Abstract
Background
Limited information is available on the financial impact of healthcare associated infections in Sub-Saharan Africa. A prospective case-control study was undertaken at Korle-Bu Teaching Hospital, Ghana, to calculate the cost of surgical site infections (SSI).
Methods
We studied 446 adults undergoing surgery from the surgical department. In all, 40 patients with SSI and 40 control patients without SSI were matched by type of surgery, wound class, ASA, sex and age. The direct and indirect costs to patients were obtained from patients and their carers, daily. The cost of drugs was confirmed with the pharmacy at the department.
Results
The prevalence rate for SSI was 11% of the total 446 cases sampled between June and August 2017. On average patients with SSI who undertook hernia surgery paid approximately US$ 392 more than the matched controls without SSI. The least difference was recorded amongst patients who had thyroid surgery, a difference of US$ 42. The results show that for all surgical procedures, SSI patients report excess length of stay. The additional days range from 1 day for limb amputation, to 16 days for rectal surgery.
Conclusions
In this study, patients with SSI experienced significant prolongation of hospitalisation and increased use of health care costs. In many cases, the indirect costs were much higher than direct costs. These findings support the need to implement preventative interventions for patients hospitalised for various surgical procedures at the Korle Bu Teaching Hospital.
Keywords: Attributable, Cost, Surgical site infection, Ghana, Teaching hospital
Introduction
Nosocomial or hospital acquired infections (HAI) remain high, in spite of the advancement in medical technology and surgery-related management procedures in both developed and developing countries [1]. Across countries surgical site infections (SSI) are among the most important. Thus, in Europe SSI is estimated to account on average for 20% of HAI, ranging from 9% in Luxembourg to 29% in Spain [2]. A recent meta-analysis focusing on the limited evidence available from developing countries found that SSI with an estimated incidence of 5.6 per 100 surgical procedures was the leading HAI and considerably higher than in developed countries [3].
Apart from the negative effects on patient health, HAI can be costly to the health system, the individual patient and society at large as HAI require additional treatment in hospital or at home and may also require additional absence from work.
Although HAI cannot be completely eliminated, a large number of HAI is deemed to be avoidable [4]. Interventions to increase quality of care and reduce risk of HAI are, however, costly and should be balanced against the potential savings through fewer cases of HAI and the related additional costs. In order to demonstrate potential investment gains and help mobilise resources, estimation of the cost associated with SSI has therefore interested researchers over the years, as evidenced by the existence of substantial literature [[5], [6], [7], [8]], although mainly in developed countries.
Costing studies in developed countries consistently find that health care related costs are higher in patients with SSI compared to uninfected patients due to increased length of stay, emergency visits, prolonged use of antibiotics, investigation and treatment costs [[9], [10], [11]]. Such costs can be considerable, for example, the SSI cost estimation in a community hospital by Kirkland et al. [12] found that on average the extended period of hospitalization associated with SSI was 12 days, and the median cost of hospitalization for infected patients was US$ 7,531 - almost double of the US$ 3,844 for uninfected patients.
SSIs, however, have cost consequences beyond the health sector such as patients' own treatment costs, productivity losses by patients and relatives, cost of care related to temporal or permanent impairment of functional and mental capacity, as well as the real opportunity cost of hospital beds that cannot be utilized for other purposes due to hospitalization of SSI patients [13,14]. However, not all of these consequences are easily quantifiable, and the true costs of SSI remain understated [13]. Furthermore, many low income countries have high out-of-pocket expenditures, thus patients bear the financial consequences of SSI to a larger extent. Consequently, it is important to look beyond the health sector expenditure to understand the burden on society and the need for interventions to prevent HAIs.
The direct costs associated with HCAIs include the cost of drugs and treatment materials, medical and surgical procedures and laboratory tests [15], which may to a smaller or – especially in low income settings – larger extent be paid by the patient. Productivity losses associated with HCAIs include lost wages for patients and their family caregivers, loss of taxes to the state, and decreased productivity for employers [16]. Generally, it is difficult to measure productivity losses accurately, therefore studies often estimate only the direct costs. Furthermore, most studies rely only on additional days of stay to estimate the incremental costs associated with HCAIs, because of the difficulty in tracking patient-specific laboratory expenses, pharmacy and nursing care data, and inconsistencies in accounting practices, as well as variation in costs and charges among various hospitals [14].
Because SSIs are relatively rare, and because patients for ethical reasons cannot be randomized to SSI or no SSI, alternative study designs are required to measure the additional costs. A common approach is the matched-pair design [[17], [18], [19], [20]]. Patients have different lengths of stay and risks of SSI. Comparison of patients with and without SSI in order to isolate the effects of SSI requires that relevant criteria are used to match patients. Age, gender and type of surgery are commonly used matching criteria [11].
The variability of the risk of SSI has also led to the development of standardized criteria to predict cost of SSI based on the anatomic extent of surgery complications. The cost of SSI resulting from deep incision is higher compared to that which is associated with superficial wounds although the latter is the most common. For example, Urban [13] estimated that the average cost of superficial SSI is US$ 400 while that of deep incisional SSI is US$ 30,000. Unlike infected deep incisional wounds, it takes relatively simple treatment measures with or without antibiotics to treat superficial infected wounds whereas it is resource intensive to treat deep SSIs [21,22].
In spite of the abundance of studies on SSI cost estimation in countries such as Spain [23], Turkey [24], USA [25], United Kingdom [26] and Thailand [27], a literature search revealed a knowledge gap on the cost of SSI in Sub-Saharan Africa. This paper therefore seeks to contribute to filling this knowledge gap by providing an empirical estimate of SSI cost from a societal perspective in Ghana's major health referral center, the Korle-Bu Teaching Hospital (KBTH).
Methods
Setting
The study was undertaken in Korle-Bu Teaching Hospital (KBTH), Accra, Ghana. The KBTH is Ghana's major public tertiary referral hospital with approximately 2,000 bed capacity. Except for critical emergency cases most patients are admitted to the KBTH through referral from other hospitals. Hospital care in public hospitals in Ghana is financed through a combination of government funding and user payment. The government pays staff salaries, some goods and services, capital and maintenance of equipment. Cost recovery of non-wage direct services, such as medicine, consultation and laboratory takes place either as out-of-pocket payment or reimbursement by the National Health Insurance Scheme (NHIS). Currently, the NHIS enrolment covers about 38 percent of Ghana's population.
Study design and sampling
The study population comprised all persons admitted for surgery through the surgical outpatient department or the emergency/accident department to any of the 4 general surgical wards of the surgical department in KBTH. All patients who underwent surgery between June 2017 and September 2017 were included in the study. A matched pair study design was employed. Patients with SSI were identified up to 30 days after surgery by the medical staff through daily in-patient surveillance of surgery patients, followed by post discharge surveillance by means of a healthcare personnel-based survey and a patient-based telephone survey [28]. Identified patients with SSI were matched with patients with no SSI using age (±1 year), sex, type of surgery and wound class as matching criteria. Age matching was carefully done to avoid potential disparity in age-related earning and cost. Patients who had an implant inserted or underwent procedures where primary closure of incision was not completed in theatre or had procedures performed by endoscopy were excluded. The study received ethical approval from Korle Bu Teaching Hospital (KBTH) Ethical Committee.
Outcomes
The primary outcomes evaluated in this study included additional days of hospitalisation and extra costs. Extra cost attributable to SSI was defined as the estimated mean difference in direct costs and productivity losses between patients with SSI and matched patients without SSI.
Data collection
For all patients, data were recorded on demographical characteristics (gender and age), postoperative variables such as SSI status, wound class and length of stay (LOS). Length of stay was defined as days after surgery that the patient was discharged. Patients' length of stay in the department was obtained prospectively on daily rounds. Those who were discharged the same day of surgery were given a LOS status of ‘0’.
Patients identified as having SSI and matched patients were additionally administered a structured questionnaire postoperatively to capture their direct costs and productivity losses associated with their hospitalisation covering 30 days after discharge.
Data analysis
Patients' Direct Costs
Direct costs included costs on pharmaceuticals such as antibiotics; laboratory and diagnostic tests; and surgical interventions. The direct costs also included transportation costs incurred by patients and their carers and costs of review and wound dressing. All direct costs were added for each patient and mean cost per patient calculated and compared between SSI and non-SSI patients.
Productivity loss
Productivity losses refer to the opportunity costs to patients and their carers related to the hospital admission, i.e. the loss of income due to illness or caring activities during admission and the subsequent 30 days after discharge. The productivity loss is calculated as a product of the number of days respondents were unable to work and their daily wage. Data was collected on the number of days of sick leave (absenteeism) of patients and their caregivers, employment status of patients and carers (employed, retired, homemaker, student or unemployed), type of employment, monthly income and normal weekly work hours. For employed patients with paid jobs the 2017 national average monthly income specified by sex and type of employment [29] was calculated and used to value time loss per day. For those aged 18–60 years engaged in informal sector work and could not provide specific monthly income, their indirect cost was computed using same national average wage values for informal sector workers. For patients accompanied by carers, the daily wage of their carers was estimated in a similar manner. The reason for using the national average wage instead of the actual patient wage was to enable generalisation of the result, and consequently, avoid potential over-estimation and under-estimation of the indirect cost.
Hospital costs
To estimate the institutional cost of SSI, the study used a composite/gross-costing approach rather than a disaggregated/micro-costing approach [30]. The former captures the sum of all expenditures incurred by the specific health facility or department. This includes staff related cost, cost of clinical support, capital equipment and the cost of all other consumables purchased by the Surgical Department of KBTH in 2017. These expenditure data were obtained from the Human Resource Directorate and the Accounts Department of KBTH. The total number of admissions to the surgical department in 2017 was obtained and the total number of inpatient days estimated. The average cost per inpatient day was then calculated and used to estimate the hospital cost incurred based on length of stay of the patients with SSI and their matches. Cost calculations were made in Ghana cedis (GH₵) and converted to purchasing power parity in United States Dollars (PPP-US$) using a web-based tool for purchasing power parity conversion recommended by Ian et al. [31].
Results
Description of participants
We studied 446 adults undergoing surgery from the surgical department. In all, 62 patients were identified but only 40 patients with SSI and 40 control patients without SSI were matched. For the 22 SSI patients excluded from the match pair analysis, reasons were that 2 absconded, 7 declined to participate in the study, 3 died, 5 were lost to follow up due to wrong contact information, while the remaining 5 had no perfect match in the control group. Of the total sample studied, females constituted 62%. The mean age of the overall sample was 46 years [SD = 18 yrs] while that of patients with SSI was 41 years [SD = 17 yrs]. In terms of wound classification, 64.7% of the total sample had clean wounds. However, 75% of the SSI patients were among those classified as having dirty, clean contaminated and contaminated wounds. The most common surgical procedure performed among SSI patients was herniorrhaphy, followed by breast, appendix and colon surgery (Table 1).
Table 1.
Descriptive statistics of the overall sample cum patients with and without SSI.
| Total sample (N = 446) | Matched groups |
||
|---|---|---|---|
| SSI (n = 40) | Non-SSI (n = 40) | ||
| Sex | |||
| Male | 171 [38.0] | 9 [22.5] | 9 [22.5] |
| Female | 275 [62.0] | 31 [77.5] | 31 [77.5] |
| 446 [100.0] | 40 [100.0] | 40 [100.0] | |
| Wound Class | |||
| Clean | 289 [64.7] | 10 [25.0] | 10 [25.0] |
| Clean contaminated | 30 [6.7] | 3 [7.5] | 3 [7.5] |
| Contaminated | 57 [12.7] | 9 [22.5] | 9 [22.5] |
| Dirty | 70 [15.9] | 18 [45.0] | 18 [45.0] |
| Total | 446 [100.0] | 40 [100.0] | 40 [100.0] |
| Procedure | |||
| Colon surgery | 16 [3.6] | 5 [12.5] | 5 [12.5] |
| Herniorrhaphy | 88 [19.7] | 11 [27.5] | 11 [27.5] |
| Thyroid surgery | 40 [9.0] | 3 [7.5] | 3 [7.5] |
| Appendix surgery | 69 [15.5] | 6 [15.0] | 6 [15.0] |
| Breast surgery | 64 [14.3] | 7 [17.5] | 7 [17.5] |
| Rectal surgery | 8 [1.8] | 1 [2.5] | 1 [2.5] |
| Small bowel surgery | 8 [1.8] | 2 [5.0] | 2 [5.0] |
| Gall bladder surgery | 5 [1.1] | 2 [5.0] | 2 [5.0] |
| Limb amputation | 98 [22.0] | 2 [5.0] | 2 [5.0] |
| Bile duct, liver | 3 [0.7] | – | – |
| Laparotomy | 47 [10.5] | 1 [2.5] | 1 [2.5] |
| Total | 446 [100.0] | 40 [100.0] | 40 [100.0] |
| Mean age (years) | 46 [6–98] | 41 [14–78]a | 40 [16–76] |
Minimum and maximum ages in parenthesis.
Patient direct costs
In general, patients with SSI recorded higher costs [95% CI = $1,543 – $1,953] compared to non-SSI patients [95% CI = $1,211 – $1,650]. For instance, on average patients with SSI who underwent hernia surgery paid approximately US$ 392 more than similar patients without SSI. The least difference US$ 42 was recorded amongst patients who had thyroid surgery (Table 2). On average patients with SSI spent US$ 298 more than patients that were similar in age, sex, wound class and type of surgery. The higher level of expenditures among SSI patients was mainly due to the cost of drugs (25.8%), laboratory tests (7.2%), consultation (39%), cost of infected wound dressing (4.6%), and transport cost (23.4%).
Table 2.
Direct cost of patients with and without SSI in US$.
| SSI |
Non-SSI |
Average difference in cost per patient | |||||
|---|---|---|---|---|---|---|---|
| No. | Total cost | Average cost per patient | No. | Total cost | Average cost per patient | ||
| Colon surgery | 5 | 9,092 | 1,818 [486–2,976] | 5 | 7,249 | 1,450 [634–2,208] | 368 |
| Herniorrhaphy | 11 | 16,810 | 1,528 [518–2,527] | 11 | 12,498 | 1,136 [352–1,837] | 392 |
| Thyroid surgery | 3 | 5,521 | 1,840 [1,675–2,145] | 3 | 5,393 | 1,798 [1,290–2,080] | 42 |
| Appendix surgery | 6 | 10,684 | 1,781 [484–2,786] | 6 | 9,933 | 1,655 [634–2,165] | 126 |
| Breast surgery | 7 | 11,227 | 1,605 [757–2,354] | 7 | 9,330 | 1,938 [525–1,853] | 333 |
| Rectal surgery | 1 | 2,343 | 2,343 | 1 | 1,510 | 1,510 | 833 |
| Small bowel surgery | 2 | 4,030 | 2,015 [1,825–2,206] | 2 | 3,856 | 1,928 [1,607–2,248] | 87 |
| Gall bladder surgery | 2 | 3,508 | 1,754 [1,648–1,860] | 2 | 2,692 | 1,346 [1,725–1,186] | 408 |
| Limb amputation | 2 | 4,433 | 2,217 [1,988–2,446] | 2 | 3,655 | 1,827 [1,508–2,146] | 390 |
| Laparotomy | 1 | 2,260 | 2,260 | 1 | 1,880 | 1,880 | 380 |
| All | 40 | 1,748 | 40 | 1,450 | 298 | ||
Note: Minimum and maximum cost in bracket.
Productivity loss
Table 3 shows the number of days lost and estimated productivity loss for matched patients. For almost all the surgical procedures, those with SSI reported higher number of days lost and higher indirect costs [95% CI = $381 – $893] compared to the non-SSI patients [95% CI = $185 – $730]. The highest difference was costs associated with rectal surgery, a difference of US$ 2,834. The difference in indirect cost was driven by the generally high number of productive loss days among SSI patients compared to their matches. Except we noticed that for those who underwent breast and small bowel surgery, the indirect cost was highest among non-SSI patients despite a lower number of days lost. On average, the productivity loss of SSI patients exceeded that of matched non-SSI patients by US$ 168.
Table 3.
Indirect cost of patients with and without SSI in US$.
| SSI |
Non-SSI |
Difference in average productivity loss | |||||
|---|---|---|---|---|---|---|---|
| No. | Average number of days lost | Average productivity loss | No. | Average number of days lost | Average productivity loss | ||
| Colon surgery | 5 | 17 [9–23] | 486 (60–1,100) | 5 | 16 [7–48] | 274 (275–2,103) | 212 |
| Herniorrhaphy | 11 | 15 [5–36] | 670 (30–2,598) | 11 | 5 [2–11] | 508 (7–3,164) | 162 |
| Thyroid surgery | 3 | 12 [7–16] | 360 (91–901) | 3 | 5 [3–7] | 57 (30–89) | 303 |
| Appendix surgery | 6 | 12 [7–19] | 902 (88–1,719) | 6 | 7 [3–11] | 823 (38–2,751) | 79 |
| Breast surgery | 7 | 10 [4–22] | 145 (125–364) | 7 | 5 [4–7] | 217 (13–558) | −72 |
| Rectal surgery | 1 | 52 | 3,114 | 1 | 18 | 280 | 2,834 |
| Small bowel surgery | 2 | 20 [19,20] | 686 (127–1245) | 2 | 15 [6–23] | 2,049 (676–3,423) | −1,363 |
| Gall bladder surgery | 2 | 17 [16,17] | 682 (229–1,133) | 2 | 8 [5–10] | 83 (39–127) | 599 |
| Limb amputation | 2 | 9 [6–11] | 876 (33–1,719) | 2 | 7 [5–9] | 41 (20–61) | 836 |
| Laparotomy | 1 | 28 | 100 | 1 | 13 | 89 | 11 |
| Average | 40 | 625 | 40 | 457 | 168 | ||
Hospital costs
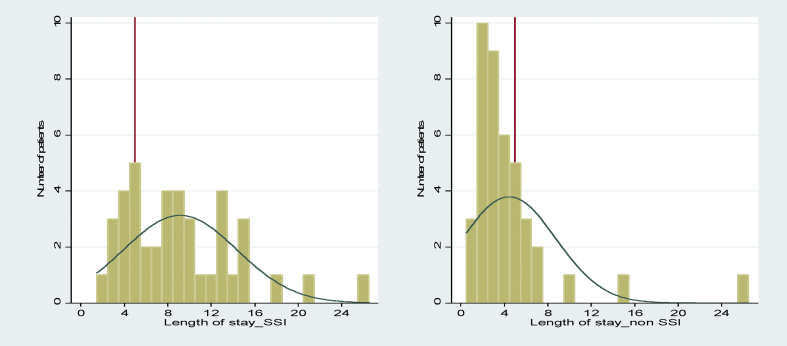
Hospital cost estimates were based on LOS and average departmental cost per day. The average LOS for SSI patients were 9.2 compared to 4.6 in the control group (Chi2: P = 0.003). This is also illustrated in Figure 1 which shows, for example, that 27 patients with SSI stayed more than 5 days in the hospital compared to 7 in the matched control group. The extra LOS is consistent across surgical procedures. The number of extra days in hospital range from an average of 1 day for limb amputation to an average of 16 extra days for rectal surgery (Table 4).
Figure 1.
Length of stay for patients with and without SSI in days.
Table 4.
Additional average length of stay (ALOS) for patients with and without SSI.
| SSI |
Non-SSI |
Difference in average LOS | |||
|---|---|---|---|---|---|
| No. | Average LOS | No. | Average LOS | ||
| Colon surgery | 5 | 14 (9–18)a | 5 | 9 (3–26) | 5 |
| Herniorrhaphy | 11 | 9 (3–21) | 11 | 3 (1–5) | 6 |
| Thyroid surgery | 3 | 7 (4–9) | 3 | 4 (2–5) | 3 |
| Appendix surgery | 6 | 7 (4–13) | 6 | 4 (2–7) | 4 |
| Breast surgery | 7 | 6 (2–13) | 7 | 3 (2–4) | 3 |
| Rectal surgery | 1 | 26 | 1 | 10 | 16 |
| Small bowel surgery | 2 | 13 (10–15) | 2 | 9 (3–15) | 4 |
| Gall bladder surgery | 2 | 9 (8–10) | 2 | 4 (3–5) | 5 |
| Limb amputation | 2 | 4 (3–5) | 2 | 3 (2–4) | 1 |
| Laparotomy | 1 | 15 | 1 | 7 | 8 |
| All | 40 | 9.2 | 40 | 4.6 | 4.6 |
Minimum and maximum LOS in parenthesis.
The total expenditures in the surgical department in 2017 amounted to US$ 10,761,838. Of this amount, monthly salaries and allowances of established and non-established staffs constituted 56%, followed by the cost of medical supplies 22.6% while the remaining 21.4% covered cost of capital equipment and other consumables. The surgical department admitted 3,991 patients in 2017. Assuming an average LOS of 8.3 days, as observed for the 446 patients enrolled in the present study, this corresponds to 33,125 patient day and the average patient day cost at the surgical department of KBTH thus amounts to US$ 325.
Overall
Overall, the estimated mean additional cost per patient due to SSI is US$ 1,985, of which 78% is institutional costs, 15% direct costs paid by patients and 7% productivity loss. With an annual SSI prevalence rate of 11% from historical routine patient record at the surgical department, the estimated annual cost to society amount to US$ 871,058. Likewise, from the estimated average patient day costs, the additional institutional costs per patient with SSI is US$ 1,519 (Table 5). Juxtaposing Ghana's 10% annual salary increase with an average consumer price index of 9.4% between 2017 and 2019 [32], we adjusted the hospital cost of SSI from US$ 666,651 to US$ 806,649, equivalent to US$ 925,280 in total cost.
Table 5.
Summary of estimated additional annual costs of SSI (US$).
| Mean cost - SSI | Mean cost, non- SSI | Estimated mean additional cost per patient due to SSI | Estimated total annual cost of SSIa | |
|---|---|---|---|---|
| Patient direct costs | 1,748 | 1,450 | 298 | 130,736 |
| Productivity loss | 625 | 457 | 168 | 73,670 |
| Hospital costs | 3,038 | 1,519 | 1,519 | 666,652 |
| Total | 5,411 | 3,426 | 1,985 | 871,058 |
Estimated annual number of SSI cases = 439.
Discussion
In line with the literature, we find that SSI patients incur higher cost than comparable matched patients. Other studies on the cost associated with surgical site infections have taken place in contexts that are quite different from the situation in Ghana. Due to differences in the health care system, the level of economic development and price level and structures, it is difficult to compare our results to other studies. While the magnitude of costs is likely to vary a lot, we would expect to see some consistency in the relative cost of SSI patients compared to similar patients without SSI.
As expected, comparing our results with other studies, we noticed some differences in the SSI cost per patient. For instance, while it cost additional US$ 1,985 per patient for SSI treatment, the amount is more than that reported in Italy (€1,216; US$ 1363), but much less when compared with some other European countries [9]. We also noticed that the differences in cost could be as a result of differences in types and number of surgical procedures studied, as well as differences in the overall regional economic conditions and its attendant implications on cost of medical inputs such as drugs for surgical operations and SSI treatment [11]. The study by Jenks et al. [33] at the Plymouth Hospital in the United Kingdom is one such example that involved a total of 19 surgical procedures resulting into 2017 equivalence of US$5,249 SSI attributable cost per patient.
We found that hospital costs for SSI patients are on average double of those for non-SSI patients. This is in line with other studies that found costs associated with SSI patients to be almost double of non-SSI patients, and mainly driven by additional LOS [11]. Including both direct and indirect costs our study shows that costs associated with patients with SSI at the KBTH are on average 20.8% higher compared to matched patients without SSI. To some extent, our observation corroborates with findings from Duke University Medical Centre and the Durham Regional Hospital, United States, that the total median cost incurred by SSI patients is approximately 32.4% higher than the total cost incurred by non-SSI patients [12].
Very few studies consider the wider impact of SSIs on society, in terms of absenteeism from work and lost productivity [9]. We found that the patients with SSI on average incurred 1.2 times the direct expenditures of comparable patients without SSI, and experienced almost 1.4 times as high income loss. The share of additional costs attributable to SSI that is borne by patients depends on the financing system. We maintain regardless of the differences in the SSI attributable cost per patient across many other studies, that SSI result in elevated cost, a significant part of which is indisputably borne by patients and their caregivers through out-of-pocket payments and lost incomes.
The significant LOS difference between SSI and non-SSI patients means that the hospital itself incurs significant cost due to the extra days and resources dedicated to patients with SSI. For instance, the study has observed that it on average costs the Surgical Department an extra US$ 1,519 attending to each SSI patient. This corresponds to 6.2% of the 2017 departmental expenditures being used for SSI. The majority of these institutional cost (56%) is payment of healthcare professionals and other support staffs, similar to observation by Rechner and Lipman [34] at the Royal Brisbane and Women's Hospital in Queensland, Australia. Staff and beds that are occupied by SSI patients cannot be used by other patients, which imply that fewer patients get adequate treatment.
A surprising finding of this study was that SSI patients who underwent breast and small bowel surgeries, on average, incurred relatively lesser indirect cost compared with their match cases without SSI. This was, however, due to differences in the reported daily amount lost due to absence from work, as the number of days of work lost was higher in the SSI group. Specifically, closer inspection of the data revealed that more than half of the SSI patients did not work and thus incurred a value of 0 as compared to less than a third of those without SSI.
Since SSI and its associated cost is surgically induced, it is prudent that medical staffs and the hospital in general adopt preventive measures to reduce risk factors such as those observed by Weber et al. [35]. The estimated annual cost of SSI to KBTH was almost US$ 700,000 and almost US$ 900,000 to society more broadly. Because the cost of SSI was limited to 30 days post-discharge, we anticipate an under-estimation of the reported direct and indirect cost of SSI. We only assessed productivity losses due to absence from work. However, to sustain household income some patients may have presented at work despite an SSI, which may have reduced their productivity. Such productivity losses due to presenteeism were not included and thus potentially result in an underestimation of costs. Nevertheless, the finding implies that preventive measures that would reduce SSIs by 20% would roughly be economically advantageous to the health sector, if they could be implemented at a cost of up to US$ 137,552 annually, and more from a societal perspective. Similarly, our estimation suggests that without SSI the surgical department can save additional 11,043 patient bed days annually and thus be able to admit 1,330 extra patients.
Limitations of the study
This study was undertaken in one teaching hospital in Ghana and therefore the evidence provided is not a general reflection of what pertains in other hospitals. We acknowledge the limitation in the small sample size. However, this was as a result of the study time frame of four months and the fact that the sampling took place at one hospital. Furthermore, the study required eliciting information from both patients and caregivers undergoing different degree of emotional, economic, and physical stress, and in this situation it was difficult interviewing all 62 confirmed SSI patients and their respective match without SSI. In all, 22 patients with SSI and 21 match patients without SSI declined to participate in the survey for various reasons including death of patients. In some instances, few patients absconded from the hospital before and after discharge because they could not afford to pay their bills. In few cases, there was a mismatch in the number of reviews attended by patients obtained through official wound card data and those reported by the patients.
For post-discharged patients who could not afford cost of reviews such as transport cost and cost of prescribed drugs, the total direct cost for such patients was limited to the amount spent within the sampling period. Also, we used the average cost per admission day to calculate the costs associated with the extra days in hospital of patients with SSI compared to those without SSI. The marginal cost of one extra day in the hospital may, however, differ; for example, if majority of treatment takes place during the first days of admission, then the average cost per bed day will underestimate the cost per additional day in the beginning of the admission and overestimate the cost per additional day at the end of the admission. The exclusion of the value of time for persons who were not economically active such as in our estimation of the indirect cost also means that certain costs were overlooked. For instance, there were rare cases where such persons may be working but were excluded because by Ghana Labour Laws such persons are not expected to be gainfully employed. Our inability to quantify the emotional stress suffered by patients and their caregivers due to SSI is also a limitation. Also, the exclusion of presenteeism in our estimation of productivity loss may imply an underestimation of the indirect cost.
Furthermore, we anticipate that the omission of the administrative overhead cost incurred by the central administration of the KBTH may also imply an underestimation of the hospital cost attributable to SSI.
Conclusion
This study adds to existing literature on the cost of SSI and is the first of its kind in Ghana and SSA. SSIs in patients lead to extra cost due to prolonged hospital stay and cost of review and wound dressing, as well as lost working days of patients and caregivers and productivity loss. The study provides evidence to support good infection control practices in the hospital. It demonstrates that poor quality care is costly and leads to inefficient resource use, as more could have been achieved with the resources.
CRediT authorship contribution statement
Ama Pokuaa Fenny: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Felix Ankomah Asante: Conceptualization, Methodology, Writing - review & editing, Supervision. Evans Otieku: Data curation, Formal analysis, Writing - review & editing. Antionette Bediako-Bowan: Validation, Writing - review & editing. Ulrika Enemark: Conceptualization, Methodology, Writing - review & editing, Supervision.
Conflict of interest statement
Declarations of interest: none.
Funding
Financial support for this study was provided by the Danish Ministry of Foreign Affirs as part of the HAI-Ghana project (DANIDA Grant No. 16-PO1-GHA).
References
- 1.Sullivan E., Gupta A., Cook C. Cost and consequences of surgical site infections: a call to arms. Surg Infect. 2017;18(4):451–454. doi: 10.1089/sur.2017.072. [DOI] [PubMed] [Google Scholar]
- 2.Cassini A., Plachouras D., Eckmanns T., Abu Sin M., Blank H.P., Ducomble T. Burden of six healthcare-associated infections on European population health: Estimating incidence-based disability-adjusted life years through a population prevalence-based modelling study. Plos Med. 2016;13(10) doi: 10.1371/journal.pmed.1002150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allegranzi B., Bagheri Nejad S., Combescure C., Graafmans W., Attar H., Donaldson L. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 2011. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 4.Umscheid C.A., Mitchell M.D., Doshi J.A., Agarwal R., William K., Brennan P.J. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32(2):101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- 5.Hollenbeak C., Murphy D., Dunagan W., Fraser V. Nonrandom selection and the attributable cost of surgical-site infections. Infect Contr Hosp Epidemiol. 2002;23(4):177–182. doi: 10.1086/502032. [DOI] [PubMed] [Google Scholar]
- 6.Fry D.E. The economic costs of surgical site infection. Surg Infect (Larchmt) 2002. 2002;3(suppl 1):S37–S43. doi: 10.1089/sur.2002.3.s1-37. [DOI] [PubMed] [Google Scholar]
- 7.Olsen M.A., Butler A.M., Willers D.M., Gross G.A., Hamilton B.H., Fraser V.J. Attributable costs of surgical site infection and endometritis after low transverse cesarean section. Infect Contr Hosp Epidemiol. 2010;31(3):276–282. doi: 10.1086/650755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bakkum-Gamez J.N., Dowdy S.C., Borah B.J., Haas L.R., Mariani A., Martin J.R. Predictors and costs of surgical site infections in patients with endometrial cancer. Gynecol Oncol. 2013;130(1):100–106. doi: 10.1016/j.ygyno.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badia J.M., Casely A.L., Petrosillo N., Hudson P.M., Mitchell S.A., Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017:1–15. doi: 10.1016/j.jhin.2017.03.004. 96920170. [DOI] [PubMed] [Google Scholar]
- 10.Zimlichman E., Henderson D., Tamir O., Franz C., Song P., Yamin C.K. Health care associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013. 2013;173:2039–2046. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 11.Broex E.C.J., van Asselt A.D.I., Bruggeman C.A., van Tiel F.H. Surgical site infections: how high are the costs? J Hosp Infect. 2009;72:193–201. doi: 10.1016/j.jhin.2009.03.020. (2009) [DOI] [PubMed] [Google Scholar]
- 12.Kirkland K., Briggs J., Trivette S., Wilkinson W., Sexton D. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Contr Hosp Epidemiol. 1999;20(11):725–730. doi: 10.1086/501572. [DOI] [PubMed] [Google Scholar]
- 13.Urban J.A. Cost analysis of surgical site infections. Surg Infect. 2006;7(1):19–22. doi: 10.1089/sur.2006.7.s1-19. [DOI] [PubMed] [Google Scholar]
- 14.Graves N., Halton K., Jarvis W. Springer; New York: 2009. Economics and preventing healthcare acquired infection. 2009. [Google Scholar]
- 15.Rothe C., Schlaich C., Thompson S. Healthcare associated infections in sub-Saharan Africa. J Hosp Infect. 2013;88(4):257–267. doi: 10.1016/j.jhin.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Orsi G.B., Di Stefano L., Noah N. Hospital-acquired, laboratory-confirmed bloodstream infection: increased hospital stay and direct costs. Infect Control Hosp Epidemiol. 2002;23(4):190–197. doi: 10.1086/502034. [DOI] [PubMed] [Google Scholar]
- 17.Coello R., Charlett A., Wilson J., Ward V., Pearson A., Borriello P. Adverse impact of surgical site infections in English hospitals. J Hosp Infect 2005. 2005;60:93–103. doi: 10.1016/j.jhin.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 18.Thakore R.V., Greenberg S.E., Shi H., Foxx A.M., Francois E.L., Prablek M.A. Surgical site infection in orthopedic trauma: A case control study evaluating risk factors and cost. J Clin Orthop Trauma. 2015;6(4):220–226. doi: 10.1016/j.jcot.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mansournia M.A., Jewell N.P., Greenland S. Case-control matching: effects, misconceptions, and recommendations. Eur J Epidemiol. 2018;33(1):5–14. doi: 10.1007/s10654-017-0325-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graves N., Halton K., Curtis M., Doidge S., Lairson D., McLaws M. Costs of Surgical site infections that appear after hospital discharge. Emerg Infect Dis. 2006;12(5):831–834. doi: 10.3201/eid1205.051321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mangram A.J., Horan T.C., Pearson M.L., Silver L.C., Jarvis W.R. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999. 1999;20:250–278. doi: 10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 22.Merollini K.M.D., Crawford R.W., Graves N. Surgical treatment approaches and reimbursement costs of surgical site infections post hip arthroplasty in Australia: a retrospective analysis. BMC Health Serv Res. 2013;13:91. doi: 10.1186/1472-6963-13-91. http://www.biomedcentral.com/1472-6963/13/91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alfonso J.L., Pereperez S.B., Canoves J.M., Martinez M.M., Martinez I.M., Martin-Moreno J.M. Are we really seeing the total costs of surgical site infections? A Spanish study. Wound Repair Regen, 2007. 2007;(15):474–481. doi: 10.1111/j.1524-475X.2007.00254.x. [DOI] [PubMed] [Google Scholar]
- 24.Coskun D., Aytac J., Aydinli A., Bayer A. Mortality rate, length of stay and extra cost of sternal surgical site infections following coronary artery bypass grafting in a private medical centre in Turkey. J Hosp Infect. 2005;2005(60):176–179. doi: 10.1016/j.jhin.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Anderson D.J., Kirkland K.B., Kaye K.S., Thacker P.A. Under resourced hospital infection control and prevention programs: penny wise, pound foolish? Infect Control Hosp Epidemiol. 2004;2007(28):767–773. doi: 10.1086/518518. [DOI] [PubMed] [Google Scholar]
- 26.Pollard T.C., Newman J.E., Barlow N.J., Price J.D., Willett K.M. Deep wound infection after proximal femoral fracture: consequences and costs. J Hosp Infect 2006. 2006;(63):133–139. doi: 10.1016/j.jhin.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 27.Kasatpibal N., Thongpiyapoom S., Narong M.N., Suwalak N., Jamulitrat S. Extra charge and extra length of postoperative stay attributable to surgical site infection in six selected operations. J Med Assoc Thai, 2005. 2005;(88):1083–1091. [PubMed] [Google Scholar]
- 28.Centre for Disease Prevention and Control Surgical site infection (SSI) event. 2018. https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf Retrieved from.
- 29.Ghana Statistical Service 2015 Labour force report. 2016. http://www2.statsghana.gov.gh/docfiles/publications/Labour_Force/LFS%20REPORT_fianl_21-3-17.pdf Retrieved from.
- 30.Simoens S. Health Economic Assessment: A Methodological Primer. Int J Environ Res Public Health. 2009;7(4):1831–1834. doi: 10.3390/ijerph6122950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ian S., James T., Marcello M. A web-based tool for adjusting costs to a specific target currency and price year. Evid Policy J Res Debate Pract. 2010;6(1):51–59. [Google Scholar]
- 32.Ghana Statistical Service Consumer price index. 2019. https://www.statsghana.gov.gh/gssmain/fileUpload/Price%20Indices/Bulletin%20July%20CPI%202019.pdf Retrieved from.
- 33.Jenks P.J., Laurent M., MaQuarry S., Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. J Hosp Infect. 2014;86:24–33. doi: 10.1016/j.jhin.2013.09.012. (2014) [DOI] [PubMed] [Google Scholar]
- 34.Rechner I.J., Lipman J. The cost of caring for patients in a tertiary referral Australian intensive care unit. Anaesth Intensive Care. 2005;23(4):477–482. doi: 10.1177/0310057X0503300409. [DOI] [PubMed] [Google Scholar]
- 35.Weber W.P., Zwahlen M., Reck S., Feder-Mengus C., Misteli H., Rosenthal R. Economic burden of surgical site infections at a European University Hospital. Infect Contr Hosp Epidemiol. 2008;29(7):261–269. doi: 10.1086/589331. [DOI] [PubMed] [Google Scholar]