Abstract
COVID-19 is a contagious viral disease caused by SARS-CoV-2 that led to an ongoing pandemic with massive global health and socioeconomic consequences. The disease is characterized primarily, but not exclusively, by respiratory clinical manifestations ranging from mild common cold symptoms, including cough and fever, to severe respiratory distress and multi-organ failure. Macrophages, a heterogeneous group of yolk-sac derived, tissue-resident mononuclear phagocytes of complex ontogeny present in all mammalian organs, play critical roles in developmental, homeostatic and host defense processes with tissue-dependent plasticity. In case of infection, they are responsible for early pathogen recognition, initiation and resolution of inflammation, as well as repair of tissue damage. Monocytes, bone-marrow derived blood-resident phagocytes, are recruited under pathological conditions such as viral infections to the affected tissue to defend the organism against invading pathogens and to aid in efficient resolution of inflammation. Given their pivotal function in host defense and the potential danger posed by their dysregulated hyperinflammation, understanding monocyte and macrophage phenotypes in COVID-19 is key for tackling the disease’s pathological mechanisms. Here, we outline current knowledge on monocytes and macrophages in homeostasis and viral infections and summarize concepts and key findings on their role in COVID-19. While monocytes in the blood of patients with moderate COVID-19 present with an inflammatory, interferon-stimulated gene (ISG)-driven phenotype, cellular dysfunction epitomized by loss of HLA-DR expression and induction of S100 alarmin expression is their dominant feature in severe disease. Pulmonary macrophages in COVID-19 derived from infiltrating inflammatory monocytes are in a hyperactivated state resulting in a detrimental loop of pro-inflammatory cytokine release and recruitment of cytotoxic effector cells thereby exacerbating tissue damage at the site of infection.
Keywords: monocytes, macrophage, COVID-19, SARS-CoV-2, hyperinflammation, scRNA-seq, alveolar macrophage, viral infection
Introduction
COVID-19 (1, 2) is primarily a mild to moderate respiratory tract infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), an enveloped, single-stranded RNA betacoronavirus (3–5). While 80% of the infections lead to asymptomatic or mild disease with common cold symptoms including dry cough, headache, loss of taste, dyspnea, fatigue and fever, contained by an efficient immune response (6–8), 15% of the patients go on to develop severe disease requiring intensive care and oxygen support and 5% develop critical disease with life-threatening pneumonia, acute respiratory distress syndrome (ARDS) and septic shock often culminating in multi-organ dysfunction and death (9).
Age, various comorbidities, including diabetes, obesity, lung and cardiovascular diseases, as well as genetic polymorphisms correlate with a higher risk of respiratory failure (10–13).
SARS-CoV-2, similar to SARS-CoV (14), enters host cells via the angiotensin-converting enzyme 2 (ACE2) receptor and uses the human protease TMPRSS2 as entry activator (15, 16). These genes are expressed in a wide range of cells, including nasal and bronchial epithelial cells, enterocytes, cardiomyocytes, vascular and testicular cells, placental trophoblasts, bile duct cells (17, 18) as well as macrophages (19, 20). Furthermore, additional entry molecules, such as Neuropilin (NRP1), have been discussed to facilitate viral cell entry (21, 22).
Although acute respiratory manifestations are the most common feature, COVID-19 can have multiple acute extra-pulmonary clinical effects likely to be related to vascular pathology (23), and also long-lasting complications referred to as the post-COVID syndrome or long COVID, including fatigue or neurological sequelae (24–27).
Control of viral infections and resolution of inflammation generally depends on dose and route of infection, viral virulence properties as well as host immune factors (28, 29). Tightly regulated interactions between epithelial cells and immune cells, orchestrated by cytokine signaling and direct cellular contacts, play a critical role, also in COVID-19 (30, 31). Moreover, viral clearance does not necessarily mean recovery to a healthy state. Hyperactivated and dysregulated immune cells pose a substantial danger for exacerbated tissue damage (32–34) and alter susceptibility to secondary bacterial superinfection (35, 36).
Severe COVID-19 has been associated with pronounced changes in peripheral immune activity (37, 38), including increased levels of acute phase reactants and pro-inflammatory cytokines (39, 40), neutrophilia and emergence of immature and low-density neutrophils (41, 42), increased neutrophil-to-lymphocyte ratio and lymphopenia (43) as well as myeloid inflammation (44) and reduced expression of the human leukocyte antigen DR isotype (HLA-DR) by circulating monocytes (42, 45).
A time-dependent, multi-stage disease model for COVID-19 has been proposed (28). Early and efficient activation of the immune system through induction of a potent interferon response is crucial for controlling the virus. However, a delayed and/or prolonged interferon response may lead to progressive tissue damage, which may ultimately result in a deleterious hyperinflammation characterized by excessive activation of mononuclear phagocytes (MNPs) and coagulation in combination with dysregulation of tissue repair mechanisms and fibrosis (46).
Together with dendritic cells (DC), macrophages and monocytes form the MNP system (47). In addition to being professional antigen-presenting cells (APC), MNPs sense and phagocytose pathogens, mediate leukocyte recruitment, initiate and shape immune responses and regulate inflammation.
Macrophages are a heterogeneous family of tissue-resident, phagocytic innate immune cells, including brain microglia, liver Kupffer cells and lung alveolar and interstitial macrophages, that play an important role in tissue homeostasis and immune defense (48). In case of infection, macrophages sense danger signals from microbial pathogens or tissue damage via a plethora of pattern recognition receptors (PRRs), and respond by release of inflammatory molecules that eliminate pathogens, initiate inflammation and recruitment of additional effector cells and promote tissue repair (32). However, as is the case for example in macrophage activation syndrome (MAS), an overwhelming macrophage response can be detrimental to the host (33).
Monocytes are blood-circulating, phagocytic innate immune cells classically divided into three subsets based on their respective expression of CD14 and CD16 [classical (CD14+CD16−), non-classical (CD14dimCD16+), and intermediate (CD14+CD16+)] (48, 49). Under pathological conditions, including viral infections, monocytes, activated and recruited by inflammatory mediators, infiltrate affected tissues and acquire inflammatory macrophage and DC-like phenotypes to fulfil their effector functions of pro- and anti-inflammatory activities, antigen-presentation and tissue remodeling (50).
Here, we outline major findings concerning the role of monocytes and macrophages in COVID-19 and put them into the context of general knowledge of these cells in viral infections.
Alveolar and Interstitial Macrophage Ontogeny and Function
Every day, the lung inhales thousands of liters of air containing high amounts of pathogens including viruses, bacteria, and fungi (51). To prevent infection and its resulting complications for the organism, a tight control by the immune system is needed. In the lung, macrophages are the most abundant immune cell type under homeostatic conditions. Based on their exact location, they can be separated in at least two different populations; the interstitial macrophages (IMs) and alveolar macrophages (AMs) (52, 53).
IMs reside in the parenchyma between the microvascular endothelium and alveolar epithelium, while AMs have close contact to epithelial cells of alveoli and reside in the airspace lumen. However, a recent study by Neupane et al. showed that AMs are, in contrast to macrophages in other tissues, not sessile but can crawl in and between alveoli using the pores of Kohn (54). By expression of integrins, CD11cnegCD11bpos IMs can be distinguished from CD11cposCD11bneg AMs (52).
In addition to mucus and the epithelial barrier, AMs are the first defenders against pathogens entering the respiratory system. They originate from the yolk sac and populate the lung early after birth (55, 56). AMs have proliferative capacity, thus can persist over the lifespan by self-renewal and are independent of replacement from the bone marrow (57–59). AMs detected in bronchoalveolar lavage fluid (BALF) after lung transplantation were almost exclusively donor derived (60). Following depletion of lung macrophages in mice, repopulation occurred almost entirely by in situ proliferation (61). In contrast, analysis of pulmonary MNPs in patients receiving bone marrow transplantation for hematologic disorders provided evidence for replenishment of AMs by monocytes of bone marrow origin (62). The current understanding of the plastic composition and complex ontogeny of pulmonary MNPs is best described by a dynamic interplay of cells derived from yolk sac macrophages, fetal liver, and adult monocytes given pathologic threats and vacant niches (63).
The functional phenotype of AMs strongly depends on the local microenvironment and can change with contact with epithelial cells, oxygen tension and surfactant-rich fluid, highlighting the relevance of AM plasticity (64, 65). Therefore, AMs can be pro-/anti-inflammatory, pro-/anti-fibrotic, pro-asthmatic, pro-resolving and/or tissue-reparative. In the physiological state, AMs are critical for homeostasis by removing apoptotic cells, foreign materials, and surfactant, thereby ensuring that the lungs remain free of debris. Of note, they typically show an immunosuppressive phenotype (52). The anti-inflammatory program is critical to prevent unwanted inflammation in the lung that can be of serious danger for the organism. Although AMs have antigen presenting capacities and express HLA-DR, they promote tolerance and suppress lymphocyte activation under homeostatic conditions by producing immunosuppressive prostaglandins and TGFβ, of which the latter together with retinoic acid may drive the development of FOXP3+ regulatory T cells (Treg), further strengthening the anti-inflammation (66–68). By signaling through various receptors, such as by CD200R (69), SIRPα (70), mannose receptor CD206 (71), MACRO (72), TREM2 (73), and soluble mediators including Interleukin (IL)-10 (74), TGFβ (75) and PPARγ (76) AMs experience negative regulation. For instance, CD200 is expressed on the luminal side of respiratory epithelial cells and binding to CD200R on AMs leads to the suppression of pro-inflammatory genes in AMs (69).
Upon lung injury or infection, AMs can mount inflammatory responses (77). Destruction of airway epithelium can lead to a loss of exposure to regulatory ligands, such as CD200, resulting in a switch to a pro-inflammatory program in AMs (69). Recognition of pathogen associated molecular patterns (PAMP) of invading pathogens by AMs via PRRs further enhances this activation. These activated AMs are characterized by enhanced phagocytic capacity, higher oxidative burst and increased release of pro-inflammatory cytokines and chemokines, which results in inflammation and recruitment of other immune effector cells to the lung, including neutrophils (78). Recruited cells also include monocytes, which can differentiate into macrophage and DC-like cells, thus often referred to as monocyte-derived AMs (Mo-AMs) and DC (Mo-DC), upon arrival in peripheral tissues and can further enhance inflammation (79, 80). Their different ontogeny and functionality can influence the outcome of infection and inflammation.
Importantly, prolonged, and dysregulated inflammation caused by macrophages and monocytes can cause collateral tissue damage (81). To prevent prolonged inflammation and to limit tissue damage and fibrosis, AMs have evolved several strategies. These include phagocytosis of dying cells, e.g. neutrophils (82) preventing the release of their pro-inflammatory and toxic contents and triggering the secretion of TGFβ, IL-10, prostaglandin E2 and platelet-activating factor from AMs (83).
Respiratory pathologies such as asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis and idiopathic pulmonary fibrosis (IPF) are characterized by defective AM phagocytosis resulting in continuous inflammation (84–87).
Besides respiratory pathologies, cigarette smoking also presents a major risk factor for impaired AM function. AMs of smokers are expanded in numbers compared to non-smoking controls but show less phagocytic activity, glucose oxidation rate and cytokine production compared to non-smoking controls, which increases the risk of severe disease progression upon bacterial and viral infection (88–91).
After a successful inflammation, suppressive stimuli as described above are restored and AMs shift to an anti-inflammatory, tissue reparative phenotype restoring the homeostasis of the lung (65).
The Role of Lung Macrophages in Viral Respiratory Infections
As described above, the lung is at permanent risk of infection by several pathogens, amongst them viruses such as rhinovirus, respiratory syncytial virus, influenza virus and coronavirus. Despite their obvious relevance, investigation of human lung MNPs during respiratory infections has been limited so far and most of our knowledge comes from animal models. For instance, Schneider et al. showed that AM-depleted WT mice infected with influenza A virus had impaired gas exchange and fatal hypoxia (92). Similar results were obtained in pigs which, after AM depletion by dichloromethlyene diphosphonate, were infected with seasonal human H1N1 influenza virus resulting in 40% mortality rate and increased suffering from severe respiratory signs, whereas infected control pigs showed less severe symptoms with no mortality (93).
Notably, various viruses, including Influenza, Chikungunya, human herpes and Zika virus, have been shown to utilize monocytes and macrophages as vessels for virus replication, dissemination, or long-term persistence within tissues. They enter the cells through endocytosis, phagocytosis, macropinocytosis or membrane fusion and induce elevated expression of proinflammatory signaling and antiviral molecules (94–99). Direct infection of macrophages with SARS-CoV has also been shown, which, however, did not lead to dissemination or virus amplification but rather to an impaired type I interferon (IFN) response potentially worsening disease outcome (100).
Upon viral infection, AMs produce high levels of cellular mediators, including IL-1β, CCL3, CCL7 and CCL2, also known as monocyte chemotactic protein 1 (MCP1), which rapidly recruits CCR2-expressing bone marrow-derived monocytes into the lung. Furthermore, AMs are the main producers of type I IFN to trigger an antiviral response in influenza infection (101, 102). Of note, type I IFN production by AMs was higher than by plasmacytoid DCs (pDCs), coined as the natural “IFN producing cells”, in response to virus, indicating that pDCs may play a subordinate role in the defense against viral infections in the lung (102). Moreover, alveolar epithelial cells also did not produce any type I IFN in response to influenza, further stressing the key role of AMs (103). Type I IFNs can signal autocrine and paracrine resulting in the activation of antiviral transcriptional programs including the transcription of ISG such as ISG15, IFIT1 and STAT2, which can suppress viral replication (104, 105). Interestingly, not all virus infections trigger an increased type I IFN response. For instance, when human AMs were infected with coronavirus strain 229E (HCoV-299E), they secreted increased amounts of TNF, CCL5 and CCL4 (MIP-1β), causing inflammation, but IFN-β levels remained unchanged (106).
Viral infection triggers the migration of circulating monocytes to the lung guided by pro-inflammatory cytokines, such as CCL2 and CCL3, increasing the number of defending mononuclear phagocytes and enhancing inflammation (79). This is a necessary defense response, since viruses such as influenza can either reduce the numbers of resident AMs dramatically or impair their phenotype. When BALB/c mice were infected with influenza, 90% of resident AMs were lost in the first week after infection (107). This, however, was strain specific, since C57B1/6 mice did not show loss of AMs but rather an impaired phenotype. Nevertheless, both consequences were driven by IFN-γ and resulted in increased susceptibility to bacterial superinfections leading to significant body weight loss and mortality. Furthermore, a recent study by Neupane et al. showed that crawling of AMs, which is critical for AM function, was impaired after influenza infection. Again, this impairment was mediated by the IFN-γ pathway and resulted in increased risk for bacterial superinfections (54).
The Role of Monocytes and Alveolar Macrophages in COVID-19
The Involvement of Monocytes and Macrophages in SARS-CoV-2 Induced Hyperinflammation
COVID-19 is characterized by a systemic increase of numerous cytokines, including IL-1α, IL-1β, IL-6, IL-7, tumor necrosis factor (TNF), type I and II IFN, and the inflammatory chemokines CCL2, CCL3 and CXCL10 (40, 108, 109). Elevated levels of CCL2 and CCL7, two chemokines potent at the recruitment of CCR2+ monocytes, have also been found in BALF from patients with severe COVID-19 (110).
The term “cytokine storm”, historically described as an influenza-like syndrome that occurred after systemic infections and immunotherapies (111), has quickly become widely used, both in scientific publications and the media, to describe the cytokine response in COVID-19 (39). Although the increased systemic cytokine response in COVID-19 is undisputed, the term “cytokine storm” in COVID-19 pathophysiology is a topic of debate, as TNF, IL-6, and IL-8 concentrations in COVID-19 are less strong compared to sepsis, acute respiratory distress syndrome unrelated to COVID-19, trauma, cardiac arrest, and cytokine release syndrome (CRS) (112–115). Moreover, COVID-19 immune responses are highly dynamic as shown by time-dependent alterations of the systemic levels of many cytokines including IL-6 (40). Considering the co-occurrence of distinct systemic pro-inflammatory cytokine waves with the emergence of aberrant and immunosuppressive innate immune cells further complicates the exact terminology of immunopathology in severe COVID-19 and suggests a much more complex host-pathogen interaction better described by the term viral sepsis (28). In any case, the systemic cytokine profile observed in patients suffering from severe COVID-19 does resemble those observed in CRS, such as macrophage activation syndrome (MAS), which led early on to the working hypothesis that dysregulated activation of the MNP compartment contributes to COVID-19-associated hyperinflammation (33, 113).
The induction of cytokine production in MNPs in COVID-19 can either be triggered via recognition of damage-associated molecular patterns (DAMPS) released from epithelial cells affected by SARS-CoV-2 by PRRs or by direct recognition of viral pathogen-associated molecular patterns (PAMPs) via specific Toll-like receptors, i.e. TLR2 and TLR4, the retinoic acid-inducible gene I (RIG-I) or the melanoma differentiation associated gene (MDA)-5 (116–119). Furthermore, C-type lectin receptors, including DC-SIGN, L-SIGN, LSECtin, ASGR1, CLEC4K (Langerin) and CLEC10A (MGL), as well as Tweety family member 2 have been identified to interact with the SARS-CoV-2 spike protein inducing proinflammatory responses, but not allowing direct infection. Notably, however, these interactions were shown to promote virus transfer to ACE+ cells (120, 121).
SARS-CoV-2 infection of lung-resident MNPs might result either from phagocytosis of infected alveolar epithelial cells followed by viral escape from the lysosome or by direct infection. In vitro experiments with human monocyte-derived DC and macrophages with SARS-CoV-2 have demonstrated that both cell types are permissive to SARS-CoV-2 as measured by quantification of SARS-CoV-2 nucleocapsid protein expression after in vitro infection, but did not support productive viral replication. Interestingly, expression of proinflammatory cytokines and chemokines however was only triggered in macrophages and not DC under these experimental conditions (122). Additional independent infection experiments confirmed the abortive SARS-CoV-2 infection in human monocyte-derived DC and macrophages in vitro and corroborated the induction of antiviral and proinflammatory cytokines, including IFN-α/β, TNF, IL-1β, -6, and -10, as well as CXCL10, leading to type I IFN–mediated host cell death (123). Accordingly, investigation of cell tropism and immune activation profiles of SARS-CoV-2 in ex vivo organ cultures of human lung tissues revealed infection of type I and II pneumocytes as well as AMs (124), confirmed by detection of SARS-CoV-2 in AMs in autopsy samples from COVID-19 patients (125). Interestingly, analysis of murine AMs derived from human (h)ACE2 transgenic animals revealed different susceptibility to SARS-CoV-2 infection depending on their cytokine-induced polarization as in vitro treatment with IFN-γ and LPS caused increased infection rates compared to pre-treatment with IL-4 (126). Furthermore, in vitro treatment of PMA-differentiated THP-1 human macrophages and isolated CD14+ monocytes with SARS-CoV-2 spike protein after LPS stimulation exposed a hyperresponsiveness to TLR signals by suppression of IRAK-M (127). Moreover, antibody-dependent mechanisms of infection present a conceivable alternative pathway and have been described for SARS-CoV (128, 129). Besides this body of evidence demonstrating the induction of inflammatory pathways in monocytes and macrophages upon recognition of SARS-CoV-2, metabolic alterations in these cells have been reported. Ex vivo infected human monocytes shifted their metabolism and became highly glycolytic leading to elevated glucose levels promoting SARS-CoV-2 replication and cytokine production (130). Moreover, monocytes derived from COVID-19 patients were shown to have increased lipid droplet accumulation, which was explained by the modulation of lipid synthesis and uptake investigated using in vitro infection models and again favored virus replication and inflammatory mediator production (131). Interestingly, the pharmacological inhibition of DGAT1, a key enzyme in lipid droplet formation, inhibited SARS-CoV-2 replication and production of pro-inflammatory mediators presenting a new opportunity for therapeutic intervention.
Corresponding to the systemic increase of cytokine and chemokine levels, quantitative and qualitative changes in immune cell populations, particularly in the myeloid compartment, have been observed in blood and lungs of patients with COVID-19 dependent on disease severity.
Flow cytometric analyses of peripheral blood reported reduced percentages of total monocytes in the blood of severe COVID-19 cases (38, 132, 133). Notably, this reduction was observed only transiently in a longitudinal study of immune cells in severe cases pointing to the highly time-sensitive immune response (134).
Beyond quantitative changes, striking disease-specific differences in monocyte phenotypes in the blood and monocyte–macrophage composition in the lung have been consistently reported. A significant expansion of CD14+CD16+ monocytes featuring high expression of IL-6 in the blood discriminated patients with COVID-19 admitted to ICUs from those who did not require intensive care (132). Moreover, significantly reduced numbers of non-classical and intermediate monocytes are found in acute patients with symptoms of severe SARS-CoV-2 infection (135) and circulating classical monocytes show clear signs of activation, including increased expression of CD169 (135). In addition, experimentally infected monocytes and those from patients with severe COVID-19 requiring intensive care feature inflammasome activation and increased pyroptosis associated with caspase-1 activation (136). Furthermore, increased proliferation of monocytes derived from patients with severe COVID-19 after in vitro challenge with lipopolysaccharide was discussed as an indicator for a release of immature myeloid cells from the bone marrow reminiscent of emergency myelopoiesis (137) and contributing to innate immune dysfunction (138). Most prominently and consistent across all studies, reduced HLA-DR expression on monocytes – a well-established marker of immune suppression – was reported in patients suffering from severe COVID-19 (41, 42, 134, 139, 140). Decreased HLA-DR expression appeared to be strongly associated with COVID-19 disease severity, exemplified by lower expression of HLA-DR by monocytes in patients admitted to the ICU versus non-ICU patients (140) and in non-survivors versus survivors (141). Furthermore, the presence of HLA-DRlo monocytes in severe cases of COVID-19 was found to be positively correlated with levels of the soluble immunosuppressive factors IL-10, TGF-β, VEGFA, and AREG (142). In addition, reduced HLA-DR and CD86 expression together with elevated levels of IL-1β, IL-6, IL-8, IL-10, IL-17 and IFN-γ were observed in children with multisystem inflammatory syndrome (MIS-C) associated with SARS-CoV-2 infection (143). Downregulation of HLA-DR is a molecular feature often described for monocytic myeloid-derived suppressor cells (MDSC) – a cellular state of monocytes described to develop during chronic inflammation, especially late-stage cancers, and defined by T cell immunosuppressive functions (144). Functional assessment of HLA-DR- monocytes derived from COVID-19 patients indeed confirmed their capacity to suppress T cell proliferation, partly via ARG-1, and thus supports the MDSC state beyond phenotypic description (145). Interestingly, the HLA-DR- monocytes specific for severe acute COVID-19 have furthermore been found to express CPT1, an enzyme essential for fatty acid oxidation, again highlighting the relevance of immunometabolic effects of SARS-CoV-2 infection (146).
High-Resolution Single-Cell Omics Characterization of Monocytes and Macrophages in the Blood and Lungs of COVID-19 Patients
Application of high-resolution omics technologies with single-cell resolution, which were only developed and became widely applied within the last decade, has confirmed their great potential to rapidly decipher the immune response to an emerging pathogen during the COVID-19 pandemic. The first transcriptomic immune atlas of circulating peripheral blood mononuclear cells (PBMC) from 10 COVID-19 patients demonstrated globally decreased lymphocyte counts, while inflammatory myeloid cells were found to be more abundant (147). By now, at least 16 other studies have used scRNA-seq to characterize the immune response to SARS-CoV-2 (31, 41, 42, 45, 108, 148–158). While initial studies were based on low sample numbers limiting their explanatory power, latest reports comprised samples derived from more than 100 individuals, included longitudinal samples or profiled matched samples from multiple tissues. Single-cell transcriptomic analysis of PBMC in 7 hospitalized COVID-19 patients revealed a depletion of CD16+ monocytes in peripheral blood and the induction of an ISG signature in CD14+ monocytes, but detected no substantial induction of pro-inflammatory cytokine genes, such as TNF, IL6, IL1β, CCL3, CCL4 or CXCL2 in these cells, suggesting that peripheral monocytes are no major contributors to the cytokine response in COVID-19 (155). The lack of expression of inflammatory cytokines in innate immune cells in the periphery of COVID-19 patients was confirmed by multiplex plasma cytokine analysis, mass cytometry, and scRNA-seq in a cohort of 76 COVID-19 patients and 69 healthy individuals from two cohorts. Despite significantly upregulated levels of inflammatory molecules in the plasma of COVID-19 patients and transiently induced expression of ISGs in peripheral immune cells, an impaired cytokine response in blood myeloid cells and pDCs, with markedly reduced expression of IL-6, TNF and IL-1β upon TLR stimulation, was observed emphasizing a tissue origin of the plasma cytokines (108). Interestingly, the lack of ISG-expressing cells associated with mild disease was linked to severe disease-specific production of antibodies suppressing cellular interferon responses (159). In a dual-center, two-cohort study, we combined scRNA-seq and single-cell proteomics of whole-blood and PBMC and determined changes in the immune cell composition and activation in mild versus severe COVID-19 over time. While non-classical monocyte numbers were diminished in COVID-19, HLA-DRhiCD11chi inflammatory monocytes with an ISG signature were elevated in mild COVID-19 and monocytes in severe COVID-19 featured strongly reduced HLA-DR expression, high expression levels of genes with anti-inflammatory and immature properties, including SELL (CD62L), CD163, MPO and PLAC8, as well as increased expression of S100A family members, e.g. S100A12 (42). Loss of non-classical monocytes, reduced HLA-DR expression in monocytes and massive release of S100A family members was observed in severe cases of COVID-19 in multiple additional studies (41, 151, 156, 157), albeit disease stratification into mild, moderate, severe and critical disease showed slight differences. In addition, calprotectin (S100A8/S100A9) plasma levels and decreased frequencies of non-classical monocytes were found to discriminate patients who develop a severe form of COVID-19 (41).
Although the analysis of blood was extremely instructive particularly when assessing systemic effects of COVID-19, the lung presents the primary site of infection for SARS-CoV-2 and investigating the local immune system response is key to understanding the pathology. Activated monocytes of the blood have been shown to infiltrate the lungs in patients with COVID-19 and in animal models of SARS-CoV-2 infection (160, 161). In their seminal study, Liao et al. characterized BALF from patients with varying severity of COVID-19 and healthy individuals using scRNA-seq and reported striking shifts in cellular composition with increased proportions of macrophages and neutrophils and lower proportions of DCs and T cells in samples from severe/critical COVID-19 compared to those from moderate disease and healthy individuals. Within the MNP compartment, they observed a depletion of tissue-resident AMs and a replacement by inflammatory monocyte-derived macrophages in patients with severe disease. Notably, cytokine and chemokine expression levels differed dependent on disease severity. While CXCL9, CXCL10 and CXCL11 expression levels were increased both in moderate and severe disease compared to healthy levels, IL1β, IL6, TNF as well as CCL2, CCL3, CCL4 and CCL7 were expressed at higher levels in lung macrophages from patients with severe COVID-19. CXCL16, which interacts with the chemokine receptor CXCR6 and attracts subsets of T cells, was specifically induced in patients with moderate disease. These distinct expression profiles suggest that lung macrophages in patients with severe COVID-19 may promote tissue infiltration of inflammatory monocytes enhancing local inflammation, whereas macrophages in patients with moderate COVID-19 preferentially attract T cells. Furthermore, macrophage subpopulations specific for severe disease presented with immunoregulatory features but also expression of the profibrotic genes TREM2, TGFB2, and SPP1 (45). In agreement with this study, scRNA-seq data of nasopharyngeal and bronchial samples from 19 COVID-19 patients revealed the presence of inflammatory non-tissue resident and monocyte-derived macrophages expressing various cytokines, including IL1, TNF, CCL2 and CCL3, as well as enhanced interactions between epithelial and immune cells as determined by ligand–receptor expression profiling, in critical compared to moderate disease (31). Interestingly, comparing macrophages from the lower to the upper airways demonstrated increased expression of inflammatory cytokines and chemokines in the bronchia. Furthermore, monocyte-to-macrophage trajectory analysis in scRNA-seq of BALF samples from COVID-19 patients exposed enrichment of chronic hyperinflammatory monocytes in critical COVID-19 presenting with elevated expression levels of inflammasome-related genes (NLRP3, IL1-β, IL10RA) and genes associated with fibrosis (FGL2, TGFB1, COTL1) potentially contributing to tissue damage in severe COVID-19 (154). Single-nucleus (sn)RNA-seq on lung autopsies from 19 COVID-19 decedents confirmed the lungs to be highly inflamed with dense infiltration of aberrantly activated monocyte-derived macrophages and alveolar macrophages in the tissue (153). Another cross-sectional scRNA-seq of 780,000 PBMC sampled from 130 patients collected across three medical centers in the UK revealed the presence of a non-classical monocyte population characterized by the expression of complement transcripts C1QA/B/C in COVID-19. The complement system is a key host-defense mechanism with capacity to exacerbate tissue injury through its proinflammatory effects. Notably, integration of these PBMC transcriptomes with data derived from BALF samples (45) followed by partition-based graph abstraction (PAGA) analysis demonstrated transcriptional similarity between the circulating C1QA/B/C+CD16+ monocytes and alveolar macrophages in COVID-19 emphasizing the altered composition of the lung MNP compartment (150). The consistent reports of aberrant CD163hi and HLA-DRlo monocyte populations expressing the chemokine receptor CCR2 in the blood and hyperactivated airway monocytes and macrophages producing pro-inflammatory chemokines, including CCL2 and CCL3, were furthermore confirmed by high-dimensional phenotypic, transcriptomic, and functional profiling of immune cells from paired airway and blood samples obtained longitudinally from patients with severe COVID-19 (149).
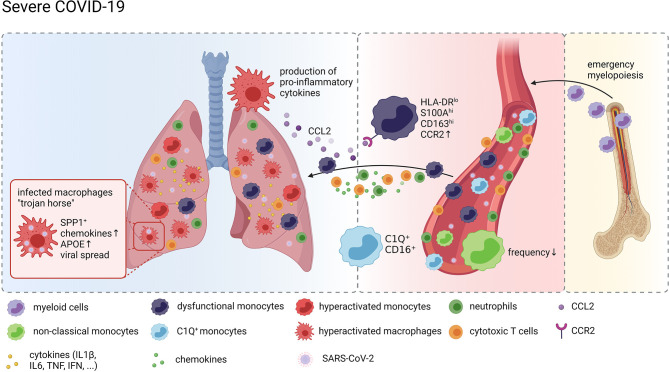
Taken together, these data strongly suggest a model of a vicious cycle of pro-inflammatory cytokine release by hyperactivated lung MNPs resulting in erratic infiltration of pro-inflammatory effector cells, including dysregulated monocytes and cytotoxic T cells, which in turn exacerbates tissue damage and fuels macrophage activation ( Figure 1 ).
Figure 1.
Monocytes and Macrophages in COVID-19. Graphical overview of the compositional and molecular alterations in monocyte and alveolar macrophage populations in COVID-19 created with BioRender.com. Distinct monocyte and macrophage phenotypes were identified in the peripheral blood of patients with severe COVID-19 including immature cells indicating emergency myelopoiesis, dysfunctional HLA-DRlo classical monocytes and complement gene expressing non-classical monocytes. These cells are attracted to the lung by pro-inflammatory chemokines resulting in a continuous accumulation of hyperactivated MNPs producing more pro-inflammatory mediators recruiting more inflammatory cells, including cytotoxic T cells and neutrophils, thus further exacerbating inflammation and tissue damage. SARS-CoV-2 infected macrophages in the lung may act as trojan horses propagating SARS-CoV-2 infection and spreading hyperinflammation across the lung.
Detection of SARS-CoV-2 RNA in Single-Cell RNA Profiles of Monocytes and Macrophages
Since SARS-CoV-2 exploits the host cell transcriptional machinery to express viral genes, viral transcripts can be detected alongside human mRNA transcripts in scRNA-seq data, thereby allowing for identification of infected cells and their unique properties at single-cell resolution. Bost et al. developed a new computational pipeline, called Viral-Track, to quantify viral RNA in single-cell transcriptomic data. Application of their approach to scRNA-seq data of BALF from the aforementioned study by Liao et al. revealed the presence of viral reads in samples derived from patients with severe, but not mild disease, suggestive of a differential viral load in the lung (162). The highest levels of viral RNA were observed in ciliated and epithelial progenitor cells. However, viral RNA was also detected in a subset of macrophages characterized by expression of SPP1. Whether these transcripts resulted from direct infection of and viral replication within the myeloid cells or whether the cells phagocytosed cellular material carrying viral RNA could not be clarified by this approach. However, the results of the single-cell specific viral RNA quantification allowed for differential gene expression in infected vs bystander SPP1+ macrophages, which revealed increased expression of chemokines (CCL7, CCL8, and CCL18) and APOE in virus-positive cells. The approach was further advanced by Wauters et al. who stratified SARS-CoV-2 infected cells in scRNA-seq data from BALF samples derived from patients with mild and critical COVID-19 by the presence of viral transcripts from distinct viral open reading frames (ORF). Detection of spike protein (S) specific transcripts in epithelial cells and consequentially reduced expression of ISGs suggests that S+ epithelial cells have actively been infected. In contrast, transcripts of the nucleocapsid protein (N) and the ORF10 and ORF1a were detected in myeloid and lymphoid cells at much higher levels than in epithelial cells. Comparing N+ vs N- alveolar and monocyte-derived macrophages determined genes involved in MHC class-II expression and ISG to be upregulated in response to the virus. Grant et al. followed an alternative approach to answer whether SARS-CoV-2 productively infects myeloid cells. Adding the negative-strand SARS-CoV-2 transcripts, which are transiently formed during viral replication, to the reference genome during alignment and quantification of their single-cell and bulk BALF transcriptome data allowed for evaluation of replicating SARS-CoV-2 in AMs. Besides the expected detection of positive and negative strand transcripts in epithelial cells, viral reads were also detected in subsets of macrophages suggesting that AMs harbor SARS-CoV-2 and allow viral replication in vivo (158), challenging the results on abortive infection gained from in vitro experiments. Interestingly, immunostaining of post-mortem tissue from patients who had died from COVID-19 revealed the presence of SARS-CoV-2 nucleoprotein in and the expression of ACE2 on populations of CD169+ macrophages in lymph nodes and the spleen (20). Given the increasing body of evidence in support of active infection of and the indication of productive viral replication in AMs by SARS-CoV-2, Grant et al. have come up with the hypothesis that AMs may act as a Trojan horse, transferring the virus to adjacent lung regions, thereby slowly propagating SARS-CoV-2 infection and spreading hyperinflammation across the lung ( Figure 1 ).
Outlook and Open Questions
After more than a year into the pandemic, it is rather clear that the innate immune system and in particular monocytes and macrophages are linked to the heterogeneity of the COVID-19 disease courses. For example, HLA-DRhi monocytes are typically seen in mild cases, while HLA-DRlo S100+ cells dominate in severe COVID-19. Future work needs to untangle which molecular mechanisms are responsible for these different cellular responses. For example, are certain signals from the microenvironment normally increasing the induction of HLA-DR molecules missing in patients with severe disease course? Are elevated levels of inhibitory factors such as certain prostaglandins or TGFβ responsible for the molecular phenotype of MNPs in severe COVID-19. Furthermore, is there a direct link between fibrotic lung disease as a result of severe COVID-19 with ARDS and changes in the MNP compartment or other immune cells like NK cells. And if this is the case, are the anti-fibrotic molecular programs of monocytes and macrophages not working or do these cells suddenly gain pro-fibrotic functionality. Are molecular changes seen in these cells early during the disease predictive for disease courses leading to irreversible tissue damage as it is proposed for some patients with Long COVID-19? Even if the pandemic will be under control due to world-wide vaccination programs and other medical measures, the sequelae of Long COVID-19 and its potential burden on long-term health requires further studies into the role of the immune system, in particular the innate immune system with monocytes, macrophages and granulocytes requiring special attention.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Funding
The work of JS was supported by the German Research Foundation (DFG) under Germany’s Excellence Strategy (EXC2151–390873048), the EU project SYSCID (grant number 733100), the BMBF-funded grant iTREAT (01ZX1902B), ERA CVD (grant number 00160389), and the BMBF-funded excellence project Diet–Body–Brain (DietBB) (grant number 01EA1809A).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
AMs, alveolar macrophages; APC, antigen-presenting cells; COPD, chronic obstructive pulmonary disease; COVID-19, Coronavirus disease 2019; DC, dendritic cells; IL, intereukin; IFN, interferon; IPF, idiopathic pulmonary fibrosis; ISG, interferon-stimulated genes; MNPs, mononuclear phagocytes; Mo-AMs, monocyte-derived AMs; Mo-DC, monocyte-derived DC; ORF, open reading frames; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; scRNA-seq, single-cell RNA-sequencing; snRNA-seq, single-nucleus RNA-sequencing.
References
- 1. Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med (2020) 383:2451–60. 10.1056/NEJMcp2009575 [DOI] [PubMed] [Google Scholar]
- 2. Gandhi RT, Lynch JB, del Rio C. Mild or Moderate Covid-19. N Engl J Med (2020) 383:1757–66. 10.1056/NEJMcp2009249 [DOI] [PubMed] [Google Scholar]
- 3. Kim D, Lee JY, Yang JS, Kim JW, Kim VN, Chang H. The Architecture of SARS-CoV-2 Transcriptome. Cell (2020) 181:914–21.e10. 10.1016/j.cell.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A New Coronavirus Associated With Human Respiratory Disease in China. Nature (2020) 579:265–9. 10.1038/s41586-020-2008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang YZ. Holmes EC. A Genomic Perspective on the Origin and Emergence of SARS-CoV-2. Cell (2020) 181:223–7. 10.1016/j.cell.2020.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, China. Lancet (2020) 395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thevarajan I, Nguyen THO, Koutsakos M, Druce J, Caly L, van de Sandt CE, et al. Breadth of Concomitant Immune Responses Prior to Patient Recovery: A Case Report of Non-Severe COVID-19. Nat Med (2020) 26:453–5. 10.1038/s41591-020-0819-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med (2020) 382:1708–20. 10.1056/nejmoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical Characteristics of Coronavirus Disease 2019 (COVID-19) in China: A Systematic Review and Meta-Analysis. J Infect (2020) 80:656–65. 10.1016/j.jinf.2020.03.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang Q, Liu Z, Moncada-Velez M, Chen J, Ogishi M, Bigio B, et al. Inborn Errors of Type I IFN Immunity in Patients With Life-Threatening COVID-19. Science (2020) 370:eabd4570. 10.1126/science.abd4570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beck DB, Aksentijevich I. Susceptibility to Severe COVID-19. Science (2020) 370:404–5. 10.1126/science.abe7591 [DOI] [PubMed] [Google Scholar]
- 12. Pairo-Castineira E, Clohisey S, Klaric L, Bretherick AD, Rawlik K, Pasko D, et al. Genetic Mechanisms of Critical Illness in COVID-19. Nature (2021) 591:92–8. 10.1038/s41586-020-03065-y [DOI] [PubMed] [Google Scholar]
- 13. Osuchowski MF, Winkler MS, Skirecki T, Cajander S, Shankar-Hari M, Lachmann G, et al. The COVID-19 Puzzle: Deciphering Pathophysiology and Phenotypes of a New Disease Entity. Lancet Respir Med (2021) 9(6):622–42. 10.1016/s2213-2600(21)00218-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Drosten C, Günther S, Preiser W, van der Werf S, Brodt H-R, Becker S, et al. Identification of a Novel Coronavirus in Patients With Severe Acute Respiratory Syndrome. N Engl J Med (2003) 348:1967–76. 10.1056/nejmoa030747 [DOI] [PubMed] [Google Scholar]
- 15. Shang J, Wan Y, Luo C, Ye G, Geng Q, Auerbach A, et al. Cell Entry Mechanisms of SARS-CoV-2. Proc Natl Acad Sci USA (2020) 117:11727–34. 10.1073/pnas.2003138117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell (2020) 181:271–80.e8. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C. The Protein Expression Profile of ACE2 in Human Tissues. Mol Syst Biol (2020) 16:e9610. 10.15252/msb.20209610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 Entry Factors are Highly Expressed in Nasal Epithelial Cells Together With Innate Immune Genes. Nat Med (2020) 26:681–7. 10.1038/s41591-020-0868-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Song X, Hu W, Yu H, Zhao L, Zhao Y, Zhao X, et al. Little to No Expression of Angiotensin-Converting Enzyme-2 on Most Human Peripheral Blood Immune Cells But Highly Expressed on Tissue Macrophages. Cytom Part A (2020) 2020:1–10. 10.1002/cyto.a.24285 [DOI] [PubMed] [Google Scholar]
- 20. Xiang Q, Feng Z, Diao B, Tu C, Qiao Q, Yang H, et al. SARS-CoV-2 Induces Lymphocytopenia by Promoting Inflammation and Decimates Secondary Lymphoid Organs. Front Immunol (2021) 12:661052. 10.3389/fimmu.2021.661052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Daly JL, Simonetti B, Klein K, Chen KE, Williamson MK, Antón-Plágaro C, et al. Neuropilin-1 Is a Host Factor for SARS-CoV-2 Infection. Science (2020) 370:861–5. 10.1126/science.abd3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, et al. Neuropilin-1 Facilitates SARS-CoV-2 Cell Entry and Infectivity. Science (2020) 370:856–60. 10.1126/science.abd2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary Manifestations of COVID-19. Nat Med (2020) 26:1017–32. 10.1038/s41591-020-0968-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fraser E. Long Term Respiratory Complications of Covid-19. BMJ (2020) 370:m3001. 10.1136/bmj.m3001 [DOI] [PubMed] [Google Scholar]
- 25. Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med (2020) 382:2268–70. 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19. JAMA - J Am Med Assoc (2020) 324:603–5. 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-Acute COVID-19 Syndrome. Nat Med (2021) 27:601–15. 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schultze JL, Aschenbrenner AC. COVID-19 and the Human Innate Immune System. Cell (2021) 184:1671–92. 10.1016/j.cell.2021.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rouse BT, Sehrawat S. Immunity and Immunopathology to Viruses: What Decides the Outcome? Nat Rev Immunol (2010) 10:514–26. 10.1038/nri2802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Branchett WJ, Lloyd CM. Regulatory Cytokine Function in the Respiratory Tract. Mucosal Immunol (2019) 12:589–600. 10.1038/s41385-019-0158-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chua RL, Lukassen S, Trump S, Hennig BP, Wendisch D, Pott F, et al. COVID-19 Severity Correlates With Airway Epithelium–Immune Cell Interactions Identified by Single-Cell Analysis. Nat Biotechnol (2020) 38:970–9. 10.1038/s41587-020-0602-4 [DOI] [PubMed] [Google Scholar]
- 32. Merad M, Martin JC. Pathological Inflammation in Patients With COVID-19: A Key Role for Monocytes and Macrophages. Nat Rev Immunol (2020) 20:355–62. 10.1038/s41577-020-0331-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schulert GS, Grom AA. Pathogenesis of Macrophage Activation Syndrome and Potential for Cytokine-Directed Therapies. Annu Rev Med (2015) 66:145–59. 10.1146/annurev-med-061813-012806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Karki R, Sharma BR, Tuladhar S, Williams EP, Zalduondo L, Samir P, et al. Synergism of TNF-α and IFN-γ Triggers Inflammatory Cell Death, Tissue Damage, and Mortality in SARS-CoV-2 Infection and Cytokine Shock Syndromes. Cell (2021) 184:149–68.e17. 10.1016/j.cell.2020.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Goulding J, Godlee A, Vekaria S, Hilty M, Snelgrove R, Hussell T. Lowering the Threshold of Lung Innate Immune Cell Activation Alters Susceptibility to Secondary Bacterial Superinfection. J Infect Dis (2011) 204:1086–94. 10.1093/infdis/jir467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Oliver BGG, Lim S, Wark P, Laza-Stanca V, King N, Black JL, et al. Rhinovirus Exposure Impairs Immune Responses to Bacterial Products in Human Alveolar Macrophages. Thorax (2008) 63:519–25. 10.1136/thx.2007.081752 [DOI] [PubMed] [Google Scholar]
- 37. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and Immunological Features of Severe and Moderate Coronavirus Disease 2019. J Clin Invest (2020) 130:2620–9. 10.1172/JCI137244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis (2020) 71:762–8. 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression. Lancet (2020) 395:1033–4. 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lucas C, Wong P, Klein J, Castro TBR, Silva J, Sundaram M, et al. Longitudinal Analyses Reveal Immunological Misfiring in Severe COVID-19. Nature (2020) 584:463–9. 10.1038/s41586-020-2588-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Silvin A, Chapuis N, Dunsmore G, Goubet AG, Dubuisson A, Derosa L, et al. Elevated Calprotectin and Abnormal Myeloid Cell Subsets Discriminate Severe From Mild COVID-19. Cell (2020) 182:1401–18.e18. 10.1016/j.cell.2020.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schulte-Schrepping J, Reusch N, Paclik D, Baßler K, Schlickeiser S, Zhang B, et al. Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment. Cell (2020) 182:1419–40.e23. 10.1016/j.cell.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cao X. COVID-19: Immunopathology and its Implications for Therapy. Nat Rev Immunol (2020) 20:269–70. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Aschenbrenner AC, Mouktaroudi M, Krämer B, Oestreich M, Antonakos N, Nuesch-Germano M, et al. Disease Severity-Specific Neutrophil Signatures in Blood Transcriptomes Stratify COVID-19 Patients. Genome Med (2021) 13:7. 10.1186/s13073-020-00823-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, et al. Single-Cell Landscape of Bronchoalveolar Immune Cells in Patients With COVID-19. Nat Med (2020) 26:842–4. 10.1038/s41591-020-0901-9 [DOI] [PubMed] [Google Scholar]
- 46. Siddiqi HK, Mehra MR. COVID-19 Illness in Native and Immunosuppressed States: A Clinical–Therapeutic Staging Proposal. J Hear Lung Transplant (2020) 39:405–7. 10.1016/j.healun.2020.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. van Furth R, Cohn ZA. The Origin and Kinetics of Mononuclear Phagocytes. J Exp Med (1968) 128:415–35. 10.1084/JEM.128.3.415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bassler K, Schulte-Schrepping J, Warnat-Herresthal S, Aschenbrenner AC, Schultze JL. The Myeloid Cell Compartment-Cell by Cell. Annu Rev Immunol (2019) 37:269–93. 10.1146/annurev-immunol-042718-041728 [DOI] [PubMed] [Google Scholar]
- 49. Kapellos TS, Bonaguro L, Gemünd I, Reusch N, Saglam A, Hinkley ER, et al. Human Monocyte Subsets and Phenotypes in Major Chronic Inflammatory Diseases. Front Immunol (2019) 10:2035. 10.3389/fimmu.2019.02035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Guilliams M, Mildner A, Yona S. Developmental and Functional Heterogeneity of Monocytes. Immunity (2018) 49:595–613. 10.1016/j.immuni.2018.10.005 [DOI] [PubMed] [Google Scholar]
- 51. Prussin AJ, Garcia EB, Marr LC. Total Concentrations of Virus and Bacteria in Indoor and Outdoor Air. Environ Sci Technol Lett (2015) 2:84–8. 10.1021/acs.estlett.5b00050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hussell T, Bell TJ. Alveolar Macrophages: Plasticity in a Tissue-Specific Context. Nat Rev Immunol (2014) 14:81–93. 10.1038/nri3600 [DOI] [PubMed] [Google Scholar]
- 53. Franke-Ullmann G, Pförtner C, Walter P, Steinmüller C, Lohmann-Matthes ML, Kobzik L. Characterization of Murine Lung Interstitial Macrophages in Comparison With Alveolar Macrophages In Vitro. J Immunol (1996) 157:3097–104. [PubMed] [Google Scholar]
- 54. Neupane AS, Willson M, Chojnacki AK, Vargas E Silva Castanheira F, Morehouse C, Carestia A, et al. Patrolling Alveolar Macrophages Conceal Bacteria From the Immune System to Maintain Homeostasis. Cell (2020) 183:110–25.e11. 10.1016/j.cell.2020.08.020 [DOI] [PubMed] [Google Scholar]
- 55. Schulz C, Perdiguero EG, Chorro L, Szabo-Rogers H, Cagnard N, Kierdorf K, et al. A Lineage of Myeloid Cells Independent of Myb and Hematopoietic Stem Cells. Science (2012) 335:86–90. 10.1126/science.1219179 [DOI] [PubMed] [Google Scholar]
- 56. Guilliams M, De Kleer I, Henri S, Post S, Vanhoutte L, De Prijck S, et al. Alveolar Macrophages Develop From Fetal Monocytes That Differentiate Into Long-Lived Cells in the First Week of Life. via GM-CSF. J Exp Med (2013) 210:1977–92. 10.1084/jem.20131199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Tarling JD, Lin HS, Hsu S. Self-Renewal of Pulmonary Alveolar Macrophages: Evidence From Radiation Chimera Studies. J Leukoc Biol (1987) 42:443–6. 10.1002/jlb.42.5.443 [DOI] [PubMed] [Google Scholar]
- 58. Sawyer RT, Strausbauch PH, Volkman A. Resident Macrophage Proliferation in Mice Depleted of Blood Monocytes by Strontium-89. Lab Investig (1982) 46:165–70. [PubMed] [Google Scholar]
- 59. Golde DW, Byers LA, Finley TN. Proliferative Capacity of Human Alveolar Macrophage. Nature (1974) 247:373–5. 10.1038/247373a0 [DOI] [PubMed] [Google Scholar]
- 60. Eguíluz-Gracia I, Schultz HHL, Sikkeland LIB, Danilova E, Holm AM, Pronk CJH, et al. Long-Term Persistence of Human Donor Alveolar Macrophages in Lung Transplant Recipients. Thorax (2016) 71:1006–11. 10.1136/thoraxjnl-2016-208292 [DOI] [PubMed] [Google Scholar]
- 61. Hashimoto D, Chow A, Noizat C, Teo P, Beasley MB, Leboeuf M, et al. Tissue-Resident Macrophages Self-Maintain Locally Throughout Adult Life With Minimal Contribution From Circulating Monocytes. Immunity (2013) 38:792–804. 10.1016/j.immuni.2013.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Thomas ED, Ramberg RE, Sale GE, Sparkes RS, Golde DW. Direct Evidence for a Bone Marrow Origin of the Alveolar Macrophage in Man. Science (1976) 192:1016–8. 10.1126/science.775638 [DOI] [PubMed] [Google Scholar]
- 63. Guilliams M, van de Laar L. A Hitchhiker’s Guide to Myeloid Cell Subsets: Practical Implementation of a Novel Mononuclear Phagocyte Classification System. Front Immunol (2015) 6:406. 10.3389/fimmu.2015.00406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Joshi N, Walter JM, Misharin AV. Alveolar Macrophages. Cell Immunol (2018) 330:86–90. 10.1016/j.cellimm.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 65. Watanabe S, Alexander M, Misharin AV, Budinger GRS. The Role of Macrophages in the Resolution of Inflammation. J Clin Invest (2019) 129:2619–28. 10.1172/JCI124615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Coleman MM, Ruane D, Moran B, Dunne PJ, Keane J, Mills KHG. Alveolar Macrophages Contribute to Respiratory Tolerance by Inducing FoxP3 Expression in Naive T Cells. Am J Respir Cell Mol Biol (2013) 48:773–80. 10.1165/rcmb.2012-0263OC [DOI] [PubMed] [Google Scholar]
- 67. Soroosh P, Doherty TA, Duan W, Mehta AK, Choi H, Adams YF, et al. Lung-Resident Tissue Macrophages Generate Foxp3+ Regulatory T Cells and Promote Airway Tolerance. J Exp Med (2013) 210:775–88. 10.1084/jem.20121849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lipscomb MF, Lyons CR, Nunez G, Ball EJ, Stastny P, Vial W, et al. Human Alveolar Macrophages: HLA-DR-Positive Macrophages That are Poor Stimulators of a Primary Mixed Leukocyte Reaction. J Immunol (1986) 136(2):497–504. [PubMed] [Google Scholar]
- 69. Snelgrove RJ, Goulding J, Didierlaurent AM, Lyonga D, Vekaria S, Edwards L, et al. A Critical Function for CD200 in Lung Immune Homeostasis and the Severity of Influenza Infection. Nat Immunol (2008) 9:1074–83. 10.1038/ni.1637 [DOI] [PubMed] [Google Scholar]
- 70. Janssen WJ, McPhillips KA, Dickinson MG, Linderman DJ, Morimoto K, Xiao YQ, et al. Surfactant Proteins A and D Suppress Alveolar Macrophage Phagocytosis via Interaction With Sirpα. Am J Respir Crit Care Med (2008) 178:158–67. 10.1164/rccm.200711-1661OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Zhang J, Tachado SD, Patel N, Zhu J, Imrich A, Manfruelli P, et al. Negative Regulatory Role of Mannose Receptors on Human Alveolar Macrophage Proinflammatory Cytokine Release In Vitro . J Leukoc Biol (2005) 78:665–74. 10.1189/jlb.1204699 [DOI] [PubMed] [Google Scholar]
- 72. Ghosh S, Gregory D, Smith A, Kobzik L. MARCO Regulates Early Inflammatory Responses Against Influenza: A Useful Macrophage Function With Adverse Outcome. Am J Respir Cell Mol Biol (2011) 45:1036–44. 10.1165/rcmb.2010-0349OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gao X, Dong Y, Liu Z, Niu B. Silencing of Triggering Receptor Expressed on Myeloid Cells-2 Enhances the Inflammatory Responses of Alveolar Macrophages to Lipopolysaccharide. Mol Med Rep (2013) 7:921–6. 10.3892/mmr.2013.1268 [DOI] [PubMed] [Google Scholar]
- 74. Fernandez S, Jose P, Avdiushko MG, Kaplan AM, Cohen DA. Inhibition of IL-10 Receptor Function in Alveolar Macrophages by Toll-Like Receptor Agonists. J Immunol (2004) 172:2613–20. 10.4049/jimmunol.172.4.2613 [DOI] [PubMed] [Google Scholar]
- 75. Morris DG, Huang X, Kaminski N, Wang Y, Shapiro SD, Dolganov G, et al. Loss of Integrin αvβ6-Mediated TGF-β Activation Causes Mmp 12-Dependent Emphysema. Nature (2003) 422:169–73. 10.1038/nature01413 [DOI] [PubMed] [Google Scholar]
- 76. Gautier EL, Chow A, Spanbroek R, Marcelin G, Greter M, Jakubzick C, et al. Systemic Analysis of Pparγ in Mouse Macrophage Populations Reveals Marked Diversity in Expression With Critical Roles in Resolution of Inflammation and Airway Immunity. J Immunol (2012) 189:2614–24. 10.4049/jimmunol.1200495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lambrecht BN. Alveolar Macrophage in the Driver’s Seat. Immunity (2006) 24:366–8. 10.1016/j.immuni.2006.03.008 [DOI] [PubMed] [Google Scholar]
- 78. Steinmüller C, Franke-Ullmann G, Lohmann-Matthes ML, Emmendörffer A. Local Activation of Nonspecific Defense Against a Respiratory Model Infection by Application of Interferon-γ: Comparison Between Rat Alveolar and Interstitial Lung Macrophages. Am J Respir Cell Mol Biol (2000) 22:481–90. 10.1165/ajrcmb.22.4.3336 [DOI] [PubMed] [Google Scholar]
- 79. Trapnell BC, Whitsett JA. GM-CSF Regulates Pulmonary Surfactant Homeostasis and Alveolar Macrophage-Mediated Innate Host Defense. Annu Rev Physiol (2002) 64:775–802. 10.1146/annurev.physiol.64.090601.113847 [DOI] [PubMed] [Google Scholar]
- 80. Baharom F, Rankin G, Blomberg A, Smed-Sörensen A. Human Lung Mononuclear Phagocytes in Health and Disease. Front Immunol (2017) 8:499. 10.3389/fimmu.2017.00499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Laskin DL, Sunil VR, Gardner CR, Laskin JD. Macrophages and Tissue Injury: Agents of Defense or Destruction? Annu Rev Pharmacol Toxicol (2011) 51:267–88. 10.1146/annurev.pharmtox.010909.105812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ortega-Gómez A, Perretti M, Soehnlein O. Resolution of Inflammation: An Integrated View. EMBO Mol Med (2013) 5:661–74. 10.1002/emmm.201202382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Fadok VA, Bratton DL, Konowal A, Freed PW, Westcott JY, Henson PM. Macrophages That Have Ingested Apoptotic Cells In Vitro Inhibit Proinflammatory Cytokine Production Through Autocrine/Paracrine Mechanisms Involving TGF-β, PGE2, and PAF. J Clin Invest (1998) 101:890–8. 10.1172/JCI1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Fitzpatrick AM, Holguin F, Teague WG, Brown LAS. Alveolar Macrophage Phagocytosis is Impaired in Children With Poorly Controlled Asthma. J Allergy Clin Immunol (2008) 121(6):1372–8. 10.1016/j.jaci.2008.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Hodge S, Hodge G, Scicchitano R, Reynolds PN, Holmes M. Alveolar Macrophages From Subjects With Chronic Obstructive Pulmonary Disease are Deficient in Their Ability to Phagocytose Apoptotic Airway Epithelial Cells. Immunol Cell Biol (2003) 81:289–96. 10.1046/j.1440-1711.2003.t01-1-01170.x [DOI] [PubMed] [Google Scholar]
- 86. Vandivier RW, Richens TR, Horstmann SA, DeCathelineau AM, Ghosh M, Reynolds SD, et al. Dysfunctional Cystic Fibrosis Transmembrane Conductance Regulator Inhibits Phagocytosis of Apoptotic Cells With Proinflammatory Consequences. Am J Physiol - Lung Cell Mol Physiol (2009) 297(4):L677–86. 10.1152/ajplung.00030.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Morimoto K, Janssen WJ, Terada M. Defective Efferocytosis by Alveolar Macrophages in IPF Patients. Respir Med (2012) 106:1800–3. 10.1016/j.rmed.2012.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Aoshiba K, Tamaoki J, Nagai A. Acute Cigarette Smoke Exposure Induces Apoptosis of Alveolar Macrophages. Am J Physiol - Lung Cell Mol Physiol (2001) 281(6):L1392–401. 10.1152/ajplung.2001.281.6.l1392 [DOI] [PubMed] [Google Scholar]
- 89. Gleeson LE, O’Leary SM, Ryan D, McLaughlin AM, Sheedy FJ, Keane J. Cigarette Smoking Impairs the Bioenergetic Immune Response to Mycobacterium Tuberculosis Infection. Am J Respir Cell Mol Biol (2018) 59:572–9. 10.1165/rcmb.2018-0162OC [DOI] [PubMed] [Google Scholar]
- 90. Sussan TE, Gajghate S, Thimmulappa RK, Ma J, Kim JH, Sudini K, et al. Exposure to Electronic Cigarettes Impairs Pulmonary Anti-Bacterial and Anti-Viral Defenses in a Mouse Model. PloS One (2015) 10:e0116861. 10.1371/journal.pone.0116861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wallace WAH, Gillooly M, Lamb D. Intra-Alveolar Macrophage Numbers in Current Smokers and non-Smokers: A Morphometric Study of Tissue Sections. Thorax (1992) 47:437–40. 10.1136/thx.47.6.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Schneider C, Nobs SP, Heer AK, Kurrer M, Klinke G, van Rooijen N, et al. Alveolar Macrophages Are Essential for Protection From Respiratory Failure and Associated Morbidity Following Influenza Virus Infection. PloS Pathog (2014) 10:e1004053. 10.1371/journal.ppat.1004053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Kim HM, Lee Y-W, Lee K-J, Kim HS, Cho SW, van Rooijen N, et al. Alveolar Macrophages Are Indispensable for Controlling Influenza Viruses in Lungs of Pigs. J Virol (2008) 82:4265–74. 10.1128/jvi.02602-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Yilla M, Harcourt BH, Hickman CJ, McGrew M, Tamin A, Goldsmith CS, et al. SARS-Coronavirus Replication in Human Peripheral Monocytes/Macrophages. Virus Res (2005) 107:93–101. 10.1016/j.virusres.2004.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Smith MS, Bentz GL, Alexander JS, Yurochko AD. Human Cytomegalovirus Induces Monocyte Differentiation and Migration as a Strategy for Dissemination and Persistence. J Virol (2004) 78:4444–53. 10.1128/jvi.78.9.4444-4453.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Nottet HS, Persidsky Y, Sasseville VG, Nukuna AN, Bock P, Zhai QH, et al. Mechanisms for the Transendothelial Migration of HIV-1-Infected Monocytes Into Brain. J Immunol (1996) 156:1284–95. [PubMed] [Google Scholar]
- 97. Desforges M, Miletti TC, Gagnon M, Talbot PJ. Activation of Human Monocytes After Infection by Human Coronavirus 229E. Virus Res (2007) 130:228–40. 10.1016/j.virusres.2007.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Al-Qahtani AA, Lyroni K, Aznaourova M, Tseliou M, Al-Anazi MR, Al-Ahdal MN, et al. Middle East Respiratory Syndrome Corona Virus Spike Glycoprotein Suppresses Macrophage Responses via DPP4-Mediated Induction of IRAK-M and Pparγ. Oncotarget (2017) 8:9053–66. 10.18632/oncotarget.14754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Nikitina E, Larionova I, Choinzonov E, Kzhyshkowska J. Monocytes and Macrophages as Viral Targets and Reservoirs. Int J Mol Sci (2018) 19:2821. 10.3390/ijms19092821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Cheung CY, Poon LLM, Ng IHY, Luk W, Sia S-F, Wu MHS, et al. Cytokine Responses in Severe Acute Respiratory Syndrome Coronavirus-Infected Macrophages In Vitro: Possible Relevance to Pathogenesis. J Virol (2005) 79:7819–26. 10.1128/jvi.79.12.7819-7826.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Wang J, Nikrad MP, Travanty EA, Zhou B, Phang T, Gao B, et al. Innate Immune Response of Human Alveolar Macrophages During Influenza a Infection. PloS One (2012) 7:e29879. 10.1371/journal.pone.0029879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Kumagai Y, Takeuchi O, Kato H, Kumar H, Matsui K, Morii E, et al. Alveolar Macrophages Are the Primary Interferon-α Producer in Pulmonary Infection With RNA Viruses. Immunity (2007) 27:240–52. 10.1016/j.immuni.2007.07.013 [DOI] [PubMed] [Google Scholar]
- 103. Wang J, Nikrad MP, Phang T, Gao B, Alford T, Ito Y, et al. Innate Immune Response to Influenza A Virus in Differentiated Human Alveolar Type II Cells. Am J Respir Cell Mol Biol (2011) 45:582–91. 10.1165/rcmb.2010-0108OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Wong MT, Chen SSL. Emerging Roles of Interferon-Stimulated Genes in the Innate Immune Response to Hepatitis C Virus Infection. Cell Mol Immunol (2016) 13:11–35. 10.1038/cmi.2014.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Hambleton S, Goodbourn S, Young DF, Dickinson P, Mohamad SMB, Valappil M, et al. STAT2 Deficiency and Susceptibility to Viral Illness in Humans. Proc Natl Acad Sci USA (2013) 110:3053–8. 10.1073/pnas.1220098110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Joel Funk C, Wang J, Ito Y, Travanty EA, Voelker DR, Holmes KV, et al. Infection of Human Alveolar Macrophages by Human Coronavirus Strain 229E. J Gen Virol (2012) 93:494–503. 10.1099/vir.0.038414-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Califano D, Furuya Y, Metzger DW. Effects of Influenza on Alveolar Macrophage Viability Are Dependent on Mouse Genetic Strain. J Immunol (2018) 201:134–44. 10.4049/jimmunol.1701406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Arunachalam PS, Wimmers F, Mok CKP, Perera RAPM, Scott M, Hagan T, et al. Systems Biological Assessment of Immunity to Mild Versus Severe COVID-19 Infection in Humans. Science (2020) 369:1210–20. 10.1126/SCIENCE.ABC6261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, et al. Impaired Type I Interferon Activity and Inflammatory Responses in Severe COVID-19 Patients. Science (2020) 369:718–24. 10.1126/science.abc6027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Zhou Z, Ren L, Zhang L, Zhong J, Xiao Y, Jia Z, et al. Heightened Innate Immune Responses in the Respiratory Tract of COVID-19 Patients. Cell Host Microbe (2020) 27:883–90.e2. 10.1016/j.chom.2020.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med (2020) 383:2255–73. 10.1056/nejmra2026131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Kox M, Waalders NJB, Kooistra EJ, Gerretsen J, Pickkers P. Cytokine Levels in Critically Ill Patients With COVID-19 and Other Conditions. JAMA - J Am Med Assoc (2020) 324:1565–7. 10.1001/jama.2020.17052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Monneret G, Benlyamani I, Gossez M, Bermejo-Martin JF, Martín-Fernandez M, Sesques P, et al. COVID-19: What Type of Cytokine Storm Are We Dealing With? J Med Virol (2021) 93:197–8. 10.1002/jmv.26317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sinha P, Matthay MA, Calfee CS. Is a “Cytokine Storm” Relevant to COVID-19? JAMA Intern Med (2020) 180:1152–4. 10.1001/jamainternmed.2020.3313 [DOI] [PubMed] [Google Scholar]
- 115. Leisman DE, Ronner L, Pinotti R, Taylor MD, Sinha P, Calfee CS, et al. Cytokine Elevation in Severe and Critical COVID-19: A Rapid Systematic Review, Meta-Analysis, and Comparison With Other Inflammatory Syndromes. Lancet Respir Med (2020) 8:1233–44. 10.1016/S2213-2600(20)30404-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Khanmohammadi S, Rezaei N. Role of Toll-Like Receptors in the Pathogenesis of COVID-19. J Med Virol (2021) 93:2735–9. 10.1002/jmv.26826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Yang D, Geng T, Harrison AG, Wang P. Differential Roles of RIG-I-Like Receptors in SARS-CoV-2 Infection. bioRxiv Prepr Serv Biol (2021). 10.1101/2021.02.10.430677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Zhao Y, Kuang M, Li J, Zhu L, Jia Z, Guo X, et al. SARS-CoV-2 Spike Protein Interacts With and Activates TLR4. Cell Res (2021) 31:818–20. 10.1038/s41422-021-00495-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Zheng M, Karki R, Williams EP, Yang D, Fitzpatrick E, Vogel P, et al. TLR2 Senses the SARS-CoV-2 Envelope Protein to Produce Inflammatory Cytokines. Nat Immunol (2021) 22:829–38. 10.1038/s41590-021-00937-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Thépaut M, Luczkowiak J, Vivès C, Labiod N, Bally I, Lasala F, et al. Dc/L-SIGN Recognition of Spike Glycoprotein Promotes SARS-CoV-2 Trans-Infection and can be Inhibited by a Glycomimetic Antagonist. PloS Pathog (2021) 17:e1009576. 10.1371/journal.ppat.1009576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Lu Q, Liu J, Zhao S, Gomez Castro MF, Laurent-Rolle M, Dong J, et al. SARS-CoV-2 Exacerbates Proinflammatory Responses in Myeloid Cells Through C-Type Lectin Receptors and Tweety Family Member 2. Immunity (2021) 54:1304–1319.e9. 10.1016/j.immuni.2021.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Yang D, Chu H, Hou Y, Chai Y, Shuai H, Lee ACY, et al. Attenuated Interferon and Proinflammatory Response in SARS-CoV-2-Infected Human Dendritic Cells is Associated With Viral Antagonism of STAT1 Phosphorylation. J Infect Dis (2020) 222:734–45. 10.1093/infdis/jiaa356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Zheng J, Wang Y, Li K, Meyerholz DK, Allamargot C, Perlman S. Severe Acute Respiratory Syndrome Coronavirus 2-Induced Immune Activation and Death of Monocyte-Derived Human Macrophages and Dendritic Cells. J Infect Dis (2021) 223:785–95. 10.1093/infdis/jiaa753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Chu H, Chan JFW, Wang Y, Yuen TTT, Chai Y, Hou Y, et al. Comparative Replication and Immune Activation Profiles of SARS-CoV-2 and SARS-CoV in Human Lungs: An Ex Vivo Study With Implications for the Pathogenesis of COVID-19. Clin Infect Dis (2020) 71:1400–9. 10.1093/cid/ciaa410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Martines RB, Ritter JM, Matkovic E, Gary J, Bollweg BC, Bullock H, et al. Pathology and Pathogenesis of SARS-CoV-2 Associated With Fatal Coronavirus Disease, United States. Emerg Infect Dis (2020) 26:2005–15. 10.3201/eid2609.202095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Lv J, Wang Z, Qu Y, Zhu H, Zhu Q, Tong W, et al. Distinct Uptake, Amplification, and Release of SARS-CoV-2 by M1 and M2 Alveolar Macrophages. Cell Discovery (2021) 7:24. 10.1038/s41421-021-00258-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Pantazi I, Al-Qahtani AA, Alhamlan FS, Alothaid H, Matou-Nasri S, Sourvinos G, et al. SARS-CoV-2/ACE2 Interaction Suppresses IRAK-M Expression and Promotes Pro-Inflammatory Cytokine Production in Macrophages. Front Immunol (2021) 12:683800. 10.3389/FIMMU.2021.683800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Liu L, Wei Q, Lin Q, Fang J, Wang H, Kwok H, et al. Anti-Spike IgG Causes Severe Acute Lung Injury by Skewing Macrophage Responses During Acute SARS-CoV Infection. JCI Insight (2019) 4:e123158. 10.1172/jci.insight.123158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Jaume M, Yip MS, Cheung CY, Leung HL, Li PH, Kien F, et al. Anti-Severe Acute Respiratory Syndrome Coronavirus Spike Antibodies Trigger Infection of Human Immune Cells via a pH- and Cysteine Protease-Independent Fc R Pathway. J Virol (2011) 85:10582–97. 10.1128/jvi.00671-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Codo AC, Davanzo GG, Monteiro L de B, de Souza GF, Muraro SP, Virgilio-da-Silva JV, et al. Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response Through a HIF-1α/Glycolysis-Dependent Axis. Cell Metab (2020) 32:437–46.e5. 10.1016/j.cmet.2020.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. da Silva Gomes Dias S, Soares VC, Ferreira AC, Sacramento CQ, Fintelman-Rodrigues N, Temerozo JR, et al. Lipid Droplets Fuel SARS-CoV-2 Replication and Production of Inflammatory Mediators. PloS Pathog (2020) 16:e1009127. 10.1371/journal.ppat.1009127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T-Cells and Inflammatory Monocytes Incite Inflammatory Storms in Severe COVID-19 Patients. Natl Sci Rev (2020) 7:998–1002. 10.1093/nsr/nwaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Laing AG, Lorenc A, del Molino del Barrio I, Das A, Fish M, Monin L, et al. A Dynamic COVID-19 Immune Signature Includes Associations With Poor Prognosis. Nat Med (2020) 26:1623–35. 10.1038/s41591-020-1038-6 [DOI] [PubMed] [Google Scholar]
- 134. Payen D, Cravat M, Maadadi H, Didelot C, Prosic L, Dupuis C, et al. A Longitudinal Study of Immune Cells in Severe COVID-19 Patients. Front Immunol (2020) 11:580250. 10.3389/fimmu.2020.580250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Gatti A, Radrizzani D, Viganò P, Mazzone A, Brando B. Decrease of Non-Classical and Intermediate Monocyte Subsets in Severe Acute SARS-CoV-2 Infection. Cytom Part A (2020) 97:887–90. 10.1002/cyto.a.24188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Ferreira AC, Soares VC, de Azevedo-Quintanilha IG, Dias S da SG, Fintelman-Rodrigues N, Sacramento CQ, et al. SARS-CoV-2 Engages Inflammasome and Pyroptosis in Human Primary Monocytes. Cell Death Discov (2021) 7:43. 10.1038/s41420-021-00428-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Schultze JL, Mass E, Schlitzer A. Emerging Principles in Myelopoiesis at Homeostasis and During Infection and Inflammation. Immunity (2019) 50:288–301. 10.1016/j.immuni.2019.01.019 [DOI] [PubMed] [Google Scholar]
- 138. Mann ER, Menon M, Knight SB, Konkel JE, Jagger C, Shaw TN, et al. Longitudinal Immune Profiling Reveals Key Myeloid Signatures Associated With COVID-19. Sci Immunol (2020) 5:eabd6197. 10.1126/SCIIMMUNOL.ABD6197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Giamarellos-Bourboulis EJ, Netea MG, Rovina N, Akinosoglou K, Antoniadou A, Antonakos N, et al. Complex Immune Dysregulation in COVID-19 Patients With Severe Respiratory Failure. Cell Host Microbe (2020) 27:992–1000.e3. 10.1016/j.chom.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Spinetti T, Hirzel C, Fux M, Walti LN, Schober P, Stueber F, et al. Reduced Monocytic Human Leukocyte Antigen-DR Expression Indicates Immunosuppression in Critically Ill COVID-19 Patients. Anesth Analg (2020) 131:993–9. 10.1213/ANE.0000000000005044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Wang F, Hou H, Yao Y, Wu S, Huang M, Ran X, et al. Systemically Comparing Host Immunity Between Survived and Deceased COVID-19 Patients. Cell Mol Immunol (2020) 17:875–7. 10.1038/s41423-020-0483-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Kvedaraite E, Hertwig L, Sinha I, Ponzetta A, Myrberg IH, Lourda M, et al. Major Alterations in the Mononuclear Phagocyte Landscape Associated With COVID-19 Severity. Proc Natl Acad Sci USA (2021) 118(6):e2018587118. 10.1073/pnas.2018587118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Carter MJ, Fish M, Jennings A, Doores KJ, Wellman P, Seow J, et al. Peripheral Immunophenotypes in Children With Multisystem Inflammatory Syndrome Associated With SARS-CoV-2 Infection. Nat Med (2020) 26:1701–7. 10.1038/s41591-020-1054-6 [DOI] [PubMed] [Google Scholar]
- 144. Hegde S, Leader AM, Merad M. MDSC: Markers, Development, States, and Unaddressed Complexity. Immunity (2021) 54:875–84. 10.1016/j.immuni.2021.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Falck-Jones S, Vangeti S, Yu M, Falck-Jones R, Cagigi A, Badolati I, et al. Functional Monocytic Myeloid-Derived Suppressor Cells Increase in Blood But Not Airways and Predict COVID-19 Severity. J Clin Invest (2021) 131(6):e144734. 10.1172/JCI144734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Thompson EA, Cascino K, Ordonez AA, Zhou W, Vaghasia A, Hamacher-Brady A, et al. Metabolic Programs Define Dysfunctional Immune Responses in Severe COVID-19 Patients. Cell Rep (2021) 34:108863. 10.1016/j.celrep.2021.108863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Wen W, Su W, Tang H, Le W, Zhang X, Zheng Y, et al. Immune Cell Profiling of COVID-19 Patients in the Recovery Stage by Single-Cell Sequencing. Cell Discov (2020) 6:6. 10.1038/s41421-020-0168-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Lee JS, Park S, Jeong HW, Ahn JY, Choi SJ, Lee H, et al. Immunophenotyping of Covid-19 and Influenza Highlights the Role of Type I Interferons in Development of Severe Covid-19. Sci Immunol (2020) 5:1554. 10.1126/sciimmunol.abd1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Szabo PA, Dogra P, Gray JI, Wells SB, Connors TJ, Weisberg SP, et al. Longitudinal Profiling of Respiratory and Systemic Immune Responses Reveals Myeloid Cell-Driven Lung Inflammation in Severe COVID-19. Immunity (2021) 54:797–814.e6. 10.1016/j.immuni.2021.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Stephenson E, Reynolds G, Botting RA, Calero-Nieto FJ, Morgan MD, Tuong ZK, et al. Single-Cell Multi-Omics Analysis of the Immune Response in COVID-19. Nat Med (2021) 27:904–16. 10.1038/s41591-021-01329-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Su Y, Chen D, Yuan D, Lausted C, Choi J, Dai CL, et al. Multi-Omics Resolves a Sharp Disease-State Shift Between Mild and Moderate COVID-19. Cell (2020) 183:1479–95.e20. 10.1016/j.cell.2020.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Cao Y, Su B, Guo X, Sun W, Deng Y, Bao L, et al. Potent Neutralizing Antibodies Against SARS-CoV-2 Identified by High-Throughput Single-Cell Sequencing of Convalescent Patients’ B Cells. Cell (2020) 182:73–84.e16. 10.1016/j.cell.2020.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Melms JC, Biermann J, Huang H, Wang Y, Nair A, Tagore S, et al. A Molecular Single-Cell Lung Atlas of Lethal COVID-19. Nature (2021) 33:15. 10.1038/s41586-021-03569-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Wauters E, Van Mol P, Garg AD, Jansen S, Van Herck Y, Vanderbeke L, et al. Discriminating Mild From Critical COVID-19 by Innate and Adaptive Immune Single-Cell Profiling of Bronchoalveolar Lavages. Cell Res (2021) 31:272–90. 10.1038/s41422-020-00455-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Wilk AJ, Rustagi A, Zhao NQ, Roque J, Martínez-Colón GJ, McKechnie JL, et al. A Single-Cell Atlas of the Peripheral Immune Response in Patients With Severe COVID-19. Nat Med (2020) 26:1070–6. 10.1038/s41591-020-0944-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Bernardes JP, Mishra N, Tran F, Rosenstiel P. Longitudinal Multi-Omics Analyses Identify Responses of Megakaryocytes, Erythroid Cells, and Plasmablasts as Hallmarks of Severe COVID-19. Immunity (2020) 53:1296–314.e9. 10.1016/j.immuni.2020.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Zhang JY, Wang XM, Xing X, Xu Z, Zhang C, Song JW, et al. Single-Cell Landscape of Immunological Responses in Patients With COVID-19. Nat Immunol (2020) 21:1107–18. 10.1038/s41590-020-0762-x [DOI] [PubMed] [Google Scholar]
- 158. Grant RA, Morales-Nebreda L, Markov NS, Swaminathan S, Querrey M, Guzman ER, et al. Circuits Between Infected Macrophages and T Cells in SARS-CoV-2 Pneumonia. Nature (2021) 590:635–41. 10.1038/s41586-020-03148-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Combes AJ, Courau T, Kuhn NF, Hu KH, Ray A, Chen WS, et al. Global Absence and Targeting of Protective Immune States in Severe COVID-19. Nature (2021) 591:124–30. 10.1038/s41586-021-03234-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Nouailles G, Wyler E, Pennitz P, Postmus D, Kazmierski J, Pott F, et al. Longitudinal Omics in Syrian Hamsters Integrated With Human Data Unravel Complexity 1 of Moderate Immune Responses to SARS-CoV-2 2 3. bioRxiv (2020) 2020:12. 10.1101/2020.12.18.423524 [DOI] [Google Scholar]
- 161. Sánchez-Cerrillo I, Landete P, Aldave B, Sánchez-Alonso S, Sánchez-Azofra A, Marcos-Jiménez A, et al. COVID-19 Severity Associates With Pulmonary Redistribution of CD1c+ DCs and Inflammatory Transitional and Nonclassical Monocytes. J Clin Invest (2020) 130:6290–300. 10.1172/JCI140335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Bost P, Giladi A, Liu Y, Bendjelal Y, Xu G, David E, et al. Host-Viral Infection Maps Reveal Signatures of Severe COVID-19 Patients. Cell (2020) 181:1475–1488.e12. 10.1016/j.cell.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]