Abstract
Purpose
to report the utility of Anterior Segment Optical Coherence Tomography (AS OCT) for planning superficial sclerectomy in a patient with nevus of Ota.
Observations
Oculodermal melanocytosis, also called nevus of Ota, is a benign pigmentary disorder that involves the skin innervated by the first and second branches of the trigeminal nerve. To reduce these black or brownish lesions, different surgical treatments have been reported, such as flipped scleral flap, sclera allograft and the grabbing method. Superficial sclerectomy is a recent technique that has proven effective in improving scleral pigmentation. Although this procedure allows the operating time to be reduced and results in a smoother scleral bed surface, it has a limitation, represented by the difficulty of estimating the depth of the sclerectomy: an inaccurate estimate or incorrect depth could cause an inadequate deep scleral dissection with excessive weakening of the sclera. We report a case of a 27-year-old patient with nevus of Ota undergoing superficial sclerectomy. The depth of scleral pigmentation was evaluated with AS OCT images before the surgery, allowing a superficial sclerectomy to be performed with a precalibrated diamond blade.
Conclusions and Importance
In oculodermal melanocytosis (nevus of Ota) the use of AS OCT images showing the depth of scleral pigmentation could lead to the most effective and safest surgical choice for each case.
Keywords: Nevus of ota, Oculodermal melanocytosis, Superficial sclerectomy, Anterior segment OCT, Cosmetic improvement
1. Introduction
Oculodermal melanocytosis is a brownish, blue gray or black pigmentation of the eye and periorbital skin along the distribution of the ophthalmic and maxillary branches of the trigeminal nerve.1,2 The pathology was first described in the mid 1800s in reference to a patient with cutaneous hyperpigmentation and melanoma of the sclera.3 The condition is also called nevus of Ota, since Ota described the ocular pigmentation in the 1939.1 The nevus can be unilateral (95%) or bilateral (5%) and, in addition to the skin, it can involve the ipsilateral episclera and sclera, conjunctiva, choroid and even the optic nerve.4 Oculodermal melanocytosis occurs more frequently in women and Asians, with an incidence of 0.2–1%.5 The etiology is not completely known, but it is probably related to an incomplete melanocyte migration from the neural crest to the epidermis during the embryonic stage.6 Numerous patients with oculodermal melanocytosis suffer because of their condition and this is reflected in personal relationships. Several methods have been used to reduce these black or brownish lesions, including flipped scleral flap,4 sclera allograft5 and the grabbing method.2 Some authors have shown good results with superficial sclerectomy7: the main problem in this case is knowing how much scleral tissue should be removed to eliminate the pigmented area without weakening the sclera. We report the utility of Anterior Segment Optical Coherence Tomography (AS OCT) in the preoperative planning of superficial sclerectomy in a patient with nevus of Ota. The preoperative depth of scleral involvement was evaluated with AS OCT images with a measurement of scleral melanocytosis depth in order to quantify the size of the sclerectomy.
2. Case report
We report a case of 27-year-old Caucasian man with a right congenital periocular hyperpigmentation with cutaneous and scleral involvement (Fig. 1, Fig. 2). The patient came to us expressing a desire to remove the scleral pigmentation, as it caused him great discomfort in social relations. During the examination, we realized how much the physical problem created distress for him in his interpersonal relationships. He avoided direct eye contact during conversations and feared social interactions. The patient reported that this discomfort had created a qualitative impairment of his social life that required the intervention of a psychotherapist. Therefore, we considered a superficial sclerectomy to improve this emotional wellbeing, believing that this would have positive repercussions on the patient's quality of life and self-confidence.
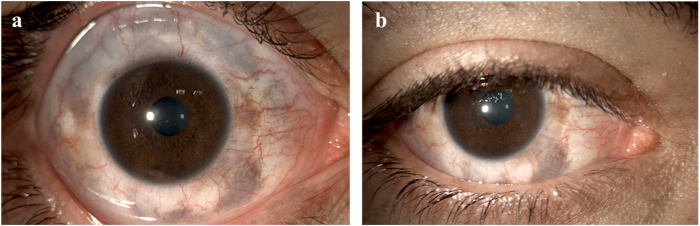
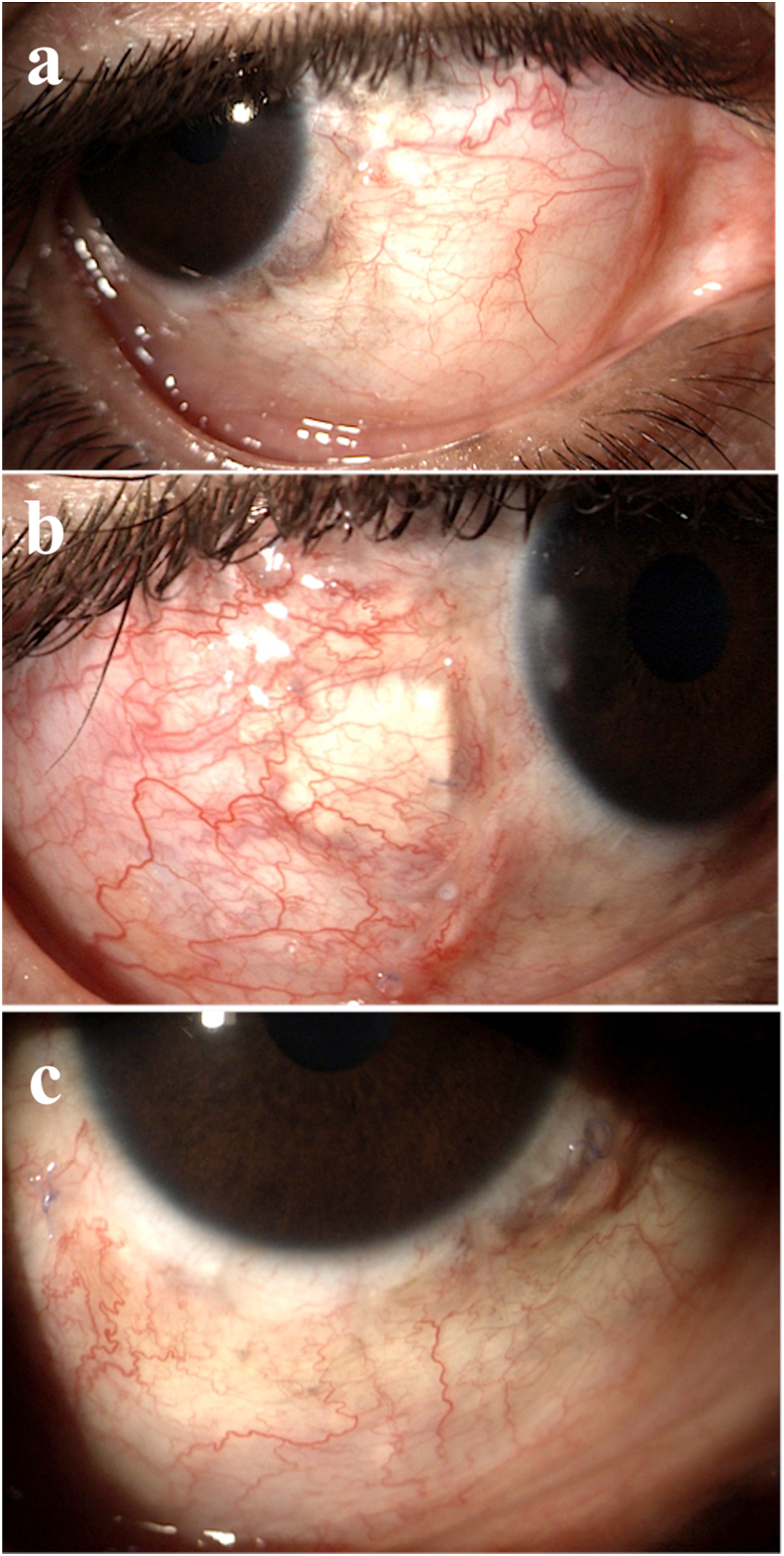
Fig. 1.
A 27-year-old Caucasian man with a right congenital oculodermal melanocytosis of the eye and periorbital skin. Most of the scleral pigmentation involved the superior sector (1a), but it was hidden by the upper eyelid (1b).
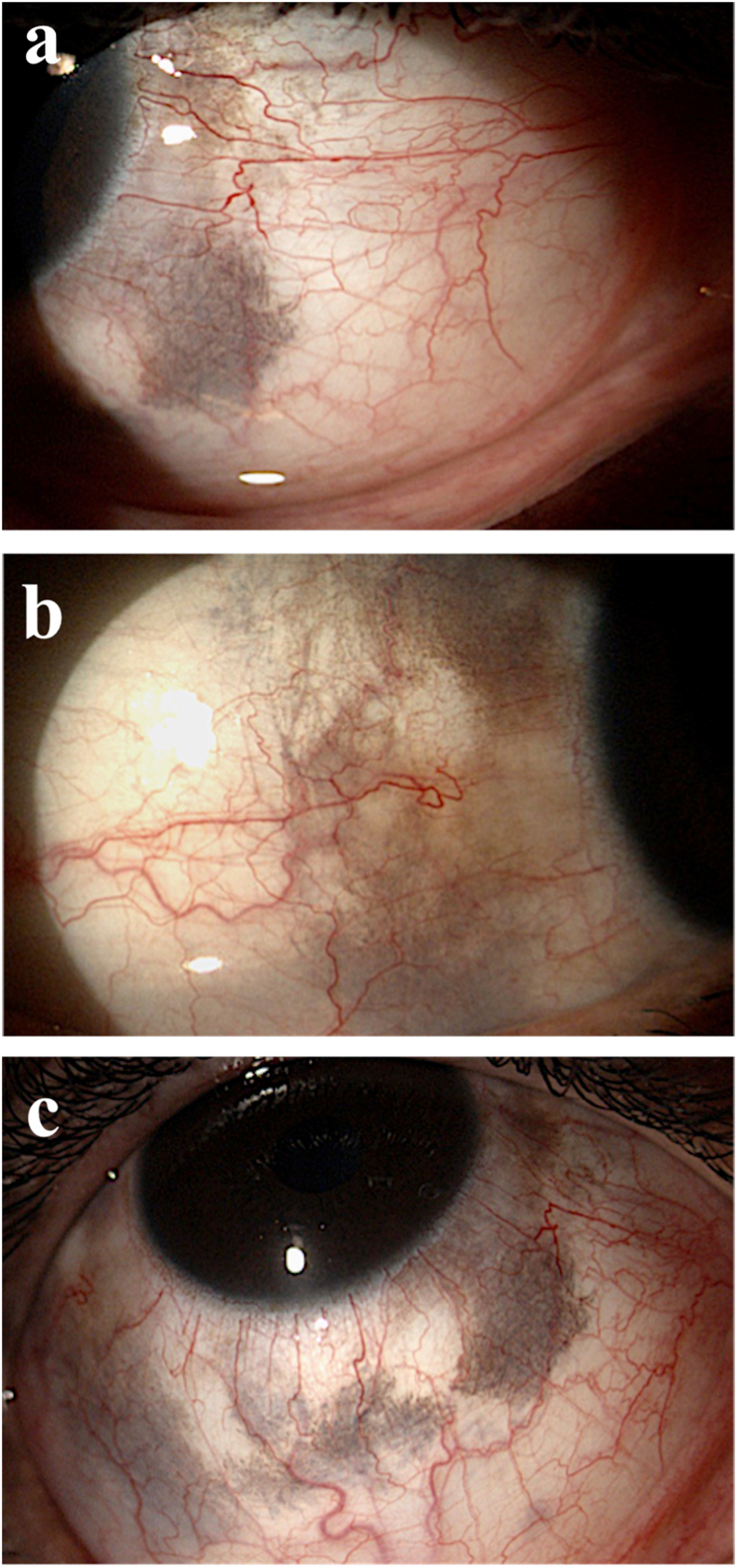
Fig. 2.
Scleral pigmentation was most noticeable in the nasal (2a) and temporal (2b) scleral areas, such as the inferior sector (2c).
The pros and cons of treatment, such as an improvement in scleral pigmentation versus a risk of perforation, neuropathy, infections, scleropathy and scleral weakening, were discussed with the patient who expressed his willingness to undergo the surgery. The study was conducted in accordance with the tenets of the World Medical Association's Declaration of Helsinki and informed consent for the surgical reduction of ocular pigmentation was obtained from the patient.
The patient had preoperative and postoperative assessments, including refraction with best corrected visual acuity (BCVA), intraocular pressure (IOP), slit lamp examination and fundus examination. BCVA was 20/20 and IOP was normal in both eyes. On slit lamp examination there were no abnormalities in the cornea, anterior chamber or crystalline lens except the sclera hyperpigmentation. The fundus finding was normal. Scleral pigmentation was more marked in inferior temporal and inferior nasal sectors as well as in the superior one, but we decided not to treat this quadrant because it was hidden by the upper eyelid (Fig. 1, Fig. 2).
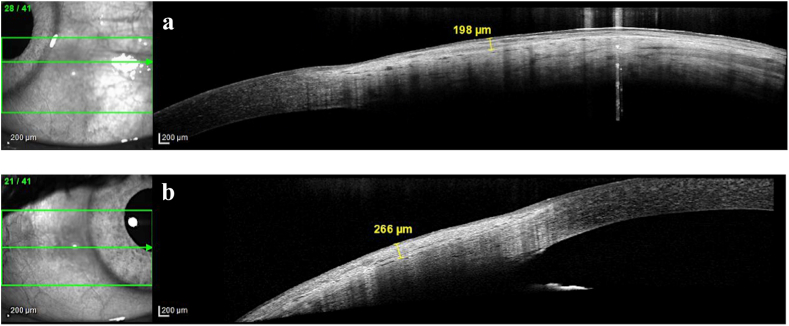
In order to plan the surgical sclerectomy we investigated the scleral pigmentation with the Spectralis Anterior Segment Module (Spectralis HRA OCT 2 MC; Anterior Segment Module, Heidelberg Engineering GmbH, Heidelberg, Germany). The Spectralis Anterior Segment Module enables high resolution OCT imaging of the cornea, sclera, and anterior chamber angles. The acquisition speed is 80,000 A scans per second. We used 15 × 10° scans (8.3 mm × 5.6 mm) for a total of 161 B scans spaced at 35 μm; each scan has an axial resolution of 3.9 μm/pixel and a side resolution of 5.7 μm/pixel. This technology seems appropriate for the study of scleral tissue, as it allows us to evaluate the pigment depth and the amount of scleral involvement. The OCT scans showed the presence of pigmented areas in the sclera, with a greater density in the superficial than in the deep sclera, as well as a different reflectivity between the superficial and deep sclera, marked by a separation line. The depth of the superficial scleral pigmentation was measured with AS OCT, which enabled us to plan the depth of the sclerectomy (Fig. 3A–B).
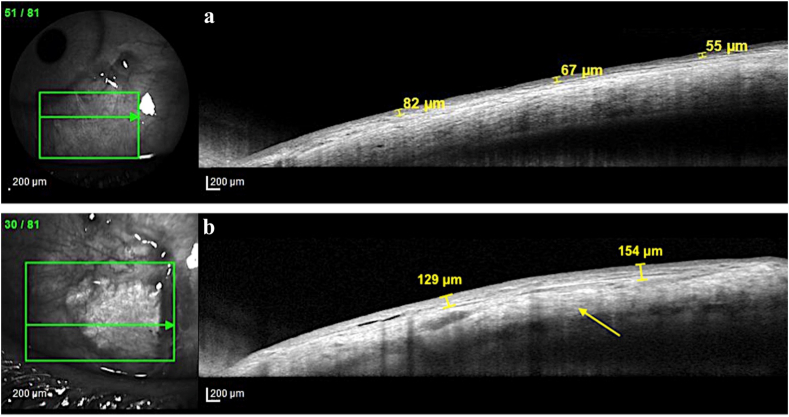
Fig. 3.
In order to plan surgical sclerectomy we investigated scleral pigmentation with Anterior Segment OCT. 3a) Pigmentation in the inferior nasal sclera had a maximum depth of 198 μm. 3b) Inferior temporal sclera involvement was found to be deeper, with a maximum depth of 266 μm.
Since the upper and lower eyelids covered the superior and inferior portions of the sclera, we limited the reduction of ocular pigmentation to the inferior and inferior temporal areas.
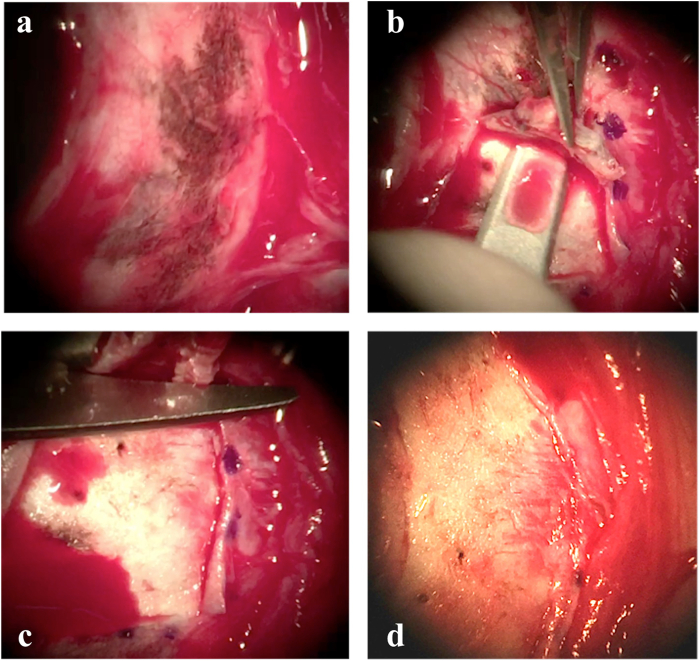
After the application of topical and peribulbar anesthesia, the conjunctiva and Tenon capsule on the temporal and nasal sides of the eye were incised and dissected using Vannas scissors. A two-step surgical approach was used. The first step involved the inferior nasal area of the sclera. Based on the information provided by AS OCT, we were able to plan a 200 μm scleral incision with a precalibrated diamond blade and perform a superficial sclerectomy of 200 μm (Fig. 4). The second step involved the inferior temporal quadrant of the sclera, which we operated one month after the first surgery. In this area, the AS OCT images showed a pigmentation reaching over 250 μm in depth. We performed a sclerectomy of 250 μm and we noticed a lower pigmentation in the deeper part of the scleral flap compared to the superficial area. For this reason, we decided to perform a flipped scleral flap surgery (Fig. 5): after the free scleral flap was dissected, it was flipped over and attached to the scleral bed with 7/0 Vicryl interrupted sutures. This procedure hides the episcleral pigmentation internally, resulting in a less pigmented surface and avoiding excessive weakening of the sclera. Conjunctival peritomy was approximated and sutured using 7/0 Vicryl. Topical 0.3% ofloxacin and 0.1% fluorometholone were used for approximately 2 months postoperatively.
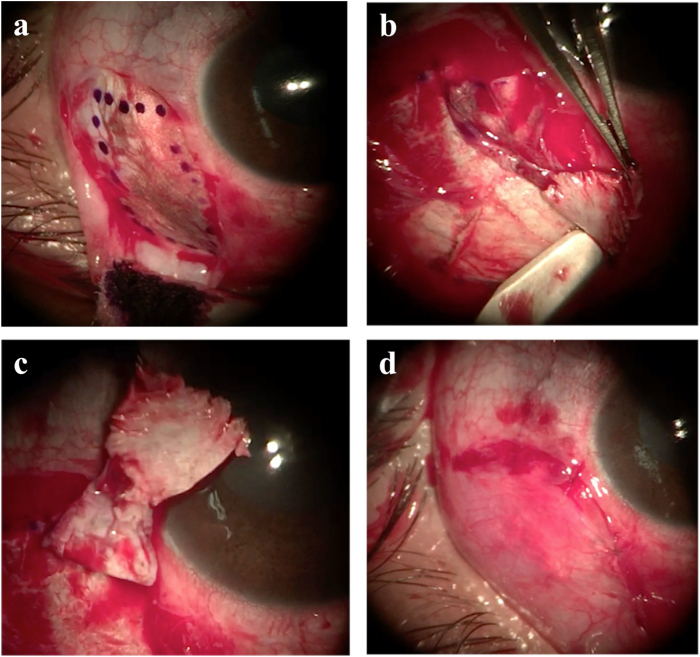
Fig. 4.
Sclerectomy of inferior nasal area. 4a) After conjunctival peritomy and Tenon's capsule dissection, the scleral area of melanocytosis was exposed. 4b) The surgeon did a partial thickness scleral incision with a diamond blade set at at 200 μm based on the AS OCT measurement. Then, superficial scleral dissection of the nevus area was performed using a bevel up knife. 4c) The scleral area affected by the nevus was removed with the Vannas scissors. 4d) At the end of the surgery, most of the scleral melanocytosis had been removed.
Fig. 5.
Sclerectomy of inferior temporal area. 5a) After conjunctival peritomy and Tenon's capsule dissection, the inferior-temporal area of melanocytosis was exposed and marked. 5b) The surgeon performed a 250 μm scleral dissection of the affected sclera using a bevel up knife. 5c) The scleral area affected by the nevus was removed with the Vannas scissors. As shown in the image, the scleral flap had less pigmentation in the deeper part than the superficial one. 5d) The scleral flap was inverted, positioned and sutured in order to avoid weakening of the sclera.
No intra- or postoperative complications occurred. The patient was followed up for 12 months postoperatively. Postoperative digital photos showed a reduction in scleral pigmentation (Fig. 6). The histopathological study showed an increased density of dendritic and oval-shaped melanocytes located in the superficial lamellar tissues, thus confirming the nevus of Ota diagnosis (Fig. 7). There were no differences between preoperative and postoperative visual acuity, IOP or fundus finding. Conjunctival injection and chemosis gradually disappeared within 1 month after surgery. The patient was examined to assess the surgical results and screened for complications at 1 day, 2 weeks and at 1, 3, 6 and 12 months after the surgery. One month after surgery there was a significant reduction in scleral pigmentation (Fig. 6). Postoperative AS OCT images showed a reduction in scleral thickness and pigment compared to preoperative images (Fig. 8). Scleral thickness remained stable after 12 postoperative months. No complications linked to the transection of neural and vascular components, such as neurotrophic, esthesiometric and ischemic alterations, occurred during the follow up.
Fig. 6.
One month postoperative results. After surgery there was a significant reduction in scleral pigmentation in the nasal (6a), temporal (6b) and inferior (6c) areas.
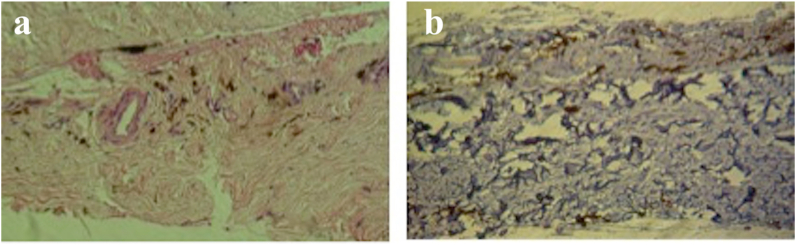
Fig. 7.
Histopathology of removed pigmented scleral lamellar tissue. Dendritic and oval-shaped melanocytes located in the superficial and middle layers of the removed scleral lamellar tissue correlating with nevus of Ota. 7a) MART 1 staining; 7b) Iron staining.
Fig. 8.
Three months postoperative AS OCT images. 8a) In the inferior nasal area, after superficial sclerectomy, a thinning of the superficial sclera is observed with a reduction in the melanocytic pigment; the thickness remained stable 12 months after surgery. 8b) The inferior temporal sector, treated with the flipped scleral flap technique, shows a superficial scleral thickness similar to the preoperative one. The flipped scleral flap is clearly visible (arrow). The appearance was unchanged 12 months after surgery.
3. Discussion
Several authors have reported using different surgical techniques to reduce or cover scleral pigmentation in patients with oculodermal melanocytosis.2,4,5,7 Each technique gives good results and has some limitations.
Kim et al.4 were the first to propose a possible surgical treatment of oculodermal melanocytosis. Due to the fact that a less pigmented scleral bed was observed during lamellar scleral dissection, their technique was based on the excision of a free scleral flap that was flipped over and attached to the scleral bed, allowing the episcleral pigmentation to be hidden internally. The main disadvantages of flipped scleral flap surgery are a longer surgical time together with a more difficult surgical procedure.
Cho et al.5 proposed a scleral graft overlay for cosmetic treatment of oculodermal melanosis. This technique involves the preparation of an allogeneic sclera from a cadaver donated eye, which is appropriately cut and thinned to cover the recipient sclera. Despite giving good results, this technique has a number of limitation, including the scarce availability of scleral grafts obtained from donor eyes and the possibility of transmission of infectious diseases transmission such as HIV, HBV and HCV.
Kim et al.2 described a grabbing and cutting technique for reducing scleral pigmentation. This procedure consists in gently grabbing and pulling the superficial pigmented area and then cutting with scissors. However, not all scleral pigmentations are eliminated, especially when the pigmentations are located deep in the sclera, and in cases of extensive ocular pigmentation patients have to undergo multiple operations to reduce all the scleral pigment.
In 2017 Jung et al.7 proposed a superficial sclerectomy as an alternative approach for oculodermal melanocytosis. This technique involves grabbing the sclera with forceps and performing a shallow, partial thickness scleral incision using scissors. Then a superficial scleral dissection is performed. The authors reported that the pigmented sclera was easily removed from the deep sclera; they assumed the presence of a cleavage plane in the scleral lamellar structure, due to the lamellar arrangement in the deep sclera, similar to that present in the anterior cornea at a depth of approximately 200 μm.8,9 After superficial scleral dissection, the authors observed a greater pigmentation of the outer scleral surface compared to the inner area, as similarly reported in previous studies.4 The advantages of this technique are a shorter operating time and a smoother postoperative scleral surface, which facilitates scleral bed healing. As noted by the authors, the limitation of this procedure lies in the difficulty of estimating the depth of scleral pigmentation and this could result in an inadequate deep dissection with excessive weakening of the sclera.
Preoperative evaluation with AS OCT images allows us to study the depth of scleral pigmentation and to plan the depth of the sclerectomy accordingly. The depth of melanocyte involvement differs from patient to patient, as some have the melanocytes in the superficial sclera, whereas others in the deeper sclera.
In our case, all AS OCT scans in the infero nasal area showed a maximum depth of pigmentation not exceeding 200 μm μm; the images showed a different reflectivity between the superficial and deep sclera, marked by a separation line (Fig. 3 A), which could correspond to the cleavage plane described previously by Jung.7 We performed a 200 μm superficial sclerectomy, peeling the superficial dissected sclera: at the end of the procedure, the scleral bed was cleaned of pigment (Fig. 4 D). The inferior temporal area showed a deeper scleral involvement, with a depth of pigmentation exceeding 250 μm, as well as the same features in terms of the reflectivity and separation line of the inferior nasal area (Fig. 3 B). We performed a 250 μm superficial sclerectomy, observing, as also reported by other authors,4,7 a lower pigmentation in the inner surface of the scleral flap (Fig. 5 C). Therefore, in order to avoid weakening the sclera, we flipped over the scleral flap and attached it to the scleral bed to hide the pigmentation internally. The use of a calibrated diamond blade to perform sclerectomy has made surgery safer and faster. AS OCT scans are an effective and accurate method for planning the depth of sclerectomy, as they may show the presence of a cleavage plane between superficial and deep sclera. In our case, most scleral pigmentation was located between 200 and 250 μm of depth of the superficial sclera, so we think that the sclerectomy should be kept within this depth to avoid an excessive weakening of the sclera.
The cosmetic result was satisfactory and no complications occurred. The patient expressed high postoperative satisfaction, claiming that he was more self-confident in social relationships, wore sunglasses less frequently, and did not avoid eye contact during conversations. Postoperative AS OCT images showed a thinning in scleral tissue with reduced pigmentation and a progressive healing process during the follow up (Fig. 8). A longer follow up will be necessary to verify the long term scleral stability revealed by the AS OCT images, as well as to check for any possible malignant transformation, given that patients with oculodermal melanocytosis are at higher risk of melanoma than those who do not have any abnormal pigmentation conditions.10 Furthermore, a longer follow up will serve to exclude any long-term scleropathy or vascular and esthesiometric alterations.
The advantage of our technique is that we can determine the depth of the pigmentation, allowing us to cut the sclera accordingly. In cases where the pigment is panscleral, a superficial sclerectomy may not give satisfactory results. This could be predicted based on the pre-operative AS OCT images.
4. Conclusions
In conclusion, surgical planning of superficial sclerectomy with AS OCT scans combined with the use of a precalibrated diamond blade is an effective procedure for cosmetic improvement of oculodermal melanocytosis. Because the main purpose of our procedure was cosmetic, we aimed to reduce scleral pigmentation by minimally thinning the sclera: the use of AS OCT images could lead to the most effective and safest surgical technique for each case, providing useful information about the extent of the pigmentation inside the sclera.
Patient consent
Written informed consent was obtained from the patient.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
No conflict of interest exists.
Acknowledgments
None.
References
- 1.Ota M. Nevus fusco-caeruleus ophthalmo-maxillaris. Jpn J Dermatol. 1939;46:369–372. [Google Scholar]
- 2.Kim J.Y., Hong J.T., Lee S.H., Lee J., Kim M.J., Tchah H. Surgical reduction of ocular pigmentation in patients with oculodermal melanocytosis. Cornea. 2012;31:520–524. doi: 10.1097/ICO.0b013e3182248110. [DOI] [PubMed] [Google Scholar]
- 3.Hulke J.W. A series of cases of carcinoma of the eye ball. Ophthalmic Hosp Rep. 1861;3:279–286. [Google Scholar]
- 4.Kim T.I., Yoon J., Choi J., Tchah H. Flipped scleral flap surgery for reduction of ocular pigmentation in oculodermal melanosis. Cornea. 2005;24:482–485. doi: 10.1097/01.ico.0000151546.00489.c9. [DOI] [PubMed] [Google Scholar]
- 5.Cho B.J., Kwon J.W., Han Y.K., Kim J.H., Wee W.R., Lee J.H. Cosmetic improvement of nevus of Ota by scleral allograft overlay. Can J Ophthalmol. 2011;46:428–430. doi: 10.1016/j.jcjo.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Benson M.T., Rennie I.G. Hemi-naevus of Ota: perturbation of neural crest differentiation as a likely mechanism. Graefes Arch Clin Exp Ophthalmol. 1992;230:226–229. doi: 10.1007/BF00176293. [DOI] [PubMed] [Google Scholar]
- 7.Jung S., Kwon T., Zhang C.C., Chuck R.S., Kwon J.W. A novel surgical approach for oculodermal melanocytosis: superficial sclerectomy. Eye Contact Lens. 2017;43:253–256. doi: 10.1097/ICL.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 8.Almubrad T., Akhtar S. Structure of corneal layers, collagen fibrils, and proteoglycans of tree shrew cornea. Mol Vis. 2011;17:2283–2291. [PMC free article] [PubMed] [Google Scholar]
- 9.Watson P.G., Young R.D. Scleral structure, organisation and disease. A review. Exp Eye Res. 2004;78:609–623. doi: 10.1016/s0014-4835(03)00212-4. [DOI] [PubMed] [Google Scholar]
- 10.Patel B.C., Egan C.A., Lucius R.W., Gerwels J.W., Mamalis N., Anderson R.L. Cutaneous malignant melanoma and oculodermal melanocytosis (nevus of Ota): report of a case and review of the literature. J Am Acad Dermatol. 1998;38:862–865. doi: 10.1016/s0190-9622(98)70477-3. [DOI] [PubMed] [Google Scholar]