Abstract
Introduction:
Dentin hypersensitivity (DH) adversely affects quality of life by impairing the ability to eat and drink certain foods, therefore, should be addressed promptly with a contingency plan that includes initial treatment with a noninvasive prophylactic home care approach, followed by in-office treatment if desired result is not achieved.
Aim:
The purpose of this study was to evaluate the effectiveness of four different pastes containing 5% NovaMin (Sensodyne Repair and Protect®), Propolis (Phytoshield Propolis®), 5% potassium nitrate (Sensodyne®), and 8% arginine (Colgate Sensitive Pro Relief®) based toothpastes in the treatment of DH.
Materials and Methods:
One hundred dentin slices were cut from the crown section of molars. Etching with 37% orthophosphoric acid was done to open the tubules. Scanning electron microscope (SEM) study was done to ensure that the tubules are opened. The dentin specimens were divided into four groups: Group 1 –5% NovaMin, Group 2 – Propolis, Group 3 – 5% potassium nitrate, and Group 4 – 8% arginine. Samples were brushed for 2 min twice daily with a soft toothbrush for 15 days and were stored in distilled water. The samples were rinsed under running water to remove the toothpaste. The SEM was performed to check the obliteration of tubules.
Results:
5% NovaMin group showed more completely occluded dentinal tubules when compared to other groups. The differences among all the groups were statistically significant (P ≤ 0.05).
Conclusion:
In the present study, all materials, NovaMin, Propolis, potassium nitrate, and arginine, were effective in occluding dentinal tubules but NovaMin appeared most proficient in occluding tubules, followed by arginine, potassium nitrate, and Propolis. Topical NovaMin is an upcoming agent demonstrating desensitization and remineralization properties.
Keywords: Dentin hypersensitivity, scanning electron microscope, toothpaste
INTRODUCTION
Dentin hypersensitivity (DH) accounts for a widespread issue and is a mystery in diagnosis. The uneasiness that arises as a result of DH is said to enormously influence the quality of life (QoL) of the patients. Review of literature reveals the prevalence of DH anywhere from 4.8% to 62.3%.[1] The terms dentin sensitivity (DS) and DH have been used interchangeably to describe the same clinical condition. Compared with the typical sharp pain of short duration seen in DH, true hypersensitivity due to pulpal inflammation presents with severe lingering pain, the features of irreversible pulpitis.[2] Exposure of dentin due to erosion of the enamel by abrasion, erosion, attrition, and abfraction or cementum at the root surface from gingival recession are the two most common pathways that lead to dentin exposure and DH.[3]
Several products have been developed for DH treatment, but the effects are often temporary, and DH relapses as soon as the desensitizing agents are removed by the daily challenge of diet.[4]
Although there are numerous treatment modalities such as LASER, regenerative procedures (guided tissue regeneration), and 8% nano-carbonated hydroxyapatite collagen/poly (lactic-co-glycolic acid).,[1] toothpastes are still the most widely used dentifrices for delivering over-the-counter desensitizing agents. There is a vast array of agents available for desensitization containing fluoride, calcium hydroxide, strontium chloride, potassium and sodium nitrate, glutaraldehyde, etc., A product consisting of calcium sodium phosphosilicate (NovaMin, Sensodyne Repair and Protect®) has been introduced recently. It claims to reduce the sensitivity by blocking open tubules and by supplying calcium and phosphorus ions when the environment is optimum.[5,6]
The present in vitro study was conducted to evaluate the effectiveness of four different pastes containing 5% NovaMin (Sensodyne Repair and Protect®), Propolis (Phytoshield Propolis®), 5% potassium nitrate (Sensodyne®), and 8% arginine (Colgate Sensitive Pro Relief®), based toothpastes in the treatment of DH.
MATERIALS AND METHODS
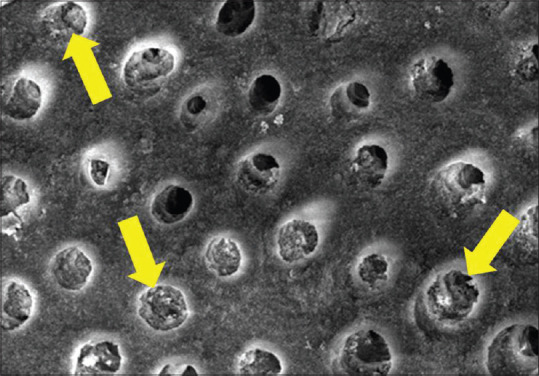
After the ethical clearance from the institutional review board, 100 extracted premolar and molar teeth were collected. The extractions were indicated either for orthodontic or periodontal conditions. Included teeth were caries free and without any erosion or abrasion. Endodontically treated teeth were excluded. Following cleaning of the teeth from debris and tissue, the teeth were sectioned to 1 mm thickness from the region below the crown and above the root canal and were stored in 10% formalin. The dentin discs were etched with 37% phosphoric acid for 20 s and rinsed with distilled water. The teeth were randomly divided in four groups: Group 1 (25 teeth) – application of NovaMin containing paste, Group 2 (25 teeth) – application of Propolis containing paste, Group 3 (25 teeth) – application of potassium nitrate containing paste, and Group 4 (25 teeth) – application of Arginine containing paste. The discs were subjected to a pretreatment scanning electron microscope (SEM) analysis [Figure 1].
Figure 1.
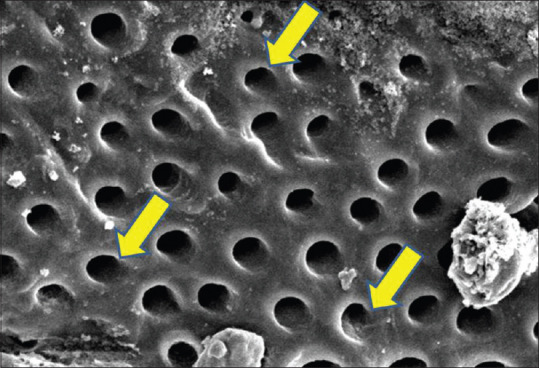
Scanning electron microscope image of dentin disc presenting open dentinal tubules
Examination (scanning electron microscope)
All the specimens of the respective groups were kept in 10% formalin solution for 48 h to fix the samples. These specimens were dehydrated in ascending concentrations of aqueous alcohol solutions which were 70%, 80%, 90%, and 100% alcohol for 10 min each. Following the dehydration process, specimens were first air dried and then kept in a desiccator jar overnight. Dried samples were mounted on SEM stubs. Specimens were then sputter coated with gold in a fine coat (JEOL 10 Nsputter JFC 1100) by a sputtering device. The mounted specimens were evaluated using model JEOL 6100 (SEM).
Samples were brushed for 2 min twice daily with a soft toothbrush with respective toothpaste for 15 days and were stored in distilled water. The samples were rinsed under running water to remove the toothpaste. The SEM study was performed. The micrographs were taken at appropriate magnification and were evaluated for patent dentinal tubules. The obtained data were tabulated and statistically analyzed used pair and unpaired t-test.
RESULTS
The mean number of occluded tubules was maximum for NovaMin, followed by arginine, potassium nitrate, and Propolis [Figure 2].
Figure 2.
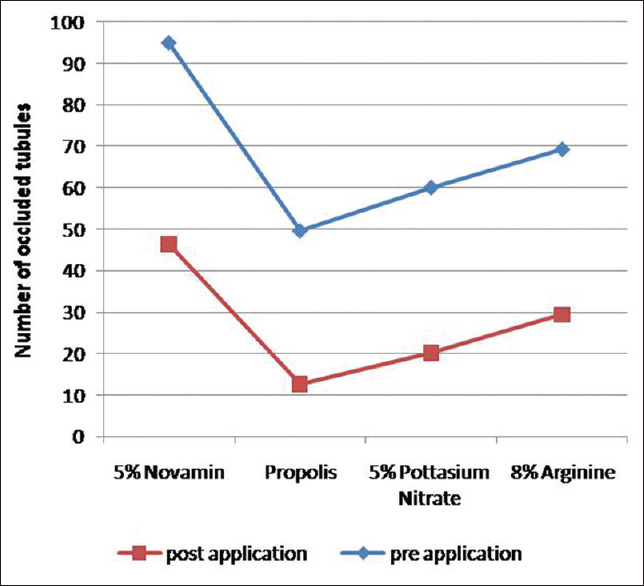
Intergroup comparison of different groups
The mean total number of tubules before application of 5% NovaMin (Group 1) was 48.40 ± 3.96, and after the application, the mean number of occluded tubules was 46.40 ± 1.76; hence, it was statistically nonsignificant. The mean value of percentage of occluded tubules was 95.8 ± 2.20 [Figure 3].
Figure 3.
Scanning electron microscope image of dentin disc following the application of 5% NovaMin sample (Group 1)
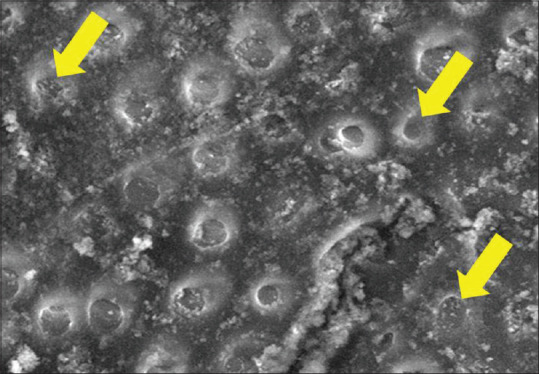
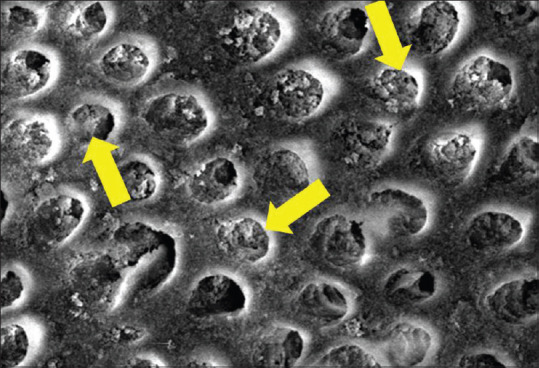
The mean total number of tubules before application of Propolis (Group 4) was 37 ± 5.63, and after the application, the mean number of occluded tubules was 12.60 ± 3.00. The mean value of the percentage of occluded tubules was 33.84 ± 11.76, which was highly significant (P = 0.02) [Figure 4].
Figure 4.
Scanning electron microscope image of dentin disc following the application of Propolis (Group 2)
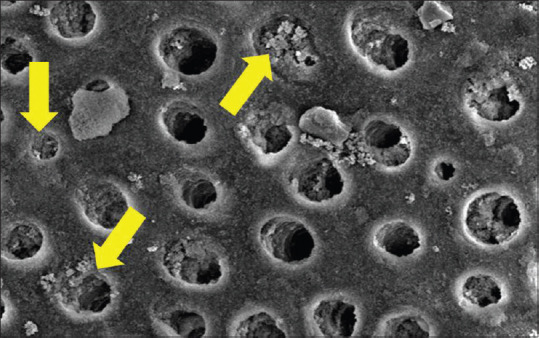
The mean total number of tubules before application of 5% potassium nitrate (Group 6) was 39.80 ± 5.63, and after the application, the mean number of occluded tubules was 20.20 ± 3.00. The mean value of percentage of occluded tubules was 51.12 ± 11.76 which was highly significant (P = 0.02) [Figure 5].
Figure 5.
Scanning electron microscope image of dentin disc following the application of 5% potassium nitrate (Group 3)
The mean total number of tubules before application of 8% arginine (Group 4) was 39.80 ± 7.19, and after the application, the number of mean occluded tubules was 29.40 ± 3.84. The mean value of percentage of occluded tubules was 73.70 ± 13.35 and was highly significant (P = 0.023) [Figure 6].
Figure 6.
Scanning electron microscope image of dentin disc following the application of 8% arginine (Group 4)
DISCUSSION
Pain being a persistent presenting feature of DH adversely affects the QoL.[7] Several theories have been proposed to explain the mechanism of DH, but the hydrodynamic theory has been widely accepted.[8] This theory states that pain can be perceived by the patient due to fluid movement in the dentinal tubules, which causes nerve ending deformation at the pulp dentin junction.[9] It is a well-known fact that the agents effective in the treatment of DH have affinity for dentin and occlude the tubules and are effective for tooth sensitivity.
The width of the dentinal tubule is significant, as the rate of fluid flow is dependent on the fourth power of the radius. With the tubule diameter being doubled, a 16-fold increase in fluid flow results. Sensitive teeth have many more tubules (about 8 times) and almost double the width at the buccal cervical area compared with nonsensitive teeth. The episodic condition of DS is resultant of the tubule patency, which is altered by smear layer formation and elimination.[10]
There is a direct correlation between DH and thickness of the tubules.[11,12,13] In in vitro study, dentin surface area, thickness, and surface characteristics can be controlled. Hydraulic conductance causing DH is higher in coronal dentin when compared with radicular dentin. A positive correlation exists between tubule density and diameter and the measured hydraulic conductance.[14]
Keeping these findings in view, this in vitro study was carried out to evaluate the tubular occlusion formed by four different desensitizing dentifrices containing 5% NovaMin, Propolis, 5% potassium nitrate, and 8% arginine.
Sensodyne Repair and Protect® contains NovaMin key constituent, which is an over-the-counter DH dentifrice. It is technically described as an inorganic amorphous calcium sodium phosphosilicate (CSP) material that was designed based on a class of materials known as bioactive glasses.[15] Silicate acts as foci for precipitation of calcium and phosphate. SEM analysis has shown that the application of bioglass causes the formation of an apatite layer which further leads to the occlusion of dentinal tubules.[3] Topical NovaMin application has significant remineralization potential along with desensitization action which is a win-win situation for the patients.[16]
Propolis, obtained from honey bees, is a nontoxic, resinous substance composed of resins, wax, essential oils, and pollen exhibiting anti-inflammatory, antimicrobial, antiparasitic, antiviral, antioxidant, anesthetic, and free-radical scavenger properties.[17] The use of Propolis to study the occlusion of dentinal tubules, as a treatment modality for DH, is scarce in the literature, making this study innovative, and the concept of a naturally derived product adds further to the innovation.[18]
Potassium possibly blocks the transmission of nerve endings by its oxidizing effect or blocking of tubules by crystallization, but the exact mechanism has not been proven.[19,20] potassium salts (potassium nitrate, potassium chloride, or potassium citrate) depolarize the nerve cells, causing them to become refractory to excitatory stimuli by diffusion along the dentinal. The cumulative effect of potassium nitrate may take several weeks for reducing DH.[20]
Arginine-containing toothpastes (arginine bicarbonate and calcium carbonate) mimic natural desensitizing processes of the saliva and can form a plug to physically block and seal the open dentinal tubules so as to minimize DH.[21] Arginine suppresses protein interactions with other molecules or surfaces exhibiting antiviral properties.[22]
Arantes et al. compared the clinical efficacy of Pro-Arginine and NovaMin toothpastes, in which they concluded that no statistical difference was observed among the two toothpastes and both can be prescribed to treat DH in adults with equivalent effectiveness up to 4 weeks.[23]
A similar study by Bansal and Mahajan comparing 1:5% NovaMin, 8% arginine, and herbal desensitizing toothpaste found that there was a significant change in the VAS scores in NovaMin when compared to arginine and herbal toothpastes. NovaMin showed a better reduction in hypersensitivity which is in accordance with our results.[24]
Results of Burwell et al. also were in accordance with our study, where he stated that a mechanically strong, mineralized layer, resistant to acid challenge was formed when exposed dentin reacted with NovaMin. There was a sustained release of calcium over time which suggested to maintain the protective effects on dentin.[25] However, a study by Hoffman et al. and Khijmatgar et al. advocated that NovaMin has nonsignificant effects on remineralizing effects on white spot lesions. Our results indicate that a toothpaste containing,[26,27] whereas Haghgoo et al. confirmed that topical NovaMin and nano-hydroxyapatite were effective on surface remineralization.[28]
Askari and Yazdani proposed that Propolis extracts were uniformly effective irrespective of their concentration and were equally efficacious to the application of single bond universal in relieving DH.[29] Kripal et al. also implied propolis varnish as a natural treatment modality for DH. It also has antimicrobial, anti-inflammatory, healing. and cariostatic properties along with stimulation of reparative dentin formation.[30]
Martins et al. concluded that strontium and potassium showed moderate effectiveness for tactile stimulus and arginine for air stimulus. The combination of potassium with SnF2 or hydroxyapatite was effective for tactile and air stimuli with moderate certainty of evidence. Among all active ingredients, calcium sodium phosphosilicate (CSP) was more effective for all three stimuli with high-to-moderate certainty. Furthermore, SnF2-based formulations seem to be more effective than regular-fluoride toothpastes to manage DH due to tactile and air stimuli with high-to-moderate certainty.[31] Another systematic review of 74 articles suggested marked long-term reduction in DH with agents such as potassium nitrate, arginine, glutaraldehyde with hydroxyethyl methacrylate (HEMA), hydroxyapatite, adhesive systems, glass ionomer cements, and LASER, whereas short-term relief (1 week) was seen by the use of glutaraldehyde with HEMA, glass ionomer cements, and laser, and intermediate DH reduction (up to 1 month) was seen in stannous fluoride, glutaraldehyde with HEMA, hydroxyapatite, glass ionomer cements, and laser groups. Moreover, in-office treatments were more efficacious for immediate DH reduction and at-home treatments are recommended for long-time effects.[32]
With the advent of newer materials, many recent studies have shown promising results. Li et al. have suggested that procyanidins, tannic acid, and naringin can effectively seal dentinal tubules, which provided a basis for clinical treatment of DH.[33] Polymers containing catechol groups exhibited modification of demineralized dentin by promoting imitating the role of charged noncollagenous proteins. The use of poly (catechols) may be encouraged for the development of a therapeutic technique for DH.[34] Mir et al. compared the effectiveness of home-use photobiomodulation toothbrush with fluoride varnish and combination of the two and observed a significant reduction in dentin pain and hypersensitivity concluding photobiomodulation toothbrush a convenient, safe, and effective method for the management of DH.[35] Mesoporous bioactive glass combined with Graphene Oxide Quantum Dot is a promising treatment modality for DH which needs to be explored on a larger study sample size.[36]
CONCLUSION
DH adversely affects QoL by impairing the ability to eat and drink certain foods therefore should be addressed promptly by clinicians with a contingency plan
Therapy should be initiated with a prophylactic home care approach, followed by in-office treatment with nerve desensitization, precipitating, or plugging agents if desired result is not achieved
In the present study, all materials, NovaMin, Propolis, potassium nitrate, and arginine, were effective in occluding dentinal tubules but NovaMin appeared more promising in occluding tubules and formation of dentin matrix-like surface layer completely after initial application followed by arginine, potassium nitrate. Propolis was least efficacious
Topical NovaMin is an upcoming agent demonstrating desensitization and remineralization properties.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Janani K, Ajitha P, Sandhya R. Improved quality of life with dentin hypersensitivity. Saudi Endod J. 2020;10:81–2. [Google Scholar]
- 2.Trowbridge HO. Mechanism of pain induction in hypersensitive teeth. In: Rowe NH, editor. Hypersensitive Dentine: Origin and Management. Ann Arbor, USA: University of Michigan; 1985. pp. 1–10. [Google Scholar]
- 3.Absi EG, Addy M, Adams D. Dentine hypersensitivity. The development and evaluation of a replica technique to study sensitive and non-sensitive cervical dentine. J Clin Periodontol. 1989;16:190–5. doi: 10.1111/j.1600-051x.1989.tb01639.x. [DOI] [PubMed] [Google Scholar]
- 4.Arantes DC, Limeira FI, Yamauti M, Moreira AN, Abreu LG, Magalhães CS. Comparison of clinical efficacy of pro-argin and novamin toothpastes in relieving dentin hypersensitivity: A systematic review and meta-analysis. Oral Health Prev Dent. 2019;17:403–12. doi: 10.3290/j.ohpd.a43272. [DOI] [PubMed] [Google Scholar]
- 5.Litkouski L. Pilot clinical & in vitro studies evaluating NovaMin in desensitizing dentifrice. J Dent Res. 1998;77:199. [Google Scholar]
- 6.Joshi S, Gowda AS, Joshi C. Comparative evaluation of NovaMin desensitizer and Gluma desensitizer on dentinal tubule occlusion: A scanning electron microscopic study. J Periodontal Implant Sci. 2013;43:269–75. doi: 10.5051/jpis.2013.43.6.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Idon PI, Sotunde OA, Ogundare TO. Beyond the relief of pain: Dentin hypersensitivity and oral health-related quality of life. Front Dent. 2019;16:325–34. doi: 10.18502/fid.v16i5.2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umberto R, Claudia R, Gaspare P, Gianluca T, Alessandro del V. Treatment of dentine hypersensitivity by diode laser: A clinical study. Int J Dent. 2012;2012:858950. doi: 10.1155/2012/858950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Augusto R, Elias B, Karol R, Joselyn N, Luis R, Mateo B, et al. Efficacy in reducing dentine hypersensitivity of arginine using a toothpaste containing 8% arginine and calcium carbonate, a mouthwash containing 0.8% arginine, pyrophosphate and PVM/MAcopolymer and a toothbrush compared to potassium and negative control regimens: An eight-week randomized clinical trial'. J Dent. 2015;4:42–9. doi: 10.1016/j.jdent.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 10.West NX. Dentine hypersensitivity: Preventive and therapeutic approaches to treatment. Periodontol 2000. 2008;48:31–41. doi: 10.1111/j.1600-0757.2008.00262.x. [DOI] [PubMed] [Google Scholar]
- 11.Miglani S, Aggarwal V, Ahuja B. Dentin hypersensitivity: Recent trends in management. J Conserv Dent. 2010;13:218–24. doi: 10.4103/0972-0707.73385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cummins D. Recent advances in dentin hypersensitivity: Clinically proven treatments for instant and lasting sensitivity relief. Am J Dent. 2010;23(Spec No A):3A–13. [PubMed] [Google Scholar]
- 13.Davari A, Ataei E, Assarzadeh H. Dentin hypersensitivity: Etiology, diagnosis and treatment; a literature review. J Dent (Shiraz) 2013;14:136–45. [PMC free article] [PubMed] [Google Scholar]
- 14.Ling TY, Gillam DG, Barber PM, Mordan NJ, Critchell J. An investigation of potential desensitizing agents in the dentine disc model: A scanning electron microscopy study. J Oral Rehabil. 1997;24:191–203. [PubMed] [Google Scholar]
- 15.Närhi MV. The characteristics of intradental sensory units and their responses to stimulation. J Dent Res. 1985;64(Spec No):564–71. doi: 10.1177/002203458506400411. [DOI] [PubMed] [Google Scholar]
- 16.Altan H, Göztaş Z, Kahraman K, Kuş M, Tosun G. Inhibition effects of different toothpastes on demineralisation of incipient enamel lesions. Oral Health Prev Dent. 2019;17:179–85. doi: 10.3290/j.ohpd.a42202. [DOI] [PubMed] [Google Scholar]
- 17.Przybyłek I, Karpiński TM. Antibacterial properties of propolis. Molecules. 2019;24:2047. doi: 10.3390/molecules24112047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santiago KB, Conti BJ, Cardoso EO, Golim MA, Sforcin JM. Immunomodulatory/anti-inflammatory effects of a propolis-containing mouthwash on human monocytes. Pathog Dis. 2016;74:081. doi: 10.1093/femspd/ftw081. [DOI] [PubMed] [Google Scholar]
- 19.James JM, Puranik MP, Sowmya KR. Dentinal tubule occluding effect of potassium nitrate in varied forms, frequencies and duration: An in vitro SEM analysis. J Clin Diagn Res. 2017;11:ZC06–8. doi: 10.7860/JCDR/2017/26442.10340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bartold PM. Dentinal hypersensitivity: A review. Aust Dent J. 2006;51:212–76. [PubMed] [Google Scholar]
- 21.Petrou I, Heu R, Stranick M, Lavender S, Zaidel L, Cummins D, et al. A breakthrough therapy for dentin hypersensitivity: How dental products containing 8% arginine and calcium carbonate work to deliver effective relief of sensitive teeth. J Clin Dent. 2009;20:23–31. [PubMed] [Google Scholar]
- 22.Ohtake S, Arakawa T, Koyama AH. Arginine as a synergistic virucidal agent. Molecules. 2010;15:1408–24. doi: 10.3390/molecules15031408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arantes DC, Limeira FI, Yamauti M, Moreira AN, Abreu LG, Magalhães CS. Comparison of clinical efficacy of pro-argin and NovaMin toothpastes in relieving dentin hypersensitivity: A systematic review and meta-analysis. Oral Health Prev Dent. 2019;17:403–12. doi: 10.3290/j.ohpd.a43272. [DOI] [PubMed] [Google Scholar]
- 24.Bansal D, Mahajan M. Comparative evaluation of effectiveness of three desensitizing toothpastes for relief in the dentinal hypersensitivity. Contemp Clin Dent. 2017;8:195–99. doi: 10.4103/ccd.ccd_135_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burwell A, Jennings D, Muscle D, Greenspan DC. NovaMin and dentin hypersensitivity-in vitro evidence of efficacy. J Clin Dent. 2010;21:66–71. [PubMed] [Google Scholar]
- 26.Khijmatgar S, Reddy U, John S, Badavannavar AN, D Souza T. Is there evidence for NovaMin application in remineralization. A Systematic review? J Oral Biol Craniofac Res. 2020;10:87–92. doi: 10.1016/j.jobcr.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffman DA, Clark AE, Rody WJ, Jr, McGorray SP, Wheeler TT. A prospective randomized clinical trial into the capacity of a toothpaste containing NovaMin to prevent white spot lesions and gingivitis during orthodontic treatment. Prog Orthod. 2015;16:25. doi: 10.1186/s40510-015-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haghgoo R, Ahmadvand M, Moshaverinia S. Remineralizing effect of topical novamin and nano-hydroxyapatite on caries-like lesions in primary teeth. J Contemp Dent Pract. 2016;17:645–9. doi: 10.5005/jp-journals-10024-1905. [DOI] [PubMed] [Google Scholar]
- 29.Askari M, Yazdani R. Comparison of two desensitizing agents for decreasing dentin hypersensitivity following periodontal surgeries: A randomized clinical trial. Quintessence Int. 2019;50:320–9. doi: 10.3290/j.qi.a42096. [DOI] [PubMed] [Google Scholar]
- 30.Kripal K, Chandrasekaran K, Chandrasekaran S, Kumar VR, Chavan SKD, Dileep A. Treatment of dentinal hypersensitivity using propolis varnish: A scanning electron microscope study. Indian J Dent Res. 2019;30:249–53. doi: 10.4103/ijdr.IJDR_400_18. [DOI] [PubMed] [Google Scholar]
- 31.Martins CC, Firmino RT, Riva JJ, Ge L, Carrasco-Labra A, Brignardello-Petersen R, et al. Desensitizing toothpastes for dentin hypersensitivity: A network meta-analysis. J Dent Res. 2020;99:514–22. doi: 10.1177/0022034520903036. [DOI] [PubMed] [Google Scholar]
- 32.Marto CM, Baptista Paula A, Nunes T, Pimenta M, Abrantes AM, Pires AS, et al. Evaluation of the efficacy of dentin hypersensitivity treatments A systematic review and follow-up analysis. J Oral Rehabil. 2019;46:952–90. doi: 10.1111/joor.12842. [DOI] [PubMed] [Google Scholar]
- 33.Li Y, Chen J, Duan Y, Zhou Z. Sealing effects of different Chinese herbal medicines on dentinal tubules: A scanning electron microscopic observation. Ultrastruct Pathol. 2020;2:1–7. doi: 10.1080/01913123.2020.1749198. [DOI] [PubMed] [Google Scholar]
- 34.Figueiredo ML, Aguiar JM, Puppin RR, Pereira RF, Suzy LP, Calegaro ML, et al. Bioinspired catechol chemistry for dentin remineralization: A new approach for the treatment of dentin hypersensitivity. Dent Mater. 2020;36:501–11. doi: 10.1016/j.dental.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Mir M, Mojahedi SM, Tunér J, Shabani M, Darabi F, Rohban A. The effectiveness of home-use photobiomodulation toothbrush for treating dentin hypersensitivity: A pilot study. Laser Ther. 2019;28:193–8. doi: 10.5978/islsm.28_19-OR-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Son SA, Kim DH, Yoo KH, Yoon SY, Kim YI. Mesoporous bioactive glass combined with graphene oxide quantum dot as a new material for a new treatment option for dentin hypersensitivity. Nanomaterials Basel. 2020;27:10. doi: 10.3390/nano10040621. [DOI] [PMC free article] [PubMed] [Google Scholar]


