Summary
Background
Cleaning is a critical tool for infection prevention and control, and is a key intervention for preventing healthcare associated infections (HCAIs) and controlling intermediate transmission routes between patient and environment. This study sought to identify potential areas of weakness in clinical surface cleaning, and assess the effectiveness of a staff group specific training intervention.
Observations
One-hundred hours of audit observations in a paediatric cardiac intensive care unit (CICU) assessed surface cleaning technique of healthcare staff within bedspaces. Cleaning was assessed with a 5-component bundle, with each cleaning opportunity scored out of five.
Training Intervention
Fifty hours of audit observations before and after a training intervention tested the efficacy of a staff group specific education intervention. The intervention was developed and implemented for 69% of nurses and 100% of cleaners.
Results
One hundred and eighteen cleaning opportunities were observed before training, and scored an average of 2.4. One hundred and twenty-one cleaning opportunities were observed after training and scored an average 3.0. On average, before training, each cleaning opportunity by nurses and cleaners fulfilled 2.4 and 2.5, respectively, of the 5 bundle components. Following training, this improved to 3.3 and 2.9 respectively. There was a statistically significant improvement in bundle scores for nurses (P=.004) and cleaners (P=.0003).
Conclusions
Surface wipe methods were inconsistent between all staff groups. The education based intervention resulted in a small improvement in most of the cleaning components. This study has identified how a small but targeted cleaning training intervention can have a significant (P= <.0001) impact on cleaning bundle compliance for both nurses and cleaners.
Keywords: Cleaning, Hospital, Infection prevention and control, Intervention study
Introduction
Surfaces are a known vehicle for transmission of HCAI, and it is proven that pathogens can survive on surfaces for months in the clinical environment if effective cleaning has not taken place [1]. While cleaning is an important component of infection control, many studies have identified that cleaning has not been effective within the hospital environment [2,3].
Cleaning is critical to the reduction of HCAI. It has been shown that effective cleaning is associated with lower HCAI [4]. Several studies have assessed the different components required to clean effectively with wipes [[5], [6], [7]], and all these components must be followed in order to achieve a clean, safe surface [5]. To ensure cleaning is effective, training to clean to a high standard and keeping compliance consistent with all these components is critical. Despite this, training is often lacking and inconsistent across all staff groups, and staff members can be left confused as to where to check cleaning find themselves uncomfortable with asking for help [8].
Furthermore, choice of cleaning agent can be difficult and is dependant on hospital setting or local policy. Choice and implementation of cleaning training can also be confusing, as training and audit process varies [9]. Cleaning audits can range from visual inspection alone, use of fluorescent markers, adenosine triphosphate (ATP) devices or microbiological sampling [10].
Education-based interventions have been shown to improve cleaning compliance [[11], [12], [13]], and studies that focus on balancing infection prevention knowledge with engagement of cleaners have a positive impact on their knowledge and attitudes, and consequently, their cleaning compliance [12]. It is also highlighted how smaller interventions focused on feedback by use of a ultraviolet marker can produce small-scale and effective ways at improving compliance by allowing cleaners to measure their progress [13]. Unfortunately, training and guidance for training is lacking, and knowing when, how, and how often to train all staff on cleaning can be difficult to ascertain and, as such, training content varies considerably [9,10]. An international survey revealed only 46% of staff were given yearly cleaning training, 15% twice-yearly, and 20% sporadic [10].
Bundle-style training with audit and re-audit is a well-known practise for infection prevention and control interventions and are an important tool for improving professional practise [14,15]. These bundles are a small set of evidence-based interventions, when implemented together, allow greater improvement than if they were applied alone. These bundles usually consist of 3–5 elements [16]. A well-known bundle-style intervention is the ‘5 moments for hand hygiene’ campaign [17]. The 5 bundle components chosen for this study were determined from good practise thought to improve cleaning, such as using the appropriate number of wipes for each surface and selecting the correct wipe [[5], [6], [7],18].
The aim of this study was to design and trial an audit tool to assess compliance of best practise surface cleaning, as established by review of the literature and opinion of the hospital infection prevention and control staff. The audit tool would allow assessment of cleaning practise and implementation in parallel with a targeted educational training intervention to improve bundle compliance across different staff groups within a clinical setting.
Methods
Audit criteria – the cleaning bundle
An evidence-based audit tool was developed to produce an audit standard for observations to be assessed against. This cleaning was based on 5 key moments, as bundle-based interventions usually adopt 3–5 evidence-based components [19], such as the ‘5 moments for hand hygiene’ campaign [17] and have been effective in delivering training in clinical settings [20]. The bundle was used to judge each cleaning opportunity recorded and generate a score, in which each component had equal weight. The following criteria completed the cleaning bundle shown in the text box below.
The 5 component cleaning bundle.
-
1.
Has the entire surface been cleaned?
This ensures all components of a surface are cleaned, including the undersides of objects.
-
2.
Was an ‘s’ shape motion with overlap used?
This motion is proven to clean the most effectively and ensure contamination is not dragged across a previously cleaned area.
-
3.
Was one wipe used for each surface (or until dirty or soiled)?
The size of the surface must be assessed and the amount of wipes used as appropriate.
-
4.
Was the wipe folded out entirely?
Folding out the wipe allows maximum surface area for cleaning, and for the capillary action of the wipes to work as per manufacturer design.
-
5.
Was the correct wipe used?
Correct wipes or cloth was determined as per the local cleaning protocol. For cleaners, cloths and chlorine-based cleaning agent are to be used for surface cleaning. For nurses, alcohol wipes are to be used for IV tray cleaning, and Clinell Universal for all other surface cleaning. Paper towels or chlorhexidine cannula wipes are not to be used for surface cleaning.
The five components of the bundle were chosen by assessing the literature, and by consultation with the Infection Prevention and Control team at Great Ormond Street Hospital.
Bundle component 1
Bundle component 1 was determined by an important discussion by Sattar and Maillard [5], in which failure to decontaminate the entire surface means a surface cannot be deemed safe, and can allow easy re-contamination.
Bundle component 2
This component was chosen as this method is the gold standard for surface cleaning and ensures a dirty cloth cannot contaminate the surface during cleaning [7]. This motion ensures the entire surface is cleaned and potential soiling is not pulled across previously cleaned surfaces [7].
Bundle component 3
Component 3 was introduced following evidence from several studies in which soaked cloths and impregnated wipes have a limited volume, therefore a limited capacity to clean a certain surface area. Use depletes the ‘wetness’ and disinfectant, and therefore must be replaced as appropriate to lose decontamination potential and risk poor cleaning or contaminating surfaces [[5], [6], [7]].
Bundle component 4
Component 4 ensures the wipe is used to maximum effect. Improper use of cloths or wipes could allow release of pathogens from the wipe [5].
Bundle component 5
Finally, this component follows evidence discussing how incorrect wipe and therefore inappropriate cleaning agent can allow transfer of pathogens, and that different wipes are more effective against different organisms [5,6].
Audit observations
Observations were undertaken for 50 hours within a 4-bedded bay within a paediatric cardiac intensive care unit (CICU). Observations were completed by two individuals using the same scoring criteria, trained in cleaning and bundle compliance by the GOSH IPC team, to ensure consistency of results. The observing staff members were placed at the ends of a 4-bed bay unit, to remain out of the way of clinical practise and, as much as possible, reduce the hawthorn effect [21]. Observations were recorded over 15 days, encompassing a range of times to reflect different ward activity in the mornings, afternoons, and evenings. All healthcare staff undertaking surface cleaning, with either surface wipes or microfiber cloths and chlorine-based cleaner, within occupied and unoccupied bedspace environments were observed, including how and what they cleaned, and the technique used. Patients and parents were not included within the study. Staff were broken down into four groups; doctors, nurses, cleaners and others. The others category included housekeepers, physiotherapists, healthcare assistants and x-ray technicians. Each group had different cleaning responsibilities, as defined in the local training matrix, and have different levels of knowledge on the role of cleaning in preventing HCAI due to different training. Nurses were responsible for cleaning surfaces within their immediate working area; IV tray, bed tables, nurses station keyboard and mouse, equipment trolley. Cleaners were responsible for cleaning fixed features within the bedspace such as the floors, walls and wider environment, as well as non-clinical equipment surfaces within the bedspace during post-discharge cleans.
Development of the education intervention
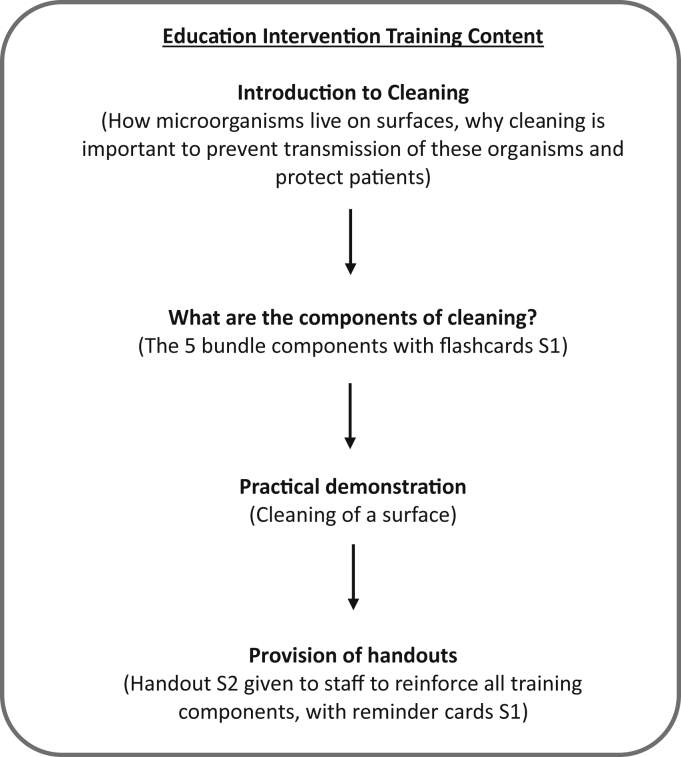
The training was delivered over 2 weeks within the ward. Nurses had not received prior cleaning training elsewhere. One hundred and three nurses (69% of total team) and the entire cleaning team of five individuals (100%) were captured during this time. Other staff groups, such as healthcare assistants and physiotherapists, were not trained as they comprised of very small numbers. Training was delivered by a practical demonstration of using wipes on a surface (trolley) and using flashcards (S1). Training was undertaken for approximately 15 minutes per session and was based on the ward in order to capture the maximum number of staff, allowing staff to drop in during each session.
A leaflet (S2) with more detailed information on the importance of cleaning and more detail for each component trained in was made available. The leaflets were also placed on the staff notice board, and left in the break room. They were topped up throughout the study process. While focusing on the bundle components, emphasis was made on the rationale behind each aspect to try and enhance overall understanding and the fundamentals of cleaning and how cleaning works.
Delivery of the education intervention
The education intervention was delivered with the following components:
Face-to-face education interventions have been proven effective in improving IPC knowledge and the role cleaning plays in domestic workers [8]. Training sessions for nurses and cleaners were structured in an identical fashion, with training sessions for both staff groups covering the same content. Where initial observations identified reduced compliance (components 1 and 2 for nurses, and components 2 and 3 for cleaners) training ensured that these points were adequately covered.
Statistical analysis
Analysis of scores was undertaken using an unpaired t-test, and analysis to individual bundle components was assessed using one-way ANOVA. All statistical analysis was undertaken in OriginLab2018.
Results
Pre-intervention audit
Prior to the training intervention, nurses and cleaners scored 2.4 and 2.5 respectively of a possible 5 from an observed 26 (nurses) and 92 (cleaners) cleaning opportunities. Following the intervention, both nurses and cleaners had significant compliance improvement, scoring 3.3 and 2.9 (P=.004, P=.0003) respectively of a possible 5, following 33 (nurses) and 88 (cleaners) observed cleaning opportunities. This equates to an improvement of 18 % in the nurses and 8 % in the cleaners.
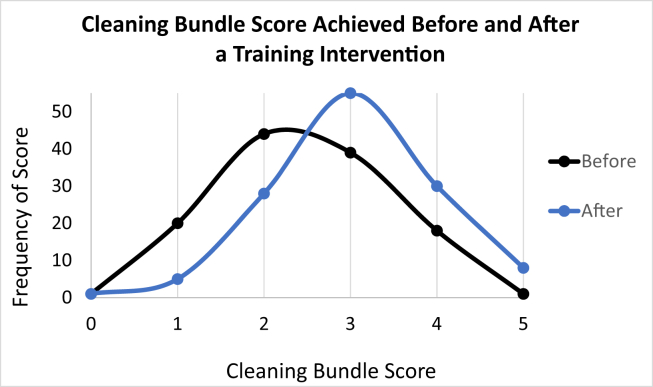
Figure 1 shows the improvement, overall, in bundle compliance scores, leading to a right shift following cleaning training. There was a small increase in cleaning observations following the training, increasing from 118 to 122. On average, before the training, each cleaning opportunity fulfilled 2.4 bundle components of a possible 5, highlighting the need for improvement. Following the training, this improved to 3 out of 5, which was a small but significant (P<.0001) increase in compliance.
Figure 1.
Cleaning bundle score achieved and compliance to each bundle component before and after a targeted training intervention, for nurses and cleaners.
Post-intervention audit
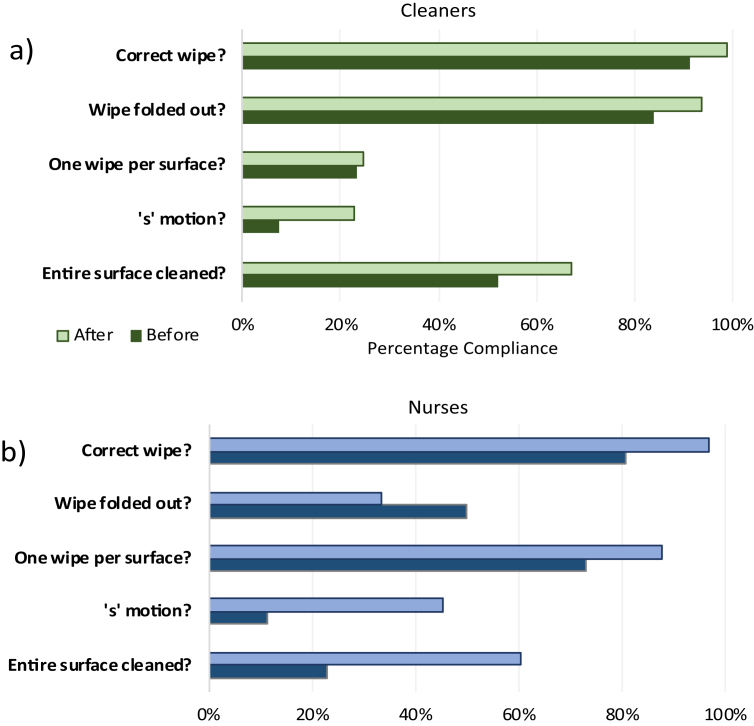
When auditing individual compliance to each bundle component by staff group, it was identified that compliance varies between each component of the bundle and staff group. Individual compliance for each cleaning opportunity varied between nurses and cleaners, with ranges of 0–80%, and 20–80%. It was found, from the initial observations, nurses had the lowest compliance in cleaning the entire surface and using the ‘s’ motion (23% and 12% compliance respectively) as shown in Figure 2. Cleaners had lower compliance with using ‘s’ motion and a single wipe for each surface (8% and 23% compliance). Following the training, focusing on these specific areas, overall improvement was found for nurses (P= .004) and cleaners (P= .0003), as well as a change in compliance for each bundle component. All bundle components for both staff groups showed improvement following training, except for a reduction (-17%) in compliance for folding out the wipe for nurses.
Figure 2.
Percentage compliance to each bundle component before and after the training intervention for (a) cleaners (n= 92 & 88 cleaning opportunities) and (b) nurses (n = 26 & 33 cleaning opportunities).
Following training, for nurses, the most significant improvements were cleaning the entire surface (P= .003) and using ‘s’ motion (P= .004) which were the two targeted components for the training. For cleaners, improvements were in the same two components, only one of which (using ‘s’ motion) was a focus for improvement, which had a small but significant improvement of 15% (P=.004). Despite being a target for improvement, using one wipe per surface had insignificant improvement (P= .855) at just 2%.
Education intervention
During the education intervention, 69% of nurses and 100% of cleaners received training. A total of 38 leaflets were handed out, and 118 reminder cards were taken (S3). Cleaning staff had a particular interest in the bundle components and asking questions to ensure they were doing their role to their best capability. A large number of staff trained, both nurses and cleaners, commented on how they had not been taught the understanding behind folding out a wipe and using it flat. For nurses, these comments were reflected in a lower pre-intervention compliance of just 50% for unfolding the wipe fully, however this was the only component to have reduced compliance, at 33%, following the training. Some comments were also made on how the wipes were “too wet”, a problem which was rectified by only taking one wipe at a time.
Discussion
This study sought to assess how effective cleaning was on a paediatric CICU by use of an audit re-audit study, in which all cleaning opportunities were assessed against an audit standard of a 5 component bundle, where all 5 components must be fulfilled in order to achieve good cleaning practise. Following this assessment, a specific training package was designed to target areas in which the different staff groups were less competent, which was rolled out over 2 weeks. Following a 1.5 week waiting period, the audit was repeated and cleaning assessed with the same audit standard. It was found that the training intervention had a small but significant impact on cleaning bundle compliance overall (P= < .0001) and for nurses (P= .004) and cleaners (P= .0003).
This study followed a clear need for improvement for surface cleaning in light of surface contamination recovered from hospital surfaces [[22], [23], [24]]. Multiple studies have reported how cleaning competency is poor and requires intervention to reduce the associated HCAI. The intervention was designed to be of a size which would ensure feasible enrolment throughout the ward, while trying to remain as effective as possible.
The 5-point cleaning bundle
Bundle-style training interventions have been proven to be extremely effective [12,[25], [26], [27]]. All five components of the bundle were to be fulfilled for a cleaning opportunity to be effective. These components represented the lowest requirement to still achieve effective cleaning. Other components are important to ensure effective cleaning such as; the order of cleaning (clean to dirty) to ensure contamination is not spread, using the correct concentration of cleaning agent [28] and adhering to contact times, however, all these components could not be captured within the constraints of a small-scale intervention and audit study. All bundle components were trained, with emphasis on the specific components of failure between nurses and cleaners.
Understanding and attitudes with education interventions
It is clear that some training interventions have a greater impact when compared with others [11,12] and that the size of the intervention can vary widely [13]. This study sought to assess if a smaller yet carefully targeted intervention could have a significant impact on cleaning audit compliance, and represent a useful and feasible cleaning intervention that could be implemented within a busy ward environment. It has been shown that smaller interventions in the form of a questionnaire can improve compliance and attitudes of cleaners [8]. Larger interventions, while often effective, are both time consuming and require extensive resources, and are often multifaceted [12]. This scale of intervention is not always possible, especially in smaller NHS trusts, in which time and resources are in short supply. This intervention represents a small yet still effective intervention that could be advocated for, rather than a larger training scheme in which critical personnel need to take time out of their working day. In the case of CICU, which was the study setting, nurses could not leave their patient unattended. The training was designed to be flexible and was most frequently delivered bedside, with the flashcards (S1), whereas a larger or lecture-based training intervention could miss these critical staff groups.
During the study, for both staff groups, the importance of cleaning was reiterated. Cleaning is the cornerstone of infection prevention and control and one of the most important defence strategies for preventing HCAI. With the rise of antibiotic resistance, cleaning may soon be the barrier between a patient and surface-mediated pan-drug resistant organisms. It is important for staff to remember just how critical cleaning is, and how this often-overlooked component is vital to running the hospital; without cleaning, the hospital could not function safely.
As cleaners are responsible for the majority of cleaning within the clinical space, and have such an important role, it was critical training was both informative and inclusive. During training, the importance of their role was emphasised, with reference to keeping the patients safe from HCAI. Effective training can only be completed following a change in attitude. Multiple studies have shown how cleaners do not feel valued, and how they often do not feel a part of the wider team [29]. The increasing reliance on subcontracted services within the NHS has only worsened this issue. Other studies have shown how easy it can be to change the attitudes of the cleaners by ensuring they know they are valued [30] while emphasising how their personal perception of their environment can have an active impact on cleaning efficacy [31]. It has also been shown by multiple studies that feedback of cleaning efforts have a positive impact on cleaning efficacy [30].
Reception of the training was extremely positive. The domestic cleaning team were eager to learn and were pleased to receive some structured training, making them feel more valued, which is a key component for compliance [29]. The cleaners also asked the most questions and were not afraid to speak up regarding any confusion. Despite this excitement for training and willingness to ask questions nurses still had better improvement in the components they were trained in when compared to cleaners.
Reminder cards with the bundle components (S3) were offered. All staff took the cards. It was the hope that these cards would provide a way in which staff could remind themselves and check best practise without fear of admitting fault. By fitting into the standard NHS cardholders, the cards would be non-offensive, easy to access, and could be wiped down if required.
How individual bundle and overall compliance has improved
Improvements were assessed overall, and by each component. Nurses had a 38% and 33% improvement in the components, and cleaners a 15% and 2% improvement. This demonstrates how nurses had a greater improvement in their targeted bundle components following training. On average, for all bundle components, nurses had a greater improvement, at 17%, whereas the cleaners had a more modest 10% improvement. Cleaners, however, had 3.8% better overall compliance prior to the training.
This distribution in improvements and initial compliance could be explained by the nature of the job roles. Cleaners are only required to clean to fulfil their role, whereas nurses have multiple duties, of which cleaning forms only a small part. Therefore, it could be expected that cleaners should have better compliance overall. The enhanced improvement for nurses in comparison to cleaners could be a result of the targeted training working to complement their background knowledge of infection control, whereas cleaners have no background training in infection control, and would therefore not have this knowledge to build upon.
By breaking down the compliance for each component of the bundle, the importance for targeted training was highlighted, such as overall compliance in using the ‘s’ motion at 6%, whereas compliance for the correct wipe was 92%. By looking at compliance between staff groups, the differences again showed the need for training, delivered in slightly different ways. Cleaners and nurses had a similar compliance to wipe selection, at 94% and 80% respectively. However, there was a great difference between the other components, such as using a single wipe for each surface, nurses had 70% compliance while cleaners only had 19%. There was also a noticeable difference when assessing if the entire surface was cleaned. While the training components (S1, S2, S3) and content remained the same for each staff group, delivery and emphasis on different components was made.
The study design in which the areas of failure were afforded extra emphasis could have introduced some bias. This study was limited by its size and time period. Due to the length of the study, it was not possible to ascertain efficacy of the training over time, and to identify when re-training should be provided to ensure the most effective coverage, as compliance could possibly wane over time, as has been reported in other studies [30]. It is the hope that the distribution of the leaflets and reminder cards would extend this process as long as possible. Completing this training regularly could lead to a cumulative effect of improvements to extend the bundle score of 3 to the maximum 5 over time, but further speculation would require continued intervention and observation. Furthermore, nurses were shown to have greater overall improvement in compliance following training, despite 69% of nurses receiving training in comparison with the whole cleaning team. This is surprising when considering the difference in size of the staff groups, (103 individual nurses and 5 cleaners) in which a proportion of nurses may not have been captured during the post-intervention observations due to high staff numbers and limited time of the study.
Conclusions
This study sought to assess the compliance to the cleaning bundle on a paediatric CICU by use of a 5-component bundle as an audit standard. Overall compliance to bundle components was a 2.5 score of a possible 5. A targeted training intervention was found to have a small but significant (P <.0001) improvement to 3.0 overall in cleaning compliance, in both nurses and cleaners. This study highlights how smaller, inexpensive, targeted interventions can be effective and represent a feasible way of introducing training to enhance compliance. It was found that the design of this training was effective, and the different areas for focus for nurses and cleaners were demonstrated to have the most improvement.
Author contribution
Stacey Rawlinson: Conceptualisation, Methodology, Investigation, Analysis, Writing – Original draft, Writing – Review & Editing. Faiza Asadi: Methodology, Investigation. Helen Saraqi: Methodology, Resources. Barbara Childs: Resources. Lena Ciric: Conceptualisation, Methodology, Resources, Writing – Review & Editing, Supervision, Funding acquisition. Elaine Cloutman-Green: Conceptualisation, Methodology, Resources, Writing – Review & Editing, Supervision, Funding acquisition.
Funding
This project was funded by a PhD Impact Studentship in partnership with UCL and GAMA Healthcare. Dr Cloutman-Green received salary funding from the National Institute for Health Research (ICA-CL 2015-01-002).
Acknowledgements
All study materials were designed independently by the authors, but printing and production was funded by GAMA healthcare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.infpip.2020.100083.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kramer A., Schwebke I., Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. Bmc Infect Dis. 2006;6 doi: 10.1186/1471-2334-6-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carling P.C., Von Beheren S., Kim P. Woods C, Healthcare Environmental Hygiene Study G. Intensive care unit environmental cleaning: an evaluation in sixteen hospitals using a novel assessment tool. J Hosp Infect. 2008;68:39–44. doi: 10.1016/j.jhin.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 3.Dharan SM P., Copin P., Bessmer G., Tschanz B., Pittet D. Routine disinfection of patients’ environmental surfaces. Myth or reality? J Hosp Infect. 1999;42:113–117. doi: 10.1053/jhin.1999.0567. [DOI] [PubMed] [Google Scholar]
- 4.Dancer S.J. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect. 2009;73:378–385. doi: 10.1016/j.jhin.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 5.Sattar S.A., Maillard J.Y. The crucial role of wiping in decontamination of high-touch environmental surfaces: review of current status and directions for the future. Am J Infect Control. 2013;41:S97–S104. doi: 10.1016/j.ajic.2012.10.032. [DOI] [PubMed] [Google Scholar]
- 6.West A.M., Nkemngong C.A., Voorn M.G., Wu T., Li X., Teska P.J. Surface area wiped, product type, and target strain impact bactericidal efficacy of ready-to-use disinfectant Towelettes. Antimicrob Resist Infect Control. 2018;7:122. doi: 10.1186/s13756-018-0416-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bergen L.K., Meyer M., Hog M., Rubenhagen B., Andersen L.P. Spread of bacteria on surfaces when cleaning with microfibre cloths. J Hosp Infect. 2009;71:132–137. doi: 10.1016/j.jhin.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell B.G., White N., Farrington A., Allen M., Page K., Gardner A. Changes in knowledge and attitudes of hospital environmental services staff: The Researching Effective Approaches to Cleaning in Hospitals (REACH) study. Am J Infect Control. 2018 doi: 10.1016/j.ajic.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell B.G., Farrington A., Allen M., Gardner A., Hall L., Barnett A.G. Variation in hospital cleaning practice and process in Australian hospitals: A structured mapping exercise. Infect Dis Health. 2017;22:195–202. [Google Scholar]
- 10.Kenters N., Gottlieb T., Hopman J., Mehtar S., Schweizer M.L., Tartari E. An international survey of cleaning and disinfection practices in the healthcare environment. J Hosp Infect. 2018;100:236–241. doi: 10.1016/j.jhin.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell B.G., Hall L., White N., Barnett A.G., Halton K., Paterson D.L. An environmental cleaning bundle and health-care-associated infections in hospitals (REACH): a multicentre, randomised trial. Lancet Infect Dis. 2019;19:410–418. doi: 10.1016/S1473-3099(18)30714-X. [DOI] [PubMed] [Google Scholar]
- 12.Allen M., Hall L., Halton K. Graves N. Improving hospital environmental hygiene with the use of a targeted multi-modal bundle strategy. Infecti, Dis Health. 2018;23:107–113. doi: 10.1016/j.idh.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Gillespie E., Wright P.L., Snook K., Ryan S., Vandergraaf S., Abernethy M. The role of ultraviolet marker assessments in demonstrating cleaning efficacy. Am J Infect Control. 2015;43:1347–1349. doi: 10.1016/j.ajic.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 14.Ivers N., Jamtvedt G., Flottorp S., Young J.M., Odgaard-Jensen J., French S.D. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charrier L., Allochis M.C., Cavallo M.R., Gregori D., Cavallo F., Zotti C.M. Integrated audit as a means to implement unit protocols: a randomized and controlled study. J Eval Clin Pract. 2008;14:847–853. doi: 10.1111/j.1365-2753.2008.01042.x. [DOI] [PubMed] [Google Scholar]
- 16.Wilson J. Rethinking the use of audit to drive improvement. J Infect Prev. 2018;19:3–4. doi: 10.1177/1757177417746732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO . 2009. WHO guidelines on hand hygiene in Health care. [Google Scholar]
- 18.Boyce J.M. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob Resist Infect Control. 2016;5:10. doi: 10.1186/s13756-016-0111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karapanou A., Vieru A.M., Sampanis M.A., Pantazatou A., Deliolanis I., Daikos G.L. Failure of central venous catheter insertion and care bundles in a high central line-associated bloodstream infection rate, high bed occupancy hospital. Am J Infect Control. 2020 doi: 10.1016/j.ajic.2019.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Sax H., Allegranzi B., Uckay I., Larson E., Boyce J., Pittet D. Pittet D ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67:9–21. doi: 10.1016/j.jhin.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Megeus V., Nilsson K., Karlsson J., Eriksson B.I., Andersson A.E. Hand hygiene and aseptic techniques during routine anesthetic care - observations in the operating room. Antimicrob Resist Infect Control. 2015;4:5. doi: 10.1186/s13756-015-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganime A.C., Carvalho-Costa F.A., Mendonca M.C., Vieira C.B., Santos M., Costa Filho R. Group A rotavirus detection on environmental surfaces in a hospital intensive care unit. Am J Infect Control. 2012;40:544–547. doi: 10.1016/j.ajic.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 23.Rocha I.V., Xavier D.E., Almeida K.R.H., Oliveira S.R., Leal N.C. Multidrug-resistant Acinetobacter baumannii clones persist on hospital inanimate surfaces. Braz J Infect Dis. 2018;22:438–441. doi: 10.1016/j.bjid.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rawlinson S., Ciric L., Cloutman-Green E. How to carry out microbiological sampling of healthcare environment surfaces? A review of current evidence. J Hosp Infect. 2019 doi: 10.1016/j.jhin.2019.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Aboelela S.W., Stone P.W., Larson E.L. Effectiveness of bundled behavioural interventions to control healthcare-associated infections: a systematic review of the literature. J Hosp Infect. 2007;66:101–108. doi: 10.1016/j.jhin.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 26.Kulali F., Calkavur S., Oruc Y., Demiray N., Devrim I. Impact of central line bundle for prevention of umbilical catheter-related bloodstream infections in a neonatal intensive care unit: A pre-post intervention study. Am J Infect Control. 2019;47:387–390. doi: 10.1016/j.ajic.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen H.B., Daniel-Underwood L., Van Ginkel C., Wong M., Lee D., Lucas A.S. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: an evaluation for medical student training. Resuscitation. 2009;80:674–679. doi: 10.1016/j.resuscitation.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 28.Keah K.C., Jegathesan M., Tan S.C., Chan S.H., Chee O.M., Cheong Y.M. Bacterial contamination of hospital disinfectants. Med J Malaysia. 1995;50:291–297. [PubMed] [Google Scholar]
- 29.Cross S., Gon G., Morrison E., Afsana K., Ali S.M., Manjang T. An invisible workforce: the neglected role of cleaners in patient safety on maternity units. Glob Health Action. 2019;12:1480085. doi: 10.1080/16549716.2018.1480085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doll M., Stevens M., Bearman G. Environmental cleaning and disinfection of patient areas. Int J Infect Dis. 2018;67:52–57. doi: 10.1016/j.ijid.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Rawlinson S., Cloutman-Green E., Asadi F., Ciric L. Surface sampling within a pediatric ward—how multiple factors affect cleaning efficacy. Am J Infect Control. 2020;48:740–745. doi: 10.1016/j.ajic.2019.10.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.