Summary
Background
Despite successful efforts to reduce Meticillin Resistant Staphylococcus aureus bloodstream infections (BSI) and Clostridium difficile infection, Gram-negative BSI (GNBSI) have continued to increase in England. Public Health England (PHE) and NHS Improvement (NHSI) were tasked by the Minister for Health to lead the development of tools and resources to support healthcare workers to reduce these infections.
Aim
To work with commissioners and providers of healthcare to collaboratively develop resources to support whole health economies to reduce GNBSI using a combination of behavioural insights and quality improvement methods.
Methods
We took a unique approach to develop these tools and resources using a combination of behavioural insights, quality improvement and front-line collaboration to ensure the tools and resources were designed around the needs of those who would use them. The approach taken was a stepwise iterative process in two distinct phases: a development phase and a testing phase. Both phases used a combination of behavioural insights, human factors, quality improvement and co-production methods to engage stakeholders in co-designing resources that would support them in their work to reduce GNBSI.
Findings
During the development phase, feedback from workshops and stakeholder reviews indicated that tools needed to be reduced, simplified, and communicated clearly. Stakeholders wanted tools that could be used by a cross-system group and indicated that leadership was key to ensuring resources were adopted to drive improvements. The final tools were published on the NHS Improvement GNBSI hub. This electronic platform had 30,000 visits between May 2017 and October 2018.
Key words: Gram-negative bloodstream infections, Behavioural insights, Collaboration, Infection prevention and control, Co-design, Co-production
Introduction
In 2011, the Chief Medical Officer for England outlined the global threat of antimicrobial resistance (AMR) and put forward recommendations to address this threat, one of which was the implementation of a cross-government UK AMR Strategy (2013–18) [1], [2]. In 2014, the World Health Organization (WHO) further defined the scale of the challenge through its situation analysis and established a formal tripartite alliance between public health, animal health and food safety under a ‘One Health’ approach [3]. Although many had predicted this AMR threat, the WHO demonstrated that AMR is present globally in every region of the world with individuals of all ages and in every country affected [4]. Subsequently, Lord O'Neill chaired a review on AMR on behalf of the UK Government and found that ‘AMR is one of the biggest health threats that mankind faces now and in the coming decades’ [5].
The availability of effective antimicrobials to treat infections is at the heart of modern medicine. It allows individuals who need them to live longer and healthier lives and allows healthcare interventions, such as surgery and chemotherapy, to be delivered safely. Without urgent global action, WHO stresses that the world is headed for a ‘post-antibiotic era’ [4]. Countries are urged to undertake a range of measures to tackle AMR, including enhancing infection prevention and control (IPC) and prescribing antimicrobials correctly and only when needed (antimicrobial stewardship) [6]. Healthcare workers are key to ensuring that individuals are protected by preventing infections at every opportunity and advocating appropriate antimicrobial use.
In England, Gram-negative bloodstream infections (GNBSIs) continue to increase despite the decreases seen in Meticillin-Resistant Staphylococcus aureus (MRSA) bloodstream infection and Clostridium difficile infections (CDI) [7]. A large proportion of these GNBSIs are caused by Escherichia coli (E. coli), so a focused effort on targeting such infections is essential [8]. A total of 41,060 cases of E.coli BSI were reported through the mandatory reporting in England between 1 April 2017 and 31 March 2018; an increase of 1.1% from 2016/17 and an increase of 27.1% from 2012/13 [9].
Voluntary information on the primary focus of infection from the surveillance data detailed that urinary tract infection (UTI) is the most common reason for E.coli BSI (45–49%). The majority of E.coli BSI cases have their onset in the community, defined as infections detected within the first 48 hours of admission; in comparison 7,704 (18.8 %) were hospital onset cases [9].
In November 2016 the Health Minister announced plans to halve healthcare-associated (defined as healthcare hospital intervention or antibiotic use in the 28 days prior to the detection of the BSI) GNBSI at a health summit which was attended by a wide range of experts and frontline healthcare workers [3]. Subsequently the Health Minister announced that a resource toolkit would be developed to help support the plans to reduce GNBSI. To successfully deliver this resource toolkit, engaging and collaborating with frontline health care workers was key, as was the use of insights from behavioural science and quality improvement.
Using behavioural insights to develop and deliver interventions to reduce healthcare-associated infections
Delivery of health and social care is complex and interventions that may suit one area of England will not automatically translate to another. The National Health Service Five Year Forward View (FYFV) outlined the shared vision of a number of partner organisations in England with the mandate for improving the delivery of healthcare. It articulated a new approach whereby there is more engagement with those leading the delivery of care and patients receiving care so that communities were more involved and resources to support them were closely aligned with their needs [10].
We know that increasing knowledge and awareness of an issue such as the rising rates of GNBSIs is rarely enough to trigger successful and sustained behaviour change. Even when people intend to do something differently, they often don't which is described as the ‘intention-behaviour gap’ [11]. Barriers to behaviour change are complex and include psychological factors such as competing motivations, physical or environmental factors such as lack of resources, suitable working areas and social or organisational factors such as prevailing practices and social norms in a given workplace. Identifying these barriers to intended actions is a key part of the behavioural insights approach, as this enables interventions to be targeted more directly at the factors that are influencing people's behaviour [11].
In recent years co-production has been recognised as a fundamental approach in the development health and social care services [12]. This model recognises the unique role that individuals, be they healthcare workers or patients, play in the development of tools, resources and services. Following this principle, healthcare workers are seen as active contributors as opposed to, in more traditional healthcare approaches, simply passive recipients. By using a “whole systems” approach, co-production makes use of participatory techniques to proactively engage healthcare workers in decision-making through all the stages of design, delivery and, ultimately, evaluation. Designing resources with those that will use them in practice makes them more valuable, effective and more likely to be utilised in the long term. The development of an improvement resource package to reduce GNBSI that supports those working in the front line must therefore be delivered in equal partnership, rather than through a top down approach. This project involved collaboration between staff from key national bodies and those working in healthcare to co-design resources. The process of development was supported and informed by the use of behavioural insights.
Methods
Ethical consideration
Research ethics approval was not required for this work according to the definitions provided by the United Kingdom medical research council; this was not primary research but service improvement.
Design
There were two distinct phases in this project; the resource development phase and the resource testing phase. Both phases used a combination of behavioural insights, human factors and quality improvement methodologies to engage stakeholders in co-design.
Phase 1- Development
A steering group was established in December 2016 to oversee the project and included experts from each of the national organisations leading this work: NHS Improvement (NHSI), NHS England (NHSE) and Public Health England (PHE) with experts from each of the following professions: antimicrobial stewardship, behavioural science, infection prevention and control, public health/health protection and microbiology.
The first step in developing the resource was identifying the underpinning causes of patients acquiring GNBSI. When dealing with complex issues such as these, it is often difficult to differentiate between cause and effect, making it harder to identify the change projects that are needed. Quality Improvement driver diagrams were developed to help identify what changes will likely cause the desired effect [13].
The driver diagram allowed the steering group to focus on interventions that might make the biggest impact. The group drafted initial resources targeted at five distinct audiences; each were slightly different depending on the audience's characteristics and needs.
The next step was inviting and involving stakeholders in the design process. This was conducted in three stages; collaborative co-design workshop which involved active participation, stakeholder virtual review/stakeholder site visits and a redesign workshop.
The collaborative co-design workshop was convened at the end of January 2017 with 30 stakeholders being recruited from those who had attended the health summit in November 2016 [3]. The aim of the workshop was to review the initial package of resources the steering group had developed and, being guided by behavioural science methods, to collaboratively redesign them.
Attendees were placed in five groups depending on their expertise and each group focused on resources for the target audiences identified by the steering group; Boards and Leadership, Community Healthcare Providers (CHP), Directors of Infection Prevention and Control/Infection Prevention and Control experts, Clinical Commissioning Groups (CCGs) who are responsible for planning and commissioning health care services for their local area were clustered with General Practitioners (GPs)/primary care. Each group provided expert insight into what resources would help support their target audience and, following the workshop, members volunteered to be involved in the stakeholder virtual review, stakeholder site visits and the redesign workshop.
Phase 1. Virtual Stakeholder Review and Stakeholder site visits
Volunteers from each of the five working groups were emailed and asked to respond to a set of questions about the resources (Appendix 1). These questions were informed by two behaviour change models: COM-B, which proposes that people need to have the Capability, Opportunity and Motivation to perform a given Behaviour, [14] and SHEL, which looks at how the interfaces between Software (resources), Hardware (systems), Environment and Liveware (people) affect behaviours [15]. The project team also visited a number of volunteers from the working groups to understand the work environment and explore a similar set of questions.
Phase 1. Redesign Workshop
Following the completion of the virtual review and site visits, the resources were modified based on participants' insights and a redesign workshop was convened in mid-March 2017 with experts representing PHE, NHSI and NHSE. The “EAST” framework was used to guide the redesign process as a reminder to those designing the resources to ensure end users were kept in mind [16]. This framework proposes that interventions should be made Easy, Attractive, Social and Timely (EAST). The resources were updated following this workshop to be presented at the final collaborative workshop.
Phase 1. Final collaborative workshop
A workshop was held at the end of March 2017 with invites extended to those who attended the first workshop and who participated in the working groups. Attendees were asked to focus their comments on design, structure and content and if there were any resources missing. Following final refinements, the resources were published on the NHS Improvement website and additional tools, as suggested by the group, were developed and tested with voluntary clinical commissioning groups (CCGs).
Phase 2- Testing
The testing phase was carried out using Quality Improvement Methodology; the Plan, Do, Study, Act (PDSA) cycles, first developed by Deming [17]. This method uses continuous improvement, engaging front-line workers in identifying problems and solutions, and focuses on changing processes [18].
Findings
Phase 1- Development
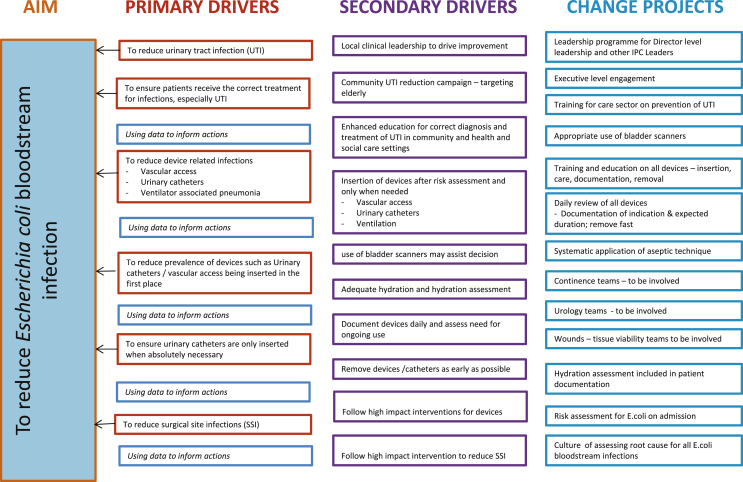
The steering group used this model to identify primary and secondary drivers and projects that may lead to effective change (Figure 1). The driver diagram was a valuable tool, as it facilitated understanding within the steering group of the key underlying issues that needed to be addressed by the resources. The diagram also prompted discussion about what change project tools could support efforts to tackle these issues.
Figure 1.
Driver Diagram with change projects to reduce E.coli Bloodstream infections.
Involvement of stakeholders from the outset was an important part of the development of the resources. Comments from all members of the workshop and the steering group were documented and included in a report that was fed back at the final workshop in an open and transparent way.
Phase 1. Virtual Stakeholder Review and Stakeholder site visits
Key findings from insights collated from conducting Virtual Stakeholder Review and Site visits were grouped into three themes: “existing levers for”; “barriers to” embedding behaviour changes aimed at reducing GNBSIs; and “requirements of a GNBSI IPC resource”. The themes and key comments were summarised in Table I.
Table I.
Feedback themes from virtual stakeholder review, site visits and redesign workshop
| Feedback themes | Key insights provided by stakeholders |
|---|---|
| Existing levers for embedding behaviour changes aimed at reducing GNBSIs |
|
| Barriers to embedding behaviour changes aimed at reducing GNBSIs |
|
| What resources would support a reduction in GNBSI |
|
| Key messages |
|
Phase 2- Testing
The four CCGs who agreed to test the resources convened a cross-system working group where the tools were introduced and each group asked to use the them over a period of one month and then complete the questions (Appendix I). The results from these CCGs were submitted and summarised in themes. The findings, outlined in Table II, led to further changes to the resource tools.
Table II.
Testing of the resources in 4 Clinical Commissioning Groups - results summarised
| Question | Key themes |
|---|---|
| 1. How ‘user-friendly’ are the resources? |
|
| 2. Do you think these resources might fit into your current working practices |
|
| 3. What are the barriers for people using the resources? |
|
| 4. How could these barriers be overcome? |
|
| 5. What do you think might encourage people to make use of these resources? |
|
| 6. What processes (if any) are already in place in your workplace to prevent/reduce/manage E. coli BSI? |
|
| 7. Could any of the processes or resources you already use for IPC be of use to inform the development of this resource? If so, how? |
|
| Feedback on the specific tools | Summary of responses |
| a) Patient case improvement tool |
|
| b) Organisation self-assessment and improvement tool – to support a gap analysis |
|
| c) Self-assessment against the Health and Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance |
|
Discussion
The improvement resource to support the reduction in GNBSI was co-designed with stakeholders and providers from across the healthcare sector. This collaborative stepwise process was valuable as the resources were developed in line with what health and social care workers felt would support them in reducing GNBSI in their locality. The resources originally designed by the project steering group were very different to the final product published on the NHS Improvement GNBSI hub, which demonstrates the value of ensuring end user stakeholder groups are actively engaged in every step of development of such resources. Between the publication date in May 2017 and October 2018 there were 30,000 views of the resource website.
This was a unique and novel project in three key ways. Firstly, the development phase was enhanced by the engagement of frontline staff from across the healthcare sector. Secondly, the development and testing of the resource was informed by the use of behavioural insights and human factors models of behaviour, COM-B [14] and SHEL, which we believe is a novel application in this context [15]. The questionnaire (Appendix I) used in both the development and testing phases was designed using these behavioural science models to ensure we captured factors that might encourage or hinder staff in using the resources. Finally, the collaborative and iterative development of the resource was supported in the testing phase through the use of the quality improvement PDSA method [17], [18], which is not usually applied in the development and dissemination of resources.
Throughout the process of developing and testing the resources, there were lessons we learned. We engaged with two patient representatives in the second workshop but could have included patient representatives throughout the whole process, to ensure a fully co-produced approach. The care home and social care sector were not involved and more work needs to be done with this sector. This gap is indicative of wider health and social integration that is yet to be realised in England [12].
Reducing GNBSIs will require cross-system multidisciplinary groups meeting and developing a plan at a local level in order to address this complex issue. The project demonstrates that understanding the full range of factors that drive local health leads' and professionals' behaviours is essential for designing and delivering a resource that aims to bring about reductions in infection rates. A top down approach to developing such a tool without full engagement and participation of providers who will be using those tools will likely result in resources that are not utilised effectively. The methods we used are different to those used in a top down approach. Meeting the needs of different areas requires engagement with those working in those areas and also understanding behaviour change theories. The Five Year Forward View makes it clear that healthcare is diverse and a single model is no longer seen as the approach that will make the biggest impact on health and social care [10]. Using the novel, co-production, multidimensional approach we took resulted in the original resources being significantly redesigned following participants' insights and testing and the publication of a co-designed resource already adapted with the end users involved.
Acknowledgements
Thank you to all those who participated in the workshops and working groups.
Appendix I. Questions used for Stakeholder feedback
| Question |
|---|
| 1. How ‘user-friendly’ are the resources? |
| 2. Do you think these resources might fit into your current working practices? |
| 3. What are the barriers for people using the resources? |
| 4. How could these barriers be overcome? |
| 5. What do you think might encourage people to make use of these resources? |
| 6. What processes (if any) are already in place in your workplace to prevent/reduce/manage E. coli BSI? |
| 7. Could any of the processes or resources you already use for IPC be of use to inform the development of this resource? If so, how? |
References
- 1.Department of Health . Department of Health; England: 2012. Annual Report of the Chief medical officer 2011: volume two. [Google Scholar]
- 2.UK D.H. Department of Health; 2013. Five year antimicrobial resistance Strategy 2013 to 2018. [Google Scholar]
- 3.Reducing infections in the NHS. 2016. [press release] [Google Scholar]
- 4.WHO . Global Report on Surveillance; Geneva: 2014. Antimicrobial resistance. [Google Scholar]
- 5.O'Neill J. 2016. Tackling drug resistant infections globally: final report amd recommendations. [Google Scholar]
- 6.Global W.H.O. World Health Organization; Geneva, Switzerland: 2015. Action plan on antimicrobial resistance. [Google Scholar]
- 7.Wilcox M.H. The start of another infection prevention learning curve: reducing healthcare-associated Gram-negative bloodstream infections. Journal of Hospital Infection. 2017;97(3):205–206. doi: 10.1016/j.jhin.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Abernethy J., Guy R., Sheridan E.A., Hopkins S., Kiernan M., Wilcox M.H. Epidemiology of Escherichia coli bacteraemia in England: results of an enhanced sentinel surveillance programme. Journal of Hospital Infection. 2017;95(4):365–375. doi: 10.1016/j.jhin.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Public Health England . Healthcare associated infection and antimicrobial resistance department. 2018. Annual Epidemiological Commentary Mandatory MRSA, MSSA and E.coli bacteraemia and C.difficile infection data 2016/17. [Google Scholar]
- 10.National Health Service . Five Year Forward View. In: Service N.H., editor. National Health Service (NHS); 2014. [Google Scholar]
- 11.Webb TLaS P. Does Changing Behavioural Intentions Engender Behaviour Change? A Meta-Analysis of the Experimental Evidence. Psychological Bulletin. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 12.Filipe A., Renedo A., Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLOS Biology. 2017;15(5) doi: 10.1371/journal.pbio.2001403. e2001403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NHS Improvement. Driver Diagrams 2018 [Available from: https://improvement.nhs.uk/resources/driver-diagrams-tree-diagrams/.
- 14.Michie S., van Stralen M., West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science. 2011;6(42):2–11. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molloy GJaOB C.A. The SHEL model: a useful tool for analyzing and teaching the contribution of Human Factors to medical error. Academic Medicine. 2005;80(2):152–155. doi: 10.1097/00001888-200502000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Service O., Hallsworth M., Halpern D., Algate F., Gallagher R., Nguyen S. partnership with the Cabinet Office; 2014. EAST; Four simple ways to apply behavioural insights. [Google Scholar]
- 17.Deming W.E. MIT Center for Advanced Engineering Study.; 1986. Out of the crisis. [Google Scholar]
- 18.Health Education England . 2017. Quality improvement education and training. [Google Scholar]