Abstract
The sum total of life course exposures creates an exposome that has a significant impact on age-related health. Understanding the interplay between exposome factors and the (epi) genome, offers pertinent insights into the ageing process and its relationship with the accumulation of allostatic load. We propose to exploit this to develop a biomimetic approach that will provide insight into how evolution through natural selection in other species has solved many age related human health issues. In particular, we will emphasise the need to reconnect a more mechanistic approach to medical science with a broader natural sciences approach, using biomimetics to mitigate the global burden of age related ill health. In particular, we will discuss how such an approach indicates leverage of the activities of the Nrf 2 gene to enhance health span via reintroduction of the classical ‘Food as Medicine’ concept, including modulation of the microbiome and the creation of more salutogenic and biophilic environments. Additionally, we will discuss how this approach integrates with novel and developing senotherapies.
Keywords: ageing, allostatic load, biomimetics, exposome, microbiome, Nrf2
Background
There has been a slow response to adapt to a tsunami of non-communicable disease in the ageing global population. This ‘diseasome of ageing’ [1,2] reflects a range of ‘burden of lifestyle’ related conditions, such as cancer, chronic kidney disease, type-2 diabetes, arteriosclerosis, Alzheimer's disease, non-alcoholic steatohepatitis and osteoporosis. Pre-Covid, the economic burden on health care systems was calculated at $47 trillion over the period 2010–2030 [3]. This figure is expected to grow significantly in the post-Covid decades and to disproportionately affect low- and middle-income countries and those at lower socio-economic position in high-income countries; hence earlier intervention is critical.
In mammals, the diseasome of ageing is typified by a common underlying dysregulated ageing process per se, accompanied by low-grade persistent inflammation, mitochondrial dysfunction, phosphate toxicity, systemic diminished Nrf2 expression and altered gut microbiome diversity [4]. In turn, these are influenced by an interplay between the (epi)genome and individual components of the exposome, defined as the sum of all environmental exposures across the life course [5]. This entails interplay between the (epi)genome and both biotic and abiotic factors, such as socio-economic position, psychology, nutrition, lifestyle and geo-physical environment, all of which can accelerate ageing processes and engender early onset of age-related morbidities [6]. The mechanistic basis for this is not well defined, but does involve cortisol mediated stress responses, elevated inflammatory and oxidative burden and altered mitochondrial biogenesis.
The importance of the exposome to age-related health can be gauged from the observation that only three basic exposome factors, comprising air pollution, tobacco smoke and diet, account for ∼50% of global deaths [7]. This review will explore how the exposome interplays with the molecular and cellular biology of ageing. Critically, it will emphasise and demonstrate how this requires a cross disciplinary approach to mitigate exposome stress and how features of the exposome can be modulated to improve health span. As such, this will highlight a renaissance of a more holistic natural sciences approach, using biomimetics to mitigate ill health, while underpinning it with solid mechanistic science.
The biology of ageing
The phenotype of ageing can be hallmarked with a series of features that are common across taxa [8], including genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, dysregulated nutrient-sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion and altered intercellular communication. In mammals, these are layered upon diminished expression of Nrf2, a chronic low level inflammatory burden termed ‘inflammageing’, de-repression of genomic retrotransposons and altered composition of the gut microbiota [2,9,10].
The consequences of ageing result in a loss of physical and physiological capability over time. The rate of loss varies between individuals, between tissues and organs with in the same individual and between different stages of the life course. Ageing is subject to antagonistic pleiotropy [11] and as such its effects on physical and physiological capability can be mitigated differentially. Whether these hallmarks of ageing function independently, cumulatively or synergistically with exposome factors, remains to be understood [12]. The hallmarks of ageing are cellular and molecular features that reflect the burden of ‘wear and tear’ accumulated over time. As such, they are a measure of allostatic (over)load at a cellular and molecular level and from this perspective of systemic burden, a better handle on age-related physical and physiological capability might be gleaned, both in the context of normative ageing and in disease. To do so, it is informative to explore individual aspects of the exposome for their capacity to influence ageing and how these might be exploited to mitigate decline in health span (i.e. years of healthy living).
Allostatic measures of ageing
Allostatic load is a subclinical description of overall health, based on a range of measures across different biological systems. First described to account for the increased burden of biological ‘wear and tear’ arising from differential activation of the Hypothalmic Pituitary Adrenal (HPA) axis in response to exposome stresses [13], it has been adapted to describe how exposome factors predispose and contribute to loss of normative physiological function with age [14,15]. As such, allostatic (over)load has been ascribed as a systemic factor within the diseasome of ageing [12]. In essence, it reflects the loss of adaptative homeostasis in the later stages of the life course and with age-related disease. This concept can also be extrapolated to systemic ‘wear and tear’ at a cellular and molecular level and be used as an indicator of when and where normative physiological function can be lost. For example, when applied to renal allografts it can be identified at a transcriptional level. Grafts exhibiting a failure to work immediately after transplantation (i.e. delayed graft function (DGF)) fail to achieve transcriptional homeostasis in a key IFN gamma regulatory network as a result to transplantation stress upon meeting the immune system of the recipient. Typically, these transcripts show a one order of magnitude greater change in transcriptional amplitude when exposed to the recipient immune system and fail to start working. Grafts showing immediate graft function, however, show reduced amplitude of transcriptional change and restore transcriptional homeostasis more quickly. Notably, their respective gene promoters are hypomethylated in organs showing DGF, indicating that their epigenetic regulation is dysregulated and that their responses to exposome stressors, such as the recipient immune system, will be aberrant [15].
Methylation clocks
Epigenetic measures of allostatic (over)load can be found in a range of models that estimate biological age based on DNA methylation markers [16,17]. These DNA methylation (DNAm clocks) show strong correlation between DNAm levels and chronological age and can give a robust indication of the likelihood of mortality [18,19], though they have an inherent degree of overfit. Second generation DNAm clocks, which include PhenoAge and GrimAge [20,21] have been improved compared with the first generation models, by using a composite estimate of biological age based on a range of biochemical parameters as a target, not solely chronological age. While these accurately demonstrate an acceleration in biological age in disease, they often fall short in estimating normative physiological function (e.g. renal function) as a consequence of a lack of a ‘gold standard’ determination of what actually constitutes normative ageing. Additionally, they fail to account for the influence of the microbiome, microbial metabolites and nutrition among other exposome factors in the context of adaptive homeostasis at differing life course stages. They are, however, highly successful in demonstrating disconnection between chronological age and loss of physiological function in disease, and hence when excessive allostatic load has been accumulated and interventions might be required to maintain or restore physiological homeostasis. It remains to be determined how these clocks are mechanistically distinct from cellular ageing and how this is influenced by cell type and life stage. Notably, DNAm clocks can be used to provide insight into exceptionally long lived mammalian species [22]. Coupling such insights with an understanding of species and organ specific metabolomics should provide superior understanding of how differing exposomes affect longevity and health span [23,24].
Modulation of Nrf2 activity by the exposome
The inflammatory burden of ageing and the diminished capacity of Nrf2 within the diseasome of ageing, offers an exciting route to tackling a wide range of age-related morbidities and is centred around nutrition, a proven exposome factor influencing age-related health. The recent global burden of disease study [7] has shown that poor dietary habits accounted for 22% of global deaths and were a stronger risk factor than other risks, including tobacco smoking.
The rationale for targeting Nrf2 to improve health span is based on the following. A common feature of animals living under extreme environmental pressure is an enhanced capacity for Nrf2 expression, resulting from convergent evolution to cope with primordial atmospheric oxygen toxicity [2,25]. The Nrf2–Keap 1 system acts as a molecular dimmer switch and regulates over >350 cytoprotective genes in numerous aquatic and terrestrial species, to combat elevated levels of physiological oxidative stress associated with the extremes of their lifestyle and environmental niche, including heat stress and dehydration. Naked mole rats, for example, have proven of particular interest, as they defy Gompertzian law, being extremely long-lived (over >30 years lifespan vs. 2–3 years typical of other rodents), have increased Nrf2 expression and are resistant to cardiovascular disease and cancer [2]. Similarly bats, which live as much as four times longer than similar-sized animals [26,27], exploit Nrf2 to mitigate the effects of the diseasome of ageing [22,28].
The Nrf2/Keap 1 signalling pathway enables an adaptive homeostatic response to both external exposome stressors (e.g. temperature, oxygen levels, nutrition) and internal metabolic stressors (e.g. redox stress). The mechanistic basis for the salutogenic effects of Nrf2 revolves around its ability to bind and activate the antioxidant response elements of a host of cytoprotective genes and to facilitate maintenance of proteostasis, mitigate inflammatory burden and facilitate mitochondrial biogenesis (Figure 1). Upon exposure to a stressor, Keap1 which acts as a molecular rheostat for this signalling pathway, dissassociates from Nrf2 facilitating its nuclear translocation and subsequent triggering of cytoprotective responses. Additionally, Nrf2 interplays with nuclear factor (NF)-κB to modulate stress-related inflammation [2]. Consequently, the diminution of Nrf2 expression with increasing chronological age in mammals and the associated inflammageing, reflects an increase in allostatic load [25] and an inability to restore physiological homeostasis appropriately [15]. In the context of normative ageing, this is exemplified by renal allografts (as a source of healthy tissue) failing to work immediately following transplant, due to an inability to restore transcriptional homeostasis and associated physiological function as a consequence of elevated biological age [15].
Figure 1. How changes in the exposome are mediated by the action of Nrf2.
Exposome stress, either external (e.g. environmental and psycho-social), or internal (e.g. redox imbalance, hypoxia, uraemic toxins), results in disassociation of Keap1 from Nrf2. Nrf 2 then translocase to the nucleus, binds to the AREs of cytoprotective genes and inhibits NFkB mediated inflammatory responses, enables maintenance of the Proteosome and enhances mitochondrial activity. Consequently, these actions result in geroprotection through facilitation of adaptive homeostasis in the face of the exposome stress.
The Nrf2–Keap 1 system is accessible and amenable to therapeutic intervention via a range of synthetic and natural agents [29], including bioactive nutrients. In particular, phenolic acids acquired from dietary intake of fruit and vegetables, are catabolised by gut microbes to generate alkyl-catechols, natural Nrf2 agonists. Critically, these microbes are not well supported by the Western diet [30]. Some specific foods, such as fructose that is ingested or endogenously produced, might have direct roles in ageing by both stimulating mitochondrial oxidative stress [31] while inhibiting Nrf2 [32,33]. Indeed, animals lacking the ability to metabolise fructose via the fructokinase pathway appear to be protected from aging-associated hypertension and kidney disease [34].
As a consequence, the Western diet that is rich in both calories and added sugars, results in a diminution of physiological resilience with age. Novel preventive treatment strategies for human diseases of ageing may thus re-utilise the classical Hippocratic concept of ‘food as medicine' [35]. This also has relevance for protection against exposome related conditions linked to heat stress and air pollution-mediated disease, as Nrf2 plays a role in their mitigation via down-regulation of inflammatory pathways and particulate matter induced cardiovascular diseases and atherosclerosis [36]. Enhanced consumption of natural Nrf2 agonists, such as resveratrol, flavanoids, cinnamaldehyde, lycopene, curcumin, and sulforaphane, have already shown good effect in treating a number of diseases of ageing. Notably, Fisetin and Quercetin have both been demonstrated to be natural senolytics that improve both health span and lifespan in pre-clinical models [37].
The gut microbiota
The dietary exposome also has a significant impact on the maintenance of the diversity of the gut microbiome, which cannot be underestimated with respect to health span. As the composition and individuality of the gut microbiota changes with increasing chronological age [1] changes in the levels of microbial metabolites have been proposed to affect both ‘inflammageing’ and health span [38–41]. Observations on the frail elderly have indicated that dietary differences were associated with both diversity of the microbiota and inflammation [42]. In keeping with these observations, two microbial metabolites, namely trimethylamine N-oxide (TMAO) and phenylacetylglutamine (PAG), have been reported to impact dramatically on the ‘diseaseome of ageing’ [43,44]. In particular, much interest has been generated by TMAO, as it is produced in the liver from trimethylamine (TMA), following processing of dietary carnitine acquired from red meat, on a different branch of the same biochemical pathway that produces the osmolyte and methyl donor betaine. This provides a further emerging role for the microbiota in provision of a bridge between diet, the intermediate inflammatory phenotype (i.e. inflammageing) and maintenance of the epigenetic landscape, where the capacity of the gut microbiota to generate betaine from nutritional sources provides a source of methyl donor groups that contribute to the maintenance of the methylome [45].
Differences in the diversity of the microbiota are also associated with biological age in man. Those at lower SEP (socio-economic position) and at higher biological age exhibit a significantly higher abundance of circulatory pathogenic bacteria, while those less biologically aged possess more circulatory salutogenic (i.e. health promoting) bacteria. Similarly and analogously, captive animals are known to display loss of microbial diversity associated with poorer health, than their wild type counterparts [46–48]. Indeed their microbiomes have been reported to ‘humanise’ [49].
The presence of salutogenic bacteria is consistent with a capacity to metabolise and produce Nrf2 agonists [50]. These differences are also reflected in betaine levels, which similarly display a difference with SEP, consistent with reduced global DNA methylation levels in those at lower SEP. Potential confounding factors in unravelling how the human gut microbiota interplays with ageing are actually constitutes normative ageing and a normative microbiota and how these are influenced by other exposome factors. The inherent difficulties are exemplified by the use of a Mediterranean diet to improve health span. When applied to elderly subjects, it has been reported to increase abundance of salutogenic bacteria and lower inflammatory burden [51]. While these findings seem intuitive and biologically plausible, they must be tempered with an appreciation of antagonistic pleiotropy and the exposome. Critically, when SEP is factored into the analysis of the use a Mediterranean diet, the apparent health benefits are explained away [52], implying that in this instance, nutrition is not the sole driver of age-related health and that other exposome factors need to be explored. In this respect. Intriguingly, any mechanistic link between the microbiota and SEP might centre on vegetable intake. Those at higher SEP consume more fibre and vegetables than those at low SEP, potentially enhancing dietary provision of Nrf2 agonists. This should intuitively provide cyto-protection and promote better health span. Conversely, this protection is lost in the lower SEP group, with a lower relative intake of fruit and vegetables, and with an increased prevalence of pathobionts that have the potential to contribute to systemic age-related diseases.
Geo-physical and social environment
A confluence of global stressors has emerged that is having a singular and immediate impact on both human health and that of the natural world, with extreme sequelae expected over the remainder of the century. These include climate change, loss of biodiversity, pollution, deforestation, industrial monocultural farming, a shortage of portable water, a zoonotic pandemic layered upon an ongoing sixth mass extinction and a growing aged human population [28]. The societal implications of climate change are enormous and include a growth in environmental refugees, as habitat is lost. In 2017 alone, 155 billion hours of labour were estimated lost, mostly in the agricultural sector, through heat exposure. Heat-triggered renal disease is already evident in several regions of the planet [53] and water shortage has been linked to sex specific oxidative stress and accelerated ageing in animals [54]. Social and geo-physical environments can be both salutogenic and pathogenic. Psychological stress imposed by a threatening social and geo-physical environment accelerates ageing processes and can lead to adiposity and associated sequelae of poor health, especially in women [55]. Pertinent to this, women also seem to bear a disproportionate effect of the stress of the current and past pandemics [56]. By 2050, 66% of the world's population is expected to be urban, which is likely to exacerbate the impact of the ‘diseasome of ageing’, as residents of urban areas appear less resilient to exposure to physiological stress than rural dwellers. Reduced biodiversity in urban settings may lead to loss of diversity in gut microbiota associated with an increase in prevalence of asthma, allergic and inflammatory bowel diseases, diabetes and obesity [57,58]. It should also be noted that pharmaceutcals used regularly, such as proton pump inhibitors [59] and non-steroidal anti-inflammatory drugs [60] may contribute to a decrease in microbiome diversity.
Holistic approaches to health, including One Health, EcoHealth, and Planetary Health have been proposed as a blueprint to address the growing global health crisis, focussed mainly on food safety and disease transmission between humans and animals, not specifically burden of lifestyle-related diseases [61]. Consequently, the 2019 Nobel Symposium on Medical Biomimetics, provided a platform for the discussion of bio-inspirational medicine (i.e. solutions to human health challenges derived from the natural world) to address this shortfall [1,25]. We have recently proposed the concept of ‘Planetary health'[62] which, in addition to the original manifesto by Horton et al. [6], incorporates a biomimetic approach to improve human health span. Here we discuss how this may be achieved via direct modulation of human exposomes.
Biomimetics
As part of an initiative to identify naturally occurring solutions to human health problems, a biomimetic approach seeks to identify these in the wild. This has a distinct advantage over conventional lab-based animal models, in that the latter are typically metabolically morbid, they don't recapitulate human disease states fully and their microbiomes are often ‘humanised’. The geo-physical and social exposomes are also unnatural [49]. Notably, in hibernating animals, such as bears, biomimetics offers pertinent insight into regulation of metabolism, fat mass and insulin resistance, which appear to be governed by changes in the microbiome, driven by consumption of plant polyphenols [40,63]. This has ramifications for human health, given a global trend towards a more carnivorous diet, which predisposes to renal dysfunction and cancer in obligate carnivores, such as felids, and which has already been associated with similar diseases in humans at low SEP [64–66].
Additionally, to reduce inflammatory burden, maintain organ function and enable epigenomic regulation of the metabolic changes required for emergence from hibernation, a metabolic switch is used to drive production of the methyl-donor betaine instead of TMAO in hibernation [63]. Tellingly, this switch is not found in captive bears. Such changes may be transmissible via faecal xenotransplantation, with the metabolic and physical changes observed in the bear being imparted to mice [67]. As such, these insights have highlighted novel targets for therapeutic intervention in cardio-reno disease in man and other mammals. More biomimetic insights have been described in depth elsewhere [40], though of particular pertinence to the diseasome of ageing and climate change, has been the growing use of sodium-glucose co-transporter 2 (SGLT2) sodium-glucose co-transporter 2 (SGLT2) inhibitors. These mimic the metabolic patterns observed during aestivation in a diverse range of animals, including crocodiles, tortoises and hedgehogs, that adopt this process to conserve metabolic functions during periods of environmental stress [68]. Clinically, SGLT2-inhibitors induce a biomimesis, improving cardiac and renal function as a consequence.
How might exposome based solutions tackle the diseasome of ageing?
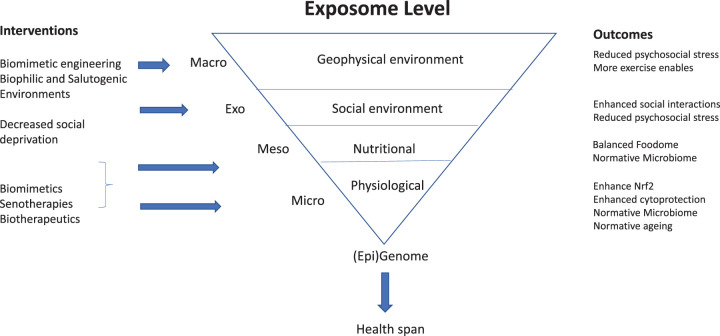
Figure 2 depicts how differing levels of the exposome might be exploited to enable interventions to improve health span. Biomimetics offers clear insight into how the exposome can be modified to improve health span in man. This concept has been in widespread use in engineering for some time but has only been sparingly adopted by biomedical science. Critical insights into its application in clinical and veterinary medicine have been described comprehensively and elsewhere [40]. Below, however, we discuss how specific exposome factors can be modified inspired by biomimetics. Design of urban environments to be more salutogenic, may be one aspect of the exposome that can be modified to help [69]. Salutogenic effects can be driven by biophilia, i.e. an innate tendency to connect with natural environments, features of which have been evolutionary benefit. This has been incorporated in the concept of biophilic building design but might be enhanced by a biomimetic approach to improve the health of human populations subject to the effects of climate change [70]. For example, the Sahara Forest Project mimics the Namibian desert beetle's ability to ability to self-regulate its body temperature and collect water from the air, for a building that aims to rely on solar energy alone to operate as a zero-waste system. The Eastgate Centre in Zimbabwe, is also pertinent, employing the physics of air circulation and temperature control in termite mounds, which resembles that of an organ in physiology, to make it more eco-friendly, and suitable to a wide variety of climates. All these initiatives are expected to reduce exposome stress on their inhabitants and thus improve health span.
Figure 2. Manipulating the exposome to improve health-span.
A schematic representation of the exposome, defining differing levels of interaction with the (epi)genome. Potential interventions to mitigate the effects of cumulative allostatic and subsequent ill health are indicated beside the respective exposome levels, from the macro-geophysical environmental level to the micro-tissue and cellular physiology level. Potential outcomes are listed on the right hand side of the respective levels.
Additionally, coupling biomimetic design with medical innovation may have a number of direct benefits. Firstly, the incorporation of edible forest gardens instead of ubiquitous lawns into modern design of habitation offers the opportunity to grow sources of natural Nrf2 agonists and mitigate loss of diversity in gut microbiota associated with life in urban environments. Secondly, it would create a more diverse environment for local wildlife. Furthermore, it would create a salutogenic environment that mitigates the loss of physiological resilience associated with exposome stress [55,71] and improve health span as a consequence.
Additionally, the creation of vertical forest gardens to combat air pollution is a notable exemplar of biomimetic design. For example, the Bosco Verticale in Milan, which consists of two residential tower blocks with foliage cover equivalent to 10 000 square metres of forest. Such urban greenness has well stablished salutogenic effects on diabetes, hypertension and cardiovascular diseases (CVD) in urban environments [72–74]. A meta-analysis of studies comparing urban green spaces for prevention of NCD within the diseasome of ageing, (via mitigating air and noise pollution, reducing psycho-social stress and supporting physical activity) identified an inverse association between greenness and all-cause mortality. This is a clear indication that interventions designed to manipulate the exposome to enhance exposure to green spaces, should be public health strategy [75]. The links between deforestation, changes in soil microbiome, plant growth and nutritional content of and the long term effects on the human microbiome and health outcomes need further studies [76]. These approaches are in keeping with UN Ecosystem Restoration project (2021–2030), which aims to conserve, restore and grow 1 trillion trees by 2030. This is particular pertinent to low- and middle-income countries where 4.2 million death were attribute to air pollution in 2016 alone. The use the Cotoneaster franchetii, which is 20% more effective at soaking up urban pollution compared with other shrubs [77] is highly pertinent in this respect.
Future perspectives
Modulation of the exposome is both viable and effective at improving human health. Individual, cumulative and synergistic strategies operating at all exposome levels offer ‘low hanging’ and often cost effective means of both improving health in the general population and tackling the diseasome of ageing. In essence, these might reduce the gap between health span and lifespan, by increasing years of healthy living. Putting a fixed number of extra years of health these might achieve is extremely challenging, but in the setting of deprivation an extra 10 years does not seem improbable. It is worth emphasising however, that they are unlikely to increase overall maximum human longevity, simply health span.
To improve health span, incorporation of dietary supplementation seems a straightforward way of enabling agonism of Nrf2 and potentially providing a natural means of low level senolysis (e.g. by fisetin or quercetin supplementation in the diet). This, however, also needs to be tempered by the fact that de novo mutation in NEFL2, the gene encoding Nrf2, affecting it regulation by Keap 1, leads to an early onset multisystem disorder and redox imbalance [78]. Nrf2 accumualtion is also a feature of drug resistant cancer cells, which exhibit similar mutations. Defining a regulated ‘sweet spot’ for Nrf2 is thus desirable.
Synergistic with this approach is modification of the microbiome to enhance the presence of salutogenic bacteria, or restore a normative microbiota in the context of disease. Such a strategy may include use of live biotherpeutics, or dietary modification. It is already in practice, and has recently shown promise in treating kidney disease, through dietary modification to support growth of short chain fatty acid producing salutogenic bacteria in dialysis patients, thus reducing inflammatory burden, reducing gut leak and increasing physiological resilence [79].
Modulation of the microbiome might also provide a means to combat antibiotic resistance clinically, through the use of commensal microbes to combat antibiotic resistant pathogens in hospitals, or to prime an immune system to fight cancer [80]. Additionally, this approach may be transposed to food production, where salutogenic bacteria might be used as a probiotic, to prevent infections and improve yield in livestock.
Recently, the identification of microbes in ruminants to digest plastic, has provided a dramatic counterpoint and novel avenue for making the anthropogenic biosphere more sustainable and less environmentally toxic [81], which bodes well for the future.
The use of biological biomimetics, for example, might also offer us a greater alignment with our natural exposome. Biomimetic inspired medicines, for instance, might also provide both direct and particularly indirect benefits, such as a reduction in the use of modern synthetic medicines. These are typically derived via a pharmaceutical/drug discovery model, which is costly and incorporates pre-clinical testing in a range of inadequate and metabolically morbid animal models, from which findings often do not translate to man. As synthetic medicines find their way into the watercourse, they can have calamitous effects on both human and marine health. Secondly, they have indeterminate effects on the microbiome (‘drug-bug effects'), with inadvertent long-term health consequences. Thirdly, they may have effects on the natural selective pressures for diseases of ageing. While modern medicine allows individuals who previously would not have survived and reproduced to do so, natural selection continues to impact human health, now shaped by our ability to adapt. Over hundreds of millions of years successful species have evolved adaptations as their worlds changed. If we are to survive, we must too. For the first time during evolution one species — Homo sapiens — can determine the fate of the whole biosphere (Martin Rees).
Abbreviations
- CVD
cardiovascular diseases
- DGF
delayed graft function
- HPA
Hypothalmic Pituitary Adrenal
- SEP
socio-economic position
- SGLT2
sodium-glucose co-transporter 2
- TMAO
trimethylamine N-oxide
Competing Interests
P.S. serves on a Scientific Advisory Board for REATA. R.J.J. has equity in XORTX Therapeutics and Colorado Research Partners, LLC. P.G.S. is in receipt of research awards form 4D Pharma and Constant Pharma.
References
- 1.O'Toole, P.W. and Shiels, P.G. (2020) The role of the microbiota in sedentary lifestyle disorders and ageing: lessons from the animal kingdom. J. Intern. Med. 287, 271–282 10.1111/joim.13021 [DOI] [PubMed] [Google Scholar]
- 2.Stenvinkel, P. and Shiels, P.G. (2019) Long-lived animals with negligible senescence: clues for ageing research. Biochem. Soc. Trans. 47, 1157–1164 10.1042/BST20190105 [DOI] [PubMed] [Google Scholar]
- 3.Chen, S., Kuhn, M., Prettner, K. and Bloom, D.E. (2018) The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLoS ONE 13, e0206702 10.1371/journal.pone.0206702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebert, T., Pawelzik, S.-C., Witasp, A., Arefin, S., Hobson, S., Kublickiene, K.et al. (2020) Inflammation and premature ageing in chronic kidney disease. Toxins 12, 227 10.3390/toxins12040227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wild, C.P. (2005) Complementing the genome with an ‘Exposome’: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomarkers Prev. 14, 1847–1850 10.1158/1055-9965.EPI-05-0456 [DOI] [PubMed] [Google Scholar]
- 6.Horton, R., Beaglehole, R., Bonita, R., Raeburn, J., McKee, M. and Wall, S. (2014) From public to planetary health: a manifesto. Lancet 383, 847 10.1016/S0140-6736(14)60409-8 [DOI] [PubMed] [Google Scholar]
- 7.Lim, S.S., Vos, T., Flaxman, A.D., Danaei, G., Shibuya, K., Adair-Rohani, H., et al. (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 380, 2224–2260 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López-Otín, C., Blasco, M.A., Partridge, L., Serrano, M. and Kroemer, G. (2013) The hallmarks of aging. Cell 153, 1194–1217 10.1016/j.cell.2013.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon, M., Van Meter, M., Ablaeva, J., Ke, Z., Gonzalez, R.S., Taguchi, T., et al. (2019) LINE1 derepression in aged wild-type and SIRT6-Deficient mice drives inflammation. Cell Metab. 29, 871–885.e5 10.1016/j.cmet.2019.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Cecco, M., Ito, T., Petrashen, A.P., Elias, A.E., Skvir, N.J., Criscione, S.W., et al. (2019) L1 drives IFN in senescent cells and promotes age-associated inflammation. Nature 566, 73–78 10.1038/s41586-018-0784-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams, G.C. (1957) Pleiotropy, natural selection, and the evolution of senescence. Evolution 11, 398 10.1111/j.1558-5646.1957.tb02911.x [DOI] [Google Scholar]
- 12.Shiels, P.G., Buchanan, S., Selman, C. and Stenvinkel, P. (2019) Allostatic load and ageing: linking the microbiome and nutrition with age-related health. Biochem. Soc. Trans. 47, 1165–1172 10.1042/BST20190110 [DOI] [PubMed] [Google Scholar]
- 13.McEwen, B.S. and Stellar, E. (1993) Stress and the individual. Arch. Intern. Med. 153, 2093–2101 10.1001/archinte.1993.00410180039004 [DOI] [PubMed] [Google Scholar]
- 14.Kooman, J.P., Kotanko, P., Schols, A.M.W.J., Shiels, P.G. and Stenvinkel, P. (2014) Chronic kidney disease and premature ageing. Nat. Rev. Nephrol. 10, 732–742 10.1038/nrneph.2014.185 [DOI] [PubMed] [Google Scholar]
- 15.McGuinness, D., Mohammed, S., Monaghan, L., Wilson, P.A., Kingsmore, D.B., Shapter, O., et al. (2018) A molecular signature for delayed graft function. Aging Cell 17, e12825 10.1111/acel.12825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hannum, G., Guinney, J., Zhao, L., Zhang, L., Hughes, G., Sadda, S., et al. (2013) Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol. Cell 49, 359–367 10.1016/j.molcel.2012.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horvath, S. (2013) DNA methylation age of human tissues and cell types. Genome Biol. 14, R115 10.1186/gb-2013-14-10-r115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marioni, R.E., Shah, S., McRae, A.F., Chen, B.H., Colicino, E., Harris, S.E., et al. (2015) DNA methylation age of blood predicts all-cause mortality in later life. Genome Biol. 16, 25 10.1186/s13059-015-0584-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen, B.H., Marioni, R.E., Colicino, E., Peters, M.J., Ward-Caviness, C.K., Tsai, P.-C., et al. (2016) DNA methylation-based measures of biological age: meta-analysis predicting time to death. Aging 8, 1844–1865 10.18632/aging.101020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levine, M.E., Lu, A.T., Quach, A., Chen, B.H., Assimes, T.L., Bandinelli, S., et al. (2018) An epigenetic biomarker of aging for lifespan and healthspan. Aging 10, 573–591 10.18632/aging.101414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu, A.T., Quach, A., Wilson, J.G., Reiner, A.P., Aviv, A., Raj, K., et al. (2019) DNA methylation grimAge strongly predicts lifespan and healthspan. Aging 11, 303–327 10.18632/aging.101684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilkinson, G.S., Adams, D.M., Haghani, A., Lu, A.T., Zoller, J., Breeze, C.E., et al. (2021) DNA methylation predicts age and provides insight into exceptional longevity of bats. Nat. Commun. 12, 1615 10.1038/s41467-021-21900-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma, S., Yim, S.H., Lee, S.-G., Kim, E.B., Lee, S.-R., Chang, K.-T., et al. (2015) Organization of the mammalian metabolome according to organ function, lineage specialization, and longevity. Cell Metab. 22, 332–343 10.1016/j.cmet.2015.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma, S., Lee, S.-G., Kim, E.B., Park, T.J., Seluanov, A., Gorbunova, V.et al. (2015) Organization of the mammalian ionome according to organ origin, lineage specialization, and longevity. Cell Rep. 13, 1319–1326 10.1016/j.celrep.2015.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stenvinkel, P., Painer, J., Johnson, R.J. and Natterson-Horowitz, B. (2020) Biomimetics: nature's roadmap to insights and solutions for burden of lifestyle diseases. J. Intern. Med. 287, 238–251 10.1111/joim.12982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Irving, A.T., Ahn, M., Goh, G., Anderson, D.E. and Wang, L.-F. (2021) Lessons from the host defences of bats, a unique viral reservoir. Nature 589, 363–370 10.1038/s41586-020-03128-0 [DOI] [PubMed] [Google Scholar]
- 27.Yin, Q., Zhu, L., Liu, D., Irwin, D.M., Zhang, S. and Pan, Y.-H. (2016) Molecular evolution of the nuclear factor (Erythroid-Derived 2)-Like 2 gene Nrf2 in Old world fruit bats (Chiroptera: Pteropodidae). PLoS ONE 11, e0146274 10.1371/journal.pone.0146274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stenvinkel, P., Painer, J., Shiels, P.G., Bansal, A., Fereidouni, S., Natterson-Horowitz, B.et al. (2021) SARS-COV-2 and biomimetics: what saves the planet will save our health. J. Intern. Med. 289, 244–246 10.1111/joim.13128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stenvinkel, P., Meyer, C.J., Block, G.A., Chertow, G.M. and Shiels, P.G. (2019) Understanding the role of the cytoprotective transcription factor nuclear factor erythroid 2–related factor 2—lessons from evolution, the animal kingdom and rare progeroid syndromes. Nephrol. Dial. Transplant. 35, 2036–2045 10.1093/ndt/gfz120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Senger, D.R., Li, D., Jaminet, S.-C. and Cao, S. (2016) Activation of the Nrf2 cell defense pathway by ancient foods: disease prevention by important molecules and microbes lost from the modern western diet. PLoS ONE 11, e0148042 10.1371/journal.pone.0148042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lanaspa, M.A., Sanchez-Lozada, L.G., Choi, Y.-J., Cicerchi, C., Kanbay, M., Roncal-Jimenez, C.A., et al. (2012) Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress. J. Biol. Chem. 287, 40732–40744 10.1074/jbc.M112.399899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.García-Arroyo, F.E., Gonzaga, G., Muñoz-Jiménez, I., Osorio-Alonso, H., Iroz, A., Vecchio, M.et al. (2019) Antioxidant supplements as a novel mean for blocking recurrent heat stress-induced kidney damage following rehydration with fructose-containing beverages. Free Radic. Biol. Med. 141, 182–191 10.1016/j.freeradbiomed.2019.06.016 [DOI] [PubMed] [Google Scholar]
- 33.García-Arroyo, F.E., Gonzaga-Sánchez, G., Tapia, E., Muñoz-Jiménez, I., Manterola-Romero, L., Osorio-Alonso, H., et al. (2021) Osthol ameliorates kidney damage and metabolic syndrome induced by a high-Fat/High-Sugar diet. Int. J. Mol. Sci. 22, 2431 10.3390/ijms22052431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roncal-Jimenez, C.A., Ishimoto, T., Lanaspa, M.A., Milagres, T., Hernando, A.A., Jensen, T., et al. (2016) Aging-associated renal disease in mice is fructokinase dependent. Am. J. Physiol. Ren. Physiol. 311, F722–F730 10.1152/ajprenal.00306.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mafra, D., Borges, N.A., Lindholm, B., Shiels, P.G., Evenepoel, P. and Stenvinkel, P. (2021) Food as medicine: targeting the uraemic phenotype in chronic kidney disease. Nat. Rev. Nephrol. 17, 153–171 10.1038/s41581-020-00345-8 [DOI] [PubMed] [Google Scholar]
- 36.Ebert, T., Neytchev, O., Witasp, A., Kublickiene, K., Stenvinkel, P. and Shiels, P.G. (2021) Inflammation and oxidative stress in CKD and dialysis patients. Antioxid. Redox Signal. 10.1089/ars.2020.8184 [DOI] [PubMed] [Google Scholar]
- 37.Xu, M., Pirtskhalava, T., Farr, J.N., Weigand, B.M., Palmer, A.K., Weivoda, M.M., et al. (2018) Senolytics improve physical function and increase lifespan in old age. Nat. Med. 24, 1246–1256 10.1038/s41591-018-0092-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koeth, R.A., Wang, Z., Levison, B.S., Buffa, J.A., Org, E., Sheehy, B.T., et al. (2013) Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 19, 576–585 10.1038/nm.3145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang, Z., Klipfell, E., Bennett, B.J., Koeth, R., Levison, B.S., Dugar, B., et al. (2011) Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63 10.1038/nature09922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stenvinkel, P., Painer, J., Kuro-o, M., Lanaspa, M., Arnold, W., Ruf, T.et al. (2018) Novel treatment strategies for chronic kidney disease: insights from the animal kingdom. Nat. Rev. Nephrol. 14, 265–284 10.1038/nrneph.2017.169 [DOI] [PubMed] [Google Scholar]
- 41.Janeiro, M., Ramírez, M., Milagro, F., Martínez, J. and Solas, M. (2018) Implication of trimethylamine N-Oxide (TMAO) in disease: potential biomarker or New therapeutic target. Nutrients 10, 1398 10.3390/nu10101398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Claesson, M.J., Jeffery, I.B., Conde, S., Power, S.E., O'Connor, E.M., Cusack, S., et al. (2012) Gut microbiota composition correlates with diet and health in the elderly. Nature 488, 178–184 10.1038/nature11319 [DOI] [PubMed] [Google Scholar]
- 43.Ottosson, F., Brunkwall, L., Smith, E., Orho-Melander, M., Nilsson, P.M., Fernandez, C.et al. (2020) The gut microbiota-related metabolite phenylacetylglutamine associates with increased risk of incident coronary artery disease. J. Hypertens. 38, 2427–2434 10.1097/HJH.0000000000002569 [DOI] [PubMed] [Google Scholar]
- 44.Nemet, I., Saha, P.P., Gupta, N., Zhu, W., Romano, K.A., Skye, S.M., et al. (2020) A cardiovascular disease-Linked Gut microbial metabolite acts via adrenergic receptors. Cell 180, 862–877.e22 10.1016/j.cell.2020.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mafra, D., Esgalhado, M., Borges, N.A., Cardozo, L.F.M.F., Stockler-Pinto, M.B., Craven, H.et al. (2019) Methyl donor nutrients in chronic kidney disease: impact on the epigenetic landscape. J. Nutr. 149, 372–380 10.1093/jn/nxy289 [DOI] [PubMed] [Google Scholar]
- 46.Gibson, K.M., Nguyen, B.N., Neumann, L.M., Miller, M., Buss, P., Daniels, S.et al. (2019) Gut microbiome differences between wild and captive black rhinoceros – implications for rhino health. Sci. Rep. 9, 7570 10.1038/s41598-019-43875-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKenzie, V.J., Song, S.J., Delsuc, F., Prest, T.L., Oliverio, A.M., Korpita, T.M., et al. (2017) The effects of captivity on the mammalian Gut microbiome. Integr. Comp. Biol. 57, 690–704 10.1093/icb/icx090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chong, R., Grueber, C.E., Fox, S., Wise, P., Barrs, V.R., Hogg, C.J.et al. (2019) Looking like the locals - gut microbiome changes post-release in an endangered species. Anim. Microbiome 1, 8 10.1186/s42523-019-0012-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clayton, J.B., Vangay, P., Huang, H., Ward, T., Hillmann, B.M., Al-Ghalith, G.A., et al. (2016) Captivity humanizes the primate microbiome. Proc. Natl Acad. Sci. U.S.A. 113, 10376–10381 10.1073/pnas.1521835113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Craven, H., McGuinness, D., Buchanan, S., Galbraith, N., McGuinness, D.H., Jones, B., et al. (2021) Socioeconomic position links circulatory microbiota differences with biological age. Sci. Rep. 11, 12629 10.1038/s41598-021-92042-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ghosh, T.S., Rampelli, S., Jeffery, I.B., Santoro, A., Neto, M., Capri, M., et al. (2020) Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: the NU-AGE 1-year dietary intervention across five european countries. Gut 69, 1218–1228 10.1136/gutjnl-2019-319654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bonaccio, M., Di Castelnuovo, A., Pounis, G., Costanzo, S., Persichillo, M., Cerletti, C.et al. (2017) High adherence to the Mediterranean diet is associated with cardiovascular protection in higher but not in lower socioeconomic groups: prospective findings from the moli-sani study. Int. J. Epidemiol. 46, 1478–1487 10.1093/ije/dyx145 [DOI] [PubMed] [Google Scholar]
- 53.Haines, A. and Ebi, K. (2019) The imperative for climate action to protect health. N. Engl. J. Med. 380, 263–273 10.1056/NEJMra1807873 [DOI] [PubMed] [Google Scholar]
- 54.Johnson, R.J., Sánchez-Lozada, L.G., Newman, L.S., Lanaspa, M.A., Diaz, H.F., Lemery, J., et al. (2019) Climate change and the kidney. Ann. Nutr. Metab. 74, 38–44 10.1159/000500344 [DOI] [PubMed] [Google Scholar]
- 55.Ellaway, A., Dundas, R., Olsen, J. and Shiels, P. (2018) Perceived neighbourhood problems over time and associations with adiposity. Int. J. Environ. Res. Public. Health 15, 1854 10.3390/ijerph15091854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wenham, C., Smith, J., Davies, S.E., Feng, H., Grépin, K.A., Harman, S.et al. (2020) Women are most affected by pandemics — lessons from past outbreaks. Nature 583, 194–198 10.1038/d41586-020-02006-z [DOI] [PubMed] [Google Scholar]
- 57.Mills, J.G., Brookes, J.D., Gellie, N.J.C., Liddicoat, C., Lowe, A.J., Sydnor, H.R.et al. (2019) Relating urban biodiversity to human health With the ‘Holobiont’ concept. Front. Microbiol. 10, 550 10.3389/fmicb.2019.00550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roslund, M.I., Puhakka, R., Grönroos, M., Nurminen, N., Oikarinen, S., Gazali, A.M., et al. (2020) Biodiversity intervention enhances immune regulation and health-associated commensal microbiota among daycare children. Sci. Adv. 6, eaba2578 10.1126/sciadv.aba2578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Imhann, F., Bonder, M.J., Vich Vila, A., Fu, J., Mujagic, Z., Vork, L., et al. (2016) Proton pump inhibitors affect the gut microbiome. Gut 65, 740–748 10.1136/gutjnl-2015-310376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rogers, M.A.M. and Aronoff, D.M. (2016) The influence of non-steroidal anti-inflammatory drugs on the gut microbiome. Clin. Microbiol. Infect. 22, 178.e1–178.e9 10.1016/j.cmi.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lerner, H. and Berg, C. (2017) A comparison of three holistic approaches to health: one health, ecoHealth, and planetary health. Front. Vet. Sci. 4, 163 10.3389/fvets.2017.00163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stenvinkel, P., Shiels, P.G., Painer, J., Miranda, J.J., Natterson-Horowitz, B. and Johnson, R.J. (2020) A planetary health perspective for kidney disease. Kidney Int. 98, 261–265 10.1016/j.kint.2020.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ebert, T., Painer, J., Bergman, P., Qureshi, A.R., Giroud, S., Stalder, G., et al. (2020) Insights in the regulation of trimetylamine N-oxide production using a comparative biomimetic approach suggest a metabolic switch in hibernating bears. Sci. Rep. 10, 20323 10.1038/s41598-020-76346-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Junginger, J., Hansmann, F., Herder, V., Lehmbecker, A., Peters, M., Beyerbach, M.et al. (2015) Pathology in captive wild felids at German zoological gardens. PLoS ONE 10, e0130573 10.1371/journal.pone.0130573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McClelland, R., Christensen, K., Mohammed, S., McGuinness, D., Cooney, J., Bakshi, A., et al. (2016) Accelerated ageing and renal dysfunction links lower socioeconomic status and dietary phosphate intake. Aging 8, 1135–1149 10.18632/aging.100948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maxwell, F., McGlynn, L.M., Muir, H.C., Talwar, D., Benzeval, M., Robertson, T.et al. (2011) Telomere attrition and decreased fetuin-A levels indicate accelerated biological aging and Are implicated in the pathogenesis of colorectal cancer. Clin. Cancer Res. 17, 5573–5581 10.1158/1078-0432.CCR-10-3271 [DOI] [PubMed] [Google Scholar]
- 67.Sommer, F., Ståhlman, M., Ilkayeva, O., Arnemo, J.M., Kindberg, J., Josefsson, J.et al. (2016) The Gut microbiota modulates energy metabolism in the hibernating brown bear ursus arctos. Cell Rep. 14, 1655–1661 10.1016/j.celrep.2016.01.026 [DOI] [PubMed] [Google Scholar]
- 68.Marton, A., Kaneko, T., Kovalik, J.-P., Yasui, A., Nishiyama, A., Kitada, K.et al. (2021) Organ protection by SGLT2 inhibitors: role of metabolic energy and water conservation. Nat. Rev. Nephrol. 17, 65–77 10.1038/s41581-020-00350-x [DOI] [PubMed] [Google Scholar]
- 69.Lederbogen, F., Kirsch, P., Haddad, L., Streit, F., Tost, H., Schuch, P., et al. (2011) City living and urban upbringing affect neural social stress processing in humans. Nature 474, 498–501 10.1038/nature10190 [DOI] [PubMed] [Google Scholar]
- 70.Wilson, E.O. (1984) Biophilia: the Human Bond with Other Species, Harvard Univ. Press, Cambridge, Mass [Google Scholar]
- 71.Ellaway, A., Dundas, R., Robertson, T. and Shiels, P.G. (2019) More miles on the clock: neighbourhood stressors are associated with telomere length in a longitudinal study. PLoS ONE 14, e0214380 10.1371/journal.pone.0214380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang, B.-Y., Markevych, I., Bloom, M.S., Heinrich, J., Guo, Y., Morawska, L., et al. (2019) Community greenness, blood pressure, and hypertension in urban dwellers: the 33 communities Chinese health study. Environ. Int. 126, 727–734 10.1016/j.envint.2019.02.068 [DOI] [PubMed] [Google Scholar]
- 73.Dzhambov, A.M., Markevych, I. and Lercher, P. (2018) Greenspace seems protective of both high and low blood pressure among residents of an alpine valley. Environ. Int. 121, 443–452 10.1016/j.envint.2018.09.044 [DOI] [PubMed] [Google Scholar]
- 74.Astell-Burt, T. and Feng, X. (2020) Urban Green space, tree canopy and prevention of cardiometabolic diseases: a multilevel longitudinal study of 46 786 Australians. Int. J. Epidemiol. 49, 926–933 10.1093/ije/dyz239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rojas-Rueda, D., Nieuwenhuijsen, M.J., Gascon, M., Perez-Leon, D. and Mudu, P. (2019) Green spaces and mortality: a systematic review and meta-analysis of cohort studies. Lancet Planet. Health 3, e469–e477 10.1016/S2542-5196(19)30215-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Torp Austvoll, C., Gallo, V. and Montag, D. (2020) Health impact of the anthropocene: the complex relationship between gut microbiota, epigenetics, and human health, using obesity as an example. Glob. Health Epidemiol. Genomics 5, e2 10.1017/gheg.2020.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Blanuša, T., Qadir, Z.J., Kaur, A., Hadley, J. and Gush, M.B. (2020) Evaluating the effectiveness of urban hedges as Air pollution barriers: importance of sampling method, species characteristics and site location. Environments 7, 81 10.3390/environments7100081 [DOI] [Google Scholar]
- 78.Huppke, P., Weissbach, S., Church, J.A., Schnur, R., Krusen, M., Dreha-Kulaczewski, S., et al. (2017) Activating de novo mutations in NFE2L2 encoding NRF2 cause a multisystem disorder. Nat. Commun. 8, 818 10.1038/s41467-017-00932-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kemp, J.A., Regis, B., Fragoso dos Santos, H., de Jesus, H.E., Craven, H., Ijaz, U.Z.et al. (2021) The impact of enriched resistant starch type-2 cookies on the gut microbiome in hemodialysis patients. Mol. Nutr. Food Res. In press [DOI] [PubMed] [Google Scholar]
- 80.Sonnenburg, J.L. and Sonnenburg, E.D. (2019) Vulnerability of the industrialized microbiota. Science 366, eaaw9255 10.1126/science.aaw9255 [DOI] [PubMed] [Google Scholar]
- 81.Quartinello, F., Kremser, K., Schoen, H., Tesei, D., Ploszczanski, L., Nagler, M., et al. (2021) Together Is better: the rumen microbial community as biological toolbox for degradation of synthetic polyesters. Front. Bioeng. Biotechnol. 9, 500 10.3389/fbioe.2021.684459 [DOI] [Google Scholar]