Abstract
After birth, separation of mothers and newborn is a common practice in many hospitals in our country. After delivery, we take the normal newborn to the radiant warmer in the resuscitation area for routine care. This was the existing process of care at our hospital. The frontline delivery team undertook quality improvement initiative to understand and document factors creating challenges in delivering evidence-based practice of providing immediate skin-to-skin care (SSC), delayed cord clamp (DCC) and early breast feeding within 1 hour of birth. Some of the barriers identified were early newborn mother separation and late transfer of mother from delivery room to the observation area. Additionally, there was a challenge of high delivery load with variation in understanding and provision of SSC and drying on mother’s abdomen. These made sustenance of improved care practices difficult. Using the Plan-Do-Study-Act (PDSA) approach some successful change ideas tested were pre-delivery counselling, avoiding separation of mother and newborn at birth by providing SSC and continuing it in the post-delivery observation area and getting family member’s help in first breast feed. The delivery team adapted these successful change ideas by multiple iterations, group discussions and feedback. This resulted in improved and sustained compliance of pre-delivery counselling, SSC, DCC and initiating breast feed within 1 hour, from minimal compliance to a median compliance of 51%, 56%, 59% and 61%, respectively, over 36 months period. We undertook this quality improvement initiative at Delhi (India) at a tertiary care teaching hospital. The implementation of WHO recommended evidence-based practices benefitted more than 10 000 mother–newborn dyads annually over 2 years, using Point of Care Quality Improvement method. Implementation of evidence-based practice is possible in challenging situations using PDSA approach. The resultant contextualised processes are convenient and have better success at sustainability.
Keywords: evidence-based practice, PDSA, compliance, continuous quality improvement
Problem
India has diverse geographical, economic and sociocultural variability along with resource limitation. This makes implementing evidence-based maternal and neonatal care practices difficult. At our hospital, similar challenges lead to continuous pressure on maternal and newborn service delivery. There is also overcrowding and shortage of medics and paramedics. Due to above factors, equity and the quality of services offered is the first casualty.
Our hospital is a public sector tertiary care teaching hospital, catering to an annual delivery load of about 20 000 deliveries. We conduct about 15 000 vaginal deliveries at two labour rooms. The doctors and nurses are posted on rotation basis and the period of posting is variable. In a shift, there are 3–4 nurses on duty. These nurses conduct on average 6–8 vaginal deliveries every 8 hours, at each of the two delivery areas. Additionally, there are about 10–15 expectant and post-delivered mothers in these delivery areas. Nurse to client ratio translates to 1:4. Besides monitoring the expectant mothers to conducting normal deliveries, this team also has to attend to complicated deliveries (ie, preparing them for emergency caesarean section, and monitoring recently delivered mother–newborn dyad for about 6–8 hours in the post-delivery observation area). These nurses also do documentation of treatment records and so on.
Translation of the evidence-based interventions into effective clinical practice is a challenge in this setup. After birth, we usually separate mother and normal newborn to provide routine care to the newborn on the radiant warmer. This causes delay in initiation of first breast feed and accompanied stress to the mother. Before the present study, the delivery team followed process of care, which could be, improved as per the WHO recommended evidence-based practices.1 The challenge was to implement and bring sustainable change in existing process of care. In this study, we describe the improvement in existing process of care for normal deliveries, using Point of Care Quality Improvement (POCQI) methodology by the frontline delivery team.2 Before intervention, the compliance of recommended skin-to-skin care (SSC), delayed cord clamp (DCC) and early initiation of breast feeding (EIBF) within 1 hour of birth was low and not documented. The Quality Improvement (QI) team aimed to improve compliance of above in normal delivery by 50% over a period of 18 months using POCQI methodology.
Background
WHO recommends four essential elements of care at birth, namely (1) immediate and thorough drying, (2) providing SSC, (3) DCC after 1 min and (4) EIBF within 1 hour of birth.3–6
India ranks first in having highest number of newborn deaths in the world.2 Immediate SSC after birth and EIBF are simple and effective methods to improve quality of care after birth. They reduce morbidity and mortality in newborn due to hypothermia and septicaemia.4 5 These practices also reduce postnatal maternal complication of postpartum haemorrhage. Early skin-to-skin contact prevents hypothermia, promotes physiological stability, increases colonisation with protective bacteria and facilitates EIBF within 1 hour.7 DCC decreases the incidence of anaemia in neonate.8
In India, the compliance rate of EIBF is 41.6% of all live births.9 Translation of these evidence-based interventions into effective clinical practice is difficult. Documentation and sharing of learning’s of the present study in sustained implementation of these lifesaving low-cost interventions has the potential of reducing neonatal and maternal morbidity and mortality in low-income and middle-income countries.
Measurement
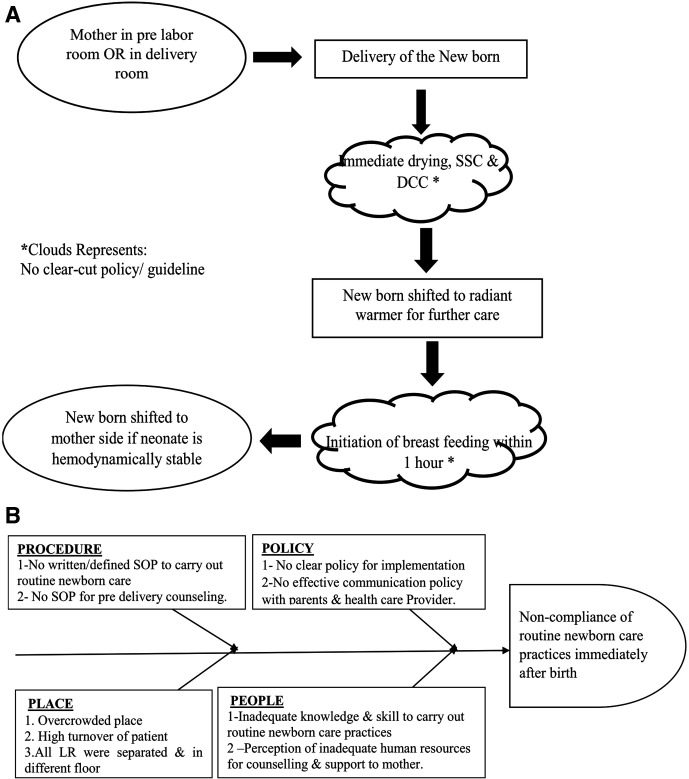
To understand the existing process of care of normal newborn after delivery, the team used process flow chart and fish bone (figure 1). We used following process indicators to monitor and document improvement.
Figure 1.
(A–B) Process flow and fish bone. DCC, delayed cord clamp; LR, labour room; OR, operating room; SOP, Standard Operating Protocol; SSC, skin-to-skin care.
For compliance in providing pre-delivery counselling (PDC), we recorded total delivering mothers counselled before delivery and expressed it as a percentage of total normal vaginal deliveries in the labour room. Compliance to SSC was measured by recording total number of deliveries, where the newborn was dried and kept on mother’s abdomen (immediately after birth) and continued SSC in post-delivery observation room for at least 1 hour after birth. This we expressed as a percentage of all normal vaginal deliveries. We documented DCC, if the nurse clamped and cut umbilical cord at least 1 min after birth. We expressed it as a percentage of total normal vaginal deliveries. EIBF compliance, was calculated by recording number of newborns receiving breast feed within 1 hour of birth and dividing by total number of normal vaginal deliveries. This was expressed as a percentage.
After every delivery, the delivery team were asked to voluntarily record if the processes of PDC, providing SSC, DCC and EIBF, were provided by them. We added four separate columns to the labour room register with one additional column for recording their voluntary feedback, comments, if any.
For this study, we, defined normal vaginal delivery as a delivery where both newborn and mother had normal outcome.
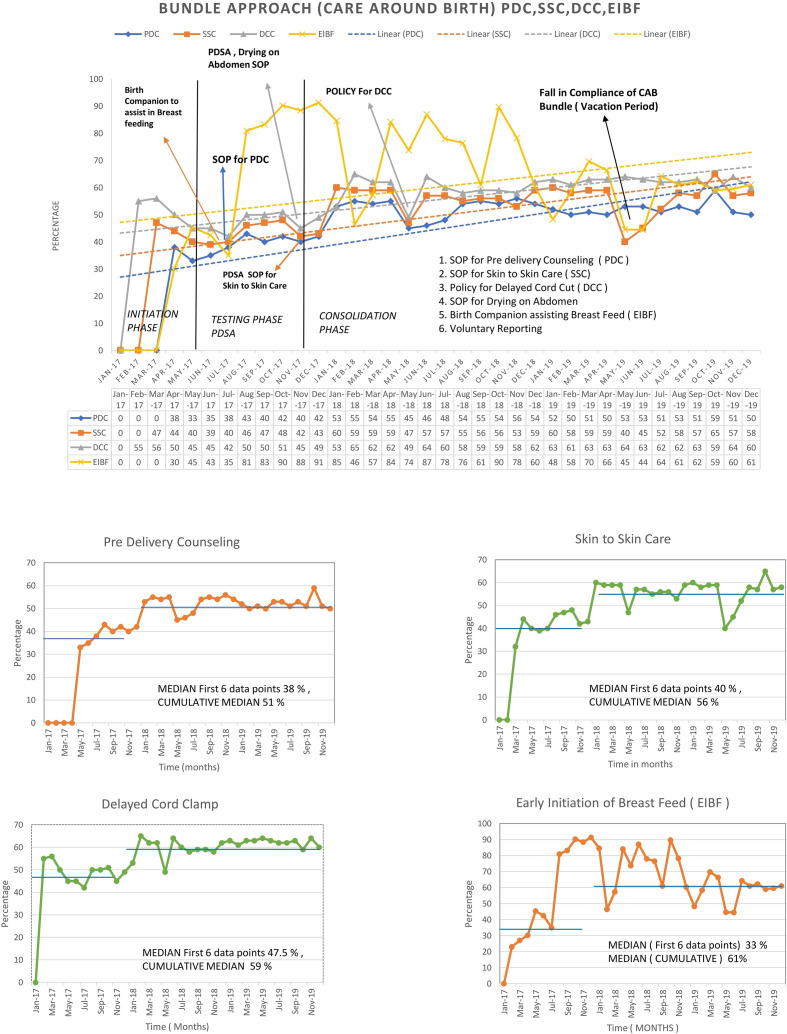
We calculated these process indicators from the record register, every week for first 6 months then monthly over remaining 30 months period (2017–2019). We plotted these percentages over time in a time series chart (figure 2).
Figure 2.
Time series CAB bundles. SOP, Standard Operating Protocol; PDSA, Plan-Do-Study-Act.
To ensure immediate drying while doing DCC and providing SSC, the delivery team assessed neonatal hypothermia by touch method after 1 hour of delivery (balancing indicator). Touch method is not very accurate method but is a good screening method (Facility Based Newborn Care Guidelines by Ministry of Health and Family Welfare, Government of India). Percentage of newborn on exclusive breast feed at the time of discharge was a surrogate indicator of improved practices at birth.
Ethics approval
This study was a QI initiative to implement recommended evidence guidelines and hence no ethical clearance was required. This was a programme implementation as per Government of India, Ministry of Health and Family Welfare’s Labour Room Quality Improvement initiative, known as LaQshya.10 Only data recommended by the LaQshya programme was collected. The QI team had permission from the concerned facility and Ministry of Health and Family Welfare. Moreover, as per the national guidelines for biomedical research, ‘research on publicly available information, documents, records, works, performances, reviews, quality assurance studies, archival materials or third-party interviews, service programs for benefit of public having a bearing on public health programs, and consumer acceptance studies’ are waived from voluntary informed consent process.11
Design
We used POCQI methodology developed by WHO-SEARO.2 We formed a QI team consisting of two paediatricians, two obstetricians, two senior nursing officers in charge of two delivery points (labour room), and two nursing staff trained in POCQI methodology.
We improved the compliance to successful change idea implementation by allowing the delivery teams to exercise voluntary choice as per the contextual limitation (delivery load and variability in number of nurses available in different shifts). We conducted informal periodic team briefings, discussion of challenges and appreciation of efforts to offset variability due to frequent transfer and inertia to change process. We shared the successful Plan-Do-Study-Act (PDSA) experience of QI teams with delivery teams at every available opportunity. We conducted regular on-site group discussion to reinforce successful change implementation. The above steps increased the acceptability of change process by the delivery teams.
After analysis of the problem, the QI team tested these ideas at single delivery point, where the staff nurse in charge was enthusiastic. We recorded learnings from this labour room in select shifts when enthusiastic QI trained nurses were on duty. We then replicated them in second delivery area and shifts where more resistant teams were on duty. We found that delivery team were reluctant to adopt new change ideas due to contextual limitations of delivery load and shortage of work force. Therefore, the QI team first started with an aim of improving early initiation of breast feed within 1 hour of delivery. This was done with the aim to (a) sensitise frontline teams in QI methodology, (b) demonstrate that in the given context evidence-based recommendations of EIBF can be implemented and (c) the success in this single intervention should convince all concerned (including supervising team) members to adopt recommended evidence-based care around the birth practices.
We conducted this study in three phases (steps) of 6 months duration each. Following this we sustained the new process of care over the next 18 months.
Initiation Phase. First 6 months, the QI trained and enthusiastic team of nurses and doctors would use POCQI in testing (PDSAs) change ideas with new process flow of care around birth. The QI team conducted periodic group discussion involving non-QI team members to sensitise all regarding the experience from the PDSAs.
Testing Phase. Next 6 months, the QI team upscaled the successful change ideas that was tested in one delivery area in select shifts (initiation phase) to all the shifts and both delivery rooms. This would result in better compliance and lesser effort required than in first training all frontline workers working in shifts. It will be like learn and train while you work.
Consolidation Phase. Next 6 months, the QI team continued to monitor the implementation of changed process of care in both the delivery areas, with regular supervisions, group discussions and actively incorporating feedbacks or modifications in the ongoing process.
The QI team supported the delivery team’s decision to follow the new process of care or old process with appreciative inquiry, exploring contextual reasons. This ensured active participation of all concerned, in improving the compliance of SSC, DCC and EIBF in normal deliveries.
The QI team standardised the successful change ideas, based on feedback as Standard Operating Protocol (SOP). The QI team then disseminated it to all concerned on a regular basis.
Strategy
During problem analysis, the QI team found that the delivery team used to separate normal newborn from mother immediately after birth. In addition, the nurse transferred mother after delivery to the post-delivery observation room late. Therefore, the delivery team could not initiate breast feeding within 1 hour of birth in majority of the cases.
Delivery team could not delay the cord clamp application, as many were not aware about this, and some were aware of the recommendation, but since there was no policy, they did not practice it.
The QI team decided to test one change at a time, addressing specific identified challenges. At first, the QI team tested a change idea by multiple iterations (PDSA) in select shifts, in one delivery area.
The delivery team did not know about the practice of providing SSC on mother’s abdomen, immediately after birth and hence they did not practice it.
For improving early breast feeding, change idea of early transfer of mother from delivery area to post-delivery observation room was tested. The PDSA planned was that the delivery area nurse would ensure early transfer of mother to the post-delivery observation room. Nurses from QI team in different shifts tested this for 4–5 days and QI team leader (nurse in charge) analysed the results. They discovered that this change idea facilitated early breast feeding, as both mothers and newborn were together within 1 hour of delivery. The nurse observed that for almost all normal deliveries, she could easily transfer mother half an hour after the delivery of newborn.
The QI team found out that many times mothers needed someone to facilitate breast feeding in the observation room. The nurse on duty had difficulty in supervising breast feed every time. Hence, the QI team tested second change idea by allowing one family member to assist mother in breast feeding. QI nurse in their duty shifts tested this over a week and observations discussed with QI team. This further improved breastfeeding rates by mothers.
Third change idea tested, was of providing SSC immediately after birth and facilitating breast feed on delivery bed. However, the nurse observed that she could facilitate SSC for some time, but breast feeding on delivery bed by mother was difficult. It required supervision and the nurse on duty could not attend other emergencies. Hence, this change idea was not adopted.
The QI team facilitated early breast feeding by providing SSC and early transfer of mother to post-delivery area to continue SSC and initiate breast feeding within 1 hour. The family member would facilitate and supervise this care process.
The QI team had started testing other change ideas by one more team. The change idea was to test whether PDC could facilitate SSC care immediately after birth. Second QI nurse tested this by doing a brief counselling and taking verbal consent of mother in delivery room regarding the process of care to be provided to her, which included keeping the newborn on her abdomen after birth and allowing her to hold and provide SSC. This change idea, the QI team tested for 1 week. The practice of PDC was beneficial in getting active participation of mother in the subsequent process of care. It also facilitated the understanding and participation of the obstetrician and paediatrician in the ongoing care. However, there was variability in counselling content observed when undertaken by other nurses in their respective shifts. This led to the testing of pre-designed counselling content over 4 weeks period by different delivery teams supervised by QI team leader. After every week, based on the feedback, modified counselling content was re-tested.
The QI team finalised the counselling format as a SOP. This finalised format took less than a couple of minutes to undertake, was easy to understand and remember.
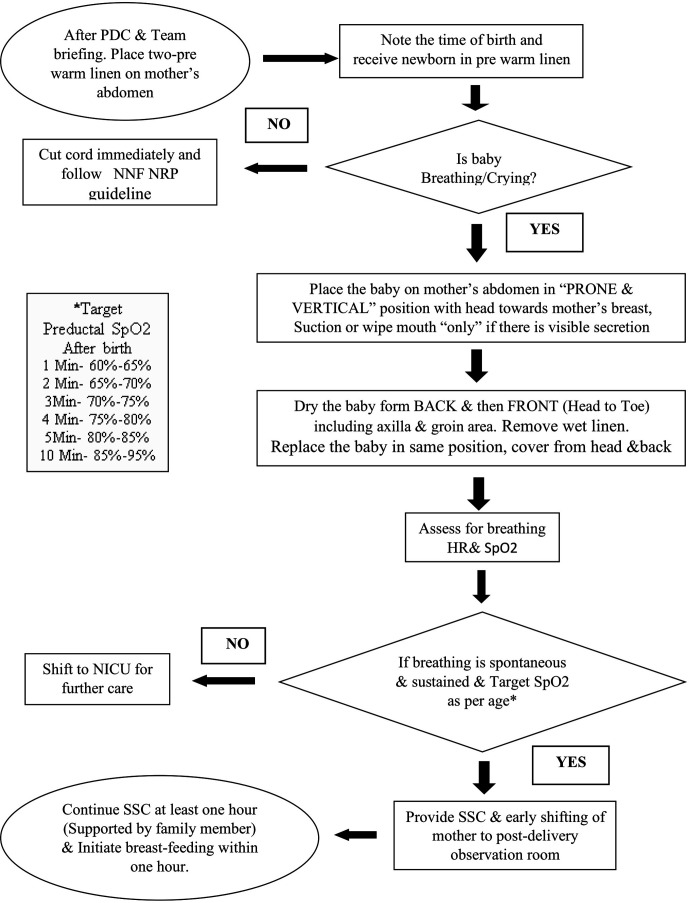
To provide SSC process on mother’s abdomen, the QI team tested different methods and steps of drying the newborn on mother’s abdomen. The QI team found that the steps required for providing SSC and baby drying on mother’s abdomen is not clear in existing literature. It has significant process variability in different parts of the world. Contextualisation and standardisation of process of drying on mother’s abdomen and continuing SSC is necessary for improved compliance. The QI nurse assisted nurse on duty in select shifts to document and help them drying the newborn on mother’s abdomen. The QI team took 6 weeks to complete on-site orientation of all delivery teams for drying and providing SSC on mother’s abdomen. This was the period when they took feedback and on-site observation. This helped them to standardised the process of providing SSC care and drying on mother’s abdomen (figure 3).
Figure 3.
Algorithm. HR, heart rate; NICU, neonatal intensive care unit; NNF NRP, National Neonatology Forum of India Neonatal Resuscitation Programme; PDC, Predelivery Counselling; SSC, skin-to-skin care; SpO2, Oxygen saturation.
Despite repeated reminder for DCC, the delivery teams as a habit, used to separate normal newborn immediately after birth. However, when QI team standardised the process of SSC, it became easy (for detailed PDSAs, refer online supplemental file).
bmjoq-2021-001445supp001.pdf (94.6KB, pdf)
Due to frequent transfers of frontline health workers, the QI team would repeat efforts of sensitising about new change process and reinforce the new SOP. The QI team circumvented the challenge of shortage of work force by allowing the delivery team the voluntary choice, of deciding either to follow earlier process of care around birth or to follow the ‘new improved process of care’.
The QI team intentionally went slow in upscaling of the process of SSC after birth. It was convenient, in comparison to one time training of all teams and ensured focused reinforcement.
Results
The time series graph (figure 2) shows baseline compliance of PDC, SSC, DCC and EIBF were low in initial 6 months of starting the intervention. The first initiative of improving EIBF, with the aim of achieving 75% at the end of 12 weeks, was only 27% to begin with. This could be achieved by early transfer of mother and newborn to the post-delivery observation room. With testing for SSC and PDC which emphasised breast feeding, the EIBF rates at the end of 6 months were 43% (June 2017). This could be due to the simultaneous testing of PDC, and SSC. Involvement of family member accompanying the mother to assist in breast feeding in post-delivery room was a successful change idea. The breastfeeding rates rose to 81% (August 2017).
The QI team on every visit reinforced the practice of DCC in the delivery area. The compliance to the same rose to 56%, over 12 weeks. Linking the practice of SSC with immediate drying followed by DCC after 1 min was easy to understand and follow. Subsequently the QI team finalised the SOP for drying on mother’s abdomen, SSC and DCC (May 2018).
For approximately 9 months, February 2017 to November 2017, QI team tested and took feedback for providing SSC at both the delivery areas, by delivery teams, on voluntary basis. The team standardised the practice of giving SSC, after December 2017 (figure 2).
PDC of mother was tested as one of the change ideas to improve SSC during fifth month of start of intervention (May 2017). The content of PDC was tested and standardised over 12 weeks (August 2017).
The QI team regularly carried on-site sensitisation of the care process; this included the SOP for conducting PDC. The overall practice of SSC rose to 60% (Jan 2018).
We observed an overall reduction in the compliance of care around birth practices during the month of May 2018. This was due to the addition of two intensive care beds in one of the delivery areas. We observed another decrease in compliance during the summer vacation period (May 2019 to Jun 2019), when both the on-site supervision (infrequent QI meetings) reduced and the ratio of available frontline health worker to delivering mothers worsened.
The compliance of PDC, SSC after birth, DCC and EIBF shows sustained improvement over more than a 2-year period as seen in the run charts (median of first 6 months compliance percentage) (figure 3). Median ‘sustained compliance’ of 51%, 56%, 59% and 61% can be seen over 36 months period for PDC, SSC, DCC and EIBF within 1 hour respectively.
Lessons and limitations
This was our first improvement initiative using POCQI methodology, and initially we faced difficulty in having regular meeting at fixed intervals. The documentation of pre-intervention process of care also required multiple on-site visits and feedback. This was due to variable contextual limitations, like shortage of workforce due to sudden transfer, leaves. The night shifts frequently faced a worsened nurse to mother ratio of 1:8. Sometimes the QI team could not test the planned PDSA in a shift due to high delivery load. Due to beginner’s enthusiasm instead of picking small SMART aim the team worked on different process of care simultaneously. This provided the opportunity, for process redesigning in small steps. On analysis of multiple processes, the QI team understood the relationship among seemingly different outcomes. For example, drying on mother’s abdomen facilitated DCC. Similarly, PDC facilitated active teamwork and active participation by mother in the care process. The slow pace of improvement provided the QI team an opportunity to connect to all delivery teams and sensitise them about the QI process and its need. This facilitated their voluntary active engagement in the end. This helped in standardisation and uniformity in the care process. Encouragement from supervising teams favoured increase compliance of the recommended practices by frontline health workers. In a period of 12 months, it brought ownership, sensitisation and a system ready to learn.
Given a choice, the QI team would have first trained/sensitised all frontline teams and supervising team with POCQI methodology and would have attempted to have a regular meeting and pre-induction training programme in place. The core QI team with only job responsibility of improvement, might have accelerated the improvement process.
Although in this study, we used a simple methodology to assess quality of routine newborn care, it has limitations. The major limitation of the study is that because of shortage and rapid turnover of nurses and doctors every month, re-orientation of new teams remains a challenge. We did not document routine newborn care provided to babies born via caesarean delivery or following resuscitation of newborns not breathing or crying at birth. We also could not evaluate the short-term and long-term impact of all the four improved newborn care practices on neonatal mortality and morbidity.
Conclusion
The results of this study demonstrate that using simple POCQI methodology can improve the process of care for routine newborn care practices immediately after birth. The improved process of care is feasible, scalable and replicable in a resource constrained setting.
We recommend that a healthcare staff in the labour room receive regular refresher training in essential newborn care and supporting breast feeding. Monthly drills or simulation exercise in supportive supervision must be an integral part of any quality of care programmes. Multidimensional approach is necessary to close the quality gaps and in designing future programmes for newborn care.
Acknowledgments
The authors would like to acknowledge the cooperation of Nurses Roma,
Harpal, Vijay Laxmi, Sapna Kumari and Reji Tito. We also thank all nursing staffs and resident doctors posted in labour room of our hospital during the study period. Special mention of Nationwide Quality Improvement (NQOCN) team efforts in training and mentoring the concerned QI team and labour room teams in POCQI methodology.
Footnotes
Twitter: @SushilUCMS
Contributors: Contributors RS, HS, SS, SB and PA all made substantial contributions to the conception or design of the work and/or the acquisition, analysis or interpretation of data for the work. RS and SS drafted the paper. SG provided necessary administrative support for the quality improvement initiative. All authors critically appraised, reviewed and approved the final version of the paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. Publication of this article is made Open Access with funding from the Nationwide Quality of Care Network.
Competing interests: None declared.
Patient and public involvement statement: Patients, mothers or the public WERE NOT involved in the design, or conduct, or reporting, or dissemination plans of our research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
References
- 1.World Health Organisation (WHO) . Standards for improving quality of maternal and newborn care in health facilities. Geneva: WHO Press, 2016. [Google Scholar]
- 2.Deorari A, Mehta R, Livesley N. Improving the quality of care for mothers and newborns in health facilities: point of care quality improvement. facilitator manual. New Delhi, India: World Health Organisation, Regional Office for South-East Asia, 2017. http://www.pocqi.org/wp-content/uploads/2018/01/POCQI-Facilitator-Manual.pdf [Google Scholar]
- 3.WHO . Newborns: improving survival and well-being, 2020. Available: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
- 4.Boundy EO, Dastjerdi R, Spiegelman D, et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics 2016;137:e20152238. 10.1542/peds.2015-2238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takahashi K, Ganchimeg T, Ota E, et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the who global survey. Sci Rep 2017;7:44868. 10.1038/srep44868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation,, United Nations Children’s Fund . In: every newborn: an action plan to end preventable deaths. Geneva: WorldHealth Organisation, 2014. [Google Scholar]
- 7.Bramson L, Lee JW, Moore E, et al. Effect of early skin-to-skin mother--infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. J Hum Lact 2010;26:130–7. 10.1177/0890334409355779 [DOI] [PubMed] [Google Scholar]
- 8.Tamura T, Goldenberg RL, Hou J, et al. Cord serum ferritin concentrations and mental and psychomotor development of children at five years of age. J Pediatr 2002;140:165–70. 24. 10.1067/mpd.2002.120688 [DOI] [PubMed] [Google Scholar]
- 9.Ministry of Health and Family Welfare . National family health Survey-4 2015-16 India Factsheet. Available: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf [Accessed 17 Feb 2018].
- 10.LaQshya . Labour room & quality improvement initiative. Ministry of health & family welfare, government of India, 2017. [Google Scholar]
- 11.Indian Council of Medical Research . Ethical guidelines for biomedical research on human participants. 110. New Delhi: Indian Council of Medical Research, 2006: 029. http://icmr.nic.in/ethical_guidelines.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2021-001445supp001.pdf (94.6KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.