Summary
Large-scale studies of human gut microbiomes have revealed broad differences in composition across geographically distinct populations. Yet, studies examining impacts of microbiome composition on various health outcomes typically focus on single populations, posing the question of whether compositional differences between populations translate into differences in susceptibility. Using germ-free mice humanized with microbiome samples from 30 donors representing three countries, we observe robust differences in susceptibility to Citrobacter rodentium, a model for enteropathogenic Escherichia coli infections, according to geographic origin. We do not see similar responses to Listeria monocytogenes infections. We further find that cohousing the most susceptible and most resistant mice confers protection from C. rodentium infection. This work underscores the importance of increasing global participation in microbiome studies related to health outcomes. Diverse cohorts are needed to identify both population-specific responses to specific microbiome interventions and to achieve broader-reaching biological conclusions that generalize across populations.
Keywords: gut microbiome, infectious disease, global health, microbiota, gastrointestinal, inflammation, inclusion, diversity
Graphical abstract

Highlights
-
•
Germ-free mice were humanized with microbiota from three global populations
-
•
Mice exhibit geography-specific susceptibilities to Citrobacter rodentium infection
-
•
Resistance to C. rodentium infection may be driven by high basal inflammation levels
-
•
Co-housing mice from different geographies improves resistance to infection
Significant differences in gut microbiome composition distinguish human populations around the globe. Using germ-free mice, Porras et al. show that microbial differences alone can impact immune responses and susceptibility to enteric infection. They show that, by co-housing mice humanized with microbiomes from different geographies, they can transfer resistance to infection.
Introduction
Mechanistic studies have provided causal linkages between the human gut microbiome and diseases ranging from inflammatory bowel disease (Britton et al., 2019; Ni et al., 2017) to atherosclerosis (Koeth et al., 2013), obesity (Ridaura et al., 2013), diabetes (Uusitalo et al., 2016; Zhang et al., 2020), and mental disorders (Zheng et al., 2016, 2019). However, these studies have primarily involved human subjects from high-income and upper-middle-income nations across North America, Europe, and Asia (Almeida et al., 2019; Brewster et al., 2019; Gupta et al., 2017; Magne et al., 2016; Nayfach et al., 2019; Olesen et al., 2020; Pasolli et al., 2019; Porras and Brito, 2019). In spite of the growing appreciation for the large-scale differences in the composition of microbiomes throughout the world (Almeida et al., 2019; Brito et al., 2016; De Filippo et al., 2010; He et al., 2018; Lin et al., 2013; Martínez et al., 2015; Nayfach et al., 2019; Pasolli et al., 2019; Yatsunenko et al., 2012; Zhong et al., 2019), studies causally linking the microbiome to health and disease outcomes have not broadly considered the global diversity of human gut microbiomes. This unexplored diversity in the composition of the gut microbiome can have important consequences for immunological function in the host (Sonnenburg and Sonnenburg, 2019).
The microbiome factors significantly into the regulation of immune homeostasis, and alterations of the gut microbiome can lead to the development of autoimmune and metabolic disorders, altered innate and adaptive immune responses to infection, and inflammation (Libertucci and Young, 2019; Wu and Wu, 2012). Furthermore, there is supporting evidence that the organisms that differ in their global distribution may contribute to promoting or reducing inflammation and maintaining homeostasis. For example, mucus-degrading species abundant in high-income countries like those of the Bacteroides and Akkermansia genera have been linked to anti-inflammatory properties and improved metabolic function (Brown et al., 2019; Plovier et al., 2017; Png et al., 2010). Species of the Prevotella genus, which dominate many microbiomes in low- and middle-income countries, have been linked to improved glucose metabolism in Swedish adults (Kovatcheva-Datchary et al., 2015). Yet, both the Prevotella and Bacteroides genera have been associated in other clinical and mouse studies with rheumatoid arthritis (Maeda et al., 2016; Scher et al., 2013), hypertension (Scher et al., 2013), obesity (Hu et al., 2015), and inflammatory bowel disease (Hickey et al., 2015; Saitoh et al., 2002) in high-income settings. Given these conflicting results, it is very difficult to translate the roles of specific members of each population’s microbiomes and rather, consideration of geographic differences in gut microbiota composition on host health may be more relevant in the context of global health.
In particular, diarrheal and enteric diseases remain a leading cause of mortality with low- and middle-income countries bearing most of the burden (GBD 2016 Diarrheal Disease Collaborators, 2018). Although many factors (host genetics, exposure to pathogens, sanitation infrastructure, delivery of clinical services, etc.) may contribute to population-level susceptibility to enteric infections (Mandeville et al., 2009), reports from populations around the world have demonstrated the crucial role of the gut microbiome in providing protection against exogenous enteropathogens. Fecal microbiota transplants in Italian, US, Canadian, and Dutch populations have proved effective for the treatment of Clostridioides difficile infections (Ianiro et al., 2018; Jiang et al., 2017; Lee et al., 2016; van Nood et al., 2013). Moreover, an individual’s gut microbiome composition can predict colonization by gut parasites like Entamoeba and soil-transmitted helminths in rural African populations (Morton et al., 2015; Rubel et al., 2020), and by Vibrio cholera in a pediatric Bangladeshi cohort (Midani et al., 2018). These seminal reports highlight the importance of exploring the causal relationship between the gut microbiome and enteric infections while considering global differences in microbiomes.
Studies in mice provide further evidence that gut microbes mediate colonization resistance to prevent infections (Libertucci and Young, 2019; McKenney and Pamer, 2015). For example, a metabolite produced by Bacteroides species inhibits colonization by Salmonella enterica (Jacobson et al., 2018), and, in both immune-deficient Raggc and chemotherapy-treated mice, gut microbes provide a defense against Listeria monocytogenes infection (Becattini et al., 2017). Similarly, changes in the microbiome can lead to increased pathogen colonization in mouse models of Escherichia coli infections (Bailey et al., 2010; Mullineaux-Sanders et al., 2017). Gut microbes regulate colonization by enteropathogens not only through direct inter-species competition but also through modulation of the host’s immune system (Caballero and Pamer, 2015). Commensal gut microbes have the capacity to induce interleukin (IL)-22- and Th17-dependent immune responses to enteric infections (Ivanov et al., 2008; Willing et al., 2011). Nonetheless, studies that explore the causal relationship between the gut microbiome and bacterial enteropathogens have not yet incorporated cohorts that test the impact of global variation in gut microbiome composition. We hypothesized that differences in the human microbiome, largely defined by geography, may underlie differences in susceptibility to enteric infection.
To test this hypothesis, we sought to transplant stool samples from three geographically distinct populations into germ-free (GF) mice. We chose to compare individuals from an urban population in Guatemala, a suburban population in the United States, and an agrarian community in the Fiji Islands. Humanized GF mice have been used extensively to study the causal relationship between gut microbiota and disease state (Baxter et al., 2014; Berer et al., 2017; Chiu et al., 2017; De Palma et al., 2017; Ridaura et al., 2013; Turnbaugh et al., 2006). Often, the ability of these models to capture the inter-individual variability of the human microbiome is limited by small donor numbers (one to five) or pseudo-replication of animal specimens (Walter et al., 2020). This pseudo-replication arises when stool from a single donor or pooled donors is transplanted into multiple mice that are later analyzed as individual biological units, thus inflating the biologically relevant sample size. To address these issues, we included 30 individual donors (10 per country), whose microbiota were individually transplanted into separate mice such that the individual biological replicates were conserved. Following colonization of the mouse guts, the animals were challenged with two enteric pathogens: (1) Citrobacter rodentium, to model enteropathogenic and enterohermmorrhagic E. coli infections (Crepin et al., 2016) and (2) L. monocytogenes. This approach allowed us to evaluate whether microbiome differences impact susceptibility to enteric infection in mice with microbiomes representative of those found in populations in the United States, Fiji, and Guatemala.
Results
Humanized gnotobiotic mice reflect their human donors and respective populations
We first chose human donors in the United States, Fiji, and Guatemala whose microbiomes were representative of their respective populations. We identified suitable donors within a cohort of Guatemalan donors from the city of Quetzaltenango recruited for this study and a subset of 36 donors from the Fiji Community Microbiome Project (Brito et al., 2016) so that they were gender and age (within 5 years) matched. For the subjects from the United States, we recruited donors with similar demographics and compared them to publicly available gut microbiome data from the same country (Yatsunenko et al., 2012). We selected a total of 10 donors (five male and five female) per country between the ages of 23 and 43 with mean ages of 32.1, 32.8, and 31.2 years old for the American, Fijian, and Guatemalan donors, respectively (Table 1). As expected based on previously published studies (Brito et al., 2016; Yatsunenko et al., 2012), after rarefying the samples and performing community-level analyses, we observed strong separation between the cohorts (Figure 1A) and significant differences in phylogenetic diversity between countries but not between donors and their respective populations (Figures S1A–S1C). Additionally, the taxonomic composition of the selected donor microbiomes was similar to that observed in other subjects within their respective populations (Figure S1D). More specifically, analysis of composition of microbes (Mandal et al., 2015) at the family level revealed eight differentially abundant families between US donors and the population, most of which are of low relative abundance (Table S1). Only one differentially abundant family between Fijian donors and population were identified, and no differences were observed between the Guatemalan groups. In this way, we confirmed that the selected donor microbiomes were representative of their respective population microbiomes.
Table 1.
Metadata of the human donors selected for this study
| United States |
Fiji |
Guatemala |
||||||
|---|---|---|---|---|---|---|---|---|
| DonorID | Gender | Age | DonorID | Gender | Age | DonorID | Gender | Age |
| U1 | F | 28 | F1 | F | 26 | G1 | F | 27 |
| U2 | F | 35 | F2 | F | 34 | G2 | F | 37 |
| U3 | M | 23 | F3 | M | 25 | G3 | M | 23 |
| U4 | F | 24 | F4 | F | 26 | G4 | F | 24 |
| U5 | M | 29 | F5 | M | 27 | G5 | M | 27 |
| U6 | F | 33 | F6 | F | 35 | G6 | F | 32 |
| U7 | M | 34 | F7 | M | 35 | G7 | M | 31 |
| U8 | M | 34 | F8 | M | 40 | G8 | M | 32 |
| U9 | M | 43 | F9 | M | 40 | G9 | M | 39 |
| U10 | F | 38 | F10 | F | 40 | G10 | F | 40 |
Ten donors per country were selected after matching for age and gender.
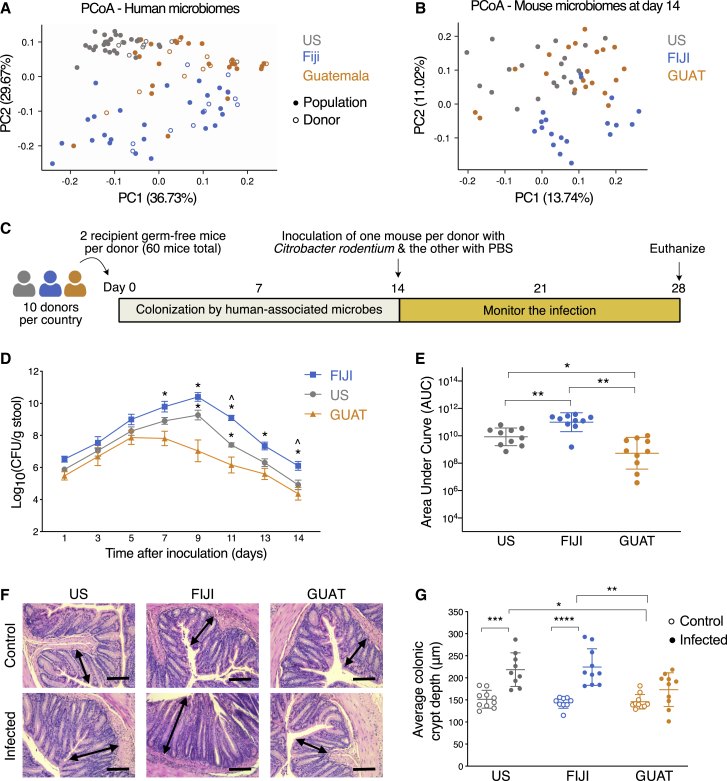
Figure 1.
Geographic differences in the microbiome lead to differences in susceptibility to C. rodentium infection in humanized mice
(A) PCoA of weighted UniFrac distances for the gut microbiomes of subjects from their respective populations including the human donors.
(B) PCoA of unweighted UniFrac distances for the gut microbiomes of the humanized mice 14 days after colonization with donor-associated microbiota.
(C) Experimental design. We obtained stool samples from 10 donors per country. Two germ-free mice received microbiota transplants from a single human donor within 24 h of arrival at our facility. For each pair of mice associated with a single donor, one mouse was inoculated with C. rodentium and the other with PBS. The infection was monitored for the following 14 days.
(D) Quantification of C. rodentium shedding in stool. Data are presented as mean ± SEM and n = 10 mice per country from two independent experiments. ∗p < 0.05 compared to GUAT mice at the same time point and ˆp < 0.05 compared to US mice at the same time point (repeated-measures two-way ANOVA followed by Tukey’s multiple comparison test).
(E) Quantification of the area under the C. rodentium shedding curve.
(F) Representative images of H&E-stained colon sections of control and infected mice 14 days after infection. The arrows depict average crypt length with hyperplasia observed in the US and FIJI mice. Scale bar represents 100 μm.
(G) Quantification of average colonic crypt depth in control and infected mice 14 days after infection.
For (E)–(G), data are presented as mean values ± SD, with ∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001, ∗∗∗∗p < 0.0001 for comparisons shown (two-way ANOVA followed by Tukey’s multiple comparison test). See also Figures S1–S5.
We next evaluated whether the microbiomes of the humanized gnotobiotic mice reflected those of their human donors. Mice whose guts were colonized with microbiota from the same donor were housed in pairs prior to inoculation with pathogenic microorganisms. A paired analysis (Fouladi et al., 2020) revealed that 53.6% ± 12.7%, 30.6% ± 13.6%, and 51.8% ± 12.6% of all amplicon sequence variants (ASVs) present in the US, FIJI, and GUAT mice, respectively, originated from their corresponding human donor (Figure S2A). This limited colonization by human donors is comparable to that reported by others in similar studies using gnotobiotic mice (Fouladi et al., 2020). After considering all ASVs in the dataset, we were able to identify that, on average, the remaining ASVs likely originated from other donors in the same country (24.1% ± 12.7% for all mice) and to a lesser extent, from donors in other countries (12.2% ± 8.6%). A small proportion of all mouse microbiomes was made up of ASVs identified only in the mice (Figures S2B–S2D; Table S2). It is important to note that even though the mice were housed in sterile filter-top cages and handled with sterile technique, rather than in gnotobiotic isolators, their microbiomes remained relatively stable over the course of the 4-week experiment (Figure S5).
To further understand the composition of the humanized mouse microbiomes, it was necessary to move beyond a presence/absence analysis and quantify the relative abundances of these ASVs. We identified that most of the US (85.3% ± 7.7%) and GUAT (70.7% ± 20.2%) microbiomes are composed of ASVs that were successfully transferred from the corresponding donor (Figures S2B–S2D). While colonization of the FIJI guts by microbiota associated with the corresponding donor was less successful (37.6% ± 18.1%), most of the ASVs in these microbiomes originated from either the original donor or another Fijian donor (total of 77.82% ± 13.4%). Not all bacterial phyla exhibit the same colonization efficiency. Taxa belonging to the Proteobacteria and Bacteroidetes phyla were better able to colonize mouse guts compared to those in the Firmicutes phylum (Figure S2E). No statistically significant differences in phylogenetic diversity were found across these mouse cohorts (Figures S3A and S3B). An analysis of the beta diversity across experimental groups revealed separation between them similar to that observed in the human donors (Figure 1B).
Geographic differences in the microbiome lead to differences in susceptibility to C. rodentium infection in humanized mice
To determine whether geographic differences in the human microbiome lead to differences in susceptibility to enteric infection, we challenged the mice with C. rodentium (1 × 109 CFU) or PBS 14 days after colonization of their guts with human-associated microbiota (Figure 1C). Monitoring of C. rodentium shedding in the stool after inoculation revealed an infection peak at day 5 for the GUAT mice compared to day 9 for both the US and FIJI mice (Figure 1D). Moreover, the GUAT mice exhibited significantly lower bacterial shedding than the FIJI and US mice starting at days 7 and 9 post-infection, respectively, with the FIJI mice presenting the highest levels of shedding throughout the course of the experiment. These differences in C. rodentium shedding between countries are also reflected in the AUC values calculated over 14 days post-infection (Figure 1E). Differences in susceptibility according to the geography of the donors were confirmed by histological analysis of explanted colons 14 days post-infection, where evidence of colonic crypt hyperplasia was observed in the US and FIJI mice but not in the GUAT mice (Figures 1F and 1G). Similar differences in cell proliferation in the colon post-infection were also observed through staining of the ki67 marker (Figure S4A). No significant differences in mouse weight and food consumption between countries were identified at any point of the experiment (Figures S4B and S4C).
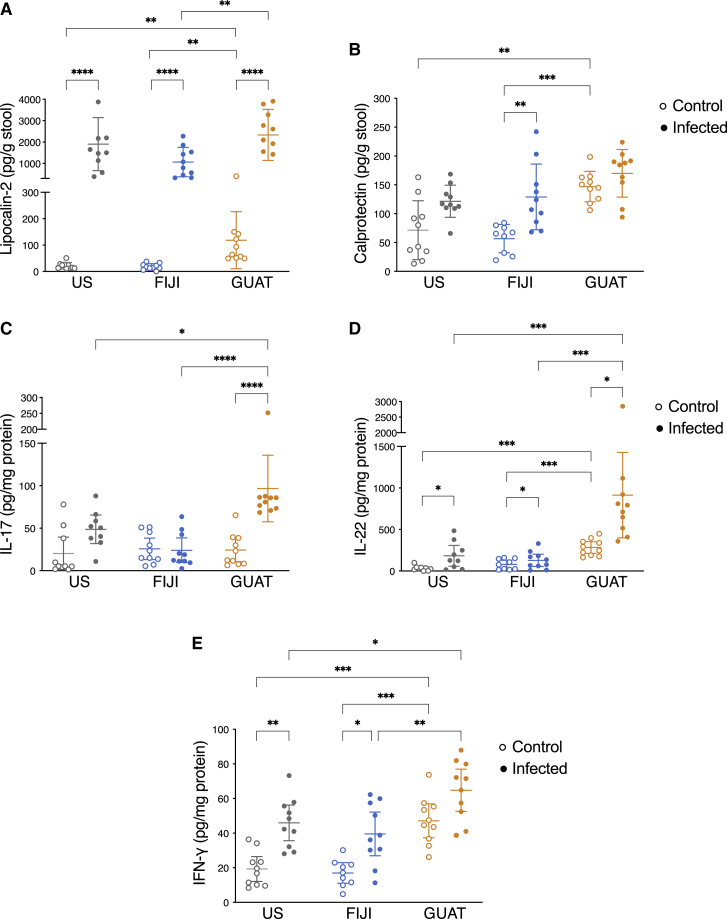
Basal inflammation levels in the GUAT mice may drive resistance to C. rodentium infection
To assess the role of inflammation in these differences, we quantified lipocalin-2 (LCN-2) and calprotectin levels in the mouse stool at the end of the experiment. Elevated levels of LCN-2 were found in the stool when comparing infected to control mice in all three cohorts, as expected after a pathogenic infection (Figure 2A). Calprotectin levels in contrast were only significantly elevated in the FIJI infected mice compared to the controls (Figure 2B). In both cases, GUAT control mice exhibited higher LCN-2 and calprotectin levels compared to their US and FIJI counterparts. We also evaluated the secretion of several inflammatory cytokines known to be involved in the defense against C. rodentium through ex vivo culture of the colon at the end of the experiment (Atarashi et al., 2015; Basu et al., 2012; Chen et al., 2015; Ivanov et al., 2009). Due to the financial and logistical limitations of germ-free mouse experiments, we were not able to assess the production of these cytokines in the early stages or at the peak of the infection, when they would be expected to be at their highest levels (Silberger et al., 2017; Waki et al., 2017). Nonetheless, colonic sections isolated from the infected GUAT mice produced significantly higher amounts of the inflammatory cytokines interleukin-17 (IL-17; Figure 2C), interleukin-22 (IL-22; Figure 2D) and interferon gamma (IFN-γ; Figure 2E) compared to their infected US and FIJI counterparts. No statistically significant differences were observed in the secretion of tumor necrosis factor alpha (TNF-α; Figure S4D) or interleukin-10 (IL-10; Figure S4E). As was the case for LCN-2 and calprotectin, IL-22 and IFN-γ were secreted in higher quantities in the GUAT control mice compared to the other two uninfected mouse cohorts (Figures 2D and 2E). These results indicate a basal level of increased inflammation in the GUAT mice that could explain the resistance against and early clearance of C. rodentium in these mice, as well as the continued elevated levels of these molecules in this cohort 14 days after inoculation.
Figure 2.
Basal inflammation levels in the GUAT mice may drive resistance to C. rodentium infection
(A and B) Assessment of (A) lipocalin-2 and (B) calprotectin levels in the stool of control and infected mice 14 days after infection.
(C–E) Quantification of the production of the inflammatory cytokines (C) IL-17, (D) IL-22, and (E) IFN-γ in ex vivo colon culture.
Data are presented as mean values ± SD, with ∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001, ∗∗∗∗p < 0.0001 for comparisons shown (two-way ANOVA followed by Tukey’s multiple comparison test, n = 10 biological replicates). See also Figure S4.
After analyzing the microbiome of all mice, we found no significant changes in microbiome composition after inoculation with either C. rodentium or PBS in any of the experimental groups (Figures S5A–S5E). Phylogenetic factorization using PhyloFactor (Washburne et al., 2017) did not identify specific ASVs or clades definitely correlated with severity of infection (Figures S5F–S5N), perhaps due to the inherent variability in the data. Additionally, our microbiome analysis may be incomplete given that it does not contained sequencing of mucosal-associated microbes that are greatly impacted during C. rodentium infections (Hoffmann et al., 2009). Overall, the results from this experiment suggest that the GUAT mice are more resistant to C. rodentium infection than their US and FIJI counterparts and are able to mount a stronger immune response against this pathogen. Moreover, these differences in susceptibility to infection mediated by the immune system are observed only 2 weeks post-transplantation of human-associated microbiota.
Country-specific microbiome differences in susceptibility to infection do not extend to a Th1 L. monocytogenes infection
Many extracellular enteric pathogens like C. rodentium and E. coli elicit a strong immune response mediated by T-helper 17 (Th17) cells (Atarashi et al., 2015; Collins et al., 2014; Zambrano-Zaragoza et al., 2014). We were interested in determining whether the same geographic effect on susceptibility to infection would be observed when the mice were challenged with a pathogen that primarily elicits a Th1 immune response (Hsieh et al., 1993; Yang et al., 2014). Using microbiota from the same donors as the C. rodentium experiments, germ-free mice were humanized in two independent experiments (5 distinct donors per country per experiment, same 10 donors total as the C. rodentium experiment; Figure 3A). Half of the mice (one per donor) were then inoculated with L. monocytogenes (1 × 104 CFU) and the other half with PBS either 2 or 4 weeks after microbiota transplantation to model an acute systemic infection. No differences in pathogen burden in the liver or spleen were observed across countries in either experiment (Figure 3B). Similarly, the gut microbiomes of these mice did not change significantly post-infection (Figure 3C; Figure S6). These results indicate that the observed differences in susceptibility to infection may be limited to the mucosal Th17 pathway within our experimental setup.
Figure 3.
Country-specific microbiome differences in susceptibility to infection do not extend to a Th1 L. monocytogenes infection
(A) Experimental design. Using stool samples from the same donors in the C. rodentium infection model, two germ-free mice per donor received microbiota transplants within 24 h of arrival at our facility. Two independent experiments were conducted, in which one mouse per pair was infected with L. monocytogenes, with the other mouse receiving a PBS mock injection, either 2 or 4 weeks after colonization with human-associated microbiota. Pathogen burden in the liver and spleen were assessed 3 days after inoculation with this pathogen.
(B) Quantification of L. monocytogenes burden in the liver and spleen of the humanized mice 3 days after infection. Horizontal line represents the mean.
(C) Unweighted UniFrac distances between samples immediately before and 3 days post-infection. No statistically significant differences were observed between countries (ns, not significant, two-way ANOVA followed by Tukey’s multiple comparison test). For all panels, n = 6–10 biological replicates. See also Figure S6.
Resistance to Citrobacter rodentium infection in susceptible gnotobiotic mice is transferrable after exposure to resistant gnotobiotic mice
We next sought to establish whether resistance to C. rodentium infection could be transferred through gut microbiota. First, we identified the 5 most susceptible and 5 most resistant mice to this pathogen in our previous experiment by comparing AUC values for C. rodentium shedding in the stool (Table S3). Coincidentally, the most susceptible and most resistant mice were originally gavaged with stool slurries prepared from Fijian and Guatemalan donors, respectively. We then transplanted the cecal contents of each of these 10 mice into 2 germ-free mice per donor. Two weeks after colonization of their guts, one mouse per donor was moved to a different cage to be cohoused with a mouse of the other experimental group for a total of 5 cohoused FIJI and GUAT pairs (Figure 4A). All mice were challenged with C. rodentium (1 × 109 CFU) 2 weeks after the beginning of the cohousing window.
Figure 4.
Resistance to Citrobacter rodentium infection in susceptible gnotobiotic mice is transferrable after exposure to resistant gnotobiotic mice
(A) Experimental design. After identifying the 5 most (FIJI) and 5 least (GUAT) susceptible mice to C. rodentium infection, we transplanted the cecal contents of those mice into germ-free mice (2 per donor, 20 mice total). Two weeks later, one mouse per donor was moved to a cage containing a mouse of the other experimental group for cohousing. Fourteen days after the beginning of the cohousing stage, all mice were infected with C. rodentium.
(B) Quantification of C. rodentium shedding in stool. Data are presented as mean ± SEM and n = 5 mice per experimental group. ∗p < 0.05 compared to single-housed Guatemalan mice at the same time point (repeated-measures two-way ANOVA followed by Tukey’s multiple comparison test).
(C) Quantification of the area under the C. rodentium shedding curve.
(D) Representative images of H&E-stained colon sections 14 days after infection. Scale bar represents 100 μm.
(E) Quantification of average colonic crypt depth 14 days after infection.
(F and G) Quantification of the production of the inflammatory cytokines (F) IL-17 and (G) IL-22 in ex vivo colon culture at the end of the experiment.
(H) Assessment of LCN-2 in the stool 2 weeks after cohousing and immediately prior to inoculation with C. rodentium.
For (C)–(H), data are presented as mean values ± SD, with ∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001, ∗∗∗∗p < 0.0001 for comparisons shown (two-way ANOVA followed by Tukey’s multiple comparison test). See also Figure S7.
As observed in the previous experiment, the single-housed FIJI mice exhibited significantly higher levels of pathogen shedding in the stool compared to the single-housed GUAT mice (Figure 4B). While the cohoused GUAT mice shed comparable amounts of C. rodentium to their single-housed counterparts, the cohoused FIJI mice excreted significantly lower levels of bacteria compared to the single-housed controls matching the levels of bacterial shedding observed in the GUAT mice (Figures 4B and 4C). Differences in pathophysiology were also evident through histological analysis of explanted colons (Figure 4D), where the average colonic crypts were significantly deeper in the single-housed FIJI mice compared to both the cohoused FIJI mice and GUAT group (Figure 4E). Furthermore, the cohoused FIJI mice secreted significantly higher quantities of IL-17 (Figure 4F) and IL-22 (Figure 4G) compared to the single-housed FIJI mice and equivalent quantities to those produced by both GUAT groups 14 days post-infection. Meanwhile, cohousing appeared to have no effect on inflammatory cytokine production for the GUAT mice (Figures 4F and 4G). No differences in the production of TNF-α (Figure S7A), IL-10 (Figure S7B), or IFN-γ (Figure S7C) were observed across donor countries or cohousing conditions. To evaluate the role of basal inflammation in this experiment, we measured LCN-2 levels in the stool on day 28, 2 weeks after cohousing, and immediately prior to inoculation with C. rodentium. Consistent with prior results, higher levels of LCN-2 were found in the single-housed GUAT mice compared to the single-housed FIJI mice (Figure 4H). In contrast, the cohoused FIJI mice exhibited significantly higher secretion of LCN-2 in the stool to levels comparable to both GUAT groups. Given that the cohoused GUAT mice remained resistant to the infection and the cohoused FIJI mice became less susceptible, the transfer of microbiota and subsequent increase in basal inflammation levels appeared to be sufficient in conferring resistance against C. rodentium.
Transfer of microbiota from resistant to susceptible mice confers resistance to infection after cohousing
We next examined the changes in the microbiome potentially responsible for this transfer of resistance to C. rodentium infection. We identified increases in beta diversity in the FIJI mice after 2 weeks of cohousing with GUAT mice but not their single-housed counterparts (Figures 5A and 5B; Figure S7D). Specifically, the microbiome composition of the cohoused FIJI mice started to resemble that of their GUAT counterparts. To confirm these observations, we performed a paired analysis of the ASV transfer between the pairs of cohoused mice. We identified a total of 94 ASVs that transferred from the GUAT to the FIJI mice across all pairs during cohousing (Table S4; Figure 5C). In contrast, only 41 ASVs were transferred from the FIJI to the GUAT mice (Table S4; Figure S7G). Among the ASVs transferred from the GUAT to the FIJI mice, those belonging to the Bacteroides genus (including B. intestinalis, B. fragilis, B. xylanisolvens, and B. stercoris), Akkermansia muciniphila, and Prevotella copri were among those present in the FIJI guts at highest abundances after cohousing (Table S4; Figure 5C). These results perhaps suggest a role for these taxa in modulating resistance to enteric infection by C. rodentium.
Figure 5.
Transfer of microbiota from resistant to susceptible mice confers resistance to infection after cohousing
(A) PCoA of unweighted UniFrac distances for the gut microbiomes of the mice on day 28 of the experiment, 2 weeks after cohousing. Labels for the paired mice are found next to each other on the figure legend.
(B) UniFrac distance between paired mice prior to (day 14) and after (day 28) the cohousing period. Horizontal line represents the mean, with ∗∗p < 0.01 and ∗∗∗p < 0.001 for comparisons shown (two-way ANOVA followed by Tukey’s multiple comparison test).
(C) Heatmap of the percent relative abundances of the top 20 most abundant taxa transferred from the GUAT mice to their FIJI cohousing partners after cohousing. The mice are presented according to their corresponding cohousing pair.
(D) Quantification of the relative abundances of the ASVs originally present in the mice prior to cohousing and transferred from their cohousing partner. See also Figure S7 and Table S4.
Notably, the ASVs that originated in the GUAT microbiomes were able to colonize the FIJI mouse guts effectively, representing 28.7% ± 22.8% of the taxa identified in these mice, whereas the ASVs that originated in the FIJI mice only made up 4.8% ± 4.4% of the GUAT microbiomes 2 weeks after cohousing (Figure 5D). No statistically significant changes in alpha diversity were observed across experimental groups after 2 weeks of cohousing (Figure S7E). The transfer of microbiota from the GUAT to FIJI mice appeared to be greater than transfer in the opposite direction. We also assessed the effect of C. rodentium infection on the microbiomes of all mice. As was the case in the previous experiment, inoculation with this pathogen did not lead to significant changes in the microbiome composition of FIJI and GUAT mice regardless of their housing status (Figure S7F). Thus, the transfer of ASVs from the GUAT to the FIJI mice was sufficient to confer resistance to C. rodentium infection.
Discussion
Here, we show that protection to enteric infection can be improved by the introduction of gut microbiota from donors depending on their geographic origins. We found microbiome-induced differences, according to population, in the protection against C. rodentium infections. More specifically, we saw increased resistance to the infection in mice that exhibited higher levels of basal inflammation after human microbiota transplantation. These effects were dynamic and could be modulated within a 2-week time period, advancing the promise of immune-modulatory microbiome-based therapies. We suspect that these effects may translate to other Th17-mediated responses, such as those involved in autoimmune disorders like rheumatoid arthritis, multiple sclerosis, or systemic lupus erythematosus, which have been linked with the microbiome (Jangi et al., 2016; López et al., 2016; Maeda et al., 2016; Scher et al., 2013). Evaluating the effects of microbiome compositions in the context of gnotobiotic mice, such as we demonstrate here, may help decouple the effects of microbiome composition from confounding factors, including population genetics, differences in diet, and disparities in access to healthcare or sanitation infrastructure. These analyses may prove important for understanding contributions of local microbiome compositions to global patterns of infectious disease and Th17-mediated autoimmune disorders (Porras and Brito, 2019; Shapira et al., 2010).
The cohousing experiment presented here highlights the malleable nature of the gut microbiome. Similar changes in microbiota composition have been reported in humans as a result of changes in diet (Gehrig et al., 2019), temporary travel (Leo et al., 2019), or permanent immigration (Vangay et al., 2018). Furthermore, the transfer of resistance to infection from GUAT to FIJI mice reinforces the potential for therapeutics that restore healthy functions to the host through the modification of the gut microbiome. This is consistent with both mouse (Rosshart et al., 2017; Smith et al., 2019; Villarino et al., 2016; Willing et al., 2011) and human microbiota transplantation studies in the context of resistance to infection (AlQahtani et al., 2020; Cheng et al., 2019, 2020; Ianiro et al., 2018; Jiang et al., 2017; Krajicek et al., 2019; Shin et al., 2019). These results support the hypothesis that geographic-level differences in gut microbiome composition may influence health outcomes. Our data supports a causal role for the microbiota irrespective of direct impacts of population genetics, health infrastructure, and other confounding factors. Nonetheless, we caution against interpreting these results as evidence of the relative benefits or side effects of any specific populations’ microbiome composition over another for various reasons. First, these experiments measure a single health outcome, susceptibility to C. rodentium and L. monocytogenes infection. Additionally, microbiota or microbiome compositions identified as deleterious for one outcome may provide a health benefit in another context or vice versa (Gilbert and Lynch, 2019). Finally, the interpretation of gnotobiotic mouse studies must consider the possibility that differences between cohorts arise due to the underlying colonization potential of the microbiomes being tested. Our results cannot exclude this explanation, as the FIJI mice experienced lower colonization by donor-associated microbiota overall. Mouse studies, including ours, provide initial validation for hypotheses but require follow-up experiments in human populations.
Our work also emphasizes the importance of study design in drawing conclusions from necessarily small-scale germ-free or gnotobiotic mouse experiments. Gnotobiotic mouse experiments require additional care to ensure control over the gut microenvironment and therefore are not amenable to a large number of donors. A recent meta-analysis of this type of experiments (Walter et al., 2020) found that most studies use a small (one to five) number of donors, whose microbiomes are then transplanted into a larger number of mice. Careful choice of multiple representative donors is therefore critical in extrapolating results obtained with small sample sizes to entire disease cohorts or geographic populations. A strength of our approach is our utilization of 30 individuals as donors, an unusually large number of donors, across several control and experimental conditions. The inherent limitations of germ-free mouse work can be partially mitigated by the use of more donors and accounting of colonization efficacy.
Overall, this study highlights the need to expand microbiome studies to account for the greater diversity in microbiome compositions globally not only in cohort-based studies (Mejía-León et al., 2014; Monaco et al., 2016; Subramanian et al., 2014; Zhong et al., 2019) but also in gnotobiotic animal experiments, which serve as a predominant tool for examining causal linkages between the microbiome and disease. On one hand, these studies may reveal population-level differences that can contribute to our understanding of the mechanisms by which the microbiome affects immunity and disease and which may contribute to geographic differences in incidence. At the same time, comparative studies may also uncover universal principles that more broadly capture mechanistic links between the microbiome and disease. Increasing the participation and inclusion of diverse populations around the world is crucial for the advancement of biomedicine. The historically poor representation of women and racial/ethnic minorities in clinical trials performed in the United States (Coakley et al., 2012; Oh et al., 2015) has resulted in the under-appreciation of sex-based or ethnicity/race-based differences in disease risk and therapeutic responses (Anderson, 2005; Dirks et al., 2004; Phan et al., 2009; Rotger et al., 2006; Zopf et al., 2008). Intentional study designs that consider the vast differences in microbiome composition across global populations will impact the development of future strategies to prevent or treat disease and inform their expected efficacy across populations (Brooks et al., 2018; Gehrig et al., 2019; Klatt et al., 2017; Mosquera et al., 2019; Panigrahi et al., 2017; Rekdal et al., 2019). This is crucial for the development of microbiome-based solutions to global health challenges.
STAR★Methods
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Biological samples | ||
| US human donor fecal samples | Cornell University | N/A |
| Guatemalan human donor fecal samples | CeSSIAM | N/A |
| Fijian human donor fecal samples | FijiCOMP | N/A |
| Antibodies | ||
| Rabbit anti-ki-67 | Thermo Fisher | RRID: AB_2341197 |
| Mouse anti-E-cadherin | BD Biosciences | RRID: AB_397581 |
| Goat anti-mouse IgG secondary antibody Alexa Fluor 488 | Thermo Fisher | RRID: AB_2534069 |
| Goat anti-rabbit Rhodamine Red-x | Thermo Fisher | RRID: AB_2556551 |
| Bacterial strains | ||
| Citrobacter rodentium | A gift from Valerie Crepin, Imperial College London | ICC 180 |
| Listeria monocytogenes | A gift from Brian Rudd, Cornell University | gB |
| Chemicals, peptides, and recombinant proteins | ||
| Brain heart infusion broth | VWR | Cat#89405-138 |
| LB Broth | VWR | Cat#97064-110 |
| Antigen unmasking solution, citrate-based | Vector Laboratories | Cat#H-3300-250 |
| DAPI | Sigma-Aldrich | Cat#D9542 |
| Fetal bovine serum | VWR | Cat#89510 |
| Penicillin-streptomycin | Sigma | Cat#P4333 |
| RPMI cell culture medium | Sigma-Aldrich | Cat#R8758 |
| AMPure XP beads | Beckman Coulter | Cat#A63880 |
| Critical commercial assays | ||
| Mouse TNF-alpha DuoSet ELISA | R&D Systems | DY410 |
| Mouse IFN-gamma DuoSet ELISA | R&D Systems | DY485 |
| Mouse IL-10 DuoSet ELISA | R&D Systems | DY417 |
| Mouse IL-17 DuoSet ELISA | R&D Systems | DY421 |
| Mouse IL-22 DuoSet ELISA | R&D Systems | DY582 |
| Mouse Lipocalin-2 DuoSet ELISA | R&D Systems | DY1851 |
| Mouse S100A8/S100A9 Heterodimer DuoSet ELISA | R&D Systems | DY582 |
| Micro BCA protein assay kit | Thermo Fisher | Cat#23235 |
| DNeasy PowerSoil HTP kit | QIAGEN | Cat#12955 |
| Platinum Hot Start PCR Master Mix | Thermo Fisher | Cat#130000014 |
| Deposited data | ||
| V4 16S rRNA genomic sequences | This study | BioProject ID PRJNA694000 |
| Experimental models: Mouse strains | ||
| Germ-free C57BL/6NTac | Taconic Biosciences | Black 6 (B6NTac), B6 |
| Germ-free C57BL/6 | National Gnotobiotic Rodent Resource Center | C57BL/6 |
| Oligonucleotides | ||
| 16S rRNA-Forward Primer 515F GTGYCAGCMGCCGCGGTAA | (Parada et al., 2016) | NA |
| 16S rRNA-Reverse Primer 806R GGACTACNVGGGTWTCTAAT | (Apprill et al., 2015) | NA |
| Software and algorithms | ||
| PRISM 9 | GraphPad | https://www.graphpad.com/scientific-software/prism/ |
| QIIME2 | (Bolyen et al., 2019) | https://qiime2.org/ |
| PhyloFactor | (Washburne et al., 2017) | https://github.com/reptalex/phylofactor |
| PhyloSeq | (Callahan et al., 2016) | https://joey711.github.io/phyloseq/ |
| DADA2 | (McMurdie and Holmes, 2013) | https://benjjneb.github.io/dada2/ |
| BioRender | BioRender | https://biorender.com/ |
| Other | ||
| gentleMACS dissociator | Miltenyi Biotec | Cat#130-093-235 |
| Coy vinyl anaerobic chamber | COY Lab Products | Cat#032714 |
Resource availability
Lead contact
Further information and requests for resources and reagents should be directed to and will be fulfilled by the Lead Contact, Dr. Ilana Brito (ibrito@cornell.edu).
Materials availability
This study did not generate new unique reagents.
Data and code availability
• V4-16S rRNA DNA sequences are available in raw format at the NCBI’s BioProject database (BioProject: PRJNA694000; https://www.ncbi.nlm.nih.gov/bioproject/694000). Relevant metadata can be found in Table S5.
• This paper does not report original code.
• Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
Experimental model and subject details
Human stool donors
Human donors were recruited in a small college town in the United States (Ithaca, NY), the third largest urban center in Guatemala (Quetzaltenango), and three agrarian villages in the Fiji Islands (Vanua Levu). Donors were required to be citizens of the respective country. Donors were recruited country between the ages of 23 and 43 years old with equal representation of subjects who identified as male and female (Table 1), Each participant provided fecal samples that were frozen within 30 minutes of collection at −20°C for a maximum of 1 hour and then moved to storage at −80°C. The samples were shipped and permanently stored at −80°C. Informed consent was obtained from all participants in accordance to the protocols approved by the Institutional Review Boards at Cornell University, Columbia University, the Massachusetts Institute of Technology, and the Broad Institute, the Human Subjects Committee at CeSSIAM in Guatemala, and the Research Ethics Review Committees at the Fiji National University and the Ministry of Health in the Fiji Islands for the Fiji Community Microbiome Project (Brito et al., 2016).
Mouse strain and husbandry
Ethical considerations
This study conformed to the National Institutes of Health guidelines on the care and use of laboratory animals. Mouse studies were performed at Cornell University (Protocol ID #2016-0088) following protocols approved by the Cornell Institutional Animal Care and Use Committee.
Mouse lines
Female germ-free C57BL/6 mice at 4-6 weeks of age were obtained from either Taconic Biosciences (C. rodentium experiments) or the National Gnotobiotic Rodent Resource Center at the University of North Carolina at Chapel Hill (L. monocytogenes experiments). Within 24 hours of arrival, the gnotobiotic mice were transferred from germ-free shipping containers to sterile filter-top cages, and orally gavaged with a human stool slurry. Mice were maintained in barrier facilities with ad libitum access to autoclaved water and rodent chow (autoclavable Teklad global 14% protein rodent maintenance diet #2014-S; Envigo) and water. To avoid cage effects on the microbiota, mice were initially housed in pairs that received stool from the same human donor and were split into individual cages upon infection of one mouse per donor. Every week, food intake and animal weight were recorded, and mice were placed in clean cages with freshly autoclaved chow and water. Mice were handled under inside a biosafety cabinet with frequent glove changes and disinfection between mice during stool collection and monitoring of body weight. Stool was collected weekly throughout the course of all experiments.
Bacterial strains
The Citrobacter rodentium ICC800 (Crepin et al., 2016) and Listeria monocytogenes gB (Rudd et al., 2011) strains were obtained, respectively, from Professor Valerie Crepin (Imperial College) and Professo Brian Rudd (Cornell University). The strains were grown aerobically at 37°C in LB media (C. rodentium; VWR) or Brain Heart Infusion Broth (L. monocytogenes; VWR).
Method details
Preparation of human stool slurries
Frozen human feces (∼100mg) were resuspended in a coy anaerobic chamber (COY Lab Products) in 1mL of reduced phosphate buffered saline (PBS) containing 0.05% L-cysteine-HCl (VWR). The fecal material sat in PBS for 15 minutes to soften followed by vortexing for 10 minutes. To separate the suspended bacteria from fibrous material, the slurries were centrifuged at 1000 g for 5 minutes. The mice were randomized into country and donor groups, and gavaged orally with 10 μL/g body weight of the corresponding slurry. Mice were monitored daily following microbiota transfer.
C. rodentium infection model
Mice were infected with C. rodentium ICC800 two weeks after the transfer of human-associated microbiota following protocols for this infection model outlined by Crepin et al. (Crepin et al., 2016). On the day prior to infection, a 15mL liquid culture of LB was inoculated from frozen C. rodentium glycerol stocks. The next day, the culture was centrifuged at 3,000xg at 4°C for 10 minutes and the pellet was resuspended in sterile PBS to obtain a final concentration of 1x109 CFUs/mL. For each pair of mice inoculated with stool from the same donor, one mouse per donor was inoculated with 200 μL of the C. rodentium suspension and the other was inoculated with 200 μL of PBS. At that point, mice were individually caged for the rest of the experiment. Mice were monitored for recovery 4-6hr after the procedure. On the day after the infection and every 2 days after, mice were weighted, and stool pellets were collected and frozen. Mice were euthanized through decapitation 14 days after inoculation with C. rodentium (4 weeks after arrival and gavage with human stool slurries).
Monitoring C. rodentium shedding
Stool pellets were collected on the first day after inoculation and every two days after. Samples were weighed and resuspended at a ratio of 0.1g/ml of PBS. Twenty minutes later, the stool was vortexed, and the mixture was centrifuged for 3 s at 2,500 g to separate suspended bacteria from filamentous material. Serial dilutions were prepared in PBS; 25 μL of each dilution was plated in triplicate onto LB agar containing kanamycin (50 μg/mL; VWR) (Crepin et al., 2016). CFUs were enumerated 24 hours later after incubation at 37°C.
Listeria Monocytogenes Infection Model
Mice were inoculated with L. monocytogenes gB 2 or 4 weeks after transfer of human-associated microbiota. Each of these experiments was conducted using stool samples from 5 unique donors per country for a total of the same 10 donors included in the C. rodentium experiments. Two days prior to inoculation, frozen stocks of L. monocytogenes were streaked onto a BHI plate and incubated at 37°C. The next day, an individual colony was picked from this plate, placed into 3mL of BHI media containing streptomycin, and incubated at 37°C overnight. The starter culture was diluted 1:10 in fresh BHI media and cultured at 37°C for 2.5-3 hours. Once the culture reached an OD600 between 0.4-0.7, the bacteria was centrifuged at 2,500 g for 10 mins and the pellet was resuspended in PBS to a final concentration of 1x105 CFU/(Smith et al., 2018; Zhang et al., 2017) One mouse per donor was inoculated with 100 μL of the L.monocytogenes solution and another with 100 μL of PBS through an intraocular injection. At that point, mice were individually caged for the rest of the experiment. Three days post-infection, mice were euthanized through decapitation.
Measurement of L. monocytogenes burden in the liver and spleen
Three days after inoculation with L. monocytogenes, the liver and spleen were collected, weighed, and placed in sterile-filtered 0.02% NP-40 (Sigma-Aldrich) in distilled deionized water. Organs were homogenized using the protein_01 program in a gentleMACS Tissue Dissociator (Milteny Biotec). Serial dilutions of these homogenates were prepared in PBS; 25 μL of each dilution was plated in triplicate on BHI plates supplemented with streptomycin and incubated at 37°C overnight (Rudd et al., 2011). Pathogen burden in the liver and spleen was then calculated after counting the L. monocytogenes CFUs on these plates.
Cohousing experiment
First, we identified the 5 most and 5 least susceptible mice to the C. rodentium infection, which happened to be those originally gavaged with stool from Fijian and Guatemalan donors, respectively. These mice were identified by comparing the area under the curve for C. rodentium shedding in the stool of each individual mice in the original experiment (Table S3). Frozen cecal contents from these donor mice was resuspended in 1ml of sterile PBS and processed as described for the human stool prior to oral gavage. Two germ-free mice per donor were orally gavaged with cecum slurry within 24 hours of arrival and housed in pairs in sterile-filter top cages. Two weeks later, one mouse per least susceptible (originally GUAT) donor was randomly assigned for cohousing with one of the mice that received a transplant from the most susceptible FIJI donors. The remaining mice (one per donor) were single housed for the remainder of the experiment. Two weeks after the beginning of cohousing, all mice were inoculated with C. rodentium. Colonization by this pathogen was monitored for 2 weeks and the mice were euthanized 14 days after inoculation (6 weeks after arrival).
Histological and immunofluorescent characterization of explanted colons
Upon euthanasia, 0.5cm of the terminal colon was collected and cut open longitudinally. Stool was removed from the colon by quickly flushing with cold PBS using a feeding needle (Braintree Scientific Inc.). Tissue sections were fixed in formalin for at least 48 hours. The samples were then sent to the Animal Health Diagnostic Center at the Cornell University College of Veterinary Medicine for paraffin embedding, sectioning, and H&E staining. Colorimetric images of the histological stain were collected on an Olympus upright BX-50 microscope at the Cornell Institute of Biotechnology’s Imaging Facility.
Prior to immunofluorescent staining, tissue sections were deparaffinized and antigen retrieval was performed for 30 minutes in citric acid buffer (pH 6.0; Vector Laboratories) at 90°C. Tissue sections were permeabilized with 0.05% Triton X-100. Autofluorescence by the tissue was quenched by incubating with 10mg/ml sodium borohydride (Sigma-Aldrich) in PBS for 30 mins at 4°C, followed by washing in PBS and blocking with 10% goat serum for 1 hour at room temperature. This was followed by staining with monoclonal antibodies against E-cadherin (1:200; BD Biosciences, RRID: AB_397581) and ki-67 (1:100, Thermo Fischer, RRID: AB_2341197) diluted in 1% goat serum in PBS overnight at 4°C. After rinsing with PBS, secondary antibodies (Thermo Fisher, RRID: AB_2534069 and AB_2556551) were applied diluted 1:500 in 1% goat serum in PBS. Finally, cell nuclei were stained with DAPI (1:500) for 10 minutes at room temperature and coverslips were placed to image the tissues. Fluorescent images were obtained on an inverted Leica DMi8 microscope.
Quantification of LCN-2 and calprotectin in mouse stool
To quantify lipocalin-2 and calprotectin levels in the stool, we followed the protocol described by Chassaing et al. (Chassaing et al., 2012). Briefly, stool pellets were weighed and reconstituted in PBS containing 0.1% Tween 20 (100mg stool per mL) followed by 10mins of vortexing. Stool sampels were then centrifuged at 10,000xg for 10 mins and the supernatant was collected and frozen at −20°C. LCN-2 and calprotectin levels were then quantified by ELISA (R&D Systems).
Quantification of inflammatory cytokine production ex vivo
Two small (1cm) sections of the colon were removed per mice after euthanasia and cut open longitudinally. The tissue was rinsed thrice with sterile PBS and stored at 4°C for transport. Upon arrival at the cell culture laboratory, the tissues were transferred into 500 μL of RPMI medium (Sigma Aldrich) supplemented with 10% fetal bovine serum (VWR) and 1% penicillin-streptomycin (Sigma) and incubated at 37°C for 24 hours in a humidified incubator. On the next day, the supernatants were collected and frozen at −20°C. The concentration of secreted inflammatory cytokines (TNF-α, IFN-γ, IL-10, IL-17, and IL-22) present in these ex vivo colonic cultures was quantified using by ELISA (R&D Systems). Cytokine concentrations were normalized to the total amount of protein in the corresponding tissue section measured using a Micro BCA protein assay kit (Thermo Fisher) after tissue lysis.
16S rRNA gene sequencing
Microbial genomic DNA was extracted from frozen human stool slurries and frozen mouse fecal pellets using QIAGEN DNeasy PowerSoil kits following the manufacturer’s instructions. The extracted DNA was cleaned using AMPure XP beads (Beckman Coulter). Following standard Earth Microbiome Project protocols (Caporaso et al., 2011), the V4 region of the 16S rRNA gene was amplified in triplicate using 515F (Parada et al., 2016) and 806R (Apprill et al., 2015) primers (barcodes 515rcbc0 to 515rcbc287), and the Platinum Hot Start PCR Master Mix (Thermo Fisher). PCR products were cleaned using AMPure XP beads and pooled for each sample. The amplicon pools were then quantified with Quant-iT PicoGreen dsDNA Reagent (Invitrogen), and 100ng of amplicons per sample were pooled prior to submission for sequencing. Paired-end sequencing (2x250bp) was performed on the Illumina MiSeq platform at the Cornell Institute of Biotechnology.
Quantification and statistical analysis
Analysis of 16S rRNA gene sequencing
16S rRNA gene sequences were imported into the Quantitative Insights into Microbial Ecology (QIIME2; https://qiime2.org/) (Bolyen et al., 2019; Caporaso et al., 2010) pipeline for analysis. First, we used DADA2 (Callahan et al., 2016) for quality control to remove chimeric sequences, retain unique sequence variants, and trim forward and reverse reads to remove poor-quality bases. Taxonomies were assigned using QIIME2′s Naive Bayes classifier trained with the SILVA rRNA database (https://www.arb-silva.de/). Prior to diversity analyses, the feature table was rarefied to 10,000 sequences per sample. We then used the ‘core-metrics-phylogenetic’ function to compute alpha and beta diversity metrics. The UniFrac distance matrices were then exported to R v 4.0.0 to generate principal coordinate analysis plots.
To analyze the transfer of the ASVs found in the microbiomes after microbiota transplantation, ASVs that were present in fewer than 10% of samples of all three countries were removed prior to any statistical analyses, resulting in the identification of a total of 367 ASVs. We compared the presence of ASVs that were originally found in the corresponding donor, in other donors of the same country, in donors of a different country, and only found in the mice following methods reported by Fouladi et al. (Fouladi et al., 2020). Briefly, we compared the presence of ASVs between recipient mice, the corresponding human donor, and donors of the same or different countries using paired and unpaired analyses. For each mouse, we quantified ASVs that were detected only in the mouse, shared with the corresponding human donor, shared with human donors (other than the original donor) of multiple countries, or shared with human donors (other than the original donor) of a single country. The relative abundances of the ASVs belonging to each of these categories were also calculated.
PhyloFactor (choice = ‘F’, nfactor = 30), a method for identifying phylogenetic edges along which putative functional ecological traits may have arisen, was used to identify the phylogenetic factors driving C. rodentium colonization and bacterial shedding (Washburne et al., 2017). To analyze the transfer of microbiota from resistant to susceptible mice after cohousing, without excluding any ASVs, we compared the presence of SVs that were originally found in the mice prior to cohousing and transferred from their cohousing partners. The transfer of an ASV between cohoused mice was determined only if the ASV was detected in the recipient mouse after cohousing but not prior to it,
Human donor selection and comparison to their respective populations
To identify suitable donors for these experiments, we first selected human donors from a Guatemalan cohort recruited for this experiment and a subset of thirty-six donors from the Fiji Community Microbiome Project (Brito et al., 2016). These donors were selected taking into account age- (within 5 years and gender-matching criteria, and taxonomic composition of their microbiomes (Figure S1D). Age- and gender-matched human donors in the United States were also recruited for this experiment. In order to evaluate the suitability of these donors, we obtained additional publicly available data from another cohort in the United States (Yatsunenko et al., 2012). The sample names for the downloaded data can be found in Figure S1D. Alpha and beta diversity metrics were calculated to compare donors and their respective cohorts within and across countries. Finally, ANCOM (Mandal et al., 2015) was employed to identify differentially abundant features between donors and their respective population for all countries.
Statistical analysis
We used GraphPad Prism v9 to perform statistical analysis for all data excluding that obtained from 16S rRNA gene sequencing. Experimental groups were compared using two-way ANOVA followed by Tukey’s multiple comparisons test. Whenever time-series data was included, repeated-measured ANOVA was used instead. The specific statistical tests used and significance thresholds are indicated in figure legends.
Acknowledgments
This work was partially supported by the Gates Foundation (OPP1161064). Additionally, A.M.P. was supported throughout this work by funding from Cornell University’s Presidential Postdoctoral Fellowship program.
Author contributions
Conceptualization, A.M.P., and I.L.B.; resources, G.M.B., and N.S.; methodology, A.M.P., Q.S., and I.L.B.; validation, A.M.P. and Q.S.; investigation, A.M.P., R.C., and Q.S.; formal analysis, data curation, and visualization, A.M.P. and H.Z.; writing – original draft, A.M.P. and I.L.B.; writing – review & editing, all authors; supervision, I.L.B.; project administration, A.M.P., Q.S., and I.L.B.; funding acquisition: I.L.B.
Declaration of interests
The authors declare no competing interests.
Inclusion and diversity
We worked to ensure gender balance in the recruitment of human subjects. We worked to ensure ethnic or other types of diversity in the recruitment of human subjects. We worked to ensure that the study questionnaires were prepared in an inclusive way. One or more of the authors of this paper self-identifies as an underrepresented ethnic minority in science. The author list of this paper includes contributors from the location where the research was conducted who participated in the data collection, design, analysis, and/or interpretation of the work.
Published: July 27, 2021
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.celrep.2021.109457.
Supplemental information
Ones and zeroes represent presence or absence, respectively in the mice from the corresponding mouse.
The data are presented as percent relative abundance in the corresponding mouse.
References
- Almeida A., Mitchell A.L., Boland M., Forster S.C., Gloor G.B., Tarkowska A., Lawley T.D., Finn R.D. A new genomic blueprint of the human gut microbiota. Nature. 2019;568:499–504. doi: 10.1038/s41586-019-0965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlQahtani H., Baloch S., Tabb D. Treatment of Recurrent Clostridium difficile Infection in an Immunocompromised Patient with Severe Neutropenia Not Responding to Standard Therapy. Case Rep. Infect. Dis. 2020;2020:3089023. doi: 10.1155/2020/3089023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G.D. Sex and racial differences in pharmacological response: where is the evidence? Pharmacogenetics, pharmacokinetics, and pharmacodynamics. J. Womens Health (Larchmt.) 2005;14:19–29. doi: 10.1089/jwh.2005.14.19. [DOI] [PubMed] [Google Scholar]
- Apprill A., McNally S., Parsons R., Weber L. Minor revision to V4 region SSU rRNA 806R gene primer greatly increases detection of SAR11 bacterioplankton. Aquat. Microb. Ecol. 2015;75:129–137. [Google Scholar]
- Atarashi K., Tanoue T., Ando M., Kamada N., Nagano Y., Narushima S., Suda W., Imaoka A., Setoyama H., Nagamori T. Th17 Cell Induction by Adhesion of Microbes to Intestinal Epithelial Cells. Cell. 2015;163:367–380. doi: 10.1016/j.cell.2015.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey M.T., Dowd S.E., Parry N.M.A., Galley J.D., Schauer D.B., Lyte M. Stressor exposure disrupts commensal microbial populations in the intestines and leads to increased colonization by Citrobacter rodentium. Infect. Immun. 2010;78:1509–1519. doi: 10.1128/IAI.00862-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R., O’Quinn D.B., Silberger D.J., Schoeb T.R., Fouser L., Ouyang W., Hatton R.D., Weaver C.T. Th22 cells are an important source of IL-22 for host protection against enteropathogenic bacteria. Immunity. 2012;37:1061–1075. doi: 10.1016/j.immuni.2012.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter N.T., Zackular J.P., Chen G.Y., Schloss P.D. Structure of the gut microbiome following colonization with human feces determines colonic tumor burden. Microbiome. 2014;2:20. doi: 10.1186/2049-2618-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becattini S., Littmann E.R., Carter R.A., Kim S.G., Morjaria S.M., Ling L., Gyaltshen Y., Fontana E., Taur Y., Leiner I.M., Pamer E.G. Commensal microbes provide first line defense against Listeria monocytogenes infection. J. Exp. Med. 2017;214:1973–1989. doi: 10.1084/jem.20170495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berer K., Gerdes L.A., Cekanaviciute E., Jia X., Xiao L., Xia Z., Liu C., Klotz L., Stauffer U., Baranzini S.E. Gut microbiota from multiple sclerosis patients enables spontaneous autoimmune encephalomyelitis in mice. Proc. Natl. Acad. Sci. USA. 2017;114:10719–10724. doi: 10.1073/pnas.1711233114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolyen E., Rideout J.R., Dillon M.R., Bokulich N.A., Abnet C.C., Al-Ghalith G.A., Alexander H., Alm E.J., Arumugam M., Asnicar F. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019;37:852–857. doi: 10.1038/s41587-019-0209-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster R., Tamburini F.B., Asiimwe E., Oduaran O., Hazelhurst S., Bhatt A.S. Surveying Gut Microbiome Research in Africans: Toward Improved Diversity and Representation. Trends Microbiol. 2019;27:824–835. doi: 10.1016/j.tim.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brito I.L., Yilmaz S., Huang K., Xu L., Jupiter S.D., Jenkins A.P., Naisilisili W., Tamminen M., Smillie C.S., Wortman J.R. Mobile genes in the human microbiome are structured from global to individual scales. Nature. 2016;535:435–439. doi: 10.1038/nature18927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton G.J., Contijoch E.J., Mogno I., Vennaro O.H., Llewellyn S.R., Ng R., Li Z., Mortha A., Merad M., Das A. Microbiotas from Humans with Inflammatory Bowel Disease Alter the Balance of Gut Th17 and RORγt+ Regulatory T Cells and Exacerbate Colitis in Mice. Immunity. 2019;50:212–224.e4. doi: 10.1016/j.immuni.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks A.W., Priya S., Blekhman R., Bordenstein S.R. Gut microbiota diversity across ethnicities in the United States. PLoS Biol. 2018;16:e2006842. doi: 10.1371/journal.pbio.2006842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E.M., Ke X., Hitchcock D., Jeanfavre S., Avila-Pacheco J., Nakata T., Arthur T.D., Fornelos N., Heim C., Franzosa E.A. Bacteroides-Derived Sphingolipids Are Critical for Maintaining Intestinal Homeostasis and Symbiosis. Cell Host Microbe. 2019;25:668–680. doi: 10.1016/j.chom.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero S., Pamer E.G. Microbiota-Mediated Inflammation and Antimicrobial Defense in the Intestine. Annu. Rev. Immunol. 2015;33:227–256. doi: 10.1146/annurev-immunol-032713-120238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan B.J., McMurdie P.J., Rosen M.J., Han A.W., Johnson A.J.A., Holmes S.P. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods. 2016;13:581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso J.G., Kuczynski J., Stombaugh J., Bittinger K., Bushman F.D., Costello E.K., Fierer N., Peña A.G., Goodrich J.K., Gordon J.I. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso J.G., Lauber C.L., Walters W.A., Berg-Lyons D., Lozupone C.A., Turnbaugh P.J., Fierer N., Knight R. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc. Natl. Acad. Sci. USA. 2011;108(Suppl 1):4516–4522. doi: 10.1073/pnas.1000080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassaing B., Srinivasan G., Delgado M.A., Young A.N., Gewirtz A.T., Vijay-Kumar M. Fecal lipocalin 2, a sensitive and broadly dynamic non-invasive biomarker for intestinal inflammation. PLoS ONE. 2012;7:e44328. doi: 10.1371/journal.pone.0044328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Waddell A., Lin Y.-D., Cantorna M.T. Dysbiosis caused by vitamin D receptor deficiency confers colonization resistance to Citrobacter rodentium through modulation of innate lymphoid cells. Mucosal Immunol. 2015;8:618–626. doi: 10.1038/mi.2014.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y.-W., Phelps E., Ganapini V., Khan N., Ouyang F., Xu H., Khanna S., Tariq R., Friedman-Moraco R.J., Woodworth M.H. Fecal microbiota transplantation for the treatment of recurrent and severe Clostridium difficile infection in solid organ transplant recipients: A multicenter experience. Am. J. Transplant. 2019;19:501–511. doi: 10.1111/ajt.15058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y.-W., Phelps E., Nemes S., Rogers N., Sagi S., Bohm M., El-Halabi M., Allegretti J.R., Kassam Z., Xu H., Fischer M. Fecal Microbiota Transplant Decreases Mortality in Patients with Refractory Severe or Fulminant Clostridioides difficile Infection. Clin. Gastroenterol. Hepatol. 2020;18:2234–2243. doi: 10.1016/j.cgh.2019.12.029. [DOI] [PubMed] [Google Scholar]
- Chiu C.-C., Ching Y.-H., Li Y.-P., Liu J.-Y., Huang Y.-T., Huang Y.-W., Yang S.-S., Huang W.-C., Chuang H.-L. Nonalcoholic Fatty Liver Disease Is Exacerbated in High-Fat Diet-Fed Gnotobiotic Mice by Colonization with the Gut Microbiota from Patients with Nonalcoholic Steatohepatitis. Nutrients. 2017;9:1220. doi: 10.3390/nu9111220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coakley M., Fadiran E.O., Parrish L.J., Griffith R.A., Weiss E., Carter C. Dialogues on diversifying clinical trials: successful strategies for engaging women and minorities in clinical trials. J. Womens Health (Larchmt.) 2012;21:713–716. doi: 10.1089/jwh.2012.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins J.W., Keeney K.M., Crepin V.F., Rathinam V.A.K., Fitzgerald K.A., Finlay B.B., Frankel G. Citrobacter rodentium: infection, inflammation and the microbiota. Nat. Rev. Microbiol. 2014;12:612–623. doi: 10.1038/nrmicro3315. [DOI] [PubMed] [Google Scholar]
- Crepin V.F., Collins J.W., Habibzay M., Frankel G. Citrobacter rodentium mouse model of bacterial infection. Nat. Protoc. 2016;11:1851–1876. doi: 10.1038/nprot.2016.100. [DOI] [PubMed] [Google Scholar]
- De Filippo C., Cavalieri D., Di Paola M., Ramazzotti M., Poullet J.B., Massart S., Collini S., Pieraccini G., Lionetti P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA. 2010;107:14691–14696. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Palma G., Lynch M.D.J., Lu J., Dang V.T., Deng Y., Jury J., Umeh G., Miranda P.M., Pigrau Pastor M., Sidani S. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci. Transl. Med. 2017;9:eaaf6397. doi: 10.1126/scitranslmed.aaf6397. [DOI] [PubMed] [Google Scholar]
- Dirks N.L., Huth B., Yates C.R., Meibohm B. Pharmacokinetics of immunosuppressants: a perspective on ethnic differences. Int. J. Clin. Pharmacol. Ther. 2004;42:701–718. doi: 10.5414/cpp42701. [DOI] [PubMed] [Google Scholar]
- Fouladi F., Glenny E.M., Bulik-Sullivan E.C., Tsilimigras M.C.B., Sioda M., Thomas S.A., Wang Y., Djukic Z., Tang Q., Tarantino L.M. Sequence variant analysis reveals poor correlations in microbial taxonomic abundance between humans and mice after gnotobiotic transfer. ISME J. 2020;14:1809–1820. doi: 10.1038/s41396-020-0645-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Diarrheal Disease Collaborators Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018;18:1211–1228. doi: 10.1016/S1473-3099(18)30362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehrig J.L., Venkatesh S., Chang H.-W., Hibberd M.C., Kung V.L., Cheng J., Chen R.Y., Subramanian S., Cowardin C.A., Meier M.F. Effects of microbiota-directed foods in gnotobiotic animals and undernourished children. Science. 2019;365:eaau4732. doi: 10.1126/science.aau4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert J.A., Lynch S.V. Community ecology as a framework for human microbiome research. Nat. Med. 2019;25:884–889. doi: 10.1038/s41591-019-0464-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta V.K., Paul S., Dutta C. Geography, Ethnicity or Subsistence-Specific Variations in Human Microbiome Composition and Diversity. Front. Microbiol. 2017;8:1162. doi: 10.3389/fmicb.2017.01162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y., Wu W., Zheng H.-M., Li P., McDonald D., Sheng H.-F., Chen M.-X., Chen Z.-H., Ji G.-Y., Zheng Z.-D.-X. Regional variation limits applications of healthy gut microbiome reference ranges and disease models. Nat. Med. 2018;24:1532–1535. doi: 10.1038/s41591-018-0164-x. [DOI] [PubMed] [Google Scholar]
- Hickey C.A., Kuhn K.A., Donermeyer D.L., Porter N.T., Jin C., Cameron E.A., Jung H., Kaiko G.E., Wegorzewska M., Malvin N.P. Colitogenic Bacteroides thetaiotaomicron antigens access host immune cells in a sulfatase-dependent manner via outer membrane vesicles. Cell Host Microbe. 2015;17:672–680. doi: 10.1016/j.chom.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann C., Hill D.A., Minkah N., Kirn T., Troy A., Artis D., Bushman F. Community-wide response of the gut microbiota to enteropathogenic Citrobacter rodentium infection revealed by deep sequencing. Infect. Immun. 2009;77:4668–4678. doi: 10.1128/IAI.00493-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh C.S., Macatonia S.E., Tripp C.S., Wolf S.F., O’Garra A., Murphy K.M. Development of TH1 CD4+ T cells through IL-12 produced by Listeria-induced macrophages. Science. 1993;260:547–549. doi: 10.1126/science.8097338. [DOI] [PubMed] [Google Scholar]
- Hu H.-J., Park S.-G., Jang H.B., Choi M.K., Park K.-H., Kang J.H., Park S.I., Lee H.-J., Cho S.-H. Obesity Alters the Microbial Community Profile in Korean Adolescents. PLoS ONE. 2015;10:e0134333. doi: 10.1371/journal.pone.0134333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ianiro G., Masucci L., Quaranta G., Simonelli C., Lopetuso L.R., Sanguinetti M., Gasbarrini A., Cammarota G. Randomised clinical trial: faecal microbiota transplantation by colonoscopy plus vancomycin for the treatment of severe refractory Clostridium difficile infection-single versus multiple infusions. Aliment. Pharmacol. Ther. 2018;48:152–159. doi: 10.1111/apt.14816. [DOI] [PubMed] [Google Scholar]
- Ivanov I.I., Frutos R. de L., Manel N., Yoshinaga K., Rifkin D.B., Sartor R.B., Finlay B.B., Littman D.R. Specific microbiota direct the differentiation of IL-17-producing T-helper cells in the mucosa of the small intestine. Cell Host Microbe. 2008;4:337–349. doi: 10.1016/j.chom.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov I.I., Atarashi K., Manel N., Brodie E.L., Shima T., Karaoz U., Wei D., Goldfarb K.C., Santee C.A., Lynch S.V. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–498. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson A., Lam L., Rajendram M., Tamburini F., Honeycutt J., Pham T., Van Treuren W., Pruss K., Stabler S.R., Lugo K. A Gut Commensal-Produced Metabolite Mediates Colonization Resistance to Salmonella Infection. Cell Host Microbe. 2018;24:296–307.e7. doi: 10.1016/j.chom.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangi S., Gandhi R., Cox L.M., Li N., von Glehn F., Yan R., Patel B., Mazzola M.A., Liu S., Glanz B.L. Alterations of the human gut microbiome in multiple sclerosis. Nat. Commun. 2016;7:12015. doi: 10.1038/ncomms12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Z.D., Ajami N.J., Petrosino J.F., Jun G., Hanis C.L., Shah M., Hochman L., Ankoma-Sey V., DuPont A.W., Wong M.C. Randomised clinical trial: faecal microbiota transplantation for recurrent Clostridum difficile infection - fresh, or frozen, or lyophilised microbiota from a small pool of healthy donors delivered by colonoscopy. Aliment. Pharmacol. Ther. 2017;45:899–908. doi: 10.1111/apt.13969. [DOI] [PubMed] [Google Scholar]
- Klatt N.R., Cheu R., Birse K., Zevin A.S., Perner M., Noël-romas L., Grobler A., Westmacott G., Xie I.Y., Butler J. Vaginal bacteria modify HIV tenofovor microbicide efficacin African women. Science. 2017;945:938–945. doi: 10.1126/science.aai9383. [DOI] [PubMed] [Google Scholar]
- Koeth R.A., Wang Z., Levison B.S., Buffa J.A., Org E., Sheehy B.T., Britt E.B., Fu X., Wu Y., Li L. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013;19:576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovatcheva-Datchary P., Nilsson A., Akrami R., Lee Y.S., De Vadder F., Arora T., Hallen A., Martens E., Björck I., Bäckhed F. Dietary Fiber-Induced Improvement in Glucose Metabolism Is Associated with Increased Abundance of Prevotella. Cell Metab. 2015;22:971–982. doi: 10.1016/j.cmet.2015.10.001. [DOI] [PubMed] [Google Scholar]
- Krajicek E., Bohm M., Sagi S., Fischer M. Fulminant Clostridium difficile Infection Cured by Fecal Microbiota Transplantation in a Bone Marrow Transplant Recipient With Critical Neutropenia. ACG Case Rep. J. 2019;6:e00198. doi: 10.14309/crj.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.H., Steiner T., Petrof E.O., Smieja M., Roscoe D., Nematallah A., Weese J.S., Collins S., Moayyedi P., Crowther M. Frozen vs fresh fecal microbiota transplantation and clinical resolution of diarrhea in patients with recurrent clostridium difficile infection a randomized clinical trial. JAMA - JAMA. 2016;315:142–149. doi: 10.1001/jama.2015.18098. [DOI] [PubMed] [Google Scholar]
- Leo S., Lazarevic V., Gaïa N., Estellat C., Girard M., Matheron S., Armand-Lefèvre L., Andremont A., Schrenzel J., Ruppé E. The intestinal microbiota predisposes to traveler’s diarrhea and to the carriage of multidrug-resistant Enterobacteriaceae after traveling to tropical regions. Gut Microbes. 2019;10:631–641. doi: 10.1080/19490976.2018.1564431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libertucci J., Young V.B. The role of the microbiota in infectious diseases. Nat. Microbiol. 2019;4:35–45. doi: 10.1038/s41564-018-0278-4. [DOI] [PubMed] [Google Scholar]
- Lin A., Bik E.M., Costello E.K., Dethlefsen L., Haque R., Relman D.A., Singh U. Distinct distal gut microbiome diversity and composition in healthy children from Bangladesh and the United States. PLoS ONE. 2013;8:e53838. doi: 10.1371/journal.pone.0053838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López P., de Paz B., Rodríguez-Carrio J., Hevia A., Sánchez B., Margolles A., Suárez A. Th17 responses and natural IgM antibodies are related to gut microbiota composition in systemic lupus erythematosus patients. Sci. Rep. 2016;6:24072. doi: 10.1038/srep24072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda Y., Kurakawa T., Umemoto E., Motooka D., Ito Y., Gotoh K., Hirota K., Matsushita M., Furuta Y., Narazaki M. Dysbiosis Contributes to Arthritis Development via Activation of Autoreactive T Cells in the Intestine. Arthritis Rheumatol. 2016;68:2646–2661. doi: 10.1002/art.39783. [DOI] [PubMed] [Google Scholar]
- Magne F., O’Ryan M.L., Vidal R., Farfan M. The human gut microbiome of Latin America populations: a landscape to be discovered. Curr. Opin. Infect. Dis. 2016;29:528–537. doi: 10.1097/QCO.0000000000000300. [DOI] [PubMed] [Google Scholar]
- Mandal S., Van Treuren W., White R.A., Eggesbø M., Knight R., Peddada S.D. Analysis of composition of microbiomes: a novel method for studying microbial composition. Microb. Ecol. Health Dis. 2015;26:27663. doi: 10.3402/mehd.v26.27663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandeville K.L., Krabshuis J., Ladep N.G., Mulder C.J.J., Quigley E.M.M., Khan S.A. Gastroenterology in developing countries: issues and advances. World J. Gastroenterol. 2009;15:2839–2854. doi: 10.3748/wjg.15.2839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez I., Stegen J.C., Maldonado-Gómez M.X., Eren A.M., Siba P.M., Greenhill A.R., Walter J. The gut microbiota of rural papua new guineans: composition, diversity patterns, and ecological processes. Cell Rep. 2015;11:527–538. doi: 10.1016/j.celrep.2015.03.049. [DOI] [PubMed] [Google Scholar]
- McKenney P.T., Pamer E.G. From Hype to Hope: The Gut Microbiota in Enteric Infectious Disease. Cell. 2015;163:1326–1332. doi: 10.1016/j.cell.2015.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurdie P.J., Holmes S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejía-León M.E., Petrosino J.F., Ajami N.J., Domínguez-Bello M.G., de la Barca A.M.C. Fecal microbiota imbalance in Mexican children with type 1 diabetes. Sci. Rep. 2014;4:3814. doi: 10.1038/srep03814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midani F.S., Weil A.A., Chowdhury F., Begum Y.A., Khan A.I., Debela M.D., Durand H.K., Reese A.T., Nimmagadda S.N., Silverman J.D. Human Gut Microbiota Predicts Susceptibility to Vibrio cholerae Infection. J. Infect. Dis. 2018;218:645–653. doi: 10.1093/infdis/jiy192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaco C.L., Gootenberg D.B., Zhao G., Handley S.A., Ghebremichael M.S., Lim E.S., Lankowski A., Baldridge M.T., Wilen C.B., Flagg M. Altered Virome and Bacterial Microbiome in Human Immunodeficiency Virus-Associated Acquired Immunodeficiency Syndrome. Cell Host Microbe. 2016;19:311–322. doi: 10.1016/j.chom.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton E.R., Lynch J., Froment A., Lafosse S., Heyer E., Przeworski M., Blekhman R., Ségurel L. Variation in Rural African Gut Microbiota Is Strongly Correlated with Colonization by Entamoeba and Subsistence. PLoS Genet. 2015;11:e1005658. doi: 10.1371/journal.pgen.1005658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosquera M.J., Kim S., Zhou H., Jing T.T., Luna M., Guss J.D., Reddy P., Lai K., Leifer C.A., Brito I.L. Immunomodulatory nanogels overcome restricted immunity in a murine model of gut microbiome-mediated metabolic syndrome. Sci. Adv. 2019;5:eaav9788. doi: 10.1126/sciadv.aav9788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullineaux-Sanders C., Collins J.W., Ruano-Gallego D., Levy M., Pevsner-Fischer M., Glegola-Madejska I.T., Sågfors A.M., Wong J.L.C., Elinav E., Crepin V.F., Frankel G. Citrobacter rodentium Relies on Commensals for Colonization of the Colonic Mucosa. Cell Rep. 2017;21:3381–3389. doi: 10.1016/j.celrep.2017.11.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayfach S., Shi Z.J., Seshadri R., Pollard K.S., Kyrpides N.C. New insights from uncultivated genomes of the global human gut microbiome. Nature. 2019;568:505–510. doi: 10.1038/s41586-019-1058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni J., Shen T.D., Chen E.Z., Bittinger K., Bailey A., Roggiani M., Sirota-Madi A., Friedman E.S., Chau L., Lin A. A role for bacterial urease in gut dysbiosis and Crohn’s disease. Sci. Transl. Med. 2017;9:9. doi: 10.1126/scitranslmed.aah6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh S.S., Galanter J., Thakur N., Pino-Yanes M., Barcelo N.E., White M.J., de Bruin D.M., Greenblatt R.M., Bibbins-Domingo K., Wu A.H.B. Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled. PLoS Med. 2015;12:e1001918. doi: 10.1371/journal.pmed.1001918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen S.W., Panchal P., Chen J., Budree S., Osman M. Global disparities in faecal microbiota transplantation research. Lancet Gastroenterol. Hepatol. 2020;5:241. doi: 10.1016/S2468-1253(19)30452-2. [DOI] [PubMed] [Google Scholar]
- Panigrahi P., Parida S., Nanda N.C., Satpathy R., Pradhan L., Chandel D.S., Baccaglini L., Mohapatra A., Mohapatra S.S., Misra P.R. A randomized synbiotic trial to prevent sepsis among infants in rural India. Nature. 2017;548:407–412. doi: 10.1038/nature23480. [DOI] [PubMed] [Google Scholar]
- Parada A.E., Needham D.M., Fuhrman J.A. Every base matters: assessing small subunit rRNA primers for marine microbiomes with mock communities, time series and global field samples. Environ. Microbiol. 2016;18:1403–1414. doi: 10.1111/1462-2920.13023. [DOI] [PubMed] [Google Scholar]
- Pasolli E., Asnicar F., Manara S., Zolfo M., Karcher N., Armanini F., Beghini F., Manghi P., Tett A., Ghensi P. Extensive Unexplored Human Microbiome Diversity Revealed by Over 150,000 Genomes from Metagenomes Spanning Age, Geography, and Lifestyle. Cell. 2019;176:649–662.e20. doi: 10.1016/j.cell.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan V.H., Moore M.M., McLachlan A.J., Piquette-Miller M., Xu H., Clarke S.J. Ethnic differences in drug metabolism and toxicity from chemotherapy. Expert Opin. Drug Metab. Toxicol. 2009;5:243–257. doi: 10.1517/17425250902800153. [DOI] [PubMed] [Google Scholar]
- Plovier H., Everard A., Druart C., Depommier C., Van Hul M., Geurts L., Chilloux J., Ottman N., Duparc T., Lichtenstein L. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat. Med. 2017;23:107–113. doi: 10.1038/nm.4236. [DOI] [PubMed] [Google Scholar]
- Png C.W., Lindén S.K., Gilshenan K.S., Zoetendal E.G., McSweeney C.S., Sly L.I., McGuckin M.A., Florin T.H.J. Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am. J. Gastroenterol. 2010;105:2420–2428. doi: 10.1038/ajg.2010.281. [DOI] [PubMed] [Google Scholar]
- Porras A.M., Brito I.L. The internationalization of human microbiome research. Curr. Opin. Microbiol. 2019;50:50–55. doi: 10.1016/j.mib.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rekdal V.M., Bess E.N., Bisanz J.E., Turnbaugh P.J., Balskus E.P. Discovery and inhibition of an interspecies gut bacterial pathway for Levodopa metabolism. Science. 2019;364:1055. doi: 10.1126/science.aau6323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridaura V.K., Faith J.J., Rey F.E., Cheng J., Duncan A.E., Kau A.L., Griffin N.W., Lombard V., Henrissat B., Bain J.R. Gut Microbiota from Twins Discordant for Obesity Modulate Metabolism in Mice. Science. 2013;341 doi: 10.1126/science.1241214. 1241214–1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosshart S.P., Vassallo B.G., Angeletti D., Hutchinson D.S., Morgan A.P., Takeda K., Hickman H.D., McCulloch J.A., Badger J.H., Ajami N.J. Wild Mouse Gut Microbiota Promotes Host Fitness and Improves Disease Resistance. Cell. 2017;171:1015–1028.e13. doi: 10.1016/j.cell.2017.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotger M., Csajka C., Telenti A. Genetic, ethnic, and gender differences in the pharmacokinetics of antiretroviral agents. Curr. HIV/AIDS Rep. 2006;3:118–125. doi: 10.1007/BF02696655. [DOI] [PubMed] [Google Scholar]
- Rubel M.A., Abbas A., Taylor L.J., Connell A., Tanes C., Bittinger K., Ndze V.N., Fonsah J.Y., Ngwang E., Essiane A. Lifestyle and the presence of helminths is associated with gut microbiome composition in Cameroonians. Genome Biol. 2020;21:122. doi: 10.1186/s13059-020-02020-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd B.D., Venturi V., Li G., Samadder P., Ertelt J.M., Way S.S., Davenport M.P., Nikolich-Žugich J. Nonrandom attrition of the naive CD8+ T-cell pool with aging governed by T-cell receptor:pMHC interactions. Proc. Natl. Acad. Sci. USA. 2011;108:13694–13699. doi: 10.1073/pnas.1107594108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitoh S., Noda S., Aiba Y., Takagi A., Sakamoto M., Benno Y., Koga Y. Bacteroides ovatus as the predominant commensal intestinal microbe causing a systemic antibody response in inflammatory bowel disease. Clin. Diagn. Lab. Immunol. 2002;9:54–59. doi: 10.1128/CDLI.9.1.54-59.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher J.U., Sczesnak A., Longman R.S., Segata N., Ubeda C., Bielski C., Rostron T., Cerundolo V., Pamer E.G., Abramson S.B. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. eLife. 2013;2:e01202. doi: 10.7554/eLife.01202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapira Y., Agmon-Levin N., Shoenfeld Y. Defining and analyzing geoepidemiology and human autoimmunity. J. Autoimmun. 2010;34:J168–J177. doi: 10.1016/j.jaut.2009.11.018. [DOI] [PubMed] [Google Scholar]
- Shin J.H., Chaplin A.S., Hays R.A., Kolling G.L., Vance S., Guerrant R.L., Archbald-Pannone L., Warren C.A. Outcomes of a Multidisciplinary Clinic in Evaluating Recurrent Clostridioides difficile Infection Patients for Fecal Microbiota Transplant: A Retrospective Cohort Analysis. J. Clin. Med. 2019;8:1036. doi: 10.3390/jcm8071036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberger D.J., Zindl C.L., Weaver C.T. Citrobacter rodentium: a model enteropathogen for understanding the interplay of innate and adaptive components of type 3 immunity. Mucosal Immunol. 2017;10:1108–1117. doi: 10.1038/mi.2017.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith N.L., Patel R.K., Reynaldi A., Grenier J.K., Wang J., Watson N.B., Nzingha K., Yee Mon K.J., Peng S.A., Grimson A. Developmental Origin Governs CD8+ T Cell Fate Decisions during Infection. Cell. 2018;174:117–130.e14. doi: 10.1016/j.cell.2018.05.029. [DOI] [PubMed] [Google Scholar]
- Smith A.D., Foss E.D., Zhang I., Hastie J.L., Giordano N.P., Gasparyan L., VinhNguyen L.P., Schubert A.M., Prasad D., McMichael H.L. Microbiota of MR1 deficient mice confer resistance against Clostridium difficile infection. PLoS ONE. 2019;14:e0223025. doi: 10.1371/journal.pone.0223025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenburg E.D., Sonnenburg J.L. The ancestral and industrialized gut microbiota and implications for human health. Nat. Rev. Microbiol. 2019;17:383–390. doi: 10.1038/s41579-019-0191-8. [DOI] [PubMed] [Google Scholar]
- Subramanian S., Huq S., Yatsunenko T., Haque R., Mahfuz M., Alam M.A., Benezra A., DeStefano J., Meier M.F., Muegge B.D. Persistent gut microbiota immaturity in malnourished Bangladeshi children. Nature. 2014;510:417–421. doi: 10.1038/nature13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- Uusitalo U., Liu X., Yang J., Aronsson C.A., Hummel S., Butterworth M., Lernmark Å., Rewers M., Hagopian W., She J.X., TEDDY Study Group Association of Early Exposure of Probiotics and Islet Autoimmunity in the TEDDY Study. JAMA Pediatr. 2016;170:20–28. doi: 10.1001/jamapediatrics.2015.2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Nood E., Vrieze A., Nieuwdorp M., Fuentes S., Zoetendal E.G., de Vos W.M., Visser C.E., Kuijper E.J., Bartelsman J.F.W.M., Tijssen J.G.P. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 2013;368:407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- Vangay P., Johnson A.J., Ward T.L., Kashyap P.C., Culhane-Pera K.A., Knights Correspondence D. US Immigration Westernizes the Human Gut Microbiome. Cell. 2018;175:962–972. doi: 10.1016/j.cell.2018.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarino N.F., LeCleir G.R., Denny J.E., Dearth S.P., Harding C.L., Sloan S.S., Gribble J.L., Campagna S.R., Wilhelm S.W., Schmidt N.W. Composition of the gut microbiota modulates the severity of malaria. Proc. Natl. Acad. Sci. USA. 2016;113:2235–2240. doi: 10.1073/pnas.1504887113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waki N., Kuwabara Y., Yoshikawa Y., Suganuma H., Koide H., Oku N., Ohashi N. Amelioration of Citrobacter rodentium proliferation in early stage of infection in mice by pretreatment with Lactobacillus brevis KB290 and verification using in vivo bioluminescence imaging. FEMS Microbiol. Lett. 2017;364:364. doi: 10.1093/femsle/fnw254. [DOI] [PubMed] [Google Scholar]
- Walter J., Armet A.M., Finlay B.B., Shanahan F. Establishing or Exaggerating Causality for the Gut Microbiome: Lessons from Human Microbiota-Associated Rodents. Cell. 2020;180:221–232. doi: 10.1016/j.cell.2019.12.025. [DOI] [PubMed] [Google Scholar]
- Washburne A.D., Silverman J.D., Leff J.W., Bennett D.J., Darcy J.L., Mukherjee S., Fierer N., David L.A. Phylogenetic factorization of compositional data yields lineage-level associations in microbiome datasets. PeerJ. 2017;5:e2969. doi: 10.7717/peerj.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willing B.P., Vacharaksa A., Croxen M., Thanachayanont T., Finlay B.B. Altering host resistance to infections through microbial transplantation. PLoS ONE. 2011;6:e26988. doi: 10.1371/journal.pone.0026988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H.J., Wu E. The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes. 2012;3:4–14. doi: 10.4161/gmic.19320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Torchinsky M.B., Gobert M., Xiong H., Xu M., Linehan J.L., Alonzo F., Ng C., Chen A., Lin X. Focused specificity of intestinal TH17 cells towards commensal bacterial antigens. Nature. 2014;510:152–156. doi: 10.1038/nature13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatsunenko T., Rey F.E., Manary M.J., Trehan I., Dominguez-Bello M.G., Contreras M., Magris M., Hidalgo G., Baldassano R.N., Anokhin A.P. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano-Zaragoza J.F., Romo-Martínez E.J., Durán-Avelar M.D.J., García-Magallanes N., Vibanco-Pérez N. Th17 cells in autoimmune and infectious diseases. Int. J. Inflam. 2014;2014:651503. doi: 10.1155/2014/651503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T., Abel S., Abel Zur Wiesch P., Sasabe J., Davis B.M., Higgins D.E., Waldor M.K. Deciphering the landscape of host barriers to Listeria monocytogenes infection. Proc. Natl. Acad. Sci. USA. 2017;114:6334–6339. doi: 10.1073/pnas.1702077114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P.P., Li L.L., Han X., Li Q.W., Zhang X.H., Liu J.J., Wang Y. Fecal microbiota transplantation improves metabolism and gut microbiome composition in db/db mice. Acta Pharmacol. Sin. 2020;41:678–685. doi: 10.1038/s41401-019-0330-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng P., Zeng B., Zhou C., Liu M., Fang Z., Xu X., Zeng L., Chen J., Fan S., Du X. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry. 2016;21:786–796. doi: 10.1038/mp.2016.44. [DOI] [PubMed] [Google Scholar]
- Zheng P., Zeng B., Liu M., Chen J., Pan J., Han Y., Liu Y., Cheng K., Zhou C., Wang H. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice. Sci. Adv. 2019;5:eaau8317. doi: 10.1126/sciadv.aau8317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong H., Ren H., Lu Y., Fang C., Hou G., Yang Z., Chen B., Yang F., Zhao Y., Shi Z. Distinct gut metagenomics and metaproteomics signatures in prediabetics and treatment-naïve type 2 diabetics. EBioMedicine. 2019;47:373–383. doi: 10.1016/j.ebiom.2019.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zopf Y., Rabe C., Neubert A., Gassmann K.G., Rascher W., Hahn E.G., Brune K., Dormann H. Women encounter ADRs more often than do men. Eur. J. Clin. Pharmacol. 2008;64:999–1004. doi: 10.1007/s00228-008-0494-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Ones and zeroes represent presence or absence, respectively in the mice from the corresponding mouse.
The data are presented as percent relative abundance in the corresponding mouse.
Data Availability Statement
• V4-16S rRNA DNA sequences are available in raw format at the NCBI’s BioProject database (BioProject: PRJNA694000; https://www.ncbi.nlm.nih.gov/bioproject/694000). Relevant metadata can be found in Table S5.
• This paper does not report original code.
• Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.