ABSTRACT
Objective:
High prevalences of muscle weakness and impaired physical performance in hospitalized patients recovering from COVID-19-associated pneumonia have been reported. Our objective was to determine whether the level of exercise capacity after discharge would affect long-term functional outcomes in these patients.
Methods:
From three to five weeks after discharge from acute care hospitals (T0), patients underwent a six-minute walk test (6MWT) and were divided into two groups according to the distance walked in percentage of predicted values: <75% group and ≥75% group. At T0 and three months later (T1), patients completed the Short Physical Performance Battery and the Euro Quality of Life Visual Analogue Scale, and pulmonary function and respiratory muscle function were assessed. In addition, a repeat 6MWT was also performed at T1.
Results:
At T0, 6MWD values and Short Physical Performance Battery scores were lower in the <75% group than in the ≥75% group. No differences were found in the Euro Quality of Life Visual Analogue Scale scores, pulmonary function variables, respiratory muscle function variables, length of hospital stay, or previous treatment. At T1, both groups improved their exercise capacity, but only the subjects in the <75% group showed significant improvements in dyspnea and lower extremity function. Exercise capacity and functional status values returned to predicted values in all of the patients in both groups.
Conclusions:
Four weeks after discharge, COVID-19 survivors with exercise limitation showed no significant differences in physiological or clinical characteristics or in perceived health status when compared with patients without exercise limitation. Three months later, those patients recovered their exercise capacity.
Keywords: Exercise; Health status; Rehabilitation, Respiratory muscles; Dyspnea
RESUMO
Objetivo:
Há relatos de altas prevalências de fraqueza muscular e de comprometimento do desempenho físico em pacientes hospitalizados em recuperação de pneumonia associada à COVID-19. Nosso objetivo foi determinar se o nível de capacidade de exercício após a alta altera os desfechos funcionais em longo prazo nesses pacientes.
Métodos:
Três a cinco semanas após a alta dos cuidados agudos (T0), os pacientes foram submetidos ao teste de caminhada de seis minutos (TC6) e divididos em dois grupos de acordo com a distância percorrida no TC6 (DTC6) em percentual do previsto: grupo <75% e grupo ≥75%. Em T0 e três meses depois (T1), os pacientes responderam à Short Physical Performance Battery e à Euro Quality of Life Visual Analogue Scale, e foram avaliadas a função pulmonar e a função muscular respiratória. Além disso, o TC6 foi repetido em T1.
Resultados:
Em T0, a DTC6 e as pontuações na Short Physical Performance Battery foram menores no grupo <75% do que no grupo ≥75%. Não foram encontradas diferenças nas pontuações na Euro Quality of Life Visual Analogue Scale, nas variáveis de função pulmonar e função muscular respiratória, no tempo de internação hospitalar ou no tratamento anterior. Em T1, ambos os grupos melhoraram a capacidade de exercício, mas apenas os indivíduos do grupo <75% apresentaram melhoras significativas na dispneia e na função dos membros inferiores. Os valores de capacidade de exercício e estado funcional retornaram aos valores previstos em todos os pacientes de ambos os grupos.
Conclusões:
Quatro semanas após a alta, os sobreviventes da COVID-19 com limitação ao exercício não apresentaram diferenças significativas nas características fisiológicas e clínicas ou na percepção do estado de saúde em comparação aos pacientes sem limitação ao exercício. Três meses depois, esses pacientes recuperaram sua capacidade de exercício.
Descritores: Exercício, Nível de saúde, Reabilitação, Músculos respiratórios, Dispneia
INTRODUCTION
The COVID-19 pandemic has been having impressive effects worldwide, with tens of million people infected and more than one million casualties.1 Approximately 80% of the infected individuals are asymptomatic, whereas 15% and 5% of those present with moderate/severe and critical disease, respectively.2 Pulmonary infection can cause alveolar damages that result in hypoxemic acute respiratory failure, requiring mechanical ventilation (MV).3 , 4 Muscle impairment in patients admitted to the ICU can be associated with systemic inflammation, MV, sedation, and prolonged bed rest, among other causes.5 Long-term physical, psychological, and cognitive impairment of both survivors and caregivers needs to be investigated.6 A high prevalence of muscle weakness and impaired physical performance was described in hospitalized patients recovering from COVID-19 who had had no previous motor limitations.7 COVID-19 survivors complain of fatigue, muscle weakness, sleep difficulties, anxiety, and depression six months after acute infection.8 COVID-19 survivors with functional and muscular performance impairment, dyspnea, and poor perceived health status9 can benefit from pulmonary rehabilitation.10
It is unclear whether the level of exercise capacity after discharge would affect long-term functional outcomes. Therefore, the aim of the present study was to evaluate the exercise capacity of patients four weeks after discharge from an acute care facility and after a three-month follow-up.
METHODS
This was an observational prospective controlled study. The study was approved by the Central Ethics Committee of Istituti Clinici Scientifici Maugeri (CEC no. 2435; May 26, 2020), and the participants signed the informed consent form.
Participants
Between May 27 and September 17 of 2020, consecutive patients recovering from COVID-19-associated pneumonia enrolled in a follow-up program at the Istituti Clinici Scientifici Maugeri outpatient clinic, in the city of Tradate, Italy, were included in the study. The clinic is part of the network of referral institutions for pulmonary rehabilitation, diagnosis, and care of post-acute and post-chronic patients.11 , 12 All patients had previously been admitted to an ICU, an intermediate care unit, or a respiratory unit and had been discharged home or to an inpatient multidisciplinary program in accordance with the Italian Position Paper.10 , 13 , 14 The patients were included in the follow-up program from three to five weeks after discharge.
Measurements
The following data were collected from patients at inclusion in the follow-up program (baseline: T0): demographics; anthropometrics; number and type of comorbidities using the Cumulative Illness Rating Scale,15 which includes a comorbidity index and a severity index; length of hospital stay; and use of invasive or noninvasive MV. According to the distance walked on the six-minute walk test (6MWT) at T0, that is, six-minute walk distance (6MWD) at T0, patients were divided into two groups: those with a 6MWD < 75% of the predicted values (<75% group) and those with a 6MWD ≥ 75% of the predicted values (≥75% group).
Outcome measures were assessed, using full protective measures,16 both at T0 and three months after T0 (T1). Exercise tolerance was assessed by means of the 6MWT.17 ) 6MWD was expressed in meters and in percentage of the predicted values.18 At the beginning and at the end of the test, the perception of dyspnea and leg fatigue were assessed by means of the modified Borg scale.19 SpO2 and HR were monitored with a pulse oximeter (8500M; Nonin Medical, Inc., Plymouth, MN, USA) and baseline SpO2, baseline HR, SpO2nadir and HRpeak were recorded. Exercise-induced desaturation was defined as baseline SpO2 − SpO2nadir (∆SpO2) > 4% during the 6MWT.17 , 20 Lower extremity function was assessed by means of the Short Physical Performance Battery (SPPB)21 using the values predicted by Bergland et al.22 The total SPPB score results from the sum of three components: standing balance, four-meter walk test, and moving from a sitting to a standing position (five times). The total SPPB score ranges from 0 to 12 points: 1-2, severe disability; 3-8, moderate disability; and 9-12, no disability. The minimal clinically important difference for SPPB is considered to be 1 point.23 Arterial blood gases were measured by means of an automated analyzer in samples collected from the radial artery with the patient breathing room air or oxygen in a sitting position for at least 1 h. Motor performance was assessed by the Barthel index24; the total score ranges from 0 (maximum level of dependency) to 100 (complete autonomy). A score ≤ 70 corresponds to severe dependency. Dyspnea was measured by the Barthel index dyspnea.25 Total scores range from 0 (absence of dyspnea) to 100 (extremely severe dyspnea). A reduction of 9 and 12 points is considered as the minimal clinically important difference in COPD patients without and with chronic respiratory failure, respectively.26 Perceived health status was measured by the Euro Quality of Life Visual Analogue Scale.27 Total scores range from 0 to 100 (higher scores represent better quality of life). Dynamic lung volumes were assessed in accordance with standards28 using the values predicted by Quanjer,29 whereas MIP and MEP were assessed in accordance with international guidelines30 using the values predicted by Bruschi et al.31
Statistical analysis
Qualitative variables were described as absolute and relative frequencies; quantitative variables were summarized as means and standard deviations or medians and interquartile ranges, depending on their parametric or nonparametric distribution. Between-group comparisons of qualitative variables were performed with the chi-square test or Fisher’s exact test. To detect any statistical difference in the comparison of parametric and nonparametric quantitative variables, respectively, the Student’s t-test and the Mann-Whitney test were used. We used the Student’s t-test and Wilcoxon signed-rank test to evaluate paired differences. We used Spearman’s and Pearson’s correlations to detect the relationships between 6MWD measured during the follow-up and clinical variables. On the basis of previously published data,10 a baseline 6MWD of 86.7 m and a pre- and post-intervention difference of 105 m, an alpha error of 0.05, and a statistical power of 0.9 estimated a sample size = 8. A two-tailed p < 0.05 was considered statistically significant. All statistical analyses were performed with the Stata statistical software package, version 16 (StataCorp LP, College Station, TX, USA).
RESULTS
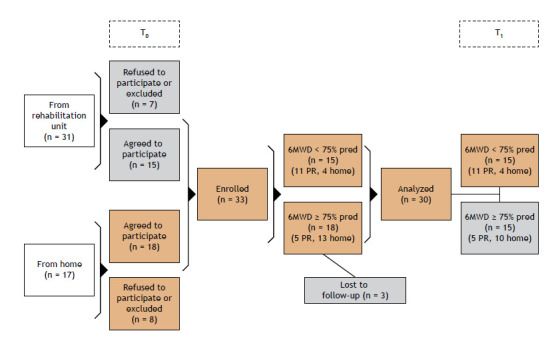
Figure 1 shows the patient selection process. During the study period, 48 individuals were referred to our clinic, 33 met the inclusion criteria, and 3 were lost to follow-up; therefore, 30 patients were included in the analysis (Figure 1). According to 6MWD at T0, 15 and 15 patients were included in the <75% group and in the ≥75% group, respectively. Eleven patients (73%) in the <75% group and 5 patients (33%) in the ≥75% group underwent pulmonary rehabilitation (p = 0.03).14
Figure 1. Flow chart of the patient selection process. T0: enrolment visit; T1: follow-up visit; 6MWD: six-minute walk distance; pred: of predicted; and PR: pulmonary rehabilitation.
Demographic, anthropometric, physiological, and clinical characteristics of patients at T0 are shown in Table 1. No significant differences were found between the groups. At T0, all of the subjects had a BMI > 23.2 kg/m2, 11 (33.3%) of whom had a BMI ≥ 30 kg/m2 (4 and 7 in the <75% and ≥75% groups, respectively).
Table 1. Demographic, anthropometric, physiological, and clinical characteristics of patients at baseline (T0).a .
| Characteristic | Whole sample | Group | p | |
|---|---|---|---|---|
| <75% | ≥75% | |||
| (N = 30) | (n = 15) | (n = 15) | ||
| Male gender, n (%) | 21 (70.0) | 11 (73.3) | 10 (66.7) | 1.00 |
| Age, years | 63.6 ± 12.2 | 65.2 ± 12.5 | 62.0 ± 12.0 | 0.48 |
| BMI, kg/m2 | 27.0 (25.3-31.0) | 26.7 (23.9-30.1) | 28.4 (25.5-35.2) | 0.15 |
| Current or former smoker, n (%) | 12 (42.9) | 9 (60.0) | 3 (23.1) | 0.07 |
| Length of hospital stay, days | 43.0 ± 20.1 | 44.1 ± 23.7 | 41.6 ± 15.4 | 0.76 |
| Previous IMV, n (%) | 6 (20.0) | 4 (26.7) | 2 (13.3) | 0.65 |
| Previous NIV, n (%) | 13 (43.3) | 9 (60.0) | 4 (26.7) | 0.14 |
| Previous oxygen therapy, n (%) | 23 (76.7) | 11 (73.3) | 12 (80.0) | 1.00 |
| COPD, n (%) | 2 (6.7) | 1 (6.7) | 1 (6.7) | 1.00 |
| Asthma, n (%) | 3 (10.0) | 1 (6.7) | 2 (13.3) | 1.00 |
| Pulmonary embolism, n (%) | 1 (3.3) | 1 (6.7) | 0 (0.0) | 1.00 |
| Diabetes, n (%) | 5 (17.2) | 2 (13.3) | 3 (21.4) | 0.65 |
| FiO2 | 0.21 (0.21-0.24) | 0.21 (0.21-0.28) | 0.21 (0.21-0.21) | 0.21 |
| PaO2, mmHg | 83.3 ± 9.3 | 81.6 ± 9.5 | 84.7 ± 9.2 | 0.43 |
| PaO2/FiO2 | 394.7 ± 45.4 | 388.7 ± 45.2 | 399.7 ± 46.8 | 0.57 |
| SaO2, % | 96.5 ± 1.4 | 96.4 ± 1.46 | 96.5 ± 1.40 | 0.87 |
| PaCO2, mmHg | 36.1 ± 2.8 | 36.5 ± 3.2 | 35.8 ± 2.4 | 0.56 |
| pH | 7.412 ± 0.026 | 7.401 ± 0.180 | 7.420 ± 0.280 | 0.06 |
| CIRS-SI | 1.5 ± 0.2 | 1.6 ± 0.2 | 1.4 ± 0.2 | 0.07 |
| CIRS-CI | 2.4 ± 1.5 | 2.6 ± 1.6 | 2.1 ± 1.4 | 0.40 |
| MIP, cmH2O | 90.0 ± 26.3 | 93.3 ± 21.2 | 88.7 ± 29.1 | 0.78 |
| MIP, % predicted | 113.3 ± 40.0 | 96.5 ± 19.7 | 120.0 ± 44.8 | 0.34 |
| MEP, cmH2O | 142.4 ± 48.5 | 147.5 ± 48.2 | 140.4 ± 51.1 | 0.82 |
| MEP, % predicted | 128.0 ± 34.5 | 116 ± 37.7 | 132.8 ± 34.0 | 0.43 |
| FEV1, L | 3.0 ± 1.2 | 3.5 ± 1.3 | 2.8 ± 1.1 | 0.27 |
| FEV1, % predicted | 97.1 ± 23.4 | 103.8 ± 38.4 | 94.4 ± 16.5 | 0.52 |
| FVC, L | 3.7 ± 1.3 | 4.4 ± 1.3 | 3.4 ± 1.3 | 0.20 |
| FVC, % predicted | 96.9 ± 21.3 | 104.5 ± 37.4 | 93.9 ± 12.4 | 0.42 |
| FEV1/FVC, % | 77.4 (74.3-80.4) | 78.6 (75.7-83.2) | 76.4 (70.0-78.7) | 0.37 |
IMV: invasive mechanical ventilation; NIV: noninvasive ventilation; CIRS-SI: Cumulative Illness Rating Scale severity index; and CIRS-CI: Cumulative Illness Rating Scale comorbidity index. aValues expressed as mean ± SD or median (IQR), except where otherwise indicated.
Table 2 shows the exercise capacity and functional status of the patients at T0.. As expected, when compared with patients in the ≥75% group, those in the <75% group had reduced exercise capacity and more severe dyspnea and had lower scores on the SPPB, but not on the Euro Quality of Life Visual Analogue Scale.
Table 2. Exercise capacity and functional status at baseline (T0).
| Variable | Whole sample | Group | p | |
|---|---|---|---|---|
| <75% | ≥75% | |||
| (N = 30) | (n = 15) | (n = 15) | ||
| BI score | 100 (100-100) | 100 (95-100) | 100 (100-100) | 0.41 |
| BI-d score | 5 (2-16) | 16 (5-12) | 2 (0-5) | 0.0004 |
| SPPB total score | 11 (9-12) | 8.5 (6-11) | 11 (10-12) | 0.006 |
| SPPB, % predicted | 92.3 (76.0-101.4) | 74.3 (54.5-91.7) | 99.9 (92.3-102.6) | 0.001 |
| 6MWD, m | 406.5 (318.0-521.0) | 318.0 (250.0-380.0) | 510.0 (433.0-570.0) | < 0.0001 |
| 6MWD, % predicted | 77.0 (64.0-98.0) | 64.0 (57.0-70.0) | 98.0 (85.0-109.0) | < 0.0001 |
| SpO2mean, % | 93.8 ± 2.4 | 92.7 ± 2.9 | 94.6 ± 1.7 | 0.04 |
| SpO2nadir, % | 92.0 (89.0-94.0) | 89.5 (87.5-92.0) | 93.0 (92.0-95.0) | 0.01 |
| ∆SpO2 (baseline/nadir), % | −4.8 ± 3.4 | −6.8 ± 3.9 | −3.3 ± 1.9 | 0.005 |
| Borg dyspnea scale score | 2.9 ± 1.9 | 3.4 ± 1.9 | 2.6 ± 1.9 | 0.29 |
| Borg leg fatigue scale score | 2 (0.5-3.0) | 2.0 (0.5-3.5) | 3.0 (1.0-3.0) | 0.69 |
| EuroQoL-VAS score | 80.3 ± 12.7 | 79.1 ± 15.0 | 81.5 ± 10.2 | 0.61 |
BI: Barthel index; BI-d: Barthel index dyspnea; SPPB: Short Physical Performance Battery; 6MWD: six-minute walk distance; and EuroQoL-VAS: Euro Quality of Life Visual Analogue Scale. aValues expressed as mean ± SD or median (IQR).
Table 3 shows the values of demographic, physiological, and functional variable results at T1, as well as the differences (T1 − T0) regarding exercise capacity, dyspnea, and lower extremity function. No significant differences between the groups were found in anthropometric or physiological variables at T1. However, 6MWD values and SPPB scores were higher in the ≥75% group than in the <75% group. Both groups showed improvement in exercise capacity, but only the <75% group showed significant improvements in dyspnea and in lower extremity function. As also shown in Table 3, exercise capacity and functional status results returned to predicted values in all of the patients in both groups.
Table 3. Anthropometric, physiological, and functional variables at T1 and p-values of the differences between T1 and T0 within the groupsa and between the groups.b,c .
| Variable | <75% group | pa | ≥75% group | pa | pb |
|---|---|---|---|---|---|
| BMI, kg/m2 | 28.0 (24.0-30.0) | 0.87 | 27.8 (25.2-35.0) | 0.68 | 0.32 |
| PaO2, mmHg | 84.3 ± 8.1 | 0.22 | 83.4 ± 6.4 | 0.29 | 0.76 |
| PaCO2, mmHg | 36.8 ± 2.9 | 0.46 | 37.6 ± 2.9 | 0.17 | 0.49 |
| pH | 7.421 ± 0.03 | 0.005 | 7.417 ± 0.03 | 0.85 | 0.69 |
| SaO2, % | 96.8 ± 1.1 | 0.29 | 96.8 ± 0.8 | 0.55 | 0.95 |
| PaO2/FiO2 | 401.7 ± 38.8 | 0.22 | 397.2 ± 30.6 | 0.29 | 0.76 |
| MIP, cmH2O | 84.5 ± 25.6 | 0.91 | 93.5 ± 21.8 | 0.01 | 0.31 |
| MIP, % predicted | 103.7 ± 28.1 | 0.87 | 121.6 ± 40.3 | 0.02 | 0.17 |
| MEP, cmH2O | 133.3 ± 46.5 | 0.03 | 144.7 ± 47.3 | 0.29 | 0.51 |
| MEP, % predicted | 119.9 ± 28.9 | 0.03 | 134.3 ± 35.7 | 0.35 | 0.24 |
| FEV1, L | 2.8 ± 0.8 | 0.66 | 3.0 ± 1.0 | 0.01 | 0.63 |
| FEV1, % predicted | 101.3 ± 21.9 | 0.72 | 103.5 ± 18.4 | 0.04 | 0.77 |
| FVC, L | 3.3 (2.7-4.7) | 0.12 | 3.6 (2.7-5.0) | 0.02 | 1.00 |
| FVC, % predicted | 106 (77-123) | 0.48 | 96 (88.127) | 0.02 | 1.00 |
| FEV1/FVC | 75.0 ± 9.1 | 0.13 | 78.1 ± 6.7 | 0.56 | 0.30 |
| BI-d score | 2 (0-5) | 0.0007 | 0 (0-2) | 0.20 | 0.09 |
| ∆BI-d score | −10.9 ± 9.5 | - | −1.0 ± 4.6 | - | 0.002 |
| SPPB total score | 10 (10-12) | 0.003 | 12 (12-12) | 0.06 | 0.007 |
| ∆SPPB total score | +2.3 ± 2.4 | - | +0.7 ± 1.3 | - | 0.03 |
| SPPB, % predicted | 94.4 (90.8-102.2) | 0.002 | 101.9 (100.1-102.6) | 0.06 | 0.02 |
| 6MWD, m | 479.4 ± 65.9 | 0.0001 | 545.2 ± 95.2 | 0.004 | 0.04 |
| ∆6MWD, m | +158 (100-200) | - | +43 (5-97) | - | 0.0001 |
| 6MWD, % predicted | 94.1 ± 12.2 | 0.0005 | 109.5 ± 10.8 | 0.003 | 0.001 |
| ∆6MWD, % predicted | +28.0 (19.0-44.0) | - | +9.0 (3.0-19.0) | - | 0.0005 |
| SpO2mean, % | 93.8 (90.0-95.1) | 0.94 | 95.2 (94.5-96.1) | 0.90 | 0.05 |
| SpO2nadir, % | 92 (88-93) | 0.23 | 94 (93-96) | 0.52 | 0.04 |
| ∆SpO2 baseline/nadir, % | −4 (−8.3 to −2.6) | 0.15 | −3 (−4.3 to −0.5) | 0.97 | 0.15 |
| EuroQoL-VAS score | 78.7 ± 14.2 | 0.91 | 85.7 ± 11.5 | 0.06 | 0.15 |
BI-d: Barthel index dyspnea; SPPB: Short Physical Performance Battery; 6MWD: six-minute walk distance; and EuroQoL-VAS: Euro Quality of Life Visual Analogue Scale. aValues expressed as mean ± SD or median (IQR).
Table 4 shows the correlations of demographic, physiological, and clinical characteristics at T0 with 6MWD at T1. Being older, having longer length of hospital stay, having comorbidities, and having needed invasive MV correlated with having lower 6MWD values at T1. Having lower 6MWD values and lower SPPB scores at T0 correlated with having higher 6MWD values at T1. Because of the small sample, participating in the pulmonary rehabilitation program was not significantly correlated with exercise capacity at T1.
Table 4. Correlations of demographic, physiological, and clinical characteristics at T0 with the six-minute walk distance at T1.
| Characteristic | rho | p |
|---|---|---|
| IMV | -0.39 | 0.03 |
| NIV | -0.36 | 0.05 |
| Oxygen therapy | -0.27 | 0.14 |
| Exposure to rehabilitation | -0.30 | 0.11 |
| Age | -0.62 | 0.0002 |
| Previous LoS in acute phase | -0.58 | 0.002 |
| BMI, kg/m2 | -0.10 | 0.61 |
| CIRS-SI | -0.61 | 0.0004 |
| CIRS-CI | -0.52 | 0.003 |
| BI-d | -0.45 | 0.01 |
| SPPB total score | 0.65 | 0.0001 |
| 6MWD at T0 | 0.75 | < 0.0001 |
| VC, % | -0.28 | 0.37 |
IMV: invasive mechanical ventilation; NIV: noninvasive ventilation; LoS: Length of hospital stay; CIRS-SI: Cumulative Illness Rating Scale severity index; CIRS-CI: Cumulative Illness Rating Scale comorbidity index; BI-d: Barthel index dyspnea; SPPB: Short Physical Performance Battery; and 6MWD: six-minute walk distance.
DISCUSSION
The present study shows that half of the patients recovering from COVID-19-associated pneumonia may present with exercise limitation four weeks after discharge from acute care hospitals. Patients with exercise limitation and worse functional status, when compared with those without them, showed no significant differences in terms of demographic, anthropometric, physiological, or clinical characteristics, or in perceived health status. Three months after T0, exercise capacity and functional status results returned to predicted values in both groups.
Our results confirm that COVID-19 survivors can have impaired physical functioning when they are discharged home, even after early mobilization.32 The absence of differences at baseline highlights that the decline in physical performance cannot be attributed to lung impairment or respiratory muscle dysfunction.
As shown by the comparison with predicted values, three months after T0, all patients recovered their exercise capacity and functional status. A large study reported that, six months after the acute infection, COVID-19 survivors complained of fatigue or muscle weakness, sleep difficulties, and anxiety or depression.8 The length of hospital stay in acute care facilities in our sample was similar to that in the aforementioned study8 with patients on invasive MV, noninvasive ventilation, or high flow nasal cannula (mean: 43 vs. 35 days). Exercise capacity as assessed by 6MWD three months after discharge was similar to that in the aforementioned study with patients assessed six months after discharge from acute care hospitals (mean: 94% vs. 88 % of the predicted values).8
The vast majority of patients (73%) with exercise limitation (<75% group) underwent pulmonary rehabilitation in accordance with the Italian Position Paper,14 in comparison with 33% of the patients in the ≥75% group. The small sample size impedes a reliable comparison between patients who did and did not undergo pulmonary rehabilitation. However, our results confirm those of another study10 that showed that a pulmonary rehabilitation program could improve but not fully recover exercise capacity. Furthermore, in our study, due to the small sample size, participation in a pulmonary rehabilitation program was not associated with exercise capacity at T1.
There was no difference in perceived health status between patients with or without exercise limitation. In other words, at least in this sample of patients, there was a dissociation between exercise capacity and health status. This observation has been also reported in other studies about other diseases33 and probably reflects the fact that health status does not depend on exercise capacity only. This underlines the importance of evaluating this parameter specifically.
The present study has limitations. Standard respiratory muscle or lung function tests, including assessment of diffusing capacity at discharge from acute care hospitals, could not be performed for safety reasons. The small sample size impedes a reliable comparison between patients who did and did not undergo pulmonary rehabilitation.
In conclusion, patients recovering from COVID-19-associated pneumonia may present with exercise limitation four weeks after discharge from acute care hospitals. No significant differences were found in any demographic, anthropometric, physiological, or clinical characteristics or in perceived health status between patients with or without exercise limitation. However, three months later, the measurements of exercise capacity and functional status returned to the predicted values in both groups. Despite the small sample size and the possible lack of external validity, our findings may guide clinicians who treat COVID-19 survivors to design suitable rehabilitation programs.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Denise Rossato Silva (Federal University of Rio Grande do Sul, Porto Alegre, Brazil) for her useful comments about the manuscript.
Footnotes
Financial support: None.
Study carried out at the Istituti Clinici Scientifici Maugeri - IRCCS - Tradate, Italia.
REFERENCES
- 1.Johns Hopkins University . Covid-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Baltimore (MD): CCSE; https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX. Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020;46(4):637–653. doi: 10.1007/s00134-020-05944-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vitacca M, Migliori GB, Spanevello A, Melazzini MG, Ambrosino N. COVID-19 ICS Maugeri IRCCS network Management and outcomes of post-acute COVID-19 patients in Northern Italy. Eur J Intern Med. 2020;78:159–160. doi: 10.1016/j.ejim.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paneroni M, Simonelli C, Saleri M, Bertacchini L, Venturelli M, Troosters T. Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID-19 Pneumonia. Am J Phys Med Rehabil. 2021;100(2):105–109. doi: 10.1097/PHM.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 8.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X. 6-month consequences of COVID-19 in patients discharged from hospital a cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zampogna E, Migliori GB, Centis R, Cherubino F, Facchetti C, Feci D, et al. Functional impairment during post-acute COVID-19 phase: Preliminary finding in 56 patients [published online ahead of print, 2021 Jan 6] Pulmonology. 2021;S2531-0437(20):30268–30263. doi: 10.1016/j.pulmoe.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zampogna E, Paneroni M, Belli S, Aliani M, Gandolfo A, Visca D. Pulmonary Rehabilitation in Patients Recovering from COVID-19. Respiration. 2021;100(5):416–422. doi: 10.1159/000514387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ceriana P, Nava S, Vitacca M, Carlucci A, Paneroni M, Schreiber A. Noninvasive ventilation during weaning from prolonged mechanical ventilation. Pulmonology. 2019;25(6):328–333. doi: 10.1016/j.pulmoe.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Maestri R, Bruschi C, Fracchia C, Pinna GD, Fanfulla F, Ambrosino N. Physiological and clinical characteristics of patients with COPD admitted to an inpatient pulmonary rehabilitation program A real-life study. Pulmonology. 2019;25(2):71–78. doi: 10.1016/j.pulmoe.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Winck JC, Ambrosino N. COVID-19 pandemic and non invasive respiratory management Every Goliath needs a David. An evidence based evaluation of problems. Pulmonology. 2020;26(4):213–220. doi: 10.1016/j.pulmoe.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vitacca M, Carone M, Clini EM, Paneroni M, Lazzeri M, Lanza A. Joint Statement on the Role of Respiratory Rehabilitation in the COVID-19 Crisis The Italian Position Paper. Respiration. 2020;99(6):493–499. doi: 10.1159/000508399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16(5):622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 16.Ippolito M, Vitale F, Accurso G, Iozzo P, Gregoretti C, Giarratano A. Medical masks and Respirators for the Protection of Healthcare Workers from SARS-CoV-2 and other viruses. Pulmonology. 2020;26(4):204–212. doi: 10.1016/j.pulmoe.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D. An official European Respiratory Society/American Thoracic Society technical standard field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. doi: 10.1183/09031936.00150314. [DOI] [PubMed] [Google Scholar]
- 18.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults [published correction appears in Am J Respir Crit Care. Med. 2020;201(3):393–393. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [Google Scholar]
- 19.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. doi: 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Poulain M, Durand F, Palomba B, Ceugniet F, Desplan J, Varray A. 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest. 2003;123(5):1401–1407. doi: 10.1378/chest.123.5.1401. [DOI] [PubMed] [Google Scholar]
- 21.Bernabeu-Mora R, Medina-Mirapeix F, Llamazares-Herrán E, García-Guillamón G, Giménez-Giménez LM, Sánchez-Nieto JM. The Short Physical Performance Battery is a discriminative tool for identifying patients with COPD at risk of disability [published correction appears in Int J Chron Obstruct Pulmon. Dis. 2016;11:623–623. doi: 10.2147/COPD.S94377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergland A, Strand BH. Norwegian reference values for the Short Physical Performance Battery (SPPB) the Tromsø Study. BMC Geriatr. 2019;19(1):216–216. doi: 10.1186/s12877-019-1234-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 24.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 25.Vitacca M, Paneroni M, Baiardi P, De Carolis V, Zampogna E, Belli S. Development of a Barthel Index based on dyspnea for patients with respiratory diseases. Int J Chron Obstruct Pulmon Dis. 2016;11:1199–1206. doi: 10.2147/COPD.S104376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vitacca M, Malovini A, Balbi B, Aliani M, Cirio S, Spanevello A. Minimal Clinically Important Difference in Barthel Index Dyspnea in Patients with COPD. Int J Chron Obstruct Pulmon Dis. 2020;15:2591–2599. doi: 10.2147/COPD.S266243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schweikert B, Hahmann H, Leidl R. Validation of the EuroQol questionnaire in cardiac rehabilitation. Heart. 2006;92(1):62–67. doi: 10.1136/hrt.2004.052787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 29.Quanjer PH. Working party on "Standardization of lung function test" Bull Eur Physiopathol. Respir. 1983;19(Suppl 5):7–10. [PubMed] [Google Scholar]
- 30.American Thoracic Society/European Respiratory Society ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624. doi: 10.1164/rccm.166.4.518. [DOI] [PubMed] [Google Scholar]
- 31.Bruschi C, Cerveri I, Zoia MC, Fanfulla F, Fiorentini M, Casali L. Reference values of maximal respiratory mouth pressures a population-based study. Am Rev Respir Dis. 1992;146(3):790–793. doi: 10.1164/ajrccm/146.3.790. [DOI] [PubMed] [Google Scholar]
- 32.Belli S, Balbi B, Prince I, Cattaneo D, Masocco F, Zaccaria S. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived hospitalisation. Eur Respir J. 2020;56(4):2002096–2002096. doi: 10.1183/13993003.02096-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Foglio K, Bianchi L, Bruletti G, Porta R, Vitacca M, Balbi B. Seven-year time course of lung function, symptoms, health-related quality of life, and exercise tolerance in COPD patients undergoing pulmonary rehabilitation programs. Respir Med. 2007;101(9):1961–1970. doi: 10.1016/j.rmed.2007.04.007. [DOI] [PubMed] [Google Scholar]


