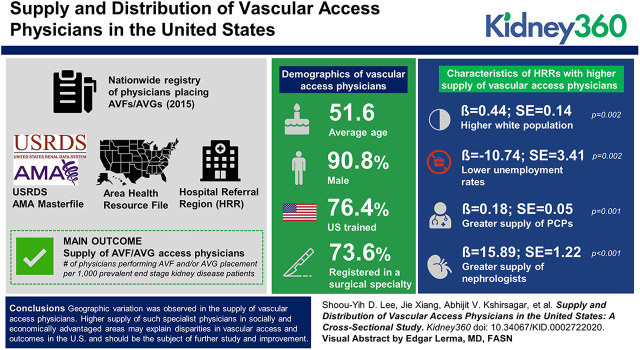
Visual Abstract
Keywords: dialysis, arteriovenous fistula, arteriovenous graft, demography, distribution, health care sector, health resources, kidney failure, chronic, physicians, primary care, referral and consultation, registries, renal dialysis, supply, vascular access
Abstract
Background
Because functioning permanent vascular access (arteriovenous fistula [AVF] or arteriovenous graft [AVG]) is crucial for optimizing patient outcomes for those on hemodialysis, the supply of physicians placing vascular access is key. We investigated whether area-level demographic and healthcare market attributes were associated with the distribution and supply of AVF/AVG access physicians in the United States.
Methods
A nationwide registry of physicians placing AVFs/AVGs in 2015 was created using data from the United States Renal Data System and the American Physician Association’s Physician Masterfile. We linked the registry information to the Area Health Resource File to assess the supply of AVF/AVG access physicians and their professional attributes by hospital referral region (HRR). Bivariate analysis and Poisson regression were performed to examine the relationship between AVF/AVG access physician supply and demographic, socioeconomic, and health resource conditions of HRRs. The setting included all 50 states. The main outcome was supply of AVF/AVG access physicians, defined as the number of physicians performing AVF and/or AVG placement per 1000 prevalent patients with ESKD.
Results
The majority of vascular access physicians were aged 45–64 (average age, 51.6), male (91%), trained in the United States (76%), and registered in a surgical specialty (74%). The supply of physicians varied substantially across HRRs. The supply was higher in HRRs with a higher percentage white population (β=0.44; SEM=0.14; P=0.002), lower unemployment rates (β=−10.74; SEM=3.41; P=0.002), and greater supply of primary care physicians (β=0.18; SEM=0.05; P=0.001) and nephrologists (β=15.89; SEM=1.22; P<0.001).
Conclusions
Geographic variation was observed in the supply of vascular access physicians. Higher supply of such specialist physicians in socially and economically advantaged areas may explain disparities in vascular access and outcomes in the United States and should be the subject of further study and improvement.
Introduction
Vascular access is a lifeline to the health and well being for patients receiving chronic hemodialysis; it is also one of the most challenging and expensive aspects of hemodialysis care (1,2). The Medicare fee-for-service program spent an estimated $2.8 billion for services related to dialysis vascular access, half of which was dedicated to inpatient vascular access procedures or complications (3). In 2004, the Centers for Medicare and Medicaid Services (CMS) established the Fistula First Breakthrough Initiative (FFBI) in the wake of initial evidence on the durability, low rates of infection and thrombosis, and low patient mortality of arteriovenous fistulas (AVFs) (4–6). The FFBI set a goal of optimizing vascular access that prioritized AVFs over arteriovenous grafts (AVGs) and central venous catheters (7,8). Although there has been demonstrated improvement in fistula frequency since FFBI implementation, newer research reveals similar patency outcomes between AVFs and AVGs in the United States (9–12).
When providers and patients discuss vascular access options, currently the choice of fistula or graft relies heavily on patient-level factors such as age, race, and vessel caliber. Despite careful considerations of these factors, >30% of fistulas have primary failure, and >60% need interventions before use (13). Potential explanations for the poor primary and secondary outcomes of AVFs and AVGs have continued to focus on patient factors that are often unmodifiable. An important but understudied factor in the choice and success of vascular access is the physician who creates the fistula or graft. Earlier studies have examined the role of surgeons in vascular access outcomes. A single-site German study found the surgeon performing the procedure was the strongest predictor of AVF failure in the early 1990s (14). O’Hare and colleagues (15) found that Veterans Health Administration surgeons’ practice patterns in 2000–2001 were associated with type of vascular access use. Using data from 12 countries in the Dialysis and Practice Patterns Study, Saran et al. (16) showed surgical training was key to fistula placement and survival, consistent with Goodkin and colleagues’ (17) 2010 review that vascular access surgery performed by surgeons who had placed a greater number of AVFs during their training was associated with higher odds of AVF placements and a reduced risk of AVF failure.
Although this heterogenous group of studies suggests that physicians who create vascular access may be an important driver of vascular access utilization and outcomes, no study has systematically examined the supply, location, and types of physicians creating vascular access across the United States. We sought to demonstrate the feasibility of developing a nationwide registry using existing data sources. In this paper, we described the methodology toward developing such a registry and examined the geographic distribution and characteristics of physicians placing permanent vascular access—specifically, AVFs and AVGs. Furthermore, we investigated area-level socioeconomic status and market attributes in relation to the distribution of AVF/AVG access physicians (i.e., physicians who performed AVF and/or AVG placement). Lastly, we examined whether the distribution of AVF/AVG access physicians was related to the supply of primary care physicians and nephrologists in the local area.
Materials and Methods
To test the feasibility of creating a nationwide registry of physicians who performed AVF and AVG placements, we conducted a cross-sectional observational study based on patient-level 2015 Medicare claims data. We then matched this claims-based registry to the American Physician Association (AMA) Physician Masterfile and Area Health Resource File to identify vascular access physicians’ demographic, specialty, training and certification attributes, practice locations, and area attributes of their practice locations. Variables were aggregated to the hospital referral region (HRR) level. HRRs are a common measure of healthcare markets; their boundaries are based on actual patient utilization, reflecting the geographic extent of healthcare markets for tertiary care (18). They are appropriate for studies of ESKD services because patients with ESKD receive a significant amount of specialized nondialysis care in tertiary care settings (19).
Data Sources
The primary source of data was the United States Renal Data System (USRDS), which is the national repository of data and trends on all patients with ESKD and providers. Patient information came from the Medical Evidence Report (CMS Form 2728), which ESKD providers are required to complete any time a patient begins or re-enters dialysis treatment or kidney transplantation services. Medicare claims data included inpatient, outpatient, and physician/supplier claims and were used to identify physicians who performed vascular access procedures. Data from these files were merged to construct a comprehensive baseline patient record and aggregated to the HRR level for covariate adjustment.
We used the AMA Physician Masterfile to ascertain professional and practice attributes of physicians performing AVF and/or AVG placement procedures. The AMA Physician Masterfile contains demographic, medical training, certification, and specialty information on >1,168,000 physicians (>98% coverage), members and nonmembers, residents, and medical students in the United States.
We used information in the Area Health Resources File (AHRF) to measure demographic and socioeconomic conditions of HRRs. AHRF contains a comprehensive array of county-level population statistics, including population counts, healthcare resources, personal income, and land area statistics. We converted county-level demographic and socioeconomic statistics from AHRF to the zip code level based on land area weighting, and then aggregated zip code–level information to HRRs. Zip code assignments to HRRs were obtained from publicly available geographic boundary files from the Dartmouth Atlas of Health Care.
Participants
The primary subjects of the study were physicians who performed AVF and/or AVG placement procedures in 2015. To construct a registry of such physicians over a single year, we first identified all patients with pre-ESKD or ESKD in the USRDS data who had evidence of a Medicare claim for AVF or AVG placement during January 1 through December 31, 2015 (N=151,428) (Figure 1). Current Procedural Terminology codes 36800, 36810, 36818, 36819, 36820, 36821, and 35825 were used to identify claims of AVF placement. Current Procedural Terminology code 36830 was used to identify claims of AVG placement. We excluded claims (1) without a national provider identifier (NPI), a unique identifier of the physician who performed the placement procedure (N=2); (2) related to care for patients who were 20 and younger and patients who did not have Medicare as the primary insurer in 2015 (N=71,154); and (3) that were duplicative (N=29,740). From the remaining 50,532 claims, we identified a total of 5464 unique clinicians who performed at least one AVF or AVG access placement procedure in 2015. After excluding clinicians practicing in the territories of the United States (N=97), we removed another 615 clinicians (11%) because their NPIs did not have a match in the AMA Physician Masterfile. In total, we identified 4752 vascular access physicians in 2015.
Figure 1.
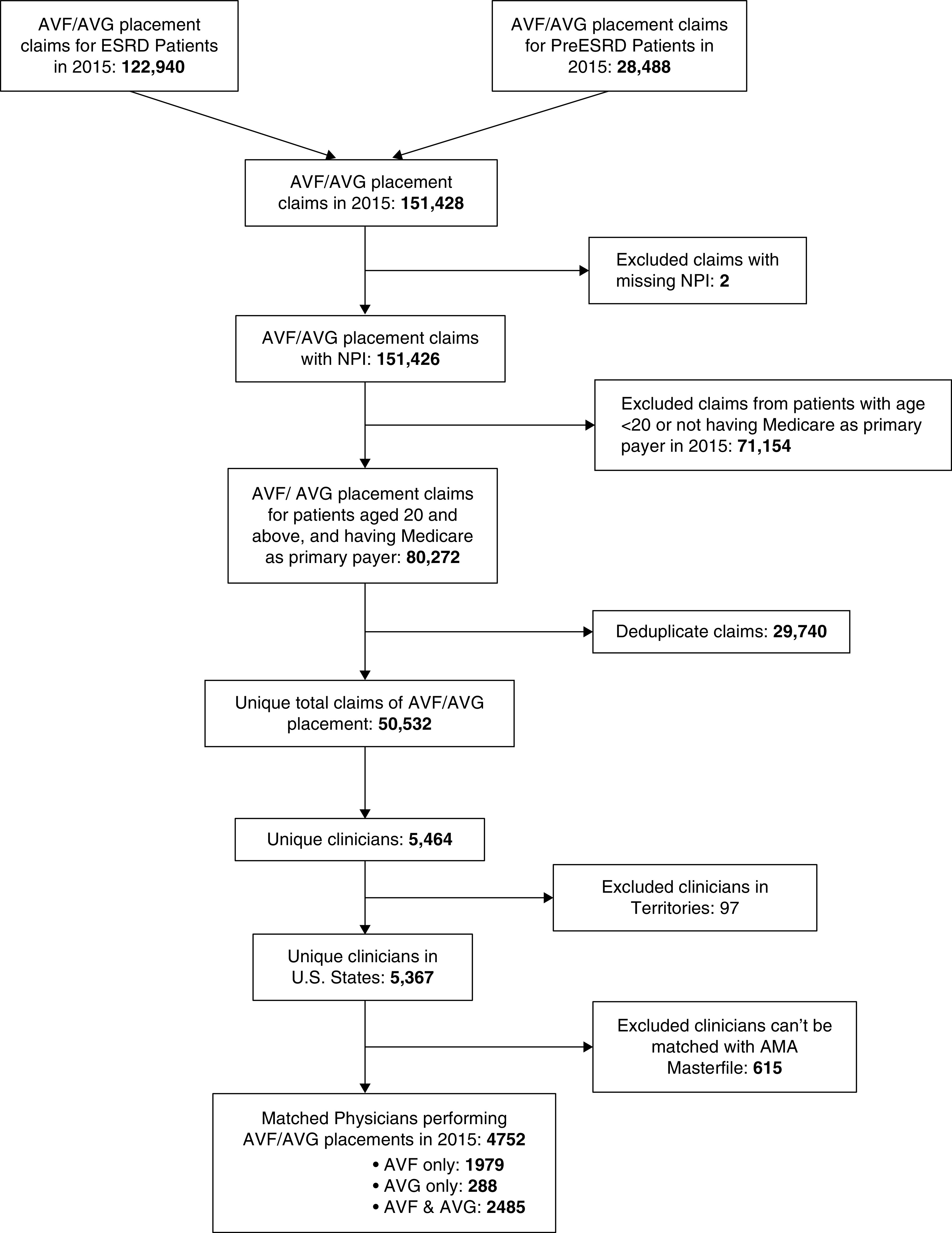
Flowchart of the processes for identifying 4752 physicians performing arteriovenous fistulas (AVF)/arteriovenous graft (AVG) placements in 2015. AMA, American Physician Association; NPI, national provider identifier.
Measurement
The main outcome in this study was the supply of AVF/AVG access physicians, defined as the number of physicians performing AVF and/or AVG placement per 1000 prevalent patients with ESKD, across HRRs in 2015.
Linked NPI and AMA Physician Masterfile data were used to obtain the following physician characteristics: age, sex, zip code, MD versus DO degree, indicator of United States versus international medical graduates, year of graduation (before 1980, 1980–1989, 1990–2000, after 2000), years in practice (≤10, 11–20, 21–30, 31–40, 41–50, >50), and primary specialty (vascular surgery, thoracic/cardiac surgery, transplant surgery, urology, general surgery, other surgery, urology, radiology, nephrology, others).
We characterized the demographic and socioeconomic conditions of physicians’ HRRs in 2015 as percentage white population, percentage urban population, percentage adults with a high school diploma population, percentage population in poverty, unemployment rate, and per capita income (average income earned per person in the HRR). We also calculated the supply of primary care physicians (number of primary care physicians per 1000 patients with ESKD) and nephrologists (number of nephrologists per 1000 patients with ESKD) in each HRR based on physician counts in the AMA Physician Masterfile.
Statistical Analyses
Descriptive statistics (counts, mean, 95% confidence interval, and proportions) were used to examine the dispersion and distribution of AVF/AVG access physician supply and professional characteristics (e.g., specialty, year of practice). Choropleth maps were generated to display the regional (HRR) supply of AVF/AVG access physicians across the United States. We then used multivariate analysis using Poisson regression in generalized linear models to examine the relationship between AVF/AVG access physician supply (response variable) and demographic/socioeconomic conditions of HRRs.
All analyses used SAS statistical software (version 9.4; Statistical Analysis Institute Inc.) and R (version 3.5.0; R Foundation for Statistical Computing). Statistical significance was defined as P<0.05.
Results
Supply, Geographic Distribution, and Characteristics of AVF/AVG Access Physicians
A total of 4752 unique physicians performed 50,532 Medicare claims for vascular access procedures in 2015. Of those physicians, 1979 performed AVF placement only, 288 performed AVG placement only, and 2485 performed both AVFs and AVGs. On average, there were 20.1 AVF/AVG access physicians in HRRs per 1000 prevalent patients with ESKD. There was substantial variation across HRRs (Figure 2), ranging from 2.6 in Wichita Falls, Texas (HRR, 276) to 68.3 in Hinsdale, Illinois (HRR, 86). The supply of vascular access physicians appeared to be higher in the New England, Mideast, Great Lakes regions, as well as the area between the Midwest/Plains and Mountain West regions. By contrast, many HRRs in the South (Georgia, Alabama, Mississippi, and Louisiana), Appalachia, and Midwest/Plains regions had low supply of vascular access physicians.
Figure 2.
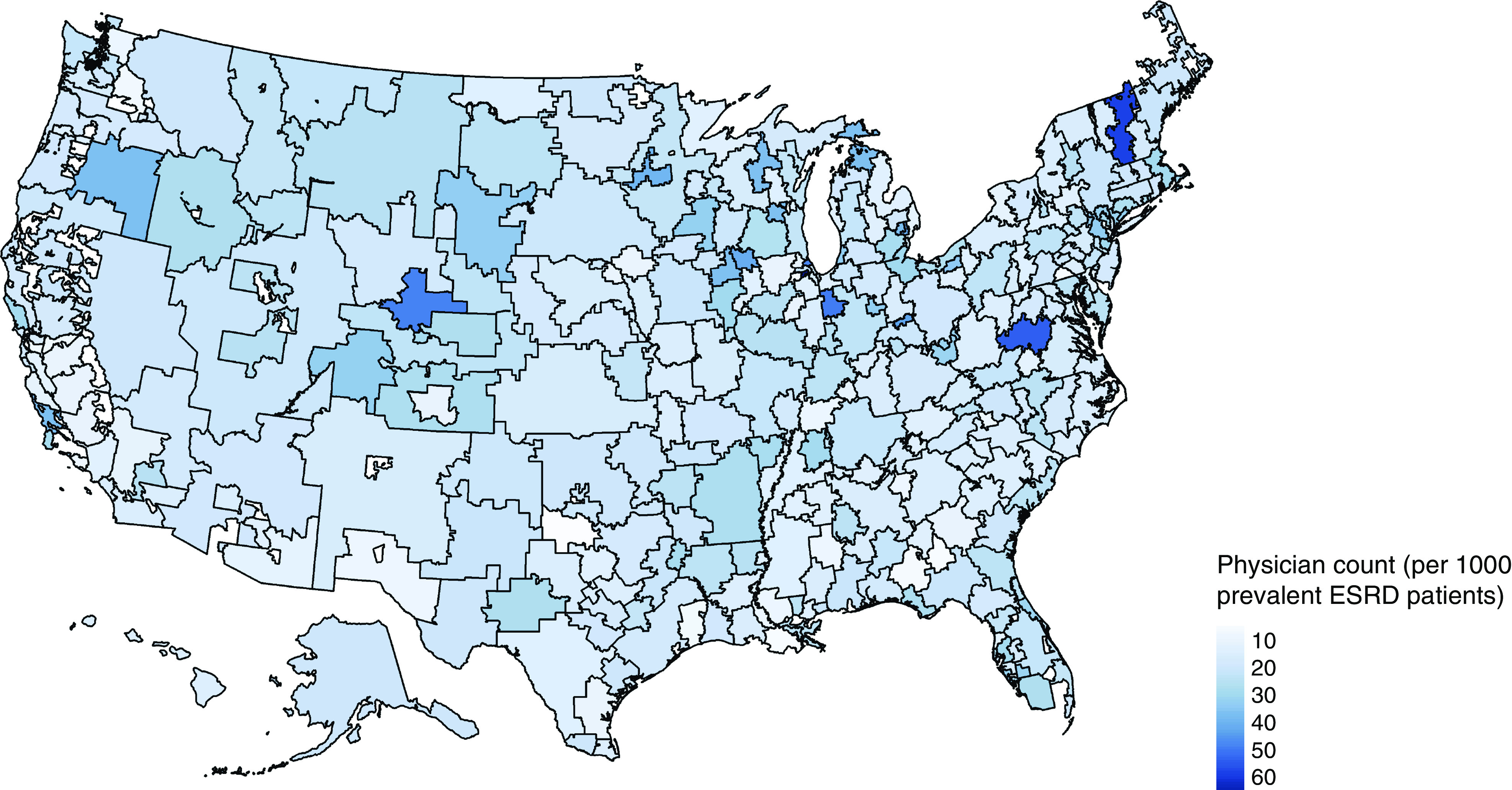
Substantial variation in the supply of AVF/AVG access physicians across hospital referral regions.
The average age of AVF/AVG access physicians was 51.6 years, with the majority in the 45–64 age group (58%) (Table 1). An overwhelming majority of the physicians were male (91%), had an MD degree (96%), and received their medical school education in the United States (76%). The distribution of physicians by medical school graduation year was skewed toward recent decades, consistent with the distribution by number of years in practice, where nearly a third of physicians (32%) had <10 years of practice experience with an average length of practice of 17.4 years. In terms of medical specialty, 45% of physicians identified vascular surgery as their primary specialty, 39% were in other surgical specialties (thoracic/cardiac, transplant, general, urology, and others), and the remainder were in nephrology (3%), radiology (0.1%), and other medical specialties (14%).
Table 1.
Characteristics of physicians performing AVF/AVG placements
| Characteristics | All (N=4752) | AVF Only (N=1979) | AVG Only (N=288) | AVF and AVG (N=2485) | |
| Age, yr (SD) a | 51.6 (51.2, 51.9) | 50.9 (50.4, 51.4) | 51.4 (49.9, 52.8) | 52.1 (51.7, 52.5) | |
| 18–44 (%) | 30 | 33 | 32 | 27 | |
| 45–64 (%) | 58 | 56 | 52 | 60 | |
| 64–74 (%) | 11 | 10 | 14 | 12 | |
| 75+ (%) | 2 | 2 | 2 | 1 | |
| Sex (%) | |||||
| Female | 9 | 11 | 16 | 7 | |
| Male | 91 | 89 | 84 | 93 | |
| Degree flag (%) | |||||
| MD | 96 | 96 | 94 | 96 | |
| DO | 4 | 4 | 6 | 4 | |
| United States trained (%) | |||||
| Yes | 76 | 73 | 73 | 79 | |
| No (IMG) | 24 | 27 | 27 | 21 | |
| Year of graduation (%) | |||||
| Before 1980 | 19 | 17 | 22 | 20 | |
| 1980–1989 | 27 | 27 | 25 | 28 | |
| 1990–2000 | 29 | 29 | 24 | 29 | |
| After 2000 | 25 | 27 | 30 | 23 | |
| Years in practice, yr (SD) | 17.4 (17.1, 17.8) | 16.7 (16.2, 17.2) | 17.3 (15.8, 18.8) | 18.1 (17.6, 18.5) | |
| ≤10 yr (%) | 32 | 35 | 35 | 30 | |
| 11–20 yr (%) | 28 | 29 | 22 | 28 | |
| 21–30 yr (%) | 21 | 20 | 20 | 22 | |
| 31–40 yr (%) | 14 | 12 | 15 | 15 | |
| 41–50 yr (%) | 2 | 2 | 2 | 2 | |
| >50 yr (%) | 0.1 | 0.1 | 0.4 | 0.1 | |
| Specialty group (%) | |||||
| Vascular surgery | 45 | 31 | 39 | 57 | |
| General surgery | 29 | 29 | 23 | 30 | |
| Thoracic/Cardiac surgery | 8 | 7 | 9 | 8 | |
| Transplant surgery | 1 | 0.6 | 0.4 | 2 | |
| Urology | 0.1 | 0.2 | 0.0 | 0 | |
| Other surgeryb | 0.9 | 1 | 2 | 0.4 | |
| Nephrology | 3 | 5 | 7 | 0.3 | |
| Radiology | 0.1 | 0.2 | 0 | 0 | |
| Other medical specialtiesc | 14 | 26 | 20 | 3 | |
Data given are percentages/mean (SD). AVF, arteriovenous fistula; AVG, arteriovenous graft; IMG, International Medical Graduates (physicians who obtained their medical school diplomas outside the United States).
Age as of January 1, 2015.
Other surgery includes the following specialty categories in the American Physician Association file: critical care surgery, traumatic surgery, abdominal surgery, colon and rectal surgery, pediatric surgery, neurologic surgery, orthopedic surgery, pediatric cardiothoracic surgery, and plastic surgery.
Other specialty primarily includes pulmonary critical care medicine, internal medicine, critical care medicine, anesthesiology, cardiovascular disease, family practice, and vascular and interventional radiology.
A substantial portion of vascular access physicians performed only one type of vascular access placement, rather than both. We suspected this practice pattern may be associated with personal and professional attributes. Thus, for comparison, Table 1 also reports the personal and professional attributes of physicians who placed AVFs only (N=1979), AVGs only (N=288), and both AVFs and AVGs (N=2485). There are several notable differences: In comparison to physicians who placed both AVFs and AVGs, physicians who performed only one type of vascular access placement were more likely to be female (11% [AVF only] and 16% [AVG only] versus 7% [AVF and AVG]), to receive their medical school education outside the United States (27% [AVF only] and 27% [AVG only] versus 21% [AVF and AVG]), to be in nephrology (5% [AVF only] and 7% [AVG only] versus 0.3% [AVF and AVG]) and other medical specialties (26% [AVF only] and 20% [AVG only] versus 3% [AVF and AVG]), and less likely to have vascular surgery as their primary specialty (31% [AVF only] and 39% [AVG only] versus 57% [AVF and AVG]).
The practice volume of vascular access physician varied substantially. The large majority of physicians (N=3494; 74%) performed less than ten procedures in 2015. Of the 1258 physicians performing more than ten procedures in 2015, 1197 performed both AVFs and AVGs, 61 performed AVFs only, and none performing AVGs only. In general, high-volume physicians were older, more likely to be male, graduated from the medical school in earlier years, and had more years of practice than physicians who performed less than ten vascular access procedures in 2015. With few exceptions (2%), all of them had a surgical background and 68% were vascular surgeons (detailed results available from the corresponding author).
Analysis of the Vascular Access Physician Supply
As a framework for assessing factors that were associated with the distribution of AVF/AVG access physicians, we drew on location theory. The theory assumes generally that physicians are economic agents acting in their own self-interest and that their choice of practice location reflects personal preferences for income as well as environmental and professional considerations (20–22). Based on these assumptions, we expected there would be a greater supply of AVF/AVG access physicians in HRRs with a higher degree of urbanicity, higher percentage white population, higher percentage population with a high school diploma, and better economic conditions, because these HRR conditions meant there would be a higher demand for vascular access placement and the living conditions would be more favorable to physicians. Similarly, AVF/AVG access physicians may be more likely to practice in HRRs with a higher supply of primary care physicians and nephrologists, because there would be more patient referrals and better medical support for vascular access services.
Figure 3 displays the distribution of AVF/AVG access physician supply by HRR characteristics. As expected, the supply of AVG/AVG access physicians was significantly higher in HRRs with a higher percentage white population (r=0.22, P<0.001), a higher percentage population with high school diploma (r=0.25, P<0.001), and a higher level of per capita income (r=0.15, P=0.01); the supply was significantly lower in HRRs with a higher percentage population in poverty (r=−0.24, P<0.001) and a higher unemployment rate (r=−0.23, P<0.001). Consistent with our expectation, the supply of AVF/AVG access physicians was also positively associated with the supply of primary care physicians (r=0.36, P<0.001) and nephrologists (r=0.53, P<0.001) in HRRs. There was no difference in AVF/AVG access physician supply by the level of urbanicity (r=−0.03, P=0.63).
Figure 3.
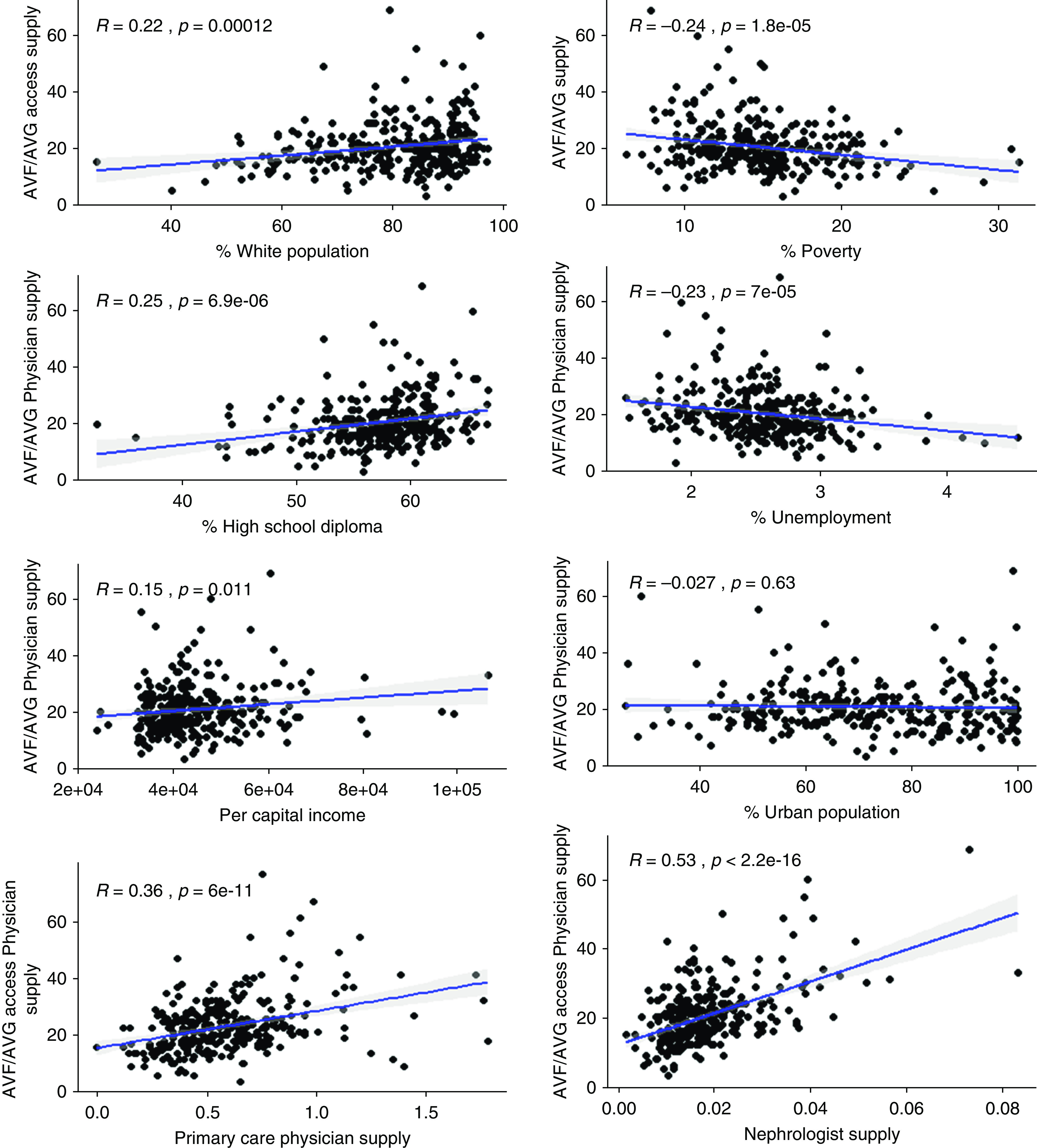
Supply AVF/AVG access physician associated with population and health resource characteristics of hospital referral regions. “Primary care physician supply” and “nephrologist supply” represent the counts of physicians per 1000 prevalent patients with ESKD.
In adjusted analysis (Table 2), percentage white population (β=0.44; SEM=0.14; P=0.002), supply of primary care physicians (β=0.18; SEM=0.05; P=0.001), and supply of nephrologists (β=15.89; SEM=1.22; P<0.001) were significantly and positively associated with the distribution of vascular access physicians across HRRs. On the other hand, unemployment rates of HRRs (β=−10.74; SEM=3.41; P=0.002) were significantly and negatively associated with the supply of vascular access physicians.
Table 2.
Poisson regression analysis
| Measure | Coefficient | SEM | P Value |
| Intercept | 2.24 | 0.34 | <0.001 |
| White population | 0.44 | 0.14 | 0.002 |
| High school diploma | 0.59 | 0.37 | 0.11 |
| Urban population | −0.04 | 0.10 | 0.65 |
| Per capita income | −1.36 × 10−06 | 1.86 × 10−06 | 0.49 |
| Unemployment rate | −10.74 | 3.41 | 0.002 |
| Primary care physician supplya | 0.18 | 0.05 | 0.001 |
| Nephrologist supplya | 15.89 | 1.22 | <0.001 |
Supply represents the count of vascular access performing physicians per 1000 prevalent patients with ESKD.
We also compared the location differences between AVF only, AVG only, and AVF and AVG physicians and between high (more than ten procedures) and low-volume (ten or fewer procedures) physicians (detailed results are available from the corresponding author). In general, physicians performing AVF only and AVG only were more likely to be located in HRRs with a higher percentage white population, better economic conditions (i.e., lower poverty, lower unemployment rates, and higher per capita income), and higher supply of primary care physicians and nephrologists. In multivariate analysis, the only factor significantly associated with the geographic distribution of high-volume (more than ten) physicians, who were more likely to perform both AVFs and AVGs, was the supply of nephrologists, suggesting their practice location was determined primarily by referral sources.
Discussion
In this nationally representative study, we developed a novel registry of 4752 vascular access physicians by systematically matching Medicare claims data on patients with ESKD and pre-ESKD with the AMA Physician Masterfile for the year 2015. We found the majority of physicians creating fistulas and grafts were vascular surgeons or general surgeons. Although the majority of these physicians created both types of access, surprisingly 31% created only AVFs and 6% created only AVGs. A minority of vascular access physicians performed more than ten placements in 2015 and they were almost exclusively surgeons. Furthermore, the registry demonstrated marked variation in the supply of vascular access physicians across the country. Additionally, area-level characteristics were associated with the supply of vascular access physicians.
Building on the methodology in Shahinian et al. (23), our study is one of the first to detail the demographic and specialty profiles of vascular access physicians across the 50 states of the United States. It is interesting to note that the vast majority of vascular access physicians are male, likely reflecting the general sex distribution of physicians in surgical specialties. Similar to previous studies using United States and international data (16,17), we found wide variation in specialty among vascular access physicians. Physicians in surgical specialties—primarily those in vascular surgery (45%) and general surgery (29%)—constituted the vast majority (84%) of physicians who performed AVF and/or AVG placement procedures in 2015. In contrast, a Dialysis Outcomes and Practice Patterns Study showed that, in 2003, 61% of vascular access surgeries in the United States were conducted by vascular surgeons and 31% by general surgeons (16). The different findings suggest a possibility that there may be increasing involvement of medical specialists in vascular access creation over time, and a shift in the professional background of vascular access physicians from surgical to medical specialties.
Our findings reveal a stark contrast in the role of medical specialists in vascular access creation. According to our analysis, nephrologists constituted only 3% of vascular access physicians in the United States. This rate was lower than those observed in other countries. Approximately 30% of vascular access surgeries in Japan were conducted by nephrologists; in Italy, nephrologists were the primary vascular access operators in 85% of hemodialysis facilities (16). Such practice pattern differences may be due to medical training and credential issues across countries and may continue to evolve with the introduction of the percutaneous AVF creation technique. Moreover, the medical specialties represented in our study were considerably diverse—including pulmonary critical care medicine, internal medicine, critical care medicine, anesthesiology, cardiovascular disease, family practice, and vascular and interventional radiology—and a small percentage of those physicians claims surgery as their second specialty. This level of diversity appears unique in the United States and has important implications regarding the quality of vascular access placement in consideration of a small number of placement procedures they tended to perform as well as three prior research findings. First, research indicated that adequate training in vascular access creation predicted vascular access patency in patients on hemodialysis (16,17). Second, a surgeon’s prior volume of AVF placement was shown to be associated with successful AVF maturation (23). Third, United States surgeons had less vascular access training than surgeons in other countries (17). Medical specialists, conceivably, may receive even less training on vascular access placement, they may not focus a significant portion of their practice on the procedures, and the volume they performed tended to be small. If so, a sizable number of the vascular access procedures performed in the United States may not produce reliable and sustainable access for patients on hemodialysis. To verify this concern, future research linking the professional background and specialty of vascular access physicians to quality and outcomes of vascular access procedures is needed.
Surprisingly, we found nearly half of vascular access physicians performed only AVF or AVG placement in 2015. The reasons for this specialization are not clear, and cannot be plausibly attributable to the measured physician characteristics such as sex, country of medical graduation, and others. In a comparison of high- and low-volume vascular access physicians, we found high-volume physicians were more likely to perform both AVFs and AVGs and were more likely to be in areas with a lower percentage white population and poorer economic conditions. These findings suggest the degree of specialization may be related to local practice patterns or reimbursement. Future research is needed to further investigate and corroborate the findings.
Our analysis showed substantial geographic variation in physician supply. Comparatively, HRRs in the South (particularly, Georgia, Alabama, Mississippi, and Louisiana), Appalachia, and Midwest/Plains regions were underserved by physicians who performed vascular access procedures for patients on hemodialysis. Besides such regional differences, the distribution of vascular access physicians was associated with demographic, economic, and health resource conditions of HRRs in a manner that is consistent with the prediction of the location theory (20–22). Specifically, we found vascular access physicians were more likely to locate in HRRs with a higher percentage white population and less likely to be in HRRs with higher unemployment rates.
These findings are interesting in light of the persistent geographic and demographic variation in fistula prevalence despite the overall success of the FFBI initiative. Geographic variation has been observed across the 18 ESRD Networks. Patients on hemodialysis in New England have the highest rates of initiation with AVFs, whereas patients in the Southeast have the lowest rates (24,25). At the county level, variation in incident and baseline prevalent AVF rates was associated with the concentration of poverty in a dialysis center’s county (26). Moreover, racial and ethnic variation has been observed in AVF utilization. Using CMS Medical Evidence Report data, Arce et al. (27) found that Hispanics were less likely to use AVFs for first outpatient hemodialysis compared with non-Hispanics. In a different study, Zarkowsky et al. (28) showed that black and Hispanic patients were less likely to initiate hemodialysis with an AVF than white patients, despite being younger and having fewer comorbidities, and that the differences were not explained by factors related to healthcare such as medical insurance status and predialysis nephrology care. In consideration of all this previous evidence, the findings of our study suggest the supply of vascular access physicians may be a crucial and previously overlooked factor. Specifically, the tendency of vascular access physicians to practice in socially and economically advantaged areas may explain the persistent evidence that minority patients on dialysis have a lower frequency of functional AVFs and AVGs than white patients. If this is confirmed by further research that directly links the supply of vascular access physicians to prevalence and success of AVG and AVG placement, improvement in the medical school curriculum and training of vascular access as well as changes in reimbursement policy would be needed to increase the supply of vascular access physicians in underserved areas and disadvantaged patient populations.
We also found that vascular access physicians, particularly those who performed a high number of procedures, tended to practice in HRRs where there was an abundant supply of primary care physicians and nephrologists. This finding suggests that solving maldistribution of vascular access physicians needs to consider the overall distribution of medical resources, as indicated by supply of primary care physicians and nephrologists.
Our study was limited by its cross-sectional design. We demonstrated the feasibility of reliably identifying vascular access physicians, their professional attributes and practice information using ESKD and pre-ESKD claims data and existing secondary data sets. Future work to expand the registry using longitudinal data to track the supply of vascular access surgeons and specialists would enable further important examination of the relationships between supply, professional background, skill, and practice settings of those physicians to vascular access use and outcomes in patients on hemodialysis. It should be noted that we did not capture all permanent vascular access procedures in 2015—particularly, those that were performed on patients age <65—due to Medicare’s eligibility and coverage rules for new ESKD program enrollees and transition to Medicare primary payer coverage. This may not be a major limitation and was unlikely to affect the construction of the physician registry because very few vascular access physicians, if any, perform AVF procedures exclusively on non-Medicare patients.
The overall supply, professional background, and skill of vascular access surgeons are arguably some of the most important, yet understudied, factors of vascular access quality. Identifying the drivers of the observed findings may help to develop policy changes to reimbursement or other incentives that would increase the supply of vascular access surgeons and specialists in underserved areas with disadvantaged patient populations. Furthermore, periodic updates to the registry would enable longitudinal monitoring of the supply of vascular access physicians and track the changes in physician attributes and practices. The information would contribute to improving vascular access care and inform the needs for modifying medical training and physician workforce policy to enhance the supply of vascular access physicians, particularly in underserved areas.
Disclosures
All authors have nothing to disclose.
Funding
Funding for the study was provided by National Institute of Diabetes and Digestive and Kidney Diseases grant R21DK117446.
Acknowledgments
The USRDS, the AMA, and the Health Resources and Services Administration of the US Department of Health and Human Services supplied the data for the study.
The analysis, interpretation, and reporting of data used in the study are the responsibility of the authors and in no way reflect the official policy and stand of the funding agency, the US Government, or any other institutions. Dr. Virginia Wang reports grants from the National Institutes of Health and grants from the Department of Veterans Affairs, outside the submitted work.
Author Contributions
S. Lee provided supervision; S. Lee, A. Kshirsagar, and V. Wang conceptualized the study and were responsible for funding acquisition and investigation; S. Lee, A. Kshirsagar, R. Saran, V. Wang, and J. Xiang were responsible for methodology and validation; S. Lee and R. Saran were responsible for resources; S. Lee and R. Saran were responsible for data curation; S. Lee, D. Steffick, and J. Xiang were responsible for project administration; S. Lee, V. Wang, and J. Xiang reviewed and edited the manuscript; D. Steffick, V. Wang, and J. Xiang were responsible for formal analysis; V. Wang and J. Xiang were responsible for visualization; and all authors wrote the original draft and approved the final version of the manuscript.
References
- 1.Nassar GM, Ayus JC: Infectious complications of the hemodialysis access. Kidney Int 60: 1–13, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Fokou M, Teyang A, Ashuntantang G, Kaze F, Eyenga VC, Chichom Mefire A, Angwafo F 3rd: Complications of arteriovenous fistula for hemodialysis: An 8-year study. Ann Vasc Surg 26: 680–684, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Thamer M, Lee TC, Wasse H, Glickman MH, Qian J, Gottlieb D, Toner S, Pflederer TA: Medicare costs associated with arteriovenous fistulas among US hemodialysis patients. Am J Kidney Dis 72: 10–18, 2018 [DOI] [PubMed] [Google Scholar]
- 4.Tokars JI, Light P, Anderson J, Miller ER, Parrish J, Armistead N, Jarvis WR, Gehr T: A prospective study of vascular access infections at seven outpatient hemodialysis centers. Am J Kidney Dis 37: 1232–1240, 2001 [DOI] [PubMed] [Google Scholar]
- 5.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK: Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 60: 1443–1451, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Pisoni RL, Albert JM, Elder SE, et al.: Lower mortality risk associated with native arteriovenous fistula (AVF) vs graft (AVG) use in patient and facility-level analyses: Results from the DOPPS. J Am Soc Nephrol 16: 259A, 2005 [Google Scholar]
- 7.Lee Timmy: Fistula First Initiative: Historical Impact on Vascular Access Practice Patterns and Influence on Future Vascular Access Care. Cardiovasc Eng Technol 8[3]: 244–254, 2017. 10.1007/s13239-017-0319-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lok CE: Fistula first initiative: Advantages and pitfalls. Clin J Am Soc Nephrol 2: 1043–1053, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Xue H, Lacson E Jr., Wang W, Curhan GC, Brunelli SM: Choice of vascular access among incident hemodialysis patients: A decision and cost-utility analysis. Clin J Am Soc Nephrol 5: 2289–2296, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sgroi MD, Patel MS, Wilson SE, Jennings WC, Blebea J, Huber TS: The optimal initial choice for permanent arteriovenous hemodialysis access. J Vasc Surg 58: 539–548, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Jadlowiec CC, Mannion EM, Lavallee M, Brown MG: Hemodialysis access in the elderly: Outcomes among patients older than seventy. Ann Vasc Surg 31: 77–84, 2016 [DOI] [PubMed] [Google Scholar]
- 12.Greenberg J, Jayarajan S, Reddy S, Schmieder FA, Roberts AB, van Bemmelen PS, Lee J, Choi ET: Long-term outcomes of fistula first initiative in an urban university hospital—is it still relevant? Vasc Endovascular Surg 51: 125–130, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wish JB, Moe SM: Moving beyond the assumed: Improving fistula success rates. J Am Soc Nephrol 28: 2827–2829, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prischl FC, Kirchgatterer A, Brandstätter E, Wallner M, Baldinger C, Roithinger FX, Kramar R: Parameters of prognostic relevance to the patency of vascular access in hemodialysis patients. J Am Soc Nephrol 6: 1613–1618, 1995 [DOI] [PubMed] [Google Scholar]
- 15.Pearce WH, Parker MA, Feinglass J, Ujiki M, Manheim LM: The importance of surgeon volume and training in outcomes for vascular surgical procedures. J Vasc Surg 29: 768–776; discussion 777–778, 1999 [DOI] [PubMed] [Google Scholar]
- 16.Saran R, Elder SJ, Goodkin DA, Akiba T, Ethier J, Rayner HC, Saito A, Young EW, Gillespie BW, Merion RM, Pisoni RL: Enhanced training in vascular access creation predicts arteriovenous fistula placement and patency in hemodialysis patients: Results from the Dialysis Outcomes and Practice Patterns Study. Ann Surg 247: 885–891, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Goodkin DA, Pisoni RL, Locatelli F, Port FK, Saran R: Hemodialysis vascular access training and practices are key to improved access outcomes. Am J Kidney Dis 56: 1032–1042, 2010 [DOI] [PubMed] [Google Scholar]
- 18.Wennberg J, Wennberg D: The Dartmouth Atlas of Health Care in Michigan, Detroit, MI, Trustees of Dartmouth College, Blue Cross Blue Shield of Michigan, 2000 [Google Scholar]
- 19.Jalbert JJ, Gerhard-Herman MD, Nguyen LL, Jaff MR, Kumamaru H, Williams LA, Chen CY, Liu J, Seeger JD, Rothman AT, Schneider P, Brott TG, Tsai TT, Aronow HD, Johnston JA, Setoguchi S: Relationship between physician and hospital procedure volume and mortality after carotid artery stenting among Medicare beneficiaries. Circ Cardiovasc Qual Outcomes 8[Suppl 3]: S81–S89, 2015 [DOI] [PubMed] [Google Scholar]
- 20.Newhouse JP: Geographic access to physician services. Annu Rev Public Health 11: 207–230, 1990 [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal MB, Zaslavsky A, Newhouse JP: The geographic distribution of physicians revisited. Health Serv Res 40: 1931–1952, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang V, Lee SY, Patel UD, Maciejewski ML, Ricketts TC: Longitudinal analysis of market factors associated with provision of peritoneal dialysis services. Med Care Res Rev 68: 537–558, 2011 [DOI] [PubMed] [Google Scholar]
- 23.Shahinian VB, Zhang X, Tilea AM, He K, Schaubel DE, Wu W, Pisoni R, Robinson B, Saran R, Woodside KJ: Surgeon characteristics and dialysis vascular access outcomes in the United States: A retrospective cohort study. Am J Kidney Dis 75: 158–166, 2020 [DOI] [PubMed] [Google Scholar]
- 24.Lynch JR, Wasse H, Armistead NC, McClellan WM: Achieving the goal of the Fistula First breakthrough initiative for prevalent maintenance hemodialysis patients. Am J Kidney Dis 57: 78–89, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zarkowsky DS, Hicks CW, Arhuidese I, Canner JK, Obeid T, Qazi U, Schneider E, Abularrage CJ, Black JH 3rd, Freischlag JA, Malas MB: Quality improvement targets for regional variation in surgical end-stage renal disease care. JAMA Surg 150: 764–770, 2015 [DOI] [PubMed] [Google Scholar]
- 26.McClellan WM, Wasse H, McClellan AC, Holt J, Krisher J, Waller LA: Geographic concentration of poverty and arteriovenous fistula use among ESRD patients. J Am Soc Nephrol 21: 1776–1782, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arce CM, Mitani AA, Goldstein BA, Winkelmayer WC: Hispanic ethnicity and vascular access use in patients initiating hemodialysis in the United States. Clin J Am Soc Nephrol 7: 289–296, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zarkowsky DS, Arhuidese IJ, Hicks CW, Canner JK, Qazi U, Obeid T, Schneider E, Abularrage CJ, Freischlag JA, Malas MB: Racial/ethnic disparities associated with initial hemodialysis access. JAMA Surg 150: 529–536, 2015 [DOI] [PubMed] [Google Scholar]