Abstract
Background
Young oncologists are at particular risk of professional burnout, and this could have a significant impact on their health and care of their patients. The coronavirus disease 2019 (COVID-19) pandemic has forced rapid changes in professionals' jobs and training, with the consequent physical and psychological effects. We aimed to characterize burnout levels and determinants in young oncologists, and the effects of the pandemic on their training and health.
Methods
Two online surveys were conducted among oncology residents and young oncology specialists in Spain. The first addressed professional burnout and its determinants before the COVID-19 pandemic, while the second analyzed the impact of the pandemic on health care organization, training, and physical and psychological health in the same population.
Results
In total, 243 respondents completed the first survey, and 263 the second; 25.1% reported significant levels of professional burnout. Burnout was more common among medical oncology residents (28.2%), mainly in their second year of training. It was significantly associated with a poor work–life balance, inadequate vacation time, and the burnout score. Nearly three-quarters of respondents (72%) were reassigned to COVID-19 care and 84.3% of residents missed part of their training rotations. Overall, 17.2% of this population reported that they had contracted COVID-19, 37.3% had scores indicating anxiety, and 30.4% moderate to severe depression. Almost a quarter of young oncologists (23.3%) had doubts about their medical vocation.
Conclusions
Burnout affects a considerable number of young oncologists. The COVID-19 pandemic has had a profound impact on causes of burnout, making it even more necessary to periodically monitor it to define appropriate detection and prevention strategies.
Key words: professional burnout, young oncologists, residents, cancer care, COVID-19
Highlights
-
•
Oncologists are susceptible to burnout. The COVID-19 pandemic has significantly impacted health care workers' mental health.
-
•
This study analyzes professional burnout and its determinants as well as the impact of COVID-19 among young oncologists.
-
•
Ensuring specialized training and preventing burnout are essential to ensure quality medical oncology care in the future.
Introduction
In recent years, the impact of the emotional well-being of health professionals on the quality of patient care has become evident. Cancer care professionals in particular are well known to be at special risk of developing burnout syndrome, due mainly to direct contact with seriously ill patients and their families and a continuously changing medical landscape.
The 11th revision of the International Classification of Diseases (ICD-11) defines burnout as a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: feelings of energy depletion or exhaustion; increased mental distance from one's job, or feelings of negativism or cynicism related to one's job; and reduced professional efficacy.1,2
Professional burnout is an important issue for health care systems, with potentially significant consequences on the quality of patient care. Studies indicate that physician burnout affects quality of care, patient safety, and patient satisfaction.3 It also carries numerous personal costs4 with a subsequent effect on organizational costs, including absenteeism, increased turnover, and a decline in job performance. Understanding the variety of factors that are responsible for professional burnout will help highlight key leverage points for prevention.5
Young oncologists (oncology residents and oncology specialists in their first 5 years of practice) are a special risk population, due to a heavy workload, academic pressure, and other specific factors related to cancer care.6 Low perceived health status and a desire to leave medicine or change specialty are significantly associated with burnout, according to a study conducted among hematology and medical and radiation oncology residents.7 An European Society for Medical Oncology (ESMO) study of professional burnout in young European oncologists showed that it is common in this population, although rates vary across regions. It reported that achieving a good work–life balance, access to support services, and adequate vacation time may reduce burnout levels.8
A more recent study showed that to reduce professional burnout and restore job satisfaction, organizations should achieve the following three primary goals: meet human social and psychological needs, eliminate or mitigate structural and functional drivers of burnout, and strengthen individual resilience.9 Evidence suggests that investing in reducing burnout and promoting engagement is fully justified and return on investment measurable.10
During the analytical phase of the study, we witnessed the worldwide emergence of the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated coronavirus disease 2019 (COVID-19). This precipitated a global health problem that was declared a pandemic on 11 March 2020. By the closing of this article on 7 June 2021, 173 005 553 cases had been diagnosed worldwide, with a total of 3 727 605 confirmed deaths, of which 80 099 occurred in Spain.11 As a result, our health systems had to be reorganized to attend the large number of COVID-19 patients.
A recent ESMO study has shown, for the first time, how COVID-19 is impacting the well-being and job performance of oncology professionals,12 indicating that urgent measures to address well-being and improve resilience are essential.
Since previous studies have shown that doctors in training and specialists in their first years of practice are especially susceptible to burnout,13,14 we focused on the impact of COVID-19 on the young oncologist population in Spain in terms of occupational, educational, and psychological effects, and propose a set of interventions that might help minimize the impact of future COVID-19 waves or similar health emergencies.
Methods
We conducted a study to assess the prevalence of burnout among young oncologists in Spain, before and after the onset of the SARS-CoV-2 pandemic. Work and lifestyle factors were also investigated in this population to evaluate their potential correlation with burnout levels and to define specific interventions to reduce and prevent burnout.
The study was supported by the Spanish Society of Medical Oncology (SEOM) + MIR Section [represented by 12 oncologists, including specialists, residency mentors, and resident medical interns (or MIR, Médico Interno Residente)], a section devoted to analyzing and addressing the specific concerns of young medical oncologists in Spain.
Pre-COVID-19 burnout analysis
A survey based on the validated Maslach Burnout Inventory–Human Services Survey for Medical Personnel (MBI-HSS MP)2 was conducted to analyze pre-pandemic burnout levels amongst young Spanish oncologists (residents and oncologists in the first 5 years of their professional career). This online survey remained open for 7 months and 15 days, between 16 May and 31 December 2019. It was sent individually to a total of 913 young oncologists. The survey consists of 22 items on work and emotional reactions toward it. The respondent must answer each item by expressing how often they have experienced that feeling. Answers range from 0 to 6, as follows: 0: never; 1: a few times a year or less; 2: once a month or less; 3: a few times a month; 4: once a week; 5: a few times a week; and 6: every day. Burnout syndrome was also classified following the model defined by Leiter and Maslach in 2016, which classifies the syndrome into five profiles15 based on the results obtained in each of the three dimensions of burnout: exhaustion, cynicism, and efficacy (see Supplementary Table S1, available at https://doi.org/10.1016/j.esmoop.2021.100215). Participants were classified into five profile groups according to the reported answers: (i) Burnout: problematic results on both emotional exhaustion and depersonalization; (ii) Disengaged: high depersonalization score. The disengaged individual has energy and confidence but finds it difficult to dedicate themselves to their work; (iii) Overextended: high emotional exhaustion score. The individual is fulfilled and involved, but emotionally drained; (iv) Ineffective: low personal accomplishment score, characterized by diminished feelings of competence and successful achievement in one's work; and (v) Engaged: scores well on all three scales.
Twenty-three additional questions were added to explore work and lifestyle factors in terms of demographics, workplace, and lifestyle (see Supplementary Material, available at https://doi.org/10.1016/j.esmoop.2021.100215).
Statistical analyses, including linear regression, were carried out to test the relationships between overall burnout score and work and lifestyle factors. This statistical analysis was carried out using IBM SPSS Statistics v27 software (Armonk, NY). A linear regression model was fitted to assess the association between overall burnout score and work and lifestyle factors, using the overall burnout score (total of three individual subscales) as a continuous variable. Two types of association analyses, univariate and multivariate, were conducted. Variables that were significantly associated with the presence of burnout in the univariate analysis were included in the multivariate analysis. All P values <0.05 were considered statistically significant.
COVID-19 impact analysis
An online questionnaire was designed to study the effect of the pandemic on young oncologists (see Supplementary Material, available at https://doi.org/10.1016/j.esmoop.2021.100215). The survey consisted of 23 questions on employment status, COVID-19 data, health care and training activities, and three psychological questionnaires [Professional Quality of Life Scale-30 (ProQOL-30),16 Generalized Anxiety Disorder-7 (GAD-7),17and Patient Health Questionnaire-9 (PHQ-9)18].
The Eval&GO platform (https://www.evalandgo.com/es/) was used to design and administer the online survey. This online survey is compliant with General Data Protection Regulation rules and the confidentiality and anonymity of the participants are guaranteed.
Psychological scales
To analyze the psychological status among this same population during the pandemic, three specific validated questionnaires were used (see COVID-19 impact survey in the Supplementary Material, available at https://doi.org/10.1016/j.esmoop.2021.100215).
ProQOL-30 questionnaire
This scale is used to measure the positive and negative effects of helping others who experience suffering and trauma. ProQOL has subscales for compassion satisfaction, burnout, and compassion fatigue.
GAD-7 questionnaire
This is a seven-item instrument to measure or assess the severity of anxiety.
PHQ-9 questionnaire
This scale helps to screen for depression and grade severity of symptoms in general medical and mental health settings.
The online survey designed to analyze the impact of COVID-19 remained open for 26 days, between 12 June and 8 July 2020. This period coincided with a fall in the number of cases detected in Spain, when most of the country was in the advanced stages of lockdown de-escalation. The invitation and link to access the survey were sent individually by e-mail to a total of 952 physicians, including 482 residents and 470 medical oncologists in their first 5 years post-residency, comprising a geographical and profile sample representative of the whole country.
Results
Burnout survey: participant demographics and lifestyle
A total of 243 completed surveys were received, with a response rate of 26.6%. The sample was representative in terms of age, sex, geographic region, and professional profile (residents and specialists). Most participants were between 26 and 30 years of age. Distribution of participants according to the year of residency was homogeneous, with a slight predominance of fourth-year residents (31.3%). Respondents' demographics and work and lifestyle data are summarized in Table 1.
Table 1.
Burnout survey participant demographics
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 93 (38.3) |
| Female | 147 (60.5) |
| Prefer not to answer | 3 (1.2) |
| Position | |
| Resident | 131 (53.9) |
| Specialist (first 5 years of career) | 96 (39.5) |
| Prefer not to answer | 16 (6.6) |
| Residents by year | |
| First-year resident | 12 (9.2) |
| Second-year resident | 28 (21.4) |
| Third-year resident | 29 (22.1) |
| Fourth-year resident | 41 (31.3) |
| Fifth-year resident | 21 (16.0) |
| Age range (years) | |
| 21-25 | 8 (3.3) |
| 26-30 | 122 (50.2) |
| 31-35 | 95 (39.1) |
| 36-40 | 11 (4.5) |
| 41-45 | 4 (1.6) |
| >45 | 1 (0.4) |
| Prefer not to answer | 2 (0.8) |
| Hospital type | |
| University hospital | 205 (84.4) |
| Cancer center | 10 (4.1) |
| General hospital | 21 (8.6) |
| Private clinic | 5 (2.1) |
| Other | 2 (0.8) |
| Lifestyle and work factors | |
| 1. Currently in a relationship | |
| Yes | 183 (75.3) |
| No | 53 (21.8) |
| Prefer not to answer | 7 (2.9) |
| 2. Has children | |
| Yes | 34 (14.0) |
| No | 208 (85.6) |
| Prefer not to answer | 1 (0.4) |
| 3. Perceived good work–life balance | |
| Yes | 86 (35.4) |
| No | 150 (61.7) |
| Prefer not to answer | 6 (2.9) |
| 4. Lives alone | |
| Yes | 65 (26.7) |
| No | 177 (72.8) |
| Prefer not to answer | 1 (0.4) |
| 5. Perceived sufficient vacation time | |
| Yes | 92 (37.9) |
| No | 145 (59.7) |
| Prefer not to answer | 6 (2.5) |
| 6. Hospital offers psychological support services | |
| Yes | 23 (9.9) |
| No | 156 (64.2) |
| Prefer not to answer | 63 (25.9) |
| 7. Work commute (minutes) | |
| 0-15 | 81 (33.3) |
| 15-30 | 98 (40.3) |
| 30-45 | 37 (15.2) |
| 45-60 | 23 (9.9) |
| 60-90 | 2 (0.8) |
| 90-120 | 1 (0.4) |
| >120 | 0 (0.0) |
Most respondents (84.4%) worked in a university hospital. Almost two-thirds (64.2%) of them reported that their hospitals did not offer their physicians access to psychological support, while 61.7% believed that they did not have a good work–life balance.
The most effective measure to alleviate the risk of burnout identified by respondents was to reduce the number of patients seen, increase the time per patient, and relieve the burden of care. Offering anti-stress sessions, psychological help, or in-hospital support was also widely proposed by the respondents.
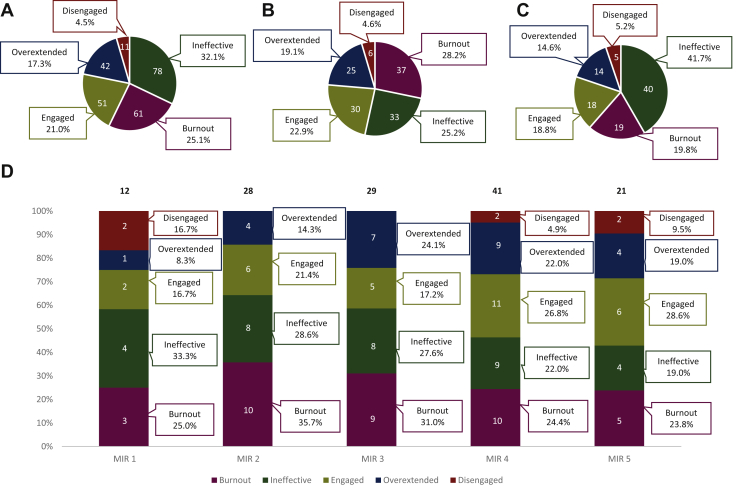
Burnout status
One-quarter of the young medical oncologist population was identified as having a burnout profile. The predominant profile was ineffective, representing 32.1% of the population analyzed. The proportion of burnout profiles was higher among medical oncology residents (28.2%) than among young specialists (19.8%), and higher in men (29.0%) than in women (22.5%). Moreover, the highest percentage of burnout profiles was observed in second-year residents (35.7%). These figures gradually decreased, in parallel with an increase in the engaged profile (Figure 1).
Figure 1.
Burnout rates among young Spanish oncologists.
(A) Overall burnout profile types. (B) Burnout profiles among medical oncology residents. (C) Burnout profiles among young specialists. (D) Burnout profiles among residents by year of residency. Five burnout profiles are based on the three dimensions (exhaustion, cynicism, and inefficacy) of the Maslach Burnout Inventory (MBI): burnout (score high on all three dimensions), engagement (score low on three dimensions), overextended (high on exhaustion only), disengaged (high on cynicism only), and ineffective (high on inefficacy only).
MIR, Médico Interno Residente.
A multivariate correlation analysis was carried out using the burnout score and demographic and lifestyle variables. Younger age (P = 0.005), perceived lack of leisure time (P = 0.043) or vacation time (P < 0.0001), and a poor perception of work–life balance (P < 0.0001) were variables positively associated with burnout; these four items were independent prognostic factors. The variables living alone and having children were removed for the multivariate analysis as they were not statistically significant (see Table 2).
Table 2.
Multivariate correlation analysis
| Variable | Coefficient (95%CI) P value |
|---|---|
| Burnout score | |
| Age | −3.55 (−6.02 to 1.09) P = 0.005 |
| Hours of recreational activities | −0.20 (−0.40 to 0.01) P = 0.043 |
| Perceived lack of work–life balance | 7.85 (3.89 to 11.82) P < 0.0001 |
| Perceived lack of vacation time | 7.94 (4.08 to 11.81) P < 0.0001 |
CI, confidence interval.
COVID-19 impact survey: participant demographics and lifestyle
A total of 263 responses were received (27.6% participation rate), of which 91 (34.6%) were from oncology specialists and 172 (65.4%) from residents, most of whom were in their third or fourth year; 87 of the respondents (33.1%) had also completed the previous burnout survey. The median age of respondents was 30 years. Nearly 21.7% reported having risk factors for severe SARS-CoV-2 (see Table 3).
Table 3.
COVID-19 impact survey participants' demographics
| Variable | n (%) |
|---|---|
| Gender | |
| Men | 105 (39.9) |
| Women | 158 (60.1) |
| Employment situation during the pandemic | |
| First and second year | 47 (17.9) |
| Third and fourth year | 83 (31.6) |
| Fifth year | 42 (16.0) |
| Medical oncologist for 1-5 years | 91 (34.6) |
| Age, years (median) | 30 |
| Participants with risk factors for severe COVID-19 | |
| No | 206 (78.3) |
| Yes | 57 (21.7) |
COVID-19, coronavirus disease 2019.
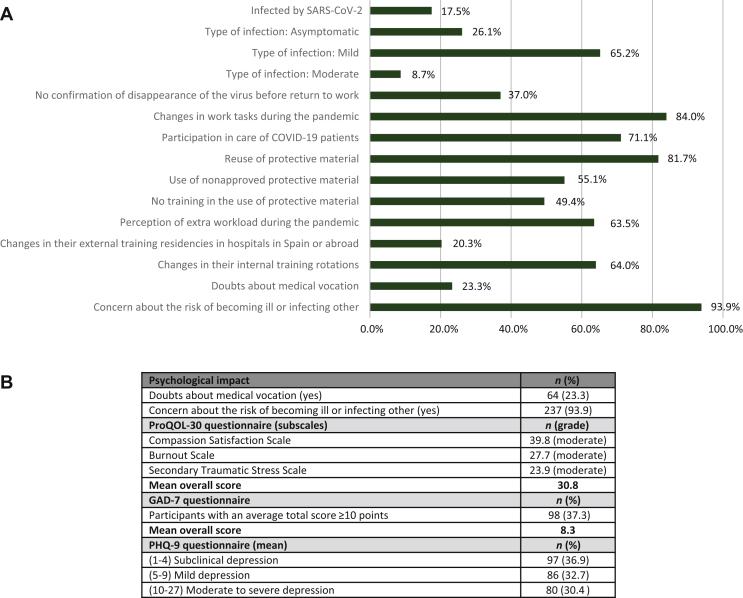
COVID-19 impact survey
Physical impact
In total, 46 respondents (17.2%) reported having been infected with SARS-CoV-2. Most of them had mild or asymptomatic forms of the illness and only 8.7% developed a moderate form of viral pneumonia, with or without hospital admission (see Figure 2A).
Figure 2.
COVID-19 impact survey: main findings.
(A) Physical, occupational, and training impact. (B) Psychological impact.
COVID-19, coronavirus disease 2019; GAD-7, Generalized Anxiety Disorder-7; PHQ-9, Patient Health Questionnaire-9; ProQOL-30, Professional Quality of Life Scale-30; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Occupational and training impact
Most respondents (84%) reported changes in their daily work tasks; 71% of survey respondents participated in COVID-19 patient care in the first wave of the pandemic.
Over 84% of residents reported some disruption of their planned training program, with 64% reporting changes in their internal training rotations and 20.3% in their external training residencies in hospitals in Spain or abroad. The participation of medical oncologists in the care of COVID-19 patients has been high. Specifically, residents' professional activity was primarily centered on hospital wards and emergency departments, while remote monitoring was led by oncology specialists.
Psychological impact
See Figure 2B for detailed information regarding psychological impact.
Sixty-four participants (23.3%) reported having doubts about their medical vocation. Almost 94% were concerned at some point with becoming infected or infecting others.
Results of the ProQOL-30 questionnaire on professional quality of life
In the three subscales, the mean scores were in the range of moderate impairment of professional quality of life.
Results of the GAD-7 questionnaire for generalized anxiety disorder screening
A total of 37.3% of respondents had a mean score >10, indicating an increased risk of suffering a anxiety.
Results of the PHQ-9 questionnaire for major depressive disorder screening
A total of 30.4% of respondents obtained scores within the range of moderate to severe symptoms of depression.
Overall, the results showed that, during the COVID-19 pandemic, one-third of the professionals tested had scores indicating anxiety and moderate depression levels.
Young oncologists' proposals for improvement
The main improvements noted by the survey respondents were related to providing sufficient care, recognition, and remuneration to young oncologists for their work during the pandemic, and improved work distribution and organization. The respondents also strongly demanded that residents' training during the pandemic be guaranteed.
Discussion
For medical oncologists and many other specialties, training is one of the most intense and challenging periods in their working life. Medical oncology is a wide-ranging and highly demanding specialty. Rapid changes as new scientific evidence emerges require that clinicians remain abreast of the latest developments, in addition to a strong daily commitment and adaptability, especially when starting out on their career. Young medical oncologists and residents have experienced an added burden caused by the COVID-19 pandemic, which has profoundly disrupted their daily life, training, and health. The real impact of the pandemic on the mental and physical health of young oncologists is still unknown, but these individuals, who are immersed in an intensive few years of training, are especially vulnerable.
The aim of this study was to investigate the prevalence and characteristics of burnout syndrome in young oncologists, and the effect that the pandemic has had on their health and training.
Previous studies have indicated the need to investigate the causes of burnout among young medical professionals as a growing trend.19,20 In the case of young oncologists in Spain, along these lines, our study showed that the overall prevalence of burnout profile among young oncologists and residents was 25.1%, reaching a peak in the second year of training (35.7%). During the first year of residence, the trainees are assigned to different training rotations in the main specialties of general medicine. In the second year, they usually enter the clinical oncology department. Although there may be several causes for the second-year burnout peak, one possible explanation is that this transition may be difficult for residents.
Our study is one of the first to date to specifically describe the evolution of burnout profiles over time during the early years of the medical oncologist's professional career. Furthermore, multiple variables were identified as significantly correlated with the appearance of burnout: a perceived lack of time spent on leisure activities and vacations, a younger age, and a difficulty in achieving a balance between work and family life. Our data are consistent with the results obtained from previous studies that suggested that burnout is common amongst young European oncologists, reaching a prevalence between 44% and 79.1%7,8 but with important variations between countries across Europe. They suggested that achieving a good work–life balance, access to support services, and adequate vacation time may reduce burnout levels, and recommended raising awareness, support, and interventional research.
Organizational research has shown that institutional resources are essential for optimizing the clinical practice environment and promoting the well-being of clinicians.6 On an individual level, emphasis has been placed on the importance of identifying burnout symptoms, acquiring resilience skills, and building positive relationships among colleagues. Interventions, such as psychological support, lecture series, or contact with colleagues,21 are key to both identifying and reducing burnout. Our findings highlighted differences in burnout profiles and the need for adapted interventions to prevent and reduce burnout among young oncologists, reinforcing the need for interventions to improve work–life balance and stress management. These efforts should focus on the early years of training as when professional the burnout profile is more prevalent.
The COVID-19 pandemic has added countless challenges to this already sensitive situation. The training program of 84.3% of the residents surveyed had been disrupted, and electives in other hospitals in Spain and abroad were suspended. Due to demands on the organization of care and the provision of services, it is very unlikely that these rotations will be rescheduled or even conducted at all.
Almost three-quarters of respondents (71.1%) were reassigned to COVID-19 care under clearly inadequate working conditions and almost a fifth were infected by COVID-19, rates that are clearly higher than overall rates among European health professionals (8.5%)22 and those reported by other specialties.23 A recent study of a group of young oncologists in France reported that only one-third was reassigned to COVID-19 care. Almost 70% of French oncologists had adequate, adapted personal protective equipment (PPE), compared to <30% of our sample.24
In addition to the impact on physical health, the mental health of professionals was also analyzed. The results revealed that 37.3% had scores indicating anxiety, and 30.4% moderate to severe depression. As a study limitation, we should point out that these findings are only based on psychological questionnaires, and a clinical interview may be necessary to confirm a diagnosis; furthermore, we have no data to compare with the situation before the COVID-19 pandemic. Overall, respondents reported a moderate deterioration in the quality of their working life. Alarmingly, 23.4% had doubts about their medical vocation. The cumulative effect of constant overexertion and the lack of adequate training may further aggravate the effects that the pandemic is having on these professionals.25 These levels are similar to those observed in European studies, where 25% of participants indicated being at risk of distress (poor well-being), 38% reported feeling burnout, and 66% reported not being able to perform their job compared with the pre-COVID-19 period.12
Despite these figures, 64.2% of respondents said that they did not have access to psychological support in their workplace. It is striking in the face of such alarming data that so few measures are in place to reduce burnout among young professionals in this critical situation. Most survey respondents noted the importance of caring for oncology residents, as well as recognizing and remunerating their efforts during the pandemic.
Given the likelihood of future waves and foreseeable infection outbreaks, the psychological effects of the pandemic in this group should be monitored and prevented in the mid and long term. It is also important to highlight the future impact on the mental health of these professionals associated with neglecting chronic non-COVID-19 diseases detected after the pandemic.
In short, this study reveals even more worrisome data on the physical and mental health of young Spanish oncologists than similar studies carried out in other countries. We believe that these differences are largely due to the dramatic situation that Spain found itself in during the first wave of the pandemic, which saw a mortality rate of 62.1/100 000 inhabitants.26 As the ESMO Resilience Task Force points out, one of the main predictors of well-being and job performance in oncologists was the COVID-19 mortality rate in the reference country.12 Spain was one of the first countries in the world in which the disease spread on a large scale, when medical knowledge was still scant, and the infrastructures to respond to it (PPE, dedicated units, specialized personnel, etc.) were virtually nonexistent.
A potential limitation of our study is the selection bias of an online survey, as individuals who have experienced more extreme and more negative situations are most likely to respond. The time frame in which the survey was conducted could also have influenced our findings. The current pandemic has evolved constantly, changing the health care landscape rapidly and without precedent, and the responses obtained would probably have been different if the data had been collected at the peak of the first wave (end of March 2020). Another main limitation of the study is that it is not possible to compare the psychological status of this population before and after the pandemic, as we used different scales. We considered using the MBI-HSS MP to measure burnout levels to compare our data with previous international studies. However, we eventually decided to use psychological scales during the pandemic to evaluate issues not only related to the occupational context, as we already knew the baseline burnout levels in our population, which was indicative of a population at special risk for impact by additional psychological stress. Despite this limitation, we believe that our paper establishes an appropriate connection between the two studies, since it involves the same study population: medical oncology residents and newly trained young specialists, in two different scenarios (pre- and post-pandemic) with up to 33.1% of respondents participating in both studies (2019 and 2020).
Based on the results obtained in these two surveys and the suggestions provided by the respondents of the second, we also propose a series of measures aimed at reducing burnout in our specialty. In terms of prevention, we consider it essential not to exceed the established working hours so as to guarantee leisure and vacation time. In terms of detection and management, we propose more exhaustive mentoring in critical periods of residency, such as the second year, to detect and address burnout, as well as progressive integration into the medical oncology department. It is also necessary to implement psychological counseling programs for doctors who need them. Regarding the current COVID-19 pandemic situation, it is essential that young oncologists do not miss training in their specialty or in the safe management of infected patients. Recognition and remuneration of young doctors who have been in the front line during the pandemic should also be reconsidered.
This nationwide survey highlights worrisome and previously unknown data on pre-pandemic burnout profiles of residents and young specialists in medical oncology, and a preliminary approach to the COVID-19 impact. According to the pre-pandemic situation and the predicted long-term COVID-19 pandemic effects, burnout detection and prevention strategies are highly necessary. Interventions aimed at improving the work–life balance, stress management, and training of young Spanish oncologists could be effective in improving their mental and physical health and ensure better health care for cancer patients in the long term.
Acknowledgements
We thank SEOM for their technical and human support. The analysis of the psychological impact was made possible thanks to the help of Dr. Annabel Cebrià with the psychological questionnaires. This report has been possible thanks to the collaboration of the MIR community that participated in the survey and the Spanish Society of Medical Oncology (SEOM), and the SEOM + MIR section in particular. The project received technical support from Ascendo Sanidad & Farma.
Funding
This project received funding from the Spanish Society of Medical Oncology (SEOM).
Disclosure
The authors have declared no conflict of interest.
Supplementary data
References
- 1.Burn-out an “occupational phenomenon”: International Classification of Diseases. WHO; 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases Available at. [Google Scholar]
- 2.Maslach C., Jackson S.E., Leiter M.P., Schaufeli W.B., Schwab R.L. Vol. 21. Consulting Psychologists Press; Palo Alto, CA: 1986. pp. 3463–3464. (Maslach Burnout Inventory). [Google Scholar]
- 3.Shanafelt T.D., Noseworthy J.H. Executive leadership and physician well-being. Mayo Clin Proc. 2017;92(1):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Physician Burnout Solutions. https://www.mindgarden.com/content/34-physician-burnout-solutions Available at.
- 5.DeChant P., Shannon D.W. CreateSpace Independent Publishing Platform; 2016. Preventing Physician Burnout: Curing the Chaos and Returning Joy to the Practice of Medicine. [Google Scholar]
- 6.Hlubocky F.J., Back A.L., Shanafelt T.D. Addressing burnout in oncology: why cancer care clinicians are at risk, what individuals can do, and how organizations can respond. Am Soc Clin Oncol Educ Book. 2016;36:271–279. doi: 10.1200/EDBK_156120. [DOI] [PubMed] [Google Scholar]
- 7.Blanchard P., Truchot D., Albiges-Sauvin L. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer. 2010;46(15):2708–2715. doi: 10.1016/j.ejca.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Banerjee S., Califano R., Corral J. Professional burnout in European young oncologists: results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol. 2017;28(7):1590–1596. doi: 10.1093/annonc/mdx196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swensen S.J., Shanafelt T. An organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf. 2017;43(6):308–313. doi: 10.1016/j.jcjq.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt T., Goh J., Sinsky C. The business case for investing in physician well-being. JAMA Int Med. 2017;177(12):1826. doi: 10.1001/jamainternmed.2017.4340. [DOI] [PubMed] [Google Scholar]
- 11.WHO Health Emergency Dashboard WHO (COVID-19) Homepage. https://covid19.who.int/ Available at.
- 12.Banerjee S., Lim K.H.J., Murali K. The impact of COVID-19 on oncology professionals: results of the ESMO Resilience Task Force survey collaboration. ESMO Open. 2021;6(2):1–10. doi: 10.1016/j.esmoop.2021.100058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murali K., Makker V., Lynch J., Banerjee S. From burnout to resilience: an update for oncologists. Am Soc Clin Oncol Educ Book. 2018;38:862–872. doi: 10.1200/EDBK_201023. [DOI] [PubMed] [Google Scholar]
- 14.Semiglazova T., Safina S., Tsimafeyeu I. Results of emotional burnout study among oncologists in Russia. J Clin Oncol. 2020;38:11011. [Google Scholar]
- 15.Maslach C., Jackson S.E., Leiter M.P. Mind Garden, Inc Manual 4th edition. 2018. www.mindgarden.coms Available at.
- 16.ProQOL webpage. https://proqol.org/ProQol_Test.html Available at.
- 17.Data sheet of GAD-7 at Cibersam. https://bi.cibersam.es/busqueda-de-instrumentos/ficha?Id=238 Available at.
- 18.Data sheet of PHQ-9 at Oncology Nursing Society (ONS) https://www.ons.org/sites/default/files/PatientHealthQuestionnaire9_Spanish.pdf Available at.
- 19.Hariharan T.S. A review of the factors to burnout at the early-career stage of medicine. Med Teach. 2019;41(12):1380–1391. doi: 10.1080/0142159X.2019.1641189. [DOI] [PubMed] [Google Scholar]
- 20.Tang L., Pang Y., He Y., Chen Z., Leng J. Burnout among early-career oncology professionals and the risk factors. Psychooncology. 2018;27(10):2436–2441. doi: 10.1002/pon.4847. [DOI] [PubMed] [Google Scholar]
- 21.Rogers S.C., Benson D.M., Kraut E.H. Storytelling as a means of improving community and decreasing burnout in a large academic cancer center. J Clin Oncol. 2020;38:11018. [Google Scholar]
- 22.Gebbia V., Bordonaro R., Blasi L. Liability of clinical oncologists and the COVID-19 emergency: between hopes and concerns. J Cancer Policy. 2020;25:100234. doi: 10.1016/j.jcpo.2020.100234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Resident survey of the Digestive System specialty promoted by the Spanish Society of Digestive Pathology. 2020. https://sepd.es/storage/cid/Investigacion/SEPD_EncuestaResidentes_ResultadosPreliminares.pdf Available at.
- 24.Hilmi M., Boilève A., Ducousso A. Professional and psychological impacts of the COVID-19 pandemic on oncology residents: a national survey. JCO Global Oncol. 2020;6:1674–1683. doi: 10.1200/GO.20.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mason D., Friese C.R. Protecting health care workers against COVID-19—and being prepared for future pandemics. JAMA Forum. 2020 doi: 10.1001/jamahealthforum.2020.0353. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings Available at. [DOI] [PubMed] [Google Scholar]
- 26.Villani L., McKee M., Cascini F., Ricciardi W., Boccia S. Comparison of deaths rates for COVID-19 across Europe during the first wave of the COVID-19 pandemic. Front Public Health. 2020;8:620416. doi: 10.3389/fpubh.2020.620416. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.