Abstract
Introduction
The COVID-19 pandemic placed unprecedented strain on the medical supply chain. Early in the pandemic, uncertainty regarding personal protective equipment (PPE) was high. Protecting health care workers from contracting illness is critical to preserve trust and workforce capacity.
Methods
We describe an initiative to design and manufacture a novel, re-usable, half-face respirator in case conventional medical supply chain failed to meet demand. It required new collaboration between the hospital, physicians, the medical school, and the school of engineering. We describe organizational priorities, constraints, and process of design, testing and approval as the health system engaged for the first time directly with the design and manufacturing process for PPE.
Results
An original mask design was developed, and the University Hospital had an initial batch of this novel mask manufactured during the first wave of the SARS-COV-2 pandemic. These masks, and the die necessary to produce more, are in reserve in case of depletion of stores of conventionally sourced PPE.
Conclusions
The COVID-19 pandemic demonstrated fragility of medical supply chain. Organizations considering similar efforts should anticipate constraints on raw material supply chain and be flexible, adaptive, and fast. The incident command structure was vital to identifying priority areas needing alternative approaches, creating connections, and providing rapid approvals. We found organizational value in demonstrating commitment to assuring PPE supplies for health care worker safety.
Key Words: SARS-CoV-2, Infection control, Personal protective equipment, Incident command, Pandemic
Introduction
In December of 2019, the first recognized case of COVID-19 caused by the novel coronavirus SARS-COV-2 was reported.1 The World Health Organization (WHO) soon declared a global pandemic as the illness caused by this novel infectious agent spread rapidly across national borders and overwhelmed hospitals in one country after another.2 By March of 2020, the WHO announced a shortage of personal protective equipment (PPE) endangering health workers worldwide (WHO).2 Global supply of medical masks was rapidly depleting with estimates that industry would need to increase manufacturing by 40% to avoid frontline workers being left “dangerously ill-equipped to care for COVID-19 patients.”2 Within the USA the Federal Emergency Management Agency's Strategic National Stockpile's reserve of N-95 masks to provide aerosol respiratory protection was reported to be exhausted by April 2020, and traditional medical supply chains were disrupted as a result of simultaneously surging demand across the globe.3
Individual hospitals were closely examining use rate of disposable masks. Many implemented contingency capacity conservation measures recommended by the Centers for Disease Control such as minimizing elective procedures to reduce facemask utilization rate and extended use of a disposable mask across multiple patients with COVID-19.4 Other hospitals began implementing CDC crisis capacity measures such as minimizing the number of clinicians interacting with a patient over the course of the day, reusing contaminated masks, or recycling used masks through sterilization processes.4 Despite these measures, media reported hospitals running short of PPE, health care workers protesting, and lawsuits being filed against hospital systems for allegedly providing inadequate protection against spread of infection to health care workers.5 , 6 In planning for extreme shortages, the CDC even offered the option of health care providers using homemade masks, such as bandana or scarf, as a last resort and calls were made for novel sourcing of PPE.4 , 7
We describe an innovative component of a larger organizational response to contingency planning in the event of failure of conventional medical supply chain to meet the needs of health care workers at our institution. We offer insights from the collaboration between front-line clinicians, an engineering design lab, and academic medical center leadership to rapidly design and manufacture novel PPE amid a pandemic.
Network
Work on novel PPE began informally through pre-existing relationships, had an intermediary phase mediated by access to the Incident Command Center, and in the final stage progressed to a formal organizational project management structure. The University of Colorado's Department of Surgery had previously collaborated with Inworks, an innovation initiative within the College of Engineering, Design, and Computing, on engineering-physician partnerships to implement novel concepts such as 3D-printed models from radiologic imaging for surgical planning. In the days leading up to the state mandated stay-at-home order, Inworks began round-the-clock work to spin-up a grass-roots volunteer network (of designers, local fabricators, engineers, sewists, etc.) in an attempt to address a variety of state-wide PPE needs.8 The Department of Surgery began a collaboration with Inworks (and by extension, the volunteer network, Make4Covid) in exploring designing and testing novel respiratory masks for clinicians on March 23, 2020 (Table 1 ). The core initiative team included a front-line physician caring for COVID patients, a number of designers and engineers, a project manager, and an administrative leader from both the Department of Surgery and the University Hospital. As the process moved through design and prototyping, the Hospital's Incident Command Center was a key facilitator of additional connections to the executive team, emergency preparedness, infection prevention, and supply chain. Once the Hospital CEO made the decision to move forward, a multidisciplinary novel manufacturing taskforce with a dedicated executive sponsor and project manager was initiated with mandate to address all equipment for which conventional supply chain was tenuous including masks, face shields, ventilator components, and nasal swabs. This manuscript will focus primarily on the development of novel manufactured masks.
Table 1.
Timeline
| Date | Event |
|---|---|
| December 2019 | Report of novel SARS-COV-2 virus in China |
| February 26, 2020 | First case of community spread of COVID-19 in USA |
| March 3, 2020 | the WHO announced a shortage of personal protective equipment (PPE) endangering health workers worldwide |
| March 19, 2020 | A young designer (whom days later become a volunteer with Make4Covid) begins working on a design in his spare time for a novel filtered mask, motivated by keeping his partner, a frontline health care professional, safe. |
| March 19, 2020 | Inworks begins work to establish a volunteer organization (Make4Covid) seeking to catalyze a range of talent from the greater community to address emerging statewide PPE needs. |
| March 23, 2020 | Department of Surgery begins collaboration with Inworks connecting Administrative Leadership and Front-Line Clinicians to Design team. |
| March 24, 2020 | Concept of novel design and manufacturing of reusable half-face respirator masks introduced to Incident Command Center with rough prototype. |
| April 3, 2020 | Approval to Explore Hospital-funded manufacturing of novel design N-95 Half Face Respirators by Hospital CEO. Triggered assignment to Hospital's Project Management Team. |
| April 3, 2020 | FDA approves first 3D-Printed Mask for COVID-19 support created by the Veterans Health Administration. |
| April 4, 2020 | Working prototype Delivered to Incident Command for examination by Infection Prevention Officer and Logistics Section Chief with approval to move forward with design modification requested to address durability during repeated cleanings. |
| April 6, 2020 | The Livingston Mask design is released open-source by Make4Covid; Inworks models requested revisions to prepare files for manufacturing. |
| April 8, 2020 | Communication with a second prospective US manufacturer with silicone molding capabilities in China (first manufacturer has US-based silicone molding capabilities however turnaround time was deemed too long due to their overwhelm of similar silicone PPE projects). |
| April 8, 2020 | Hospital administration gives final approval to move forward with manufacturing of an initial batch of 350 units, size small. |
| April 26, 2020 | Tooling of mold (for silicone bodies) is completed in-spec by manufacturer. |
| April 28, 2020 | Manufacturer ships batch. |
| May 6, 2020 | Batch of 400 silicone mask body units received from manufacturing in China. Team observes manufacturer deviated from material specs by using a material not certified for biocompatibility and calls for a new batch with correct material. |
| May 2020 | Team recognizes the opportunity to add a tool-safe change in mold to improve wearability (edge ridge) as well as adjust material durometer. This lengthens turnaround time for 2nd batch but deemed important to reduce risk of pressure injury. |
| June 11, 2020 | Second batch of silicone mask bodies arrives from manufacturer. Silicone body edge still reported bothersome (on bridge of nose) during usability testing. |
| June 17, 2020 | Team proceeds with post-production modifications of mask edge (belt sanding). Usability testing reports major improvement. |
| June 22, 2020 | Assembled novel mask units ready for testing. |
Core considerations of the hospital
The primary motivation of our hospital was to adequately meet the PPE needs of all front-line care team members in order to keep them and the patients they care for as safe as possible. In the setting of the pandemic and seeing the challenges experienced by hospitals during outbreaks across the world, cost was not the primary concern, although avoiding waste of limited resources and attentional bandwidth remained a valid consideration. At the same time, the strategy of putting novel designs for PPE into the clinical environment raised potential for several unintended consequences.
The first was the potential to introduce a false sense of protection. It would be vital for clinicians using these masks to understand what they were designed to do as well as their inherent limitations. Communicating to end users the degree to which the combination of mask and filter material deliver aerosol respiratory protection was critical. It was decided that each clinician assigned one of the novel masks would undergo formal aerosol fit-testing to regulatory standards in Employee Health before use in the clinical environment.
A second concern was the possibility of inducing greater anxiety among clinicians, or the general public, if it were known that plans were being made for the failure of conventional medical supply chain to meet PPE needs. While the hospital was working on multiple avenues simultaneously to source PPE and to address this concern, the project team's work was not widely publicized until the ability to deliver a viable product was certain. When communicated, it was framed in terms of contingency planning.
Finally, what would be the organizational liability if non-NIOSH certified respiratory protection were introduced into the clinical environment? To address this, the decision was made that the Governor would need to declare crisis standards of care and the conventional PPE options available to the hospital would have to be exhausted before they would see use. Until such conditions were met, these masks would remain an actualized representation of contingency planning.
Design constraints
The initial stated goal was to develop a durable reusable tight-fitting mask delivering at least the droplet protection of a surgical mask with a design objective of providing protection against aerosolized viral particles at the N-95 level. From the clinical perspective, the mask needed to be tight-fitting to prevent air from entering other than through the filter in order to have potential to meet the aerosol standard yet be comfortable enough to be worn for a prolonged time. The air exchange needed to be adequate for the level of exertion commonly experienced in the clinical environment (ranging from low-intensity sedentary work with the electronic medical record to bursts of high-intensity aerobic exertion during cardiopulmonary resuscitation). It would need to be durable and able to stand up to repeated cycles of decontamination with bleach, alcohol, or disinfectant solution. Finally, the mask design would need to fit within a face shield without excessive fogging. Materials considerations included the need for impermeable materials (other than the filter material itself), biocompatibility, durability, and ability to undergo repeated cycles of disinfection9 (Table 2 ).
Table 2.
Design considerations
| Design constraint | Adaptive consideration |
|---|---|
| Conform to face forming tight fit | Use of flexible silicone mask body, contours designed to match anatomy of face and nose, multiple sizes for different face shapes, |
| Uniform pressure on face distributed sufficiently to reduce risk of pressure injury | Relatively soft, wide, and smooth surface at lip of mask body where it meets the face. |
| Adequate surface area for gas exchange during moderate exertion or short burst of high intensity exertion such as can be encountered in health care setting | Maximizing surface area for gas exchange to match commercial circular N95 filters. Minimizing surface area of obstructing materials in center of the strap chassis and filter plate. |
| Durable for multiple cycles of manual disinfection and re-use over months | Material thickness and mechanical characteristics of silicone and 3D-printed plastic strap chassis materials optimized for durability. Filter material needed to not easily be punctured during decontamination process. |
| Able to withstand multiple exposures to disinfectant chemicals, bleach, and alcohol | Chemical reactivity of materials selected. |
| Exhaled air should not cause fogging of face shields or goggles | Exhaled air direction away from visual fields. Compatibility with eye protection and face shields confirmed with prototype. |
| Impermeable materials for mask body and strap chassis | Permeability characteristics of selected silicone and plastic. Injection molded mask bodies inspected for air-bubbles. Bitrex aerosol fit testing as final confirmation of aerosol impermeability of materials and junctions. |
| Adaptable to fit both existing surplus N95 circular filters and novel filter materials if NIOSH certified N95 materials are exhausted | Mask assembly allows any flat filter material of sufficient surface area to be secured between strap chassis and filter plate. |
| Biocompatible | Medical grade liquid silicone rubber |
Filter material characteristics were a critical consideration during design phase. N-95 level filtration is achieved through mechanical and/or electrostatic mechanisms. All filter materials act via inertial impaction and interception to collect larger droplets and particles whereas diffusion removes smaller particles. Some filter materials also use charged fibers to allow electrostatic attraction to remove small particles with lesser degree of mechanical obstruction to air exchange. We found that filter materials primarily using mechanical filtration require a larger surface area for gas exchange but can be quite thin whereas electrostatic filter materials, such as the discs used in industrial half-face respirators, allowed for greater air exchange for a given surface area but were a number of millimeters thicker. Unlike many commercially-available industrial half-face respirators, unfiltered exhalation ports were assessed as undesirable for the health care use-case because of the need to protect the environment and patient from droplets created by the wearer.
Prototype testing
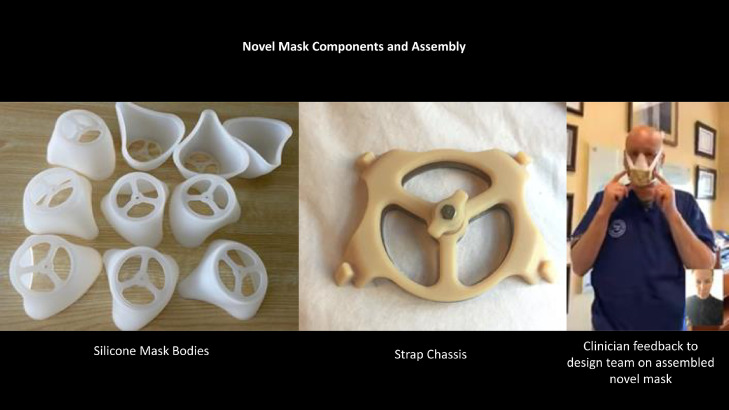
The engineering design team (Inworks in collaboration with Make4Covid) rapidly constructed a series of prototypes. These ranged from flexible industrial N-95 filter material pressed in a cup shape, 3D-printed rigid plastic masks with a grid on the front to hold filter material, and the design ultimately selected (Fig 1 ) with mask-body components of various degrees of flexibility. A frontline clinician on the team worked with the design team to provide rapid-cycle iterative feedback on the prototypes and contribute design concepts to address identified limitations (Fig 2 ). As examples, this stage identified the pressed cup N-95 filter shape as inadequately conformed to the face and excessively flexible, thus not holding a tight seal to the face. More rigid 3D-printed plastic materials were uncomfortable for prolonged use and assessed as risking pressure injury when strapped to the face sufficiently tightly to form a tight seal. In prototyping, a mask body of medical grade silicone had the best balance of flexibility while holding structure under compression. Due to this work occurring during the initial phase of the pandemic, when transmission vectors were still being elucidated, interactions between team members were largely facilitated by remote teleconference with decontamination steps when components or prototypes were physically transferred to reduce risk of COVID transmission.
Fig 1.
Novel mask filtered design.
Fig 2.
Novel mask components and assembly.
A series of hand-constructed prototypes of iterative novel designs were created using poured silicone and 3D-printed plastic materials and subjected to clinical simulation testing. Pre-clinical testing included creating a vacuum seal with inhalation when impermeable plastic was used instead of filter material. It also included passing a simulated fit test through Employee Health using aerosolized Bitrex when fitted with N-95 filter material. Subjective adequacy of gas exchange was examined through use for 2 continuous hours during low levels of exertion (working with electronic health record and normal walking [metabolic equivalent {MET} of 1-3]) as well as moderate levels of exertion (walking and ascending stairs [MET3-6]). Finally, short burst of high degrees of exertion were tested wearing the mask during 4 cycles of chest compressions on a CPR mannequin of 2 minutes each with a 2-minute rest between each cycle.
Via the Incident Command Center, our Infection Prevention Officer reviewed the prototype with key clinical and executive leadership for input and to establish buy-in during the iterative design phase. The center was also critical in approving simulated fit testing of the novel design through Employee Health. The Incident Command Center’ Logistics Section Chief was able to provide an inventory of available resources to support the initiative including a supply of 350 replacement NIOSH approved N-95 electrostatic filter discs with ten provided to the project team for prototype development.
Manufacturing considerations
Components would need to be manufactured at scale from raw materials from disparate industrial production companies not traditionally engaged in creating PPE for health care workers. These fell outside of traditional business-to-business relationships with the health system, and connections were facilitated by the engineering component of the design team. The initial design would need to undergo tool and die making, entailing an upfront cost, followed by per-piece cost driven primarily by that of the raw material with manufacturing discounts at volume thresholds. Simplicity of design and abundance of the raw material both impact cost. However, in the setting of pandemic even the supply of raw material became constrained, and availability and price could change daily. This included specialty components such as N-95 filter material but also more common components such as elastic bands and bulk silicone. Continuous shifting of material availability was a significant complicating factor, and rapid effective communication lines between all parties was critical for pivoting to alternative materials fast enough to be successful.
The interaction between cost, certainty, and speed was complex and created a fundamental challenge. The earlier an order was placed, and the larger the order, the greater certainty that the raw materials would be available; the manufacturer would prioritize the order; and the earlier the production run would be initiated. However, fully exploring alternative sourcing options for lower cost materials or manufacturers takes time, and the principle of waste reduction argues against placing orders greater than the known need. This is especially true when there is potential that the translation from design concept to manufactured product would not result in a viable clinical mask or that traditional medical supply chain capacity would become available in the future.
It was difficult for the hospital to commit to large orders early in the process when there was great uncertainty about the projected future need and the ability of supply chain to meet this need with conventional disposable medical masks. At the same time a recurring experience was that between obtaining preliminary estimates and final commitment, the availability, cost, or timeline for delivery had changed. Thus, the hospital had to balance the time necessary to achieve certainty in some domains against new uncertainties introduced by delays, the greatest of which was the potential to have to go back to the drawing board if an essential step was no longer viable by the time the decision to move forward was made.
Outcome
In an interview with NBC's Meet the Press on March 15th 2020 Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health and member of the US Coronavirus Task Force, described a golden rule for response during a pandemic “When you think you're doing too much, you're probably doing enough or not enough.” While it is challenging to know in advance where the line between prudent preparation and excessive contingency planning lies, this principle was applied in our academic medical center to creating a novel alternative to conventional medical PPE supply chain.
A US based manufacturer with LSR (liquid silicone rubber) injection molding capabilities in China was identified to produce the molds for the medical-grade silicone mask bodies per the specifications of the design team. An initial run of 350 were made and shipped to the US just before new restrictions were put in place on all new masks leaving the country. The stainless-steel filter plates were produced and press-fit into the screw assembly in Littleton, Colorado. The 3d-printed strap chassis and knob were produced in Fort Collins, Colorado. All components were shipped to the Anschutz Medical Campus where they were assembled on-site using N-95 electrostatic filters. Progress was delayed by 2 errors that required rectification. First, the initial batch of silicone mask bodies was not created using the correct biocompatible silicone. This required an additional production run with the correct material once the error was identified. Second, a ridge at the mask-face interface, not apparent on initial hand-poured prototypes, created a zone of problematic pressure. This was remediated by changing to a softer silicone and adding a post-production sanding step to remove this pressure ridge. The manufacturing capability of a hospital-owned die for molding additional masks remains in reserve in case of subsequent waves of infection, contingency planning for what had previously been practically unthinkable.
Limitations
Every disaster is unique and the resources, constraints, and demands experienced at our academic medical center are going to be different than those at other sites and with other types of emergencies. The surface area for gas exchange of the specific mask design selected by the design team has limitations in ability to sustain prolonged aerobic exertion and alternative designs may be needed for use in clinical environments requiring high levels of sustained exercise. The mask design was intended to be paired with surplus electrostatic N-95 filters, or to allow alternative filter materials to be used if commercial filters were exhausted, however the masks, paired with filter materials, were not subjected to testing for regulatory certification. The method to secure the filter material between the strap chassis and filter plate required a puncture at the center of the filter material. Use in the novel mask renders the filters unusable for reuse in commercial industrial half-face respirators.
Discussion
While there are a multitude of future needs, and potential design options to meet them, COVID-19 brought our community together in new ways and provided insights that may be helpful in the future.10 Options for PPE have been explored ranging from entirely 3D-printed plastic masks to adaptations of existing CPR masks with strap and filter for use by the health care worker.11, 12, 13, 14 The pandemic brought forward a culture of novel collaboration and willingness to explore innovation with non-traditional partners. Novel design and manufacture of reusable mask respirators represented one output of this collaboration in our hospital. It also spun off the mass production of novel 3D-printed posterior nasal swabs for SARS-COV-2 sample collection to meet an unmet need in our community, creation of 3D-printed ventilator components, face shields, and design of a novel exhalation filter for industrial half-face respirators in use in the hospital to provide patient protection from droplets for sterile procedures.
Our experience in the COVID-19 pandemic suggests that the Incident Command Structure can serve a vital role in facilitating the network of individuals, input, resources, and information necessary for success. In the setting of emergency there is a need to move rapidly, including making decisions with incomplete information. To match steps with crisis is to dance with uncertainty. A structure for decision making and executive sponsorship is necessary to allow available information to be rapidly assembled and then decisively acted upon.
Early in the pandemic, fear of spread of infection from patients to health care workers was high. In the context of concerns for running out of PPE this was amplified in a manner that caused some organizations to experience internal discord. The act of collaboration between the hospital, the University, and the clinicians who work within it to regain a sense of control and agency over PPE supplies represents an intangible but real benefit of this initiative.
Conclusion
A key question that is difficult to answer is whether the effort and resources placed in novel PPE design and manufacturing represent a prudent investment compared to reliance on stressed existing medical supply chains. Based on the vital importance of being able to deliver PPE in preserving the health and trust of the medical workforce, our academic medical center elected to pursue this avenue to meet what was potentially going to be an unmet need based on the information available early in the pandemic. As of this point, these novel masks, and the manufacturing capability to create more, remain in reserve. However, based on our experience, the iterative process from design to production required several months and subsequent waves of COVID-19 have demonstrated that regional supplies of equipment can be strained long after the initial surge has passed. Health care organizations facing similar crisis in the future need to make this decision early. One way or another, by the time the surge peaks, or next pandemic wave arrives, the die is cast.
Acknowledgments
This project was made possible by the use of an open-source design released by Make4Covid, designed by Schuyler Livingston, and Otterbox for graciously donating 3d print services for biocompatible mask components (chassis and knob).
Footnotes
Conflicts of interest: None to report.
References
- 1.Zhu N, Zhang D, Wang W. China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Timeline: WHO's COVID-19 response. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed April 27, 2020
- 3.Biesecker M. All remaining respirators, masks deployed from Strategic National Stockpile. The Washington Post. 2020 https://www.washingtontimes.com/news/2020/apr/8/strategic-national-stockpile-nearly-depleted-n95-r/ Available at: Accessed April 27, 2020. [Google Scholar]
- 4.CDC. Strategies for optimizing the supply of facemasks. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html. Accessed April 27, 2020
- 5.Mcnamara A. Nurses across the country protest lack of protective equipment. CBS News. 2020 https://www.cbsnews.com/news/health-care-workers-protest-lack-of-protective-equipment-2020-03-28/ Available at: Accessed April 27, 2020. [Google Scholar]
- 6.Ramachandran S. New York nurses allege inadequate safety protocols in lawsuits against state, hospital systems. Wall Street J. 2020 https://www.wsj.com/articles/new-york-nurses-allege-inadequate-safety-protocols-in-lawsuits-against-state-hospital-systems-11587389607 Available at: Accessed April 27, 2020. [Google Scholar]
- 7.Livingston E., Desai A, Berkwits N. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323:1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 8.CU Denver Engineering, Design, and Computing. Inworks and Make4COVID network produce and distribute PPE across Colorado. 2020. Available at:https://ucdengineeringnews.com/2020/09/16/inworks-and-make4covid-network-produce-and-distribute-ppe-across-colorado/. Accessed August 18, 2021.
- 9.Ming Hui Chua MH, Cheng W, Goh SS. Face masks in the new COVID-19 normal: materials, testing, and perspectives. Research (Wash D C) 2020;2020 doi: 10.34133/2020/7286735. PMID: 32832908; PMCID: PMC7429109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gondi S, Beckman AL, Deveau N. Personal protective equipment needs in the USA during the COVID-19 pandemic. Lancet. 2020;395:e90–e91. doi: 10.1016/S0140-6736(20)31038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phan TL, Ching CT. A reusable mask for coronavirus disease 2019 (COVID-19) Arch Med Res. 2020;51:455–457. doi: 10.1016/j.arcmed.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panda R, Kundra P, Saigal S, Hirolli D, Padhihari P. COVID-19 mask: a modified anatomical face mask. Indian J Anaesth. 2020;64:S144–S145. doi: 10.4103/ija.IJA_396_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chao FL. Face mask designs following novel coronavirus. J Public Health Res. 2020;9:1770. doi: 10.4081/jphr.2020.1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Makowski K, Okrasa M. Application of 3D scanning and 3D printing for designing and fabricating customized half-mask facepieces: a pilot study. Work. 2019;63:125–135. doi: 10.3233/WOR-192913. [DOI] [PubMed] [Google Scholar]