
- [96].Sin D, Wells H, Svenson L, et al. Asthma and COPD among aboriginals in Alberta, Canada. Chest. 2002;121(6):1841–1846. [DOI] [PubMed] [Google Scholar]
- [97].Sin D, Spier S, Svenson L et al. The relationship between birth weight and childhood asthma: a population-based cohort study. Archives of pediatrics & adolescent medicine [Internet]. 2004. [cited 2020 Jul 15];158(1):60–64. Available from: https://doi-org.acces.bibl.ulaval.ca/10.1001/archpedi.158.1.60doi:10.1378/chest.121.6.1841 [DOI] [PubMed] [Google Scholar]
- [98].Charland K, Brownstein J, Verma A, et al. Increased influenza-related healthcare utilization by residents of an urban aboriginal community. Epidemiol Infect. 2011;139(12):1902–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Rosychuk R, Klassen T, Metes D, et al. Croup presentations to emergency departments in Alberta, Canada: a large population-based study. Pediatr Pulmonol. 2010;45(1):83–91. [DOI] [PubMed] [Google Scholar]
- [100].Wen S, Goel V, Williams J. Utilization of health care services by immigrants and other ethnic/cultural groups in Ontario. Ethn Health. 1996;1(1):99–109. [DOI] [PubMed] [Google Scholar]
- [101].Shah B, Slater M, Frymire E, et al. Use of the health care system by Ontario First Nations people with diabetes: a population-based study. CMAJ Open. 2020;8(2):E313–E318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Levy D, Gunraj N, Pope J, et al. Childhood-onset systemic lupus erythematous in Ontario: long term outcomes in a population-based cohort with universal health care coverage. Arthritis Rheumatism. 2013;65(10):S533–S534. [Google Scholar]
- [103].Newton A, Rosychuk R, Dong K, et al. Emergency health care use and follow-up among sociodemographic groups of children who visit emergency departments for mental health crises. Can Med Assoc J. 2012;184(12):E665–E674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Lafond G, Haver C, McLeod V, et al. Characteristics and residence of First Nations patients and their use of health care services in Saskatchewan, Canada: informing First Nations and Métis health services. J Eval Clin Pract. 2016;23(2):294–300. [DOI] [PubMed] [Google Scholar]
- [105].Alharbi S, Van Caeseele P, Consunji-Araneta R, et al. Epidemiology of severe pediatric adenovirus lower respiratory tract infections in Manitoba, Canada, 1991-2005. BMC Infect Dis. 2012;12(1). DOI: 10.1186/1471-2334-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Newton A, Tsang C, Rosychuk R. Emergency Health Care Use among Sociodemographic Groups of Children Presenting to Emergency Departments for Self-Harm in Alberta. CJEM. 2015;17(5):497–506. [DOI] [PubMed] [Google Scholar]
- [107].Newton A, Rosychuk R, Niu X, et al. Emergency department use and postvisit care for anxiety and stress disorders among children. Pediatr Emerg Care. 2016;32(10):658–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Poling J, Kelly L, Chan C, et al. Hospital admission for community-acquired pneumonia in a First Nations population. Can J Rural Med. 2014;19(4):135–141. [PubMed] [Google Scholar]
- [109].Boeckx R, Postl B, Coodin F. Gasoline sniffing and tetraethyl lead poisoning in children. Pediatrics. 1977;60(2):140–145. [PubMed] [Google Scholar]
- [110].Houd S, Qinuajuak J, Epoo B. The outcome of perinatal care in Inukjuak, Nunavik, Canada 1998–2002. Int J Circumpolar Health. 2004;63(sup2):239–241. [DOI] [PubMed] [Google Scholar]
- [111].Lessard P, Kinloch D. Northern obstetrics: a 5-year review of delivery among Inuit women. Can Med Assoc J. 1987;137(11):1017–1021. [PMC free article] [PubMed] [Google Scholar]
- [112].Oluyomi-Obi T, Avery L, Schneider C, et al. Perinatal and Maternal Outcomes in Critically ill Obstetrics Patients With Pandemic H1N1 Influenza A. J Obstet Gynaecology Canada. 2010;32(5):443–447. [DOI] [PubMed] [Google Scholar]
- [113].Wagner V, Osepchook C, Harney E, et al. Remote Midwifery in Nunavik, Québec, Canada: outcomes of Perinatal Care for the Inuulitsivik Health Centre, 2000-2007. Birth. 2012;39(3):230–237. [DOI] [PubMed] [Google Scholar]
- [114].Houston C, Weiler R, Habbick B. Severity of lung disease in Indian children. Can Med Assoc J. 1979;120(9):1116–1121. [PMC free article] [PubMed] [Google Scholar]
- [115].Jung J, Fowler R, Long J et al. 2009-2010 H1N1-Related Critical Illness Among Aboriginal Canadians And Non-Aboriginal Canadians. B49 INTENSIVE CARE UNIT MANAGEMENT. 2011. [DOI] [PMC free article] [PubMed]
- [116].Callegari P, Alton J, Shankowsky H, et al. Burn injuries in native Canadians: a 10-year experience. Burns. 1989;15(1):15–19. [DOI] [PubMed] [Google Scholar]
- [117].Bresee L, Knudtson M, Zhang J, et al. Likelihood of coronary angiography among First Nations patients with acute myocardial infarction. Can Med Assoc J. 2014;186(10):E372–E380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Shavadia J, Okpalauwaekwe U, Rana M, et al. Cardiovascular profile and Outcomes of Acute Coronary Syndromes in Indigenous compared with non-Indigenous patients: an Observational analysis from Northern Saskatchewan. Can J Cardiol. 2020;36(10):S7–S8. [DOI] [PubMed] [Google Scholar]
- [119].Khan N, Palepu A, Norena M, et al. Differences in hospital mortality among critically Ill patients of Asian, Native Indian, and European descent. Chest. 2008;134(6):1217–1222. [DOI] [PubMed] [Google Scholar]
- [120].Cohen M, Young T, Hammarstrand K. Ethnic variation in cholecystectomy rates and outcomes, Manitoba, Canada, 1972-84. Am J Public Health. 1989;79(6):751–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Ahmed S, Humphreys S, Rivers C, et al. Traumatic spinal cord injuries among Aboriginal and non-Aboriginal populations of Saskatchewan: a prospective outcomes study. Can J Surg. 2020;63(3):E315–E320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Blackmer SC. A comparison of traumatic brain injury in the Saskatchewan native North American and non-native North American populations. Brain Inj. 1999;13(8):627–635. [DOI] [PubMed] [Google Scholar]
- [123].Beres A, Al-Abbad S, Puligandla P. Appendicitis in northern aboriginal children: does delay in definitive treatment affect outcome? Journal of pediatric surgery [Internet]. 2010. [cited 2020 Jul 15];45(5):890–893. Available from: https://doi-org.acces.bibl.ulaval.ca/10.1016/j.jpedsurg.2010.02.008 [DOI] [PubMed] [Google Scholar]
- [124].Carey L. Lead shot appendicitis in northern native people. Can Assoc Radiol J. 1977;28(3):171–174. [PubMed] [Google Scholar]
- [125].Thanh N, Toye J, Savu A, et al. Health Service Use and Costs Associated with Low Birth Weight—A Population Level Analysis. J Pediatr. 2015;167(3):551–556.e3. [DOI] [PubMed] [Google Scholar]
- [126].Barnabe C, Zheng Y, Ohinmaa A, et al. Comparison of health service utilization costs between aboriginal and non-aboriginal patients with rheumatoid arthritis requiring biologic therapy. J Rheumatol. 2016;43(6):1207. [Google Scholar]
- [127].Mbuzi V, Fulbrook P, Jessup M. Indigenous peoples’ experiences and perceptions of hospitalisation for acute care: a metasynthesis of qualitative studies. Int J Nurs Stud. 2017;71:39–49. [DOI] [PubMed] [Google Scholar]
- [128].Brown AE, Fereday JA, Middleton PF, et al. Aboriginal and Torres Strait Islander women’s experiences accessing standard hospital care for birth in South Australia – a phenomenological study. Women Birth. 2016;29(4):350–358. [DOI] [PubMed] [Google Scholar]
- [129].McGrath P, Rawson N. The experience of relocation for specialist treatment for indigenous women diagnosed with vulvar cancer in East Arnhem Land. J Psychosoc Oncol. 2013;31(5):540–555. [DOI] [PubMed] [Google Scholar]
- [130].Arnaert A, Schaack G. Cultural awareness of Inuit patients’ experiences with emergency nursing care. Accid Emergency Nurs. 2006;14(2):97–103. [DOI] [PubMed] [Google Scholar]
- [131].Watson J, Hodson K, Johnson R, et al. The maternity experiences of indigenous women admitted to an acute care setting. Aust J Rural Health. 2008;10(3):154–160. [DOI] [PubMed] [Google Scholar]
- [132].Nelson SE, Wilson K. Understanding barriers to health care access through cultural safety and ethical space: indigenous people’s experiences in Prince George, Canada. Soc Sci Med. 2018;218:21–27. [DOI] [PubMed] [Google Scholar]
- [133].Thomas DP, Anderson IPS. Use of emergency departments by Aboriginal and Torres Strait Islander people. Emergency Med Australasia. 2006;18(1):68–76. [DOI] [PubMed] [Google Scholar]
- [134].Thomas DP, Anderson IP, Kelaher MA. Accessibility and quality of care received in emergency departments by Aboriginal and Torres Strait Islander people. Aust Health Rev. 2008;32(4):648. [DOI] [PubMed] [Google Scholar]
- [135].McLane P, Barnabe C, Holroyd BR, et al. First Nations emergency care in Alberta: descriptive results of a retrospective cohort study. BMC Health Serv Res. 2021;21(1). DOI: 10.1186/s12913-021-06415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Secombe P, Brown A, McAnulty G, et al. Aboriginal and Torres Strait Islander patients requiring critical care: characteristics, resource use, and outcomes. Crit Care Resusc. 2019;21(3):200–211. [PubMed] [Google Scholar]
- [137].Davy C, Harfield S, McArthur A, et al. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health. 2016;15(1). DOI: 10.1186/s12939-016-0450-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Berg K, McLane P, Eshkakogan N, et al. Perspectives on Indigenous cultural competency and safety in Canadian hospital emergency departments: a scoping review. Int Emerg Nurs. 2019;43:133–140. [DOI] [PubMed] [Google Scholar]
- [139].Clifford A, McCalman J, Bainbridge R, et al. Interventions to improve cultural competency in health care for Indigenous peoples of Australia, New Zealand, Canada and the USA: a systematic review. Int J Qual Health Care. 2015;27(2):89–98. [DOI] [PubMed] [Google Scholar]
- [140].Lewis ME, Myhra LL. Integrated care with indigenous populations: a systematic review of the literature. Am Indian Alaska Native Mental Health Res. 2017;24(3):88–110. [DOI] [PubMed] [Google Scholar]


