Healthcare associated infections (HCAIs) are known to cause loss of life and economic burden worldwide. In the UK, the annual financial cost of HCAIs is estimated as £1 billion [1] and in Europe it is estimated to cause 37,000 deaths annually [2]. In England, surveillance data for several common HCAIs causing organisms is available through Public Health England reporting (PHE).
This study sought to compare trends in the number of organism-specific publications in relation to surveillance reports, to identify if clinical need drives academic publication.
Inclusion-exclusion criteria were determined from a previous study [3]. A PubMed literature search was used to retrieve publications, regardless of direct clinical significance (see Table S1 for search terms).
The following epidemiological surveillance data in UK NHS trusts was retrieved from PHE (Public Health England 2018): lab-confirmed carbapenem-resistant Enterobacterales (CRE), methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive Staphylococcus aureus (MSSA) bacteraemia reports, and lab-confirmed C. difficile cases. Mandatory reporting began for MRSA in 2005, MSSA in 2011 and from 2007 for C. difficile. CRE reports comprised of voluntary data, beginning in 2003.
Pearson correlation coefficient analysis was used to investigate the relationship between reports and numbers of publications. All analysis was undertaken in OriginPro (2018).
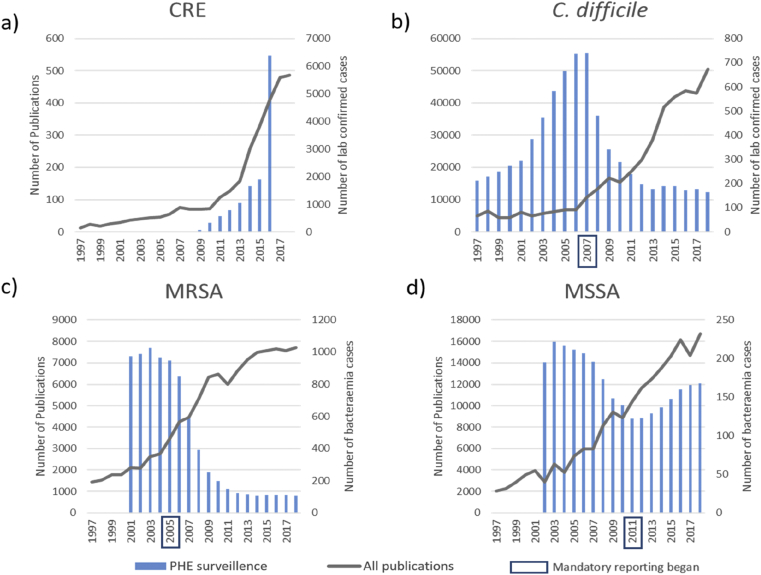
The PubMed search retrieved 106,665 publications between 1997 and 2018. Some correlations were identified between number of publications for each organism type and the PHE reports for the same period (Figure 1).
Figure 1.
Publications of a) Carbapenem-resistant Enterobacterales, b) C. difficile c) methicillin-resistant Staphylococcus aureus d) methicillin-sensitive Staphylococcus aureus in comparison with Public Health England surveillance.
The relationship between reported cases and academic publication varied between organism. For CRE, there were limited reports between 2003 and 2010 (n=545), which was followed by a sharp increase in 2016 (n=6,391). Despite this, academic publishing achieved only a steady increase each year, reaching 487 articles in 2018 (Figure 1a). C. difficile had the highest number of reported cases in 2007 (n=55,498) and the most successful reduction in reported cases (down 78% by 2018). From 2006 onwards, publications increased, peaking in 2018 (n=617), despite the reduction in reported cases (Figure 1b). MRSA reached a peak in reported cases in 2003 (n=7,700), with dramatic reductions from 2007 onwards. As PHE reported cases reduced, academic publications increased consistently (Figure 1c). MSSA did not follow this trend. There were small reductions in reported cases each year from a peak in 2004 (n=15,600 cases) until 2012. Publications have risen each year since 2004 (Figure 1d).
Higher numbers of reported cases did not have an associated increase in numbers of publication. C. difficile had the highest number of reported cases (n=507,379), but did not have the most publications. MSSA had a large number of bacteraemia reports (n=205,847) and a comparatively small number of publications (n=2,755). Interestingly, for C. difficile and MRSA, (Figures 1b and 1c), publications appear to follow a strong, moderate inverse relationship, which was statistically significant (P <.001), whereas CRE followed a strong positive relationship, (P <.001) in which publication and cases appeared to rise in parallel.
This study sought to investigate if patterns of publication were correlated to numbers of reported clinical cases from PHE. Different pathogens were studied over time, falling in and out of academic favour, by assessing overall academic publications on several pathogens and reported cases to the PHE. While this data was a free and reliable source for all reported cases of different organisms by trust, these were laboratory confirmed positive cases only, and variation in testing and clinical review may have lead to underreporting.
A variety of relationships were observed. Some organisms had much higher numbers of reported cases than others (e.g. C. difficile) and some far fewer (e.g. CRE). Positive correlations were seen between PHE reports and academic publications for CRE and MSSA, and negative correlations were seen for C. difficile and MRSA. These fluctuations could be explained by a variety of factors, such as interventions linked to national targets. The large increase in CRE reports between 2015 and 2016 may potentially have been driven by the publication of the PHE CRE detection protocol in 2014.
Head et al. found that a total £2.6 billion investment was allocated to UK infectious disease research between 1997–2010 [4]. Of this funding, 47% was allocated to C. difficile research despite the number of cases falling in 2008, (Figure 1b), which could account for continued publications despite considerable reductions in cases. Available funding may be a bigger driver for research, and therefore academic publication, than the current needs of hospitals and microbiological burden.
The findings from this study identified a failing link between academic output and clinical need. Academic publications appeared to be influenced by available funding and academic interest, rather than outbreak organisms and pathogens of most clinical concern and causing the greatest burden to healthcare services. Bridging the gap between clinical practise and academic publication could steer critical research and evidence-based publications relevant to clinicians in practise resulting in greater tangible impact on patient care and safety.
Funding
This work was funded by a University College London Impact Scholarship in collaboration with GAMA Healthcare. Dr Cloutman-Green received salary funding from the National Institute for Health Research (ICA-CL 2015-01-002).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.infpip.2020.100053.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Plowman R. The socioeconomic burden of hospital acquired infection. Euro Surveillance. 2000;5:49–50. doi: 10.2807/esm.05.04.00004-en. [DOI] [PubMed] [Google Scholar]
- 2.Simoes A.S., Couto I., Toscano C., Goncalves E., Povoa P., Viveiros M. Prevention and Control of Antimicrobial Resistant Healthcare-Associated Infections: The Microbiology Laboratory Rocks! Front Microbiol. 2016;7 doi: 10.3389/fmicb.2016.00855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rawlinson S., Ciric L., Cloutman-Green E. How to carry out microbiological sampling of healthcare environment surfaces? A review of current evidence. J Hosp Infect. 2019;86:84–91. doi: 10.1016/j.jhin.2019.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Head M.G., Fitchett J.R., Holmes A.H., Atun R. Funding healthcare-associated infection research: a systematic analysis of UK research investments, 1997–2010. J Hosp Infect. 2014;87:84–91. doi: 10.1016/j.jhin.2014.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.