Summary
Background
Caesarean section is one of the most commonly performed surgeries both in the hospital. The incidence of infections in cesarean section varies greatly around the world at 3–15%. SSI on is a multifactorial process that starts from the perioperative preparation, the patient, the type of surgery, the type of germ and other factors.
Aims
To determine the characteristics of patients, bacterial patterns, and risk factors for the incidence of SSI in Cipto Mangunkusumo National General Hospital in 2016–2018.
Method
This study was an observational study using a retrospective cohort method. The subject of this study were patients undergoing cesarean section in Cipto Mangunkusumo National General Hospital in 2016–2018 recruited using consecutive sampling method. Based on the data obtained, bivariate and multivariate analysis were conducted to determine the factors affecting post-caesarean SSI.
Results
A total of 2052 subjects were included in the study. There were 85 cases of surgical site infection (SSI) out of 2052 operations (4.14 %). A total of 85 SSI cases and 1967 control groups were included in the risk factor analysis. The most common bacteria found in surgical site infection culture were Staphylococcus aureus (16,5%), Klebsiella pneumoniae (12,9%), Escherichia coli (9,4%), Enterococcus faecalis (9,4%), and others (21,2%). Variables associated with SSI in this study is fetal distress (p=0,002; AOR = 2,265 CI 95 % 1,350–3,801) and BMI ≥30 kg/m2 (p=0,028; AOR 1,824 CI 95% 1,066–3,121).
Conclusion
Factors influencing the incidence of SSI post cesarean section was fetal distress (p=0,002; AOR = 2,265 CI 95 % 1,350–3,801) and BMI ≥30 kg/m2 (p=0,028; AOR 1,824 CI 95% 1,066–3,121).
Keywords: Surgical site infection, c-section, Bacterial pattern
Background
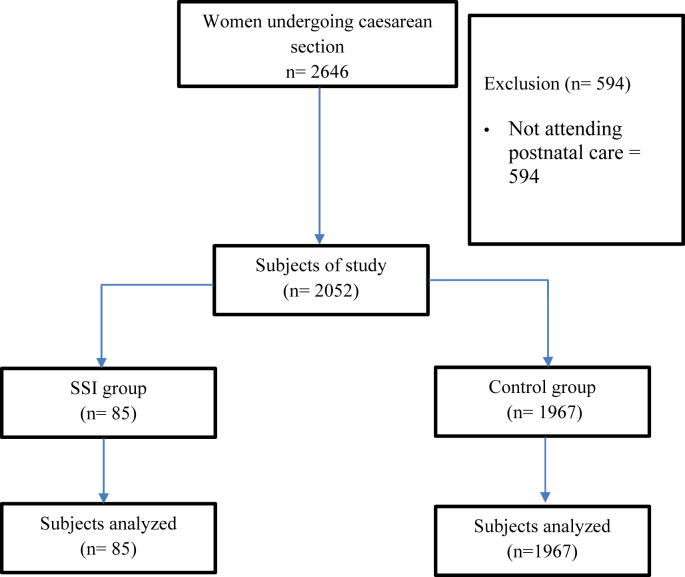
Cesarean section is one of the most frequent actions performed in the field of obstetrics within a hospital and may continue given the high incidence of cesarean section. In the last thirteen years the incidence of cesarean section has risen to 41% [1]. This is a global phenomenon, as cesarean section is now performed on 32% of total births in the United States, which concludes about 1.3 million operations yearly, while in the UK and Australia the number of cesarean section operation reached 26.5% and 32.3%. Furthermore, data in Indonesia showed that the number of cesarean sections in 2012 was 15.3% [1,2]. Like any other operation, cesarean section may be followed by various complications, one of which a surgical site infection (SSI) [1] (Figure 1).
Figure 1.
Research Flow.
Several risk factors associated with the occurrence of surgical site infection after cesarean section have been identified. The identification of these factors plays an important role in determining the methods that can be used to reduce the risk of SSI. Risk factors can be divided into three categories. 1) factors related to host, 2) factors related to pregnancy and intrapartum and 3) factors related to surgery [2].
Factors related to the host include too old or too young maternal age, obesity, living in rural areas (compared to living in urban area), gestational diabetes mellitus, history of previous cesarean section, recurrent miscarriage, preoperative maternal conditions (American Society of Anesthesiologist (ASA) score >3) [[2], [3], [4]]. While factors related to pregnancy include hypertension, gestational diabetes, multiple pregnancies, premature rupture of membranes, greater number of internal examinations, prolonged parturition of the trial before surgery, use of epidural anesthetics, use of internal fetal monitoring, and chorioamnionitis [4]. Meanwhile, factors related to cesarean section itself are emergency surgeries, no antibiotic prophylaxis, cases related to uterine rupture, cesarean section with hysterectomy, need for transfusion, and longer operative time. Operating time of more than 1 hour is associated with up to two times the risk of SSI [5].
Various studies have been performed in order to determine factors affecting the rate of surgical site infection in post caesarean patients. However, few of the studies were performed in a tertiary care hospital, which has more severe cases and therefore complications. In order to reduce the rate of surgical site infection in caesarean section patients, a study investigating the risk factors was performed.
Methods
An analytic observational study using cohort retrospective method was done. The population were all women undergoing caesarean section within the course of the study. In the study period, a sample of 2,052 women undergoing caesarean section were included. Patients with an incomplete medical record, not attending postnatal care, or died within 30 days of birth were excluded from the study. The data were then analyzed by two groups (surgical site infection group vs. control group). Ethical clearance was issued from ethical committee in Faculty of Medicine, Universitas Indonesia with ethical clearance number of 19/06/0736.
Results and discussion
In this study, there were 85 cases of surgical site infections (SSI) out of 2052 surgeries (4.14%) (Table 1). This figure is not much different from the results of similar studies in Israel with a percentage of 3.7% SSI and in North America with a percentage of 2.7% [4,6]. This figure is lower than similar studies conducted in other Southeast Asia countries such as Thailand which had a rate of 5.9% [7]. Previous research shows that the post caesarean SSI rate in developed countries ranges from 1.5% - 7.0% while the rate for developing countries is about 6% [6,8].
Table 1.
Baseline characteristics of subjects
| Variables | N = 2052 |
|---|---|
| Maternal Age | 30 (13–47) |
| Gestational age | |
| Preterm | 1.159 (56,5%) |
| Term | 893 (43,5%) |
| Gravid | |
| Primigravid | 702 (34,2%) |
| Multigravid | 1.350 (65,8%) |
| Parity | |
| Primiparous | 809 (39,4%) |
| Multiparous | 1.243 (60,6%) |
| Abortion history | |
| Yes | 446 (21,7%) |
| No | 1606 (78,3%) |
| Operation type | |
| Elective | 183 (9,0%) |
| Emergency | 1867 (91,0%) |
| Previous Caesarean Section history | |
| Yes | 560 (27,3%) |
| No | 1492 (72,7%) |
| Body mass index | 25,28 (16,89–50,59) |
| Hemoglobin level | 11,7 (6,4–17,7) |
| Premature Rupture of Membrane (PROM) | |
| Yes | 771 (37,6%) |
| No | 1281 (62,4%) |
| Gestational Hypertension | |
| Yes | 682 (33,2%) |
| No | 1370 (66,8%) |
| Fetal distress | |
| Yes | 397 (19,3%) |
| No | 1655 (80,7%) |
| Antepartum hemorrhage | |
| Yes | 143 (7%) |
| No | 1909 (93%) |
| Dystocia | |
| Yes | 75 (3,7%) |
| No | 1977 (96,3%) |
| Diabetes mellitus | |
| Yes | 71 (4,0%) |
| No | 1724 (96%) |
| Intrauterine infection | |
| Yes | 141 (6,9%) |
| No | 1911 (93,1%) |
| HIV | |
| Yes | 41 (2,0%) |
| No | 2011 (98%) |
| Glucose blood level | 105,8 (43,99) |
| Leucocyte level | 14.197 (13.110) |
| Serum albumin level | 4,01 (6,75) |
Samples for culture in this study were taken from the wound base, discharge, or lochia. However, cultures that were considered representative of SSI were cultures that taken from the wound base, but not all patients had samples taken for bacterial culture in this study, due to the financial cost, for some patients. The bacteria most often found in this study were Staphylococcus aureus (16.5%), followed by Klebsiella pneumoniae (12.9%), Escherichia coli (9.4%), Enterococcus faecalis (9.4%), and other pathogens like Streptococcus epidermidis and Acinetobacter baumanii (Table 2).
Table 2.
Characteristics of SSI
| Characteristics | N = 85 |
|---|---|
| SSI classification | |
| Incisional superficial | 79 (92,9%) |
| Incisional deep | 4 (4,7%) |
| Organ/space | 2 (2,4%) |
| Culture result | |
| Klebsiella pneumoniae ss. Pneumoniae | 11 (12,9%) |
| Escherichia coli | 8 (9,4%) |
| Enterococcus faecalis | 8 (9,4%) |
| Pseudomonas sp. | 2 (2,4%) |
| Staphylococcus aureus | 14 (16,5%) |
| Others | 18 (21,2%) |
| Sterile | 6 (7,1%) |
| Treatment | |
| Wound care | 65 (76,5%) |
| Re-operation | 20 (23,5%) |
Culture results of this study were consistent with similar studies such as a study in Tanzania showing that Staphylococcus aureus as one of the most common bacterium causing SSI in post-caesarean patients, and particular superficial infections [2,9]. In addition, the study found that S. aureus in post cesarean section SSI cultures were resistant to ampicillin, co-trimoxazole, and erythromycin. In this study antibiotic resistance tests were not included in the study. In addition, the results showed that Klebsiella pneumoniae was the second most prevalent bacteria in SSI post cesarean section, especially in internal and organ infections [9]. In research conducted in Israel, Escherichia coli is one of the organisms that are often found in post caesarean SSI [2]. In another study in Tanzania, E. coli obtained from the post-Caesarean SSI culture had high resistance to ampicillin, a combination of amoxicillin/clavulanate, tetracycline, and co-trimoxazole [9].
Besides the normal flora of the skin, vagina, and the gastrointestinal tract, there are bacteria that originate from opportunistic bacteria originating from hospital-caused infections (HCAI/Healthcare Associated Infection), namely Acinetobacter spp. In this study, it was found that 8 (9.41%) research subjects having Acinetobacter sp in cultures. Acinetobacter spp. is recognized to be a nosocomial pathogen found in healthcare enviroments, often causing hospital-acquired pneumonia (HAP) with associated significant resistance to antibiotics [10].
In the patients with SSI, 65 cases (76.5%) were treated with standard wound care, while 20 other cases needed re-operation (23.5%). SSI is generally considered as one of the causes of prolongation of the duration of postoperative hospitalization and additional costs for patients with various types of surgery, including cesarean section [11]. Uniquely, a study in the UK shows that the stitching method used in caesarean section affects the rate of SSI, with the smallest percentage of SSI occuring in subcuticular sutures and the largest percentage obtained in interrupted sutures [12].
In this study, high body mass index (BMI), BMI ≥ 30 kg/m2 was associated with increased risk of SSI (p = 0.028; OR 1.824 CI95% 1.066–3.121) (Table 3, Table 4). This is consistent with previous studies in the UK where BMI >30 kg/m2 was known as a risk factor for complications in surgery [13]. Obesity as a risk factor for SSI is due to an increase in relatively avascular adipose tissue, increase in the area of the surgical wound and reduced prophylactic antibiotic penetration into the adipose tissue [14].
Table 3.
Bivariate analysis of SSI risk factors
| Variables | Study groups |
P | OR | CI 95% | |
|---|---|---|---|---|---|
| SSI (n=85) | Control (n=1967) | ||||
| Age | 29 (17–43) | 30 (17–49) | 0,240 | ||
| Gravid | 2 (1–6) | 2 (0–12) | 0,839 | ||
| Parity | 1 (0–4) | 1 (0–10) | 0,887 | ||
| Abortion history | 0 (0–3) | 0 (0–10) | 0,212 | ||
| Gestational age | 0,635 | 1,86 | 1,19–2,9 | ||
| Preterm | 49 (57,6%) | 858 (43,6%) | |||
| Term | 34 (42,4%) | 1110 (56,4%) | |||
| Maternal age | 0,428 | 0,81 | 0,481–1,365 | ||
| < 35 | 64 (77,1%) | 1441 (73,1%) | |||
| ≥ 35 | 19 (22,9% | 528 (26,9%) | |||
| Operation type | 0,816 | 1,092 | 0,518–2,302 | ||
| Emergency | 75 (90,6%) | 1792 (91,1%) | |||
| Elective | 8 (9,4%) | 75 (8,9%) | |||
| History of diabetes | 0,173 | 1,90 | 0,74–4,88 | ||
| Yes | 5 (7,1%) | 66 (3,4%) | |||
| No | 66 (92,9%) | 1658 (96,6%) | |||
| Hemoglobin level | 11,6 ± 1,88 | 11,5 ± 1,87 | 0,836 | ||
| Hb < 11 g/dL | 28 (36,5%) | 721 (36,7%) | 0,644 | 0,89 | 0,56–1,43 |
| Hb ≥ 11 g/dL | 54 (63,5%) | 1246 (63,3%) | |||
| PROM | 0,461 | 0,84 | 0,52–1,33 | ||
| Yes | 28 (35,3%) | 743 (37,7%) | |||
| No | 55 (64,7%) | 1226 (62,3%) | |||
| Hypertension | 0,417 | 1,20 | 0,76–1,90 | ||
| Yes | 31 (38,8%) | 651 (33,0%) | |||
| No | 52 (61,2%) | 1318 (67,0%) | |||
| Fetal distress | 0,001 | 2,09 | 1,3-3,33 | ||
| Yes | 28 (32,9%) | 369 (18,7%) | |||
| No | 55 (64,7%) | 1600 (81,3%) | |||
| Intrauterine infection | 0,822 | 1,08 | 0,46–2,53 | ||
| Yes | 6 (11,8%) | 135 (7,3%) | |||
| No | 75 (88,2%) | 1823 (92,7%) | |||
| History of previous CS | 0,930 | 6,95 | 4,2–11,4 | ||
| Yes | 23 (29,42%) | 537 (27,2%) | |||
| No | 60 (70,58%) | 1432 (72,8%) | |||
| Antepartum hemorrhage | 0,513 | 0,97 | 0,44–2,15 | ||
| Yes | 7 (8,2%) | 136 (6,9%) | |||
| No | 76 (91,8%) | 1833 (95,1%) | |||
| Dystocia | 0,543 | 1,35 | 0,48–3,80 | ||
| Yes | 4 (4,7%) | 71 (3,5%) | |||
| No | 79 (95,3%) | 1898 (96,5%) | |||
| HIV history | 1,000 | 0,59 | 0,07–4,33 | ||
| Yes | 1 (1,1%) | 40 (2,0%) | |||
| No | 82 (98,9%) | 1929 (98,0%) | |||
| Additional operation | 0,04 | 1,97 | 1,019–3,792 | ||
| Yes | 11 | 142 | |||
| No | 72 | 1827 | |||
| BMI ≥ 30 | 0,035 | 1,767 | 1,035–3,017 | ||
| Yes | 48 (70,6%) | 343 (19,1%) | |||
| No | 20 (29,4% | 1455 (80,9%) | |||
Significance P<0,005.
PROM = premature rupture of membrane, CS = caesarean section, HIV = human immunodeficiency virus.
Table 4.
Risk factors of SSI
| Variables | P Value | OR | CI 95% |
|---|---|---|---|
| Fetal distress | 0,002 | 2,265 | 1,350–3,801 |
| BMI ≥ 30 kg/m2 | 0,028 | 1,824 | 1,066–3,121 |
Significance P<0,005.
Fetal distress was also considered to be one of the risk factors for SSI events in postoperative caesarean patients (p= 0.001, OR = 2.09, CI95% 1.3–3.33) (Table 4). Fetal distress is one of the indications of a cesarean section, in fact it is one of the three most frequent reasons for cesarean section [6]. One study that showed fetal distress as a risk factor for SSI was carried out by Moulton and colleagues [15]. Caesarean section due to fetal distress as a risk factor for SSI have not been widely discussed in other studies. One possible reason is the lack of optimal preparation of caesarean section in cases of fetal distress, but this requires further research.
Conclusions
This study found that the variables that played a role in the incidence of SSI were caesarean section due to fetal distress and BMI ≥ 30 kg/m2. Other variables, although clinically significant, are not considered to have statistical significance. The incidence of surgical site infection after caesarean section in this study was 4.14%.
Ethics approval and consent to participate
This study was acknowledged by Ethical Committee for Medical Research of Faculty of Medicine, University of Indonesia.
Conflict of interest statement
None declared.
Authors' contributions
MDW extracted, analyzed, and interpreted the data. AKH analyzed the data and interpreted the results. Both authors wrote, read and approved the final manuscript.
References
- 1.Kawakita T., Landy H.J. Surgical site infections after cesarean delivery: epidemiology, prevention and treatment. Matern Health Neonatol Perinatol. 2017;3(12):1–10. doi: 10.1186/s40748-017-0051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zuarez-Easton S., Zafran N., Garmi G., Salim R. Postcesarean wound infection: prevalence, impact, prevention, and management challenges. Int J Womens Health. 2017 Feb;9:81–88. doi: 10.2147/IJWH.S98876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths M. Institute for Health and Clinical Excellence; London: 2011. Royal College of obstetricians and gynaecologists, National collaborating center for women’s and children health. Caesarean section NICE clinical guideline. [Google Scholar]
- 4.Lakhan P., Doherty J., Jones M., Clements A. A systematic review of maternal intrinsic risk factors associated with surgical site infection following Caesarean sections. Healthc Infect. 2010 Jun;15(2):35–41. [Google Scholar]
- 5.Al Jama F.E. Risk factors for wound infection after lower segment cesarean section. Qatar Med J. 2012 Dec;2012(2):9. doi: 10.5339/qmj.2012.2.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ketcheson F., Woolcott C., Allen V., Langley J.M. Risk factors for surgical site infection following cesarean delivery: a retrospective cohort study. CMAJ Open. 2017 Jul 11;5(3):E546–E556. doi: 10.9778/cmajo.20160164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Assawapalanggool S., Kasatpibal N., Sirichotiyakul S., Arora R., Suntornlimsiri W. Risk factors for cesarean surgical site infections at a Thai-Myanmar border hospital. Am J Infect Control. 2016 Sep;44(9):990–995. doi: 10.1016/j.ajic.2016.01.031. [DOI] [PubMed] [Google Scholar]
- 8.Edwards J.R., Peterson K.D., Mu Y., Banerjee S., Allen-Bridson K., Morrell G. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009 Dec;37(10):783–805. doi: 10.1016/j.ajic.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Mpogoro F.J., Mshana S.E., Mirambo M.M., Kidenya B.R., Gumodoka B., Imirzalioglu C. Incidence and predictors of surgical site infections following caesarean sections at Bugando Medical Centre, Mwanza, Tanzania. Antimicrob Resist Infect Control. 2014;3(1):25. doi: 10.1186/2047-2994-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srun S., Sinath Y., Seng A.T., Chea M., Borin M., Nhem S. Surveillance of post-caesarean surgical site infections in a hospital with limited resources, Cambodia. J Infect Dev Ctries. 2013 Aug 15;7(8):579–585. doi: 10.3855/jidc.2981. [DOI] [PubMed] [Google Scholar]
- 11.Yehia N.A., Salama M.F., Al-Arbash A.J., Thomas S.A. Surveillance for surgical site infection after cesarean section: extra-length of stay and cost of infection. Egypt J Med Micro. 2007:473–479. [Google Scholar]
- 12.Johnson A., Young D., Reilly J. Caesarean section surgical site infection surveillance. J Hosp Infect. 2006 Sep;64(1):30–35. doi: 10.1016/j.jhin.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 13.Wloch C., Wilson J., Lamagni T., Harrington P., Charlett A., Sheridan E. Risk factors for surgical site infection following caesarean section in England: results from a multicentre cohort study: Risk factors for surgical site infection following c-section. BJOG Int J Obstet Gynaecol. 2012 Oct;119(11):1324–1333. doi: 10.1111/j.1471-0528.2012.03452.x. [DOI] [PubMed] [Google Scholar]
- 14.Olsen M.A., Butler A.M., Willers D.M., Devkota P., Gross G.A., Fraser V.J. Risk Factors for Surgical Site Infection After Low Transverse Cesarean Section. Infect Control Hosp Epidemiol. 2008 Jun;29(6):477–484. doi: 10.1086/587810. [DOI] [PubMed] [Google Scholar]
- 15.Moulton L.J., Munoz J.L., Lachiewicz M., Liu X., Goje O. Surgical site infection after cesarean delivery: incidence and risk factors at a US academic institution. J Matern Fetal Neonatal Med. 2018 Jul 18;31(14):1873–1880. doi: 10.1080/14767058.2017.1330882. [DOI] [PubMed] [Google Scholar]