Abstract
The increase in multidisciplinary research in the field of aging has many benefits and should be further applied to better understand and possibly reverse the stalled increase in life expectancy as well as growing social inequalities in life expectancy in many countries.
Recent years have seen increasing multidisciplinary interaction in research in the field of aging. This cross-fertilization has been useful across the broad spectrum of aging research and should continue to grow. In the spirit of suggesting where disciplines can usefully come together, I want to suggest two current trends in human populations that could benefit from multidisciplinary input to understand and potentially redirect the recent stall in increases in life expectancy in many countries in the global north and the widening of social inequalities in life expectancy.
Recent trends in life expectancy
For the last couple of decades, many researchers studying the biology of aging have been talking about extending life expectancy and delaying aging1,2. However, for the last decade, those of us who study mortality trends in human populations have become alarmed at the change in the trajectory of increase in life expectancy that has occurred in a number of countries (Fig. 1). In most Organisation for Economic Co-operation and Development (OECD) countries, the once relatively robust and regular annual increases in life expectancy have been reduced, or even eliminated3. Figure 1 shows that in 20 out of 23 OECD countries, the increase in life expectancy over the most recent six years was lower than in the six years previous; in Iceland and the USA, there were even decreases across the most recent six years. This was an unexpected turn, as most demographers and people studying aging expected a continued pattern of yearly increase in life expectancy. The idea that life expectancy could decrease in developed countries was considered unlikely, even though Russia had provided a recent example4.
Fig. 1 |. Gains in life expectancy over four six-year periods, 1990–1996, 1997–2003, 2004–2010 and 2011–2017.
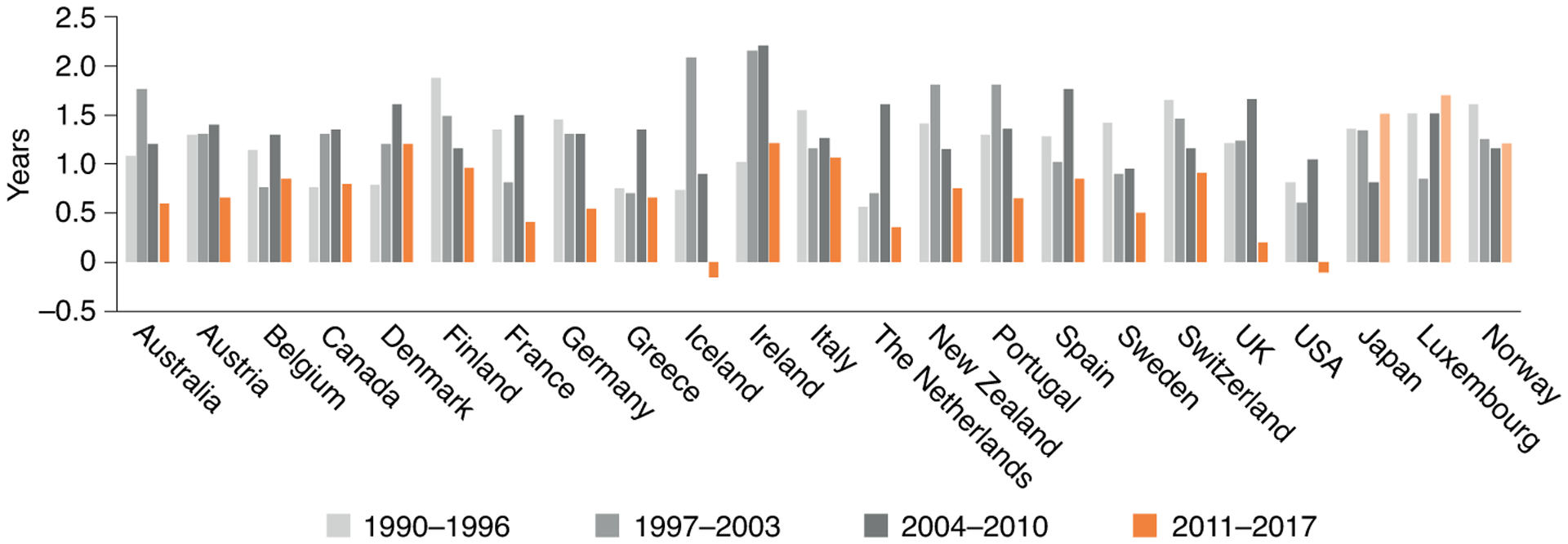
Dark orange bars indicate lower increases in life expectancy in 2011–2017 than 2004–2010, and light orange bars indicate greater recent increases in life expectancy. Relatively low gains in years of life expectancy from 2011–2017 can be seen in 20 out of 23 OECD countries compared to 2004–2010.
Life expectancy trends may be adversely affected by a number of recent trends in mortality rates. Some are specific to the USA, such as increasing maternal mortality and deaths from drug overdoses, which do not affect trends in other countries to the same extent. However, the primary reason for the decrease in the improvement in life expectancy across countries is the slowdown in the decline of mortality rates from cardiovascular disease5. Declining cardiovascular mortality was the cause of death that fueled much of the decline in mortality and increase in life expectancy at older ages, which began in the late 1960s and has continued until recently. By 2014, death rates in the USA from cardiovascular disease had tumbled to about two-thirds of what they were in 1969 (ref.6). The role of declining cardiovascular disease in promoting increasing life expectancy now appears to be ending.
There are numerous potential explanations for the decreased rate of reduction in cardiovascular mortality, including reduced importance of existing medical interventions, behavioral changes and changed cohort life cycle experiences. Medicine has allowed us to intervene in the process of aging and progression of cardiovascular disease by promoting the widespread use of antihypertensive and cholesterol-lowering medications. The use of these drugs has become so widespread that high blood pressure and high cholesterol are becoming relatively rare among older people in many countries, and it will be hard to continue to gain substantially from further treating these risks. Thus, this is one factor that is now a reduced force for decreasing cardiovascular mortality and improvement in life expectancy.
Some behavioral factors are also contributing to this trend in life expectancy, either by becoming less important as influences in the case of smoking, or working against improvement in the case of obesity. The decline in smoking has been an important influence on both declining mortality from cardiovascular disease and improving life expectancy. This influence is now waning in some countries, as smoking has been reduced to lower levels and/or is no longer declining. Obesity is a rising risk factor contributing to slowing the decrease in cardiovascular death rates. More recent entrants into older ages have had increasing exposure to obesity, beginning at earlier ages and lasting longer, and at higher levels of obesity.
Another potential factor in the slowdown in cardiovascular death rate decline is the historical change in the potential role of improvement across successive birth cohorts in preventing and treating early-life infectious diseases. Early-life infection is linked to worse health and mortality from chronic conditions at older ages7. Not having to fight infectious diseases throughout life resulted in progressively better organ development and reduced damage. This led to less expenditure of resources on repair and lower levels of inflammation among those born later. Evidence of reduced population levels of inflammation over the last 200 years is provided by the recent report of a long-term drop in body temperature of approximately 1 °C (ref.8). Persons in high-income countries now reaching older age groups when mortality is high have never lived without vaccinations to prevent many infectious diseases and antibiotic treatment for bacterial conditions. This has resulted in a gradual reduction for successive cohorts in lifetime spent with infectious conditions, which has been a force for increasing life expectancy. Thus, in countries with high life expectancy, another powerful force leading to mortality decline has largely played out.
Certainly, the COVID-19 pandemic has changed the outlook for life expectancy worldwide. In the year 2020, many countries will likely see declines in life expectancy of up to a year resulting from COVID-19 infection. There is a substantial body of research that links early exposure to the 1918 flu epidemic to greater later-life mortality and morbidity for decades9. Survivors of the 2020 pandemic that were infected may continue to have adverse physical effects that will cause earlier morbidity and mortality than they would have otherwise experienced. Even those not infected may experience adverse effects from changes in life circumstances related to the pandemic. Tracking the impact of COVID-19 on population health in the near and distant future should be an important focus of future research. This will also create a unique opportunity to study the integration of social and biological factors integrated into policy environments.
Inequality in life expectancy
One of the most important issues of our time is the growing social and economic inequality in life expectancy. While social inequality in life expectancy is virtually universal, the extent varies across countries. For example, social inequality is greater in the USA without universal access to medical care and weaker government programs providing social support. In many countries, those with lower incomes and less education are leading increasingly shorter lives relative to the wealthier and more educated, as increases in life expectancy are larger among higher socioeconomic groups and smaller among lower socioeconomic groups10.
Much social science work on risk factors for individual aging is rooted in the idea that health outcomes linked to aging are strongly socially determined by life circumstances throughout life. There is a wealth of literature linking major health outcomes at older ages to what I have called the ‘social hallmarks of aging’: low lifetime socioeconomic status, adversity in childhood and adulthood, being a member of a minority group, adverse health behaviors and adverse psychological states11. These social factors reflect underlying experiences that are linked to all the major health outcomes, a similar role to that hypothesized for the ‘biological hallmarks of aging’12. I believe we have not fully grasped the importance of social and psychological factors as determinants of trends in life expectancy, nor have we understood how these factors operate over the span of lifecycles. There is significant current work beginning to explore how biology helps us understand the way social, psychological and environmental circumstances get ‘under the skin’ to explain differences in health outcomes13. This is leading to increased understanding of how experiences, circumstances and environment at specific life stages affect the development and progression of chronic diseases and mortality. However, much more understanding is needed before this leads to targeted interventions to delay the morbidity process overall, and increased healthy life expectancy for the socially, economically and psychologically disadvantaged. These advances will be important to make clear the need to reduce inequality and the rewards for doing so.
Scientists have tended to focus on improving health and life expectancy with scientific advances akin to the revolution in antibiotics, such as delaying aging. We have not used the full complement of our multidisciplinary approaches to assess the social, psychological and health costs of being relatively poor and uneducated. Understanding the lethal consequences of inequality should clarify the importance of reducing inequality as well as ameliorating its consequences.
Opportunities for multidisciplinary research
Multidisciplinary science should better integrate the social, psychological and biological to interpret and reverse current trends in differential life expectancy. We have not yet taken full advantage of integrated multidisciplinary approaches to understanding population-level trends in life expectancy. Across the world, raising the life expectancy of those of low status to those of high status offers an opportunity for increasing life expectancy overall and improving on current trends14,15. Too much of work at the population level on life expectancy is descriptive and based on assumptions of continuing current trends. Predicting and projecting life expectancy requires knowing more about how early- and late-life health are connected, how change in risks and treatments for chronic conditions can influence trends, and how the social and biological hallmarks of aging combine to create large and growing differentials in life expectancy. The complexity introduced by changing chronic disease patterns and treatments should be part of the investigation into how population health can change with scientific advances. Work on model organisms could markedly increase understanding of the relative importance of a variety of influences on population trends and differentials in life and health expectancy.
Footnotes
Competing interests
The author declares no competing interests.
References
- 1.Partridge L Philos. T. Roy. Soc. B 365, 147–154 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaupel JW Nature 464, 536–542 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho JY & Hendi AS Brit. Med. J 362, k2562 (2018); erratum 362, k3622 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shkolnikov V, McKee M & Leon DA Lancet 357, 917–921 (2001). [DOI] [PubMed] [Google Scholar]
- 5.Mehta NK, Abrams LR & Myrskylä M Proc. Natl Acad. Sci. USA 117, 6998–7000 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weir HK et al. Prev. Chronic Dis 13, 160211 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beltrán-Sánchez H, Crimmins EM & Finch CJ Dev. Orig. Health Dis 3, 380–386 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Protsiv M, Ley C, Lankester J, Hastie T & Parsonnet J eLife 9, e49555 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Easterlin MC, Crimmins EM & Finch CE J. Dev. Orig. Health Dis 10, 1–5 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leon DA Int. J. Epidemiol 40, 271–277 (2011). [DOI] [PubMed] [Google Scholar]
- 11.Crimmins EM Ageing Res. Rev 63, 101136 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López-Otín C, Blasco MA, Partridge L, Serrano M & Kroemer G Cell 153, 1194–1217 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moffitt TE Ageing Res. Rev 63, 01146 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aburto JM, Wensink M, van Raalte A & Lindahl-Jacobsen R BMC Public Health 18, 831 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackenbach JP, Karanikolos M & McKee M Lancet 381, 1125–1134 (2013). [DOI] [PubMed] [Google Scholar]


