Abstract
Type II Diabetes Mellitus (T2DM) is a serious public health issue, affecting the global population, particularly those living in low‐ and middle‐income countries. Worldwide, the prevalence of T2DM ranges between 10.4% and 13.5%, depending on the domiciliary. T2DM negatively affects individuals' quality of life and causes high economic burden due to the increasing cost of treatment and management of the disease. Risk factors associated with T2DMs include aging, lifestyle or behavior, genetics, and important biopsychological aspects, which are psychological stress and sleep deprivation. By understanding the associations of psychological stress and sleep deprivation, which contribute to pathophysiology of T2DM, policies, programs, and guidelines were developed in Malaysia to combat the issue among population at large. This narrative review examines 19 national public health policies, programs, and guidelines from the past 20 years in Malaysia that aimed to mitigate the negative health effects of psychological stress, sleep deprivation, and T2DM, both from the government and non‐governmental organizations. Both psychological stress and sleep deprivation works independently or as combined effects in the pathophysiology of T2DM. Besides, in Malaysia, the government, in collaboration with non‐governmental organizations, have been developing and implementing policies, programs, and guidelines to combat mental health and T2DM issues, targeted to population at large. Integration of digital technology, such as usage of social media for health promotion and dissemination of public health messages to the community and good governance from government were deemed important in the effective implementation of health policies and guidelines, resulting in better health outcome.
Keywords: diabetes mellitus, noncommunicable diseases, policies, programs, psychological stress, review, sleep deprivation, T2DM
1. INTRODUCTION
Diabetes mellitus is characterized by chronic hyperglycemia due to defects in insulin secretion, insulin action, or both. 1 , 2 Worldwide, Type II Diabetes Mellitus (T2DM) is rising to an alarming epidemic level––more than 422 million people are living with diabetes, with the majority residing in low‐ and middle‐income countries (13.5%), compared to those who live in high‐income countries (10.4%). 3 A total of 1.6 million deaths in the world are attributed to diabetes while other adverse health outcomes of T2DM include stroke, heart disease, hearing loss, blindness, hypertension, kidney disease, and nerve damage. 4 , 5
In the United States, it was estimated that about 30.3 million people have diabetes and about one quarter of these (7.2 million people) were not aware that they are living with diabetes. 5 In the United Kingdom, of the 3.5 million people diagnosed with diabetes, 550,000 people remain undiagnosed. 6 Meanwhile in Australia, about 1.1 million people were diagnosed with diabetes. 7 In Thailand, the prevalence of diabetes was 9.9%, 8 meanwhile in Malaysia, the prevalence rate was much higher, at 17.5% (3.5 million people), and is projected to double to 31.3% by the year 2025. 9
In addition, diabetes causes a major global economic burden. It is expected that the cost to treat diabetes will increase from US$ 1.32 trillion in 2015 to US$ 2.12 trillion in 2030. 10 In Malaysia, annually, approximately US$ 600 million are spent for T2DM‐related healthcare, including treatment and management, and this accounted for 16% of the country's national total healthcare budget for the year 2010. 3 Thus investigating and intervening in the risk factors for T2DM are important. Beyond the usual lifestyle risk factors such as physical inactivity, sedentary behavior and smoking, poor mental health, such as psychosocial stress and sleep deprivation, have recently been associated with T2DM. 11 , 12
Mental health conditions are worsening worldwide, with an increment of 13% over the last decade. Mental health has a large impact on individuals, families, and communities and accounts for the largest disability‐adjusted life years (DALYs). 13 One of the important mental disorders that is prevalent among adults worldwide is stress. Stress is defined as a process in which environmental demands exceed the adaptive capacity of an organism, resulting in psychological and biological changes that may place persons at risk for disease. 14 , 15 Stress is being emphasized in the areas of mental health as it affects health of individuals in a broad range of categories. Stress is also reported prevalent among individuals suffering from noncommunicable diseases (NCDs). 16 , 17 Therefore, the aim of this paper is to examine the associations between psychosocial stress, sleep deprivation, and T2DM as well as to review the public health policies, programs, and guidelines developed and implemented in Malaysia to combat these issues for its population at large.
2. METHOD
The associations between psychological stress, sleep deprivation, and T2DM are multidomain and the associations could be complex. In this narrative review, we focus on psychological stress, sleep deprivation, and T2DM. Since psychological stress was in place for a very long time, as for prevalence, only papers published for the last 5 years were searched, which were between 2015 till 2020. A literature search was undertaken using the PubMed, Web of Science, and Google Scholar databases using different permutations and combinations of the key words: “prevalence” and “psychological stress” or “stress” or “mental health” or “mental disorders” and “sleep deprivation” or “sleep disorders” and “type 2 diabetes mellitus” or “type 2 diabetes” or “T2DM” or “diabetes mellitus” or “diabetes” and “Asia” or “Pacific” or “United States” or “United Kingdom” or “Europe” and “policy” or “guideline” or “initiatives” or “manual” or “program” and “Malaysia.” Only the articles published in English language were reviewed. Further references were consulted from reports published by international organizations, especially the World Health Organization (WHO) and national government and non‐government agencies such as Ministry of Health Malaysia, Malaysia Mental Health Association, and Malaysia Psychiatric Association. Literatures, reports and articles that were relevant were cited in this paper.
2.1. The associations between psychological stress, sleep deprivation, and T2DM
Psychological stress could be divided into three forms: personality traits such as hostility or anger; emotional disorders or states of distress such as anxiety or depression; and external stressors such as exposure to stressful conditions in early or adult life. 18 The Global Organization for Stress reported the prevalence of stress in multiple countries. In the United States, 75% of its adult population reported being stressed, meanwhile, in Australia, almost 50% of its adult population feel stressed about one part of their life. 19 In the United Kingdom, the prevalence of stress among its adult population was reported to be 74%. 20 In Sweden, the prevalence of stress reported from a nationally representative study among adults were 14.0%. 21 The prevalence of stress in India, based on a national mental health survey was 3.7%. 22 In Myanmar, it was reported that 18% of adults aged 18–49 years old suffer from stress. 23 In Malaysia, the National Health and Morbidity Survey (NHMS 2015) reported that 29%, one in three of its adult population suffered from mental distress. 24 Table 1 summarizes the prevalence of stress in selected countries worldwide.
TABLE 1.
Prevalence of stress according to country
| Country | Prevalence (%) | Source |
|---|---|---|
| United States (US) | 75.0 | Global Organization for Stress. Stress‐Related Facts and Statistics. 2020; http://www.gostress.com/stress‐facts/ |
| United Kingdom (UK) | 74.0 | Mental Health Foundation. Mental health statistics: stress: Result of Mental Health Foundation's 2018 study. 2020; https://www.mentalhealth.org.uk/statistics/mental‐health‐statistics‐stress |
| Australia | 50.0 | Global Organization for Stress. Stress‐Related Facts and Statistics. 2020; http://www.gostress.com/stress‐facts/ |
| Sweden | 14.0 | Höglund P, Hakelind C, Nordin S. Severity and prevalence of various types of mental ill‐health in a general adult population: age and sex differences. BMC psychiatry. 2020;20(209): 1–11. |
| India | 3.7 |
National Mental Health Survey of India. Prevalence of Mental Morbidity as per ICD−10 among Adults. 2020; http://indianmhs.nimhans.ac.in/nmhs‐results.php. Accessed 31 March, 2021. |
| Myanmar | 18.0 | Aye WT, Lien L, Stigum H, Win HH, Oo T, Bjertness E. The prevalence of mental distress and the association with education: a cross‐sectional study of 18‐ to 49‐year‐old citizens of Yangon Region, Myanmar. BMC Public Health. 2020;20(1): 94. |
| Malaysia | 29.0 | Institute for Public Health. National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non‐Communicable Diseases, Risk Factors & Other Health Problems. Malaysia: Ministry of Health Malaysia;2015. |
In general, when humans are exposed to stressful situations, activation of the sympathetic nervous system occurs. This coupled with the upregulation of the hypothalamic–pituitary–adrenal (HPA) axis results in increased release of the glucocorticoid cortisol from the adrenal cortex. 16 , 18 During stressful events, cortisol induces the release of lipids and glucose into the circulation system. In the case of T2DM, excessive amount of lipids and glucose with regards to cellular energy demands causes metabolic stress, which promotes insulin resistance and weight gain. 18 In terms of diabetes, glucose allostasis, a feedback loop occurs to control glucose metabolism and maintain equilibrium. In that situation, an increase in the level of glucose causes the increase in insulin secretion, thus maintaining glucose level in small amounts, while maintaining equilibrium. During psychological stress, allostatic load happens, which results in the regulatory system failing to operate within adaptive limit. 18
Humans spend one third of their time sleeping. Insomnia or common sleep disorder is defined as difficulties initiating or maintaining sleep, or early morning awakening associated with impaired daytime functioning, for example, reduced cognitive performance, fatigue, or mood disturbances. 25 Globally, about one third of the adult population reported insomnia symptoms, while 6%–10% met the criteria for insomnia disorder. 26 Sleep deprivation is one of the sleep disorders that is affecting human health.
Emerging evidence are reporting that qualitative and/or quantitative disruptions in human sleep results in adverse health outcomes––such as obesity, metabolic conditions, diabetes, and hypertension. 27 Ongoing sleep loss interrupts insulin secretion. When our body secretes more stress hormones (such as cortisol), this keeps people awake and makes it harder for insulin to do its job effectively, resulting in too much glucose remaining in the bloodstream. In turn, this increases the risk of developing diabetes. 28 , 29 , 30 In addition, having decreased amount of sleep also results in increased appetite and reduced level of satiety, resulting in increased craving for sugary and carbohydrate food. Overtime, this affects our insulin and blood glucose level. 31 Having a good night's sleep can be difficult in this modern world as many people are working around the clock and/or some are unable to “switch off” from their social media and gadgets. Thus, poor sleep quality remains one of the symptoms of various psychological conditions that should not be taken lightly.
2.2. Malaysia's policies, programs, and guidelines to address psychological stress and T2DM
With the rising prevalence of psychological stress, sleep deprivation, and T2DM, many countries have introduced policies and programs to combat these issues at the population level. In view of the rising prevalence and increasing burden of NCDs in Malaysia, the Ministry of Health has introduced the National Strategic Plan for Noncommunicable Diseases 2016–2025 (NSP‐NCD). 32 The NSP‐NCD 2016–2025 was developed in line with the mandates of the World Health Organization (WHO). It has five main objectives: strengthening national capacity, leadership, governance, multi‐sectoral partnerships to accelerate response for the prevention and control of NCD, reducing modifiable risk factors for NCDs and underlying social determinants through health‐promoting environments, strengthening health systems through primary healthcare and universal health coverage, promoting research and monitoring trends of NCD.
In orienting and aligning the health systems at the Primary Care Level the Enhanced Primary Health Care (EnPHC) Initiative was developed. 32 This includes boosting of the EnPHC model under the public and private health centers implementing new patient‐centered care models, parallel with disease management. The six major components in this care model are population enrollment, risk profiling, integrated care pathways for a cardiovascular care bundle––underpinned by digital health information technology, clinical and prescribing audit, information systems, and analytics and monitoring and organizational change––including development of Family Health Teams. 32
For effective implementation of the NSP‐NCD plan, an integrated approach involving many action plans and initiatives was developed. This includes the National Strategic Plan for Tobacco Control 2015–2020, Salt Reduction Strategy to Prevent and Control NCD for Malaysia 2015–2020, Malaysia Alcohol Control Action Plan 2013–2020, National Strategic Plan for Cancer Control Program 2016–2020, and the Komuniti Sihat Pembina Negara (KOSPEN) Initiative. Besides this, other initiatives outlined to combat T2DM include Policy Options to Combat Obesity in Malaysia 2016–2025 to prevent obesity focusing at (i) schools, (ii) higher learning education and workplace as well as (iii) general setting. 32 These policies are parallel with the National Plan of Action for Nutrition of Malaysia (NPANM) III 2016–2025. 32 The next initiative is the National Strategic Plan for Active Living 2016–2025 (NASPAL). This initiative was developed to promote physical activity programs in a holistic approach, not limited to government and health sectors, but also with the involvement of non‐health and non‐government sectors. 32 Some of the approaches used in NASPAL include strengthening public policy that support active living, provide environments, increase motivation and public health education, scale‐up behavior change programs, enhance collaboration, and firm up evaluation of programs, monitoring, and research. 32
Education plays an important role in disseminating public health information to community at large. There are several clinical‐based guidelines developed. The Clinical Practice Guidelines (CPG) Management of T2DM (5th Edition) was introduced by the Ministry of Health Malaysia. The aim of the guidelines is to provide evidence‐based recommendation to facilitate healthcare providers in the identification, diagnosis, and treatment of T2DM and be used for adolescents, adults, pregnant ladies as well as those who are at‐risk in developing T2DM. This CPG was developed based on strong scientific evidence and other guidelines on the management of T2DM, such as those from the American Diabetes Association (ADA). This CPG is used in all government facilities, such as hospitals and health clinics. 33 Much of emphasis was given in screening, diagnosis, treatment, and management of T2DM, such as Clinical Practice Guidelines Management of T2DM, Practical Guidelines for T2DM Insulin Treatment, and Medical Nutrition Therapy for T2DM and screening for Diabetes Retinopathy. 34 , 35 The CPG also described about mental health issues faced by people with diabetes. Sleep disturbance, poor quality of sleep, and obstructive sleep apnea has been reported among people with diabetes. Sleep disturbance and poor sleep quality are common among people with diabetes, whereas poor sleep quality is common among people with nocturnal hypoglycemia and obstructive sleep apnea is prevalent among adolescents with T2DM. 33 Moreover, since T2DM alters the physiologic changes in the body (increase in the release in stress hormones), therefore management of stress has been emphasized in the CPG, in order to manage T2DM well. 33
The introduction of Diabetes Education Manual 2016 addressed the gap between diabetes management and education. 34 This manual was developed with the objective to standardize the structure and content of T2DM education while taking into consideration individual needs. The manual was devised for care providers of T2DM such as nurses, assistant medical officers, medical practitioners, dietitians, pharmacists, physiotherapists, and clinical psychologists. 34 The manual includes education assessment, healthy eating, physical activity and exercise, medication, self‐monitoring, risk education, and behavioral intervention. 34 Sleep and stress has also been given a significant importance in managing T2DM. In the manual, it was recommended that the sleeping pattern of people with diabetes to be evaluated, in addition to managing emotional stress, as both were viewed as important in combating T2DM. 34
Malaysia's original mental health legislations and policies were developed since 1950's and it have been constantly revised from time to time. Revised and amended new legislations have also been introduced. In 2001, the Ministry of Health introduced the National Mental Health Act 36 and Mental Health Regulation in 2010, 37 with a purpose to establish a list of psychiatric care provisions, by both the government and private sectors. It encompasses the mental health healthcare service delivery such as treatment, control, comprehensive care, protection, and rehabilitation services of those with mental health issues. The Psychiatric and Mental Health Services Policy was published in November 2011. 38 This document contains important aspects of psychiatric service such as organization, asset requirements, human resources, patient management, clinical governance, and ethics. The objective behind the development of this policy is to facilitate hospital managers, mental health healthcare providers, and policy makers on the requirement, operation, and development of psychiatric services in the government health facilities. 38 In addition, the MOH also developed the National Mental Health Policy in 2012 that provides comprehensive strategies and guidelines to address issues in mental health. To date, MOH has produced guidelines, manuals, and training modules in some areas of mental health healthcare. As for psychological stress, through the Ministry of Health Malaysia's MyHEALTH portal a vast information on psychological stress, such as the causes of stress, symptoms to look out for stress, effects, coping, and prevention of stress as well as recommendations are provided. 39 The information provided was easy to access by anyone and it is written in a simple language, so as to make the information transferable to the community at large. 39
Mental health healthcare including psychological stress prevention and management is integrated into all primary healthcare centers. This integration is important in reducing stigma and encouraging those who need to seek treatment early. One such program introduced under the Community Mental Health Centers is called the Individual Placement & Support‐Supported Employment (IPS‐SE). 40 This program aims in the re‐employment of patients with mental health issues after undergoing the IPS‐SE program. 40
Furthermore, a screening questionnaire for psychological stress is also publicly available under the Ministry of Health Malaysia's official portal. The Depression, Anxiety and Stress Scale (DASS) is available from the website and can be used by both healthcare professionals as well as the members of the public. The instrument has been translated to the local language, Bahasa Melayu, so that it will be at ease to be used among members of the public. Upon self‐assessment, members of the public can head to the nearest healthcare centers to seek for further diagnosis and treatment. 41 In addition, this website also features posters on psychological stress named “Punca Stress” or sources of stress. It outlines the symptoms of and factors of stress. It is a brief poster that can be placed at public spaces to remind people about psychological stress, so that prevention could be taken. 41
Non‐governmental organizations in Malaysia have also played a prominent role in facilitating mental health issues. In 2019, the Malaysian Psychiatric Association together with the Malaysian Mental Health Association has introduced a handbook on common mental disorders titled “Mental Health Handbook.” The handbook outlines the common mental disorders in Malaysia, family, and social support, active steps that could be taken to manage mental health, self‐assessment forms, and mental health directory. 42 Some of the health promotion information is available online and can be easily accessed by anyone with internet service. Malaysia is moving toward web‐based health promotion initiative, with a portal like MyHEALTH by the Ministry of Health Malaysia. 43 In addition, with the mosaic of cultural diversity, education level, and socioeconomic status in Malaysia and with the rising of NCDs cases, both the government and private institutions have invested in the utilization of the internet to enhance public health in the country. 9 Table 2 summarizes the policies, programs, and guidelines targeted at NCDs and mental health issues in Malaysia.
TABLE 2.
Policies, programs, and guidelines on mental health and noncommunicable diseases in Malaysia
| Year Introduced | Type | Name |
|---|---|---|
| 2016 | Guidelines | Diabetes Education Manual |
| 2011 | Program | Individual Placement & Support‐Supported Employment (IPS‐SE) |
| 2013 | Program | Komuniti Sihat Pembina Negara (KOSPEN) Initiative |
| 2013 | Policy | Malaysia Alcohol Control Action Plan 2013–2020 |
| 2019 | Program | Mental Health Handbook by the Malaysian Psychiatric Association and the Malaysian Mental Health Association |
| 2008 | Program | MyHEALTH portal |
| 2001 | Act | National Mental Health Act, 2001 |
| 2012 | Policy | National Mental Health Policy, 2012 |
| 2016 | Policy | National Strategic Plan for Active Living 2016–2025 (NASPAL) |
| 2016 | Policy | National Strategic Plan for Cancer Control Program 2016–2020 |
| 2016 | Policy | National Plan of Action for Nutrition of Malaysia (NPANM) III 2016–2025. |
| 2016 | Policy | National Strategic Plan for Non‐Communicable Diseases 2016–2025 (NSP‐NCD) |
| 2015 | Policy | National Strategic Plan for Tobacco Control 2015–2020 |
| 2016 | Program | Primary Care Level the Enhanced Primary Health Care (EnPHC) Initiative |
| 2016 | Policy | Policy Options to Combat Obesity in Malaysia 2016–2025 |
| 2011 | Program | Punca Stress posters |
| 2011 | Policy | Psychiatric and Mental Health Services Operational policy |
| 2015 | Policy | Salt Reduction Strategy to Prevent and Control NCD for Malaysia 2015–2020 |
| 2015 | Guidelines | The Clinical Practice Guidelines (CPG) Management of T2DM, 2015 |
| 2011 | Guideline | The Depression, Anxiety and Stress Scale (DASS) |
Figure 1 shows the prevalence of mental health issues versus the programs that has been introduced to address those issues, from the year 1996 till 2019. The data were extracted from Malaysia's nationwide health and morbidity study called the National Health and Morbidity Survey (NHMS) by the Ministry of Health. 44 By observing the graph, generally, the prevalence of common psychiatric morbidity and depression increase over time, albeit introduction of programs, policies, and guidelines. But looking at the prevalence of depression in the years 2011 and 2019, there was only a slight increase of 0.5% (Figure 1). More studies need to be conducted to test the efficiency and efficacy of the programs, policies, and guidelines.
FIGURE 1.
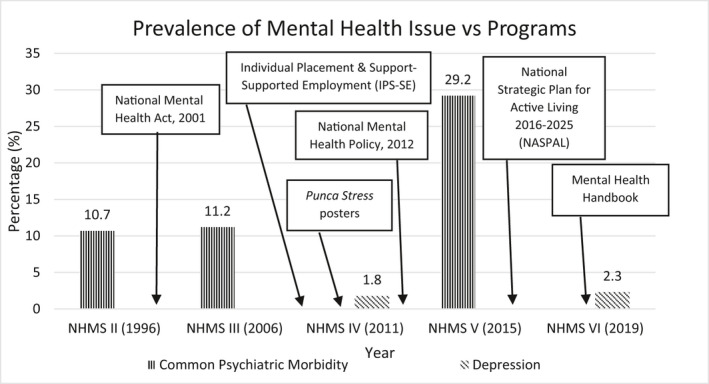
Prevalence of mental health issues and programs introduced
Evidence has shown that psychological stress and T2DM work interchangeably––psychological stress is associated with T2DM and T2DM is also related to psychological stress. 16 , 18 Therefore, in line with the CPG and Diabetes Education Manual 2016, it is hoped that these two national policies will facilitate better disease management and ultimately reduce psychological stress and sleep disturbance among people with T2DM.
3. CONCLUSION AND RECOMMENDATIONS
To date, increasing evidence has shown that besides the traditional risk factors, psychological stress and sleep deprivation may lead to T2DM via the increased release of stress hormone. With the increasing prevalence and high burden of disease, that is, cost of the treatment of T2DM, these additional risk factors need to be included in the prevention of T2DM. By understanding the pathophysiology between psychological stress, sleep deprivation, and T2DM, the relevant policies and programs in Malaysia are hoped to eradicate the issues. Efficacies of policies and programs ought to be measured by proper implementation and monitoring. Meanwhile, the integration of the internet and technology in facilitating health promotion to the population at large should be further emphasized as it is evident that it delivers health information to the community effectively.
There are many factors which facilitated the implementation of the policies, programs, and guidelines in combating NCDs and mental health issues in Malaysia, that are transferable to other countries seeking to introduce similar programs. First, it is through the good governance and leadership by government officials. The Malaysian government formed a committee called “Cabinet Committee for A Health Promoting Environment.” It aimed to determine policies that form a living environment which promotes positive behavioral changes among the Malaysian population, such as active lifestyle and healthy eating. 32 The effective implementation of heavy rules and regulation enforced by the Malaysian government have facilitated in combating NCDs. For an example, the Malaysian government has imposed a strict ban on smoking on all eateries and individuals caught smoking at this premises will be fined up to U$2444, which is very high on the peoples’ pocket for a simple breach of law. 45
In addition, health promotion via social media applications such as Facebook posts is garnering public attention at an advanced rate. In Malaysia, the Ministry of Health, through its official Facebook page, disseminates public health information to the population at large. A study further reported that health education posts, risk communication posts, and posts in the form of video are gaining higher attention from the public. 46 Besides that, multi‐sectoral collaborations, as described earlier, between the government, the Ministry of Health Malaysia, and non‐governmental organizations, such as Malaysian Mental Health Association and Malaysian Psychiatric Association, were deemed important in the development of policies and guidelines to address the NCDs as well as mental health issues in the country.
In this study, several limitations were noted. First, the effectiveness and outcomes of the implemented policies, programs, guidelines, and initiatives were not measured and reported. Therefore, future studies on the outcome and effectiveness of the implemented policies, programs, guidelines, and initiatives should be taken into consideration. Second, the policies, programs, guidelines, and initiatives reported in this study were based from Malaysia alone. Therefore, in the future, it is recommended to conduct a study to compare on the policies, programs, guidelines, and initiatives practiced in the neighboring Southeast Asian countries, as it would be interesting to look into various policies, programs, guidelines, and initiatives practice by other countries to combat similar issues, as to adopt the best practices.
This article is part of the Global Voices for Prevention of Noncommunicable Diseases Special Collection.
REFERENCES
- 1. American Diabetes Association . 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S13‐S27. [DOI] [PubMed] [Google Scholar]
- 2. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239‐2251. [DOI] [PubMed] [Google Scholar]
- 3. Ganasegeran K, Hor CP, Jamil MFA, et al. A systematic review of the economic burden of type 2 diabetes in Malaysia. Int J Environ Res Public Health. 2020;17(16):5723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . Diabetes. 2020; https://www.who.int/health‐topics/diabetes#tab=tab_1. Accessed 8 August, 2020.
- 5. Diabetes UK . Type 2 diabetes. 2020; https://diabetesmanagementnc.com/wp‐content/themes/dmnc2020/downloads/DMNC_FactSheet_Diabetes‐Jan2020.pdf. Accessed 8 August, 2020.
- 6. Diabetes.co.uk . Diabetes prevalence. 2020; https://www.diabetes.co.uk/diabetes‐prevalence.html. Accessed 25 September, 2020.
- 7. Davis WA, Peters KE, Makepeace A, et al. Prevalence of diabetes in Australia: insights from the fremantle diabetes study phase II. Intern Med J. 2018;48(7):803‐809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of diabetes and relationship with socioeconomic status in the Thai population: national health examination survey, 2004–2014. Journal of Diabetes Research. 2018;2018(2018):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Noman M, Koo AC, Tee SH, Krishnan M. Web elements for health promotion in Malaysia. Health Promotion International. 2020;35(3):458‐469. [DOI] [PubMed] [Google Scholar]
- 10. Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963‐970. [DOI] [PubMed] [Google Scholar]
- 11. Dong G, Qu L, Gong X, Pang B, Yan W, Wei J. Effect of social factors and the natural environment on the etiology and pathogenesis of diabetes mellitus. Int J Endocrinol. 2019;2019:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siddiqui A, Desai NG, Sharma SB, Aslam M, Sinha UK, Madhu SV. Association of oxidative stress and inflammatory markers with chronic stress in patients with newly diagnosed type 2 diabetes. Diabetes Metab Res Rev. 2019;35(5):1‐8. [DOI] [PubMed] [Google Scholar]
- 13. World Health Organization . Mental Health. 2020; https://www.who.int/health‐topics/mental‐health#tab=tab_2. Accessed 7th August 2020.
- 14. Cohen S, Kessler RC, Gordon LU. Strategies for Measuring Stress in Studies of Psychiatric and Physical Disorders. New York: Oxford University Press; 1995. [Google Scholar]
- 15. Wahed WYA, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria J Med. 2017;53(1):77‐84. [Google Scholar]
- 16. Agorastos A, Pervanidou P, Chrousos GP, Baker DG. Developmental trajectories of early life stress and trauma: a narrative review on neurobiological aspects beyond stress system dysregulation. Front Psychiatry. 2019;2019(10):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization . Mental health action plan 2013–2020. Geneva: World Health Organization; 2013. [Google Scholar]
- 18. Hackett RA, Steptoe A. Type 2 diabetes mellitus and psychological stress—a modifiable risk factor. Nat Rev Endocrinol. 2017;13(9):547. [DOI] [PubMed] [Google Scholar]
- 19. Global Organization for Stress . Stress related facts and statistics. 2020; http://www.gostress.com/stress‐facts/. Accessed 8 August, 2020.
- 20. Mental Health Foundation . Mental health statistics: stress: result of mental health foundation's 2018 study. 2020; https://www.mentalhealth.org.uk/statistics/mental‐health‐statistics‐stress. Accessed 8 August, 2020.
- 21. Höglund P, Hakelind C, Nordin S. Severity and prevalence of various types of mental ill‐health in a general adult population: age and sex differences. BMC psychiatry. 2020;20(209):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Mental Health Survey of India . Prevalence of Mental Morbidity as per ICD‐10 among Adults. 2020; http://indianmhs.nimhans.ac.in/nmhs‐results.php. Accessed 31 March, 2021.
- 23. Aye WT, Lien L, Stigum H, Win HH, Oo T, Bjertness E. The prevalence of mental distress and the association with education: a cross‐sectional study of 18–49‐year‐old citizens of Yangon Region, Myanmar. BMC Public Health. 2020;20(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Institute for Public Health . National health and morbidity survey 2015 (NHMS 2015). Vol. II: Non‐Communicable Diseases, Risk Factors & Other Health Problems. Malaysia: Ministry of Health Malaysia; 2015. [Google Scholar]
- 25. Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675‐700. [DOI] [PubMed] [Google Scholar]
- 26. American Psychiatric Association . What Are Sleep Disorders? 2020; https://www.psychiatry.org/patients‐families/sleep‐disorders/what‐are‐sleep‐disorders#:~:text=Sleep%20disorders%20(or%20sleep%2Dwake,%2C%20anxiety%2C%20or%20cognitive%20disorders. Accessed 14 September, 2020.
- 27. Karthikeyan R, Spence DW, Pandi‐Perumal SR. The contribution of modern 24‐hour society to the development of type 2 diabetes mellitus: the role of insufficient sleep. Sleep Science. 2019;12(3):227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Arora T, Chen MZ, Omar OM, Cooper AR, Andrews RC, Taheri S. An investigation of the associations among sleep duration and quality, body mass index and insulin resistance in newly diagnosed type 2 diabetes mellitus patients. Ther Adv Endocrinol Metab. 2016;7(1):3‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bush B, Hudson T. The role of cortisol in sleep. Nat Med J. 2010;2(6):26–29. [Google Scholar]
- 30. Hackett RA, Dal Z, Steptoe A. The relationship between sleep problems and cortisol in people with type 2 diabetes. Psychoneuroendocrinol. 2020;117:104688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lombardo C, Ballesio A, Gasparrini G, Cerolini S. Effects of acute and chronic sleep deprivation on eating behaviour. Clinical Psychologist. 2020;24(1):64‐72. [Google Scholar]
- 32. Ministry of Health Malaysia . National Strategic Plan for Non‐Communicable Diseases (NSP‐NCD) 2016–2025. Malaysia: Putrajaya; 2016. [Google Scholar]
- 33. Ministry of Health Malaysia . Clinical Practice Guidelines: Management of Type 2 Diabetes Mellitus. Malaysia: Ministry of Health, Malaysia; 2015. [Google Scholar]
- 34. Malaysian Diabetes Educators Society . Diabetes Education Manual 2016. Malaysia: The Malaysian Diabetes Educators Society; 2016. [Google Scholar]
- 35. Ministry of Health Malaysia . Management of Type 2 Diabetes Mellitus. Putrajaya: Ministry of Health; 2015. [Google Scholar]
- 36. Laws of Malaysia: Act 615: Mental Health Act 2001, 615(2001). Published by: The Commissioner of Law, Malaysia. [Google Scholar]
- 37. Ministry of Health Malaysia . Malaysian Mental Health Regulation 2010. Kuala Lumpur, Malaysia: Ministry of Health; 2010. [Google Scholar]
- 38. Ministry of Health Malaysia . Psychiatric and Mental Health Services Operational Policy. Malaysia: Ministry of Health Malaysia; 2011. [Google Scholar]
- 39. Ministry of Health Malaysia . Stress management. 2020. Offcial Portal of MyHEALTH 2020; http://www.myhealth.gov.my/en/stress‐management/. Accessed 16 September, 2020.
- 40. Ministry of Health Malaysia . Ministry of Health Strategic Plan 2016–2020. Malaysia: Ministry of Health Malaysia Planning Section; 2016. [Google Scholar]
- 41. Ministry of Health Malaysia . Mental health unit module. 2020; https://www.moh.gov.my/index.php/pages/view/1926. Accessed 16 September, 2020.
- 42. Malaysian Mental Health Association & Malaysian Psychiatric Association . Mental Health Handbook. Published: 12 November 2019. [Google Scholar]
- 43. Ministry of Health Malaysia . Official portal of MyHEALTH. 2020; http://www.myhealth.gov.my/en/. Accessed 17 September, 2020.
- 44. Institute for Public Health . National health & morbidity survey. 2021; http://iku.moh.gov.my/nhms. Accessed 31 March, 2021.
- 45. Library of Congress . Malaysia: ban on smoking in all eateries comes into effect. 2019; https://www.loc.gov/law/foreign‐news/article/malaysia‐ban‐on‐smoking‐in‐all‐eateries‐comes‐into‐effect/. Accessed 26 October, 2020.
- 46. Rahim A, Ibrahim M, A. Salim F, Ariffin M. Health information engagement factors in Malaysia: a content analysis of Facebook use by the ministry of health in 2016 and 2017. Int J Environ Res Public Health. 2019;16(4):591. [DOI] [PMC free article] [PubMed] [Google Scholar]


