Abstract
Health care providers are increasingly screening low-income patients for social needs and making referrals to social service agencies to assist in resolving them. A major assumption of this approach is that local social service providers have the capacity and resources to help. To explore this assumption, we examined 711,613 requests for 50 different social needs received from callers to 2-1-1 helplines in seven states during 2018. Analyses focused on the proportion of requests for which referrals could not be made due to low capacity in the social service system. We examined the extent to which social service system capacity varied by type of social need, ZIP code and time, and classified social needs in a new typology based on prevalence and system capacity. What emerges is a clear picture that health care’s current screening and referral approach is appropriate for some social needs but not others.
Introduction
It is well established that having unmet social needs like housing, food, child care, safety, transportation and financial resources is associated with a range of adverse health outcomes, including stress, sleep disturbances, physical and mental health problems, cognitive decline and mortality.[1–5] Unmet social needs are also associated with lower likelihood of engaging in health-promoting behaviors, managing chronic diseases, keeping health care appointments and using medication as prescribed, as well as lower self-rated health, fewer healthy days and higher health care costs.[1, 6–8]
There is now great interest across the health care sector in assessing and addressing social needs in low-income patients, and determining the effects of social needs interventions on health improvement, costs and utilization.[9–11] A recent review found that such interventions tended to have positive impacts on social needs, although evidence for health improvement was mixed, mainly due to varying quality of some of the studies considered.[12] “Linkage interventions” that aim to connect people to needed social services in their community through one-time referrals or ongoing case management are currently the most common approaches for addressing social needs. Models for providing these referrals include clinic-based interactions, proactive outreach outside of clinical appointments and community resource referral platforms.[13] A 2017 survey of Medicaid Managed Care Plans found that 91% reported assessing social needs among members and 93% linked members to social services.[14]
A key assumption of linkage interventions is that existing social service agencies have sufficient capacity to address the social needs in their communities. This is especially important because proactive and systematic screening will likely increase the number of people seeking assistance from social service agencies. To date, there have been no published data describing social service system capacity – broadly conceived as the amount of assistance a community can produce to address social needs – against which to check this assumption. This study provides the first such evidence, examining ZIP code level system capacity for 50 social needs in Missouri, and comparing the pattern of results with similar data from Alabama, Connecticut, Iowa, Minnesota, Nebraska and Nevada.
Analyses seek to: (1) describe how system capacity varies by type of social need, geographically, and seasonally over a 12-month period; (2) integrate system capacity data with social needs prevalence data to understand how the two intersect; and (3) compare patterns of system capacity for a subset of social needs across seven states to assess generalizability. The implications of these data for planning and delivering social needs interventions in health care are discussed.
Methods
Data source
All data analyzed in the study were collected by 2-1-1 helplines, which provide free information and referral services through more than 200 call centers covering all 50 states. Nationally, 2-1-1s made over 12.8 million referrals in 2018.[15] Most callers to 2-1-1 are seeking assistance with social needs like housing, utility bill payments and food.[16] Callers are disproportionately low-income women with children.
Live operators field all phone calls and record callers’ service requests using an extensive taxonomy of over 10,000 categories and sub-categories.[17] Requests are time and date-stamped and linked to the caller’s ZIP code. 2-1-1 operators then provide up to three referrals to community agencies for each social need the caller reported. In some instances, no referral can be provided because: (1) there are no agencies that both provide a needed service and serve the caller’s ZIP code; or (2) the agencies that do provide the needed service and serve the caller’s ZIP code currently have no resources available. In these instances, the caller’s request is coded by 2-1-1 as “unmet”. When the operator can provide a referral, the requests are coded as “met”. Because the research team cannot link data back to individual callers, the study was not considered human subjects research and no IRB review was required.
Using the 2-1-1 Counts classification system,[18] we collapsed the taxonomy of 10,000+ need categories into 13 top level categories (housing and shelter, food, utilities, healthcare, mental health and addictions, employment and income, clothing and household, childcare and parenting, government and legal, transportation, education, disaster, and other) and 115 sub-categories. For example, the top-level category of “housing and shelter” contains sub-categories for requests related to shelters, low-cost housing, home repair, rent assistance, mortgage assistance and landlord/tenant issues. We selected 50 of these sub-categories for analysis in this study, representing a range of needs with higher and lower prevalence. Because not all 2-1-1s code callers’ requests at the same level of detail (e.g., recording “utilities” without specifying electric, gas or water), some 2-1-1s have data on fewer than 50 sub-categories.
Data were collected for the entire calendar year of 2018. In Missouri, this included 181,418 service requests in all 50 social need categories. The other states were Alabama (47,292 requests in 45 of 50 categories) Connecticut (257,586; 49/50), Iowa (41,894; 44/50), Minnesota (87,615; 49/50), Nebraska (17,825; 43/50) and Nevada (77,983; 47/50). These states were selected because all coded callers’ social needs requests as met or unmet for the entire year and had sufficient call volume to calculate reasonably stable rates across a range of social needs.
Although 2-1-1 data on social needs service requests and unmet needs are easily the most timely, specific and comprehensive available in the U.S., two limitations of these data must be acknowledged. First, they capture the needs of only those individuals who call 2-1-1. This is almost certainly an underestimation of population risk, because some individuals with unmet social needs may not call 2-1-1, and even those who do call may not enumerate every need they are experiencing, but only the most acute among them. Moreover, 2-1-1 is not the only helpline in many communities. For example, for certain social needs (e.g., crisis intervention, gambling addiction) and certain populations (e.g., seniors, veterans), some communities also have specialized helpline services.
Second, because each 2-1-1 operates independently, there may be some variability in coding the calls they receive. For example, three of the seven states in our analysis did not distinguish between different types of utility bill assistance, whereas the remaining states coded separately for electric, gas and water bills. We don’t know whether there is similar variability in how 2-1-1s code “met” and “unmet” social need service requests.
Variables
Analyses focused on prevalence of social needs and system capacity, by time and ZIP code.
Prevalence of social needs.
For each of the 50 social needs, we summed the number of 2-1-1 service requests received in 2018 in each state and converted this to a rate of requests per 100,000 population using each state’s 2018 adult population. In Missouri, we also created rates of requests for each ZIP code.
System capacity.
For each of the 50 social needs in each state (and ZIP code, in Missouri), we divided total 2-1-1 requests in 2018 into total requests classified by 2-1-1 as “met”, yielding a system capacity score representing the proportion of 2018 requests to which the local social service system theoretically had capacity to respond. For example, if 2-1-1 received 100 requests for clothing in ZIP code 63112 and 80 of those were classified as met, system capacity for clothing assistance in 63112 would be 80%. System capacity values therefore range from 0 (lowest capacity) to 100% (highest).
We strongly emphasize that system capacity as measured in this study is not the same as actually receiving assistance. When 2-1-1s classify a request as “met” or “unmet”, it only means that a referral to a community organization could be provided (“met”) or could not be provided (“unmet”). Thus, a system capacity score of 80% does not mean that 80% of people with a particular need will receive assistance. Research suggests that aggregating across all types of needs, just over 1 in 3 will receive assistance.[19] Many others who contact service agencies find no resources available or learn that they do not qualify for assistance. For example, individuals may only be eligible to receive assistance once per year for a given service, or resources may only be available to members of certain groups (e.g., veterans, seniors). Our system capacity scores thus represent the upper limit of the proportion of callers who might receive assistance from a referral; the proportion who actually receive assistance is likely much, much lower.
For mapping, we divided system capacity into four levels (0–25%; 26–50%; 51–75%; 76–100%) to make patterns of geographic distribution easily recognizable.
Analyses
System capacity and number of requests for each social need were totaled and are reported as descriptive data.
We mapped system capacity in Missouri by ZIP code for each of the 50 social needs using ArcGIS.[20] We explored potential seasonality in statewide (MO) system capacity by examining month-to-month changes during 2018 for each social need, and plotting differences between the highest and lowest monthly scores.
To examine patterns of association between the prevalence of each social need and the system capacity to address it statewide in MO, we plotted the 50 social needs along intersecting axes of prevalence and capacity.
Because several social needs were far more prevalent than others, the distribution of social need requests was highly right skewed. We therefore used a natural log transformation on prevalence data to reduce skewness. The distribution of system capacity scores was moderately skewed in the opposite direction, so we took the square of system capacity to normalize the distribution. These transformations allowed us to plot prevalence of need and system capacity for different social needs into visually clear and conceptually meaningful quadrants.
We then explored the consistency of these plot locations using 2018 2-1-1 data from six other states to examine the relative position of social needs across states in a prevalence-by-capacity matrix.
Findings
System capacity varies by social need
Exhibit 1 shows 25 of the 50 social needs, selected because each ranked highly within in its top-level category and received at least two requests per day on average in Missouri in 2018. System capacity was highest (over 90%) for needs like food pantries and tax preparation, and lowest for needs like rent assistance (39%) and automobile assistance (26%).
Exhibit 1.
System capacity to address 25 social needs in Missouri, 2018.
| Social need | System capacity | Total requests |
|---|---|---|
| Food pantries | 92% | 9,775 |
| Tax preparation | 91% | 4,785 |
| Crisis intervention & suicide | 90% | 935 |
| Health insurance | 88% | 1,509 |
| Legal assistance | 88% | 2,130 |
| Job search | 87% | 2,419 |
| Gas | 86% | 19,625 |
| Electric | 86% | 39,151 |
| Water | 86% | 7,562 |
| Prescription medications | 84% | 1,526 |
| Mental health services | 83% | 1,110 |
| Help buying food | 81% | 1,117 |
| Clothing | 80% | 3,436 |
| Substance abuse & addictions | 80% | 1,388 |
| Child care | 79% | 744 |
| Dental care | 75% | 1,436 |
| Shelters | 69% | 11,693 |
| Holiday meals | 68% | 1,999 |
| Low-cost housing | 67% | 10,192 |
| Home furnishings | 57% | 5,699 |
| Financial assistance | 57% | 1,244 |
| Public transportation | 46% | 2,771 |
| Rent assistance | 39% | 24,922 |
| Appliances | 33% | 2,014 |
| Automobile assistance | 26% | 2,723 |
Source/Notes: SOURCE [211counts.org].
System capacity varies by ZIP code
For many social needs, system capacity varied considerably by ZIP code. Exhibits 2A and 2B, and Online Appendix A† map this variability for the six most frequently requested social needs in Missouri during 2018 (electric bill payments, rent assistance, gas bill payments, shelters, low-cost housing and food pantries). We selected these because the larger the number of requests, the more stable system capacity estimates are at the ZIP code level (analyses considered 1,024 ZIP codes in Missouri). Dark green-shaded ZIP codes had the highest system capacity (76–100%) while red-shaded ZIP codes had the lowest (0–25%). Exhibit 2A, for example, shows that although system capacity is generally high for requests for electric bill payment assistance, it is much lower in several regions of the state (e.g., southeast, southwest).
EXHIBIT 2.
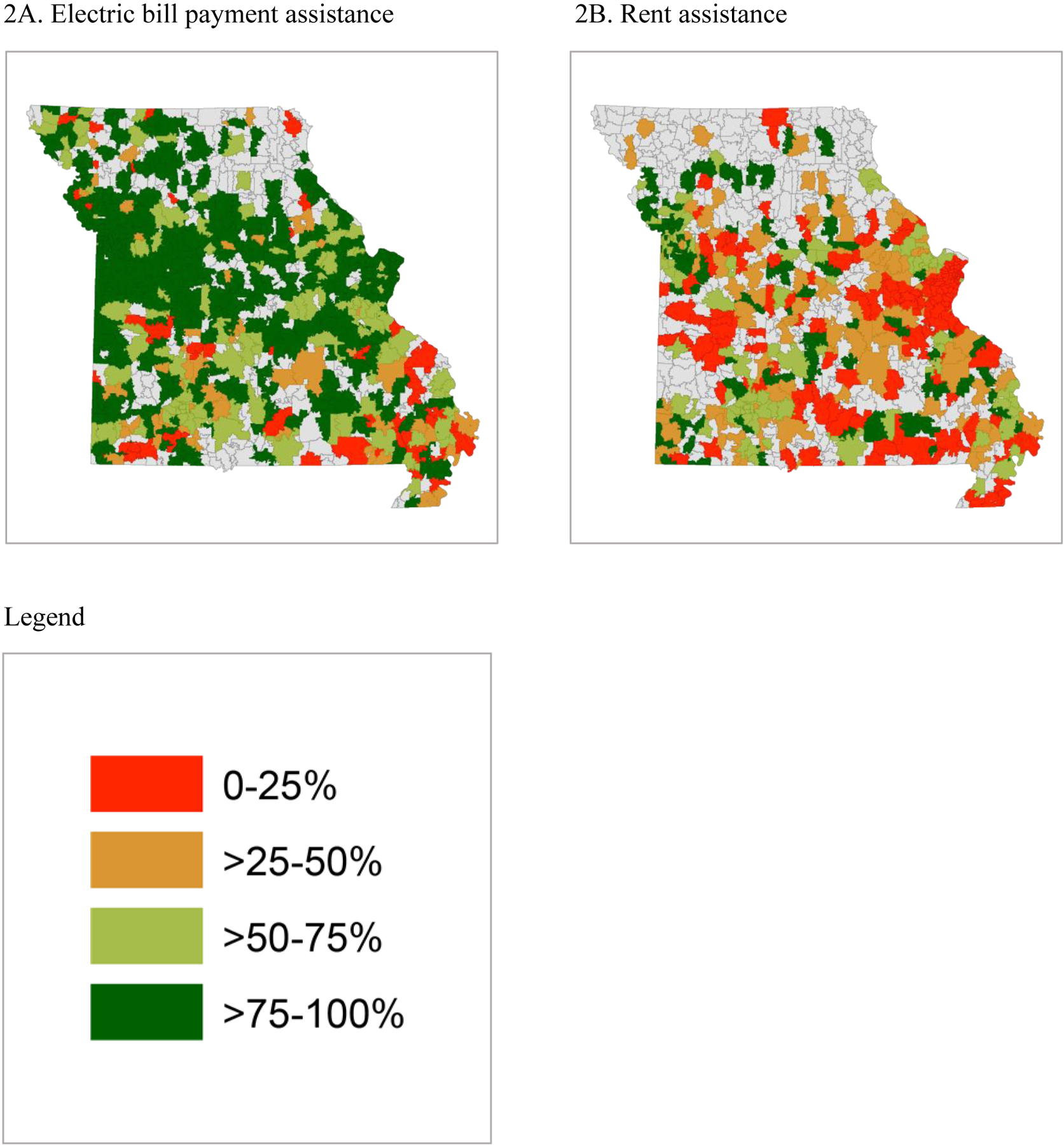
[Variability in system capacity by ZIP code.]
Source/Notes: SOURCE [211counts.org].
Seasonality in system capacity
Exhibit 3 shows the annual system capacity rate and the highest and lowest monthly rates during 2018 in Missouri for the 25 needs described in Exhibit 1. Month-to-month system capacity was very stable for most social needs, and especially so for several high prevalence needs such as food pantries, electric and water bill assistance, job search, and shelters. For example, the difference between the highest and lowest monthly levels of system capacity for food pantries was 89% to 93% and for electric bill assistance was 83% to 88%. Only four social needs had system capacity levels that varied widely from the highest to lowest capacity months: holiday meals (0% to 80%), appliances (6% to 66%), tax preparation (46% to 96%) and financial assistance (43% to 79%). According to 2-1-1 leaders, the first three of these reflect predictable and expected seasonal increases in demand due to Thanksgiving and Christmas, summer needs for window air conditioners and box fans, and tax season, respectively. It is unclear why system capacity for financial assistance requests was higher in winter months and lower in summer months.
EXHIBIT 3.
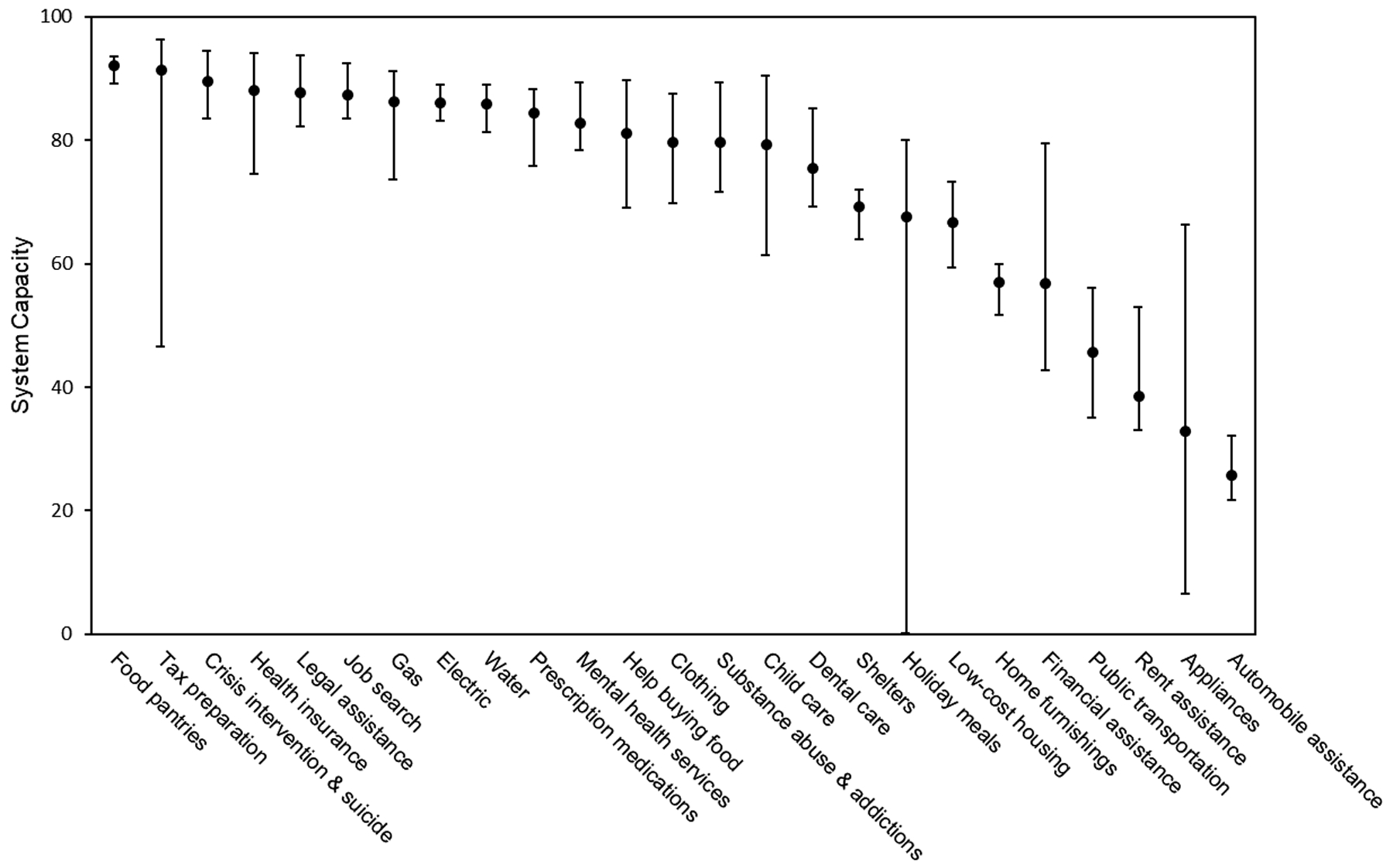
[System capacity rate and range from highest to lowest month, Missouri, 2018.]
Source/Notes: SOURCE [211counts.org].
Social need prevalence by system capacity matrix
Exhibit 4 shows how the 50 social needs are distributed across a 2 × 2 matrix of social need prevalence by system capacity in Missouri. Social needs in the upper right quadrant (higher prevalence, higher capacity) include food pantries, electric bill payments, legal assistance, job search and clothing. The lower right quadrant (higher prevalence, lower capacity) includes rent and mortgage assistance, home furnishings, appliances, public transportation and automobile assistance.
EXHIBIT 4.
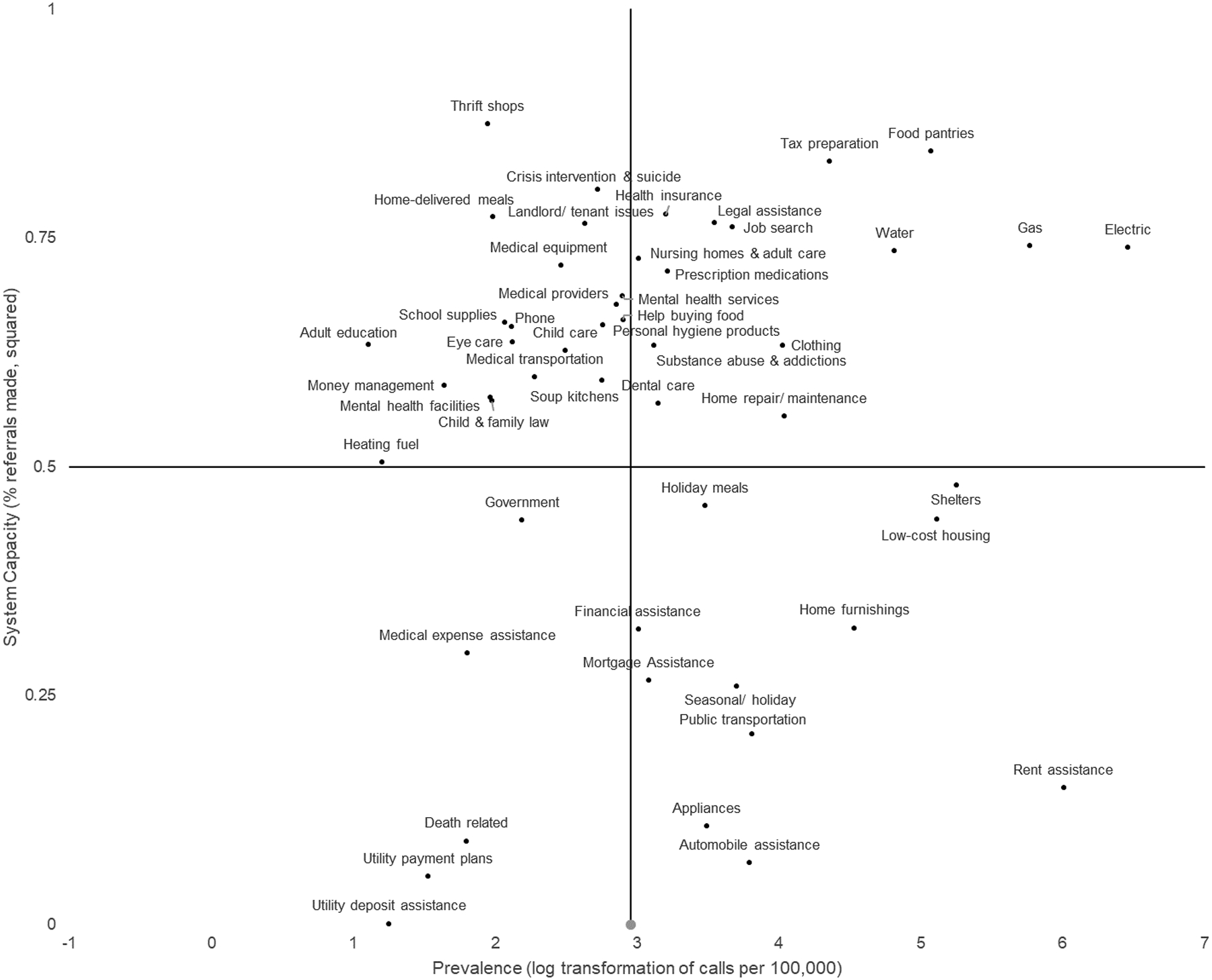
[Prevalence and system capacity for 50 social needs, Missouri, 2018.]
Source/Notes: SOURCE [211counts.org, United States Census Bureau].
The lower left quadrant (lower prevalence, lower capacity) includes death-related and utility deposit assistance, and the upper left quadrant (lower prevalence, higher capacity) includes child care, home delivered meals and crisis intervention and suicide.
Consistency of matrix locations across seven states
For 32 of the 50 social needs, the matrix location was similar across states. As examples, Online Appendix B† (panels 1–3) show the distributions for food pantries, child care and automobile assistance. Food pantry requests from the seven states were tightly clustered in the high need, high capacity quadrant (Panel 1); child care requests were less prevalent but still had relatively high capacity (Panel 2); automobile assistance requests were about as prevalent as child care requests, but with much lower capacity (Panel 3).
Other social needs that clustered similarly across states included adult education, child and family law, clothing, dental care, eye care, gas utility payments, government, health insurance, help buying food, home-delivered meals, home repair and maintenance, job search, landlord/tenant issues, legal assistance, low-cost housing, medical equipment, medical providers, medical transportation, mental health facilities, money management, nursing homes and adult care, personal hygiene products, prescription medication, public transportation, shelters, soup kitchens, substance abuse and addictions, tax preparation and thrift shops.
For other social needs, prevalence was consistent across states but capacity varied, or vice versa. For example, requests for rent assistance (Panel 4) were universally high in prevalence, but the capacity to address them varied by state, from a high of 94% to a low of 19%. Other social needs sharing this pattern included death-related expenses, home furnishings, medical expense assistance, mortgage assistance, phone utility payments, school supplies, seasonal/ holiday, utility deposit assistance and utility payment plans.
Social needs that varied in prevalence but shared similar capacity included electric utility payments, mental health services and crisis intervention and suicide. Finally, some social needs such as heating fuel (Panel 5) varied across states on both prevalence and capacity; other needs with this profile included appliances, financial assistance, holiday meals and water utility payments.
Discussion
This paper presents the first published data on capacity of local social service systems to respond to community members’ social needs. We found that system capacity can vary widely for different social needs, by state, and by ZIP codes within a state, raising important questions about possible limitations of linkage interventions now being widely used by health care organizations.
For example, housing and transportation are among the social needs recommended for screening in health care settings [21–22]. In our study, requests for assistance with these needs was common but capacity to respond to them was moderate or low in nearly all states.
Our findings align closely with those from longitudinal studies tracking the outcomes of social needs referrals in vulnerable populations. Separate studies in Missouri and Oregon found that referrals for food-related needs were the most likely to be met while referrals for housing-related needs were the least likely.[19, 23] In our analyses, system capacity was high for food pantries and much lower for rent assistance, low-cost housing, appliances and home furnishings.
In a worst case scenario, social needs interventions that unwittingly refer vulnerable patients to low capacity social service agencies could create a lose-lose-lose scenario: (1) patients are sent seeking help that largely doesn’t exist; (2) community agencies that are already stretched thin experience increased workloads, often as bearers of bad news to needy individuals; and (3) health care professionals waste precious time, lose credibility and don’t get the outcomes they sought. It’s not clear how likely this “triple blame” of health care and social needs might be. For example, research findings suggest that most patients think it is appropriate and important for their providers to screen for social needs, but many are not interested in receiving social needs referrals and have no expectation that their provider will solve their social needs problems.[24]
Exhibit 4 and Online Appendix B† introduce a proposed Typology of Social Needs for Healthcare Action. We classified social needs into the four quadrants of the 2 × 2 typology based on their prevalence and the system capacity to address them. Each quadrant can be labeled to reflect the broad types of action that might be most appropriate for social needs within it: “screen and refer” (for high prevalence, high capacity social needs); “increase capacity” (high prevalence, low capacity); “consolidate services” (low prevalence, low capacity); and “evaluate priorities” (low prevalence, high capacity).
Social needs classified in the “screen and refer” quadrant included clothing, food pantries, gas utility payments, legal assistance, low-cost housing, health insurance, help buying food, medical providers, shelters and substance abuse and addictions. At least in the seven states studied,they would appear to be good candidates for screen-and-refer linkage interventions as they meet two key criteria for population screening: importance/prevalence and availability of effective treatments[25].
Screening and referral interventions may be ill-advised or inefficient for social needs classified in other quadrants of the typology. Their effectiveness will be limited when system capacity is low, and population screening may be inefficient for very low prevalence needs.
Social needs in these quadrants present a challenge to all who aim to address social determinants of health and individual social needs, not just those in the health care sector. For example, how should communities reconcile that there are high prevalence needs like rent assistance for which little or no assistance exists,[26–27] while resources are widely available to address needs that affect far fewer people? In many communities, the process of allocating resources to address social needs could benefit greatly from such data. Studies evaluating Community Health Needs Assessments, for example, find that social determinants of health are often the least developed component, lacking even basic data to guide decisions.[28–29]
What strategies might be needed to address social needs that don’t currently lend themselves to solution through linkage interventions? For social needs in the “increase capacity” quadrant (high prevalence/low capacity), health care organizations could lead or support efforts to strengthen the community response system. This might include becoming more involved in community decision making about how finite resources are allocated to different social needs, or experimenting with new models such as “pay for success” [30] or using Medicaid funding to address social needs.[31]
Social needs such as death-related services and utility deposit assistance appeared in the “consolidate services” quadrant (low prevalence/low capacity)for several states. The relative dearth of available services for these needs likely reflects, at least in part, lower demand for the services. Services addressing needs in this quadrant might be absorbed by high functioning agencies with relevant core expertise that are looking to expand or partner to address unmet community needs.[32] For example, a utility bill payment program expanding to provide utility deposit assistance.
For many needs in the “evaluate priorities” quadrant (low prevalence/high capacity), the issue is utilitarianism. It seems fair to ask whether community resources might be allocated differently to more closely align with demonstrated needs. This is one of the foundational strategies of Accountable Health Communities.[33] Organizations that fund community services (e.g., United Ways, foundations and philanthropies) could better use social needs data to prioritize funding for some needs over others. Healthcare organizations should be engaged in these discussions at a community level, and where applicable, internally to assure that their own philanthropic and community benefit investments address priority social needs. Because prevalence of some social needs in this quadrant (e.g., crisis/suicide, medical transportation) will be underestimated if people seek help for the need through non-2-1-1 channels (e.g., crisis hotlines, their own health insurer or provider), analyses must be thorough and decisions cautious.
Another important finding with implications for health care is the geographic variability we observed in system capacity. Generally speaking, system capacity was lower in less densely populated regions of Missouri. It is well known within the social service sector that rural communities have fewer agencies and available resources.[34] This poses challenges to rural primary care providers who wish to address social needs using linkage interventions, and suggests that health plans making policy decisions about social needs interventions at a state level should consider how those decisions might exacerbate difficulties already faced in some regions.
In some cases, regional variation may reflect important differences in community investment in certain social needs. For example, the system capacity map for rent assistance (Exhibit 2B) shows dramatic differences between the Kansas City and St. Louis metropolitan areas in Missouri. When shown this map, 2-1-1 leaders examined their resource library and found that as of November 2019, the five largest counties in the St. Louis region had a total of 15 agencies providing rent assistance, 9 of which were currently out of resources. In contrast, on the same day, the four largest counties in the Kansas City region had 37 agencies providing rent assistance, only two of which were out of resources.
Some health care organizations may hedge against limited system capacity by assigning case managers to high need or high cost patients to increase the odds that those patients receive assistance. Although this might help selected individuals, it could have the unintended consequence of creating tiers of privilege within the social service safety net, disproportionately allocating limited public resources to low-income individuals with the worst health problems, best health care or best insurance.
As the evidence linking social needs and population health outcomes grows, it will be crucial to develop multi-sector collaborations and advocate for policies that expand social service resources at local, state, or federal levels, and/or require data-informed allocation of existing resources.[11, 35] In Missouri, for example, the Missouri Foundation for Health has developed The Net Benefit, a nonpartisan campaign to build support for social safety net services by educating Missourians about how meeting social needs can help improve population health.[36]
We recognize that there are likely differences between people who call 2-1-1 and people who are screened in primary care settings. 2-1-1 callers are actively seeking help with social needs while most primary care patients are not. Thus the social needs experiences of 2-1-1 callers and their willingness to accept assistance could be different from that of a primary care patient population. We cannot infer that 2-1-1 data from Missouri (or the other six states included in our analyses) are representative of data from 2-1-1s in other states, nor is it known whether the geographic or temporal distribution of the social needs reported here might be different for those who do not contact 2-1-1 for assistance, or contact a different helpline.
Conclusions
Current approaches to addressing social needs in low-SES patients are likely undermined in many communities by limited capacity in the social service system. This may be especially problematic for certain high prevalence needs, including many related to housing and transportation. Linkage approaches that rely on screening and referral to community agencies will need to be supplemented with alternative strategies including direct provision of social needs resources by health plans, community-wide evaluation of priority social needs on the basis of local data from 2-1-1s and other sources, and policy proposals to expand the availability of resources.
Supplementary Material
References
- 1.Thompson T, McQueen A, Croston M, Luke A, Caito N, Quinn K, et al. Social needs and health-related outcomes among Medicaid beneficiaries. Health Educ Behav. 2019;46:436–44. [DOI] [PubMed] [Google Scholar]
- 2.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Long-term neighborhood effects on low-income families: Evidence from moving to opportunity. Am Econ Rev. 2013;103:226–231. [Google Scholar]
- 4.Grandner M, Petrov M, Rattanaumpawan P, Jakcon N, Platt A, Patel N. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9:897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blazer D, Sachs-Ericsson N, Hybels C. Perception of unmet basic needs as a predictor of mortality among community-dwelling older adults. Am J Public Health. 2005;95:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzpatrick T, Rosella L, Calzavara A, Petch J, Pinto AD, Manson H, et al. Looking Beyond Income and Education: Socioeconomic Status Gradients Among Future High-Cost Users of Health Care. Am J Prev Med. 2015;49:161–171. [DOI] [PubMed] [Google Scholar]
- 7.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36:3093–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seligman H, Davis T, Schillinger D, Wolf M. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21:1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andermann A Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fierman A, Beck A, Chung E, Tschudy MM, Coker TR, Mistry KB, et al. Redesigning health care practices to address childhood poverty. Acad Pediatr. 2016;16:S136–S146. [DOI] [PubMed] [Google Scholar]
- 11.Alderwick HA, Gottlieb LM, Fichtenberg CM, Adler NE. Social prescribing in the US and England: emerging interventions to address patients’ social needs. Am J Prev Med. 2018;54:715–8. [DOI] [PubMed] [Google Scholar]
- 12.Gottlieb L, Ackerman S, Wing H, Adler N. Evaluation activities and influences at the intersection of medical and social services. J Health Care Poor Underserved. 2017;28:931–951. [DOI] [PubMed] [Google Scholar]
- 13.Cartier Y, Fichtenberg C, Gottlieb L. Community Resource Referral Platforms: A Guide for Health Care Organizations [Internet]. San Francisco, CA: SIREN; [cited 2019 July 24]. Available from: https://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/wysiwyg/Community-Resource-Referral-Platforms-Executive-Summary-1.pdf. [Google Scholar]
- 14.Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. 2018. May 10 [cited 2018 Dec 9]. Kaiser Family Foundation Issue Brief [Internet]. Available from: https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/. [Google Scholar]
- 15.2-1-1.org [Internet]. 2018. 211 Impact [cited 2019 July 2]. Available from: http://211.org/pages/about.
- 16.Thompson T, Kreuter MW, Boyum S. Promoting health by addressing basic needs: Effect of problem resolution on contacting health referrals. Health Educ Behav. 2016;43:201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.2-1-1 L.A. [Internet]. County Taxonomy of Human Services. 2004–2019. Information and Referral Federation of Los Angeles County, doing business as 211 LA County. Version 5.8.5. [cited 2019 July 24]. Available from: https://211taxonomy.org.
- 18. [2019 June 20];2-1-1 Counts [Internet]. About the data. [cited. ]. Available from: https://211counts.org/home/index.
- 19.Boyum S, Kreuter MW, McQueen A, Thompson T, Greer R. Getting help from 2-1-1: a statewide study of referral outcomes. J Soc Serv Res. 2016;42:402–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ArcGIS. Version 10.5.1 [software]. Redlands,CA: Environmental Systems Research Institute. 2017. [cited 2019 July 24]. [Google Scholar]
- 21.Social Interventions Research & Evaluation Network [Internet]. Social needs screening tools comparison table. San Francisco, CA: SIREN; [cited 2019 July 18]. Available from: https://sirenetwork.ucsf.edu/tools-resources/mmi/screening-tools-comparison/adult-nonspecific. [Google Scholar]
- 22.Olson DP, Oldfield BJ, Navarro SM. Standardizing Social Determinants of Health Assessments. 2019. March 18 [cited 2019 July 18]. Health Affairs Blog [Internet]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20190311.823116/full/. [Google Scholar]
- 23.Saxton ML, Naumer CM, Fisher KE. 2-1-1 Information services: Outcomes assessment, benefit–cost analysis, and policy issues. Gov Inf Q. 2007;24:186–215. [Google Scholar]
- 24.DeMarchis E, Byhoff E, Fichtenberg C. Acceptability of social risk screening to patients and caregivers. 2019. June 20 [cited 2019 Nov 7]. Presented at Social Interventions Research & Evaluation Network [Webinar]. Available from: https://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/PatientAcceptibilityWebinar.pdf [Google Scholar]
- 25.Wilson JMG, Jungner G. Principles and practice of screening for disease [Internet]. Geneva: WHO;1968. [cited 2019 July 24]. Available from: http://apps.who.int/iris/bitstream/10665/37650/17/WHO_PHP_34.pdf. [Google Scholar]
- 26.Center on Budget and Policy Priorities. United States Federal Rental Assistance Fact Sheet [Internet]. 2019. May 14 [cited 2019 Nov 7]. Available at: https://apps.cbpp.org/4-3-19hous/PDF/4-3-19hous-factsheet-us.pdf.
- 27.Urban Institute. Trends in Housing Problems and Federal Housing Assistance [Internet]. 2017. [cited 2019 Nov 7]. Available from: https://www.urban.org/sites/default/files/publication/94146/trends-in-housing-problems-and-federal-housing-assistance.pdf.
- 28.Pennel C, McLeroy K, Burdine J, Matarrita-Cascante D. Nonprofit hospitals’ approach to community health needs assessment. Am J Public Health. 2015;105:e103–e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gruber JB, Wang W, Quittner A, Salyakina D, McCafferty-Fernandez J. Utilizing Community Health Needs Assessments (CHNAs) in Nonprofit Hospitals to Guide Population-Centered Outcomes Research for Pediatric Patients: New Recommendations for CHNA Reporting. Popul Health Manag. 2019;22(1):25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galloway I Using pay-for-success to increase investment in the nonmedical determinants of health. Health Aff. 2014;33:1897–904. [DOI] [PubMed] [Google Scholar]
- 31.Hinton E, Artiga S, Musumeci M, Rudowitz R. A first look at North Carolina’s Section 1115 Medicaid waiver’s Health Opportunities Pilots. 2019. May 15 [cited 2019 July 18]. Kaiser Family Foundation Issue Brief [Internet]. Available from: https://www.kff.org/report-section/a-first-look-at-north-carolinas-section-1115-medicaid-waivers-healthy-opportunities-pilots-issue-brief/. [Google Scholar]
- 32.Alexander J Adaptive strategies of nonprofit human service organizations in an era of devolution and new public management. Nonprofit Manag Leadersh. 2000;10:287–303. [Google Scholar]
- 33.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities - addressing social needs through medicare and medicaid. N Eng J Med. 2016;374:8–11. [DOI] [PubMed] [Google Scholar]
- 34.Belanger K, Stone W. The social service divide: Service availability and accessibility in rural versus urban counties and impact on child welfare outcomes. Child Welfare. 2008. July 1;87(4):101. [PubMed] [Google Scholar]
- 35.Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. 2019. January 16 [cited 2019 July 24]. Health Affairs Blog [Internet]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20190115.234942/full/ [Google Scholar]
- 36.Missouri Foundation for Health [Internet]. Meeting our basic needs: The Net Benefit [cited 2019 July 18]. Available from: https://mffh.org/our-focus/the-net-benefit/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


