Abstract
Introduction
The aim of this mixed-method study was to determine the extent and determinants of inappropriate dispensing of antibiotics by licensed private drug retail outlets in Indonesia.
Methods
Standardised patients (SPs) made a total of 495 visits to 166 drug outlets (community pharmacies and drug stores) between July and August 2019. The SPs presented three clinical cases to drug outlet staff: parent of a child at home with diarrhoea; an adult with presumptive tuberculosis (TB); and an adult with upper respiratory tract infection (URTI). The primary outcome was the dispensing of an antibiotic without prescription, with or without the client requesting it. We used multivariable random effects logistic regression to assess factors associated with the primary outcome and conducted 31 interviews with drug outlet staff to explore these factors in greater depth.
Results
Antibiotic dispensing without prescription occurred in 69% of SP visits. Dispensing antibiotics without a prescription was more likely in standalone pharmacies and pharmacies attached to clinics compared with drug stores, with an OR of 5.9 (95% CI 3.2 to 10.8) and OR of 2.2 (95% CI 1.2 to 3.9); and more likely for TB and URTI SP-performed cases compared with child diarrhoea cases, with an OR of 5.7 (95% CI 3.1 to 10.8) and OR of 5.2 (95% CI 2.7 to 9.8). Interviews revealed that inappropriate antibiotic dispensing was driven by strong patient demand for antibiotics, unqualified drug sellers dispensing medicines, competition between different types of drug outlets, drug outlet owners pushing their staff to sell medicines, and weak enforcement of regulations.
Conclusion
This study shows that inappropriate dispensing of antibiotics by private drug retail outlets is widespread. Interventions will need to address not only the role of drug sellers, but also the demand for antibiotics among clients and the push from drug outlet owners to compete with other outlets.
Keywords: public health, health services research, cross-sectional survey, qualitative study, health systems evaluation
Key questions.
What is already known?
Increasing antibiotic resistance is a major public health concern.
While few would dispute that drug outlets have an important role to play in reducing the overuse of antibiotics in the community, to date most antimicrobial resistance strategies and policies in Indonesia have overlooked them.
What are the new findings?
This study shows that the dispensing of antibiotics without a prescription at drug outlets is common in the study sites, despite regulations prohibiting this.
Dispensing antibiotics without a prescription was more likely in standalone pharmacies and pharmacies attached to clinics compared with drug stores, with an OR of 5.9 (95% CI 3.2 to 10.8) and OR of 2.2 (95% CI 1.2 to 3.9); and more likely for tuberculosis and upper respiratory tract infection SP-performed cases compared with child diarrhoea cases, with an OR of 5.7 (95% CI 3.1 to 10.8) and OR of 5.2 (95% CI 2.7 to 9.8).
Interviews revealed that inappropriate antibiotic dispensing was driven by strong patient demand for antibiotics, unqualified staff dispensing medicines, competition between different types of outlets, drug outlet owners pushing their staff to sell medicines, and weak enforcement of regulations.
Key questions.
What do the new findings imply?
Innovative interventions in which drug outlets can be engaged as a partner have the potential to address inappropriate dispensing of antibiotics.
A multifaceted approach should be considered, taking into account the profit-maximising motives of drug outlets, the high demand for antibiotics among clients, and the push from owners to compete with other outlets, including drug stores which dispense antibiotics despite being prohibited from selling this class of medication.
Introduction
Increasing antibiotic resistance is a major public health concern and a complex phenomenon, driven by multiple factors including health seeking behaviour and antibiotic misuse.1 2 In many low-income and middle-income countries (LMICs), private drug retail outlets (drug outlets) such as community pharmacies and drug stores are often the first point of care for mild illnesses because they are conveniently located, trusted, accessible in the evening and provide easy access to essential medicines such as antibiotics, often without a prescription.3–5 There is growing evidence to suggest that drug outlets contribute to the inappropriate use of antibiotics6 owing to a range of factors including drug outlets profit-making incentives, insufficient training, weak regulations and lack of monitoring and enforcement of rules on antibiotic dispensing.7
In Indonesia, the fourth most populous country in the world, there is widespread availability and use of antibiotics in a context of high utilisation of drug outlets.8 According to recent estimates, Indonesia’s 264 million population is served by approximately 135 000 drug outlets. These outlets may be licensed (including 28 671 community pharmacies and 10 849 drug stores, the latter only being authorised to sell over-the-counter medicines) or unlicensed (including an estimated 5000 drug stores and 90 000 grocery stores which also sell over-the-counter medicines).9–11 Community pharmacies can operate independently, or be part of a chain or attached to a clinic, or both. By law, all antibiotics must only be dispensed by licensed pharmacists after the presentation of a prescription12 while drug stores are prohibited from selling any type of antibiotic under any circumstance.13 In addition, pharmacies must always be attended by a qualified pharmacist and drug stores by a pharmacy technician, who oversee the dispensing of medicines.14
Despite these provisions, past studies show that antibiotics can easily be obtained from community pharmacies without a prescription and any initial assessment as to the appropriateness of the request.11 15 16 The Indonesian government has taken steps to curb antibiotic use through greater regulation of the production and distribution of antibiotics, antimicrobial resistance (AMR) control programmes in public hospitals including surveillance of antibiotic prescribing,17–19 and educational campaigns targeting the general public, healthcare providers, and journalists.17 18 20 While few would dispute that drug outlets have an important role to play in reducing the overuse of antibiotics in the community, to date most AMR strategies and policies in Indonesia have overlooked them.21
Like many LMICs, Indonesia has developed a national AMR Action Plan to minimise the development and spread of AMR. Our team are working closely with the AMR National Taskforce led by the Indonesian Ministry of Health (MoH) and stakeholders from district and provincial health offices, industry and the community to help strengthen this plan by providing important insights into the practices and motivations of drug outlets in Indonesia. This research is part of the PINTAR Project (Protecting Indonesia from the Threat of Antibiotic Resistance: https://www.pintarstudy.org/). The aim of this paper is to determine the magnitude and determinants of inappropriate dispensing of antibiotics by drug outlets in urban and rural settings in Indonesia, with a particular focus on the problem of dispensing antibiotics without a prescription.
Methods
This mixed-method study consists of two key components: a cross-sectional survey using standardised patients (SPs); and semistructured interviews with drug outlet staff. The survey was conducted between July and August 2019 and the interviews in August and September 2019.
Study setting
The study was conducted in two locations: Bekasi city in West Java Province (urban) and Tabalong district in South Kalimantan Province (rural). In consultation with representatives from the Indonesian MoH who are part of the research team and the PINTAR Advisory Committee, these two locations were purposively selected to capture geographic variation. Bekasi is an urbanised, industrial city, with 3.5 million inhabitants,22 while Tabalong is a semi-rural district with a population of 250,000.23 In 2019, the numbers of community pharmacies in Bekasi and Tabalong were 534 and 31 respectively, while the numbers of drug stores were 87 and 31.24 25
Cross-sectional survey using SP
A cross-sectional study was conducted in both locations using SPs. Also known as ‘mystery clients’ or ‘simulated patients’, an SP is an individual who is trained to interact with healthcare providers, simulate clinical symptoms or report on another person’s symptoms, and record the details of the interactions and observations against a predefined checklist.26 This approach aims to capture social interactions and behaviours, minimising response biases27 and has been used widely in public health studies, including in pharmacy practice28 and antibiotic dispensing studies in Indonesia15 16 and other settings.29–31 The strengths and limitations of the SP approach have been reviewed elsewhere.27 32 27 32 33
In this study, SPs portrayed three different clinical case types (table 1) developed also with the support of clinicians, public health experts and representatives from the Indonesian MoH. The clinical cases included were parent of a child at home with diarrhoea, an adult with presumptive tuberculosis (TB), and an adult with an upper respiratory tract infection (URTI). These cases were chosen because they reflect common health concerns in Indonesia34 and have been used in other SP surveys, thereby facilitating comparison.30 35 36 For each case type, we developed a standardised opening statement and scripted presentation that aimed to point the provider towards an appropriate case management action. In none of the cases should the SP be given an antibiotic without prescription12 13; and the staff should provide appropriate information when dispensing medicines.37
Table 1.
Description of the SP scenarios
| Cases | Enacted scenarios |
| Child diarrhoea | Parent with a child at home who has been unwell for several days with watery diarrhoea but no blood or mucus in the stool. |
| Presumptive TB in adult | Client experiencing deep yellow/green sputum-producing cough lasting for more than 4 weeks, fever especially at night, and weight loss due to decreasing appetite. |
| URTI in adult | Client experiencing flu-like symptoms including fever, runny nose and sore throat for the previous 2–3 days. |
SPs, standardised patients; TB, tuberculosis; URTI, upper respiratory tract infection.
Twenty-one SPs (7 males and 14 females) were recruited and received 5 days of training from experienced researchers and experts in SP training for medical education. Then, each SP presented the same case to multiple providers. Each drug outlet was visited consecutively by three different SPs presenting three different clinical scenarios. To reduce suspicion and possible detection, the three SPs made their visits over a 1–3 day interval at different times of the day to reduce the chance that SPs might be attended by the same staff member.
The SP interacted with whomever served them irrespective of their specific role (pharmacy/drug store owner, pharmacist, or pharmacy technician, staff, person-in-charge). If an antibiotic was not initially offered, the SP would ask for one. Immediately following each encounter, the SP completed a structured online questionnaire on history taking, advice or information provided by drug outlet staff, treatment provided, length of interaction, and the cost of medicines dispensed. Photographs of the drug packaging and receipts were also taken. The case scenario presented by SPs was the same regardless of the availability of a pharmacy professional.
The data recorded from the checklists included characteristics of drug outlets (whether it was a drug store, a standalone pharmacy, or a pharmacy attached to a clinic), characteristics of drug outlet staff attending the SP, and if an antibiotic was dispensed, the name of that antibiotic. During the interaction, the SP also asked if the pharmacist or pharmacy technician was available, and if an antibiotic was not dispensed, reasons for not providing one—this information was also recorded in the checklist. To minimise any Hawthorne effect,38 the question on the availability of pharmacists was asked at the end of the visit, after it was established whether an antibiotic was to be provided without prescription. After data collection, our study coordinator checked whether the medicines obtained by the SPs included antibiotics.
Selection of drug outlets and sample size
The sample size was calculated using the exact binomial CI,39 and was based on previous SP surveys in LMICs that measured antibiotic dispensing by community pharmacies without a prescription for the same three clinical cases presented in this study: 20% for TB,30 40% for child diarrhoea35 36 40 and 60% for URTI.35 36 With a sample size of 420 drug outlets (ie, 140 SP visits per clinical case), the exact 95% CI around these estimates, assuming a binary endpoint, would be 14%–28% for TB, 32%–49% for child diarrhoea, and 51%–68% for URTI. We felt this was an acceptable level of precision, excluding±10% in each case. Of the 683 drug outlets registered in the two districts, we surveyed 166 (121 pharmacies and 45 drug stores). We surveyed more than 140 drug outlets to allow for a 15% drop out rate.
We used stratified random sampling to select outlets in all subdistricts in Bekasi. Licensed drug outlets were identified and stratified by subdistrict and by type of outlet (ie, community pharmacy or drug store), using the District Health Office (DHO) registries.24 25 The drug outlets were selected randomly from each subdistrict with the number of outlets determined using the probability proportional to size method (ie, proportional to the total number of drug outlets in the subdistrict). In Tabalong, all drug outlets in all subdistricts were selected due to the small number of outlets in the district. Unlicensed drug outlets were not sampled because they are not included in the DHO registries.
Data management and statistical analysis
For the primary outcome (antibiotic dispensing without a prescription)the unit of analysis was a drug outlet/SP interaction. We also present a descriptive analysis of the reasons for not dispensing antibiotics, and types of antibiotics provided. Drawing on published evidence,7 29 41 univariate random effects logistic regression, clustered on SP, was used to identify the association of each potential predictor with the dispensing of antibiotics. Multivariable random effects logistic regression was then used to determine the influence of important covariates including the type of clinical case, and client and provider characteristics on antibiotic dispensing.32 42 All variables associated with antibiotic dispensing in the univariate analysis (p value less than 0.05) were included in the multivariate analysis. The statistical analyses were conducted using STATA V.16.1. Model calibration was assessed by the Hosmer-Lemeshow test. Model sensitivity, specificity and predictive values positive and negative were then computed.
Qualitative interviews
In parallel with the SP survey, in-depth interviews were conducted with a sample of pharmacists and other drug outlet staff, randomly selected from the list of survey participants. In line with the overarching study objectives, the interviews explored factors influencing antibiotic dispensing practices. While the interviews were flexible and adapted to the type of participant, key areas of focus included: (1) the business environment; (2) the supply of antibiotics; (3) antibiotic dispensing practices; and (4) knowledge and awareness of AMR and relevant regulations.
Potential participants were approached inside their pharmacies or drug stores and invited to participate in the interview. None refused to participate or dropped out during the interview. All interviews were conducted in Bahasa Indonesia by local researchers. In total, 31 participants were interviewed—16 in Bekasi and 15 in Tabalong district. Of those, 12 were owners, 3 were pharmacists, 12 were both the owner and pharmacist, and 4 were other drug outlet staff. Interviews were audio recorded, and transcribed verbatim. Written informed consent was obtained prior to each interview. The duration of the interviews ranged from 20 minutes to approximately 1 hour. To minimise inter-interviewer variation, training in social research methods and mock interviews was conducted under the supervision of a senior social scientist prior to data collection.
The qualitative dataset was analysed thematically to generate insights on antibiotic dispensing and factors that may influence inappropriate dispensing practices. With this aim in mind, emerging themes were identified using open coding and the data analysis software NVivo V.12. The emerging themes were then grouped under broad categories and used to structure the presentation of findings.
In the process of analysis, exemplary quotes were extracted from the interviews and translated into English by the lead Indonesian qualitative researcher (AF). The English translation was refined after discussion with the other investigators to clarify meaning and interpretation. The results include a selection of anonymised quotes to illustrate the findings.
Role of the funding source
The study sponsor had no role in the study design, data collection, data analysis and interpretation, writing the report, or the decision to submit the paper for publication.
Results
Cross-sectional survey using SPs
A total of 495 SP visits, out of 498 scheduled, were completed (362 visits to pharmacies, and 133 visits to drug stores). Three visits were not performed because SPs found staff in the drug outlet to be unfriendly or rude. Interactions with drug outlet staff lasted on average 5 minutes (n=394; 79.6%) and the majority of staff interacting with SPs were female (n=375; 75.8%). A pharmacist was available for 35.3% of visits to pharmacies (n=128/362) and a pharmacy technician for 17.4% of visits to drug stores (n=23/133). Comparing urban and rural areas, a pharmacist was available in 36.9% and 29.0% of visits; and a pharmacy technician was available in 21.3% and 14.1% of visits respectively.
During the visits, various types of medicines were provided by drug outlet staff, including symptomatic medicines, vitamins, and antibiotics.
Antibiotic dispensing practices
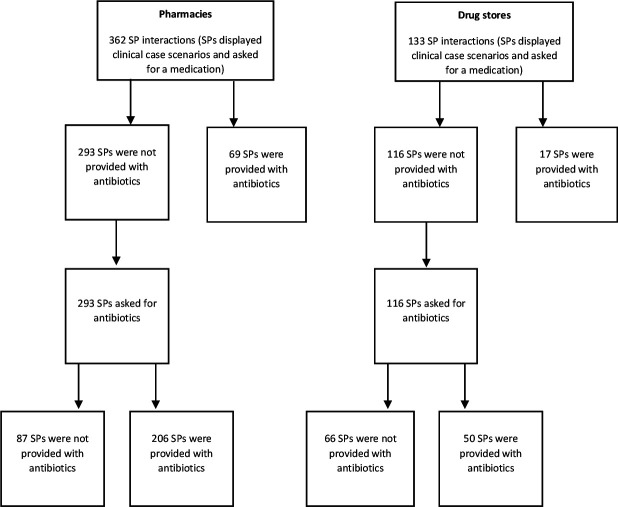
Antibiotics were given in 69% (342/495) of SP visits—76% (275/362) of pharmacy visits and 50.4% (67/133) of drug store visits. SPs presenting the child diarrhoea case obtained antibiotics in 47% (78/165) of interactions, and the figures were 80.6% (133/165) for presumptive TB, and 79.4% (131/165) for URTI. In 19.1% (69/362) and 12.8% (17/133) of SP visits to pharmacies and drug stores respectively, SPs were offered antibiotics on presentation of symptoms. Further, in 56.9% (206/362) and 37.6% (50/133) of visits, SPs received antibiotics after requesting them (table 2 and figure 1).
Table 2.
Overview of antibiotic dispensing without a prescription
| Outcomes | Number of interactions stratified by type of drug outlet | Total number of interactions N (%) (n=495) | |
| Pharmacy N (%) (n=362) |
Drug store N (%) (n=133) |
||
| Antibiotics provided before the SPs asked for them | 69 (19.1%) | 17 (12.8%) | 86 (17.4%) |
| Child diarrhoea | 10 (2.8%) | 1 (0.8%) | 11 (2.2%) |
| Presumptive TB | 22 (6.1%) | 5 (3.8%) | 27 (5.5%) |
| URTI | 37 (10.2%) | 11 (8.3%) | 48 (9.7%) |
| Antibiotics provided after the SPs asked for them | 206 (56.9%) | 50 (37.6%) | 256 (51.7%) |
| Child diarrhoea | 59 (16.3%) | 8 (6.0%) | 67 (13.5%) |
| Presumptive TB | 82 (22.7%) | 24 (18.0%) | 106 (21.4%) |
| URTI | 65 (18.0%) | 18 (13.5%) | 83 (16.8%) |
| No antibiotics were provided despite SP request | 87 (24.0%) | 66 (49.6%) | 153 (30.9%) |
| Child diarrhoea | 51 (14.1%) | 36 (27.1%) | 87 (17.6%) |
| Presumptive TB | 17 (4.7%) | 15 (11.3%) | 32 (6.5%) |
| URTI | 19 (5.2%) | 15 (11.3%) | 34 (6.9%) |
TB, tuberculosis; UTRI, upper respiratory tract infection.
Figure 1.
Flow chart of antibiotic dispensing without prescription at drug outlets. SP, standardised patient.
The reasons given by drug outlet staff for not providing antibiotics are summarised in table 3. At pharmacies, the most frequent explanation was that antibiotics can be dispensed only with a prescription (38%) or that they are not necessary or appropriate to treat the case (26.4%). At drug stores, the most common explanation was that antibiotics were not available (36.4%).
Table 3.
Reasons for not dispensing antibiotics
| Reasons for not dispensing antibiotics | Number of interactions stratified by drug outlet type N (%) |
Total number of interactions N (%) n=153 |
|
| Pharmacies (n=87) |
Drug stores (n=66) |
||
| No reasons provided | 10 (11.5%) | 12 (18.2%) | 22 (14.4%) |
| Need prescription | 33 (38.0%) | 4 (6.1%) | 37 (24.2%) |
| No need for antibiotics | 23 (26.4%) | 2 (3.0%) | 25 (16.3%) |
| Do not sell/stock antibiotics | 0 | 24 (36.4%) | 24 (15.7%) |
| Out of stock | 15 (17.2%) | 8 (12.1%) | 23 (15.0%) |
| Safety concerns | 3 (3.5%) | 4 (6.1%) | 7 (4.6%) |
| Sold other medicines | 1 (1.2%) | 4 (6.1%) | 5 (3.3%) |
| Sold herbal remedy | 0 | 5 (7.6%) | 5 (3.3%) |
| Do not sell antibiotics for 2 year olds | 0 | 3 (4.6%) | 3 (2.0%) |
| Recommended SP visit a general practitioner | 2 (2.3%) | 0 | 2 (1.3%) |
SP, standardised patient.
In almost half of the interactions where antibiotics were dispensed (43.3%), no instructions for use were provided to the SP (table 4). When instructions were given, it was most often related to the dosage regimen (frequency and duration). Specific advice on side effects (1.2%) and potential drug allergies (3.5%) was rarely provided.
Table 4.
Type of advice provided by drug outlet staff when dispensing antibiotics without prescription
| Type of advice provided when drug outlet staff dispensed antibiotics | Number of interactions N (%) n=342 |
95% CI |
| No advice at all | 148 (43.3%) | 38.0% to 49.0% |
| Dosage (frequency) | 169 (49.4%) | 44.1% to 55.0% |
| Duration | 127 (37.1%) | 32% to 42.6% |
| Directions (before or after meal, mixed with water, etc) | 90 (26.3%) | 21.8% to 31.4% |
| Drug allergies | 12 (3.5%) | 1.8% to 6.1% |
| Side effects | 4 (1.2%) | 0.3% to 3.0% |
Commonly dispensed antibiotics and their cost
Most SPs were given one antibiotic, with 3.2% (11/342) of encounters resulting in the dispensing of two antibiotics.
In child diarrhoea cases, the most commonly dispensed drug was trimethoprim (46/165, 27.9%), while amoxicillin was given in the majority of presumptive TB (83/165, 50.3%) and URTI cases (61/165, 37.0%) (table 5). In addition, lozenges containing fradiomycine and gramicidine were most commonly dispensed in the URTI cases (44/165, 26.7%), followed by cefadroxil (12/165, 7.3%) and ciprofloxacin (8/165, 4.8%). In the TB cases, ciprofloxacin or levofloxacin were dispensed in 12/165 (7.3%) and a cephalosporin (either cefadroxil or cefixime) in 32/165 (19.4%) of interactions. One SP received an unidentified antibiotic that was dispensed from a jar and packed using a plastic bag.
Table 5.
Types of antibiotics dispensed without prescription by drug outlet staff for each scenario
| Antibiotics provided for each case | Number of interactions per scenario N (%) |
Total N (%) (n=495) |
||
| Child diarrhoea (n=165) |
Presumptive TB (n=165) |
URTI (n=165) |
||
| No antibiotics provided | 87 (52.7%) | 32 (19.4%) | 34 (20.6%) | 153 (30.9%) |
| Amoxicillin | 13 (7.9%) | 83 (50.3%) | 56 (33.9%) | 152 (30.7%) |
| Trimethoprim | 43 (26.1%) | 1 (0.6%) | 1 (0.6%) | 45 (9.1%) |
| Fradiomycin/gramicidin (lozenges) | 0 | 0 | 39 (23.6%) | 39 (7.8%) |
| Cefadroxil | 2 (1.2%) | 22 (13.3%) | 11 (6.7%) | 35 (7.1%) |
| Ciprofloxacin | 0 | 10 (6.1%) | 7 (4.2%) | 17 (3.4%) |
| Cefixime | 0 | 10 (6.1%) | 5 (3.0%) | 15 (3%) |
| Nifuroxazide | 10 (6.1%) | 0 | 0 | 10 (2.0%) |
| Ampicillin | 0 | 4 (2.4%) | 1 (0.6%) | 5 (1%) |
| Amoxicillin and fradiomycin/gramicidin | 0 | 0 | 5 (3.0%) | 5 (1%) |
| Sulfamethoxazole | 4 (2.4%) | 0 | 0 | 4 (0.8%) |
| Trimethoprim/sulfamethoxazole and nifuroxazide | 3 (1.8%) | 0 | 0 | 3 (0.6%) |
| Metronidazole | 2 (1.2%) | 0 | 0 | 2 (0.4%) |
| Erythromycin | 0 | 1 (0.6%) | 1 (0.6%) | 2 (0.4%) |
| Thiamphenicol | 0 | 0 | 2 (1.2%) | 2 (0.4%) |
| Levofloxacin | 0 | 2 (1.2%) | 0 | 2 (0.4%) |
| Lincomycin | 0 | 0 | 1 (0.6%) | 1 (0.2%) |
| Amoxicillin and ciprofloxacin | 0 | 0 | 1 (0.6%) | 1 (0.2%) |
| Amoxicillin and cefadroxil | 0 | 0 | 1 (0.6%) | 1 (0.2%) |
| Cefadroxil and nifuroxazide | 1 (0.6%) | 0 | 0 | 1 (0.2%) |
The price of a full course of antibiotics for all cases ranged from IDR 4000 (US$0.27) to IDR 87 200 (US$5.9), with more than half (55%) costing IDR 10 000 (US$0.68) or below.
Factors associated with antibiotic dispensing without a prescription
In the univariate and multivariate analysis, only two covariates were associated with antibiotic dispensing without a prescription. For all scenarios, the odds of a staff member from a standalone pharmacy or a pharmacy attached to a clinic dispensing an antibiotic without a prescription, were higher compared with staff from drug stores; with an OR of 5.9 (95% CI 3.2 to 10.8) and 2.2 (95% CI 1.2 to 3.9). The odds of an SP presenting with presumptive TB and URTI receiving an antibiotic without prescription were about five times higher than for a child with diarrhoea, with an OR of 5.7 (95% CI 3.0 to 10.8) and 5.2 (95% CI 2.7 to 9.8), respectively. (table 6). Model calibration was adequate as assessed by the Hosmer-Lemeshow test (p=0.48). We observed a sensitivity of 0.60, a specificity of 0.76, a positive predictive value of 0.85 and a negative predictive value of 0.46.
Table 6.
Predictors of dispensing antibiotics without a prescription
| Predictors | Interactions | Univariate analysis | Multivariate analysis | |||
| Number of interactions in which antibiotic was dispensed N (%) n=342 |
Total number of interactions n=495 |
Or (95% CI) | P value | Or (95% CI) | P value | |
| District | ||||||
| Tabalong (rural district) | 99 (67.4%) | 147 | 1 | |||
| Bekasi (urban district) | 243 (69.8%) | 348 | 1.0 (1.0 to 1.0) | 0.786 | ||
| Type of drug outlets | ||||||
| Drugstore | 67 (50.4%) | 133 | 1 | 1 | ||
| Pharmacy attached to GP/specialist clinics | 83 (65.9%) | 126 | 2.4 (1.4 to 4.3) | 0.002 | 2.2 (1.2 to 3.9) | 0.007 |
| Standalone pharmacy | 192 (81.4%) | 236 | 7.4 (4.1 to 13.4) | <0.001 | 5.9 (3.2 to 10.8) | <0.001 |
| If a pharmacist or pharmacy technician was available during the visit | ||||||
| Yes | 98 (64.9%) | 151 | 1 | |||
| No or don’t know | 244 (70.9%) | 344 | 1.3 (0.8 to 2.0) | 0.242 | ||
| Gender of drug outlet staff | ||||||
| Female | 264 (70.4%) | 375 | 1.3 (0.8 to 2.1) | 0.348 | ||
| Male | 78 (65%) | 120 | 1 | |||
| Day or night visit | ||||||
| Day visit | 225 (67.2%) | 335 | 1 | |||
| Night visit | 117 (73.1%) | 160 | 1.3 (0.8 to 2.1) | 0.261 | ||
| Case | ||||||
| Child diarrhoea | 78 (47.3%) | 165 | 1 | 1 | ||
| Presumptive TB | 133 (80.6%) | 165 | 4.6 (2.8 to 7.6) | <0.001 | 5.7 (3.0 to 10.8) | <0.001 |
| URTI | 131 (79.4%) | 165 | 4.3 (2.6 to 7.0) | <0.001 | 5.2 (2.7 to 9.8) | <0.001 |
Model calibration was adequate as assessed by the Hosmer-Lemeshow test (p=0.48), with a sensitivity of 0.60, a specificity of 0.76, a positive predictive value of 0.85 and a negative predictive value of 0.46.
We also assessed risk factors for each infection separately (online supplemental files 1-3). In these analyses, only type of drug dispensary was statistically significant, again with standalone pharmacies and pharmacies attached to a clinic at higher odds of dispensing antibiotics compared to drug stores.
bmjgh-2021-004993supp001.pdf (70.4KB, pdf)
Qualitative study
In keeping with the survey findings, many participants (including pharmacists) said they would sell antibiotics without prescription to patients who requested them. As one pharmacist in Bekasi said, “Usually they know what they want: like ‘I want amoxicillin and paratusin – how much is it?’ That’s what they say” (32-20-1-612). However, a pharmacist in Tabalong said he was cautious when antibiotics were demanded for children: “If it is very severe, I would recommend them to go to hospital, for example if children have fever for more than three days” (63-28-1-750).
Our analysis of the interview data indicates that inappropriate dispensing was influenced by a range of different factors, considered in turn below.
Perceived patient demand
Participants explained that many people in the community believe that antibiotics are ‘powerful’ drugs which can cure many ailments, from a common cold to joint pain. One pharmacist said: “They want antibiotics for every condition even for muscle pain, and when we try to explain that antibiotics should be used for other diseases, they still want them” (32-11-1-102).
Unqualified drug sellers interacting with patients
Despite regulations requiring a qualified pharmacist (or in the case of drug stores, a pharmacy technician) to always be present during opening hours, some owners stated they could only afford to employ a pharmacist on a part-time basis. Furthermore, two owners said it was difficult to attract and retain pharmacists in rural areas as those with a university degree preferred to work in the cities.
Market competition
A common concern was that turning down a client’s request for antibiotics might have a negative impact on business, especially considering the widespread availability of antibiotics in the community. As a pharmacy owner in Tabalong explained: “Well we try to say no, but if they still want it [antibiotic without a prescription] then we just give it to them (…) If we say like ‘Oh it is not allowed’, and then they leave and go to another place, well you know we are selling stuff, we need to sell stuff out, we need to pay our staff” (32-13-1-286).
Weak power of pharmacists vis-à-vis owners
Power imbalances and conflict of interest between owners and pharmacists emerged as another driver of inappropriate dispensing. One pharmacist in Bekasi explained that “We sell antibiotics without prescription because we have no power to say [to the owner], ‘No, it should be like this’ [that antibiotics should only be sold with a prescription]” (32-11-1-102).
Weak enforcement of regulations
There was a consensus across respondents that enforcement of regulations was weak, despite the active role of professional pharmacist associations in both study locations. One pharmacist specifically complained about the sale of antibiotics at drug stores, stressing that these outlets should be monitored more frequently. In keeping with this perception, another drug store owner in Bekasi said she had never received any visits from local health authorities in the last decade.
Discussion
A striking finding from our study is that despite existing regulations, over two-thirds of visits to drug outlets in rural and urban sites in Indonesia resulted in the sale of at least one antibiotic without a prescription. Although first-line antibiotics such as amoxicillin and co-trimoxazole were the most widely dispensed antibiotics, it is of concern that second-line antibiotics including cephalosporin were dispensed without prescription. It was also troubling to see that SPs feigning presumptive TB were offered antibiotics that are not recommended for the treatment of TB and that antibiotics such as fradiomycin/gramicidin, often in the form of a lozenger, were widely used for URTIs.
Our results also showed that consultations at drug outlets were often inadequate with antibiotics frequently given with no or few instructions on their correct use. Similarly, despite regulations requiring pharmacies and drug stores to have a trained pharmacist or pharmacy technician present for patient consultations, this was not the case for 65% of visits to pharmacies and over 80% of visits to drug stores. These findings are consistent with earlier studies involving community pharmacies in Indonesia which show that patients can easily obtain antibiotics without a prescription from unqualified staff.16 Our research now shows that these problems also extend to drug stores in Indonesia.
While antibiotics were commonly dispensed without a prescription for all three clinical cases, SPs presenting with presumptive TB and URTI cases were more likely to be provided with an antibiotic compared with child diarrhoea cases. Studies among community pharmacies in India29 and China41 have found age to be an important determinant of dispensing antibiotics without a prescription, with paediatric cases being less likely to receive an antibiotic for the treatment of fever, diarrhoea and URTI.29 This is possibly due to the increased risk of adverse events in children, and people paying greater attention to medication safety in children.41 The type of drug outlet was also found to be an important determinant of dispensing antibiotics without prescription. Both standalone pharmacies and those attached to a clinic, were more likely to dispense antibiotics without prescription compared with drug stores. This may partly be due to the fact that the sale of antibiotics in drug stores is prohibited. Standalone pharmacies were more likely to dispense antibiotics without a prescription than those attached to a clinic. This may be due to closer oversight and supervision of pharmacies attached to clinics or because these pharmacies are more likely to be affiliated with the national health insurance (JKN) scheme. Under the JKN scheme, an affiliated pharmacy is responsible for the dispensing of the medicines prescribed by their GP network, and receive their income through capitation payments to those GPs.43 These affiliated pharmacies may therefore be in a stronger financial position compared with some standalone pharmacies seeking to supplement their income through dispensing of antibiotics without prescription.
A key strength of our study was the ability to explore reasons for the dispensing of antibiotics without prescription by drug outlet staff. Our qualitative analysis revealed that drug outlet staff often felt pressured by their clients to sell antibiotics without prescription. This was reinforced in the SP survey where 51.7% visits to drug outlets that did not initially offer an antibiotic, did so after being asked by the SP. This finding is consistent with several other studies in LMICs44 45 and high-income countries.46 Educational programmes targeting both drug outlets and communities could improve health seeking behaviour, and consequently reduce inappropriate antibiotic use.47 48 It has been suggested that schools of pharmacy in Indonesia need to provide further training in communication skills to better manage patient demand for antibiotics.37 Qualified pharmacists or pharmacy technicians were available in only a fraction of visits to surveyed outlets. Our interviews indicated that this is a result of difficulties in attracting and retaining graduates, especially in rural areas, and the financial pressures on pharmacy owners to reduce costs and maximise profit.
The generalisability of this research is limited by the fact that it was undertaken in two districts (ie, 24 subdistricts) in Indonesia. However, our results—in particular the high rates of dispensing without a prescription and insufficient advice given to clients—are consistent with earlier surveys conducted in other locations in Indonesia,15 16 49 suggesting that inappropriate dispensing of antibiotics among drug outlets is a widespread problem. There are some limitations concerning the SP approach that are also worthy of mention. First, our study reflects what happens when pharmacies or drug stores receive a completely unknown patient as opposed to a known, regular client, or a client who returns to the outlet after one round of ineffective treatment. It is conceivable that regular clients may be treated differently by staff at the drug outlets.30 Second, SPs are required to accurately document their interactions immediately after they leave a pharmacy or drug store. While SPs were intensively trained in the effective recall of interactions, all information may not have been recorded. Some studies audio-record interactions to minimise recall bias50 but in this study, ethics approval was not granted for this. Third, we did not measure the SP detection rate (ie, the proportion of SPs identified by providers as being SPs and not genuine clients) which helps to assess the validity of results.33 For most SP surveys in LMICs, this has been found to be quite low (0%–5%).33 Lastly, in the Indonesian context, drug stores are not permitted by law to sell antibiotics but were included in the study. While this might have lowered the magnitude of sales of antibiotics without prescription, it was important to provide an indication of the extent to which this law was being adhered to.
Enforcement of regulations around antibiotic use, especially in the private sector, continues to be the Achilles heel of resistance containment.51 This is not only because of the complex mix of factors driving dispensing practices of staff working at drug outlets but also due to concerns about equity of access (eg, difficulties accessing a prescription in remote/rural areas)52 and a lack of resources and political commitment to enforcement.53 Relying heavily on strict regulations, including prescription-only laws, to curb the use of antibiotics in the private sector is misguided.21 Innovative interventions in which the private sector can be engaged as a partner have the potential to increase policy impact, given the unique position of pharmacists and other drug sellers as major suppliers of antibiotics in the community. Establishing surveillance systems capable of tracking antibiotic sales at the community level would also help to enforce existing regulations. As discussed, however, key questions remain about important health system and structural challenges to policy implementation such as the difficulties in attracting pharmacists to rural areas, and conflicting demands arising from financial incentives and market competition. Considering Indonesia’s large population and the potential for the global spread of resistant bacteria, these questions are crucial to national planning and global health action to address AMR. To date, the results of this research have been fed back to the National AMR Taskforce, the National Health Research and Development Agency, and DHOs in the study sites. Our team continues to work with local stakeholders to support the development of low-cost scalable interventions to optimise antibiotic use by dispensing staff at drug outlets in Indonesia.
Conclusion
AMR is an important global health challenge, primarily driven by misuse and/or overuse of antibiotics. Reducing inappropriate use of antibiotics is essential in the fight against drug resistance. This study shows that the dispensing of antibiotics without a prescription at drug outlets is common in the study sites, despite their being clear regulations to prohibit this. Stronger enforcement of current regulations is one strategy to address this driver of drug resistance but is unlikely to provide a complete solution to the problem. A multifaceted approach should be considered, taking into account the profit-maximising motives of drug outlets, the high demand for antibiotics among clients, and the push from owners to compete with other outlets, including drug stores which dispense antibiotics despite being prohibited from selling this class of medication. Looking ahead, attention to the role of drug outlets as a source of inappropriate antibiotic use may become even more important in Indonesia where major healthcare reforms such as the provision of free essential medicines under the national health insurance scheme, may put drug outlets in a weaker financial position, prompting them to supplement their income through the dispensing of antibiotics without prescription. There is currently limited research focusing on drug outlets. Research identifying and evaluating strategies to address inappropriate dispensing of antibiotics by this prominent group of providers is urgently needed in order to improve the quality of care and reduce the spread of AMR.
Acknowledgments
We thank the Indonesian Ministry of Health, Indonesian Pharmacist Association, Indonesian Pharmacy Technician Association at the national, provincial, and district levels, District Health Offices of Tabalong and Bekasi, National Institute for Health Research and Development, academics, and community organisations for their support and guidance, and participants involved in this study. We would also like to acknowledge the support provided by the SP Working Group (an international collaboration to advance the use of the SP approach in public health reserach in low and middle income countries), in particular advice provided by Rosalind Miller, Catherine Goodman and Jishnu Das on the development of SP scenarios and training resources.
Footnotes
Handling editor: Sanni Yaya
Twitter: @MsLilaWulandari, @DrMishalK
Contributors: LPLW, MK, ML, AF, YAM, AP, TW, NB, GS, JK, RG, ML, RD, JH, HP, SJ, SY and VW conceptualised the study. LPLW, MK, ML, AF, YAM, AP, TW and VW collected the quantitative and qualitative data. LPLW, MK, ML, AF, YAM, AP and VW analysed and interpreted the data. LPLW developed the manuscript draft. LPLW, MK, ML, AF, YAM, AP, TW, NB, SY, VW, ML, ML, RG, JK, SJ and GS edited the manuscript draft. All the authors approved the final manuscript.
Funding: This study was funded by a grant from the Indo-Pacific Centre for Health Security (Australian Department of Foreign Affairs and Trade) under the Stronger Health Systems for Health Security Scheme.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Datasets used in the analysis may be available upon request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethics approval was granted by the Universitas Gadjah Mada (KE/FK/0161/EC/2019) and the University of New South Wales (HC190043) research ethics committees. Informed consent was obtained for all in-depth interviews and a waiver of consent granted for the drug outlet involved in the SP survey.
References
- 1. Bell BG, Schellevis F, Stobberingh E, et al. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis 2014;14:13. 10.1186/1471-2334-14-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Malik B, Bhattacharyya S. Antibiotic drug-resistance as a complex system driven by socio-economic growth and antibiotic misuse. Sci Rep 2019;9:9788. 10.1038/s41598-019-46078-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miller R, Goodman C. Performance of retail pharmacies in low- and middle-income Asian settings: a systematic review. Health Policy Plan 2016;31:940–53. 10.1093/heapol/czw007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goodman C, Kachur SP, Abdulla S, et al. Drug shop regulation and malaria treatment in Tanzania--why do shops break the rules, and does it matter? Health Policy Plan 2007;22:393–403. 10.1093/heapol/czm033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Suy S, Rego S, Bory S, et al. Invisible medicine sellers and their use of antibiotics: a qualitative study in Cambodia. BMJ Glob Health 2019;4:e001787. 10.1136/bmjgh-2019-001787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Auta A, Hadi MA, Oga E, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect 2019;78:8–18. 10.1016/j.jinf.2018.07.001 [DOI] [PubMed] [Google Scholar]
- 7. Servia-Dopazo M, Figueiras A. Determinants of antibiotic dispensing without prescription: a systematic review. J Antimicrob Chemother 2018;73:3244–53. 10.1093/jac/dky319 [DOI] [PubMed] [Google Scholar]
- 8. Widayati A, Suryawati S, de Crespigny C, et al. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes 2011;4:491. 10.1186/1756-0500-4-491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bank W. Pharmaceuticals : why reform is needed (English). Indonesia health sector review : policy and discussion notes. Washington, DC: World Bank, 2009. [Google Scholar]
- 10. Indonesian Ministry of Health . Mapping of Pharmaceutical Facilities 2013 - 2018 (Aplikasi Pemetaan Sarana Kefarmasian 2013-2018) Jakarta, 2019. Available: http://apif.binfar.depkes.go.id/index.php?req=view_services&p=pemetaanIndustriFarmasi
- 11. Chee G, Borowitz M, Barraclough A. Private sector health care in Indonesia. Bethesda, MD: Abt Associates Inc, 2009. [Google Scholar]
- 12. Indonesian Ministry of Health . Undang Undang Obat Keras (St. No. 419 tgl. 22 Desember 1949), 1949. [Google Scholar]
- 13. Indonesian Food and Drug Administration (FDA) . Peraturan BPOM No 4 Th. 2018 : Pengawasan Obat Narkotika, Psikotropika, dan Prekursor [Indonesian FDA Regulation on Monitoring and Supervison of Narcotics Psychotropics and Drug Precursor],, 2018. [Google Scholar]
- 14. Presiden Republik Indonesia . Peraturan Pemerintah Republik Indonesia Nomor 51 Tahun 2009 tentang pekerjaan kefarmasian. Jakarta, 2009. [Google Scholar]
- 15. Hadi U, van den Broek P, Kolopaking EP, et al. Cross-sectional study of availability and pharmaceutical quality of antibiotics requested with or without prescription (over the counter) in Surabaya, Indonesia. BMC Infect Dis 2010;10:203. 10.1186/1471-2334-10-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Puspitasari HP, Faturrohmah A, Hermansyah A. Do Indonesian community pharmacy workers respond to antibiotics requests appropriately? Trop Med Int Health 2011;16:840–6. 10.1111/j.1365-3156.2011.02782.x [DOI] [PubMed] [Google Scholar]
- 17. Yuliati D. Guidelines on Implementation of Antimicrobial Resistance Program in Indonesia (Landasan Pelaksanaan Program Pengendalian Resistensi Antimikroba di Indonesia). Simposium Nasional Upaya Peningkatan Kesadaran Pencegahan Penyakit dan Penggunaan Antimikroba yang Baik dan Benar :“More Protection, Less Antimicrobial”. Jakarta, 2018. [Google Scholar]
- 18. The Indonesian Ministry of Health . National action plan antimicrobial resistance Indonesia 2017-2019, 2017. [Google Scholar]
- 19. Indonesian Ministry of Health. . Ministry of health regulation number 8 2015 regarding antimicrobial resistant control at hospital settings, 2015. [Google Scholar]
- 20. Indonesian Ministry of Health . Gema cermat, 2017. Available: http://farmalkes.kemkes.go.id/category/gemacermat/#.XAo5rNszb3g
- 21. Wulandari LPL, Wiseman V. Engaging the private sector to improve antimicrobial use in the community. Phpma 2018;6:79. 10.15562/phpma.v6i2.187 [DOI] [Google Scholar]
- 22. Central Bureau Statistics of Bekasi . Bekasi in figures, 2018. [Google Scholar]
- 23. Central Bureau Statistics of Tabalong . Tabalong in figures, 2018. [Google Scholar]
- 24. Tabalong District Health Office . District health office (DHO) registry of registered community pharmacies and drugstores. Tabalong: Tabalong District Health Office, 2019. [Google Scholar]
- 25. Bekasi District Health Office . District health office (DHO) registry of registered community pharmacies and drugstores. Bekasi: Bekasi District Health Office, 2019. [Google Scholar]
- 26. Wiseman V, Lagarde M, Kovacs R, et al. Using unannounced standardised patients to obtain data on quality of care in low-income and middle-income countries: key challenges and opportunities. BMJ Glob Health 2019;4:e001908. 10.1136/bmjgh-2019-001908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Siminoff LA, Rogers HL, Waller AC, et al. The advantages and challenges of unannounced standardized patient methodology to assess healthcare communication. Patient Educ Couns 2011;82:318–24. 10.1016/j.pec.2011.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Watson MC, Norris P, Granas AG. A systematic review of the use of simulated patients and pharmacy practice research. Int J Pharm Pract 2010;14:83–93. 10.1211/ijpp.14.2.0002 [DOI] [PubMed] [Google Scholar]
- 29. Nafade V, Huddart S, Sulis G, et al. Over-The-Counter antibiotic dispensing by pharmacies: a standardised patient study in Udupi district, India. BMJ Glob Health 2019;4:e001869. 10.1136/bmjgh-2019-001869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Satyanarayana S, Kwan A, Daniels B, et al. Use of standardised patients to assess antibiotic dispensing for tuberculosis by pharmacies in urban India: a cross-sectional study. Lancet Infect Dis 2016;16:1261–8. 10.1016/S1473-3099(16)30215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Horumpende PG, Sonda TB, van Zwetselaar M, et al. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro region in Tanzania: a simulated clients approach. PLoS One 2018;13:e0207465. 10.1371/journal.pone.0207465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kwan A, Daniels B, Bergkvist S, et al. Use of standardised patients for healthcare quality research in low- and middle-income countries. BMJ Glob Health 2019;4:e001669. 10.1136/bmjgh-2019-001669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. King JJC, Das J, Kwan A, et al. How to do (or not to do) … using the standardized patient method to measure clinical quality of care in LMIC health facilities. Health Policy Plan. In Press 2019;34:625–34. 10.1093/heapol/czz078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. The Indonesian Ministry of Health . Riset Kesehatan Dasar (Riskesdas), 2018. [Google Scholar]
- 35. Chang J, Ye D, Lv B, et al. Sale of antibiotics without a prescription at community pharmacies in urban China: a multicentre cross-sectional survey. J Antimicrob Chemother 2017;72:dkw519–42. 10.1093/jac/dkw519 [DOI] [PubMed] [Google Scholar]
- 36. Erku DA, Aberra SY. Non-prescribed sale of antibiotics for acute childhood diarrhea and upper respiratory tract infection in community pharmacies: a 2 phase mixed-methods study. Antimicrob Resist Infect Control 2018;7:92. 10.1186/s13756-018-0389-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hermansyah A, Wulandari L, Kristina SA, et al. Primary health care policy and vision for community pharmacy and pharmacists in Indonesia. Pharm Pract 2020;18:2085. 10.18549/PharmPract.2020.3.2085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Franke RH, Kaul JD. The Hawthorne experiments: first statistical interpretation. Am Sociol Rev 1978;43:623–43. 10.2307/2094540 [DOI] [Google Scholar]
- 39. Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Statistical Science 2001;16:101–17. 10.1214/ss/1009213286 [DOI] [Google Scholar]
- 40. Pham DM, Byrkit M, Pham HV, et al. Improving pharmacy staff knowledge and practice on childhood diarrhea management in Vietnam: are educational interventions effective? PLoS One 2013;8:e74882. 10.1371/journal.pone.0074882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shi L, Chang J, Liu X, et al. Dispensing antibiotics without a prescription for acute cough associated with common cold at community pharmacies in Shenyang, northeastern China: a cross-sectional study. Antibiotics 2020;9. 10.3390/antibiotics9040163. [Epub ahead of print: 06 04 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kwan A, Daniels B, Saria V, et al. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med 2018;15:e1002653. 10.1371/journal.pmed.1002653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hermansyah A, Sainsbury E, Krass I. Investigating the impact of the universal healthcare coverage programme on community pharmacy practice. Health Soc Care Community 2018;26:e249–60. 10.1111/hsc.12506 [DOI] [PubMed] [Google Scholar]
- 44. Gebretekle GB, Serbessa MK. Exploration of over the counter sales of antibiotics in community pharmacies of Addis Ababa, Ethiopia: pharmacy professionals' perspective. Antimicrob Resist Infect Control 2016;5:2. 10.1186/s13756-016-0101-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nga DTT, Chuc NTK, Hoa NP, et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: an observational study. BMC Pharmacol Toxicol 2014;15:6. 10.1186/2050-6511-15-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dameh M, Norris P, Green J. New Zealand pharmacists' experiences, practices and views regarding antibiotic use without prescription. J Prim Health Care 2012;4:131–40. 10.1071/HC12131 [DOI] [PubMed] [Google Scholar]
- 47. Setiadi AP, Wibowo Y, Brata C, et al. The role of pharmacists in community education to promote responsible self-medication in Indonesia: an application of the spiral educational model. Int J Clin Pharm 2020;42:1088–96. 10.1007/s11096-020-01055-8 [DOI] [PubMed] [Google Scholar]
- 48. Cuevas C, Batura N, Wulandari LPL, et al. Improving antibiotic use through behaviour change: a systematic review of interventions evaluated in low- and middle-income countries. Health Policy Plan 2021;36:754–73. 10.1093/heapol/czab021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brata C, Schneider CR, Marjadi B, et al. The provision of advice by pharmacy staff in eastern Indonesian community pharmacies. Pharm Pract 2019;17:1452–52. 10.18549/PharmPract.2019.2.1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kwan A, Bergkvist S, Daniels B. Supplementary data: using standardized patients to measure health care quality : a manual and toolkit for projects in low- and middle-income countries. BMJ Global Health 2019;4. 10.1136/bmjgh-2019-001669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bebell LM, Muiru AN. Antibiotic use and emerging resistance: how can resource-limited countries turn the tide? Glob Heart 2014;9:347–58. 10.1016/j.gheart.2014.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Carlet J, Pittet D. Access to antibiotics: a safety and equity challenge for the next decade. Antimicrob Resist Infect Control 2013;2:1. 10.1186/2047-2994-2-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. World Health Organization . The evolving threat of antimicrobial resistance: options for action, 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-004993supp001.pdf (70.4KB, pdf)
Data Availability Statement
Datasets used in the analysis may be available upon request.