Abstract
BACKGROUND AND OBJECTIVES
We measured within-hospital concordance of mothers with opioid use disorder (OUD) and newborns with neonatal abstinence syndrome (NAS) or opioid exposure (OE). Secondarily, we described the demographics of mothers and newborns with and without opioid-related diagnoses.
METHODS
We used hospital discharge abstracts from California, Florida, New Jersey, and Pennsylvania in 2016. Descriptive statistics were used to compare newborns and mothers with and without opioid-related diagnoses. Within-hospital frequencies of mothers with OUD and newborns with NAS and OE were compared. Pearson’s correlation coefficients were calculated.
RESULTS
In 474 hospitals, we found 896 702 mothers (0.6% with OUD) and 910 867 newborns (0.47% with NAS, 0.85% with OE, and 0.07% with both). Although the frequency of mothers and newborns with opioid-related diagnoses in a hospital was strongly correlated (r = 0.81), more infants were identified than mothers in most hospitals (68.3%). Mothers with OUD were more likely to be white (79% vs 40.9%), on Medicaid (75.4% vs 44.0%), and receive care in rural hospitals (20.6% vs 17.6%), compared with mothers without OUD. Newborns with NAS had demographics similar to women with OUD. Newborns with OE were disproportionately Black (22% vs 7%) or Hispanic (22% vs 9%).
CONCLUSIONS
More newborns are diagnosed with opioid-related disorders than mothers are. Although infants diagnosed with NAS had demographics similar to mothers with OUD, infants with OE were more likely to be Black or Hispanic. The lack of diagnostic coding of maternal OUD and the racial differences in diagnoses warrant attention.
Increased rates of opioid use disorder (OUD) among pregnant women have led to a fivefold increase in newborns with neonatal abstinence syndrome (NAS) in the past 10 years.1 The risk of developing NAS varies on the basis of the length and type of prenatal opioid exposure (OE), among other factors. Estimates as to the prevalence of NAS vary for a number of reasons, including differences in sample inclusion criteria (eg, related to types of prenatal substance exposures that have NAS as a possible outcome for the neonate) and lack of granularity in coding. Although NAS is a definitive way to mark complications from prenatal OE, many newborns with OE do not receive a diagnosis of NAS.2,3
Currently, the literature is focused almost exclusively on newborns with NAS because of the severity of their withdrawal symptoms, their burden of care (eg, cost and length of stay), and the ease of identifying them via medical coding.2,4–10 Although newborns with OE may exhibit signs of withdrawal from opioids, they do not exhibit signs that are either severe or numerous enough to meet the criteria for NAS. The bases for the coding of OUD and NAS or OE include coding briefs issued by specialty societies,11 provider knowledge, and state requirements.12,13 We were interested in identifying and describing newborns with NAS and OE in administrative data and comparing diagnosis patterns of NAS and OE among newborns with OUD among mothers within hospitals.
Newborns with OE share many of the same vulnerabilities as newborns with NAS, such as a higher risk for preterm birth and low birth weight compared with newborns without NAS or OE.2 Many newborns with OE are treated with nonpharmacologic measures alone, and these treatments do not necessarily get documented in the chart.12 Newborns with OE, who are not easy to identify in administrative data,12,13 are underrepresented in the literature. The demographic characteristics of newborns with NAS, compared with those of other newborns, have been described.2 Little is known, however, about the demographics of newborns with OE. We were motivated to consider potential racial disparities in the diagnosis of infants with OE because of the implications this has for their health care.
If newborns and mothers are not coded consistently for NAS, OE, or OUD or if there are significant demographic differences between these groups, there are implications for individual and population health outcomes. For example, preparation for a successful transition to home may be undermined, leading to increased rates of readmission. At the population level, public health departments’ capacity to respond to the needs of newborns with NAS or OE and mothers with OUD is predicated on understanding the extent of the problem, which requires, at a minimum, accurate coding. Furthermore, proper coding has implications for the ability to conduct accurate research, assess quality performance, and ensure appropriate reimbursement.
The purposes of this study were to identify and describe mothers with OUD and newborns with NAS or OE in administrative data and evaluate concordance within hospitals of the frequencies of mothers and newborns with these diagnoses. In addition, we compared the demographic characteristics of mothers and newborns with opioid-related diagnoses with the demographic characteristics of those without as well those of newborns with an NAS or OE diagnosis.
Methods
Design and Data
In this descriptive observational study, we used patient data from state discharge abstracts from 2016. These annual inpatient discharge summaries were obtained from the Office of Statewide Health Planning and Development in California, Healthcare Cost and Utilization Project’s State Inpatient Database for Florida, New Jersey Department of Health and Senior Services, and Pennsylvania Health Care Cost Containment Council. Hospital characteristics data were obtained from the 2016 Annual Survey by the American Hospital Association (AHA) and merged with the patient data by using the AHA hospital identifier. Hospitals were included in the sample if they had at least 1 mother with OUD or 1 newborn with NAS or OE, given that at least 1 mother or newborn with an opioid-related diagnosis would be needed to identify whether there was concordant coding.
Procedure
To identify mothers in the data set, the enhanced algorithm by Kuklina et al14 was used to create a crosswalk from the International Classification of Diseases, Ninth Revision, (ICD-9) to the International Classification of Diseases, 10th Revision (ICD-10). In this enhanced algorithm, more diagnosis codes and diagnosis related groups are used to identify obstetric hospitalizations than the single V code for outcome of delivery. To fulfill these purposes, we adapted existing ICD-9 algorithms to ICD-10 codes to identify mothers with OUD, birth hospitalizations, and newborns with NAS or OE. Among obstetric hospitalizations, mothers with OUD were identified by using ICD-10 codes F11.1, F11.2, and F11.9 (opioid abuse, dependence, and unspecified, respectively) and T40.0 to T40.4 and T40.6 (poisoning by adverse effect of Iopioids).15,16 Newborns were identified by using ICD-10 code Z38 (liveborn infant) and included in the sample if their age was 0 years. Newborns with NAS were identified by using ICD-10 code P96.1 (neonatal withdrawal symptoms from maternal use of drugs of addiction), and newborns with OE were identified by using ICD-10 code P04.4 (newborn [suspected to be] affected by maternal use of drugs of addiction) because this code was the most specific code available in 2016 data.7 Newborns with prenatal exposure to tobacco, alcohol, and marijuana, all of which receive their own specific International Classification of Diseases (ICD) codes, are excluded from the P04.4 code. The use of P04.4 leads to an inaccurate OE prevalence, in that it includes nonopioid drugs of addiction (eg, cocaine), which are the minority of cases. We excluded P04.1 (newborn affected by other maternal medication) because we assumed that the majority of these medications were not opioids. It is possible, however, that a small number of these newborns were exposed to opioids, leading to a minor inaccuracy in the prevalence of OE among newborns. This ICD code was made more specific in 2018 with the addition of a second decimal place.12,13 We wanted only the birth hospitalization to accurately compare mothers and newborns. Therefore, only birth admissions were included in the sample. Mothers and newborns were excluded if they were transferred into the hospital. Twin and other multiple births were counted by using codes Z38.3x to Z38.8x, and we kept 1 newborn to represent each set.
Variables
Sociodemographic characteristics, including race and payer status of mothers and newborns, were measured from discharge abstract data. Hospital characteristics, including bed size, teaching status, high technology status, rurality, and state location, were measured from the AHA data.
Analyses
We calculated the sociodemographic characteristics, multiple birth status, state of residence, and rural or urban location of mothers with OUD and newborns with NAS or OE and compared them with the remaining mothers and newborns. We also compared the characteristics of newborns with OE and NAS. We described the structural characteristics of sample hospitals and distribution of hospitals by the volume of newborns with NAS and the median and interquartile range (IQR) numbers per hospital of mothers with OUD and newborns with NAS or OE. We graphed the frequencies of mothers and newborns for each hospital to visualize their degree of concordance. We calculated the frequencies of mothers and newborns by hospital. We conducted t tests, χ2 tests, analysis of variances, and Pearson’s correlation coefficients, as appropriate. We classified hospitals into 5 categories to evaluate the within-hospital concordance of OUD and NAS or OE diagnosis coding between mothers and newborns. Hospitals were divided into 5 categories, from hospitals that only had mothers with OUD to those that only had newborns with NAS or OE, with 3 categories in between. The hospitals that had both mothers with OUD and newborns with NAS or OE were put into the following categories: (1) the frequency of newborns was <80% of the frequency of mothers, (2) the newborns’ frequency was between 80% and 120% of that of the mothers, and (3) the newborn frequency was >120% of that of the mothers. Our rationale for this approach was that, ideally, concordance would be 100%. We labeled a hospital as having a close match when the frequencies of newborns with NAS and OE were between 80% and 120% of the mothers with OUD. Allowing for variation, we felt that these categories were clinically relevant, and no previous categories existed. We used a paired t test to test concordance between the mean number of infants with NAS or OE infants and mothers with OUD at the hospital level. We calculated correlation coefficients overall and by state of the number of newborns with OE or NAS and number of mothers with OUD at the hospital level.
Results
Overall, there were 896 702 mothers and 910 867 newborns in 474 hospitals in 4 states. The mothers gave birth at 474 hospitals, the majority of which were large (49.8%) and urban (79.6%). Almost one-half of the hospitals were located in California (47.9%); however, the 2 hospitals with the highest frequency of mothers with OUD were in Pennsylvania. The median number of mothers with OUD in hospitals was 5 but ranged from 0 to 269. In Table 1, we provide further description of the hospitals in the sample.
TABLE 1.
Characteristics of Hospitals
| Characteristics | Hospitals (N = 474) |
|---|---|
| Bed size, n (%) | |
| <100 | 51 (10.8) |
| 100–249 | 187 (39.5) |
| ≥250 | 236 (49.8) |
| Teaching status, n (%) | |
| None | 210 (44.3) |
| Minor | 224 (47.3) |
| Major | 40 (8.4) |
| Technology status, n (%) | |
| Low | 231 (49.5) |
| High | 236 (50.5) |
| Rural, n (%) | 84 (20.4) |
| State, n (%) | |
| California | 227 (47.9) |
| Florida | 105 (22.2) |
| New Jersey | 49 (10.3) |
| Pennsylvania | 93 (19.6) |
| NAS newborns per hospital, n (%) | |
| 0–10 | 353 (74.5) |
| 10–19 | 54 (11.4) |
| 20–39 | 48 (10.1) |
| ≥40 | 19 (4.0) |
| No. mothers with OUD per hospital, median (IQR) | 5 (12) |
| No. newborns with NAS or OE per hospital, median (IQR) | 14 (25) |
Among all mothers, 0.6% were diagnosed with OUD. Compared with all mothers, more mothers with OUD were white (79% vs 40.9%) and fewer were Hispanic (10.1% vs 33.4%) or Black (7.9% vs 11.8%). In addition, more mothers with OUD were on Medicaid (75.4% vs 44.0%), received care in rural hospitals (20.6% vs 17.6%), and were from Pennsylvania (35.5% vs 14.5%). Demographic information on the mothers in the sample is presented in Tables 2 and 3.
TABLE 2.
Characteristics of Mothers
| All Mothers (N = 896 702) | Mothers With OUD (n = 5448) | Pa | |
|---|---|---|---|
| Age, mean ± SD, y | 29.3 ± 5.9 | 28.9 ± 4.9 | <.001 |
| Race and/or ethnicity, n (%) | <.001 | ||
| White | 360 484 (40.9) | 4223 (79.0) | — |
| Black | 103 621 (11.8) | 421 (7.9) | — |
| Hispanic | 294 891 (33.4) | 538 (10.1) | — |
| Asian American | 85 676 (9.7) | 47 (0.9) | — |
| Other | 37 324 (4.2) | 116 (2.2) | — |
| Insurance status, n (%) | <.001 | ||
| Medicaid | 387 511 (44.0) | 3972 (75.4) | — |
| Private | 442 151 (50.2) | 973 (18.5) | — |
| Other | 51 358 (5.8) | 322 (6.1) | — |
| State, n (%) | <.001 | ||
| California | 455 336 (50.8) | 1305 (24.0) | — |
| Florida | 214 211 (23.9) | 1526 (28.0) | — |
| New Jersey | 97 442 (10.9) | 685 (12.6) | — |
| Pennsylvania | 129 713 (14.5) | 1932 (35.5) | — |
| Rural, n (%) | 139 438 (17.6) | 1020 (20.6) | <.001 |
—, not applicable.
We performed t tests and χ2 tests according to variable type. Mothers with and without OUD were mutually exclusive groups and were compared with each other. Newborns with and without NAS or OE were mutually exclusive groups and were compared with each other.
TABLE 3.
Characteristics of Newborns
| All Newborns (N = 910 867) | Newborns With NAS (n = 4280) | Newborns With OE (n = 7701) | Newborns With Both OE and NAS (n = 672) | Pa | |
|---|---|---|---|---|---|
| Race and/or ethnicity, n (%) | <.001 | ||||
| White | 363 564 (41.5) | 3341 (81.5) | 3813 (51.2) | 495 (77.7) | — |
| Black | 102 357 (11.7) | 280 (6.8) | 1625 (21.8) | 41 (6.4) | — |
| Hispanic | 281 530 (32.1) | 360 (8.8) | 1657 (22.2) | 75 (11.8) | — |
| Asian American | 80 649 (9.2) | 16 (0.4) | 67 (0.9) | 1 (0.2) | — |
| Other | 48 388 (5.5) | 102 (2.5) | 291 (3.9) | 25 (3.9) | — |
| Multiple birth, n (%) | 28 989 (3.2) | 100 (0.8) | 85 (1.1) | 114 (17.0) | <.001 |
| Insurance status, n (%) | <.001 | ||||
| Medicaid | 411 783 (46.0) | 3443 (83.2) | 6370 (83.7) | 542 (82.9) | — |
| Private | 423 975 (47.4) | 505 (12.2) | 784 (10.3) | 71 (10.9) | — |
| Other | 59 634 (6.7) | 190 (4.6) | 461 (6.1) | 41 (6.3) | — |
| State, n (%) | <.001 | ||||
| California | 459 043 (50.4) | 842 (19.7) | 3572 (46.4) | 204 (30.4) | — |
| Florida | 219 473 (24.1) | 1304 (30.5) | 2461 (32.0) | 190 (28.3) | — |
| New Jersey | 99 301 (10.9) | 506 (11.8) | 375 (4.9) | 81 (12.1) | — |
| Pennsylvania | 133 050 (14.6) | 1628 (38.0) | 1293 (16.8) | 197 (29.3) | — |
| Rural, n (%) | 141 988 (17.7) | 776 (19.7) | 1589 (23.1) | 155 (25.8) | <.001 |
—, not applicable.
We performed t tests and χ2 tests according to variable type. Mothers with and without OUD were mutually exclusive groups and were compared with each other. Newborns with and without NAS or OE were mutually exclusive groups and were compared with each other.
Of the 910 867 newborns in the sample, 4280 (0.47%) were diagnosed with only NAS, 7701 (0.85%) were diagnosed with only OE, and 672 (0.07%) were diagnosed with both. Thus, the total percentage of newborns with NAS or OE was 1.37%. Overall, newborn demographics followed that of their mothers. Among all newborns in the sample, most were white (41.5%) or Hispanic (32.1%), with 11.7% of newborns identified as Black. Among newborns with NAS, the vast majority were white (81.5%); few were Hispanic (8.8%), and even fewer were Black (6.8%). Although most newborns with OE were also white (51.2%), compared with newborns with NAS, more of the newborns with OE were Black (21.8%) or Hispanic (22.2%). Black infants are disproportionately in the OE group, compared with the overall newborn sample (21.8% vs 11.7%). In the overall sample, newborns were evenly split between public and private insurance. By contrast, more than four-fifths of newborns with OE only and NAS only were insured by Medicaid. Although only 14.6% of newborns in the sample were from Pennsylvania, they made up 38% of the newborns with NAS. Newborns with opioid-related diagnoses were more likely to be rural (23.1% for OE and 19.7% for NAS) than the overall sample of newborns (17.7%). Further sociodemographic details on the newborns are reported in Tables 2 and 3.
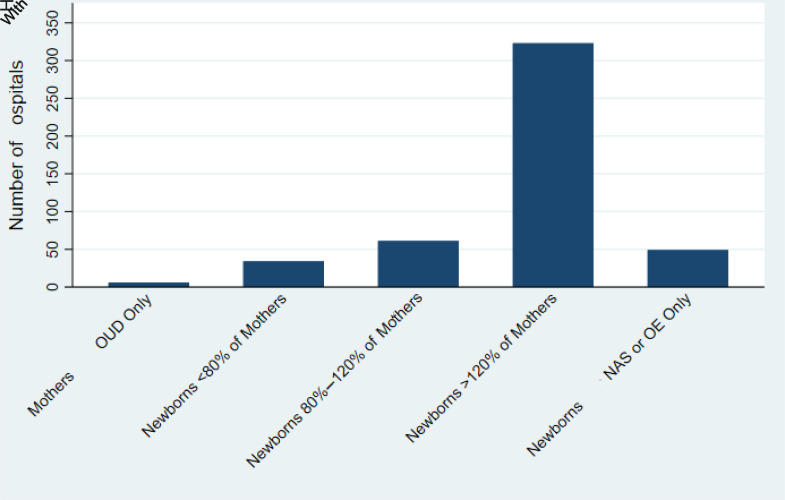
The distribution of mothers with OUD and newborns with NAS or OE varied across hospitals Supplemental Table 5). Here, NAS or OE includes diagnoses of NAS, OE, or both. Most hospitals (68.3%) had substantially more newborns with NAS or OE than mothers with OUD (the number of newborns was >120% of the number of mothers). Few hospitals (12.9%) had a close match (80%–120% of newborns relative to mothers) between the number of mothers and newborns. Similarly, 10.4% had newborns with NAS or OE but no mothers with OUD. Only 6 hospitals (1.3%) had mothers with OUD but no newborns with NAS or OE. The hospitals with only newborns all had <10 newborns with NAS per hospital.
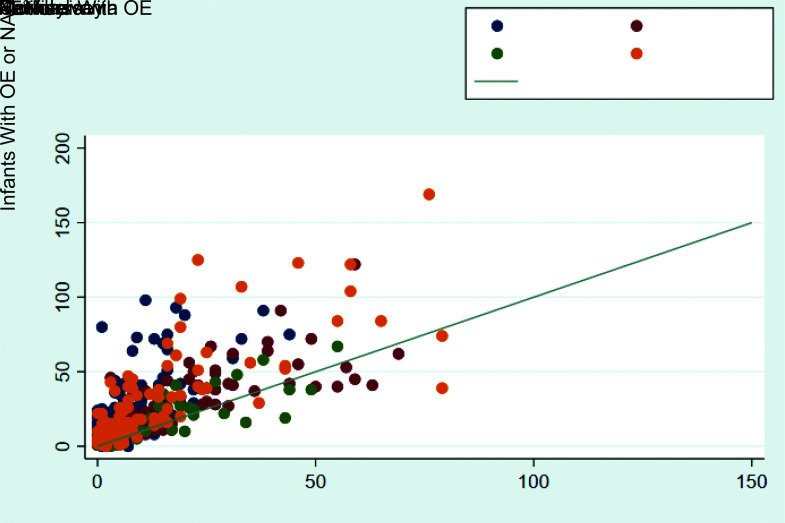
In Fig 1, we depict the concordance of frequencies of mothers and newborns per hospital. It reveals a tightly clustered group of hospitals with <∼50 mothers of newborns and newborns. The general trend is toward more newborns than mothers (ie, observations above the diagonal line of equivalence). Most hospitals had <50 newborns and 25 mothers. Three outlier hospitals that had >150 mothers were excluded from this graph for ease of displaying clustering.
FIGURE 1.
The number of newborns with NAS or OE versus the number of mothers with OUD. The 45° line is used to indicate when the number of newborns with NAS or OE equals the number of mothers with OUD within a hospital. This scatter plot reveals that there is a general trend to have more newborns with an NAS or OE diagnosis compared with mothers with an OUD diagnosis within hospitals.
Although the frequency of mothers and newborns with opioid-related diagnoses in a hospital was strongly correlated (r = 0.81), more infants were identified than mothers in most hospitals (68.3%) (Fig 2). Specifically, the average number of newborns with NAS or OE in a hospital was 23.3, whereas the average number of mothers with OUD was 11.5 (a P value of <.001 from a paired t test). This discordance was statistically significant in all states except New Jersey. In Table 4, we provide further detail.
FIGURE 2.
The distribution across hospitals of newborns with NAS or OE versus the number of mothers with OUD.
TABLE 4.
Concordance Between and Mean Numbers of Newborns With NAS or OE and Mothers With OUD at the Hospital Level Overall and by State
| No. Hospitals | Mean (Range) Newborns With NAS or OE | Mean (Range) Mothers With OUD | Pa | Correlation Coefficient, r | P for Correlation Coefficient | |
|---|---|---|---|---|---|---|
| Overall | 474 | 23.3 (0–316) | 11.5 (0–269) | <.001 | 0.81 | <.001 |
| California | 227 | 17.8 (0–98) | 5.7 (0–44) | <.001 | 0.69 | <.001 |
| Florida | 105 | 33.5 (0–316) | 14.5 (0–118) | <.001 | 0.82 | <.001 |
| New Jersey | 49 | 16.0 (0–67) | 14.0 (0–55) | .1164 | 0.83 | <.001 |
| Pennsylvania | 93 | 28.8 (0–289) | 20.8 (0–269) | <.001 | 0.93 | <.001 |
P values are from paired t tests.
Discussion
We were interested in describing mothers with OUD and newborns with NAS or OE and examining concordance between these diagnoses within hospitals. Our motivation stemmed from little being known about newborns with OE or concordance in opioid diagnoses between mothers and newborns in administrative data. The recognition of OUD and NAS or OE in hospitalized mothers and newborns has implications for intrapartum and postpartum treatment and outcomes. We were also interested in comparing the demographic characteristics of mothers and newborns with and without these opioid-related diagnoses, given the limited research on this topic. In this sample of hospitals that had at least 1 mother or newborn with an opioid-related diagnosis, we found that, on average, there were double the number of newborns with opioid-related diagnoses (23) than the number of mothers with these diagnoses (12). Despite this discrepancy, the frequencies of maternal and newborn diagnoses were highly correlated within hospitals (0.81). In two-thirds of the hospitals (68.3%), the frequency of newborns exceeded that of mothers by >120%. We also found that infants with OE were more likely to be Black or Hispanic than infants with NAS. Although infants with NAS were disproportionately white (81.5%, compared with 41.5% in the overall sample), infants with OE were disproportionately Black (21.8% vs 11.8% in the overall sample).
Although newborns with NAS and OE share some of the same vulnerabilities, most of the literature is only focused on newborns with NAS.2 Given that it is known that only a portion of newborns that are exposed to opioids prenatally go on to develop NAS, we hypothesized that we would find more newborns with OE than with NAS. Indeed, we found that OE (0.85%) was coded more frequently than NAS (0.47). In addition, 0.07% of newborns had both diagnoses. As noted above, in the Methods section, the prevalence of OE is likely inaccurate because of a lack of granular detail in the coding available at the time. Specifically, the available coding did not differentiate nonopioid addiction,12 and our exclusion of the diagnostic code for exposure to maternal medications may have also impacted the prevalence in a minor way.
We also hypothesized that the number of mothers with OUD and newborns with NAS or OE would be roughly concordant. We found that two-thirds (68.3%) of hospitals had more newborns with NAS or OE than mothers with OUD (ie, newborns exceeded mothers’ frequency by 120%). This suggests that women with prenatal OEs are not adequately identified. The basis for the lack of diagnosis of women with prenatal OE may be a lack of screening, lack of disclosure of opioid use, or lack of documentation by providers. It is important that universal verbal screening be conducted consistently, applied equitably, and documented.17 Providers’ screening decisions may be biased by their assumptions about mothers’ potential opioid use.18 Women may not feel safe disclosing prenatal opioid use because of a legitimate distrust of the health care, social, and legal systems.19–21 Providers may be reluctant to document mothers’ prenatal opioid use, given potential repercussions. The result of not identifying these mothers, however, is that their needs are left unmet.
Only ∼1 in 8 hospitals had a close match of newborns and mothers, which we defined as 80% to 120% of newborns relative to mothers. One-tenth of hospitals diagnosed newborns, but no mothers, with opioid-related diagnoses. Few hospitals had more mothers with OUD than newborns with NAS or OE (7.2%) or only mothers with OUD (1.3%). Hospitals with only mothers with OUD or only newborns with NAS or OE were exclusively in hospitals with 0 (for hospitals with mothers only) to 10 newborns with NAS. With this finding challenges are suggested with recognizing and coding among hospitals that see newborns and mothers with opioid-related diagnoses infrequently.
Similar to work by Goyal et al13 in Massachusetts, we found that hospitals tend to have more newborns with NAS or OE than mothers with OUD. The implications of the existing literature and our work are clear: we need to improve diagnoses of OUD in mothers. In addition, there is a need for greater specificity in the ICD codes used to diagnose newborns with OE. Greater detail has been facilitated by the 2018 ICD-10 coding changes.12 Despite improvements in coding since 2018, it is likely that imperfect coding persists because of factors such as state variation and provider coding practices.12,13
More mothers with OUD and newborns with NAS were white, were on Medicaid, and received hospital care in Pennsylvania than mothers and newborns without opioid-related diagnoses. More newborns with NAS (81.5%) were white, compared with newborns with OE (51.2%). More newborns with OE were Black or rural than the newborns with NAS or newborns overall. It is interesting to note the racial differences between newborns with NAS and OE in light of the fact that the most commonly used scoring system to diagnose NAS, the Finnegan Neonatal Abstinence Scoring System, is known to have poor interrater reliability and is subjective.22 There is strong evidence that providers inappropriately treat Black adults and children as if they have higher pain tolerance. Black people are less likely to receive adequate pain management as a result.23,24 There is the possibility this same phenomenon is at work here. Notably, in a recent study on racial differences in newborns with NAS, researchers reported that Black newborns “required” less pharmacologic therapy for withdrawal.25 What the study actually revealed was that Black newborns received less pharmacologic therapy, not that they required less. Our findings lead us to be concerned that Black newborns who may meet criteria for NAS are not receiving adequate attention.
The nature of discharge data and coding is imperfect; however, we used published algorithms to identify mothers, newborns, and those with opioid-related disorders.9,14–16 We also cross-walked these algorithms from ICD-9 to ICD-10, making them available for future research. Our work highlights that there are limitations with NAS or OE coding. For instance, the specific ICD code for newborn affected by newborn affected by maternal use of opioids (P04.14) did not become available until 2018.12 Despite the limitations of medical coding, we still suspect, on the basis of our findings and reports from other research, that newborns exposed to opioids prenatally are undercoded.2,12 The variation in prevalence rates because of a lack of granularity in ICD codes may impact states’ quality improvement as well as prevention and treatment programs. Future work with newer data could yield more precise estimates of newborns with OE, including more insight into the prenatal exposures included in this diagnosis. An inherent limitation of our work is that we cannot match mothers with newborns because of the lack of a linking identifier in our patient data sets. Our ICD-10 code for OE is not specific to opioid use, highlighting a larger problem in the medical coding of OE. We had data from 4 geographically diverse and populous states. Although our findings are not generalizable to the United States, having 4 states in our data is a strength because many previous studies have been focused on single states. Additionally, the perinatal opioid epidemic is a significant issue in rural communities, and our data may not be representative of those communities.
Conclusions
There is evidence of misalignment in diagnostic coding of OUD in mothers and prenatal OE in newborns. Many more newborns receive opioid-related diagnoses than mothers do. Equitable, consistent verbal screening and documentation could better support the needs of women who are presently not being diagnosed with OE. More specificity in diagnostic codes for types of prenatal exposure to opioids and other substances would lead to improved public health efforts and support better research. We found that more newborns diagnosed with OE were Black or Hispanic than those diagnosed with NAS, suggesting racial bias in diagnoses and care.
Acknowledgment
We acknowledge Morgan Peele for her contributions to data management and analysis.
Footnotes
Dr Clark and Ms French conceptualized and designed the study, coordinated data analysis, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Lorch conceptualized and designed the study and reviewed and revised the manuscript; Ms O’Rourke reviewed and revised the manuscript; Ms Rosenbaum made substantial contributions to analysis and interpretation of data and revised it critically for important intellectual content; Dr Lake conceptualized and designed the study, supervised data analysis, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Clark’s postdoctoral fellowship and Ms French’s predoctoral fellowship are supported by funding from the National Institute of Nursing Research (grant T32NR007104). Funding for Panel Study of Effects of Changes in Nursing on Patient Outcomes was provided by the National Institute of Nursing Research (grant R01NR014855; principal investigator: Aiken). The current study was also supported by funding from the Leonard Davis Institute of Health Economics titled “Disparities in Neonatal Abstinence Syndrome Infant Outcomes and Related Nursing System Factors.” The funders did not participate in the work. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1. Reddy UM, Davis JM, Ren Z, Greene MF; Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop Invited Speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: executive summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American College of Obstetricians and Gynecologists, American Academy of Pediatrics, Society for Maternal-Fetal Medicine, Centers for Disease Control and Prevention, and the March of Dimes Foundation. Obstet Gynecol. 2017;130(1):10–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics. 2015;135(5):842–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Substance Abuse and Mental Health Services Administration. Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018 [Google Scholar]
- 4. Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134(2). Available at: www.pediatrics.org/cgi/content/full/134/2/e547 [DOI] [PubMed] [Google Scholar]
- 5. Milliren CE, Gupta M, Graham DA, Melvin P, Jorina M, Ozonoff A. Hospital variation in neonatal abstinence syndrome incidence, treatment modalities, resource use, and costs across pediatric hospitals in the United States, 2013 to 2016. Hosp Pediatr. 2018;8(1):15–20 [DOI] [PubMed] [Google Scholar]
- 6. Patrick SW, Kaplan HC, Passarella M, Davis MM, Lorch SA. Variation in treatment of neonatal abstinence syndrome in US children’s hospitals, 2004-2011. J Perinatol. 2014;34(11):867–872 [DOI] [PubMed] [Google Scholar]
- 7. Patrick SW, Burke JF, Biel TJ, Auger KA, Goyal NK, Cooper WO. Risk of hospital readmission among infants with neonatal abstinence syndrome. Hosp Pediatr. 2015;5(10):513–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012 [published correction appears in J Perinatol. 2015;35(8):667]. J Perinatol. 2015;35(8):650–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934–1940 [DOI] [PubMed] [Google Scholar]
- 10. Wachman EM, Grossman M, Schiff DM, et al. Quality improvement initiative to improve inpatient outcomes for neonatal abstinence syndrome. J Perinatol. 2018;38(8):1114–1122 [DOI] [PubMed] [Google Scholar]
- 11. American College of Obstetricians and Gynecologists. Substance Use: Opioid Use Disorder, Alcohol Use Disorder, Tobacco Use. Washington, DC: American College of Obstetricians and Gynecologists; 2018 [Google Scholar]
- 12. Ernst KD, Makkar A. The opioid-exposed neonate: a review of the Oklahoma experience. J Okla State Med Assoc. 2018;111(8):768–774 [PMC free article] [PubMed] [Google Scholar]
- 13. Goyal S, Saunders KC, Moore CS, et al. Identification of substance-exposed newborns and neonatal abstinence syndrome using ICD-10-CM - 15 hospitals, Massachusetts, 2017. MMWR Morb Mortal Wkly Rep. 2020;69(29):951–955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469–477 [DOI] [PubMed] [Google Scholar]
- 15. Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization - United States, 1999-2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121(6):1158–1165 [DOI] [PubMed] [Google Scholar]
- 17. Terplan M, Minkoff H. Neonatal abstinence syndrome and ethical approaches to the identification of pregnant women who use drugs. Obstet Gynecol. 2017;129(1):164–167 [DOI] [PubMed] [Google Scholar]
- 18. Santoro TN, Santoro JD. Racial bias in the US opioid epidemic: a review of the history of systemic bias and implications for care. Cureus. 2018;10(12):e3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sobel L, O’Rourke-Suchoff D, Remis K, Sia M, Saia K, Bell SL. A qualitative study of pregnancy and birth experience for women with opioid use disorder and a history of sexual trauma. Obstet Gynecol. 2018;131:25S [Google Scholar]
- 20. Paris R, Herriott AL, Maru M, Hacking SE, Sommer AR. Secrecy versus disclosure: women with substance use disorders share experiences in help seeking during pregnancy. Matern Child Health J. 2020;24(11):1396–1403 [DOI] [PubMed] [Google Scholar]
- 21. Angelotta C, Weiss CJ, Angelotta JW, Friedman RA. A moral or medical problem? The relationship between legal penalties and treatment practices for opioid use disorders in pregnant women. Womens Health Issues. 2016;26(6):595–601 [DOI] [PubMed] [Google Scholar]
- 22. Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8(1):1–6 [DOI] [PubMed] [Google Scholar]
- 23. Lawrence AE, Deans KJ, Chisolm DJ, Wrona SK, Minneci PC, Cooper JN. Racial disparities in receipt of postoperative opioids after pediatric cholecystectomy. J Surg Res. 2020;245:309–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parikh A, Gopalakrishnan M, Azeem A, Booth A, El-Metwally D. Racial association and pharmacotherapy in neonatal opioid withdrawal syndrome. J Perinatol. 2019;39(10):1370–1376 [DOI] [PubMed] [Google Scholar]