Abstract
Backgrounds
Non-suicidal self-injury is a serious health problem among patients with depression or bipolar disorder. However, few studies within the Chinese context have investigated the prevalence of NSSI and its risk factors in above populations. The purpose of this study was to investigate the prevalence of non-suicidal self-injury and its risk factors in patients with depression or bipolar disorder in China.
Methods
The final sample comprised of 394 inpatients(Mage = 29.71; SDage = 11.95) with depression or bipolar disorder from two psychiatric hospitals in Beijing, China. A General Demographic Data Form, the Non-suicidal Self-injury Questionnaire(NSSI-Q), Impulsivity Item and the Adverse Childhood Experiences-International Questionnaire(ACE-IQ) were completed by all patients.
Results
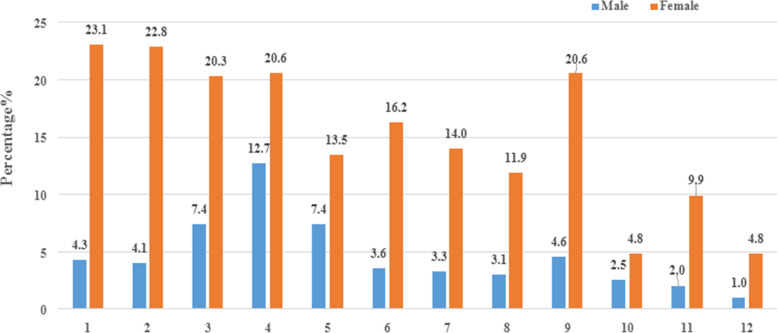
Of the 394 patients examined, 245(62.2%) of this sample reported NSSI in past year. Of the 245 patients with NSSI, 135(55.1%) were diagnosed with depression and 110(44.9%) were diagnosed with bipolar disorder. The most common methods of NSSI for female was “pinching”(23.1%) and “scratching”(22.8%), while for male it was “hiting hard objects”(12.7%). By multivariate regression analysis, young age, unemployment, a higher monthly family income, single, impulsivity, long duration of illness and ACEs were risk factors for NSSI in patients with depression and bipolar disorder(P<0.05).
Conclusions
Our study points to the fact that there was an unfortunate message about the prevalence of NSSI among patients with depression or bipolar disorder in China. It is necessary not only to raise the awareness of NSSI in families and society, but also to formulate targeted assessment and intervention. Moreover, future research should not only focus on individuals being hospitalized, but should be representative of individuals treated at home or in the community because there are no national statistics on NSSI among such patients in China.
Keywords: Non-suicidal self-injury, Prevalence, Risk factors, Depression, Bipolar disorder, China
Background
Non-suicidal self-injury(NSSI) is generally defined as “the direct, deliberate destruction of one’s own body tissue without the intention of suicidal intent” [1], including cutting or scratching the skin, burning/branding with cigarettes/lighters, scalding, striking oneself or other hard objects, banging limbs/head and hair pulling, et al. [2]. Based on previous studies, DSM-5 provided a more accurate definition of NSSI, that is, in the last year, an individual has been engaged in a behavior that intentionally causes bleeding, bruising, or pain on the body surface for 5 or more days, but only causes slight or moderate physical injury [3]. As one of the public health problems recognized globally, NSSI has provoked concern among health professionals, researchers, social workers and welfare workers, teachers, other professionals and affected families [4].
Estimated prevalence of NSSI vary widely as due to a number of factors including the time since last episode of NSSI, the number of NSSI episodes to be recognized, research tools, as well as different study areas and populations [5]. Benjet et al. found that the lifetime prevalence of NSSI was 18.56%, and the annual prevalence was 3.19% in a sample of 1071 Mexican residents of young adults [6]. In Canada, estimated prevalence range from as low as 7% [7] of student samples to as high as 77% [8] of clinical samples. As a coping strategy for maladaptive individuals [9], NSSI are more prone to be seen in clinical populations, especially in patients with depression or bipolar disorder who have poor abilities of emotional regulation and coping [10]. A recent study observed that about 37 and 52% of patients with depression and bipolar disorder had engaged in NSSI at least once, respectively [11]. Fang et al. found that 38.6% of Chinese patients with depression had committed NSSI in the past year [12]. Although there have been a few relevant studies in China, the evidence on the prevalence of NSSI is still sparse and heterogeneous due to the differences in sample sources and definitions of NSSI [13, 14]. It is necessary to carefully design studies to help better understand the epidemiology of NSSI in Chinese patients with depression or bipolar disorder.
NSSI leads to a variety of serious consequences, including physical injury [15], negative emotional experiences and a decline in learning ability, work efficiency [16], which prompted researchers to explore the risk factors relate to NSSI. A study proposed that young individuals were more prone to conduct NSSI [17]. However, the evidence on whether NSSI changes with age is insufficient. Moreover, there is contradictory evidence about whether there have a sex difference in NSSI with some studies reporting a higher prevalence among female [18] and others finding no sex difference [19]. Also, NSSI was uniquely associated with marital status, employment status, socio-economic status. Nevertheless, findings should be cited with caution [20]. Tschan et al. presented that the educational level of parents was relate to NSSI [21]. Besides, there may also be a link between impulsivity and NSSI [11], which may be more pronounced in individuals with depression or bipolar disorder than in the general population [22]. A new study revealed that cannabinoid use was connected with an increased prevalence of NSSI by elevating Δ9- THC/CBD balance [23], which makes us to think about the relationship between substance abuse experiences such as alcohol, cannabinoid and NSSI. To date, the existing literature is inconsistent with regard to whether the incidence of NSSI is related to adverse childhood experiences(ACEs). In earlier times, Glassman have failed to find a significant association between NSSI and ACEs [24]. However, new studies provided new clues. In a meta-analysis that included cross-sectional, longitudinal, and retrospective studies published in the same year, Serafini et al. observed that the increased vulnerability to NSSI seems to be related to ACEs [25].
Whereas studies from other countries have investigated the prevalence of NSSI and risk factors of NSSI [20, 25, 26], including the exploration of patients with depression or bipolar disorder [5, 11]. So far, few studies within the Chinese context have investigated the prevalence of NSSI and the risk factors for NSSI among patients with depression or bipolar disorder. Almost all of the few existing studies on NSSI in China are from the general population or relied on student samples where the characteristics are far from representative of patients with depression or bipolar disorder. The purpose of this study aimd to: 1) examine the prevalence of NSSI in patients with depression or bipolar disorder in China, and 2) determine the risk factors for NSSI.
Methods
Participants
The participants for this cross-sectional study consisted of patients who were hospitalized at one of the two Chinese biggest psychiatric hospitals in Beijing(Beijing Anding Hospital and Beijing HuiLongGuan Hospital), China, between September 2019 and May 2020. Inclusion criteria were: 1) The patients who were aged 18 to 60 years old were interviewed by two or more psychiatrists and met the diagnostic of depression or bipolar disorder according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10); 2) The patients were clinically stable(an increase in drug dosage not more than 50% in the 3 months before this investigation [27]); 3) The patients were able to read and write in simplified Chinese; 4) The patients were willing to join our study after providing informed consent. Exclusion criteria were the presence of any condition that may affect the ability to complete the questionnaire and the accuracy of the results, including accompanied by other mental illnesses, delirium, dementia, deafness, mental retardation or denial of informed consent.
Procedures
From September 2019 to May 2020, 412 adult patients were eligible for our study. Of these patients, 16 cases were excluded from the analysis because of the unwillingness to continue to participate in study. The final sample consisted of 394 patients, with a a response rate of 95.63%. Before entering our study, we explained the purpose, content and procedure of this study to the patients, and promised that the study results would only be used for academic research. Patients voluntarily decide whether to participate in the study or not. If they agree to participate, they will sign a written informed consent. Moreover, patients have the right to decide whether to continue during the study. The questionnaire information was collected face-to-face, one-on-one, by trained researchers in a quiet room in the ward after being given a verbal and written explanation of the study and having acquired informed consent. And the questionnaire was completed by themselves. If the respondents have questions about the questionnaire, the researchers can help them understand by informing them of the original intention of the question in a non-judgmental way. Additionally, the quality control procedures in the research process are also very important. Measures were taken for quality assurance, such as intensive researcher training, detailed field explanations, continuous feedback and independent supervision of supervisors and field researchers. The questionnaire was collected and checked whether there were any missing items by the researcher on the spot after completion. The study was performed according to the Declaration of Helsinki and approved by the Research Ethics Board of Peking Union Medical College (2019–18-K7).
Instruments
Demographic details
A General Demographic Data Form by self-designed was employed to collect basic information of each patient, including sex, age, marital status, employment status, monthly family income, residence, educational level of patients and their parent, left-behind experience, substance abuse experience, family type, family structure, and the clinical features of patients(details see Table 1).
Table 1.
Demographic characteristics, implusivity and ACEs between Groups (n = 394)
| (n, %) | Comparisons | ||||
|---|---|---|---|---|---|
| D-NSSI Group | BD-NSSI Group | Non-NSSI Group | χ2 | P-value | |
| Participants | 135(34.3) | 110(27.9) | 149(37.8) | ||
| Age (years) | 67.348 | < 0.001 | |||
| 18 ~ 30 | 110(81.5) | 80(72.7) | 55(36.9) | ||
| 31 ~ 45 | 17(12.6) | 21(19.1) | 61(40.9) | ||
| 46 ~ 60 | 8(5.9) | 9(8.2) | 33(22.2) | ||
| Sex | 0.559 | 0.756 | |||
| Male | 38(28.1) | 33(30.0) | 48(32.2) | ||
| Female | 97(71.9) | 77(70.0) | 101(67.8) | ||
| Education of patients | 1.586 | 0.811 | |||
| Junior school graduate and below | 18(13.3) | 18(16.4) | 17(11.4) | ||
| High school graduate | 29(21.5) | 21(19.1) | 34(22.8) | ||
| University and above | 88(65.2) | 71(64.5) | 98(65.8) | ||
| Employments status | 25.439 | < 0.001 | |||
| Employed | 40(29.6) | 55(50.0) | 88(59.1) | ||
| Unemployed | 95(70.4) | 55(50.0) | 61(40.9) | ||
| Marital status | 60.204 | < 0.001 | |||
| Single | 107(79.3) | 79(71.8) | 57(38.2) | ||
| Married | 22(16.3) | 23(20.9) | 80(53.7) | ||
| Divorced or widowed | 6(4.4) | 8(7.3) | 12(8.1) | ||
| Monthly family income (US dollar) | 11.212 | 0.024 | |||
| 400 ~ 700 | 31(23.0) | 33(30.0) | 55(36.9) | ||
| 700 ~ 1000 | 47(34.8) | 24(21.8) | 43(28.8) | ||
| > 1000 | 57(42.2) | 53(48.2) | 51(34.3) | ||
| Residence | 1.248 | 0.536 | |||
| Urban | 86(63.7) | 77(70.0) | 96(64.4) | ||
| Rural | 49(36.3) | 33(30.0) | 53(35.6) | ||
| Left-behind experience | 5.113 | 0.078 | |||
| Yes | 39(28.9) | 32(29.1) | 28(18.8) | ||
| No | 96(71.1) | 78(70.9) | 121(81.2) | ||
| Substance abuse experience | 8.638 | 0.013 | |||
| Yes | 27(20.0) | 30(27.3) | 19(12.8) | ||
| No | 108(80.0) | 80(72.7) | 130(87.2) | ||
| Family type | 0.754 | 0.945 | |||
| Nuclear family | 72(53.3) | 60(54.5) | 86(57.7) | ||
| Joint family | 25(18.5) | 18(16.4) | 24(16.1) | ||
| Single family | 38(28.2) | 32(29.1) | 39(26.2) | ||
| Family structure | 1.205 | 0.547 | |||
| Single child family | 68(50.4) | 60(54.5) | 71(47.7) | ||
| Multiple children family | 67(49.6) | 50(45.5) | 78(52.3) | ||
| Education of father | 6.071 | 0.194 | |||
| Junior school graduate and below | 64(47.4) | 44(40.0) | 73(49.0) | ||
| High school graduate | 21(15.6) | 20(18.2) | 33(2.2) | ||
| University and above | 50(37.0) | 46(41.8) | 43(28.8) | ||
| Education of mother | 5.688 | 0.224 | |||
| Junior school graduate and below | 61(45.2) | 45(40.9) | 82(55.0) | ||
| High school graduate | 30(22.2) | 28(25.5) | 28(18.8) | ||
| University and above | 44(32.6) | 37(33.6) | 39(26.2) | ||
| Duration of illness (years) | 63.705 | <0.001 | |||
| < 3 | 108(80.0) | 35(31.8) | 86(57.7) | ||
| 3 ~ 5 | 16(11.9) | 27(24.5) | 19(12.7) | ||
| 6 ~ 10 | 5(3.7) | 29(26.4) | 22(14.8) | ||
| > 10 | 6(4.4) | 19(12.3) | 22(14.8) | ||
| Times of recurrence | 26.002 | 0.001 | |||
| 0 | 45(33.4) | 15(13.6) | 42(28.2) | ||
| 1 ~ 3 | 64(47.4) | 48(43.7) | 62(41.6) | ||
| 4 ~ 5 | 13(9.6) | 20(18.2) | 26(17.5) | ||
| > 5 | 13(9.6) | 27(24.5) | 19(12.7) | ||
| Impulsivity | 12.206 | 0.002 | |||
| Yes | 41(30.4) | 43(39.1) | 29(19.5) | ||
| No | 94(69.6) | 67(60.9) | 120(80.5) | ||
| Adverse childhood experiences | 26.313 | <0.001 | |||
| Yes | 134(99.3) | 107(97.3) | 127(85.2) | ||
| No | 1(0.7) | 3(2.7) | 22(14.8) | ||
D-NSSI Group Depression-NSSI Group
BD-NSSI Group Bipolar Disorder-NSSI Group
Non-suicidal self-injury questionnaire(NSSI-q)
The Non-suicidal Self-injury Questionnaire was compiled by Wan et al. [28] in the investigation of nationwide large sample of NSSI. In 2018, Wan et al. [29] further developed the tool. There are 12 items in the questionnaire, which are divided into two dimensions: Items 1 to 7 involve NSSI without obvious tissue injury, which refers to that the NSSI carried out by individuals does not cause obvious and serious tissue damage; items 8 to 12 involve NSSI with obvious tissue injury, which refers to NSSI by individuals may result in bleeding, scratches and other tissue damage. Participants were asked to answer questions, “In the past year, have you ever engaged in the following behaviors to deliberately injure yourself but without suicidal intent?” The questionnaire investigated the occurrence of 12 categories of NSSI of the respondents in the past year, including pinching, scratching, hitting hard objects with head/fist, hitting themself with fists or hard objects, biting, pulling his/her hair, stabbing, cutting, scalding, etc. It is a 5-point Likert scale ranging from “never”(score 0) to “always”(score 4), with a total score of 0 ~ 48. A dichotomous variable of NSSI status was computed based on the 12 items. It was coded 0 when participants choosed “never” as the answer of all items, and was coded 1 when participants reported having engaged in one or more NSSI acts. NSSI-Q showed satisfactory reliability and validity as a self-report measure for NSSI [29]. In this study, the Cronbach’sαof the questionnaire was 0.82.
Impulsivity
Impulsivity was measured by the question: “Most of time in your life, no matter what the situation was, no matter who you were with, have you often done things impulsively?” Respondents who answered affirmatively were defined in this study as impulsive. For the assessment of impulsivity, it is derived from the borderline personality disorder assessment module using the NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV [30]. We cannot use test-retest reliability of individual items. However, the Cronbach’s alpha(0.77) for the borderline personality disorder assessment module was computed, indicating very good internal consistency of the section. After removing the impulsivity item, the value does not change, indicating that the item has high reliability [31]. Good convergent and divergent validity were previously embodied in this item [31].
Adverse childhood experiences-international questionnaire(ace-IQ)
ACEs were assessed using the Adverse Childhood Experiences International Questionnaire(ACE-IQ) developed by the World Health Organization [32], which covers 3 domains of childhood adversities, including childhood maltreatment, family/household dysfunction and violence outside the home. Collectively, these 3 domains on behalf of 13 categories of ACEs, which covers family dysfunction; physical, sexual and emotional abuse and neglect; peer violence; witnessing community violence, and exposure to collective violence. Each respondent was asked if they had experienced various adverse events during their childhood(prior to the age of 18). In this present study, the frequency scoring method was used to generate a conservative estimate of ACE exposure that closer to international standards. ACE scores were recorded as total counts for the number of questions to which respondents answered that they had experienced an ACE. The existence of any of the 13 categories of ACEs is considered to be the existence of ACEs. The ACE-IQ has good reliability and validity [33–36]. The Cronbach’sαof the questionnaire was 0.72 in this current study.
Statistical analysis
Descriptive statistics for all the variables were first conducted using percentages for the categorical variables. Mean, standard deviation, and range were computed for continuous variables. The prevalence of NSSI was examined and presented in terms of frequency and the proportion of those encountering it(%). Social-demographic characteristics, impulsivity and ACEs of participants between NSSI group(Depression-NSSI group/Bipolar Disorder-NSSI group) and Non-NSSI group were compared by using Chi-squared tests. After running Chi-squared tests for each putative risk factor between groups (Table 1), we included in the multivariable logistic regression models those factors that showed a statistically significant difference(P < 0.05). In addition, based on clinical experiences and literature review, it was found that the sex was closely related to the occurrence of NSSI [37]. Therefore, sex was included in logistic regression for further analysis. All the variables were entered in the model using the enter method. All statistical differences were considered significant when the P<0.05 for both directions. All statistical analyses were performed in SPSS for Windows, Version 23.0.
Results
The sample composed of 394 adult patients(Male = 119, Female = 275), with a mean age of 29.71 years(SD = 11.95). Male and female patients did not differ in age(29.81 ± 12.17 vs. 29.49 ± 11.46; t = − 0.25; P = 0.80). The response rate was 95.63%. Sixteen patients who were eligible for inclusion in this study declined to continue in the study. No patients returned incomplete or not analyzable questionnaires.
The demographics, clinical features, impulsivity and ACEs
The average age of 394 respondents (119 male, 275 female) were 29.71 years, and they were from north China(65.5%), northeast China(7.9%), etc., most of them were female(69.8%). The majority of the respondents(65.2%) had finished university or above and 53.6% of the respondents were unemployed. In addition, the monthly family income of 161 participants exceeded 1000 dollars. More than half of the respondents(61.7%) were single and from urban areas(65.7%). 99(25.1%) and 76(19.3%) respondents had left-behind experience and substance abuse experience respectively. The educational level of the parents of the respondents was mostly university or above, especially father(35.3%). Two hundred eighteen participants(55.33%) were from the nuclear family. The number of participants from single child family(50.5%) and those from multiple children family(49.5%) accounted for about half each. Clinical diagnoses of the patients were depression(52.8%) and bipolar disorder(47.2%), of whom the majority were within 3 years of illness(58.1%) and within 1–3 times of recurrence(44.2%). 28.7% of participants reported impulsivity, and the vast majority of participants(93.4%) reported ACEs.
The prevalence of NSSI and comparisons of demographics, clinical features, impulsivity and ACEs between groups
The final sample comprised 245 adult patients accompanied with NSSI(62.2%) and 149 adult patients unaccompanied with NSSI(37.8%). Among 245 participants with NSSI, 135(55.1%) were diagnosed with depression and 110(44.9%) were diagnosed with bipolar disorder. Moreover, 57(14.4%) had engaged in one type of NSSI and 188(47.6%) had attempted more than one type of NSSI, respectively. “Deliberately pinching oneself”(23.1%) was the most common way of NSSI for female, while “Deliberately hiting hard objects such as walls, tables, windows and floors with fists”(12.7%) was the most common way of NSSI for male, as detailed in Fig.1.
Fig. 1.
Frequency of 12 kinds of NSSI among male and female participants
We also compared the demographics and clinical features of patients in the Depression-NSSI group, Bipolar Disorder-NSSI group and the Non-NSSI group to explore the relationships. Chi-square test showed that age, employments status, marital status, monthly family income, substance abuse experience, duration of illness, times of recurrence, impulsivity and ACEs were statistically different between the three groups(all P < 0.05), as presented in Table 1.
Risk factors associated with NSSI of participants
As revealed in Table 1, the variables that showed significance in the above comparison of 394 participants were further analyzed by multivariate regression analysis. As mentioned above, we also included sex in multivariate logistic regression based on the evidence from clinical and academic experience. By comparing patients between D-NSSI group and Non-NSSI group, we found increased risks of NSSI in depressed patients related to have a young age(OR = 0.300 and OR = 0.278; using 18 ~ 30 years old group as the reference category), unemployment(OR = 0.466; using unemployment group as the reference category), have a higher monthly family income(OR = 0.455; using > 1000 dollars group as the reference category) and have a history of ACEs(OR = 0.049; using ACEs group as the reference category), as presented in Table 2.
Table 2.
Final multivariable model, comparing patients with D-NSSI Group and Non-NSSI Group
| Variables | Odds Ratio | Standard Error | 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Age (years) | ||||
| 18 ~ 30 a | – | – | – | – |
| 31 ~ 45 | 0.300 | 0.588 | 0.095–0.950 | 0.041 |
| 46 ~ 60 | 0.278 | 0.439 | 0.117–0.656 | 0.004 |
| Employments status | ||||
| Unemployed a | – | – | – | – |
| Employed | 0.466 | 0.302 | 0.258–0.842 | 0.011 |
| Monthly family income (US dollar) | ||||
| > 1000 a | – | – | – | – |
| 700 ~ 1000 | 0.935 | 0.349 | 0.472–1.852 | 0.848 |
| 400 ~ 700 | 0.455 | 0.351 | 0.229–0.906 | 0.025 |
| Adeverse childhood experiences | ||||
| Yes a | – | – | – | – |
| No | 0.049 | 1.074 | 0.006–0.404 | 0.005 |
D-NSSI Group Depression-NSSI Group
BD-NSSI Group Bipolar Disorder-NSSI Group
a Reference group
By comparing patients between BD-NSSI group and Non-NSSI group, 5 variables - age, marital status, impulsivity, ACEs and duration of illness - emerged as significant correlates of NSSI in patients with bipolar disorder. More specifically, in patients with bipolar disorder, the incidence of NSSI was significantly lower in 31 ~ 45 and 46 ~ 60 years old group(OR = 0.254 and OR = 0.326; using 18 ~ 30 years old group as the reference category). Next, low risks for NSSI remained associated with married status(OR = 0.318; using single group as the reference category), no impulsivity (OR = 0.415; using impulsivity group as the reference category) and no ACEs group(OR = 0.272; using ACEs group as the reference category). Finally, duration of illness for more than 10 years were more likely to have NSSI than those less than 3 years(OR = 0.255; using > 10 group as the reference category), as presented in Table 3.
Table 3.
Final multivariable model, comparing patients with BD-NSSI Group and Non-NSSI Group
| Variables | Odds Ratio | Standard Error | 95% Confidence Interval | P-value |
|---|---|---|---|---|
| Age (years) | ||||
| 18 ~ 30 a | – | – | – | – |
| 31 ~ 45 | 0.254 | 0.575 | 0.802–0.784 | 0.017 |
| 46 ~ 60 | 0.326 | 0.440 | 0.138–0.772 | 0.011 |
| Marital status | ||||
| Single a | – | – | – | – |
| Married | 0.318 | 0.459 | 0.130–0.783 | 0.013 |
| Divorced or widowed | 0.710 | 0.613 | 0.213–2.361 | 0.576 |
| Impulsivity | ||||
| Yes a | – | – | – | – |
| No | 0.415 | 0.339 | 0.214–0.808 | 0.010 |
| Adeverse childhood experiences | ||||
| Yes a | – | – | – | – |
| No | 0.272 | 0.690 | 0.070–0.983 | 0.048 |
| Duration of illness (years) | ||||
| < 3 | 0.255 | 0.516 | 0.093–0.702 | 0.008 |
| 3 ~ 5 | 0.932 | 0.529 | 0.330–2.631 | 0.894 |
| 6 ~ 10 | 1.173 | 0.504 | 0.437–3.154 | 0.751 |
| > 10 a | – | – | – | – |
D-NSSI Group Depression-NSSI Group
BD-NSSI Group Bipolar Disorder-NSSI Group
a Reference group
Discussion
In terms of NSSI, there have been a few clinical studies involving patients with depression or bipolar disorder in Western countries [5, 38], however no such study was conducted in Chinese populations. This was the first study to investigated the prevalence of NSSI and risk factors for NSSI in patients with depression or bipolar disorder in China. Moreover, our findings indicated that a large number of patients with depression or bipolar disorder had engaged NSSI in this sample, and certain demographics, impulsivity and ACEs was associated with NSSI among patients with depression or bipolar disorder in China.
In the present study, our results of prevalence of NSSI was 62.2%, which was slightly lower than the prevalence of NSSI(77%) in a Canadian study among clinical populations [8]. Equally, Weintraub et al. [11] found that about 37% of patients with depression and 52% of patients with bipolar disorder had at least one NSSI, which was also higher than the results of this study(34.3 and 27.9%, respectively). The discrepancies in estimates of the prevalence of NSSI may be relate to different sample sources and numbers, various assessment tools, wording of instructions, time frame for raising questions and data collection procedures. As mentioned above, the incidence of NSSI is higher in patients with depression than in patients with bipolar disorder(34.3% vs 27.9%). Depression is a group of prominent and persistent low mood as the main features of the clinical syndrome [39]. Affected by the low mood, depressed patients often feel extremely sad, self abasement, decadent and pessimistic, and then the germ of an idea of NSSI took root in patient’s mind. In regard to the method of NSSI, patients of different sex tried NSSI in different ways. Barrocas [40] found ‘hitting against hard objects’ to be the most common way that male injury themselves, while Brunner [41] found ‘cutting’ to be the most common way that female injury themselves. These findings of ways of NSSI are generally consistent with this present study. Explainations for sex differences are yet to be examined and may be due to personality differences and cultural differences [42].
It has been suggested that demographic characteristics and clinical features(age, sex, marital status and diagnosis, etc) should be considered when interpreting results of any NSSI research [4]. Contrary to expectation, there was no statistical significance between patient’s sex, education, residence and the incidence of NSSI in patients with depression and bipolar disorder(P>0.05), which are contrary to Tang’s study [37]. On the one hand, this study included patients with depression and bipolar disorder. Compared with the general populations, their ability of emotion regulation and coping with life events is limited [43]. Whether male or female patients, the impact of negative life events and the failure of emotion regulation will stimulate the patients’ desire to conduct adopting stress reduction behaviors (e.g., NSSI), so as to escape from feelings and thoughts associated with stressful life events [44]. This may be the reason why there was no difference in the occurrence of NSSI between male and female patients in this study. On the other hand, this present study recruited patients from two psychiatric hospitals in Beijing, most of whom came from Beijing or the affluent urban families from other cities. Most included patients had better educational opportunities and higher level of education. The patients included in this study only reflect the situation of a small part of China, so the generalization of this finding is limited. Caution should be kept in quoting this findings.
To our surprise, statistical significance between substance abuse experience and the incidence of NSSI in patients with depression and bipolar disorder was not found(P>0.05), which was partially inconsistent with Escelsior’s findings [23]. This divergence is related to the fact that the substance abuse included in this study is not confined to cannabis, but also extended to various types of substance abuse. The number of patients with each type of substance abuse is limited, and the types of substance abuse are not concentrated, so we can not analyze all kinds of substance abuse experience separately, which may affect the results of this study. Notably, cannabis, inhalants, etc. for personal use are not allowed in Chinese laws [45], so the unwillingness of reporting such experiences hinders our further exploration. Different from other studies [46, 47], there is no significant difference in the left-behind experience between three groups, which may be related to the fact that most of the samples are from Beijing rather than remote and poor areas As the capital of China, Beijing has the ability to solve the employment problem without local people going out to look for employment opportunities [48], which was also reflected by the high educational level of patients and high monthly family income in this study.
By multivariate regression analysis, we proved that young, unemployment, single, a higher monthly family income, long duration of illness, impulsivity and ACEs were risk factors leading to NSSI of patients with depression and bipolar disorders. First of all, this study showed that younger participants(18 ~ 30 years old) had a higher risk of NSSI, which is consistent with Preyde’s findings that NSSI is more prevalent in young patients with psychiatric disorders due to their difficulty in emotional regulation, adaptive ability and interpersonal relationships [8, 49]. Next, the unemployed patients with depression were more likely to conduct NSSI. Compared with the employed patients, the unemployed patients can not have a relatively fixed incomes and stable personal relationships for a long time, which implied that it is inadequate for patients to get financial support and emotional support [50], increasing the risk of NSSI [51]. Moreover, we found increased risks of NSSI in depressed patients related to have a higher monthly family income. A higher monthly family income reflects that the family members who have limited spare time invested so much time and effort in work, which resulted in the limited time to get along with the patients, and then neglected the patients [52]. Due to the untimely response to the emotional needs of patients, the corresponding emotional support is insufficient, and patients are more likely to seek psychological comfort through NSSI. These findings highlight the importance of positive parenting style to NSSI onset, with implications for prevention of NSSI onset among depressed patients [53].
In this present study, marital status is one of the important factors affecting NSSI of patients with bipolar disorder, that is, single patients are more likely to engaged in NSSI, which has been repeatedly emphasized in previous studies [54–56]. It is widely known that family support obtained by stable marriage status was most salient in onset, maintenance and cessation of NSSI [55]. Stable marriage status provides social, economic and emotional support to patients and reduces their sense of isolation by providing them with opportunities to interact with society, and spouses of married patients play an important role in monitoring their partners’ health-related behaviors for a long time, encouraging them to develop healthy lifestyle [54]. Besides, long duration of illness(more than 10 years) was the risk factor for NSSI in patients with bipolar disorder. It is a long-term process to develop from unipolar depression to bipolar disorder [57]. During this period, the patient experienced repeated fluctuations of the disease. Affected by the symptoms or discontented treatment outcome, the patient felt hopeless and desperate, and then increased the possibility of NSSI. In addition, we proposed that impulsivity remained a significant influence on NSSI in patients with bipolar disorder, and this finding was supported by Lin et al. [58]. Individuals with strong impulsivity tend to act impulsively in the face of negative emotions, because the short-term gain of emotional regulation is the most important goal at present [59]. Since NSSI has been proved to be an effective method for individuals to regulate negtive emotions, individuals with strong impulsivity are more willing to participate in NSSI to obtain the direct benefits of NSSI(i.e. emotional regulation) [60]. At the same time, it is suggested that NSSI is a rapid, effective, and easily implemented method of regulating one’s negative emotion [58]. Consequently, impulsivity may be strongly related to NSSI.
In recent years, several studies found that individuals reporting ACEs were tied up with NSSI [61, 62], which were consistent with this study. What’s more, ACEs can be strongly associated to NSSI among patients with depression and bipolar disorder [5]. Although heritability is often emphasized, NSSI is associated with environmental factors [63]. As a series of negative life events, ACEs will affect the individual’s psychological development and emotional regulation [64]. And the patients with depression or bipolar disorder already have weak ability of emotional regulation [65]. Therefore, patients with ACEs can relieve their negative emotions by adopting NSSI. This also explains why ACEs has a subtle effect on the occurrence of NSSI in patients with depression and bipolar disorder. Serafini’s study also highlighted the specific role of sexual abuse in the development of NSSI [25], so exploring specific associations between various types of ACEs and NSSI would be the next step. So far, some existing studies have investigated the mediators or moderators in relationship between ACEs and NSSI [66]. It is necessary to explore the specific connections between ACEs and NSSI, especially in the Chinese backdround.
Implications
This study investigated the prevalence of NSSI and its risk factors among patients with depression and bipolar disorder in China. Primarily, we have obtained the not encouraging prevalence to arouse the attention of domestic medical staff, relevant scholars and the public. That is to say, the coping strategies for NSSI should not be confined to hospitals but extended to the communities and families. Then, by comparing the demographic data, impulsivity and ACEs between groups, the relevant influencing factors were found, which can provide support for the exploration of prevention, treatment and etiology of this group. Eventually, the risk factors for NSSI was identified by multivariate regression analysis. Except for the assessment of general demographic data, assessment procedures of mental health may need to include an assessment of impulsivity and ACEs to more fully evaluate NSSI. A combination of the risk factors mentioned above and diagnosis of depression or bipolar disorder among patients who conduct NSSI can also alert medical staff to develop targeted interventions aimed at helping these patients and their families with emotion regulation skills so as to cope with past negative experiences and consequently improve their mental health and well-being. From an academic point of view, this study further confirmed the correlations between NSSI and some factors in patients with depression and bipolar disorder, further supported the conclusions of some scholars. This study also offered new thought for scholars of various contries to guide them to carry out more scientific and targeted research. Notably, future studies should focus on the origin of NSSI as opposed to its characteristics, in order for professionals to be able to prevent the issue.
Limitations
Several limitations of the current study need to be acknowledged. Initially, the participants included were patients in two hospitals in Beijing. As the capital of China, Beijing will attract patients from all over the country, the samples are mainly Beijing native. Considering that China is a vast country with diversified social economy, the source of sample would limits the generalizability of these findings to other cities and rural areas of China. Second, we employed retrospective self-report questionnaires, and there is no independent confirmation, which might mean our data were not sufficiently objective. Participants may forget, suppress or even identify with their experiences as they grow older and more experienced. Therefore, these data may be affected by bias to some extent. Third, an exploration of testing the directionality of the relationships is not allowed in the present study because of the design of cross-sectional. There may be a great deal of analyses and the possibility that some of the correlations were obtained by chance. Taking into account these limitations, additional studies are needed to investigate the NSSI and tease apart the association between NSSI and some factors in order to determine how generalizable the results of this study would be to other psychiatric hospitals from diffirent regions in China. Such studies should employ a large sample, multicenter, longitudinal design, and adopt tools other than self-report questionnaire(e.g., expert opinions or other objective evidence). And we should remain cautious in drawing causal inferences regarding the relationship between NSSI and some factors.
Conclusions
Despite these limitations, the current study examined the prevalence of NSSI and its risk factors in patients with depression and bipolar disorder based on data from a sample of two psychiatric hospitals in Beijing. Our study reported that NSSI was experienced by a significant number of patients with depression or bipolar disorder, and NSSI were associated with some factors, including age, employment status, marital status, impulsivity, etc. NSSI not only affects the physical and mental health of the patients, but also places an insupportable burden on the family and society. Some implications for public policy were manifested in this study. The risk of NSSI in patients with depression and bipolar disorder, especially who are young, unemployment, from family with high monthly income, single, impulsive, and have long duration of illness, ACEs should be assessed. Awareness of NSSI should be improved in the family and society. Likewise, training for health care workers and educators are needed, to help them identify and intervene as early as possible [67]. It is necessary to formulate targeted interventions, as well as provide timely social support for patients with NSSI and his family [68]. In terms of methodology, future studies should enrich the access to information, including interviews with patients and their family members, medical records or other objective documents to verify and supplement these reports of patients obtained by using self-rating scales. And future studies can also focus on the relationship between NSSI and its possible risk factors among patients with other types of mental disorders and compare them, rather than focusing on one or two mental disorders alone in order to find the differences.
Acknowledgements
We appreciated Jun Liu, Yuan Yang, Jin-Hong Li and Jiang-Ling Xu for their support during sample collection. At the same time, we also acknowledged the assistance of Peking Union Medical College, Beijing Anding Hospital and Beijing HuiLongGuan Hospital for their enthusiastic support in the whole research process.
Abbreviations
- NSSI
Non-suicidal self-injury
- ACEs
Adverse childhood experiences
- ICD-10
The 10th Revision of the International Classification of Diseases
Authors’ contributions
LW and HZ designed the study, JL and YY collected the data, LW analyzed and interpreted the data, and was a major contributor in writing the manuscript. All authors read and appro ved the final manuscript.
Funding
No funding was solicited or received for this manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
The recruitment, consent, and field procedures were approved by the Research Ethics Board of Peking Union Medical College (2019–18-K7). Written informed consent was obtained from individual or guardian participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lu Wang, Email: 275977819@qq.com.
Jun Liu, Email: 709658326@qq.com.
Yuan Yang, Email: 951797727@qq.com.
Haiou Zou, Email: haiou1018@126.com.
References
- 1.Nock MK, Favazza AR. Nonsuicidal self-injury: definition and classification. In: Nock MK, editor. Understanding nonsuicidal self-injury: origins, assessment, and treatment: American Psychological Association; 2009. p. 9–18.
- 2.Brophy M, Holmstrom R. Truth hurts: report of the national inquiry into self-harm among young people; 2006. https://www.mentalhealth.org.uk/sites/default/files/truth_hurts. Accessed 16 Mar 2020
- 3.Guha M. Diagnostic and statistical manual of mental disorders: DSM-5 (5th edition) Ref Rev. 2014;28(3):36–37. [Google Scholar]
- 4.Brown RC, Plener PL. Non-suicidal self-injury in adolescence. Curr Psychiatry Rep. 2017;19(3):20. doi: 10.1007/s11920-017-0767-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baiden P, Stewart SL, Fallon B. The role of adverse childhood experiences as determinants of non-suicidal self-injury among children and adolescents referred to community and inpatient mental health settings. Child Abuse Negl. 2017;69:163–176. doi: 10.1016/j.chiabu.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Benjet C, González-Herrera I, Castro-Silva E, Méndez E, Borges G, Casanova L, et al. Non-suicidal self-injury in Mexican young adults: prevalence, associations with suicidal behavior and psychiatric disorders, and DSM-5 proposed diagnostic criteria. J Affect Disord. 2017;215:1–8. doi: 10.1016/j.jad.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Duggan J, Heath N, Hu T. Non-suicidal self-injury maintenance and cessation among adolescents: a one-year longitudinal investigation of the role of objectified body consciousness, depression and emotion dysregulation. Child Adolesc Psychiatry Ment Health. 2015;9(1):21. doi: 10.1186/s13034-015-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Preyde M, Vanderkooy J, Chevalier P, Heintzman J, Warne A, Barrick K. (2014). The psychosocial characteristics associated with NSSI and suicide attempt of youth admitted to an In-patient psychiatric unit. J Can Acad Child Adolesc Psychiatry. 2014;23(2):100–110. [PMC free article] [PubMed] [Google Scholar]
- 9.Guerreiro DF, Cruz D, Frasquilho D, Santos JC, Figueira ML, Sampaio D. Association between deliberate self-harm and coping in adolescents: a critical review of the last 10 years' literature. Arch Suicide Res. 2013;17(2):91–105. doi: 10.1080/13811118.2013.776439. [DOI] [PubMed] [Google Scholar]
- 10.Kim KL, Galvan T, Puzia ME, Cushman GK, Seymour KE, Vanmali R, et al. Psychiatric and self-injury profiles of adolescent suicide attempters versus adolescents engaged in nonsuicidal self-injury. Suicide Life Threat Behav. 2015;45(1):37–50. doi: 10.1111/sltb.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weintraub MJ, Van de Loo MM, Gitlin MJ, Miklowitz DJ. Self-harm, affective traits, and psychosocial functioning in adults with depressive and bipolar disorders. J Nerv Ment Dis. 2017;205(11):896–899. doi: 10.1097/NMD.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang J, Li W. Investigation of status and risk factors in major depressive disorder patients with non-suicidal self-injury. J Clin Psychiatry (Chinese) 2019;29(1):19–21. [Google Scholar]
- 13.Wan Y, Chen J, Sun Y, Tao F. Impact of childhood abuse on the risk of non-suicidal self-injury in mainland Chinese adolescents. PLoS One. 2015;10(6):e0131239. doi: 10.1371/journal.pone.0131239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lang J, Yao Y. Prevalence of nonsuicidal self-injury in chinese middle school and high school students: a meta-analysis. Medicine (Baltimore) 2018;97(42):e12916. doi: 10.1097/MD.0000000000012916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bentley KH, Nock MK, Barlow DH. The four-function model of nonsuicidal self-injury: key directions for future research. Clin Psychol Sci. 2014;2(5):638–656. doi: 10.1177/2167702613514563. [DOI] [Google Scholar]
- 16.Klonsky ED. The functions of self-injury in young adults who cut themselves: clarifying the evidence for affect-regulation. Psychiatry Res. 2009;166(2–3):260–268. doi: 10.1016/j.psychres.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann N Y Acad Sci. 2008;1124(1):111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. 2015;38:55–64. doi: 10.1016/j.cpr.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Plener PL, Libal G, Keller F, Fegert JM, Muehlenkamp JJ. An international comparison of adolescent non-suicidal self-injury (NSSI) and suicide attempts: Germany and the USA. Psychol Med. 2009;39(9):1549–1558. doi: 10.1017/S0033291708005114. [DOI] [PubMed] [Google Scholar]
- 20.Calhoun PS, Van Voorhees EE, Elbogen EB, Dedert EA, Clancy CP, Hair LP, et al. Nonsuicidal self-injury and interpersonal violence in U.S. veterans seeking help for posttraumatic stress disorder. Psychiatry Res. 2017;247:250–256. doi: 10.1016/j.psychres.2016.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tschan T, Schmid M, In-Albon T. Parenting behavior in families of female adolescents with nonsuicidal self-injury in comparison to a clinical and a nonclinical control group. Child Adolesc Psychiatry Ment Health. 2015;9(1):17. doi: 10.1186/s13034-015-0051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lombardo LE, Bearden CE, Barrett J, Brumbaugh MS, Pittman B, Frangou S, et al. Trait impulsivity as an endophenotype for bipolar I disorder. Bipolar Disord. 2012;14(5):565–570. doi: 10.1111/j.1399-5618.2012.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Escelsior A, Belvederi Murri M, Corsini GP, Serafini G, Aguglia A, Zampogna D, et al. Cannabinoid use and self-injurious behaviours: a systematic review and meta-analysis. J Affect Disord. 2021;278:85–98. doi: 10.1016/j.jad.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 24.Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behav Res Ther. 2007;45(10):2483–2490. doi: 10.1016/j.brat.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serafini G, Canepa G, Adavastro G, Nebbia J, Belvederi Murri M, Erbuto D, et al. The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front Psychiatry. 2017;8:149. doi: 10.3389/fpsyt.2017.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swannell S, Martin G, Page A. Suicidal ideation, suicide attempts and non-suicidal self-injury among lesbian, gay, bisexual and heterosexual adults: findings from an Australian national study. Aust N Z J Psychiatry. 2016;50(2):145–153. doi: 10.1177/0004867415615949. [DOI] [PubMed] [Google Scholar]
- 27.Lobana A, Mattoo SK, Basu D, Gupta N. Quality of life in schizophrenia in India: comparison of three approaches. Acta Psychiatr Scand. 2010;104(1):51–55. doi: 10.1034/j.1600-0447.2001.104001051.x. [DOI] [PubMed] [Google Scholar]
- 28.Wan YH, Hu CL, Hao JH, Sun Y, Tao FB. Deliberate self-harm behaviors in Chinese adolescents and young adults. Eur Child Adolesc Psychiatry. 2011;20(10):517–525. doi: 10.1007/s00787-011-0213-1. [DOI] [PubMed] [Google Scholar]
- 29.Wan Y, Liu W, Hao J, Tao F. Development and evaluation on reliability and validity of adolescent non-suicidal self-injury assessment questionnaire. Chin J Sch Health (Chinese) 2018;39(2):170–173. [Google Scholar]
- 30.McMahon K, Hoertel N, Olfson M, Wall M, Wang S, Blanco C. Childhood maltreatment and impulsivity as predictors of interpersonal violence, self-injury and suicide attempts: a national study. Psychiatry Res. 2018;269:386–393. doi: 10.1016/j.psychres.2018.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chamorro J, Bernardi S, Potenza MN, Grant JE, Marsh R, Wang S, et al. Impulsivity in the general population: a national study. J Psychiatr Res. 2012;46(8):994–1001. doi: 10.1016/j.jpsychires.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization (WHO) Adverse childhood experiences international questionnaire (ACE-IQ) 2016. [Google Scholar]
- 33.Kim YH. Associations of adverse childhood experiences with depression and alcohol abuse among Korean college students. Child Abuse Negl. 2017;67:338–348. doi: 10.1016/j.chiabu.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Kidman R, Smith D, Piccolo LR, Kohler HP. Psychometric evaluation of the adverse childhood experience international questionnaire (ACE-IQ) in Malawian adolescents. Child Abuse Negl. 2019;92:139–145. doi: 10.1016/j.chiabu.2019.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Almuneef M, Saleheen HN, ElChoueiry N, Al-Eissa MA. Relationship between childhood bullying and addictive and anti-social behaviors among adults in Saudi Arabia: a cross-sectional national study. Int J Adolesc Med Health. 2017;31(5):/j/ijamh.2019.31.issue-5/ijamh-2017-0052/ijamh-2017-0052.xml.10.1515/ijamh-2017-0052. [DOI] [PubMed]
- 36.Ho GWK, Chan ACY, Chien WT, Bressington DT, Karatzias T. Examining patterns of adversity in Chinese young adults using the adverse childhood experiences-international questionnaire (ACE-IQ) Child Abuse Negl. 2019;88:179–188. doi: 10.1016/j.chiabu.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 37.Tang J, Li G, Chen B, Huang Z, Zhang Y, Chang H, et al. Prevalence of and risk factors for non-suicidal self-injury in rural China: results from a nationwide survey in China. J Affect Disord. 2018;226:188–195. doi: 10.1016/j.jad.2017.09.051. [DOI] [PubMed] [Google Scholar]
- 38.Thomassin K, Shaffer A, Madden A, Londino DL. Specificity of childhood maltreatment and emotion deficit in nonsuicidal self-injury in an inpatient sample of youth. Psychiatry Res. 2016;244:103–108. doi: 10.1016/j.psychres.2016.07.050. [DOI] [PubMed] [Google Scholar]
- 39.Moore A. Overcoming depression and low mood: a five areas approach: CRC Press (Taylor and Francis); 2014. p. 2–7.
- 40.Barrocas AL, Hankin BL, Young JF, Abela JR. Rates of nonsuicidal self-injury in youth: age, sex, and behavioral methods in a community sample. Pediatrics. 2012;130(1):39–45. 10.1542/peds.2011-2094. [DOI] [PMC free article] [PubMed]
- 41.Brunner R, Kaess M, Parzer P, Fischer G, Carli V, Hoven CW, et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: a comparative study of findings in 11 European countries. J Child Psychol Psychiatry. 2013;55(4):337–348. doi: 10.1111/jcpp.12166. [DOI] [PubMed] [Google Scholar]
- 42.Tresno F, Ito Y, Mearns J. Risk factors for nonsuicidal self-injury in Japanese college students: the moderating role of mood regulation expectancies. Int J Psychol. 2013;48(6):1009–1017. doi: 10.1080/00207594.2012.733399. [DOI] [PubMed] [Google Scholar]
- 43.Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: the experiential avoidance model. Behav Res Ther. 2006;44(3):371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Briere J, Hodges M, Godbout N. Traumatic stress, affect dysregulation, and dysfunctional avoidance: a structural equation model. J Trauma Stress. 2010;23(6):767–774. doi: 10.1002/jts.20578. [DOI] [PubMed] [Google Scholar]
- 45.Yang X, Xia G. Causes and consequences of drug abuse: a comparison between synthetic drug and heroin users in urban China. AIDS Educ Prev. 2019;31(1):1–16. doi: 10.1521/aeap.2019.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Y, Zhang M, Chen H. Self-injury among left-behind adolescents in rural China: the role of parental migration and parent-child attachment. Front Psychol. 2019;9:2672. doi: 10.3389/fpsyg.2018.02672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang Q, Liu X. Peer victimization and nonsuicidal self-injury among Chinese left-behind children: the moderating roles of subjective socioeconomic status and social support. J Interpers Violence. 2020:088626051989734. 10.1177/0886260519897346. [DOI] [PubMed]
- 48.Cheng J, Sun YH. Depression and anxiety among left-behind children in China: a systematic review. Child Care Health Dev. 2015;41(4):515–523. doi: 10.1111/cch.12221. [DOI] [PubMed] [Google Scholar]
- 49.Benson L, English T, Conroy DE, Pincus AL, Gerstorf D, Ram N. Age differences in emotion regulation strategy use, variability, and flexibility: an experience sampling approach. Dev Psychol. 2019;55(9):1951–1964. doi: 10.1037/dev0000727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perreault M, Touré EH, Perreault N, Caron J. Employment status and mental health: mediating roles of social support and coping strategies. Psychiatr Q. 2017;88(3):501–514. doi: 10.1007/s11126-016-9460-0. [DOI] [PubMed] [Google Scholar]
- 51.Arshad U, Farhat-Ul-Ain GJ, Husain N, Chaudhry N, Taylor PJ. A systematic review of the evidence supporting Mobile- and internet-based psychological interventions for self-harm. Suicide Life Threat Behav. 2020;50(1):151–179. doi: 10.1111/sltb.12583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lu W, Jun L, Yanhua Q, Haiou Z. A study on the status and influencing factors of non-suicidal self-injury in patients with mood disorders. J Psychiatry(Chinese) 2020;33:134–139. [Google Scholar]
- 53.Victor S, Hipwell A, Stepp S, Scott L. Parent and peer relationships as longitudinal predictors of adolescent non-suicidal self-injury onset. Child Adolesc Psychiatry Ment Health. 2019;13(1):1. doi: 10.1186/s13034-018-0261-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kyung-Sook W, SangSoo S, Sangjin S, Young-Jeon S. Marital status integration and suicide: a meta-analysis and meta-regression. Soc Sci Med. 2018;197:116–126. doi: 10.1016/j.socscimed.2017.11.053. [DOI] [PubMed] [Google Scholar]
- 55.Tatnell R, Kelada L, Hasking P, Martin G. Longitudinal analysis of adolescent NSSI: the role of intrapersonal and interpersonal factors. J Abnorm Child Psychol. 2014;42(6):885–896. doi: 10.1007/s10802-013-9837-6. [DOI] [PubMed] [Google Scholar]
- 56.Neufeld E, Hirdes JP, Perlman CM, Rabinowitz T. Risk and protective factors associated with intentional self-harm among older community-residing home care clients in Ontario, Canada. Int J Geriatr Psychiatry. 2015;30(10):1032–1040. doi: 10.1002/gps.4259. [DOI] [PubMed] [Google Scholar]
- 57.Cheniaux E, Landeira-Fernandez J, Versiani M. The diagnoses of schizophrenia, schizoaffective disorder, bipolar disorder and unipolar depression: interrater reliability and congruence between DSM-IV and ICD-10. Psychopathology. 2009;42(5):293–298. doi: 10.1159/000228838. [DOI] [PubMed] [Google Scholar]
- 58.Lin M, You J, Ren Y, Wu JY, Hu W, Yen C, et al. Prevalence of nonsuicidal self-injury and its risk and protective factors among adolescents in Taiwan. Psychiatry Res. 2017;255:119–127. doi: 10.1016/j.psychres.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 59.Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull. 2008;134(6):807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Armey MF, Crowther JH, Miller IW. Changes in ecological momentary assessment reported affect associated with episodes of nonsuicidal self-injury. Behav Ther. 2011; 42:579–88. 10.1016/j.beth.2011.01.002. [DOI] [PubMed]
- 61.Gomes Jardim GB, von Gunten A, da Silva Filho IG, Ziegelmann PK, Bumaguin DB, Nogueira EL, et al. Relationship between childhood maltreatment and geriatric depression: the mediator effect of personality traits. Int Psychogeriatr. 2019;31(12):1759–1767. doi: 10.1017/S1041610219000073. [DOI] [PubMed] [Google Scholar]
- 62.Guvendeger Doksat N, Zahmacioglu O, Ciftci Demirci A, Kocaman GM, Erdogan A. Association of suicide attempts and non-suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst Use Misuse. 2017;52(5):604–613. doi: 10.1080/10826084.2016.1245745. [DOI] [PubMed] [Google Scholar]
- 63.Maciejewski DF, Creemers HE, Lynskey MT, Madden PA, Heath AC, Statham DJ, et al. Overlapping genetic and environmental influences on nonsuicidal self-injury and suicidal ideation. JAMA Psychiatry. 2014;71(6):699–705. doi: 10.1001/jamapsychiatry.2014.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Choi JY, Oh KJ. Cumulative childhood trauma and psychological maladjustment of sexually abused children in Korea: mediating effects of emotion regulation. Child Abuse Negl. 2014;38(2):296–303. doi: 10.1016/j.chiabu.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 65.Van Rheenen TE, Murray G, Rossell SL. Emotion regulation in bipolar disorder: profile and utility in predicting trait mania and depression propensity. Psychiatry Res. 2015;225(3):425–432. doi: 10.1016/j.psychres.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 66.Gu H, Ma P, Xia T. Childhood emotional abuse and adolescent nonsuicidal self-injury: the mediating role of identity confusion and moderating role of rumination. Child Abuse Negl. 2020;106:104474. doi: 10.1016/j.chiabu.2020.104474. [DOI] [PubMed] [Google Scholar]
- 67.Hasking P, Boyes ME, Finlay-Jones A, McEvoy PM, Rees CS. Common pathways to NSSI and suicide ideation: the roles of rumination and self-compassion. Arch Suicide Res. 2019;23(2):247–260. doi: 10.1080/13811118.2018.1468836. [DOI] [PubMed] [Google Scholar]
- 68.Nemati H, Sahebihagh MH, Mahmoodi M, Ghiasi A, Ebrahimi H, Barzanjeh Atri S, et al. Non-suicidal self-injury and its relationship with family psychological function and perceived social support among Iranian high school students. J Res Health Sci. 2020;20(1):e00469. doi: 10.34172/jrhs.2020.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.