ABSTRACT
Background: Animal-assisted interventions (AAI) are increasingly applied for people with post-traumatic stress disorder (PTSD) symptoms albeit its effectiveness is unclear.Objectives: To examine the effectiveness of AAI for treating PTSD symptoms.Method: We searched 11 major electronic databases for studies reporting quantitative data on effects of AAI for children and adults with PTSD symptoms. Of 22ʹ211 records identified, we included 41 studies with 1111 participants in the systematic review comprising eight controlled studies with 469 participants in the meta-analysis. We conducted random-effects meta-analyses with all controlled studies based on standardized mean differences (SMD), and calculated standardized mean change (SMC) as effect sizes for studies with a pre-post one-group design. Two independent researchers assessed the quality of the included studies using the NIH Study Quality Assessment Tools. The primary outcome was PTSD or depression symptom severity measured via a standardized measurement at pre- and post-intervention assessments.Results: There was a small but not statistically significant superiority of AAI over standard PTSD psychotherapy (SMD = −0.26, 95% CI: −0.56 to 0.04) in reducing PTSD symptom severity while AAI was superior to waitlist (SMD = −0.82, 95% CI: −1.56 to 0.08). Getting a service dog was superior to waiting for a service dog (SMD = −0.58, 95% CI: −0.88 to −0.28). AAI led to comparable effects in reducing depression as standard PTSD psychotherapy (SMD = −0.03, CI: −0.88 to 0.83). Pre-post comparisons showed large variation for the reduction in PTSD symptom severity, with SMCs ranging from −0.38 to −1.64, and for depression symptom severity, ranging from 0.01 to −2.76. Getting a service dog lowered PTSD symptoms between −0.43 and −1.10 and depression with medium effect size of −0.74.Conclusions: The results indicate that AAI are efficacious in reducing PTSD symptomatology and depression. Future studies with robust study designs and large samples are needed for valid conclusions.
KEYWORDS: Animal-assisted intervention, animal-assisted therapy, human-animal interaction, trauma, post-traumatic stress disorder, depression, meta-analysis
HIGHLIGHTS
We conducted a systematic review with meta-analysis to provide an up-to-date summary on the state of evidence regarding the effectiveness of animal-assisted interventions in treating people with PTSD symptoms.
Results are promising but high-quality research is lacking to date.
Abstract
Antecedentes: Las intervenciones asistidas por animales (AAI por sus siglas en inglés) se aplican cada vez más a personas con síntomas de trastorno de estrés postraumático (TEPT) aunque su eficacia no es clara.
Objetivos: Examinar la efectividad de la AAI para el tratamiento del TEPT
Método: Se realizaron búsqueda en 11 bases de datos electrónicas importantes para estudios que reportaran información cuantitativa sobre los efectos de AAI para niños y adultos con síntomas de TEPT. De los 22.211 registros identificados, se incluyeron 41 estudios con 1111 participantes en la revisión sistemática que comprendían ocho estudios controlados con 469 participantes en el metanálisis. Se realizaron metanálisis de efectos aleatorios con todos los estudios controlados según las diferencias medias estandarizadas (SMD según siglas en ingles), y se calculó el cambio de medias estandarizado SMC (por sus siglas en inglés) como tamaños del efecto para los estudios con diseño de un grupo pre-post. Dos investigadores independientes evaluaron la calidad de los estudios incluidos usando las Herramientas de Evaluación de Calidad del Estudio del NIH. El resultado primario fue la medición de la severidad del TEPT o síntomas depresivos a través de mediciones estandarizadas en evaluaciones pre y post intervención.
Resultados: Hubo una pequeña superioridad, pero no estadísticamente significativa, del AAI sobre psicoterapia estándar para TEPT (SMD= −0.26, IC 95%:-0.56 a 0.04) en la reducción de la severidad de los síntomas de TEPT, mientras que la AAI fue superior a la lista de espera (SMD= −0.82, IC 95%:-1.56 a 0.08). Tener un perro de servicio fue superior a esperar por un perro de servicio (SMD= −0.58, IC 95%:-0.88 a −0.28). La AAI produjo efectos comparables en la reducción de depresión como la psicoterapia estándar para TEPT (SMD= −0.03, IC: −0.88 a 0.83). Las comparaciones pre-post mostraron una gran variación en la reducción de la severidad de síntomas de TEPT, con rangos de SMC desde −0.38 a −1.64, y para la severidad de síntomas de depresión, rangos desde 0.01 a −2.76. Tener un perro de servicio bajo los síntomas de TEPT entre −0.43 a −1.10 y la depresión con un tamaño de efecto medio de −0.74.
Conclusiones: Los resultados indican que los AAI son eficaces para reducir la sintomatología del TEPT y depresión. Se requieren estudios futuros con diseños de estudio sólidos y muestras grandes para obtener conclusiones válidas.
PALABRAS CLAVE: Intervención asistida por animales, terapia asistida por animales, interacción humano-animal, trauma, trastorno de estrés postraumático, depresión, metanálisis
背景: 尽管有效性尚不清楚, 动物辅助干预 (AAI) 正越来越多地应用于患有创伤后应激障碍 (PTSD) 症状的人。
目的: 探讨AAI治疗PTSD症状的有效性。
方法: 我们搜索了11个主要的电子数据库, 以发现报告了AAI治疗患有PTSD症状的儿童和成人效果定量数据的研究。在确定的22,211条记录中, 我们纳入了41项研究, 其中1111名参与者参加了包括8项对照研究的系统综述, 其中469名参与者参加了元分析。我们对所有对照研究进行了基于标准平均差 (SMD) 的随机效应元分析, 并计算了标准平均改变 (SMC) 作为效应的大小, 用于采用前后单组设计的研究。两名独立研究人员使用NIH研究质量评估工具评估了纳入研究的质量。主要结果是干预前, 后评估中通过标准化测量方法测得的PTSD或抑郁症状严重程度。
结果: 在降低PTSD症状严重程度方面, AAI稍优于标准PTSD心理治疗但不统计显著 (SMD = −0.26, 95%CI:-0.56至0.04), AAI优于等待清单 (SMD = −0.82, 95%, CI:-1.56至0.08) 。获得服务犬比等待服务犬好 (SMD = −0.58, 95%CI:-0.88至-0.28) 。AAI在减轻抑郁方面与标准PTSD心理疗法具有可比的效果 (SMD = −0.03, CI:-0.88至0.83) 。事前比较显示, PTSD症状严重程度的降低存在较大差异, SMC的范围从−0.38至−1.64, 抑郁症状的严重程度范围从0.01至-2.76。养一只服务犬可以将, PTSD症状降低-0.43至-1.10之间, 抑郁症能降低的中度效应值为-0.74。
结论: 结果表明, AAI在减少PTSD症状和抑郁方面有效。需要有可靠研究设计和大样本的未来研究才能得出有效的结论。
关键词: 动物辅助干预, 动物辅助治疗, 人与动物的相互作用, 创伤, 创伤后应激障碍, 抑郁, 元分析
1. Introduction
Including animals in psychological treatment is a common and still increasing therapeutic practice. Animal-assisted interventions (AAI) are defined as ‘goal-oriented and structured interventions that intentionally include or incorporate animals in health, education and human services for the purpose of therapeutic gains in humans’ (IAHAIO, 2018). One common indication for AAI found in literature is treatment of individuals who have experienced trauma and have developed post-traumatic stress disorder (PTSD) (Charry-Sanchez, Pradilla, & Talero-Gutierrez, 2018; Jones, Rice, & Cotton, 2019; Tedeschi, Jenkins, Parish-Plass, Olmert, & Yount, 2019).
Practice of AAI for people with PTSD symptoms varies broadly and comprises therapeutic interventions (animal-assisted therapy) as well as less-structured activities with animals (animal-assisted activity). A prominent form of animal-assisted therapy with this population is the integration of an animal into manualized PTSD psychotherapy, referred to as animal-assisted psychotherapy. Other intervention forms that include human–animal interaction are less specific to psychotherapeutic techniques and settings. A different and emerging approach is that patients suffering from PTSD obtain a trained PTSD service dog that lives in the patient’s home. This illustrates the diversity of AAI for people who have experienced trauma. Moreover, there is great variability in how animals are integrated into a treatment and even the involved species differ widely. Most commonly, the treatment providers work with horses and dogs. This variability combined with the fast development of the field of AAI for people with PTSD symptoms raise the question about effectiveness and research-guided standards.
Integration of animals in treatment approaches for trauma-affected individuals is based on the observation of promising outcomes of AAI for a number of populations such as psychiatric patients (Hawkins, Hawkins, Dennis, Williams, & Lawrie, 2019; Rossetti & King, 2010), patients with autism spectrum disorders and behavioural difficulties (O’Haire, 2013; Trzmiel, Purandare, Michalak, Zasadzka, & Pawlaczyk, 2019) or people with cognitive impairments or dementia (Hu, Zhang, Leng, Li, & Chen, 2018; Zafra-Tanaka, Pacheco-Barrios, Tellez, & Taype-Rondan, 2019), although results are sometimes mixed. There is also an increasing number of studies investigating the effects of AAI for people who experienced trauma including patients with PTSD. A systematic review on the effects of AAI for treating individuals who have experienced trauma included ten studies but only five of which measured PTSD symptom severity (O’Haire, Guerin, & Kirkham, 2015). The authors report that AAI lowered observed PTSD symptoms between 13 and 80% across these five studies with small to large effect sizes. A recently published meta-analysis (Germain, Wilkie, Milbourne, & Theule, 2018) also investigated the effects of animal-assisted psychotherapy for persons who have experienced trauma. The authors included eight studies in a pre-post comparison analysis and found a large effect size. In the analysis comparing animal-assisted psychotherapy versus active control treatment, only two studies were included resulting in a small to moderate effect size (Germain et al., 2018). Both the review and the meta-analysis concluded that AAI might be an effective treatment for trauma but highlighted a clear need for more research. Similar problems apply for the evidence regarding the use of PTSD service dogs. A recent review gives an overview of the effects of service dogs for veterans with PTSD (van Houtert, Endenburg, Wijnker, Rodenburg, & Vermetten, 2018). However, from 19 included articles, only six were empirical studies and the authors concluded that there is not enough empirical data supporting the effectivity of PTSD service dogs (van Houtert et al., 2018). During the last few years, the number of published research investigating the effects of AAI for trauma survivors with PTSD symptoms increased largely. However, an up-to date review with meta-analysis is lacking leaving many questions regarding the effectiveness of AAI for people with PTSD symptoms unanswered. Especially the comparative effectiveness of AAI as compared with established PTSD psychotherapy without animal assistance remains largely unclear to-date.
This systematic review with meta-analysis aims to fill this gap. We included a larger number of studies and did not restrict included studies to certain treatment forms compared to the recently published meta-analysis, but rather included all interventions that fulfill the above-mentioned definition of AAI. We calculated effect sizes for PTSD symptom severity in studies with either a pre-post one-group or a control-group design, and we conducted meta-analyses with controlled studies in which PTSD and depression outcomes were used. The aim of this article is to give a comprehensive and updated insight of the effectiveness of AAI for people with PTSD symptoms.
2. Methods
2.1. Search strategy and selection criteria
We conducted a systematic literature search in electronic databases (PsycINFO, MEDLINE, PSYNDEXplus, ERIC, Embase, PubMed, CINAHL, Web of Science, Scopus, ProQuest and PTSDpubs (ProQuest); see Appendix 1, Table A1, summarizing the applied search strategies). We checked the reference lists of a previous systematic review (O’Haire et al., 2015) and a previous meta-analysis (Germain et al., 2018). Moreover, we searched the database HABRI Central, a specific online platform for open research and collaboration in the field of human–animal interaction.
All obtained records were imported into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia), where all duplicates were removed and the screening was performed. Titles and abstracts of the retrieved records were screened by two independent researchers who excluded clearly irrelevant references. Full texts were also screened by two independent researchers. Ambiguities were resolved by consensus between all involved researchers in the screening process (KH, PK, AH, FT, CG). If the publication was not available through the university libraries, study authors were contacted. Records were excluded if we were unable to obtain the full-text (Figure 1).
Figure 1.
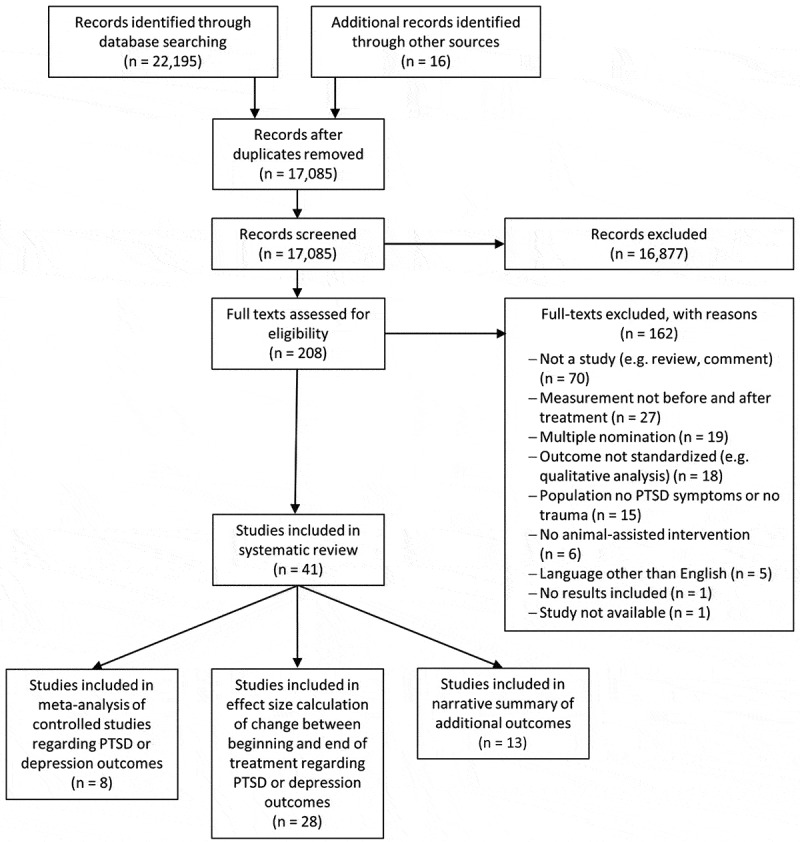
Flow chart of study selection
Study identification, screening and eligibility determination was done according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (McInnes et al., 2018). The study procedure was defined apriori and the protocol was preregistered with PROSPERO (Hediger et al., 2019).
2.2. Study selection
We included studies with participants who had experienced a traumatic event (we excluded studies with healthy participants). Participants in the included studies needed to fulfill criterion A according to the diagnostic criteria for PTSD as specified in the Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) (American Psychiatric Association, 2013), and they needed to report the occurrence of PTSD symptoms in the aftermath. Eligible studies had to report quantitative data at pre- and post-intervention assessments. With respect to the interventions, we included studies in which an animal was involved intentionally as part of the intervention to fulfill the criterion of AAI (according to the definitions of the International Association of Human Animal Interaction Organizations (IAHAIO, 2018)). Finally, we included only articles that were written in English. We did not restrict included records to studies that were published in peer-reviewed scientific journals in order to reduce publication bias, and we included studies which used control groups as well as studies with a pre-post one-group design.
We identified secondary publications of one study in several cases. This occurred for one study included in the effect size calculation and for four studies included in the narrative review. In such cases we primarily focused on the article reporting the predefined primary outcome, the article with the most comprehensive information, or the article that underwent a peer-review process. The secondary publications were used for data extraction in order to search for study information which was lacking in the primary publication (see Tables 3, 4 and Appendix 2 for detailed information).
Table 3.
Characteristics and results of the 28 studies with pre-post and pre-follow-up effect sizes of AAI regarding PTSD symptom and/or depression severity
| First author, Publication year | Study design | N analysed | Gender | Age (range, M, SD) |
Type of experienced trauma | Participating animals | Treatment provider | AAI terminology | Pre-post SMC (95% CI) at end of treatmenta | Pre-follow-up SMD (95% CI) at end of treatmenta |
|---|---|---|---|---|---|---|---|---|---|---|
| Bergen-Cico (2018) | Control | 34 | NR | M = 42, SD = 11.5 | War | Dogs | Dog trainer | Therapeutic dog ownership and training | PTSD: −0.43 (−0.66 to −0.21) | NA |
| Burton (2019) | Control | 11 | 16m/4fc | 33–63M = 47, SD = 14 | War | Horses | Occupational therapist, EAGALA-certified with professional horse handler | Equine-assisted psychotherapy | PTSD: −1.03 (−1.60 to −0.46) | NA |
| Craven (2013) | Pre-post | 5 | 4m/2fc | 26–66, M = 44, SD = 15.4 | War, sexual abuse | Horses | Clinical psychologist/equine specialist, counsellor, equine specialist | Equine-assisted psychotherapy | PTSD: −4.28 (−6.98 to −1.58) | NA |
| Dietz (2012) | Control | 121 | 10m/143fc | 7–17 | Sexual abuse | Dogs | Licenced and master’s level clinicians (social work, trained psychologists, counselling) | Animal-assisted therapy | PTSD: −0.59 (−0.71 to −0.46) | NA |
| Earles (2015) | Pre-post | 16 | 4m/12f | 33–62, M = 51.25, SD = 9.99 | Various traumas | Horses | NR | Equine-assisted therapy | PTSD: −0.78 (−1.17 to −0.39) Depression: −0.33 (−0.63 to −0.03) |
NA |
| Faye (2003) | Pre-post | 3 | 6m/7fc | 7–11, M = 9.18, SD = 1.40 | Nature | Dolphins | Psychologist | Dolphin interaction | PTSD: −0.94 (−1.94 to 0.05) | NA |
| Gómez (2016) | Pre-post | 5 | 6m/2fc | 46–76, M = 58, SD = 9.85 | War | Horses | Certified PATH International therapeutic riding instructor and certified therapeutic recreation specialist | Equine therapy | PTSD: −0.44 (−1.00 to 0.13) | PTSD: -0.58 (−1.31 to 0.15) |
| Hamama (2011) | Pre-postb | 9 | 0m/9f | 14–16,M = 14.9, SD = 1.5 | Physical or sexual abuse | Dogs | Social work students and professional animal-assisted therapist | Dog-assisted therapy | PTSD: −0.69 (−1.18 to −0.20) Depression: −0.47 (−0.89 to −0.04) |
NA |
| Johnson (2018) | RCT | 19 | 32m/6fc | 29–73, M = 54.35, SD = 12.85 | War | Horses | Occupational therapists and PATH-certified riding instructors | Therapeutic horseback riding | PTSD: −0.73 (−1.07 to −0.39) | NA |
| Kemp (2014) | Pre-post | 30 | 6m/24f | Children: 8–11, M = 9.8, SD = 1.3 Adolescents: 12–17, M = 15.5, SD = 0.8 |
Physical or sexual abuse, neglect | Horses | Counsellors | Equine-facilitated therapy | PTSD: −3.73 (−4.70 to −2.76) Depression: −1.31 (−1.70 to −0.92) |
NA |
| Kloep (2017) | Pre-post | 12 | 9m/4fc | Cohort 1: 26–70, M = 44, SD = 15.4 Cohort 2:23–53, M = 36, SD = 13 |
War | Dogs | NR | Animal-assisted therapy | PTSD: −4.31 (−6.06 to −2.56) Depression: −2.76 (−3.91 to −1.61) |
PTSD: −3.92 (−5.67 to −2.17) |
| Lanning (2013) | Pre-post | 7 | 10m/3fc | 29–52, M = 35.5, SD = 6.9 | War | Horses | Veteran volunteers | Equine-assisted activities | Depression: −0.50 (−0.99 to −0.00) | NA |
| Lanning (2017) | Pre-post | 39 | 33m/18fc | 22–57, M = 36.8, SD = 11.26 | War | Horses | Volunteers | Therapeutic horseback riding | PTSD: −0.79 (−1.07 to −0.51) | PTSD: −0.52 (−0.81 to −0.22) |
| Malinowski (2018) | Pre-post | 7 | 6m/1f | 31–68, M = 58, SD = 13.14 | War | Horses | Licenced therapist and certified equine specialist | Equine-assisted activities and therapies | PTSD: −1.16 (−1.90 to −0.42) | NA |
| McCullough (2011)/McCullough (2015) | Pre-post | 11 | 6m/5f | 10–18, M = 13.73 SD = 2.83 | Physical, sexual, emotional abuse and neglect | Horses | Psychotherapist | Equine-facilitated psychotherapy | PTSD: −0.47 (−0.86 to −0.08) | NA |
| Mueller (2017) | Control | 25 | 45m/9fc | 10–18 | Physical, sexual, emotional abuse and neglect | Horses | Licenced clinical social worker | Equine-facilitated psychotherapy | PTSD: −0.38 (−0.63 to −0.14) | NA |
| Naste (2018) | Pre-post | 2 | 0m/3f | 10–12, M = 11, SD = 1 | Sexual abuse, neglect | Horses | Registered mental health practitioner | Equine-facilitated therapy | PTSD: 0.54 (−0.40 to 1.49) | NA |
| O’Haire (2018) | Control | 75 | 110m/31fc | M = 37.1, SD = 8.3 | War | Dogs | NA | Service dog | PTSD: −1.00 (−1.21 to −0.80) | NA |
| Romaniuk (2018) | Pre-post | 42 | 30m/17fc | 26–72, M = 46.46, SD = 12, 46 | War | Horses | EEA facilitators, certified in the Equine Psychotherapy Institute, accompanied by a psychologist | Equine-assisted therapy | PTSD: Couples: −0.61 (−0.91 to −0.32) Individual: −0.79 (−1.14 to −0.44) Depression: Couples −1.04 (−1.42 to −0.65) Individual −1.18 (−1.57 to −0.78) |
PTSD: Couples −0.85 (−1.20 to −0.50) Individual 0.23 (−0.21 to 0.69) Depression: Couples −0.78 (−1.23 to −0.32) Individual 0.30 (−0.27 to 0.87) |
| Schramm (2015) | Pre-post | 6 | NR | 21–64, M = 47.67, SD = 16.06 | Not specified | Sheep | Psychotherapist | Animal-assisted mindfulness training | Depression: −0.10 (−1.72 to −0.27) | NA |
| Shambo (2010) | Pre-post | 6 | 0m/6f | NR (older than 18) | Interpersonal violence | Horses | NR | Equine-facilitated psychotherapy | Depression: −2.94 (−4.66 to −1.22) | PTSD: −3.22 (−4.94 to −1.50) |
| Sheade (2015) | Pre-post | 3 | 3m/1fc | 32–67 | War | Horses | Principal investigator, Licenced Professional Counsellor (LPC) also PATH certified equine specialist | Relational equine-partnered counselling | PTSD: – 1.64 (−3.11 to −0.18) | NA |
| Signal (2013) | Pre-post | 44 | 6m/38f | Children: 8–11, M = 9.8, SD = 1.3 Adolescents: 12–17, M = 15.5, SD = 0.8 Adults: 19–50, M = 37 |
Sexual abuse | Horses | EAGALA counsellors | Equine-facilitated therapy | Depression: Children: −1.82 (−2.53 to −1.11) Youth: −1.31 (−1.85 to −0.76) Adult: −2.19 (−3.05 to −1.33) |
NA |
| Signal (2017) | Pre-post | 20 | 12m/8f | 5–12, M = 8.0, SD = 2.0 | Sexual abuse | Dogs | Dog handler/owner and specialized RSPCA education officer in conjunction with PH staff | Animal-assisted therapy | PTSD: −0.87 (−1.23 to −0.50) | NA |
| Steele (2018) | Pre-post | 85 | 60m/25f | 22–72, M = 42.94, SD = 11.63 | War | Horses | Mental health professional and equine professional | Equine-assisted psychotherapy | PTSD: −0.70 (−0.86 to −0.54) Depression: −0.84 (−1.01 to −0.67) |
NA |
| Vincent (2017) | Pre-post | 15 | 15m/5fc | 31–61+ | War | Dogs | Dog trainers/NA | Service dog | PTSD: −1.10 (−1.59 to −0.61) Depression: −0.74 (−1.13 to −0.35) |
NA |
| Whittlesey-Jerome (2014) | Control | 6 | 0m/13f | 28–64, M = 43.75 | In abusive relationship | Horses | Mental health professional (licenced professional counsellor), or LPC credentialed by EAGALA | Equine-assisted psychotherapy | Depression: −0.37 (−0.84 to −0.09) | NA |
| Woolley (2004) | Control | 11 | 11m/10fc | 11–17 | Abuse, maltreatment | Farm animals | Staff person or volunteer | Animal-assisted therapy | Depression: 0.01 (−0.33 to 0.34) | NA |
N: number of analysed participants in the AAI group; M: mean; SD: standard deviation; SMD: standard mean change, CI: confidence interval; NR: not reported; NA: not applicable; AAI: animal-assisted intervention; anegative values indicate symptom improvement from beginning to end of treatment; bmatching group with no symptoms is not considered as control group, csome studies report gender only for included participants and not for the number of analysed participants.
Table 4.
Characteristics and results of the 13 studies included only in the narrative review
| First author, Publication year | Study design | N analysed (AAI/control) | Gender | Age (range, M, SD) |
Type of experienced trauma | Participating animals | Treatment provider | AAI terminology | Results |
|---|---|---|---|---|---|---|---|---|---|
| Balluerka (2014)a | Control | 46 (21/25) | 32m/14f | 12–17, M = 15.41, SD = 1.65 | Not specified | Dogs, horses, farm animals | Psychologist, specialized in AAT | Animal-assisted psychotherapy | Higher attachment security* after AAI compared to before treatment but no effect on other attachment dimensions; no difference between AAI and control group |
| Balluerka (2015)a | Control | 63 (39/24) | 42m/25fe | 12–17, M = 15.27, SD = 1.63 | Not specified | Dogs, horses, farm animals | Psychologist, specialized in AAT | Animal-assisted psychotherapy | No difference in clinical symptoms between AAI and control; subscale adaptive skills rated by teachers higher* in AAI compared to control but no difference in other subscales |
| Beck (2012) | Control | 24 (12/12) | 17m/7f | AAT: M = 37.08, SD = 11.79 CG: M = 35.5, SD = 9.19 |
War | Dogs | Dog handler | Animal-assisted therapy | No differences in mood, perceived stress, fatigue, functioning, and participation in everyday activities from pre- to post-assessment but decreased psychological function*, higher work performance* and higher quality of interaction*, no differences between AAI and control group. |
| Gehrke (2018) | Pre-post | 17 | NR | NR | War | Horses | Wranglers and counsellors | Equine therapy | Decreased low frequency/high frequency (LF/HF) ratio* in heart rate variability; Improvement in affect* (increase in self-esteem, reduction in irritability and anxiety) |
| Krause-Parello (2014)b | RCT | 42 (19/23) | 2m/40f | 5–14, M = 8.91, SD = 2.33 | Sexual abuse | Dogs | Therapist, dog and its handler | Animal-assisted intervention | Interaction effect* of dog and interview length on alpha amylase; trend of reduced immunoglobulin A with dog; interaction effect* of dog, age of child and interview length on heart rate |
| Krause-Parello (2015)b | RCT | 42 (19/23) | 2m/40f | 5–14, M = 8.91, SD = 2.33 | Sexual abuse | Dogs | Therapist, dog and its handler | Animal-assisted intervention | No differences regarding diastolic and systolic blood pressure and heart rate values for both the intervention and control groups; lower cortisol levels after intervention for control group* but not for AAI; no differences in immunoglobulin A before and after intervention or between AAI and control |
| Krause-Parello (2018) | Control | 25 (25/25) | 21m/4f | 33–86, M = 65.32, SD = 12.26 | War | Dog | Psychologist | Animal-assisted intervention | Therapy dog and psychologist both reduce cortisol and heart rate *; no effect on blood pressure, alpha amylase and immunoglobulin A between before and after control or treatment |
| Kruger (2012) | Pre-post | 15 | 11m/4f | 7–17, M = 11.13, SD = 3.11 | Not specified | Horses | Licenced mental health professionals | Trauma-focused equine-assisted psychotherapy | Decrease in functional impairment* (increase in subscales school behaviour*, home behaviour*, behaviour towards others*, community behaviour* and moods/emotions*; no change in subscales self-harmful behaviour scale and the problem thinking) |
| Miller (2018) | Pre-post | 31 | 31m/0f | 25–66, M = 41.23, SD = 11.86 | Not specified | Dogs | NA | Service animal | Canine presence was not a predictor of reports of nightmares and disturbed dreaming; elevated respiratory event index and lower prior-night sleep respiratory sinus arrhythmia predicted nightmares and disturbed dreams. |
| Murrow (2013) | Pre-post | 9 | 3m/6f | 4–12 | Physical or sexual abuse, domestic violence | Dogs | Therapist (not specified) and researcher (dog handler) | Animal-assisted therapy | Change in behaviour towards dog* (some more, some less approach behaviour towards dog); no change in relationship skills |
| Nevins (2013) | Pre-post | 1 | 1m/0f | 52 | War | Horses | Certified trainer | Intervention (Saratoga WarHorse Connection method) | Reduced PTSD symptomatology (clinically significant); improvements in depression, resilience, life satisfaction and social support |
| Rodriguez (2018)c | Control | 73 (45/28) | 59m/14f | M = 37.08, SD = 7.81 | War | Dogs | NA | Psychiatric service dog | Higher cortisol awakening response*; better health status*; no effect on sleep quality |
| Woodward (2017)d | Pre-post | 18 | 18m/0f | M = 39, SD = 13 | War | Dogs | NA | Service canine | Attenuated attentional bias towards images of aversive emotive scenes* or angry faces* |
| Woodward (2017)d | Pre-post | 23 | 23m/0f | M = 39, SD = 13 | War | Dogs | NA | Service dog | Lower sleep heart rate* and greater morning restedness* in presence of the service dog |
| Wortman (2018) | Pre-post | 1 | NR | NR | War | Seals | Representative from the VMARC (Veteran and Military Affiliated Research Center) | human–animal interaction | Reduced PTSD symptomatology (clinically significant) |
| Yarborough (2017) | Pre-post | 20 | NR | 23–67, M = 42, SD = 12 | War | Dogs | NA | Service dog | Reduced PTSD symptomatology*; improvements in VR-12 mental component summary*; BASIS depression/functioning subscale*; emotional lability subscale*; activity level*; happiness score* and quality of life*; moderate effect sizes for BASIS substance abuse and interpersonal relationships subscales |
| Yorke (2013) | Pre-post | 4 | NR | 8–10 | Not specified | Horses | NR | human–animal interaction | Mild to moderate symmetry between child-horse pairs |
N: number of analysed participants in the study; M: mean; SD: standard deviation; NR: not reported; NA: not applicable; AAI: animal-assisted intervention; AAT: animal-assisted therapy; a,b,dboth publications refer to the same study; csame study as O’Haire et al. (2015); esome studies report gender only for included participants and not for the number of analysed participants; * statistically significant.
Studies with a control-group design reporting PTSD and/or depression outcome were included in the meta-analysis. For all studies reporting pre-post data on PTSD and/or depression measures, we calculated the effect sizes from baseline to the end of treatment and, if applicable, from baseline to follow-up. All additional outcomes are presented narratively.
2.3. Data extraction and quality assessment
All data were independently extracted and coded in duplicate by a team of five researchers (AH, FT, PK, EP and KH) on a standardized form (Microsoft Office Excel 2016) after a training in using the form with descriptive details for coding of each item. Disagreements were resolved by consensus between the two raters who rated the respective study or by contacting a third rater (KH) when no consensus could be found. If study reports included data on healthy participants besides participants with PTSD symptoms, we excluded healthy participants data. We extracted group sizes, means and standard deviations (SDs) for the primary outcomes. We extracted other statistical data that can be converted into means and SDs if one of these values was missing. We calculated missing SDs according to the formulas provided by Lipsey and Wilson (2001), and Higgins and Green (2008). If SDs could not be calculated from the available study information, we imputed them using the SDs reported in the other included studies (Furukawa, Barbui, Cipriani, Brambilla, & Watanabe, 2006). We conducted sensitivity analyses excluding studies in which SDs had to be imputed.
We assessed risk of bias using the NIH Study Quality Assessment Tools (NIH, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools; cited 10.06.2020). This quality assessment tool includes 14 items characterizing studies with a control group and 12 items for studies with a pre-post one-group design. The individual item responses are combined to an overall quality rating for each study according to a predefined algorithm. Two independent raters assessed risk of bias and disagreements were resolved through discussion. When information regarding a certain item was not reported, we assumed the item was not fulfilled.
To characterize the included population, we first coded number of participants, drop-out rate, age and gender. Second, we coded the participant category, type of experienced trauma and if PTSD symptoms or a PTSD diagnosis were confirmed. To characterize the intervention, we recorded the number and length of the treatment sessions. We then extracted the intervention form (group or single), the treatment provider, the treatment label used in the publication (AAI terminology), the included animals and the setting in which the intervention took place. The type of intervention was clustered into ‘animal-assisted intervention’ and ‘receiving a service dog’ in the meta-analysis. With respect to additional aspects of the study, we recorded if the study was published in a peer-reviewed journal, the country in which the study was conducted, the study design, and the year of publication. Results of the meta-analysis are reported according to the PRISMA guidelines (McInnes et al., 2018). Synthesis of the narrative review is presented according to the Synthesis Without Meta-analysis (SWiM) reporting guideline (Campbell et al., 2020).
2.4. Outcome measures
Our prespecified primary outcome measure for the meta-analyses was PTSD symptom severity, assessed via a validated observer-rating or self-rating scale. If more than one trauma scale was used, we selected the most commonly used scale in order to reduce between-study heterogeneity. We included data on depression severity, assessed via a validated observer-rating or self-rating scale for study reports in which PTSD symptom severity was not reported and for study reports which included both outcomes, because PTSD and depression have a high rate of co-occurrence in trauma survivors. In the protocol we had prespecified stress, depression and anxiety as well as treatment acceptability via drop-out rates between the beginning and the end of treatment as secondary outcomes. The number of studies reporting stress and anxiety symptoms was too small to conduct a meta-analysis. However, for the narrative review, we included all reported outcomes.
2.5. Effect sizes
For the continuous outcomes, we calculated the standardized mean difference (SMD) with small sample correction for each study (Lipsey & Wilson, 2001) as effect size of differences between two intervention groups. Corresponding standard errors were calculated for all effect size indicators. In the studies with a one-group design we calculated standardized mean change (SMC) with corresponding 95% confidence intervals (CI) (Lipsey & Wilson, 2001). The magnitude of effect sizes was interpreted as small, moderate, or large, with 0.20, 0.50, and 0.80 SD units, respectively (Cohen, 1988). For the calculation of odds ratios as indicators of treatment acceptability we extracted the number of drop-outs between beginning and end of treatment. If no drop-out rates were reported we used the difference between the number of participants at the beginning of treatment and at the end of treatment.
2.6. Statistical analysis
Random-effects meta-analyses were conducted for all controlled studies. Results are presented as summary SMDs for the relevant pairs of treatments. Whenever possible, measures of uncertainty are reported in the form of the 95% CI. If two interventions were used in a study that differed only with respect to dose or other non-psychological characteristics, we combined the statistical data necessary for effect size calculation according to the recommendations in the Cochrane Handbook of Systematic Reviews (Higgins, Li, & Deeks, 2019).
We explored the presence of a small sample bias and publication bias by assessing funnel plot asymmetry (i.e. whether studies with negative or non-significant results are missing) with a regression test (Egger, Davey Smith, Schneider, & Minder, 1997). To evaluate heterogeneity between studies, we examined τ2, which is an estimate of the variance among true effect sizes. Higher τ2-values indicate greater variability between studies than would be expected by chance. Based on the definition of small, moderate, and large effect size estimates according to Cohen (1988), we interpreted τ2 as follows: τ2 = (0.2/2)2 = 0.01 was considered to represent low heterogeneity, τ2 = (0.5/2)2 = 0.06 moderate heterogeneity, and τ2 = (0.8/2)2 = 0.16 high heterogeneity between studies. In addition, we report I2, which can be interpreted as the percentage of overall heterogeneity that is due to variation of the true effects. An I2-value of 0–40% might not be important, 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity, and 75–100% may represent considerable heterogeneity (Deeks, Higgins, & Altmann, 2019).
Due to a small number of available studies, our analyses deviated from the protocol as we did not calculate an egger test for publication bias and did not conduct subgroup analyses for the intervention setting group vs individual.
All analyses are performed with the software package STATA 13.1 (Harris et al., 2010). We assumed 2-sided P < .05 to indicate statistical significance for all conducted analyses.
3. Results
3.1. Search results
We identified 22,211 records and screened 17,085 titles and abstracts after we had removed duplicates. 208 full-text studies were assessed for eligibility. We finally included 41 studies (Balluerka, Muela, Amiano, & Caldentey, 2015, 2014; Beck et al., 2012; Bergen-Cico et al., 2018; Burton, Qeadan, & Burge, 2019; Craven, 2013; Dietz, Davis, & Pennings, 2012; Earles, Vernon, & Yetz, 2015; Faye, 2003; Gehrke, Noquez, Ranke, & Myers, 2018; Gómez, 2016; Hamama et al., 2011; Johnson et al., 2018; Kemp, Signal, Botros, Taylor, & Prentice, 2014; Kloep, Hunter, & Kertz, 2017; Krause-Parello & Friedmann, 2014; Krause-Parello & Gulick, 2015; Krause-Parello, Levy, Holman, & Kolassa, 2018; Kruger, 2012; Lanning & Krenek, 2013; Lanning, Wilson, Krenek, & Beaujean, 2017; Malinowski et al., 2018; McCullough, 2011; McCullough, Risley-Curtiss, & Rorke, 2015; Miller, Jamison, Gala, & Woodward, 2018; Mueller & McCullough, 2017; Murrow, 2013; Naste et al., 2018; Nevins, Finch, Hickling, & Barnett, 2013; O’Haire & Rodriguez, 2018; Rodriguez, Bryce, Granger, & O’Haire, 2018; Romaniuk, Evans, & Kidd, 2018; Schramm, Hediger, & Lang, 2015; Shambo, Seely, & Vonderfecht, 2010; Sheade, 2015; Signal, Taylor, Botros, Prentice, & Lazarus, 2013; Signal, Taylor, Prentice, McDade, & Burke, 2017; Steele, Wood, Usadi, & Applegarth, 2018; Vincent et al., 2017; Whittlesey-Jerome, 2014; Woodward, Jamison, Gala, & Holmes, 2017; Woodwart, Jamison, Gala, & Arsenault, 2017; Woolley, 2004; Wortman et al., 2018; Yarborough et al., 2017; Yorke et al., 2013) (see Figure 1) that were published in 46 reports with 1111 analysed participants. The meta-analysis included eight controlled studies with 469 participants.
3.2. Descriptives of the 41 included studies
From 41 studies that were published in 46 reports, 38 consisted of articles published in a peer-reviewed journal and eight were unpublished studies. The study characteristics are summarized in Tables 1, 3, 4 and reported in detail in the supplementary material (Table A2). The majority (N = 32) of studies were conducted in the USA, one in Canada, four were conducted in Australia, three in Europe (with additional data from Honduras), and one in Israel. The included studies were published between 2003 and 2018. The number of published studies increased considerably over the last decade, with 20 studies published between 2017 and 2018, and only three studies published before 2010. The majority of the 41 studies had a pre-post one-group design (N = 28) whereas eight of the studies had a control group and two out of these were randomized controlled studies. These eight studies qualified for inclusion in the meta-analysis with five studies qualifying for post-post analyses comparing the effects of animal-assisted treatment versus standard PTSD psychotherapy and one study comparing AAI with waitlist. In the waitlist controlled study, the participants of the waitlist were provided AAI after the initial study period had ended, and these participants were then added to the initial treatment group for analyses, thus violating the requirement of independence between treatment and control group (Johnson et al., 2018). In two controlled studies, getting a service dog was compared with waiting for a service dog (Bergen-Cico et al., 2018; O’Haire & Rodriguez, 2018). For the 20 studies with PTSD and/or depression outcomes at the beginning and end of treatment, we calculated symptom change between beginning and end of treatment as effect sizes. Five studies had a follow-up measurement with a mean of 13 weeks.
Table 1.
Characteristics and results of the 8 included controlled studies on PTSD symptom or depression severity
| First author, Publication year | Study design | N analysed (AAI/control) | Gender | Age (range, M, SD) | Type of experienced trauma | Participating animals | Treatment provider | AAI terminology | Control intervention | Co-treatment | SMD (95% CI) at end of treatmenta |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bergen-Cico (2018) | Control | 48 (34/14) | NR | M = 42, SD = 11.5 | War | Dogs | Dog trainer | Therapeutic dog ownership and training | Waiting for service dog and engaging in social programmes (volunteering in a peer support programme) | NR | PTSD: −0.33 (−0.97 to 0.30) |
| Burton (2019) | Control | 20 (11/9) | 16m/4f | 33–63, M = 47, SD = 14 | War | Horses | Occupational therapist, EAGALA-certified with professional horse handler | Equine- assisted psychotherapy |
Ongoing PTSD therapy | Ongoing PTSD therapy | PTSD: −0.33 (−1.22 to 0.55) |
| Dietz (2012) | Control | 153 (121/32) | 10m/143f | 7–17 | Sexual abuse | Dogs | Licenced and master’s level clinicians (social work, trained psychologists, counselling) | Animal-assisted therapy | Group PTSD therapy | NR | PTSD: −0.31 (−0.70 to 0.08) |
| Johnson (2018) | RCT | 19 (19/13) |
32m/6fb | 29–73, M = 54.35, SD = 12.85 | War | Horses | Occupational therapists and PATH-certified riding instructors | Therapeutic horseback riding | Waitlist | NR | PTSD: −0.82 (−1.56 to −0.08) |
| Mueller (2017) | Control | 54 (25/29) | 45m/9f | 10–18 | Physical, sexual, emotional abuse and neglect | Horses | Licenced clinical social worker | Equine-facilitated psychotherapy | Continuation with trauma-focused cognitive behavioural therapy | NR | PTSD: −0.14 (−0.67 to 0.40) |
| O’Haire (2018) | Control | 141 (75/66) | 110m/31f | M = 37.1, SD = 8.3 | War | Dogs | NA | Service dog | Waiting for service dog; ongoing usual care | Unrestricted access to usual care | PTSD: −0.65 (−0.99 to −0.31) |
| Whittlesey-Jerome (2014) | Control | 13 (6/7) | 0m/13f | 28–64, M = 43.75 | In abusive relationship | Horses | Mental health professional or licenced professional counsellor credentialed by EAGALA | Equine-assisted psychotherapy | Ongoing regular traditional group therapy | Regular traditional group therapy | Depression: −0.32 (−1.42 to 0.78) |
| Woolley (2004) | Control | 21 (11/10) | 11m/10f | 11–17 | Abuse, maltreatment | Farm animals | Staff person or volunteer | Animal-assisted therapy | Conventional psychotherapy | Conventionalpsychotherapy | Depression: −0.03 (−0.88 to 0.83) |
N: number of analysed participants in the study; M: mean; SD: standard deviation; SMD: standard mean difference, CI: confidence interval; NR: not reported; m: male; f: female; NA: not applicable; AAI: animal-assisted intervention; RCT: randomized controlled trial; PTSD: post-traumatic stress disorder; EAGALA: equine-assisted growth and learning association; PATH: Professional Association of Therapeutic Horsemanship; anegative values indicate superiority of AAI over the comparator; bsome studies report gender only for included participants and not for the number of analysed participants.
3.2.1. Characteristics of participants
The number of analysed participants across all 41 studies ranged between 153 and one (in the narrative review) with a median of 17 (see Tables 1, 3, 4 and A3). The attrition rate across all studies varied between 0% and 75%. 18 of the studies had an attrition rate of 0% while eight studies reported attrition rates higher than 20%. Participants’ age across all studies ranged between 4 and 86 years with 15 studies focusing on children and adolescents (one of them also including adults) and 26 on adults. In 23 studies, the adult populations were veterans (including active duty service members in one study). Gender was weighted to male participants with 54% of the total analysed participants in all 41 studies (six studies did not report the gender of participants, four of them addressing veterans).
The most often examined type of trauma experienced by participants was war in 22 studies (in one study war combined with sexual abuse). In nine studies, the experienced traumas consisted of physical abuse, sexual abuse, neglect or other form of interpersonal violence while four studies investigated sexual abuse. One study included participants who experienced different traumas (interpersonal or accidental traumas mixed), while one study included participants who experienced accidental nature-based trauma. The authors of five studies did not specify the experienced trauma of the participants. In 31 of the studies, PTSD symptoms or a PTSD diagnosis of the participants was confirmed by a standardized method, while 10 studies only reported that the participants experienced a trauma and succinct posttraumatic symptoms.
3.2.2. Characteristics of AAI
Authors of 20 studies investigated interventions run in an individual format, authors of 19 studies utilized a group format and authors of two studies used a combined approach of group and individual sessions (see Tables 1, 3, 4 and Table A4). Authors of two studies did not specify the format of the program. Intervention duration ranged between four days and up to 15 months with one study that combined a three-week intervention with placement of dogs up to four years. The average duration of the intervention was 10 weeks. Participants received between one and 60 intervention sessions. The average number of sessions for interventions in all studies was 10. The length of one such session ranged between 15 minutes and two days with an overnight stay, while the average duration length (without the outlier of two days) was 90 minutes.
In most studies, interventions were run by psychologists/psychotherapists/mental health professionals (10 studies), four studies had interventions provided by counsellors. Two studies included social workers, psychologists as well as counsellors, three studies had occupational therapists as treatment providers, three used volunteers, two had dog trainers, two had dog handlers, and in one study the intervention was provided by a recreation therapist. In four studies, these providers were EAGALA certified, in three studies they were certified by PATH International, and two studies had other certifications as AAI specialist. The authors of seven studies did not specify the person providing the treatment. In four studies, the persons had an unclear background and were called therapist, trainer, and in one study the persons were indicated as a representative from a centre.
AAI terminology ranged broadly. Most studies used equine-assisted psychotherapy or equine-facilitated psychotherapy (nine studies), eight studies used equine-assisted or equine-facilitated therapy while, two used equine therapy and in two studies the terminology therapeutic horseback riding was used. Five studies used animal-assisted therapy, one study used the more specific terminology dog-assisted therapy (Hamama et al., 2011) and two used the broader terminology animal-assisted intervention. Two studies used human–animal interaction as terminology.
The majority of the studies included horses (22 studies) while 14 studies included dogs and one study had both dogs and horses as animals. One study investigated the effect of interventions with seals (Wortman et al., 2018), one with different farm animals (Woolley, 2004), one with dolphins (Faye, 2003) and one with sheep (Schramm et al., 2015).
Most treatments were provided at a treatment or a therapy centre (10 studies). In other studies, the intervention took place at a riding centre (seven studies), at a farm (five studies) or at a ranch (four studies). Other settings were at participants’ homes (three studies), in an aquarium (two studies), a school (one study) (Hamama et al., 2011), a training site (one study) (Kloep et al., 2017), a shelter (one study) (Signal et al., 2017), a hospital (one study) (Krause-Parello et al., 2018) or a lab (one study) (Woodwart et al., 2017). Authors of five studies did not specify the setting in which the intervention took place.
3.2.3. Study quality
The quality of the 41 studies included in the systematic review indicated a high risk of bias with 28 studies rated poor and 13 studies rated fair while no study was rated with good quality.
3.3. Main results for controlled studies
3.3.1. PTSD symptom severity
Authors of three studies investigated the effect of AAI compared to standard PTSD psychotherapy on PTSD symptom severity (Burton et al., 2019; Dietz et al., 2012; Mueller & McCullough, 2017). The results indicate somewhat lower symptom severity in the AAI group at baseline, which was mainly explained by one study (Mueller & McCullough, 2017) and not statistically significant overall (see Table 2 and Appendix 3, Table A5). All three studies indicated small and statistically non-significant superiority of AAI over standard PTSD psychotherapy at the end of treatment in reducing PTSD symptom severity.
Table 2.
Main results for AAI compared with standard PTSD psychotherapy or waitlist at baseline and at the end of treatment
| Treatment effects Comparison & outcome | Number of comparisons | Group difference SMD (95% CI) |
P-value for group difference | Heterogeneity (I2) | Tau2 | P-value for heterogeneity |
|---|---|---|---|---|---|---|
| AAI vs. standard PTSD psychotherapy: PTSD symptom severity | ||||||
| Baseline | 3 | −0.16 (−0.60 to 0.28) | 0.479 | 50.6% | 0.1 | 0.132 |
| End of treatment | 3 | −0.26 (−0.56 to 0.04) | 0.087 | 00.0% | 0.0 | 0.865 |
| AAI vs. waitlist: PTSD symptom severity | ||||||
| Baseline | 1 | −0.04 (−0.68 to 0.60) | 0.900 | NA | NA | NA |
| End of treatment | 1 | −0.82 (−1.56 to −0.98) | 0.029 | NA | NA | NA |
| AAI vs. standard PTSD psychotherapy: depression | ||||||
| Baseline | 2 | −0.48 (−1.16 to 0.19) | 0.162 | 00.0% | 0.0 | 0.875 |
| End of treatment | 2 | −0.14 (−0.82 to 0.54) | 0.687 | 00.0% | 0.0 | 0.677 |
| Sensitivity analysis Baseline | 1 | −0.53 (−1.40 to 0.35) | 0.238 | NA | NA | NA |
| Sensitivity analysis end of treatment | 1 | −0.03 (−0.88 to 0.83) | 0.951 | NA | NA | NA |
| Getting service dog vs. waiting for service dog: PTSD symptom severity | ||||||
| Baseline | 2 | −0.08 (−0.38 to 0.21) | 0.572 | 00.0% | 0.0 | 0.934 |
| End of treatment | 2 | −0.58 (−0.88 to −0.28) | < 0.001 | 00.0% | 0.0 | 0.390 |
|
Drop-outs Comparison |
||||||
| AAI vs. standard PTSD psychotherapy | 5 | 1.99 (0.46 to 8.55) | 0.1354 | 22.8% | 0.67 | 0.269 |
| AAI vs. waitlist | 1 | 10.8 (1.16 to 100.43) | 0.036 | NA | NA | NA |
| Getting service dog vs. waiting for service dog | 2 | 3.14 (0.35 to 28.46) | 0.310 | 00.0% | 0.0 | 0.904 |
AAI: animal-assisted intervention; N: number of included studies; SMD: standard mean difference, OR: odds ratio.
One study investigated the effect of AAI compared to waitlist on PTSD symptom severity (Johnson et al., 2018). At baseline, there was no significant difference, but a large SMD at the end of treatment indicates the superiority of AAI over waitlist.
Authors of two studies investigated the effect of getting a service dog and training the dog compared to waiting for a service dog on PTSD symptom severity (Bergen-Cico et al., 2018; O’Haire & Rodriguez, 2018). In one study, participants in the waitlist group engaged in social programmes (Bergen-Cico et al., 2018) while in the other study, participants in both groups had access to usual care (O’Haire & Rodriguez, 2018). The result revealed no significant difference between the two groups at baseline but a significant superiority of getting a service dog over waiting for a service dog at the end of treatment with a moderate effect size.
3.3.2. Depression severity
Authors of two studies investigated the effect of AAI compared to standard PTSD psychotherapy on depression severity (Whittlesey-Jerome, 2014; Woolley, 2004). The results indicate considerably, but statistically non-significant lower depression scores in AAI as compared with standard PTSD treatment at baseline. At the end of treatment, there was a small and non-significant superiority of AAI over standard PTSD psychotherapy (see Table 2; Appendix 3, Table A5).
3.3.3. Sensitivity analyses
When we excluded the study in which we had to impute the SDs from the analyses regarding depression severity as outcome (Whittlesey-Jerome, 2014), the remaining study showed considerably lower depression values in the AAI group compared to the standard PTSD psychotherapy group at baseline (Woolley, 2004). No difference between AAI and standard PTSD psychotherapy was found at the end of treatment (see Table 2).
3.3.4. Drop-outs
The number of participants who dropped out from AAI compared with PTSD psychotherapy did not differ significantly. In one study, significantly more participants dropped out of AAI compared with waitlist (Johnson et al., 2018). The number of drop-outs did not differ significantly between getting a service dog and waiting for a service dog.
3.3.5. Publication Bias
Because there were too few studies included in our meta-analysis, we did not test statistically for funnel plot asymmetry. However, visual inspection of the funnel plot suggests some asymmetry indicating the risk of publication or reporting bias (see Appendix 3, Figure A1).
3.4. Main results for pre- versus post effects
3.4.1. PTSD symptom severity
The change in PTSD symptom severity between baseline and end of treatment of AAI was reported in 20 studies (Burton et al., 2019; Craven, 2013; Dietz et al., 2012; Earles et al., 2015; Faye, 2003; Gómez, 2016; Hamama et al., 2011; Johnson et al., 2017; Kemp et al., 2014; Kloep et al., 2017; Lanning et al., 2017; Malinowski et al., 2018; McCullough, 2011; Mueller & McCullough, 2017; Naste et al., 2018; Romaniuk et al., 2018; Sheade, 2015; Signal et al., 2017; Steele et al., 2018). There is a large variability of effect sizes between different studies ranging from −0.38 to −1.64 (see Table 3).
The change in PTSD symptom severity after getting a service dog was reported in three studies with effect sizes ranging from −0.43 to −1.10 (Bergen-Cico et al., 2018; O’Haire & Rodriguez, 2018; Vincent et al., 2017) (see Table 3).
3.4.2. Depression severity
12 studies reported change in depression symptom severity between baseline and end of treatment of AAI with also a broad variability of effect sizes ranging from 0.01 to −2.76 (Earles et al., 2015; Hamama et al., 2011; Kemp et al., 2014; Kloep et al., 2017; Lanning et al., 2017; Romaniuk et al., 2018; Schramm et al., 2015; Shambo et al., 2010; Signal et al., 2013; Steele, Steele, & Fonagy, 1996; Whittlesey-Jerome, 2014; Woolley, 2004) (see Table 3).
One study reported change in depression symptom severity between baseline and end of treatment after getting a service dog indicating a medium effect size of −0.74 (Vincent et al., 2017) (see Table 3).
3.5. Main results for pre- versus follow-up effects
3.5.1. PTSD symptom severity
Four studies reported change in PTSD symptom severity between baseline and follow-up of AAI (Gómez, 2016; Kloep et al., 2017; Lanning et al., 2017; Romaniuk et al., 2018) with effect sizes ranging between 0.24 and −3.92 (see Table 3).
3.5.2. Depression severity
Two studies reported change in depression symptom severity between baseline and follow-up of AAI with effect sizes of individual studies ranging between 0.30 and −3.22 (Romaniuk et al., 2018; Shambo et al., 2010) (see Table 3).
3.6. Additional outcomes
The 13 studies included in the narrative review were published in 17 articles (one of them included in the meta-analysis (O’Haire & Rodriguez, 2018)) (see Table 4). Authors of three of these studies defined PTSD symptomatology as the primary outcome measured via one of the PTSD checklist (PCL) versions. All of these studies had a pre-post one-group design but did not meet our criteria for effect-size calculation. One study found a statistically significant reduction in the PTSD symptoms (d = −0.98) after getting a service dog (Yarborough et al., 2017), and two studies with only one participant reported a clinically significant decrease of PTSD symptoms (Nevins et al., 2013; Wortman et al., 2018). Authors of five studies measured stress via physiological parameters. Different parameters were used, and results were mixed regarding blood pressure, heart rate, cortisol, salivary alpha-amylase and immunoglobulin A. While getting a service dog might be associated with a significant higher cortisol awakening reaction as well as a significantly better health status compared to waiting for a service dog, it did not influence sleep quality (Rodriguez et al., 2018).
Several studies looked at different psychological outcomes. Most outcome measures were used in only one of all studies and the results varied widely. While AAI had positive effects on attachment security (Balluerka et al., 2014) and functional impairment (Kruger, 2012), no effects were found regarding psychosocial adaption, school maladjustment and behavioural symptoms (Balluerka et al., 2015), mood, resilience, fatigue, and daily functioning compared to the control intervention (Beck et al., 2012). Results on effects of a service dog on sleep quality were also mixed (Miller et al., 2018; Woodwart et al., 2017).
4. Discussion
4.1. Main findings
Our evaluation of the effectiveness of AAI regarding the reduction of PTSD and depression symptoms in people with PTSD symptoms was based on a small number of controlled studies and we identified only two randomized controlled trials on the effectiveness of AAI. Our meta-analysis reveals a small but not statistically significant superiority of AAI, which adds interaction with an animal to standard PTSD psychotherapy, over standard psychotherapy on PTSD symptom severity at the end of treatment. We identified one study in which AAI was compared with a waitlist control. Here AAI was statistically superior over waiting for AAI with a large effect size in reducing PTSD symptomatology (Johnson et al., 2018). Moreover, a significant superiority was found for getting a service dog and training the dog combined with standard care over waiting for a service dog combined with standard care at the end of treatment with a moderate effect size in reducing PTSD symptomatology.
The effect sizes of the individual studies for pre-post comparisons range broadly between small and large effects. We observed symptom improvement during the course of AAI from the beginning to the end of treatment, which continues to be maintained to longer-term follow-up with a mean of 13 weeks. Importantly, the lack of a control group in these studies does not allow to differentiate the observed symptom improvement from spontaneous remission. Accordingly, these studies do not allow to draw conclusions about the magnitude of the symptom improvement that can specifically be attributed to the AAI effect. One study seems to suggest adverse effects with the PTSD symptomatology at the end of treatment being even higher than the pre-intervention levels (Romaniuk et al., 2018). There was also large variability in pre-post effect sizes for studies investigating the effect of getting a service dog ranging from small to large. Together, these results suggest that AAI can be effective in reducing PTSD symptoms but is not superior to standard PTSD psychotherapy.
We found a small and non-significant superiority of AAI over standard PTSD psychotherapy at the end of treatment on depression symptom severity in controlled studies. There was a large variation of effect sizes for different studies from small to large effects for pre-post comparisons. Only one study investigated the effect of getting a service dog on depression symptom severity between baseline and end of treatment, and found a medium effect (Vincent et al., 2017). Together, these results suggest that AAI can be effective in reducing depression for people with PTSD symptoms but is not superior to standard PTSD psychotherapy.
Regarding additional outcome domains we found mixed evidence in most included studies, with some indication for beneficial effects regarding other psychological and physiological variables but in many cases, no specific benefits were documented. The results of the narrative review revealed that positive effects comprised effects such as significant higher attachment security, better adaptive skills, health status, affect as well as physiological outcomes such as significantly lowered heart rate and cortisol levels and higher heart rate variability. However, there were inconsistencies within physiological outcomes with inconclusive results or studies reporting no effects on blood pressure, alpha amylase and immunoglobulin A. Also, no effects were found on mood, resilience, fatigue, daily functioning, sleep quality, nightmares and relationship skills. None of the studies included in the narrative review reported adverse results.
All these results suggest that AAI can be effective in contributing to symptom improvement in people who experienced trauma and suffer from PTSD symptoms. AAI seems to be superior to waiting for a treatment and is as effective as standard psychotherapeutic interventions for PTSD. However, AAI is not superior to standard PTSD psychotherapy.
A relevant finding of our systematic review with meta-analysis was the observation of predominantly low quality of research in this comparably young field of research with most studies being published within the last decade. Main problems were the lack of control interventions, baseline differences in controlled studies, low numbers of participants and a high risk for publication bias.
4.2. Relation to previous research findings
Our results are largely consistent with a previous meta-analysis also showing that animal-assisted psychotherapy is efficacious in decreasing PTSD symptoms in patients who experienced trauma (Germain et al., 2018). However, Germain et al. (2018) found a small to moderate superiority of animal-assisted psychotherapy over other interventions in two studies that we could not replicate based on data of three included studies. Moreover, the authors conducted a meta-analysis on pre-post comparisons indicating a large effect size while stating in parallel that the differences found in the pre-post comparisons might be due to threats to internal validity (Germain et al., 2018). The latter statement is in line with our findings and confirms our decision not to calculate a mean effect size for comparisons from the beginning to end of AAI treatment.
Germain et al. (2018) discussed that animal-assisted psychotherapy might produce smaller attrition rates than would be predicted based on drop-out rates from trauma-focusing treatments. In our analyses, five studies looking at PTSD measures indicated that a non-significantly higher number of participants dropped out of AAI compared to standard PTSD psychotherapy and compared to waitlist based on one study. Also, the number of drop-outs did not differ significantly between getting a service dog and waiting for a service dog. Thus, the acceptability of AAI compared to standard PTSD psychotherapy seems to be equivalent.
4.3. Implications
The majority of the included participants in this systematic review experienced severe and interpersonal traumas, mostly war or otherwise physical or sexual abuse. Approximately half of the interventions were run in a group format whereas the other half used an individual format. Intervention sessions ranged from one single session (Krause-Parello & Friedmann, 2014; Krause-Parello & Gulick, 2015; Krause-Parello et al., 2018) to 60 sessions (Bergen-Cico et al., 2018) with an average intervention duration of 10 weeks. All studies included an animal in a specific form with the goal of improving a broad range of symptomatology of participants with PTSD. Dogs and horses were the most common animal species. As already noted by O’Haire and colleagues (O’Haire et al., 2015), authors of most studies provide limited information about the person delivering the intervention and their training and experience with AAI. Although we did not select for specific forms of AAI, most interventions were run by psychologists/psychotherapists/mental health professionals. This might reflect the process that AAI is more and more acknowledged by the professional field and that guidelines for quality control are being developed and enforced (Enders-Slegers, Hediger, Beetz, Jegatheesan, & Turner, 2019; Simonato, De Santis, Contalbrigo, Benedetti, & Finocchi Mahne, 2018). For clinical practice, these results suggest that AAI can be as effective as standard PTSD psychotherapy and that there can be different forms of conducting AAI. However, it is not yet clear in what way AAI should be conducted to be most effective as this might highly depend on the circumstances of a programme and the patients involved. For example, some patients might prefer working with horses over dogs or vice versa depending on their biographical experiences. Such factors must be taken into account when considering AAI and should be given more attention in future research.
4.4. Strengths and limitations
We included different forms of AAI and did not restrict them to psychotherapeutic interventions as Germain et al. (2018) did. To increase comparability, we clustered them into ‘animal-assisted intervention’ versus ‘receiving a service dog’. This ensures that approaches with similar components that are applied in practice are also included in our systematic review, and thus increasing external validity, while taking into account the internal validity as different AAI forms are considered separately. In order to minimize publication bias, we also included non-peer reviewed manuscripts albeit the study quality was sometimes low. We also calculated effect sizes for comparisons between pre- and follow-up outcome measurement. However, the number of studies with follow-up measurements is small and one study (Faye, 2003) had to be excluded as it reported to have a follow-up of three individuals at 28 weeks but did not present any data. This example underlines the fact that adherence to standard guidelines for study conduct and reporting is rather low in this field, as Germain et al. (2018) already stated. For most of the studies, detailed information regarding the study design, methodology or the intervention itself was missing. It is important to know in what way the animal was integrated (animal just being present, animal embedded in a therapeutic narrative, amount of physical contact or even riding if horses were present) as this is an important aspect of the intervention and needs to be systematically investigated rather than the presence of an animal itself (Lopez-Cepero, 2020). For example, the study by Dietz and colleagues revealed greater positive outcomes when a dog was integrated into the intervention via using therapeutic stories about the dog compared to the dog just being present during the intervention (Dietz et al., 2012). Detailed information would also help to better categorize interventions and combine or compare it with appropriate studies. There is a high variety regarding participants and even more in programme characteristics. Although Germain and colleagues found that length of the treatment, group or individual setting and the involved animal species do not appear to moderate the effect (Germain et al., 2018), it seems necessary to increase the number of studies with a high-quality design to compare specific treatment aspects such as the format (group or individual), amount of contact and type of activity with the animal. The current data basis does not allow for conclusive analyses of such predictors. Future studies should use replicable protocols and describe procedures in detail. As already noted by O’Haire et al. (2015), AAI for patients with PTSD is not yet clearly defined.
Although this meta-analysis includes a higher number of studies compared to a previous one (Germain et al., 2018), there are still relatively few studies investigating the effects of AAI in people with PTSD, especially when it comes to studies using a control group. The quality of the existing studies is mostly low with baseline differences in controlled studies, small numbers of participants and the analyses suggest the presence of publication bias. Results must therefore be interpreted with caution and there is a clear need for more quantitative studies with a high-quality study design that evaluate an increasing practice. Most studies used pre-post measurements without control and some of them reported large effect sizes. It is crucial to conduct at least two or three, preferably multi-centre, randomized controlled trials with a large population to test if these effects can be reproduced.
4.5. Future research directions
In most studies, AAI was combined with standard care and participants continued with the treatment they already had at study start which included medications or other active psychotherapeutic interventions. The results of these studies only allow measurement of the impact of the intervention as a whole but not the individual effect of its components, e.g. the effect of the human–animal contact, the effect of the psychotherapeutic intervention, or the interaction of both (Lopez-Cepero, 2020). Accordingly, the selection of an appropriate control group for future research is crucial. For example, Dietz et al. (2012) used the same protocol for the standard PTSD psychotherapy group as for the AAI groups. Such an approach allows not only to determine the effect of an AAI programme but also to draw hypotheses about the specific effects of an animal and the way an animal is integrated into treatment. It is important to note, however, that comparative studies which include comparisons between two alternative treatments require large sample sizes because the expected effect sizes between treatment groups are expected to be small (Schnurr, 2007). None of the included studies which used a comparative study design used an adequately sized sample, which decreases the chance of detecting small differences between treatment effects on the one hand, and on the other hand increases the chance that the observed findings are invalid (Cuijpers, 2016).
This review and meta-analysis focused on symptomatology while there is still a lack of knowledge about other possible outcomes of AAI. It is often hypothesized that animals can facilitate contact between therapists and patients (Julius, Beetz, Kotrschal, Turner, & Uvnäs-Moberg, 2013; Schneider & Harley, 2006). The fact that animals are less evaluative than humans, that they communicate non-verbally, that they offer opportunities to provide caregiving, or to experience physical closeness are discussed as mechanisms for explaining why some patients find it easier to establish a relationship with an animal than an unfamiliar therapist (Amerine & Hubbard, 2016; Julius et al., 2013). For future studies it might be interesting to see if those characteristics of AAI could be a specific advantage in involving patients that cannot easily be reached by other conventional interventions for trauma. The question of whether efficacy of AAI on average is equivalent to standard PTSD psychotherapy is crucial since AAI is usually more complicated, can be more expensive, and also has to take into account the ethical dimensions of ‘using’ animals. Therefore, future research should evaluate potential predictors determining for which patients conventional therapeutic approaches might be more suitable and for whom AAI might be more effective. The current literature basis suggests the hypothesis that interacting with an animal might help patients with PTSD to not refrain from avoiding unpleasant aspects of a trauma therapy (Germain et al., 2018). This highlights the importance of including measures such as therapy motivation, therapeutic relationship, adherence and drop-out rates in future trials.
The currently available evidence can be considered an important starting point which, despite the low quality of evidence, suggests that AAI has comparable effects to standard PTSD psychotherapy. Future research should move forward and focus on investigating for whom the addition of animals to the standard treatment protocols offers unique opportunities for treatment success and symptom improvement. For the establishment of AAI as evidence-based treatment, the field should essentially improve the quality of studies by following important available recommendations (Cuijpers, 2016; Schnurr, 2007).
5. Conclusion
AAIs seem to be efficacious in reducing PTSD symptomatology and depression for people with PTSD symptoms. AAIs lead to comparable effects to standard PTSD psychotherapy for people with PTSD symptoms and is superior to waiting for AAI. The quality of the included studies is rather low with baseline differences in controlled studies as well as low numbers of participants and a high risk for publication bias as the most important aspects. There is considerable heterogeneity between the studies with a pre-post design, which may be explained by the low quality of these studies or by the presence of true differences between treatment effects in sub-samples of people with PTSD symptoms. This highlights a strong need for future studies with robust study designs to quantify the effect of AAI. Future high-quality studies are needed to investigate potential moderators of the observed differences between AAI and standard PTSD psychotherapy with a specific focus on identifying individuals who particularly benefit from AAI but not from standard treatments.
Supplementary Material
Acknowledgments
We thank Andreas Ledl for his support with the systematic literature search and for creating the search strings.
Funding Statement
This work was supported by the Swiss National Science Foundation under the Ambizione grant to Karin Hediger (grant PZ00P1_174082).
Authors’ contributions
KH conceptualized and designed the project, screened records, extracted, analyzed and interpreted data and wrote the first draft of the manuscript. JW, PK, AH, FT, CG and EP were involved in screening the records, extracting and preparing the data as well as preparing the manuscript. HG conducted statistical analysis and participated in writing the manuscript. All authors contributed to and have approved the final manuscript.
Data availability statement
The data that support the findings of this study are openly available from the Dataverse database at: https://doi.org/10.7910/DVN/MAJSJZ
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Amerine, J. L., & Hubbard, G. B. (2016). Using Animal-assisted Therapy to Enrich Psychotherapy. Advances in Mind-body Medicine, 30(3), 11–21. [PubMed] [Google Scholar]
- Balluerka, N., Muela, A., Amiano, N., & Caldentey, M. A. (2014). Influence of animal-assisted therapy (AAT) on the attachment representations of youth in residential care. Children and Youth Services Review, 42(C), 103–109. doi: 10.1016/j.childyouth.2014.04.007. [DOI] [Google Scholar]
- Balluerka, N., Muela, A., Amiano, N., & Caldentey, M. A. (2015). Promoting psychosocial adaptation of youths in residential care through animal-assisted psychotherapy. Child Abuse & Neglect, 50, 193–205. doi: 10.1016/j.chiabu.2015.09.004. [DOI] [PubMed] [Google Scholar]
- Beck, C. E., Gonzales, F., Jr., Sells, C. H., Jones, C., Reer, T., & Zhu, Y. Y. (2012, April–June). The effects of animal-assisted therapy on wounded warriors in an Occupational Therapy Life Skills program. U.S. Army Medical Department Journal, 38–45. [PubMed]
- Bergen-Cico, D., Smith, Y., Wolford, K., Gooley, C., Hannon, K., Woodruff, R., … Gump, B. (2018). Dog ownership and training reduces post-traumatic stress symptoms and increases self-compassion among veterans: Results of a longitudinal control study. Journal of Alternative and Complementary Medicine, 24(12), 1166–1175. doi: 10.1089/acm.2018.0179. [DOI] [PubMed] [Google Scholar]
- Burton, L. E., Qeadan, F., & Burge, M. R. (2019). Efficacy of equine-assisted psychotherapy in veterans with posttraumatic stress disorder. Journal of Integrative Medicine, 17(1), 14–19. doi: 10.1016/j.joim.2018.11.001. [DOI] [PubMed] [Google Scholar]
- Campbell, M., McKenzie, J. E., Sowden, A., Katikireddi, S. V., Brennan, S. E., Ellis, S., … Thomson, H. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ, 368, l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charry-Sanchez, J. D., Pradilla, I., & Talero-Gutierrez, C. (2018). Animal-assisted therapy in adults: A systematic review. Complementary Therapies in Clinical Practice, 32, 169–180. doi: 10.1016/j.ctcp.2018.06.011. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: Lawrence Erlbaum Associates. [Google Scholar]
- Craven, M. B. (2013). Effectiveness of equine assisted psychotherapy in the treatment of veterans with posttraumatic stress disorder [Dissertation]. Texas A&M University, College Station. [Google Scholar]
- Cuijpers, P. (2016). The future of psychotherapy research: Stop the waste and focus on issues that matter. Epidemiology and Psychiatric Sciences, 25(4), 291–294. doi: 10.1017/S2045796015000785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks, J. J., Higgins, J. P. T., & Altmann, D. G. (2019). Analysing data and undertaking meta-analyses. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions. (Version 6.0) (pp. 241–284). Chichester, UK: John Wiley & Sons. [Google Scholar]
- Dietz, T. J., Davis, D., & Pennings, J. (2012). Evaluating animal-assisted therapy in group treatment for child sexual abuse. Journal of Child Sexual Abuse, 21(6), 665–683. doi: 10.1080/10538712.2012.726700. [DOI] [PubMed] [Google Scholar]
- Earles, J. L., Vernon, L. L., & Yetz, J. P. (2015). Equine-assisted therapy for anxiety and posttraumatic stress symptoms. Journal of Traumatic Stress, 28(2), 149–152. doi: 10.1002/jts.21990. [DOI] [PubMed] [Google Scholar]
- Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders-Slegers, M. J., Hediger, K., Beetz, A., Jegatheesan, B., & Turner, D. C. (2019). Animal-assisted interventions in an international perspective: Trends, research, and practices. In Fine A. H. (Ed.), Handbook on animal-assisted therapy. Foundations and guidelines for animal-assisted interventions (5th ed., pp. 465–477). London: Elsevier. [Google Scholar]
- Faye, E. (2003). The effects of dolphin interactions with children diagnosed with posttraumatic stress disorder (PTSD). Chicago, IL: Faculty of The Chicago School of Professional Psychology. [Google Scholar]
- Furukawa, T. A., Barbui, C., Cipriani, A., Brambilla, P., & Watanabe, N. (2006). Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology, 59(1), 7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Gehrke, E. K., Noquez, A. E., Ranke, P. L., & Myers, M. P. (2018). Measuring the psychophysiological changes in combat Veterans participating in an equine therapy program. Journal of Military, Veteran and Family Health, 4(1), 60–69. doi: 10.3138/jmvfh.2017-0015. [DOI] [Google Scholar]
- Germain, S. M., Wilkie, K. D., Milbourne, V. M. K., & Theule, J. (2018). Animal-assisted psychotherapy and trauma: A meta-analysis. Anthrozoös, 31(2), 141–164. doi: 10.1080/08927936.2018.1434044. [DOI] [Google Scholar]
- Gómez, I. B. (2016). Evaluating a program of equine therapy for veterans with PTSD symptoms. San Francisco: Alliant International University. [Google Scholar]
- Hamama, L., Hamama-Raz, Y., Dagan, K., Greenfeld, H., Rubinstein, C., & Ben-Ezra, M. (2011). A preliminary study of group intervention along with basic canine training among traumatized teenagers: A 3-month longitudinal study. Children and Youth Services Review, 33(10), 1975–1980. doi: 10.1016/j.childyouth.2011.05.021. [DOI] [Google Scholar]
- Harris, R., Bradburn, M., Deeks, J., Hardbord, R., Altman, D., Steichen, T., Sterne, J., & Higgins, J. (2010). METAN: Stata module for fixed and random effects meta-analysis. Chestnut Hill, MA: Statistical Software Components, Boston College, Department of Economics. [Google Scholar]
- Hawkins, E. L., Hawkins, R. D., Dennis, M., Williams, J. M., & Lawrie, S. M. (2019). Animal-assisted therapy for schizophrenia and related disorders: A systematic review. Journal of Psychiatric Research, 115, 51–60. doi: 10.1016/j.jpsychires.2019.05.013. [DOI] [PubMed] [Google Scholar]
- Hediger, K., Künzi, P., Felicitas, T., Häfeli, A., Gerger, H., & Wagner, J. (2019). Animal-assisted interventions for post-traumatic stress symptoms: A systematic review and meta-analysis. PROSPERO International Prospective Register of Systematic Reviews, CRD42019141584. Retrieved from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019141584
- Higgins, J. P. T., Li, T., & Deeks, J. J. (2019). Choosing effect measures and computing estimates of effect. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions (Version 6.0) (pp. 143–176). Chichester, UK: John Wiley & Sons. [Google Scholar]
- Higgins, J. P. T., & Green, S. (Eds.). (2008). Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons, Ltd. [Google Scholar]
- Hu, M., Zhang, P., Leng, M., Li, C., & Chen, L. (2018). Animal-assisted intervention for individuals with cognitive impairment: A meta-analysis of randomized controlled trials and quasi-randomized controlled trials. Psychiatry Research, 260, 418–427. doi: 10.1016/j.psychres.2017.12.016. [DOI] [PubMed] [Google Scholar]
- IAHAIO . (2018). IAHAIO White Paper 2014, updated for 2018. The IAHAIO definitions for animal assisted intervention and guidelines for wellness of animals involved in AAI. Retrieved from http://iahaio.org/wp/wp-content/uploads/2018/04/iahaio_wp_updated-2018-final.pdf2018
- Johnson, R. A., Albright, D. L., Marzolf, J. R., Bibbo, J. L., Yaglom, H. D., Crowder, S. M., … Harms, N. (2018). Effects of therapeutic horseback riding on post-traumatic stress disorder in military veterans. Military Medical Research, 5(1), 3. doi: 10.1186/s40779-018-0149-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, R. A., Johnson, P. J., Megarani, D. V., Patel, S. D., Yaglom, H. D., Osterlind, S., … Crowder, S. M. (2017). Horses working in therapeutic riding programs: Cortisol, Adrenocorticotropic hormone, glucose, and behavior stress indicators. Journal of Equine Veterinary Science, 57, 77–85. doi: 10.1016/j.jevs.2017.05.006. [DOI] [Google Scholar]
- Jones, M. G., Rice, S. M., & Cotton, S. M. (2019). Incorporating animal-assisted therapy in mental health treatments for adolescents: A systematic review of canine assisted psychotherapy. PLoS One, 14(1), e0210761. doi: 10.1371/journal.pone.0210761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julius, H., Beetz, A., Kotrschal, K., Turner, D. C., & Uvnäs-Moberg, K. (2013). Attachment to pets. An integrative view of human-animal relationships with implications for therapeutic practice. Göttingen: Hogrefe. [Google Scholar]
- Kemp, K., Signal, T., Botros, H., Taylor, N., & Prentice, K. (2014). Equine facilitated therapy with children and adolescents who have been sexually abused: A program evaluation study. Journal of Child and Family Studies, 23(3), 558–566. doi: 10.1007/s10826-013-9718-1. [DOI] [Google Scholar]
- Kloep, M. L., Hunter, R. H., & Kertz, S. J. (2017). Examining the effects of a novel training program and use of psychiatric service dogs for military-related PTSD and associated symptoms. The American Journal of Orthopsychiatry, 87(4), 425–433. doi: 10.1037/ort0000254. [DOI] [PubMed] [Google Scholar]
- Krause-Parello, C. A., & Friedmann, E. (2014). The effects of an animal-assisted intervention on Salivary Alpha-Amylase, Salivary Immunoglobulin A, and Heart Rate during forensic interviews in child sexual abuse cases. Anthrozoös, 27(4), 581–590. doi: 10.2752/089279314X14072268688005. [DOI] [Google Scholar]
- Krause-Parello, C. A., & Gulick, E. E. (2015). Forensic interviews for child sexual abuse allegations: An investigation into the effects of animal-assisted intervention on stress biomarkers. Journal of Child Sexual Abuse, 24(8), 873–886. doi: 10.1080/10538712.2015.1088916. [DOI] [PubMed] [Google Scholar]
- Krause-Parello, C. A., Levy, C., Holman, E., & Kolassa, J. E. (2018). Effects of VA facility dog on hospitalized veterans seen by a palliative care psychologist: An innovative approach to impacting stress indicators. The American Journal of Hospice & Palliative Care, 35(1), 5–14. doi: 10.1177/1049909116675571. [DOI] [PubMed] [Google Scholar]
- Kruger, A. K. (2012). Trauma-focused equine-assisted psychotherapy effects on child andadolescent functioning scale scores following six months of treatment. San Marcos, Texas: Texas State University. [Google Scholar]
- Lanning, B. A., & Krenek, N. (2013). Guest Editorial: Examining effects of equine-assisted activities to help combat veterans improve quality of life. Journal of Rehabilitation Research and Development, 50(8), vii–xiii. doi: 10.1682/JRRD.2013.07.0159. [DOI] [PubMed] [Google Scholar]
- Lanning, B. A., Wilson, A. L., Krenek, N., & Beaujean, A. A. (2017). Using therapeutic riding as an intervention for combat veterans: An International Classification of Functioning, Disability, and Health (ICF) approach. Occupational Therapy in Mental Health, 33(3), 259–278. doi: 10.1080/0164212X.2017.1283282. [DOI] [Google Scholar]
- Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Lopez-Cepero, J. (2020). Current status of animal-assisted interventions in scientific literature: A critical comment on their internal validity. Animals (Basel), 10(6), 985. doi: 10.3390/ani10060985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malinowski, K., Yee, C., Tevlin, J. M., Birks, E. K., Durando, M. M., Pournajafi-Nazarloo, H., & McKeever, K. H. (2018). The effects of equine assisted therapy on plasma cortisol and oxytocin concentrations and heart rate variability in horses and measures of symptoms of post-traumatic stress disorder in veterans. Journal of Equine Veterinary Science, 64, 17–26. doi: 10.1016/j.jevs.2018.01.011. [DOI] [PubMed] [Google Scholar]
- McCullough, L. M. (2011). Effect of Equine-facilitated Psychotherapy on Posttraumatic Stress Symptoms in Youth with History of Maltreatment and Abuse. Northcentral University: ProQuest Dissertations Publishing. doi: 10.1080/15289168.2015.1021658. [DOI] [Google Scholar]
- McCullough, L. M., Risley-Curtiss, C., & Rorke, J. (2015). Equine facilitated psychotherapy: A pilot study of effect on posttraumatic stress symptoms in maltreated youth. Journal of Infang, Child and Adolescent Psychotherapy, 14(2), 158–173. doi: 10.1080/15289168.2015.1021658. [DOI] [Google Scholar]
- McInnes, M. D. F., Moher, D., Thombs, B. D., McGrath, T. A., Bossuyt, P. M., Clifford, T., … Hunt, H. A. (2018). Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: The PRISMA-DTA statement preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: The PRISMA-DTA statement. JAMA, 319(4), 388–396. doi: 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- Miller, K. E., Jamison, A. L., Gala, S., & Woodward, S. H. (2018). Two independent predictors of nightmares in posttraumatic stress disorder. Journal of Clinical Sleep Medicine, 14(11), 1921–1927. doi: 10.5664/jcsm.7494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller, M. K., & McCullough, L. M. (2017). Effects of equine-facilitated psychotherapy on post-traumatic stress symptoms in youth. Journal of Child and Family Studies, 26(4), 1164–1172. doi: 10.1007/s10826-016-0648-6. [DOI] [Google Scholar]
- Murrow, B. L. (2013). A quantitative exploration into the effects of the human and animal connection. Carpinteria, CA: Pacifica Graduate Institute. [Google Scholar]
- Naste, T. M., Price, M., Karol, J., Martin, L., Murphy, K., Miguel, J., & Spinazzola, J. (2018). Equine Facilitated Therapy for Complex Trauma (EFT-CT). Journal of Child & Adolescent Trauma, 11(3), 289–303. doi: 10.1007/s40653-017-0187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevins, R., Finch, S., Hickling, E. J., & Barnett, S. D. (2013). The Saratoga WarHorse project: A case study of the treatment of psychological distress in a veteran of Operation Iraqi Freedom. Advances in Body-mind Medicine, 27(4), 22–25. [PubMed] [Google Scholar]
- O’Haire, M. E. (2013). Animal-assisted intervention for autism spectrum disorder: A systematic literature review. Journal of Autism and Developmental Disorders, 43(7), 1606–1622. doi: 10.1007/s10803-012-1707-5. [DOI] [PubMed] [Google Scholar]
- O’Haire, M. E., Guerin, N. A., & Kirkham, A. C. (2015). Animal-Assisted Intervention for trauma: A systematic literature review. Frontiers in Psychology, 6, 1121. doi: 10.3389/fpsyg.2015.01121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Haire, M. E., & Rodriguez, K. E. (2018). Preliminary efficacy of service dogs as a complementary treatment for posttraumatic stress disorder in military members and veterans. Journal of Consulting and Clinical Psychology, 86(2), 179–188. doi: 10.1037/ccp0000267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, K. E., Bryce, C. I., Granger, D. A., & O’Haire, M. E. (2018). The effect of a service dog on salivary cortisol awakening response in a military population with posttraumatic stress disorder (PTSD). Psychoneuroendocrinology, 98, 202–210. doi: 10.1016/j.psyneuen.2018.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romaniuk, M., Evans, J., & Kidd, C. (2018). Evaluation of an equine-assisted therapy program for veterans who identify as ‘wounded, injured or ill’ and their partners. PLoS One, 13(9), e0203943. doi: 10.1371/journal.pone.0203943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossetti, J., & King, C. (2010). Use of animal-assisted therapy with psychiatric patients. Journal of Psychosocial Nursing and Mental Health Services, 48(11), 44–48. doi: 10.3928/02793695-20100831-05. [DOI] [PubMed] [Google Scholar]
- Schneider, M. S., & Harley, L. P. (2006). How dogs influence the evaluation of psychotherapists. Anthrozoös, 19(2), 128–142. doi: 10.2752/089279306785593784. [DOI] [Google Scholar]
- Schnurr, P. P. (2007). The rocks and hard places in psychotherapy outcome research. Journal of Traumatic Stress, 20(5), 779–792. doi: 10.1002/jts.20292. [DOI] [PubMed] [Google Scholar]
- Schramm, E., Hediger, K., & Lang, U. E. (2015). From animal behavior to human health: An animal-assisted mindfulness intervention for recurrent depression. Zeitschrift Für Psychologie, 223(3), 192–200. doi: 10.1027/2151-2604/a000220. [DOI] [Google Scholar]
- Shambo, L., Seely, S. K., & Vonderfecht, H. R. (2010). A pilot study on equine-facilitated psychotherapy for trauma-related disorders. Scientific and Educational Journal of Therapeutic Riding, 11–23.
- Sheade, H. E. (2015). Effectiveness of relational equine-partnered counseling (REPC) on reduction of symptoms of PTSD in military veterans: A single case design. Denton, TX: University of North Texas. [Google Scholar]
- Signal, T., Taylor, N., Botros, H., Prentice, K., & Lazarus, K. (2013). Whispering to horses: Childhood sexual abuse, depression and the efficacy of equine facilitated therapy. Sexual Abuse in Australia and New Zealand, 5(1), 24–32. [Google Scholar]
- Signal, T., Taylor, N., Prentice, K., McDade, M., & Burke, K. J. (2017). Going to the dogs: A quasi-experimental assessment of animal assisted therapy for children who have experienced abuse. Applied Developmental Science, 21(2), 81–93. doi: 10.1080/10888691.2016.1165098. [DOI] [Google Scholar]
- Simonato, M., De Santis, M., Contalbrigo, L., Benedetti, D., & Finocchi Mahne, E. (2018). The Italian Agreement between the government and the regional authorities: National guidelines for AAI and institutional context. People and Animals: The International Journal of Research and Practice, 1(1), 1–11. [Google Scholar]
- Steele, E., Wood, D. S., Usadi, E. J., & Applegarth, D. M. (2018). TRR’s Warrior Camp: An intensive treatment program for combat trauma in active military and veterans of all eras. Military Medicine, 183, 403–407. doi: 10.1093/milmed/usx153. [DOI] [PubMed] [Google Scholar]
- Steele, H., Steele, M., & Fonagy, P. (1996). Associations among attachment classifications of mothers, fathers, and their infants. Child Development, 67(2), 541–555. doi: 10.2307/1131831. [DOI] [PubMed] [Google Scholar]
- Tedeschi, P., Jenkins, M. A., Parish-Plass, N., Olmert, M. D., & Yount, R. A. (2019). Treating human trauma with the help of animals: Trauma-informed intervention for child maltreatment and adult posttraumatic stress. In Fine A. H. (Ed.), Handbook of animal-assisted therapy. Foundations and guidelines for animal-assisted interventions (5th ed., pp. 363–380). London: Elsevier. [Google Scholar]
- Trzmiel, T., Purandare, B., Michalak, M., Zasadzka, E., & Pawlaczyk, M. (2019). Equine assisted activities and therapies in children with autism spectrum disorder: A systematic review and a meta-analysis. Complementary Therapies in Medicine, 42, 104–113. doi: 10.1016/j.ctim.2018.11.004. [DOI] [PubMed] [Google Scholar]
- van Houtert, E. A. E., Endenburg, N., Wijnker, J. J., Rodenburg, B., & Vermetten, E. (2018). The study of service dogs for veterans with post-traumatic stress disorder: A scoping literature review. European Journal of Psychotraumatology, 9(Suppl 3), 1503523. doi: 10.1080/20008198.2018.1503523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent, C., Belleville, G., Gagnon, D. H., Dumont, F., Auger, E., Lavoie, V., … Lessart, G. (2017). Effectiveness of service dogs for veterans with PTSD: Preliminary outcomes. Studies in Health Technology and Informatics, 242, 130–136. [PubMed] [Google Scholar]
- Whittlesey-Jerome, W. K. (2014). Adding equine-assisted psychotherapy to conventional treatments: A pilot study exploring ways to increase adult self-efficacy among victims of interpersonal violence. The Practitioner Scholar: Journal of Counselling and Professional Psychology, 3, 82–101. [Google Scholar]
- Woodward, S. H., Jamison, A. L., Gala, S., & Holmes, T. H. (2017). Canine companionship is associated with modification of attentional bias in posttraumatic stress disorder. PLoS One, 12(10), e0179912. doi: 10.1371/journal.pone.0179912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodwart, S. H., Jamison, A. L., Gala, S., & Arsenault, N. (2017). Posttraumatic stress disorder, canine companionship and sleep: Preliminary findings. Sleep, 40, A400. doi: 10.1093/sleepj/zsx050.1073. [DOI] [Google Scholar]
- Woolley, C. C. (2004). Changes in child symptomatology associated with animal-assisted therapy. Logan, UT: Utah State University. [Google Scholar]
- Wortman, R. A., Vallone, T., Karnes, M., Walawander, C., Daly, D., & Fox-Garrity, B. (2018). Pinnipeds and PTSD: An analysis of a human-animal interaction case study program for a veteran. Occupational Therapy International, 2018, 2686728. doi: 10.1155/2018/2686728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarborough, B. J. H., Owen-Smith, A. A., Stumbo, S. P., Yarborough, M. T., Perrin, N. A., & Green, C. A. (2017). An observational study of service dogs for veterans with posttraumatic stress disorder. Psychiatric Services, 68(7), 730–734. doi: 10.1176/appi.ps.201500383. [DOI] [PubMed] [Google Scholar]
- Yorke, J., Nugent, W., Strand, E., Bolen, R., New, J., & Davis, C. (2013). Equine-assisted therapy and its impact on cortisol levels of children and horses: A pilot study and meta-analysis. Early Child Development and Care, 183(7), 874–894.
- Zafra-Tanaka, J. H., Pacheco-Barrios, K., Tellez, W. A., & Taype-Rondan, A. (2019). Effects of dog-assisted therapy in adults with dementia: A systematic review and meta-analysis. BMC Psychiatry, 19(1), 41. doi: 10.1186/s12888-018-2009-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are openly available from the Dataverse database at: https://doi.org/10.7910/DVN/MAJSJZ


