Abstract
Objectives: Complementary health approaches include herbal products and mind–body practices. Several studies have identified predictors for complementary health approach use, yet there are two gaps: (1) How does use change? (2) Do factors associated with use influence this change over time? Using the Midlife in the United States (MIDUS), we examined how sociodemographic factors affected use longitudinally, and whether these associations differed between new and continued/discontinued use of herbal products, meditation, chiropractic, and massage therapy.
Design: MIDUS is a national probability sample of adults aged 25 or older that has collected more than 20 years of longitudinal data, including the use of complementary health approaches. We employed the Andersen Model as a framework to identify predisposing, enabling, and health need factors associated with complementary health approach use based on previously identified and hypothesized factors. We ran Chi-square analyses to first test bivariate associations between our independent variables and four modalities to further guide logistic regression models.
Results: Each of the four approaches examined saw substantial increases in prevalent use. However, only about 25% to 38% of individuals continued use from one wave to the next, whereas only 2%–9% of individuals who did not use a given approach in a wave reported use in the subsequent wave. Age, spiritual importance, and previous wave one use were all significantly associated with new use across all four modalities. Previous wave one use was associated with continued/discontinued use for all modalities. Age and education were significantly associated with discontinued use of chiropractic.
Conclusion: We present the first longitudinal analysis of complementary health approaches in a nationally representative sample. These data distinguish between new and continued/discontinued use of complementary health approaches over time and provide insights into the interpretation of complementary health approach prevalence data, as well as important predictors of use.
Keywords: Midlife in the U.S. (MIDUS), complementary therapies, herbal products, chiropractic, meditation, massage therapy
Introduction
Complementary health approaches refer to several modalities ranging from herbal products to mind and body practices. The use of these health approaches has been associated with chronic health conditions and other sociodemographic and economic characteristics.1,2 Cross-sectional studies showed that trends in adult use of both chiropractic therapy and meditation in the United States have increased between 2002 and 2017.3,4 These analyses indicated a significant quadratic trend in the overall use of complementary health approaches after controlling for sex, race, education, poverty status, and health insurance status.
Additional research has demonstrated that complementary health approach users are more likely to identify as female, report multiple chronic health conditions, are younger than 65 years of age, and have a higher socioeconomic status compared with nonusers.3,5 It has also been suggested that a history of discontinuation of some negative health behaviors may be associated with the use of complementary health approaches, particularly for the self-management of addictive behaviors such as smoking.3
Many cross-sectional studies on complementary health approach use describe several factors that can be organized by using Andersen's Behavioral Model of Health Services Use—predisposing (e.g., age, sex, and race), enabling (e.g., insurance status and income), and need factors (e.g., health or disease status).6 What is not known is whether these factors are associated with complementary health approach use over time, and how they inform new and continued or discontinued complementary health approach use. Some longitudinal studies find complementary health approach users to be “one-off users” or “earnest seekers,” who use a modality for a short time period.7,8 We believe that predisposing factors that include biological imperatives such as age and sex may have a more stable and permanent effect on complementary health approach use compared with enabling and health need factors that may fluctuate more often over time.
Although a handful of national cross-sectional data sources on complementary health approach use exist,6,9–18 no nationally representative longitudinal studies containing recent data on complementary health approaches exist19–21 despite specific guidance by the Institute of Medicine in 2005: “Longitudinal cohort studies can [explain] people's trajectories of complementary and alternative medicine use and those factors that influence upward and downward rates of use.” To fill this knowledge gap, we set two objectives for the current study: (1) to investigate an individual's use of complementary health approach modalities over time; new, continuous, or discontinued use of these approaches; and (2) to employ the Andersen Model to identify factors associated with the use of complementary health approaches over time.
We hypothesized that predisposing factors would be associated with complementary health approaches over time, with sociodemographic factors more likely to predict new use of complementary health approaches after adjusting for enabling and health need factors. To meet these objectives, we used multiple waves of data from The Midlife in the United States (MIDUS) survey. MIDUS has collected more than 20 years of data on complementary health approach use, but thus far only cross-sectional analyses have been conducted on data of complementary health approach use from wave 1 (1995–1996) to wave 2 (2004–2005) of data collection.1–2,22–24
Materials and Methods
Sample
The MIDUS survey is a national probability sample of noninstitutional, English-speaking adults aged 25–74 residing in the 48 contiguous states in the United States whose households included at least one telephone. The initial wave of MIDUS participants were recruited and interviewed between 1995 and 1996 by the MacArthur Foundation Research Network on Successful Midlife Development.25 Households were first selected with random digit dialing. An adult from each household was then selected randomly for a final sample of 7,108 noninstitutionalized, English-speaking adults.
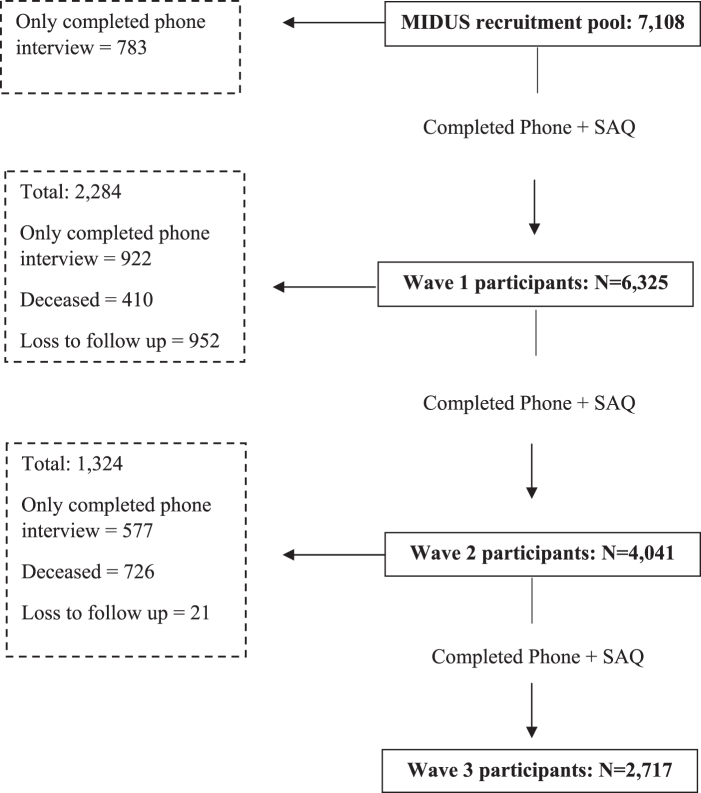
A total of 6,325 individuals sampled for wave 1 completed the interview and a self-administered questionnaire (SAQ), as shown in Figure 1. The second wave of MIDUS data collection occurred in 2004 and totaled 4,041 participants completing the phone interview and SAQ2. The average follow-up interval between wave 1 and wave 2 was ∼9 years. A third wave of follow-up occurred in 2013 and totaled 2,717 participants who completed both the phone interview and SAQ3.
FIG. 1.
Flow chart of MIDUS participants recruited in wave 1 (1995–1996), and followed in wave 2 (2004–2005), and wave 3 (2013–2014). MIDUS, Midlife in the United States; SAQ, self-administered questionnaire.
The National Institutes of Health Office of Human Subjects Research Protection (OHSRP ID#: 18-NCCIH-00693 issued 8/30/2018) authorized an exemption from the Institutional Review Board for these specific analyses, because they used publicly available, de-identified data freely available on the MIDUS website.
Measures
Dependent variables
The MIDUS survey included questions on several complementary health approaches. Participants were asked whether they had used any of these approaches to treat a physical health problem, an emotional or personal problem, maintain or enhance wellness, or to prevent the onset of an illness. The four most frequently reported approaches in the U.S. adult population—chiropractic, herbal products, meditation, and massage therapy—were dichotomized as “used” or “not used.”26–28
These approaches are not clearly defined or exemplified in the survey and, therefore, may include many different types of treatments. Chiropractic care could include treatments such as spinal manipulation, mobilization, or trigger point work. Herbal products can range from a single extract to complex mixtures in the form of a capsule or tea and could include common dietary supplements such as echinacea or turmeric. Meditation could include mindfulness, mantra meditation, and spiritual meditation, including prayer. Massage therapy could include Swedish, Shiatsu, Tuina massage, or Rolfing. Use of acupuncture, biofeedback, and homeopathy were considered for inclusion in the analysis, but they were excluded due to small sample sizes. The complete coding and questions for all variables is displayed in Supplementary Appendix SA1.
Independent variables
We chose six predisposing factors, including sociodemographic variables and psychological factors. Sociodemographic factors included sex (male [reference] and female), age in years (25–44; 45–64 [reference]; 65+), race (white, other [reference]), and education (less than high school; high school, general educational development (GED), associate's degree; bachelor's degree [reference]; advanced degree). Psychological factors included spiritual importance to the participant at the time of each survey wave (not or not very important [reference] and somewhat to very important) and depression (yes [reference], no).
Covariates
We chose five enabling and health need variables previously associated with the prevalence of complementary health approaches.3,22,29–31 Additional analysis of these variables is shown separately in Supplementary Appendices SA2 and SA3. Three of the variables represent enabling factors characterized by marital status (married/not married/never married [reference]), household total income, and health insurance status. Household total income included a calculation of total wages, pensions, social security, and other government assistance (tertiarily distributed as: $0 to 35000 [reference]; $35001 to 75000; and $75001 to 300000 U.S. dollars). We assessed health insurance status as a dichotomous variable (currently insured, uninsured [reference]), with coverage including employer-based, government, or from a spouse.
We considered health need factors as those that can precipitate the use of conventional care or promote the use of complementary health approaches. Need factors were represented by three painful conditions (migraine headaches, joint/bone disease, and sciatica/lumbago/recurring backache) and smoking status. Participants were asked whether they had experienced or been treated for each of the three chronic conditions (yes, no [reference]) in the past 12 months. Smoking status was considered never smoked, used to smoke [reference], or currently smoke at the time of the survey.
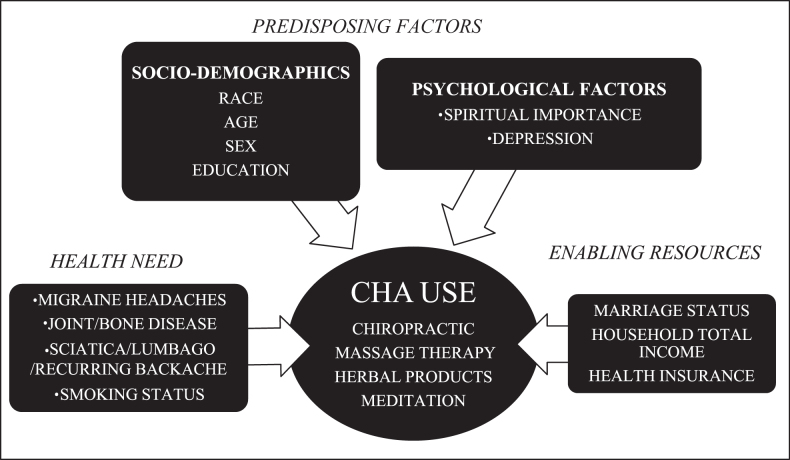
Dependent, independent, and covariate variables are categorically displayed in Figure 2.
FIG. 2.
Model variables used from MIDUS to predict complementary health approaches (chiropractic, herbal products, meditation, and massage therapy) based on the Andersen Behavioral Model of Health Services Use model. CHA, complementary health approach; MIDUS, Midlife in the United States.
Data analyses
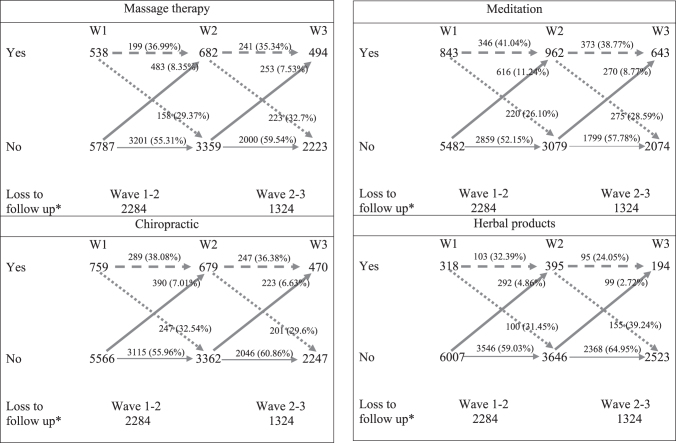
All analyses included people who completed both the survey and SAQ. Descriptive statistics, including prevalence estimates for all factor variables, are presented in Table 1 and shown for each wave. Prevalence data were analyzed from those who newly used each complementary health approach in wave 1 to 2 or wave 2 to 3, as well as participants who continued or discontinued complementary health approach use in both wave 1 and 2 or both wave 2 and 3 (Fig. 3). Longitudinal usage patterns were ascertained to restricting individuals who had completed SAQ and complementary health approach use questions for at least two of the three waves. Table 2 displays all possible usage patterns denoted by “Y” as yes, “N” as no, and “M” as missing, and read left to right signifying the order of wave 1, 2, and 3.
Table 1.
Descriptive Statistics of Measured Variables
| Wave 1 (N = 6325) |
Wave 2 (N = 4041) |
Wave 3 (N = 2717) |
|
|---|---|---|---|
| N (%) SE | N (%) SE | N (%) SE | |
| Predisposing factors | |||
| Sociodemographics | |||
| Race | |||
| White | 5600 (88.54) 0.40 | 3698 (91.92) 0.43 | 2424 (89.94) 0.58 |
| Other | 725 (11.46) 0.40 | 325 (8.08) 0.43 | 271 (10.06) 0.58 |
| Age | |||
| 25–44 years | 2885 (45.70) 0.63 | 813 (20.12) 0.63 | 56 (2.06) 0.27 |
| 45–64 | 2696 (42.71) 0.62 | 2118 (52.41) 0.79 | 1332 (49.02) 0.96 |
| 65+ | 732 (11.60) 0.40 | 1110 (27.47) 0.70 | 1329 (48.91) 0.96 |
| Sex | |||
| Female | 3321 (52.51) 0.63 | 2239 (55.41) 0.78 | 1503 (55.32) 0.95 |
| Male | 3004 (47.49) 0.63 | 1802 (44.59) 0.78 | 1214 (44.68) 0.95 |
| Education | |||
| Less than high school | 566 (8.97) 0.36 | 246 (6.10) 0.38 | 131 (4.83) 0.41 |
| High school, GED, AD | 3735 (59.17) 0.62 | 2249 (55.72) 0.78 | 1441 (53.17) 0.96 |
| BA/BS | 1322 (20.94) 0.51 | 912 (22.60) 0.66 | 651 (24.02) 0.82 |
| Advanced degree | 689 (10.92) 0.39 | 629 (15.58) 0.57 | 487 (17.97) 0.74 |
| Psychological factors | |||
| Spiritual importance | |||
| Not or not very important | 1399 (22.64) 0.53 | 664 (16.84) 0.60 | 454 (17.04) 0.73 |
| Somewhat to very important | 4779 (77.36) 0.53 | 3280 (83.16) 0.60 | 2210 (82.96) 0.73 |
| Depression | |||
| Yes | 674 (10.66) 0.39 | 349 (8.64) 0.44 | 200 (7.36) 0.50 |
| No | 5651 (89.34) 0.39 | 3692 (91.36) 0.44 | 2517 (92.64) 0.50 |
| Enabling resources | |||
| Marriage status | |||
| Married now | 4273 (67.59) 0.59 | 2865 (71.00) 0.71 | 1810 (66.69) 0.90 |
| Not married | 1307 (20.67) 0.51 | 868 (21.51) 0.65 | 710 (26.16) 0.84 |
| Never married | 742 (11.74) 0.40 | 302 (7.48) 0.41 | 194 (7.15) 0.49 |
| Household total income | |||
| 0–35,000 | 1907 (30.21) 0.59 | 1175 (30.49) 0.74 | 1058 (44.42) 1.02 |
| 35,001–75,000 | 2154 (35.25) 0.61 | 1269 (32.93) 0.76 | 797 (33.46) 0.97 |
| 75,001–300,000+ | 2049 (33.54) 0.60 | 1410 (36.59) 0.78 | 527 (22.12) 0.85 |
| Health insurance | |||
| Currently insured | 5601 (89.62) 0.39 | 3713 (92.96) 0.40 | 2577 (95.80) 0.39 |
| Uninsured | 649 (10.38) 0.39 | 281 (7.04) 0.40 | 113 (4.20) 0.39 |
| Health need | |||
| Joint/bone disease | |||
| Yes | 1226 (19.54) 0.5 | 1060 (26.23) 0.69 | 758 (28.47) 0.87 |
| No | 5049 (80.46) 0.5 | 2981 (73.77) 0.69 | 1904 (71.53) 0.87 |
| Sciatica/lumbago/recurring backache | |||
| Yes | 1222 (19.50) 0.5 | 680 (16.83) 0.59 | 511 (19.20) 0.76 |
| No | 5046 (80.50) 0.5 | 3361 (83.17) 0.59 | 2151 (80.80) 0.76 |
| Migraine headaches | |||
| Yes | 634 (10.07) 0.38 | 279 (6.90) 0.40 | 159 (5.97) 0.46 |
| No | 5662 (89.93) 0.38 | 3762 (93.10) 0.40 | 2503 (94.03) 0.46 |
| Smoking status | |||
| Never smoked | 3080 (48.73) 0.63 | 2076 (51.37) 0.79 | 1503 (55.34) 0.95 |
| Used to smoke | 1865 (29.50) 0.57 | 1376 (34.05) 0.75 | 972 (35.79) 0.92 |
| Current smoker | 1376 (21.77) 0.52 | 589 (14.58) 0.56 | 241 (8.87) 0.55 |
| Complementary health approach | |||
| Massage | |||
| Yes | 538 (8.51) 0.35 | 682 (16.88) 0.59 | 494 (18.18) 0.74 |
| No | 5787 (91.49) 0.35 | 3359 (83.12) 0.59 | 2223 (81.82) 0.74 |
| Chiropractic | |||
| Yes | 759 (12) 0.41 | 679 (16.80) 0.59 | 470 (17.3) 0.73 |
| No | 5566 (88) 0.41 | 3362 (83.20) 0.59 | 2247 (82.7) 0.73 |
| Herbal | |||
| Yes | 318 (5.03) 0.27 | 395 (9.77) 0.47 | 194 (7.14) 0.49 |
| No | 6007 (94.97) 0.27 | 3646 (90.23) 0.47 | 2523 (92.86) 0.49 |
| Meditation | |||
| Yes | 843 (13.33) 0.43 | 962 (23.81) 0.67 | 643 (23.67) 0.82 |
| No | 5482 (86.67) 0.43 | 3079 (76.19) 0.67 | 2074 (76.33) 0.82 |
AD, Associate's degree; BA/BS, Bachelor of Art or Bachelor of Science degree; GED, general educational development; SE, standard error.
FIG. 3.
Prevalence use of massage therapy, meditation, chiropractic, and herbal products across wave 1, 2, and 3.
 = Continued use
= Continued use
 = New use
= New use
 = Discontinued use
= Discontinued use
*Mortality and those who dropped out early and did not complete the survey.
W1, wave 1 (1995–1996); W2, wave 2 (2004–2005); W3, wave 3 (2013–2014).
Table 2.
Individual Usage Patterns of Complementary Health Approaches
| Massage therapy |
Chiropractic |
Herbal products |
Meditation |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Usage patterna | Frequency | Percent | Usage patterna | Frequency | Percent | Usage patterna | Frequency | Percent | Usage patterna | Frequency | Percent |
| NNN | 1751 | 42.54 | NNN | 1754 | 42.61 | NNN | 2109 | 51.24 | NNN | 1553 | 37.73 |
| NNM | 1182 | 28.72 | NNM | 1122 | 27.26 | NNM | 1267 | 30.78 | NNM | 1056 | 25.66 |
| NNY | 182 | 4.42 | NNY | 157 | 3.81 | NMN | 131 | 3.18 | NYN | 211 | 5.13 |
| NYN | 176 | 4.28 | YYY | 143 | 3.47 | NYN | 122 | 2.96 | NYY | 192 | 4.66 |
| NMY | 145 | 3.52 | NYN | 140 | 3.40 | NMY | 96 | 2.33 | NMY | 185 | 4.49 |
| NYY | 141 | 3.43 | NMY | 128 | 3.11 | NNY | 78 | 1.90 | NNY | 182 | 4.42 |
| NMN | 103 | 2.50 | YNN | 119 | 2.89 | YNN | 64 | 1.55 | YYY | 181 | 4.40 |
| YYY | 100 | 2.43 | NMN | 110 | 2.67 | NYY | 55 | 1.34 | YYM | 101 | 2.45 |
| YNN | 85 | 2.07 | NYY | 104 | 2.53 | YYY | 40 | 0.97 | NMN | 96 | 2.33 |
| MNN | 57 | 1.38 | YYM | 85 | 2.07 | MNN | 38 | 0.92 | YNN | 84 | 2.04 |
| YYM | 52 | 1.26 | YNM | 83 | 2.02 | YYN | 33 | 0.80 | YNM | 76 | 1.85 |
| YYN | 47 | 1.14 | YYN | 61 | 1.48 | YYM | 32 | 0.78 | YYN | 64 | 1.55 |
| YNM | 39 | 0.95 | MNN | 41 | 1.00 | YNM | 23 | 0.56 | YNY | 44 | 1.07 |
| YNY | 29 | 0.70 | YNY | 33 | 0.80 | YNY | 10 | 0.24 | MNN | 40 | 0.97 |
| YMN | 11 | 0.27 | YMN | 11 | 0.27 | MYN | 6 | 0.15 | YMN | 18 | 0.44 |
| MYN | 8 | 0.19 | MYN | 9 | 0.22 | YMN | 6 | 0.15 | YMY | 12 | 0.29 |
| MYY | 5 | 0.12 | YMY | 7 | 0.17 | YMY | 3 | 0.07 | MYN | 10 | 0.24 |
| YMY | 3 | 0.07 | MNY | 6 | 0.15 | MYY | 2 | 0.05 | MYY | 6 | 0.15 |
| MNY | 1 | 0.02 | MNY | 5 | 0.12 | ||||||
Usage pattern is read left to right, with the first letter signifying wave 1 use, the second letter wave 2, and third letter wave 3.
Y = yes to using complementary health approach.
N = no to using complementary health approach.
M = missing self-administered questionnaire or complementary health approach data.
Shown in Tables 3–6, bivariate analyses were used on the prevalence data for each wave to find frequencies of complementary health approach use for each of the independent/covariate variables. Chi-square analysis was used to test bivariate associations between the dependent variables and independent/covariate variables. Significant variables, as well as variables deemed important by the literature1,3,4,13–15 shown in Tables 3–6 were then included and controlled for in the final logistic regression models. We used logistic regressions to find factors associated with either incident use (new use) or continued/discontinued use (Tables 7–10). Odds ratios (ORs) >1 reflect continued complementary health approach use, whereas ORs of <1 reflect discontinued use.
Table 3.
Bivariate Analysis of Chiropractic Therapy
| Wave 1 N = 6325 |
Wave 2 N = 4041 |
Wave 3 N = 2717 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Chiropractic |
Chiropractic |
Chiropractic |
|||||||
| Yes |
Yes |
Yes |
|||||||
|
n = 759 |
n = 679 |
n = 470 |
|||||||
| Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | |
| Predisposing factors | |||||||||
| Sociodemographics | |||||||||
| Sex | 1.44 | 0.43 | 0.84 | ||||||
| Female | 414 (54.55) | 1.81 | 384 (56.55) | 1.9 | 269 (57.23) | 2.28 | |||
| Male | 345 (45.45) | 1.81 | 295 (43.45) | 1.9 | 201 (42.77) | 2.28 | |||
| Race | 18.07*** | 7.43** | 5.51* | ||||||
| White | 707 (93.15) | 0.92 | 639 (94.53) | 0.88 | 433 (92.92) | 1.19 | |||
| Other | 52 (6.85) | 0.92 | 37 (5.47) | 0.88 | 33 (7.08) | 1.19 | |||
| Age | 11.83** | 9.65** | 10.46** | ||||||
| 25–44 years | 328 (43.21) | 1.8 | 141 (20.77) | 1.56 | 14 (2.98) | 0.78 | |||
| 45–64 | 363 (47.83) | 1.81 | 384 (56.55) | 1.9 | 256 (54.47) | 2.3 | |||
| 65+ | 68 (8.96) | 1.04 | 154 (22.68) | 1.61 | 200 (42.55) | 2.28 | |||
| Education | 6.03 | 11.26* | 1.35 | ||||||
| Less than high school | 52 (6.87) | 0.92 | 31 (4.58) | 0.8 | 23 (4.9) | 1 | |||
| High school, GED, AD | 464 (61.29) | 1.77 | 415 (61.3) | 1.87 | 247 (52.67) | 2.31 | |||
| BA/BS | 151 (19.95) | 1.45 | 134 (19.79) | 1.53 | 121 (25.8) | 2.02 | |||
| Advanced degree | 90 (11.89) | 1.18 | 97 (14.33) | 1.35 | 78 (16.63) | 1.72 | |||
| Psychological factors | |||||||||
| Spiritual importance | 7.47** | 14.07*** | 13.8*** | ||||||
| Not or not very important | 139 (18.71) | 1.43 | 80 (11.9) | 1.25 | 51 (11.11) | 1.47 | |||
| Somewhat to very important | 604 (81.29) | 1.43 | 592 (88.1) | 1.25 | 408 (88.89) | 1.47 | |||
| Depression | 6.37* | 0.04 | 0.73 | ||||||
| Yes | 101 (13.31) | 1.23 | 60 (8.84) | 1.09 | 39 (8.3) | 1.27 | |||
| No | 658 (86.69) | 1.23 | 619 (91.16) | 1.09 | 431 (91.7) | 1.27 | |||
Significance level: *p < 0.05, **p < 0.01, ***p < 0.001.
AD, Associate’s degree; BA/BS, Bachelor of Art or Bachelor of Science degree; GED, general educational development; SE, standard error.
Table 4.
Bivariate Analysis of Massage Therapy
| Wave 1 N = 6325 |
Wave 2 N = 4041 |
Wave 3 N = 2717 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Massage |
Massage |
Massage |
|||||||
| Yes |
Yes |
Yes |
|||||||
|
n = 538 |
n = 682 |
n = 494 |
|||||||
| Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | |
| Predisposing factors | |||||||||
| Sociodemographics | |||||||||
| Sex | 9.71** | 73.01*** | 20.02*** | ||||||
| Female | 317 (58.92) | 2.12 | 479 (70.23) | 1.75 | 318 (64.37) | 2.16 | |||
| Male | 221 (41.08) | 2.12 | 203 (29.77) | 1.75 | 176 (35.63) | 2.16 | |||
| Race | 0.8 | 0.41 | 0.5 | ||||||
| White | 470 (87.36) | 1.43 | 620 (91.31) | 1.08 | 445 (90.82) | 1.3 | |||
| Other | 68 (12.64) | 1.43 | 59 (8.69) | 1.08 | 45 (9.18) | 1.3 | |||
| Age | 25.41*** | 60.48*** | 46.1*** | ||||||
| 25–44 years | 283 (52.6) | 2.15 | 179 (26.25) | 1.69 | 17 (3.44) | 0.82 | |||
| 45–64 | 226 (42.01) | 2.13 | 395 (57.92) | 1.89 | 302 (61.13) | 2.19 | |||
| 65+ | 29 (5.39) | 0.97 | 108 (15.84) | 1.4 | 175 (35.43) | 2.15 | |||
| Education | 46.94*** | 36.42*** | 26.23*** | ||||||
| Less than high school | 28 (5.22) | 0.96 | 20 (2.93) | 0.65 | 14 (2.84) | 0.75 | |||
| High school, GED, AD | 269 (50.19) | 2.16 | 339 (49.78) | 1.92 | 227 (46.04) | 2.25 | |||
| BA/BS | 157 (29.29) | 1.97 | 192 (28.19) | 1.72 | 132 (26.77) | 1.99 | |||
| Advanced degree | 82 (15.3) | 1.56 | 130 (19.09) | 1.51 | 120 (24.34) | 1.93 | |||
| Psychological factors | |||||||||
| Spiritual importance | 8.48** | 11.29*** | 10.97*** | ||||||
| Not or not very important | 94 (17.6) | 1.65 | 83 (12.41) | 1.27 | 58 (11.93) | 1.47 | |||
| Somewhat to very important | 440 (82.4) | 1.65 | 586 (87.59) | 1.27 | 428 (88.07) | 1.47 | |||
| Depression | 20.07*** | 7.32** | 18.59*** | ||||||
| Yes | 88 (16.36) | 1.59 | 77 (11.29) | 1.21 | 59 (11.94) | 1.46 | |||
| No | 450 (83.64) | 1.59 | 605 (88.71) | 1.21 | 435 (88.06) | 1.46 | |||
Significance level: **p < 0.01, ***p < 0.001.
AD, Associate’s degree; BA/BS, Bachelor of Art or Bachelor of Science degree; GED, general educational development; SE, standard error.
Table 5.
Bivariate Analysis of Herbal Therapy
| Wave 1 N = 6325 |
Wave 2 N = 4041 |
Wave 3 N = 2717 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Herbal |
Herbal |
Herbal |
|||||||
| Yes |
Yes |
Yes |
|||||||
|
n = 318 |
n = 395 |
n = 194 |
|||||||
| Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | |
| Predisposing factors | |||||||||
| Sociodemographics | |||||||||
| Sex | 33.24*** | 51.2*** | 17.21*** | ||||||
| Female | 217 (68.24) | 2.61 | 286 (72.41) | 2.25 | 135 (69.59) | 3.3 | |||
| Male | 101 (31.76) | 2.61 | 109 (27.59) | 2.25 | 59 (30.41) | 3.3 | |||
| Race | 6.91** | 0.98 | 0.01 | ||||||
| White | 267 (83.96) | 2.06 | 358 (90.63) | 1.47 | 174 (90.16) | 2.14 | |||
| Other | 51 (16.04) | 2.06 | 37 (9.37) | 1.47 | 19 (9.84) | 2.14 | |||
| Age | 10.01** | 18.01*** | 9.33** | ||||||
| 25–44 years | 162 (50.94) | 2.8 | 81 (20.51) | 2.03 | 9 (4.64) | 1.51 | |||
| 45–64 | 136 (42.77) | 2.77 | 240 (60.76) | 2.46 | 103 (53.09) | 3.58 | |||
| 65+ | 20 (6.29) | 1.36 | 74 (18.73) | 1.96 | 82 (42.27) | 3.55 | |||
| Education | 25.92*** | 36.06*** | 9.19* | ||||||
| Less than high school | 16 (5.06) | 1.23 | 9 (2.28) | 0.75 | 5 (2.62) | 1.16 | |||
| High school, GED, AD | 160 (50.63) | 2.81 | 186 (47.21) | 2.52 | 88 (46.07) | 3.61 | |||
| BA/BS | 92 (29.11) | 2.56 | 127 (32.23) | 2.35 | 52 (27.23) | 3.22 | |||
| Advanced degree | 48 (15.19) | 2.02 | 72 (18.27) | 1.95 | 46 (24.08) | 3.09 | |||
| Psychological factors | |||||||||
| Spiritual importance | 32.36*** | 24.05*** | 10.76** | ||||||
| Not or not very important | 30 (9.55) | 1.66 | 31 (7.99) | 1.38 | 16 (8.42) | 2.02 | |||
| Somewhat to very important | 284 (90.45) | 1.66 | 357 (92.01) | 1.38 | 174 (91.58) | 2.02 | |||
| Depression | 3.56 | 18.63*** | 7.69** | ||||||
| Yes | 44 (13.84) | 1.94 | 57 (14.43) | 1.77 | 24 (12.37) | 2.36 | |||
| No | 274 (86.16) | 1.94 | 338 (85.57) | 1.77 | 170 (87.63) | 2.36 | |||
Significance level: *p < 0.05, **p < 0.01, ***p < 0.001.
AD, Associate’s degree; BA/BS, Bachelor of Art or Bachelor of Science degree; GED, general educational development; SE, standard error.
Table 6.
Bivariate Analysis of Meditation Therapy
| Wave 1 N = 6325 |
Wave 2 N = 4041 |
Wave 3 N = 2717 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Meditation |
Meditation |
Herbal |
|||||||
| Yes |
Yes |
Yes |
|||||||
|
n = 843 |
n = 962 |
n = 643 |
|||||||
| Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | Row N (%) | χ2 | SE | |
| Predisposing factors | |||||||||
| Sociodemographics | |||||||||
| Sex | 42.87*** | 90.44*** | 46.74*** | ||||||
| Female | 531 (62.99) | 1.66 | 661 (68.71) | 1.5 | 431 (67.03) | 1.85 | |||
| Male | 312 (37.01) | 1.66 | 301 (31.29) | 1.5 | 212 (32.97) | 1.85 | |||
| Race | 4.07* | 0.55 | 0.02 | ||||||
| White | 729 (86.48) | 1.18 | 877 (91.35) | 0.91 | 572 (90.08) | 1.19 | |||
| Other | 114 (13.52) | 1.18 | 83 (8.65) | 0.91 | 63 (9.92) | 1.19 | |||
| Age | 21.37*** | 33.13*** | 23.03*** | ||||||
| 25–44 years | 415 (49.23) | 1.72 | 197 (20.48) | 1.3 | 19 (2.95) | 0.67 | |||
| 45–64 | 370 (43.89) | 1.71 | 568 (59.04) | 1.59 | 361 (56.14) | 1.96 | |||
| 65+ | 58 (6.88) | 0.87 | 197 (20.48) | 1.3 | 263 (40.9) | 1.94 | |||
| Education | 102.98*** | 82.05*** | 56.89*** | ||||||
| Less than high school | 34 (4.04) | 0.68 | 23 (2.39) | 0.49 | 18 (2.82) | 0.65 | |||
| High school, GED, AD | 421 (50.06) | 1.72 | 467 (48.6) | 1.61 | 272 (42.57) | 1.96 | |||
| BA/BS | 241 (28.66) | 1.56 | 294 (30.59) | 1.49 | 195 (30.52) | 1.82 | |||
| Advanced degree | 145 (17.24) | 1.3 | 177 (18.42) | 1.25 | 154 (24.1) | 1.69 | |||
| Psychological factors | |||||||||
| Spiritual importance | 97.21*** | 70.76*** | 79.43*** | ||||||
| Not or not very important | 77 (9.3) | 1.01 | 75 (7.92) | 0.88 | 34 (5.39) | 0.9 | |||
| Somewhat to very important | 751 (90.7) | 1.01 | 872 (92.08) | 0.88 | 597 (94.61) | 0.9 | |||
| Depression | 30.64*** | 27.55*** | 26.3*** | ||||||
| Yes | 136 (16.13) | 1.27 | 123 (12.79) | 1.08 | 77 (11.98) | 1.28 | |||
| No | 707 (83.87) | 1.27 | 839 (87.21) | 1.08 | 566 (88.02) | 1.28 | |||
Significance level: *p < 0.05, ***p < 0.001.
AD, Associate’s degree; BA/BS, Bachelor of Art or Bachelor of Science degree; GED, general educational development; SE, standard error.
Table 7.
Multivariable Analysis of Chiropractic
| Continued/discontinued use of chiropractic | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2a |
Wave 2–3a |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race | 0.01 | 0.80 | ||||
| White | 3.04 | 1.33–6.92 | 0.90 | 0.39–2.05 | ||
| Other | Ref | Ref | ||||
| Age | 0.24 | 0.04 | ||||
| 25–44 years | 0.87 | 0.62–1.24 | 0.67 | 0.42–1.07 | ||
| 45–64 | Ref | Ref | ||||
| 65+ | 0.61 | 0.34–1.10 | 0.57 | 0.35–0.95 | ||
| Sex | 0.09 | 0.74 | ||||
| Male | Ref | Ref | ||||
| Female | 1.33 | 0.95–1.86 | 1.07 | 0.73–1.55 | ||
| Education | 0.16 | 0.02 | ||||
| Less than high school | 0.58 | 0.25–1.32 | 0.49 | 0.18–1.35 | ||
| High school, GED, AD | 1.11 | 0.73–1.70 | 0.52 | 0.32–0.82 | ||
| BA/BS | Ref | Ref | ||||
| Advanced degree | 1.49 | 0.85–2.61 | 0.44 | 0.24–0.81 | ||
| Spiritual importance | 0.95 | 0.29 | ||||
| Not or not very important | Ref | Ref | ||||
| Somewhat to very important | 1.01 | 0.67–1.53 | 1.36 | 0.77–2.39 | ||
| Depression | 0.13 | 0.33 | ||||
| Yes | Ref | Ref | ||||
| No | 1.44 | 0.89–2.33 | 1.40 | 0.72–2.74 | ||
| Chiropractic use in wave 1 | — | <0.0001 | ||||
| Yes | — | — | 2.74 | 1.93–3.90 | ||
| No | — | — | Ref | |||
| New use of chiropractic | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2a |
Wave 2–3a |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race |
|
|
<0.001 |
|
|
0.20 |
| White |
2.66 |
1.60–4.42 |
|
1.50 |
0.81–2.78 |
|
| Other |
Ref |
|
|
Ref |
|
|
| Age |
|
|
<0.01 |
|
|
<0.001 |
| 25–44 years |
1.29 |
1.01–1.64 |
|
1.34 |
0.94–1.92 |
|
| 45–64 |
Ref |
|
|
Ref |
|
|
| 65+ |
0.62 |
0.39–0.97 |
|
0.52 |
0.34–0.79 |
|
| Sex |
|
|
0.33 |
|
|
0.40 |
| Male |
Ref |
|
|
Ref |
|
|
| Female |
1.12 |
0.89–1.41 |
|
1.14 |
0.84–1.56 |
|
| Education |
|
|
0.05 |
|
|
0.34 |
| Less than high school |
0.67 |
0.38–1.20 |
|
1.48 |
0.75–2.91 |
|
| High school, GED, AD |
1.23 |
0.93–1.64 |
|
1.09 |
0.75–1.58 |
|
| BA/BS |
Ref |
|
|
Ref |
|
|
| Advanced degree |
0.97 |
0.64–1.48 |
|
0.77 |
0.46–1.27 |
|
| Spiritual importance |
|
|
<0.01 |
|
|
<0.01 |
| Not or not very important |
Ref |
|
|
Ref |
|
|
| Somewhat to very important |
1.52 |
1.14–2.03 |
|
1.90 |
1.18–3.06 |
|
| Depression |
|
|
0.048 |
|
|
0.43 |
| Yes |
Ref |
|
|
Ref |
|
|
| No |
0.72 |
0.52–0.99 |
|
1.27 |
0.70–2.28 |
|
| Chiropractic use in wave 1 |
|
|
— |
|
|
<0.0001 |
| Yes |
— |
— |
|
3.33 |
2.21–5.02 |
|
| No | — | Ref | ||||
Adjusted for all variables in the table in addition to smoking status, marriage status, total household income, insurance status, joint/bone disease, sciatica/lumbago/recurring backache, and migraine headaches.
AD, Associate's degree; BA/BS, Bachelor of Art or Bachelor of Science degree; CI, confidence interval; GED, general educational development; OR, odds ratio.
Table 8.
Multivariable Analysis of Massage Therapy
| Continued/discontinued use of massage therapy | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race | 0.11 | 0.24 | ||||
| White | 1.69 | 0.89–3.23 | 1.46 | 0.78–2.75 | ||
| Other | Ref | Ref | ||||
| Age | 0.77 | 0.01 | ||||
| 25–44 years | 1.10 | 0.72–1.68 | 0.92 | 0.62–1.38 | ||
| 45–64 | Ref | Ref | ||||
| 65+ | 0.79 | 0.30–2.11 | 0.42 | 0.23–0.74 | ||
| Sex | <0.0001 | 0.67 | ||||
| Male | Ref | Ref | ||||
| Female | 2.38 | 1.56–3.63 | 1.09 | 0.74–1.60 | ||
| Education | 0.29 | 0.22 | ||||
| Less than high school | 0.40 | 0.13–1.27 | 1.05 | 0.31–3.50 | ||
| High school, GED, AD | 0.72 | 0.45–1.14 | 0.96 | 0.63–1.45 | ||
| BA/BS | Ref | Ref | ||||
| Advanced degree | 0.94 | 0.53–1.66 | 1.54 | 0.93–2.55 | ||
| Spiritual importance | 0.41 | 0.72 | ||||
| Not or not very important | Ref | Ref | ||||
| Somewhat to very important | 1.26 | 0.73–2.18 | 1.10 | 0.65–1.85 | ||
| Depression | 0.25 | 0.11 | ||||
| Yes | Ref | Ref | ||||
| No | 0.75 | 0.45–1.23 | 0.64 | 0.38–1.10 | ||
| Massage use in wave 1 | — | <0.0001 | ||||
| Yes | — | — | 2.32 | 1.61–3.35 | ||
| No | — | — | Ref | |||
| New use of massage therapy | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race |
|
|
0.09 |
|
|
0.64 |
| White |
1.38 |
0.95–2.0 |
|
0.88 |
0.52–1.49 |
|
| Other |
Ref |
|
|
Ref |
|
|
| Age |
|
|
<0.001 |
|
|
<0.001 |
| 25–44 years |
1.16 |
0.93–1.45 |
|
1.61 |
1.15–2.25 |
|
| 45–64 |
Ref |
|
|
Ref |
|
|
| 65+ |
0.44 |
0.28–0.69 |
|
0.56 |
0.35–0.87 |
|
| Sex |
|
|
<0.0001 |
|
|
0.049 |
| Male |
Ref |
|
|
Ref |
|
|
| Female |
2.75 |
2.20–3.45 |
|
1.36 |
1.00–1.85 |
|
| Education |
|
|
<0.0001 |
|
|
0.23 |
| Less than high school |
0.44 |
0.27–0.73 |
|
0.48 |
0.19–1.26 |
|
| High school, GED, AD |
0.68 |
0.53–0.87 |
|
0.81 |
0.57–1.16 |
|
| BA/BS |
Ref |
|
|
Ref |
|
|
| Advanced degree |
1.23 |
0.88–1.71 |
|
1.12 |
0.74–1.71 |
|
| Spiritual importance |
|
|
0.54 |
|
|
<0.01 |
| Not or not very important |
Ref |
|
|
Ref |
|
|
| Somewhat to very important |
1.08 |
0.84–1.39 |
|
2.05 |
1.28–3.29 |
|
| Depression |
|
|
0.44 |
|
|
0.97 |
| Yes |
Ref |
|
|
Ref |
|
|
| No |
1.15 |
0.81–1.61 |
|
0.99 |
0.59–1.66 |
|
| Massage use in wave 1 |
|
|
— |
|
|
<0.0001 |
| Yes |
— |
— |
|
3.21 |
2.04–5.05 |
|
| No | — | — | Ref | |||
Adjusted for all variables in the table in addition to smoking status, marriage status, total household income, insurance status, joint/bone disease, sciatica/lumbago/recurring backache, and migraine headaches.
AD, Associate's degree; BA/BS, Bachelor of Art or Bachelor of Science degree; CI, confidence interval; GED, general educational development; OR, odds ratio.
Table 9.
Multivariable Analysis of Herbal Products
| Continued/discontinued use of herbal products | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race | 0.79 | 0.26 | ||||
| White | 0.89 | 0.40–2.02 | 1.75 | 0.66–4.62 | ||
| Other | Ref | Ref | ||||
| Age | 0.17 | 0.20 | ||||
| 25–44 years | 0.66 | 0.36–1.21 | 1.57 | 0.84–2.93 | ||
| 45–64 | Ref | Ref | ||||
| 65+ | 0.33 | 0.08–1.39 | 0.78 | 0.41–1.49 | ||
| Sex | <0.01 | 0.34 | ||||
| Male | Ref | Ref | ||||
| Female | 2.56 | 1.35–4.85 | 0.75 | 0.42–1.35 | ||
| Education | 0.07 | 0.78 | ||||
| Less than high school | 0.10 | 0.01–0.90 | 0.52 | 0.07–3.90 | ||
| High school, GED, AD | 0.70 | 0.36–1.34 | 0.79 | 0.44–1.43 | ||
| BA/BS | Ref | Ref | ||||
| Advanced degree | 1.39 | 0.63–3.06 | 0.76 | 0.37–1.54 | ||
| Spiritual importance | 0.23 | 0.90 | ||||
| Not or not very important | Ref | Ref | ||||
| Somewhat to very important | 2.06 | 0.63–6.69 | 0.94 | 0.39–2.28 | ||
| Depression | 0.60 | 0.38 | ||||
| Yes | Ref | Ref | ||||
| No | 1.25 | 0.54–2.90 | 0.72 | 0.35–1.49 | ||
| Herbal use in wave 1 | — | <0.01 | ||||
| Yes | — | — | 2.17 | 0127–3.71 | ||
| No | — | — | Ref | |||
| New use of herbal products | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race |
|
|
0.14 |
|
|
0.81 |
| White |
1.45 |
0.89–2.36 |
0.92 |
0.44–1.91 |
|
|
| Other |
Ref |
|
|
Ref |
|
|
| Age |
|
|
0.12 |
|
|
0.02 |
| 25–44 years |
0.89 |
0.67–1.20 |
|
1.26 |
0.75–2.12 |
|
| 45–64 |
Ref |
|
|
Ref |
|
|
| 65+ |
0.58 |
0.34–0.98 |
|
0.46 |
0.24–0.87 |
|
| Sex |
|
|
<0.0001 |
|
|
0.09 |
| Male |
Ref |
|
|
Ref |
|
|
| Female |
2.79 |
2.07–3.74 |
|
1.51 |
0.94–2.44 |
|
| Education |
|
|
<0.0001 |
|
|
0.06 |
| Less than high school |
0.20 |
0.09–0.45 |
|
1.11 |
0.39–3.17 |
|
| High school, GED, AD |
0.45 |
0.33–0.62 |
|
0.82 |
0.47–1.43 |
|
| BA/BS |
Ref |
|
|
Ref |
|
|
| Advanced degree |
0.95 |
0.64–1.41 |
|
1.77 |
0.97–3.25 |
|
| Spiritual importance |
|
|
<0.01 |
|
|
0.03 |
| Not or not very important |
Ref |
|
|
Ref |
|
|
| Somewhat to very important |
1.84 |
1.26–2.69 |
|
2.34 |
1.10–4.98 |
|
| Depression |
|
|
0.36 |
|
|
0.83 |
| Yes |
Ref |
|
|
Ref |
|
|
| No |
1.23 |
0.79–1.92 |
|
1.08 |
0.53–2.21 |
|
| Herbal use in wave 1 |
|
|
— |
|
|
<0.0001 |
| Yes |
— |
— |
|
4.33 |
2.08–9.03 |
|
| No | — | — | Ref | |||
Adjusted for all variables in the table in addition to smoking status, marriage status, total household income, insurance status, joint/bone disease, sciatica/lumbago/recurring backache, and migraine headaches.
AD, Associate's degree; BA/BS, Bachelor of Art or Bachelor of Science degree; CI, confidence interval; GED, general educational development; OR, odds ratio.
Table 10.
Multivariable Analysis of Meditation
| Continued/discontinued use of meditation | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race | 0.45 | 0.07 | ||||
| White | 1.20 | 0.75–1.92 | 1.61 | 0.96–2.73 | ||
| Other | Ref | Ref | ||||
| Age | 0.28 | 0.10 | ||||
| 25–44 years | 0.76 | 0.54–1.07 | 0.82 | 0.56–1.20 | ||
| 45–64 | Ref | Ref | ||||
| 65+ | 1.01 | 0.55–1.87 | 0.66 | 0.44–0.99 | ||
| Sex | <0.001 | 0.16 | ||||
| Male | Ref | Ref | ||||
| Female | 1.78 | 1.29–2.45 | 1.26 | 0.91–1.75 | ||
| Education | <0.0001 | <0.01 | ||||
| Less than high school | 0.14 | 0.04–0.46 | 1.48 | 0.53–4.12 | ||
| High school, GED, AD | 0.54 | 0.38–0.78 | 0.61 | 0.43–0.85 | ||
| BA/BS | Ref | Ref | ||||
| Advanced degree | 1.03 | 0.66–1.62 | 1.09 | 0.72–1.65 | ||
| Spiritual importance | <0.001 | 0.04 | ||||
| Not or not very important | Ref | Ref | ||||
| Somewhat to very important | 2.74 | 1.54–4.86 | 1.71 | 1.01–2.89 | ||
| Depression | 0.53 | 0.57 | ||||
| Yes | Ref | Ref | ||||
| No | 0.88 | 0.58–1.33 | 1.14 | 0.72–1.81 | ||
| Meditation use in wave 1 | — | <0.0001 | ||||
| Yes | — | — | 2.44 | 1.81–3.28 | ||
| No | — | — | Ref | |||
| New use of meditation | ||||||
|---|---|---|---|---|---|---|
| Model variables | Wave 1–2 |
Wave 2–3 |
||||
| ORa | 95% CI | p | ORa | 95% CI | p | |
| Race |
|
|
0.02 |
|
|
0.16 |
| White |
1.49 |
1.06–2.09 |
|
0.72 |
0.45–1.14 |
|
| Other |
Ref |
|
|
Ref |
|
|
| Age |
|
|
<0.0001 |
|
|
<0.01 |
| 25–44 years |
0.90 |
0.73–1.10 |
|
1.08 |
0.75–1.55 |
|
| 45–64 |
Ref |
|
|
Ref |
|
|
| 65+ |
0.35 |
0.23–0.53 |
|
0.48 |
0.32–0.72 |
|
| Sex |
|
|
<0.0001 |
|
|
0.02 |
| Male |
Ref |
|
|
Ref |
|
|
| Female |
2.27 |
1.87–2.76 |
|
1.42 |
1.05–1.92 |
|
| Education |
|
|
<0.0001 |
|
|
<0.0001 |
| Less than high school |
0.24 |
0.14–0.40 |
|
0.24 |
0.10–0.58 |
|
| High school, GED, AD |
0.58 |
0.46–0.72 |
|
0.48 |
0.33–0.69 |
|
| BA/BS |
Ref |
|
|
Ref |
|
|
| Advanced degree |
1.16 |
0.85–1.57 |
|
0.98 |
0.66–1.46 |
|
| Spiritual importance |
|
|
<0.0001 |
|
|
0.001 |
| Not or not very important |
Ref |
|
|
Ref |
|
|
| Somewhat to very important |
2.15 |
1.65–2.80 |
|
2.07 |
1.34–3.18 |
|
| Depression |
|
|
0.04 |
|
|
0.14 |
| Yes |
Ref |
|
|
Ref |
|
|
| No |
0.75 |
0.56–0.99 |
|
0.70 |
0.44–1.12 |
|
| Meditation use in wave 1 |
|
|
— |
|
|
<0.0001 |
| Yes |
— |
— |
|
3.00 |
2.00–4.51 |
|
| No | — | — | Ref | |||
Adjusted for all variables in the table in addition to smoking status, marriage status, total household income, insurance status, joint/bone disease, sciatica/lumbago/recurring backache, and migraine headaches.
AD, Associate's degree; BA/BS, Bachelor of Art or Bachelor of Science degree; CI, confidence interval; GED, general educational development; OR, odds ratio.
These multivariate analyses were used to determine whether significant predisposing factors affect complementary health approach use over time, while adjusting for enabling and health need factors. Due to inconsistent Wald p-values across the four approaches for enabling and health need factors, these data are not discussed further but may be found in Supplementary Appendices SA2 and SA3. In addition, domain analysis was used to observe whether predisposing factors contributed to the continuation or discontinuation of complementary health approach use, and/or new use of each of the four complementary health approaches. Significant relationships with complementary health approach use were defined by p-values <0.05 and 95% confidence intervals (CIs), and all estimates and data analysis were produced by using SAS software (version 9.4; SAS Institute, Cary, NC).
Strengths and limitations of data source
When comparing the MIDUS sample with 1995 U.S. Census data, the sample underrepresented those with less than high school education and African Americans, and oversampling occurred in older males with the purpose of enabling sex comparisons by age.17 Due to low sample size and variable race and ethnicity survey questions across years, we examined only two subgroups in relation to race—white and other, which comprised black and/or African American, Native American or Aleutian Islander/Eskimo, Asian or Pacific islander, multiracial, or other. Despite these limitations, the MIDUS data set is the first survey to collect longitudinal data on a comprehensive array of complementary health approach questions, including information on the four modalities used in this analysis.
Results
Prevalence of complementary health approaches
The prevalence of massage therapy, meditation, chiropractic, and herbal products at each wave is presented in Figure 3. The pattern of complementary health approach use is consistent across all waves for all four approaches exhibiting 24%–41% of continued use, 26%–39% of discontinued use, whereas 30% of participants were lost to follow-up. In contrast, there were large differences between approaches in wave 1 (1995–1996); 8.51% (standard error [SE]: 0.35) reported using massage therapy, whereas 13.33% (SE: 0.43) used meditation, 12.0% (SE: 0.41) used chiropractic, and 5.03% (SE: 0.27) used herbal products. Between 32% and 41% of individuals using each of the complementary health approaches in wave 1 continued use into wave 2 (2004–2005). However, wave 2 saw an influx of new use for each approach, with between 4% and 11% of individuals not using these approaches in wave 1, but reporting use in wave 2.
Massage therapy, meditation, chiropractic, and herbal product use was reported by 16.88% (SE: 0.59), 23.81% (SE: 0.67), 16.8% (0.59), and 9.77% (SE: 0.47), of participants in 2004–2005, respectively. For each of these approaches, about one-quarter to one-third of those who reported use in wave 2 continued use into wave 3 (2013–2014). Wave 3 also saw an influx of new use of all approaches, with 2%–9% of individuals not using these approaches in wave 2, also reporting using these approaches in wave 3, with most recent prevalence rates of 18.18% (SE: 0.74) for massage therapy, 23.67% (SE: 0.82) for meditation, 17.3% (SE: 0.73) for chiropractic, and 7.14% (SE: 0.49) for herbal products.
Individual usage patterns of complementary health approaches
Table 2 displays the combination of individual usage patterns from wave 1 to wave 3. Most participants (60%–80%) who answered the survey questions about complementary health approaches did not report using any of the four modalities (use patterns NNN or NNM). A few respondents reporting use of chiropractic, massage therapy, herbal products, and meditation consistently said yes at all wave time points (use pattern YYY: 3.47%, 2.43%, 0.97%, and 4.40%). Most people who use herbal products (use patterns: 2.96% NYN, 2.33% NMY, 1.9% NNY) and chiropractic approaches (use patterns: 3.81% NNY, 3.4% NYN, 3.11% NMY) only used them at one wave. The rates of participants with an affirmative response to meditation and massage therapy in two latter waves but not in wave 1 (use pattern NYY) were 4.66% and 3.43%, respectively.
New use of complementary health approaches
Chiropractic
Race and depression in wave 1 were associated with chiropractic use in wave 2 (Table 7). White participants in wave 1 were more likely to initiate chiropractic (OR = 2.66, 95% CI = 1.60–4.42) in wave 2 than others. Individuals not depressed in wave 1 were less likely to use chiropractic in wave 2 (OR = 0.72, 95% CI = 0.52–0.99). Both age and spiritual importance were significant predictors for chiropractic use in waves 2 and 3. Adults aged 25–44 were more likely to initiate chiropractic use in waves 2 (OR = 1.29, 95% CI = 1.01–1.64), and 3 (OR = 1.34, 95% CI = 0.94–1.92) compared to adults aged 45–64. Adults 65+ were least likely to report chiropractic use in waves 2 (OR = 0.62, 95% CI = 0.39–0.97) and 3 (OR = 0.52, 95% CI = 0.34–0.79). Previous chiropractic use in wave 1 was a significant predictor for wave 3, with those reporting chiropractic use in wave 1 being more than three times as likely to report it nearly two decades later (OR = 3.33, 95% CI = 2.21–5.02).
Massage therapy
The reported education level in wave 1 significantly predicted massage therapy use in wave 2 (Table 8). High school, GED, and associate's degree holders were less likely to report massage therapy (OR = 0.68, 95% CI = 0.53–0.87), compared with those who held a bachelor's degree. Those with less than a high school level education had even lower odds (OR = 0.44, 95% CI = 0.27–0.73) of using massage therapy in wave 2. A report of spiritual importance in wave 2 was associated with a two-fold increase in odds in the future (wave 3) report of massage (OR = 2.05, 95% CI = 1.28–3.29). Both sex and age were significant predictors for massage therapy in waves 2 and 3. Females were more likely to start massage therapy in waves 2 (OR = 2.75, 95% CI = 2.20–3.45) and 3, although the magnitude of the association for wave 3 was attenuated, comparatively (OR = 1.36, 95% CI = 1.00–1.85).
Adults aged 25–44 were most likely to initiate massage therapy in waves 2 (OR = 1.16, 95% CI = 0.93–1.45) and 3 (OR = 1.61, 95% CI = 1.15–2.25) compared with adults aged 45–64. Adults aged 65+ years were least likely to use massage therapy in waves 2 (OR = 0.44, 95% CI = 0.28–0.69) and 3 (OR = 0.56, 95% CI = 0.35–0.87). A previous report of massage therapy (wave 1) was associated with a subsequent report (wave 3), with those reporting massage therapy use in wave 1 being more than three times as likely to report it nearly two decades later (OR = 3.21, 95% CI = 2.04–5.05).
Herbal products
Sex and education in wave 1 were associated with herbal product use in wave 2 (Table 9). Females were almost three times as likely to start using herbal products in wave 2 (OR = 2.79, 95% CI = 2.07–3.74). Participants with a high school, GED, or associate's degree were nearly half as likely to start using herbal products (OR = 0.45, 95% CI = 0.33–0.62) in wave 2 compared with those with a bachelor's degree. Spiritual importance was associated with subsequent herbal product use in both later waves. Those who reported spirituality somewhat to very important were 1.8 times as likely to use herbal products in wave 2 (OR = 1.84, 95% CI = 1.26–2.69) and 2.3 times as likely to use these products in wave 3 (OR = 2.34, 95% CI = 1.10–4.98) compared with those who stated that spirituality was not important or not very important. Previous herbal product use in wave 1 also predicted herbal product use in wave 3 (OR = 4.33, 95% CI = 2.08–9.03).
Meditation
Race and depression in wave 1 were significant predictors for meditation use in wave 2 (Table 10). White participants were more likely to start meditation (OR = 1.49, 95% CI = 1.06–2.09) than others. Individuals not reporting depression in wave 1 were slightly less likely to subsequently report meditation in wave 2 (OR = 0.75, 95% CI = 0.56–0.99). Wave 1 age, sex, education, and spiritual importance were all associated with subsequent reports of meditation use in waves 2 and 3. Adults aged 65+ were least likely to use meditation in waves 2 (OR = 0.35, 95% CI = 0.23–0.53) and 3 (OR = 0.48, 95% CI = 0.32–0.72). Participants with a high school, GED, or associate's degree were also less likely to use meditation in waves 2 (OR = 0.58, 95% CI = 0.46–0.72) and 3 (OR = 0.48, 95% CI = 0.33–0.69) compared with those with a bachelor's degree. Spiritual importance was associated with a nearly two-fold subsequent report of meditation use in waves 2 (OR = 2.15, 95% CI = 1.65–2.80) and 3 (OR = 2.07, 95% CI = 1.34–3.18). Previous use of meditation in wave 1 was also a significant predictor for use in wave 3 (OR = 3.00, 95% CI = 2.00–4.51).
Continued use of complementary health approaches
Continued use of complementary health approaches is interpreted in this analysis as an OR >1 and indicates continued complementary health approach use from one wave to the next.
Chiropractic
Age and the previous use of chiropractic were significant predictors of continued chiropractic use (Table 7). White participants in wave 1 were three times as likely to continue chiropractic use in wave 2 (OR = 3.04, 95% CI = 1.33–6.92), compared with other participants. Those who used chiropractic in wave 1 were more likely to continue using this approach from wave 2 to wave 3 (OR = 2.74, 95% CI = 1.93–3.90), compared with those who did not use chiropractic in wave 1.
Massage therapy
Sex and the previous use of massage therapy were associated with continued massage use (Table 8). Females in wave 1 were more than twice as likely to continue massage use in wave 2 (OR = 2.38, 95% CI = 1.56–3.63), compared with males. Participants with reports of prior wave 1 massage use were 2.3 times as likely to continue using massage therapy from wave 2 to wave 3 (OR = 2.32, 95% CI = 1.61–3.35), compared with those who did not use massage therapy in wave 1.
Herbal products
Sex and the previous use of herbal products were the only two significant factors related to continued use of herbal products (Table 9). Females in wave 1 were 2.5 times as likely to continue massage therapy in wave 2 (OR = 2.56, 95% CI = 1.35–4.85), compared with males. Those with a prior use of herbal products in wave 1 were more likely to continue using them from wave 2 to wave 3 (OR = 2.17, 95% CI = 1.27–3.71), compared with those who did not use herbal products in wave 1.
Meditation
Sex, spiritual importance, and the previous use of meditation were significantly associated with continued reports of meditation use (Table 10). Females in wave 1 were nearly twice as likely to continue meditation in wave 2 (OR = 1.78, 95% CI = 1.29–2.45), compared with males. Those who found spirituality in life somewhat to very important were more likely to continue practicing meditation use in waves 2 (OR = 2.74, 95% CI = 1.54–4.86) and 3, although this relationship was attenuated in wave 3 (OR = 1.71, 95% CI = 1.01–2.89). Participants in wave 2 who reported prior use of meditation in wave 1 were more than twice as likely to continue meditation use in wave 3 (OR = 2.44, 95% CI = 1.81–3.28), compared with those who did not practice meditation in wave 1.
Discontinued use of complementary health approaches
Discontinued use of complementary health approaches is interpreted as an OR <1 and indicates a likelihood of discontinuing or stopping complementary health approach use from one wave to the next.
Chiropractic
Age and education in wave 2 were significantly associated with the discontinued use of chiropractic reported in wave 3. Those aged 65+ years in wave 2 were more likely to discontinue chiropractic use in wave 3 (OR = 0.57, 95% CI = 0.35–0.95), compared with those aged 45–64 years. Those with an advanced degree in wave 2 were more likely to discontinue chiropractic use in wave 3 (OR = 0.44, 95% CI = 0.24–0.81), compared with those with a bachelor's degree.
Massage therapy
Age in wave 2 was the only significant factor associated with the discontinued use of massage therapy reported in wave 3. Those aged 65+ years in wave 2 were more likely to discontinue massage therapy in wave 3 (OR = 0.42, 95% CI = 0.23–0.74), compared with those aged 45–64.
Herbal products
There were no significant relationships between any factor and the discontinued use of herbal products between any of the waves.
Meditation
Education in wave 1 was the only factor associated with discontinued use of meditation in wave 2. Those with a high school, GED, or associate's degree in wave 1 were more likely to discontinue meditation in wave 2 (OR = 0.54, 95% CI = 0.66–0.78), compared with those with a bachelor's degree. Those with less than a high school education had the greatest magnitude of association with discontinued meditation in wave 2 (OR = 0.14, 95% CI = 0.04–0.46).
A summary of our significant model predictors for both new and continued/discontinued complementary health approach use can be found in Table 11.
Table 11.
Summary of Significant Model Predictors
| Continued/discontinued use | |||
|---|---|---|---|
| Meditation | Massage therapy | Herbal products | Chiropractic |
| Sexa | Sexa | Sexa | Racea |
| Spiritual importancea,b | Ageb | Ageb | |
| Educationa,b | Educationb | ||
| Meditation use in wave 1b | Massage use in wave 1b | Herbal use in wave 1b | Chiropractic use in wave 1b |
| New CHA use | |||
|---|---|---|---|
| Meditation | Massage therapy | Herbal products | Chiropractic |
| Agea,b |
Agea,b |
Ageb |
Agea,b |
| Spiritual importancea,b |
Spiritual importanceb |
Spiritual importancea,b |
Spiritual importancea,b |
| Meditation use in wave 1b |
Massage use in wave 1b |
Herbal use in wave 1b |
Chiropractic use in wave 1b |
| Sexa,b |
Sexa,b |
Sexa |
|
| Educationa,b |
Educationa |
Educationa |
|
| Depressiona |
|
|
Depressiona |
| Racea |
|
|
Racea |
Variable from W1 is a significant predictor for CHA use in W2.
Variable from W2 is a significant predictor for CHA use in W3.
CHA, complementary health approach.
Discussion
We present the first analyses of the longitudinal and repeated use of complementary health approaches in a national probability sample of adults. Numerous researchers have analyzed the characteristics of adults using complementary health approaches to better understand trends and health predictors but are limited to prevalence data, specific disease outcomes, and restricted periods of time.1–5,13,14,16–18,22–24,26–30 Using the MIDUS data collection from nearly two decades (1995 to 2014), we were able to address this research gap and provide greater insight on the use of multiple complementary health approaches over time, and how a variety of predisposing factors may influence the decision to use these complementary health approaches long term.
Similar to National Health Interview Survey (NHIS) prevalence data between 2002 and 2012, we saw increases in the use of meditation, chiropractic, and massage therapy.4,27 The use of meditation and chiropractic approaches was also highest among adults aged 45–64 in 2017.4 The prevalence of use across all four approaches was also highest among adults aged 45–64 from wave 2 to wave 3.
The need for treatment of low back pain and similar conditions was present in the MIDUS population. We noticed that as the MIDUS population aged, the prevalence of joint/bone disease increased across waves, and the prevalence of sciatica/lumbago/recurring backache remained steady. In response to the opioid crisis occurring during and proceeding wave 3 of MIDUS, the American College of Physicians and other medical organizations have recommended the treatment of low back pain with nonpharmacological therapies such as massage and spinal manipulation.32 Although these recommendations were made after wave 3 of our analysis (2013–2014), it remains plausible that people who experienced pain unresolved by or refusing conventional treatment, including opioids, may have been more likely to try or continue using complementary health approaches during this period of time.33–35 Thus, this may have at least partially contributed to the increase in complementary health approach use between waves, particularly waves 2 and 3 among mid-life adults.32,36
In a similar cross-sectional analysis using MIDUS data from wave 1, individuals who reported any complementary health approach use were more likely to be female, white, or college educated than those who did not use any complementary health approach.1 Having a mental health condition such as depression is also associated with complementary health approach use, especially mind–body interventions.1,37
Our results affirm the association among females across meditation, massage therapy, and herbal products for new and continued/discontinued use. Adults with higher education were more likely to use one of the four approaches, but race and depression were only significantly related to use of meditation and chiropractic. Other characteristics, including personality traits,1 health literacy skills, and health-seeking behaviors,38 may also contribute to using complementary health approaches among people with depression who may already be receiving conventional care; however, it is not possible to determine this from the data. Chiropractic use may be affected by greater barriers to access, including limited knowledge of chiropractic care and cost, which could explain these differences.39 In a one year follow-up study, patients with rheumatic conditions reported perceived expense as a common reason that patients stopped using complementary health approaches.40
It is also important to note the effect of previous complementary health approach use in wave 1. We consistently found that among wave 2 users, previous wave 1 use of each modality was a significant predictor for future use in wave 3. Our finding is unique, particularly since previous use was significantly associated for all continued/discontinued and new use models, which suggests that prior use may be a stronger predictor than other predisposing factors when analyzing long-term use. The relationships between previous use and our predisposing sociodemographic factors are complex in nature. As mentioned earlier, although certain demographics (i.e., sex, education, and race) have been typically associated with complementary health approach use by other researchers,4,13,16,19–22 our wave 2 to 3 analyses demonstrate how the addition of prior use to a comprehensive model may cause some of the these demographics to be less significant factors.
In a review of complementary health approach studies, Sharma describes types of complementary health users, including “stable users” who continuously use one modality, “one-off users” who discontinue use after a brief period, and “earnest seekers” who continuously try different modalities.7 Longitudinal studies investigating smaller disease-specific cohorts have found that most complementary health approach users were most likely “one-off users” or “earnest seekers,” whereas cross-sectional studies reported “stable users.”8,40,41 Our results support this idea with very few individual usage patterns (Table 2) depicting continued use in two or more waves. Significant factors related to new use were consistently associated with the psychological predisposing factors of spiritual importance.
Hildreth and Elman examined the impact of predisposing health beliefs, including spirituality, on complementary health approach use and found that those with higher self-rated spirituality had a greater probability of using any and increased complementary health approaches compared with those who reported lower levels of spirituality. Spirituality has been defined as a midlife phenomenon occurring later in life among older adults.31 Our analysis, which largely comprised people within this age range, describes age and spiritual importance as significant factors related to the new use chiropractic, herbal products, massage therapy, and meditation.
Two other longitudinal studies have described complementary health approach use and trends, but they are limited to women and exclude men from the sample.19,21 The first19 examined the trends (2006 to 2010) of complementary health approach use in a cohort of women in Australia and found similar prevalence when compared with the NHIS data.29 They also found that the prevalence of complementary health approach use remained stable across both young (18–23) and middle-aged (45–50) women but did not differentiate between continuous and new use as our study did, while also including a wider age range (25–74 years). These results were consistent with another longitudinal study of women aged 42–52 years in the United States, which described complementary health approach use and was grouped by menopausal status and analyzed prospectively from 1996 to 2003.21 The prevalence of complementary health approach use remained stable in this cohort as well, as did the individual per person use of complementary health approach types (nutritional and herbal remedies, physical methods, and psychological methods), but temporal trend data were not described. Our results also demonstrated that the prevalence of continued complementary health approach use was consistent across all four modalities.
Although prevalence data from the previously cited longitudinal studies19,21 did show a substantial increase in herbal and natural products (i.e., vitamins/minerals) used among women for both cohorts in the United States and Australia,21,19 age was not a significant factor associated with complementary health approach use. This is contradictory to our results, which found that age was a significant factor, especially for the association of new complementary health approach use. These differences may result from differences in the populations studied, the survey questionnaires, the analyses plan, and the length of time followed.
In addition, when conducting our prevalence and longitudinal analysis, the question of how to interpret and distinguish new and continued/discontinued complementary health approach use was confronted. We hypothesized that continued or discontinued complementary health approach use may represent a lifestyle decision or a new perspective on life that could be motivating “one-off users.” New complementary health approach use could be indicative of an event such as a new medical diagnosis, which may inspire “earnest seekers.” This distinction is especially important to consider when examining prevalence data, because it is challenging to identify groups or individuals practicing new or continued complementary health approach use.
There is limited research that describes new use of complementary health approaches at the time of diagnosis, with many studies focusing on disease treatment or management.42–44 Among patients with cancer, there is an increased use of complementary health approaches during and after treatment, with the primary intent to relieve disease and treatment related side effects.44 Future studies will need to investigate these potential associations and differences between new and continued/discontinued complementary health approach use, disease diagnosis and progression, and other life-changing events. Additional research is also needed to confirm our findings and investigate other important populations such as veterans, where there are significant gender and race/ethnicity differences among complementary health users.45,46
Study limitations and future directions
Our study team used the MIDUS data, which were restricted to participants aged 25–74 years. These analyses were not adjusted to precisely represent the general population of the United States. Additional longitudinal data sources made available on younger and older populations would identify how new and continued complementary health approach use may change for adolescents and aging adults.
Hispanic ethnicity questions were not asked among wave 1 participants, and therefore not included in our analyses. Because of sample-size issues and inconsistent survey questions between wave 1 and waves 2 and 3, we defined race into two groups (white and other) and did not see any significant association between complementary health approach use and race; this is contrary to previous findings that support significant differences.19,27,47 For instance, NHIS data support significant trends in the use of complementary health approaches among Hispanic, non-Hispanic black, and non-Hispanic other adults from 2002 to 2012.27 Health literacy, acculturation, and health care access may help explain racial and ethnic differences in the use of complementary health approaches.47,48 MIDUS is limited to English-speaking adults, which may have resulted in the exclusion of some racial and ethnic groups, especially Hispanics, Asians, and Pacific Islanders who do not speak English.49
Study sample size is another important factor that influences both ethnic representation and reporting of complementary health approaches.50,51 Nationally represented studies report limited categories for race and ethnicity and lose racial/ethnic subgroups. Larger surveys, including MIDUS, also provide very little details on the definition of complementary health approaches, which may exclude culturally specific approaches. Further exploration on how race and ethnicity affects the association of complementary health approach use could be expanded by using the Midlife in Japan (MIDJA) data set and the subsample of African Americans from the MIDUS Milwaukee cohort.52,53
The MIDUS survey instrument also limits the definition of complementary health approach use; the survey asks whether any “relaxation or meditation techniques” were used, without distinguishing between these techniques, whereas herbal products and chiropractic use do not include a definition or relevant examples. The survey used in this study also does not specify frequency of use.
Wolsko and colleagues found that, though relatively few in number, the most frequent users of complementary health approaches make up most of the expenditures for complementary health approach use.54 Among 44% of complementary health approach users in a U. S. represented sample, only 8.9% accounted for more than 75% of the complementary health approach visits in 1997. Likewise, analyses of the Medical Expenditure Panel Survey showed a 57% increase in chiropractic use (between 2000 and 2003) and a 56% increase in expenditure costs (between 1997 and 2006).55 Considering differences in the current typical cost of our four approaches of interest, we adjusted for total household income, which may have partially controlled for the potential influence of the ability to afford various cost differences associated with approaches. Future research in this area may consider how barriers (i.e., income or cost of approach) may impact or influence long-term use.
Our analyses were limited to individuals who completed the SAQ. Nonparticipants in our analyses can be placed in three categories: died between waves; lost to follow-up; and did not complete the SAQ. Consistent with a large body of research, previous analyses of MIDUS data found that higher mortality rates were seen in older individuals, participants with lower education, smokers, and those with low levels of physical activity. Body mass index, race, and age were not associated with mortality in MIDUS.56 Age, sex, education, and race are also predictors of retention in MIDUS.57 Therefore, it is not surprising that the characteristics of the MIDUS sample in wave 3 differ significantly from those in wave 1 (Table 1).
These differences may account for some of the inconsistencies in our data even after adjustment if those participants who died or were lost to follow-up were likely to use complementary health approaches than those who participated in all three waves. Interestingly, the use of complementary health approaches in the MIDUS study has been found to predict retention in subsequent waves.56 This could, at least partly, explain the increased prevalence of complementary health approaches seen in waves 2 and 3 versus wave 1. Our findings also reinforce the importance of investigating complementary health approach use since it may signal a potential increase in commitment to one's health.
Lastly, the methods used in our analysis are limited to the association of predisposing factors and the outcome of complementary health approach use; thus, we cannot interpret causality. Despite these limitations, our novel results provide a greater understanding of the factors predicting frequently used complementary health approaches, and how these factors differently impact new versus continuing/discontinuing use.
Conclusion
We present the first longitudinal study of complementary health approaches in a nationally representative adult U.S. sample; these data distinguish between new and continued/discontinued use of complementary health approaches more than nearly two decades and provide insights into the interpretation of the prevalence of complementary health approach data. Moreover, this article has compared four prominent complementary health approaches and found that predisposing factors such as age, sex, and education influence new and continued use of complementary health approaches differently, with prior use of each modality having the most significant effect on future use. As new data are collected, and additional cross-sectional findings continue to unveil important predictors of complementary health approach use in unique samples, our study will play an important role in identifying factors that drive complementary health approach use and will serve as baseline knowledge for related education and outreach efforts to patients, providers, and health plans.
Supplementary Material
Acknowledgments
The authors would like to express their gratitude to their colleagues at the National Center for Complementary and Integrative Health, Partap Khalsa, Peter Murray, Barbara Stussman, and Termeh Feinburg for reviewing and providing their comments on the previous drafts of the article.
Authors' Contributions
R.S. and R.L.N. determined the methodology used, analyzed the data, and wrote and edited the article. R.S. created the figures and identified the significant survey variables to be included in the study. W.W. analyzed the data, edited the article, and proposed the idea for this study.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was done as part of the official duties of the authors.
Supplementary Material
References
- 1. Honda K, Jacobson JS. Use of complementary and alternative medicine among United States adults: The influences of personality, coping strategies, and social support. Prev Med 2005;40:46–53 [DOI] [PubMed] [Google Scholar]
- 2. Hildreth KD, Elman C. Alternative worldviews and the utilization of conventional and complementary medicine. Sociol Inq 2007;77:76–103 [Google Scholar]
- 3. Nahin RL, Dahlhamer JM, Taylor BL, et al. Health behaviors and risk factors in those who use complementary and alternative medicine. BMC Public Health 2007;7:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clarke TC, Barnes PM, Black LI, et al. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief 2018:1–8 [PubMed] [Google Scholar]
- 5. Mbizo J, Okafor A, Sutton MA, et al. Complementary and alternative medicine use among persons with multiple chronic conditions: Results from the 2012 National Health Interview Survey. BMC Complement Altern Med 2018;18:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen's Behavioral Model of Health Services Use: A systematic review of studies from 1998–2011. Psychosoc Med 2012;9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sharma U. Complementary Medicine Today: Practitioners and Patients. London: Routledge, 1992. [Google Scholar]
- 8. Yang S, Dubé CE, Eaton CB, et al. Longitudinal use of complementary and alternative medicine among older adults with radiographic knee osteoarthritis. Clin Ther 2013;35:1690–1702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Center for Health Statistics. National Health and Nutrition Examination Survey. Online document at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm, accessed February17, 2020
- 10. National Center for Health Statistics. 2012. NAMCS MircoData File Documentation. Online document at: https://data.nber.org/namcs/docs/namcs2012.pdf, accessed February17, 2020
- 11. Midlife in the United States (MIDUS): A national longitudinal study of health and well-being. Online document at: http://midus.wisc.edu/data/index.php, accessed February17, 2020
- 12. Centers for Disease Control and Prevention. CDC National Health Interview Survey. Online document at: https://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm, accessed February17, 2020
- 13. Bausell RB, Lee WL, Berman BM. Demographic and health-related correlates to visits to complementary and alternative medical providers. Med Care 2001;39:190–196 [DOI] [PubMed] [Google Scholar]
- 14. Bridevaux IP. A survey of patients' out-of-pocket payments for complementary and alternative medicine therapies. Complement Ther Med 2004;12:48–50 [DOI] [PubMed] [Google Scholar]
- 15. Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA 1999;282:651–656 [DOI] [PubMed] [Google Scholar]
- 16. Keith VM, Kronenfeld JJ, Rivers PA, et al. Assessing the effects of race and ethnicity on use of complementary and alternative therapies in the USA. Ethn Health 2005;10:19–32 [DOI] [PubMed] [Google Scholar]
- 17. Nguyen HT, Grzywacz JG, Lang W, et al. Effects of complementary therapy on health in a national U.S. sample of older adults. J Altern Complement Med 2010;16:701–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tom Xu K, Farrell TW. The complementarity and substitution between unconventional and mainstream medicine among racial and ethnic groups in the United States. Health Serv Res 2007;42:811–826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bowe S, Adams J, Lui CW, et al. A longitudinal analysis of self-prescribed complementary and alternative medicine use by a nationally representative sample of 19,783 Australian women, 2006–2010. Complement Ther Med 2015;23:699–704 [DOI] [PubMed] [Google Scholar]
- 20. Shorofi SA, Arbon P. Complementary and alternative medicine (CAM) among Australian hospital-based nurses: Knowledge, attitude, personal and professional use, reasons for use, CAM referrals, and socio-demographic predictors of CAM users. Complement Ther Clin Pract 2017;27:37–45 [DOI] [PubMed] [Google Scholar]
- 21. Bair YA, Gold EB, Zhang G, et al. Use of complementary and alternative medicine during the menopause transition: Longitudinal results from the Study of Women's Health Across the Nation. Menopause 2008;15:32–43 [DOI] [PubMed] [Google Scholar]
- 22. Mcmahan S, Lutz R. Alternative therapy use among the young-old (Ages 65 to 74): An evaluation of the MIDUS database. J Appl Gerontol 2004;23:91–103 [Google Scholar]
- 23. Ellison CG, Bradshaw M, Roberts CA. Spiritual and religious identities predict the use of complementary and alternative medicine among US adults. Prev Med 2012;54:9–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kiefer DS, Chase JC, Love GD, et al. The Overlap of Dietary Supplement and Pharmaceutical Use in the MIDUS National Study. Evid Based Complement Alternat Med 2014;2014:823853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brim OG, Ryff CD, Kessler RC. The MIDUS National Survey: An overview. In: Brim OG, Ryff CD, Kessler RC, eds. How Healthy Are We? A National Study of Well-Being at Midlife. Chicago, IL: University of Chicago Press, 2004:1–36 [Google Scholar]
- 26. Barnes PM, Powell-Griner E, McFann K, et al. Complementary and alternative medicine use among adults: United States, 2002. Adv Data 2004;343:1–19 [PubMed] [Google Scholar]
- 27. Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report 2015;79:1–16 [PMC free article] [PubMed] [Google Scholar]
- 28. Clarke TC. The use of complementary health approaches among U.S. adults with a recent cancer diagnosis. J Altern Complement Med 2018;24:139–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008:1–23 [PubMed] [Google Scholar]
- 30. Macinko J, Upchurch DM. Factors associated with the use of meditation, U.S. Adults 2017. J Altern Complement Med 2019;25:920–927 [DOI] [PubMed] [Google Scholar]
- 31. Wink P, Dillon M. Religiousness, spirituality, and psychosocial functioning in late adulthood: Findings from a longitudinal study. Psychol Aging 2003;18:916–924 [DOI] [PubMed] [Google Scholar]
- 32. American College of Physicians (ACP). American College of Physicians issues guideline for treating nonradicular low back pain. Online document at: https://www.acponline.org/acp-newsroom/american-college-of-physicians-issues-guideline-for-treating-nonradicular-low-back-pain, accessed December9, 2020
- 33. Whedon JM, Toler AWJ, Kazal LA, et al. Impact of chiropractic care on use of prescription opioids in patients with spinal pain. Pain Med 2020;21:3567–3573 [DOI] [PubMed] [Google Scholar]
- 34. Whedon JM, Toler AWJ, Goehl JM, et al. Association between utilization of chiropractic services for treatment of low-back pain and use of prescription opioids. J Altern Complement Med 2018;24:552–556 [DOI] [PubMed] [Google Scholar]
- 35. Kazis LE, Ameli O, Rothendler J, et al. Observational retrospective study of the association of initial healthcare provider for new-onset low back pain with early and long-term opioid use. BMJ Open 2019;9:e028633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. 2018: Managing neck and back pain in America. The 2018 Gallup-Palmer College of Chiropractic Annual Report. Online document at: https://www.palmer.edu/alumni/research-publications/gallup-report/managing-neck-and-back-pain-in-america/, accessed December9, 2020
- 37. Prasad K, Ziegenfuss JY, Cha SS, et al. Characteristics of exclusive users of mind-body medicine vs. other alternative medicine approaches in the United States. Explore (NY) 2013;9:219–225 [DOI] [PubMed] [Google Scholar]
- 38. Solomon D, Adams J. The use of complementary and alternative medicine in adults with depressive disorders. A critical integrative review. J Affect Disord 2015;179:101–113 [DOI] [PubMed] [Google Scholar]
- 39. 2017: Americans prefer drug-free pain management. Gallup-Palmer College of Chiropractic Annual Report Americans' Views of Prescription Pain Medication and Chiropractic Care. Online document at: https://www.palmer.edu/alumni/research-publications/gallup-report/americans-prefer-drug-free-pain-management/Access, accessed February16, 2021
- 40. Rao JK, Kroenke K, Mihaliak KA, et al. Rheumatology patients' use of complementary therapies: Results from a one-year longitudinal study. Arthritis Rheum 2003;15;49:619–625 [DOI] [PubMed] [Google Scholar]
- 41. Rawsthorne P, Clara I, Graff LA, et al. The Manitoba Inflammatory Bowel Disease Cohort Study: A prospective longitudinal evaluation of the use of complementary and alternative medicine services and products. Gut 2012;61:521–527 [DOI] [PubMed] [Google Scholar]
- 42. Kwok JYY, Kwan JCY, Auyeung M, et al. The effects of yoga versus stretching and resistance training exercises on psychological distress for people with mild-to-moderate Parkinson's disease: Study protocol for a randomized controlled trial. Trials 2017;18:509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kwok JYY, Kwan JCY, Auyeung M, et al. Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with Parkinson disease: A randomized clinical trial. JAMA Neurol 2019;76:755–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chandwani KD, Ryan JL, Peppone LJ, et al. Cancer-related stress and complementary and alternative medicine: A review. Evid Based Complement Alternat Med 2012;2012:979213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Taylor SL, Hoggatt KJ, Kligler B. Complementary and integrated health approaches: What do veterans use and want. J Gen Intern Med 2019;34:1192–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Evans EA, Herman PM, Washington DL, et al. Gender differences in use of complementary and integrative health by U.S. Military Veterans with chronic musculoskeletal pain. Womens Health Issues 2018;28:379–386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kronenberg F, Cushman LF, Wade CM, et al. Race/ethnicity and women's use of complementary and alternative medicine in the United States: Results of a national survey. Am J Public Health 2006;96:1236–1242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kelly JP, Kaufman DW, Kelley K, et al. Use of herbal/natural supplements according to racial/ethnic group. J Altern Complement Med 2006;12:555–561 [DOI] [PubMed] [Google Scholar]
- 49. Tanaka MJ, Gryzlak BM, Zimmerman MB, et al. Patterns of natural herb use by Asian and Pacific Islanders. Ethn Health 2008;13:93–108 [DOI] [PubMed] [Google Scholar]
- 50. Gardiner P, Whelan J, White LF, et al. A systematic review of the prevalence of herb usage among racial/ethnic minorities in the United States. J Immigr Minor Health 2013;15:817–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hsiao AF, Wong MD, Goldstein MS, et al. Variation in complementary and alternative medicine (CAM) use across racial/ethnic groups and the development of ethnic-specific measures of CAM use. J Altern Complement Med 2006;12:281–290 [DOI] [PubMed] [Google Scholar]
- 52. Ryff C, Almeida D, Ayanian J, et al. Midlife in the United States (MIDUS 2): Milwaukee African American Sample, 2005–2006 (ICPSR 22840). Ann Arbor, MI: Inter-university Consortium for Political and Social Research. DOI: 10.3886/ICPSR22840.v5 [DOI] [Google Scholar]
- 53. Ryff CD, Kitayama S, Karasawa M, et al. Survey of Midlife in Japan (MIDJA), April-September 2008. (ICPSR30822). Ann Arbor, MI: Inter-university Consortium for Political and Social Research. DOI: 10.3886/ICPSR30822.v3 [DOI] [Google Scholar]
- 54. Wolsko PM, Eisenberg DM, Davis RB, et al. Insurance coverage, medical conditions, and visits to alternative medicine providers: Results of a national survey. Arch Intern Med 2002;162:281–287 [DOI] [PubMed] [Google Scholar]
- 55. Davis MA, Sirovich BE, Weeks WB. Utilization and expenditures on chiropractic care in the United States from 1997 to 2006. Health Serv Res 2010;45:748–761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Keyes CL, Simoes EJ. To flourish or not: Positive mental health and all-cause mortality. Am J Public Health 2012;102:2164–2172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. J Aging Health 2010;22:307–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.