Introduction
Facility-based births with skilled attendants increased significantly in the past decade, yet global maternal mortality rates did not decline as rapidly as anticipated. Achieving the sustainable development goals for maternal and newborn health—which includes a two-third reduction in maternal mortality by 20301—requires ensuring timely access to quality, proven critical health interventions and innovative facilitators to bridge health system barriers, particularly in rural or limited resource settings.2
Digital technology is a promising option to overcome these barriers to achieving and maintaining high-quality care standards.3–7 Numerous digital tools have been introduced within the continuum of maternity care;5 8 however, a significant opportunity remained to systematically develop and test a design hypothesis for a technology-based solution that included a focus on the 24-hour labour and delivery period, which is when quality care has the highest potential to save lives.9 In response to this need, a human-centred design (HCD) process was undertaken to inform development of iDeliver. Users indicated a need for a mobile, digital, point-of-care tool that would improve skilled birth attendants (SBAs) access to information in clinical settings to guide decisions and ensure timely and appropriate interventions in real time.
The tool was intended to support consistent evidence-based practices; enable detailed record keeping on the content of care from admission to discharge by capturing diagnosis and treatment data; streamline reporting processes, by linking facility and government health information systems, supporting integration and avoiding duplication; provide tools for routine quality measurement and monitoring and inform sustainable quality improvement (QI) efforts at facility, district and national levels.
A unique set of partners was convened by MSD for Mothers to collaborate on iDeliver development: clinical, public health and digital health experts from Johns Hopkins Bloomberg School of Public Health (JHSPH); the health service delivery human-centred design firm Scope (formerly M4ID) and VecnaCares, a Massachusetts-based technology non-governmental organization. The team worked closely with end users in Kenya to create a solution that would complement and enhance their work and that was easy to learn and to use. A focus on an intuitive software interface provided easy access to relevant, comprehensive clinical content at the point and time of care. This paper shares lessons learnt from the team’s experience designing, developing and implementing the iDeliver tool in several test facilities in Kenya and includes valuable insights for other implementers applicable to digital health endeavours pursued in similar contexts.
Using a human-centred design approach for the discovery phase
To create iDeliver, the team adopted a human-centred design approach. Aligned with the Principles for Digital Development, it uses qualitative enquiry to better understand the context, and how technological solutions may function for providers to modify the advantages and hindrances to providing quality obstetric care. Users and stakeholders were directly engaged from the start and at key points during development and deployment. Scope designed and implemented formative research in 2015 to assess the needs of SBAs and where a digital solution might improve quality intrapartum care. An embedded approach was undertaken—working with partner institutions in India and Kenya to directly observe patient care with their consent and to shadow SBAs working in local and regional hospitals. The team completed more than a dozen observation days in maternity wards, six in India (public and private) and five public facilities in Kenya. Interviews were conducted with providers and administrators. They assessed the needs and barriers to quality care and sought a better understanding of the clinical knowledge and confidence of SBAs working in under-resourced environments. They studied SBA workflows to document obstacles to optimal patient management, and which digital tools may already be in use.
Understanding the end user and how to meet their needs
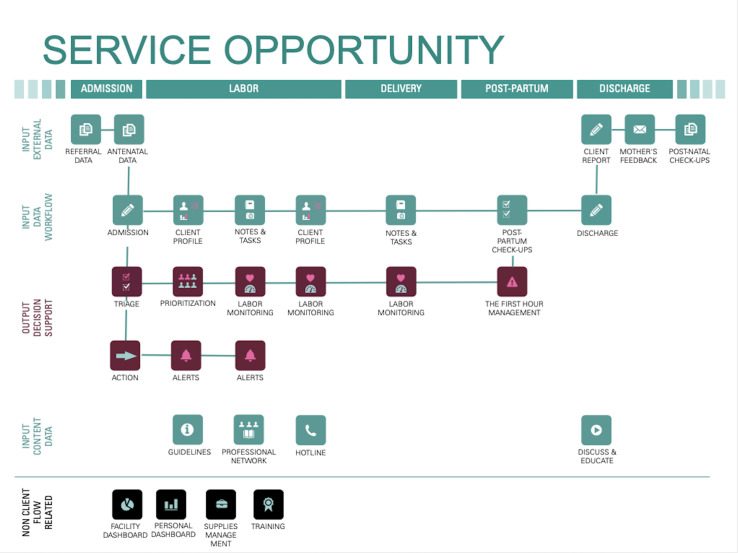
Based on learnings from the field visits, Scope defined different user types and identified specific features and functions in a digital tool that could benefit each.10 Designers drew up a decision-making journey map, illustrating the various care pathways along the pregnancy continuum. They identified key paper-based tools that staff relied on for each stage—admission form, referral letter, medical history record, shift notes, partograph, birth register—and the critical bottlenecks that commonly impeded timely recognition of risk factors and quality care. They created an opportunity map (figure 1) identifying key points at which a digital tool could perform certain functions; the specific challenges each function would solve, and for which type of user; and the clinical content that would be needed for each module.
Figure 1.
Opportunity map identifying key points at which a digital tool could perform functions to address specific challenges and for which type of user, and the clinical content that would be needed to support each module. Source: Scope (2016). iDeliver Design Research and Service Concept. Internal PowerPoint report to MSD for Mothers.
Based on this user feedback, Scope’s design concept recommended that iDeliver offer ways to facilitate and measure quality of care and drive improvements in triage, referrals, admissions and discharge protocols; support patient registration, clinical presentation, identification and initial management of key birth complications, assessment and stabilisation of mother and newborn; and postpartum check-up instructions and family planning counselling. They further proposed that the tool be equipped to manage interactive and multimedia content and connect to a facility-based or cloud-based server for data backup and synchronisation with regional or national health management information systems.
Codesigning and developing the tool alongside its future users
The team chose to focus design, development and implementation activities in Kenya. The project was well aligned with government initiatives in maternal and newborn health.11 In 2017, UN estimates indicate that Kenya’s maternal mortality ratio was still among the highest in the world, at 342 (95% CI (253 to 476)) maternal deaths per 100 000 live births,12 Kenya Ministry of Health reports documented stark inequalities in coverage of critical health interventions across regions, income and education levels and between urban and rural populations.13 Constraints to quality care were contributing factors in 90% of Kenya’s maternal deaths, with delays in treatment, inadequate clinical skills and insufficient monitoring cited as contributing factors in 33%, 28% and 27% of maternal death cases, respectively.14 Poor record keeping was found to play a role in the majority of cases as well.14 It must be noted, however, that all of these influences are heavily impacted by the underlying burdens of understaffing with its associated burnout and fatigue and lack of resources including adequate space, privacy, training and commodities.15 The iDeliver tool was intended to address these primary drivers of maternal mortality: in addition to the clinical guidance, digitising medical and facility administrative records permits easily generated reports on staffing levels and stock outs.
Another advantage to focusing the work in Kenya was that VecnaCares had ready access to ideal sites for testing the tool and gaining user input because of their established presence in public facilities in Transmara West and East subcounties of Narok County. Authorised by the National, County and District Ministries of Health and the Transmara District Health Management team, VecnaCares implemented the CliniPAK system since 2012, which consists of a ruggedised, portable server, which hosts their proprietary CliniPAK Electronic Medical Records (EMR) software and has local network capacity, and intelligent power management system and networking capability. Optimised for use in low resource settings with limited infrastructure—with independent electrical and connectivity—the system is powered by deep cycle batteries or solar panels. Early versions of iDeliver were CliniPAK compatible; developers would later convert iDeliver’s software to an open-source solution, leveraging a digital health Global Good (OpenMRS), to allow for broader EMR system compatibility.
The first round of codesign activities were conducted in 2016 with public health administrators and SBAs—cadres consistent with those in East Africa: nurse-midwives and medical officers who are physicians with extra obstetric care training including caesarean section. Between them, they provide basic and comprehensive emergency obstetric and newborn care and refer when higher levels of care are needed from a specialised obstetrician/gynaecologist. They were either based in a referral facility that offered comprehensive emergency obstetric and newborn services in Transmara West or three mid-level and lower-level facilities that offered basic obstetric care services in Transmara East. The purpose was to gather additional insights into the challenges faced in delivering quality care and to identify opportunities for introducing a technology solution during the normal workflow around labour and delivery.
Opportunities in information management and patient assessment and monitoring processes were noted. Findings from the clinical observations were aggregated, analysed and incorporated into the tool’s technical, clinical and design specifications, ultimately leading to a shift in platform functionality from a standard, linear data-collection platform to a responsive application that better mimicked the continuous but nonlinear flow of information obtained from a patient during childbirth.
To date, four technical innovations are built into the solution:
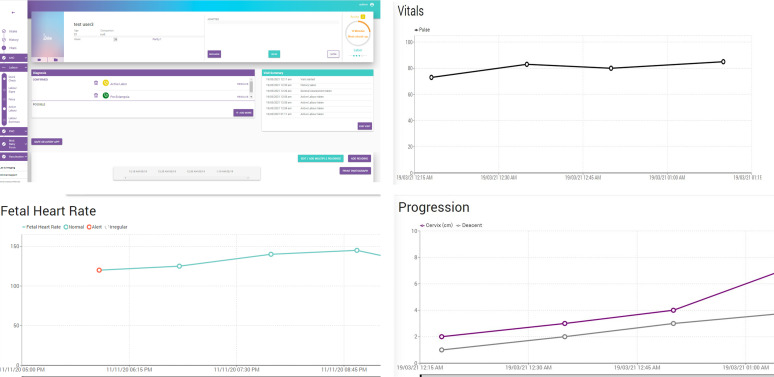
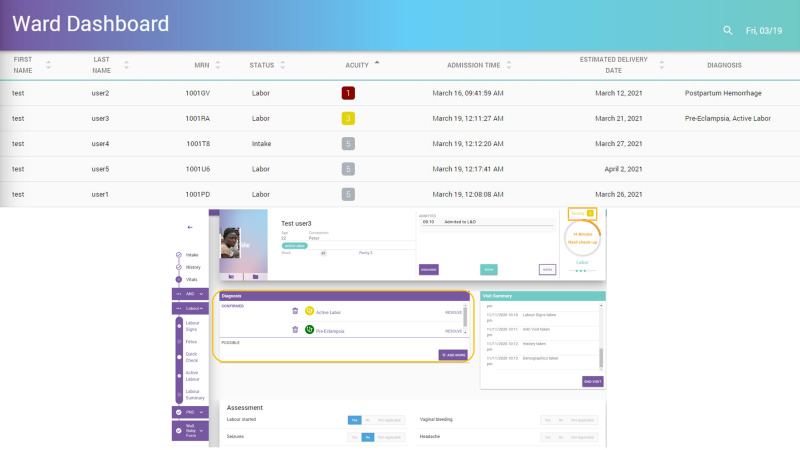
A digital obstetric-specific triage system, which assigns each patient a colour-coded acuity level based on information entered by a health worker—adapted from the Obstetric Triage Acuity Scale16–18 (figures 2 and 3).
A countdown timer, which tracks the minutes before a patient is due for a follow-up assessment.
A digital partograph (figure 2).
A clinical decision support algorithm continuously analyses the patient information entered and assigns a ‘possible diagnosis’ for the provider to review and accept or not (figure 3).
A complication management tool that guides providers through the protocols for responding to the most common life-threatening childbirth complications using clinical content adhering to the most up-to-date WHO guidelines.19
Figure 2.
Screen shots from the iDeliver application: Digital Labour and Delivery Monitoring—iDeliver creates a digital patient medical record including a dynamic, digital partograph.
Figure 3.
Ward dashboard and diagnosis acuity mapping: iDeliver is optimised to supply support for one provider to monitor multiple patients. Diagnoses are assigned a score, which updates the patient’s acuity immediately upon provider confirmation.
Enhancing iDeliver, guided by user feedback
The iDeliver team regularly sought feedback and other input from test users based on their hands-on experiences engaging with the tool, which would then help set priorities for the next phase.
A prototype of the solution was presented in early 2016 to SBAs at Transmara West subcounty hospital, who commented that the tool demonstrated real potential to help them make better, faster decisions during triage, keep better track of the detailed care provided to patients and possibly accelerate a switch to paperless records.
In April 2017, the first tablet version of the tool was deployed for nurse-midwife use in the four Transmara subcounty facilities. Training was provided prior to deployment consisting of 4 hours of small group training followed by 1 week of elbow support, followed by regular support visits by VecnaCares staff and refresher training when needed for software upgrades or staff turnover. SBAs then convened in Kilgoris to provide further clarity about quality of maternity care, to brainstorm additional ideas for how iDeliver may address those issues and potential obstacles to adoption.
A key question during December 2017 workshop with users pertained to whether iDeliver could provide a digital means of monitoring and recording a patient’s labour, essentially eliminating the need for the paper partograph, the limitations of which are well known20 21 and which iDeliver users described as visually helpful yet arduous—requiring meticulous plotting while providing only a narrow view of what constitutes ‘normal’ labour progress. Ultimately, the iDeliver team designed and engineered a labour monitoring tool that more clearly shows the relevant aspects of the partograph including maternal and fetal vital signs and labour progression. The new module’s clinical content reflects findings from the WHO’s better outcomes in labour difficulty initiative22 23 as well as the WHO’s recommendations for intrapartum care for a positive childbirth experience.24
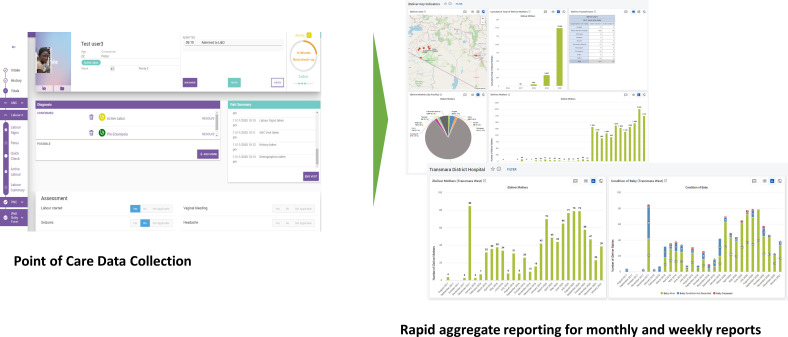
Data recording and reporting capabilities were also incorporated based on user’s described frustration with the time required to comply with hospital record keeping and reporting requirements. Consequently, the scope of patient information collected and stored was expanded, so that at patient discharge, key information could be aggregated and analysed with other anonymised patient data. Other additions based on user feedback included features for faster data entry, such as a picklist of common diagnoses, drop-downs for common responses (eg, blood type) and yes/no toggles; external tablet keyboards to ease typing; and a preloaded template for locally standard nursing notes to reduce typing time. The current version of iDeliver can be locally or cloud hosted. All system features were built keeping facility needs and infrastructure limitations in mind. One of the urban Kenyan facilities used a local server maintained by facility IT, which VecnaCares could connect to for software upgrades. In India, a single cloud-based server is being set up for all the participating facilities. Standard Ministry of Health reports are built within the iDeliver platform and also open-source aggregate reporting tools like DHIS2 (figure 4). The system capabilities to connect to regional or national health management information systems exist, although none are linked to national health management information system as yet.
Figure 4.
Data management: iDeliver collects individual-level data and automatically generates a reporting suite needed for patient records, facility operations and national health system review.
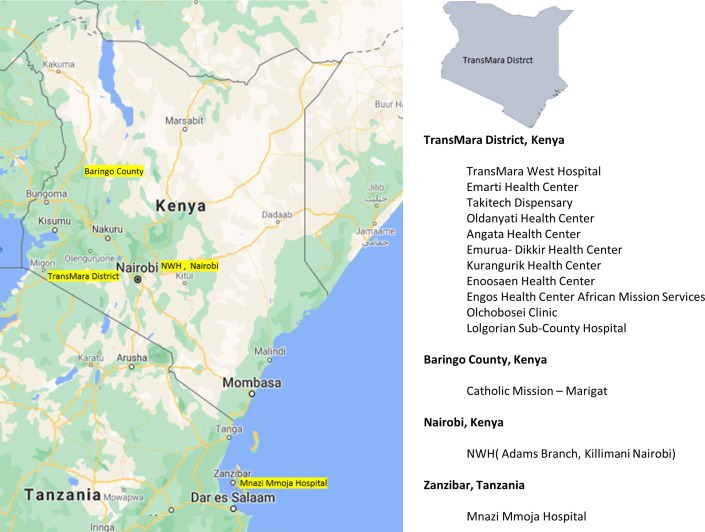
In 2018, new and existing users were trained on an updated version of iDeliver on-site at the four test facilities to allow an observation on how the new capabilities fit into existing workflows and patient care scenarios. Implementation of the tool was expanded, bringing the total number of sites to 10, including Nairobi Women’s Hospital (Adams branch), a private hospital in Nairobi; four additional facilities in Narok County and Mnazi Mmoja Hospital in Zanzibar City, Zanzibar. As of 1 June 2021, iDeliver is deployed in 13 facilities in Kenya and 1 in Zanzibar (figure 5).
Figure 5.
Project implementation area.
Implementation successes and challenges
In 2019, JHSPH hired an obstetrician/gynaecologist and public health consultant based in Nairobi to conduct an internal evaluation of the tool’s usability, acceptance, functionality and effectiveness in Transmara District. The aim was to identify strengths, shortfalls and areas where iDeliver could be improved. Evaluators interviewed 15 providers (2 doctors and 13 nurses) and conducted on-site observations and clinical and technical audits, capturing a mix of process and outcome metrics. An impact assessment is planned for a future evaluation when the number of births registered into iDeliver is sufficient for meaningful statistical analyses.
Evaluators identified three key successes: that iDeliver was easy to learn and easy to use; it improves select aspects of medical record keeping and data storage: and it makes generating reports easier and more efficient. Of the 15 providers interviewed, 8 (53%) cited medical record keeping as the tool’s primary benefit, while 7 out of 15 (47%) cited its educational support—a way for SBAs to stay abreast of global standards and best practices. When asked which functions they particularly liked, half (8 of 15 providers) cited the tool’s medical record keeping function; and half (8) noted its value for quality of care improvement, : especially the application’s ability to triage/provide acuity diagnosis and to automatically plot the partograph.
From an improved skill/knowledge perspective, 9 of the 15 providers interviewed (60%) noted that the application had strengthened their ability to diagnose the patient’s acuity level. The remaining six were unsure if the application had made any difference. The greatest challenge the 15 providers said they faced was the duplication of work due to continuing requirements to maintain paper records. Most said that by adding iDeliver, overall data entry took too long. Less than half of the providers interviewed—6 out of 15 (40%)—reported being able to complete the care recommendations made by the application in the allotted time. All providers cited high patient volume/workloads combined with limited human resources as the main barrier.
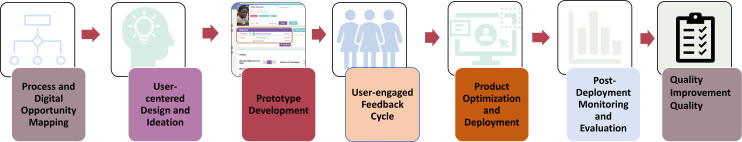
During the next phase of work (figure 6), based on evaluators’, key stakeholders and user recommendations on ways to improve the tool, partners will streamline data input requirements and enhance automated generation of required government reports on number of deliveries and other key health indicators. Partners continue to add in mHealth additional functions.25An interactive version of WHO’s managing complications in pregnancy and childbirth with links to appropriate guidance within complication tabs is available.19 Additional clinical training resources will be added—the MSD for Mothers video library and the Safe Delivery app with its clinical training materials.26 27 iDeliver is also a ready platform to link additional digital technologies, namely, point-of-care diagnostics such as hand-held ultrasound, maternal vital sign monitoring such as automatic blood pressure measures and fetal heart rate monitoring linked directly to iDeliver. Alternate data entry methods such as stylus or dictation could be developed. Partners will also explore how iDeliver’s data capture and reporting capabilities could support broader QI efforts—as a tool for documenting content and process of care, not just outputs and outcomes. Direct client interaction by means of linked health messaging for education or self-reported symptomology of maternal complications are other potential improvements.
Figure 6.
iDeliver project design and development process.
Lessons learnt
In the course of designing, developing and implementing the iDeliver tool, the project team learnt many lessons that are applicable to other digital health projects developed or implemented in the context of a lower or middle-income settings. These include:
The human-centred design approach is essential, promoting local buy-in and ownership
Keeping the user at the centre throughout design and development helped ensure that iDeliver’s content, features and functionality matched the needs and expectations of target users and their supervisors, while respecting the realities of their work environments. Human-centred design uses qualitative methods which MacDonald et al noted is essential to understand the specific setting versus generalisations about low and middle income countries (LMIC) and social and cultural norms around healthcare and use of technology.28 SBA contributions in the design workshops directly influenced design changes and enhancements, which in turn increased users’ willingness to use the tool and encourage others to use it as well. Qualitative engagement should not be limited solely to early steps of intervention design: on-going assessment with the users and beneficiaries enhances the likelihood of successful scale up and sustainability, since the human elements are intricately linked with the digital solution.28 29 Empiric evidence on the impact of HCD on health outcomes is a sparse yet growing field; however, extant data show promising associations between HCD and positive programme interventions.30 Interestingly, input from some female nurse-midwives increased when supervisors (largely male clinicians) were not present—an important consideration for others planning similar design approaches. User comfort with the solution by education level was not assessed, but familiarity with other common digital technologies (computers, smartphones) seemed to enhance easier uptake. Smaller group activities were also useful in encouraging participation and frank feedback.
Be flexible and responsive to the users
Positive feedback regarding ease of use and functional practicality does not guarantee utilisation: clinical decision support during labour and delivery was a frequent request from the providers, yet when implemented, iDeliver could not be used in real time because of the necessity to keep their attention on the mother and baby. Instead of a ‘live’ patient management tool, it was mostly used as a postevent medical record—reflecting also the time constraints in understaffed labour wards that still require paper patient records. However, the clinical guidance built into the tool as well as the aforementioned links to clinical guides can and are used as pedagogical tools for those who want to refresh their clinical knowledge before complicated cases, or after to review their management against global standards of care. To further simplify the clinical guidance, the narrative style was revised to a much simpler linear checklist.
Ensuring appropriate fit with provider workflows is critical to maximise use of a new technology, as are policies mandating use. After iDeliver implementation in the Zanzibar facility in 2017, completing both paper-based and electronic data entry records in parallel was burdensome to the busy nurses, and data incompleteness and difficulty retrieving paper files hindered access to necessary patient records. Facility administrators decided to implement a paperless policy requiring stakeholder and leadership agreement and a dedicated IT team and clinical staff to support iDeliver uptake—resulting in iDeliver birth registration reaching 100% quickly. Being flexible in real time allowed the team to adapt iDeliver for a stronger EMR function—eliminating the time requirements to reconcile paper records with iDeliver. Ministry of Health (MoH) required reports were built in to further save nurses’ time for aggregating and compiling monthly data for reports. Educational support was also included, responsively filling the needs of the providers.
Sufficient development time optimises sustainability of the solution
Five years of development support by the funder with HCD providing a foundation, plus the ‘boots on the ground’ support makes it more likely that iDeliver is a solution that is now part of the landscape: an investment for a sustainable solution and not a ‘quick fix’. iDeliver offers several on-going financial support possibilities; however, for all, the costs will be much more reasonable than if they had to pay for the more costly development phase. In Kenya, implementation will be supported by VecnaCares, while discussions with MoH continue for their contribution to operating costs; in India, a subscription model where the facility administration pay for on-going support by VecnaCares will be used. Furthermore, the fully supported development phase has allowed key users to develop a comprehensive understanding and support of the solution. For example, one of the chief iDeliver physician champions moved from Transmara for a Facility Superintendent position in another district and volunteered to bring the technology to their new facility and train and support the users there—with no request for remuneration.
Providing on-site training and readily available technical support was critical to successful facility implementation
Kenya-based VecnaCares has an office in every implementation locale so users could call for assistance 24/7. Daily support visits were made when new features were introduced and as often as necessary for ad hoc troubleshooting. Maintaining close contact with users also improved the design and implementation team’s understanding of the obstacles to behavioural and practice changes required to drive adoption.
Open source is important for an LMIC digital health solution
Leveraging the OpenMRS platform, a ‘Global Good’ EMR platform that has been adopted in over 60 countries, any developer can access the iDeliver code to amend, add or refine workflows and data elements as needed, and there is flexibility in how the solution can be deployed—as a module operating alongside an existing EMR system, over the cloud to any Linux-based server or hosted locally. Clinical decision logic was encapsulated in a custom OpenMRS module to enable rapid updates, simple expansion into other domains and deployment-specific customisation.
Diversity among partners is an asset
From the start, team members had clear roles and responsibilities that leveraged each unique skill set. As a private-sector partner, the funder provided business, scientific and technical expertise in addition to funding support. VecnaCares brought a long history of technology design and deployment in challenging settings to the table, while Scope introduced engaging and dynamic HCD processes to capture and iterate the prototype iDeliver system. Finally, JHSPH faculty’s clinical, public health and digital health proficiency provided content expertise for the decision support tools and the rigour in monitoring and evaluation to assess use and outcomes.
Conclusion
The iDeliver system is currently in use across 14 facilities in 2 East African countries: (13 in Kenya with more planned deployments, and 1 in Zanzibar) and 1 in India with planned adoption in more urban facilities in several other Indian cities. To date, over 25 000 women have been registered, and by end of 2021, we project that there will be 35 000 deliveries registered in iDeliver.
The system continues to evolve and improve: based on real-time analyses of iDeliver data variability in user engagement, data missingness and other challenges are being addressed through a combination of improvements to the software and to implementation. The team is engaging in implementation research over the coming months with a series of QI activities to strengthen incentives and motivation to increase real-time data entry and bolster the use of iDeliver data for clinical and administrative decision-making. Standardised approaches to monitor system performance and reporting outputs for facility managers are being prioritised in this next phase. Indicators that can provide an accurate measure of the tool’s impact will be generated—from SBA job performance and satisfaction, to the frequency and timeliness of intrapartum interventions, adherence to quality standards and, ultimately, maternal and fetal/newborn health outcomes.31 Efforts will be made to document evidence of that impact, to facilitate broader stakeholder buy-in and expansion within the Kenyan health system and to other contexts where improvements in maternity care are urgently needed. Sharing these findings will also help fill some of the knowledge gaps that exist within the relatively new and still evolving field of digital health.32
Acknowledgments
The authors wish to thank the staff at Transmara West sub-county hospital, the Transmara East and West Sub-county Health Management Team, the Narok County Health Management Team and the Kenya Ministry of Health for their support during this project. The authors would also like to thank Dr. Michael Gravett, Dr. Mercedes Bonet, and Dr. Zahida Qureshi for their Advisory Committee guidance; Dr. Priya Agrawal—Executive Director of Merck for Mothers from 2012 to 2016; Veronica Bluguerman and Melanie Wendland for their design work; Seth Reddy for managing the project during Phase I; and Maryanne Murray Buechner for her editorial support in preparing this article. For more information, please see https://www.vecnacares.org/ideliver.
Footnotes
Contributors: Authors made the following contributions: conceptualisation of iDeliver project goals and aims, LB, AL, MA, PA, MT; funding acquisition, MA, PA, LB, AL; investigation, JuC, JaC; RM, PP, LB, LA; methodology, MT, RM, PA, PP, MR; project administration, PP, JuC, JaC; resources, RM, PP, MR; software programming, MR; supervision/project oversight, MA, PA, PP, LB, AL; validation, LA; visualisation, RM, MT; writing (original draft), LB, MA; writing (review and editing), LB, MA, AL, PA, PP; all authors read and approved the final version of the manuscript.
Funding: This work was supported by Merck & Co., Inc, through the company’s MSD for Mothers initiative, known as Merck for Mothers in the United States and Canada.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.United nations sustainable development goal 3.1: by 2030, reduce the global maternal mortality ratio to less than 70 per 100 000 live births. Available: https://www.who.int/sdg/targets/en/
- 2.Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016;388:2176–92. 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- 3.Ilozumba O, Abejirinde I-OO, Dieleman M, et al. Targeting strategies of mHealth interventions for maternal health in low and middle-income countries: a systematic review protocol. BMJ Open 2018;8:e019345. 10.1136/bmjopen-2017-019345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ayres-de-Campos D, Stones W, Theron G, et al. Affordable and low-maintenance obstetric devices. Int J Gynaecol Obstet 2019;146:25–8. 10.1002/ijgo.12838 [DOI] [PubMed] [Google Scholar]
- 5.Amoakoh HB, Klipstein-Grobusch K, Grobbee DE, et al. Using mobile health to support clinical decision-making to improve maternal and neonatal health outcomes in Ghana: insights of frontline health worker information needs. JMIR Mhealth Uhealth 2019;7:e12879. 10.2196/12879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amoakoh HB, Klipstein-Grobusch K, Amoakoh-Coleman M, et al. The effect of a clinical decision-making mHealth support system on maternal and neonatal mortality and morbidity in Ghana: study protocol for a cluster randomized controlled trial. Trials 2017;18:157. 10.1186/s13063-017-1897-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Matern Child Health J 2012;16:1092–101. 10.1007/s10995-011-0836-3 [DOI] [PubMed] [Google Scholar]
- 8.Sondaal SFV, Browne JL, Amoakoh-Coleman M, et al. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: a systematic review. PLoS One 2016;11:e0154664. 10.1371/journal.pone.0154664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a who systematic analysis. Lancet Glob Health 2014;2:e323–33. 10.1016/S2214-109X(14)70227-X [DOI] [PubMed] [Google Scholar]
- 10.Waugaman A. From principle to practice: implementing the principles for digital development. The principles for digital development Working group, 2018. Available: https://digitalprinciples.org/wp-content/uploads/From_Principle_to_Practice_v5.pdf
- 11.Ministry of Health Kenya . Kenya reproductive, maternal, newborn, child and adolescent health (RMNCAH) investment framework, 2016. https://www.globalfinancingfacilityglobalfinancingfacility.org/kenya-reproductive-maternal-newborn-child-and-adolescent-health-investment-framework [Google Scholar]
- 12.World Health Organization . Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, WorldBank Group and the United Nations Population Division. Geneva: World Health Organization, 2019. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/ [Google Scholar]
- 13.Keats EC. Progress and priorities for reproductive, maternal, newborn, and child health in Kenya: a Countdown to 2015 country case study.. Lancet Glob Health. 2017;5(8):e782-e795.https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(17)30246-2/fulltext 10.1016/S2214-109X(17)30246-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health Kenya . Ministry of health Kenya 2017: saving mothers lives 2017. first Confidential report into maternal deaths in Kenya, 2017. https://cdn2.sph.harvard.edu/wp-content/uploads/sites/32/2018/03/Saving-Mothers-Lives.pdf [Google Scholar]
- 15.Lusambili A, Wisofschi S, Shumba C, et al. Health care workers' perspectives of the influences of Disrespectful maternity care in rural Kenya. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17218218. [Epub ahead of print: 06 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gratton RJ, Bazaracai N, Cameron I, et al. Acuity assessment in obstetrical triage. J Obstet Gynaecol Can 2016;38:125–33. 10.1016/j.jogc.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 17.Smithson DS, Twohey R, Watts N, et al. The impact of standardized acuity assessment and a fast-track on length of stay in obstetric triage: a quality improvement study. J Perinat Neonatal Nurs 2016;34:310–8. 10.1097/JPN.0000000000000193 [DOI] [PubMed] [Google Scholar]
- 18.Smithson DS, Twohey R, Rice T, et al. Implementing an obstetric triage acuity scale: interrater reliability and patient flow analysis. Am J Obstet Gynecol 2013;209:287–93. 10.1016/j.ajog.2013.03.031 [DOI] [PubMed] [Google Scholar]
- 19.Managing complications in pregnancy and childbirth: a guide for midwives and doctors – 2nd ed. Geneva: World Health Organization, 2017. Available: https://apps.who.int/iris/bitstream/handle/10665/255760/9789241565493-eng.pdf?sequence=1&isAllowed=y2
- 20.Lavender T, Hart A, Smyth RMD, et al. Effect of partogram use on outcomes for women in spontaneous labour at term. Cochrane Database Syst Rev 2013;12. 10.1002/14651858.CD005461.pub4 [DOI] [PubMed] [Google Scholar]
- 21.Bedwell C, Levin K, Pett C, et al. A realist review of the partograph: when and how does it work for labour monitoring? BMC Pregnancy Childbirth 2017;17:31. 10.1186/s12884-016-1213-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Souza JP, Oladapo OT, Bohren MA, et al. The development of a simplified, effective, labour Monitoring-to-Action (SELMA) tool for better outcomes in labour difficulty (BOLD): study protocol. Reprod Health 2015;12:49. 10.1186/s12978-015-0029-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oladapo OT, Souza JP, Fawole B, et al. Progression of the first stage of spontaneous labour: a prospective cohort study in two sub-Saharan African countries. PLoS Med 2018;15:e1002492. 10.1371/journal.pmed.1002492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO . Recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization, 2018. https://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/ [PubMed] [Google Scholar]
- 25.Labrique AB, Vasudevan L, Kochi E, et al. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract 2013;1:160–71. 10.9745/GHSP-D-13-00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Safe delivery APP. Available: https://www.maternity.dk/safe-delivery-app/27
- 27.Thomsen CF, Barrie AMF, Boas IM, et al. Health workers' experiences with the safe delivery APP in West Wollega zone, Ethiopia: a qualitative study. Reprod Health 2019;16:50. 10.1186/s12978-019-0725-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MacDonald ME, Diallo GS. Socio-cultural contextual factors that contribute to the uptake of a mobile health intervention to enhance maternal health care in rural Senegal. Reprod Health 2019;16:141. 10.1186/s12978-019-0800-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duclos D, Faye SL, Ndoye T. Envisioning, evaluating and Co-Enacting performance in global health interventions: ethnographic insights from Senegal. Anthropol Action 2019;26:21–30 https://doi-org.proxy1.library.jhu.edu/ [Google Scholar]
- 30.Roy MJ, Donaldson C, Baker R, et al. The potential of social enterprise to enhance health and well-being: a model and systematic review. Soc Sci Med 2014;123:182–93. 10.1016/j.socscimed.2014.07.031 [DOI] [PubMed] [Google Scholar]
- 31.Carter J, Sandall J, Shennan AH, et al. Mobile phone apps for clinical decision support in pregnancy: a scoping review. BMC Med Inform Decis Mak 2019;19:219. 10.1186/s12911-019-0954-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Labrique A, Vasudevan L, Mehl G, et al. Digital health and health systems of the future. Glob Health Sci Pract 2018;6:S1–4. 10.9745/GHSP-D-18-00342 [DOI] [PMC free article] [PubMed] [Google Scholar]