Summary:
After reading this article, the participant should be able to (1) almost painlessly inject tumescent local anesthesia to anesthetize small or large parts of the body, (2) improve surgical safety by eliminating the need for unnecessary sedation in patients with multiple medical comorbidities, and (3) convert many limb and face operations to wide awake surgery. We recommend the following 13 tips to minimize the pain of local anesthesia injection: (1) buffer local anesthetic with sodium bicarbonate; (2) use smaller 27- or 30-gauge needles; (3) immobilize the syringe with two hands and have your thumb ready on the plunger before inserting the needle; (4) use more than one type of sensory noise when inserting needles into the skin; (5) try to insert the needle at 90 degrees; (6) do not inject in the dermis, but in the fat just below it; (7) inject at least 2 ml slowly just under the dermis before moving the needle at all and inject all local anesthetic slowly when you start to advance the needle; (8) never advance sharp needle tips anywhere that is not yet numb; (9) always inject from proximal to distal relative to nerves; (10) use blunt-tipped cannulas when tumescing large areas; (11) only reinsert needles into skin that is already numb when injecting large areas; (12) always ask patients to tell you every time they feel pain during the whole injection process so that you can score yourself and improve with each injection; (13) always inject too much volume instead of not enough volume to eliminate surgery pain and the need for “top ups.”
INTRODUCTION
If you were a patient, would you prefer your local anesthetic injector to be a pain-inducing torturer or a magician who hardly hurts you at all? The purpose of this article is to help doctors and nurse injectors be the latter. The last article the senior author wrote on this subject laid out very reproducible tips and tricks to minimize the pain of local anesthesia injection.1 Those techniques have enabled many medical students and residents2 to reliably inject “hole in one” local anesthesia.3 This means that all the patient feels is one little sting from the first poke of a small needle, even when anesthetizing a large area. The purpose of this article is also to update injectors on improvements in the hole in one technique over the last 7 years.
Why is it important to have almost pain-free local anesthetic injection and surgery? Because the two main reasons patients feel they need sedation are (1) the possible pain of local anesthesia injection and (2) the chance that surgery might hurt because of inadequate local anesthesia. Both concerns can be reliably eliminated by following the simple tips of this article.4 Avoiding sedation eliminates nausea and vomiting, unnecessary anesthetic risks, costs, hospital admissions, and the main operating room environment.5–7 Pure local anesthesia is safer than sedation in patients with multiple medical comorbidities. Wide awake surgery makes it more affordable and grants access to millions of the worlds’ poor patients who currently cannot afford sedative surgery in the main operating room.8
Tumescent means a large enough volume of dilute local anesthesia that you can see it and feel it inflating all tissues where sharp objects or broken bones will be manipulated. Nerve decompression such as carpal tunnel,9 cubital tunnel,10 and lacertus release11 are routinely performed with wide awake local anesthesia no tourniquet (WALANT). The results of forearm tendon transfers,12 flexor tendon repairs,13,14 tendon grafts,15 and tenolysis16 can all be improved because surgeons can see comfortable awake patients move the reconstructed tendons during the surgery. In the head and neck, blepharoplasty,17 rhytidectomy, and skin cancer reconstruction such as forehead flaps can readily be accomplished safely without sedation. Surgeons can educate unsedated patients during the procedure to reduce the chances of postoperative complications.18 Eliminating sedation also simplifies and improves safety in many procedures in emergency rooms.
Minimal pain tumescent local anesthesia injection has also been used in wide awake internal fixation of fractures of metacarpals,19 distal radius,20,21 elbows,22 clavicles,23 and ankles.10 When anesthetising long bones for plate fixation, the entire periosteal surface of fracture, screw, or K wire penetration of the cortex must also be bathed with local anesthetic solution.
Perhaps the most important reason to avoid unnecessary pain with local anesthetic injection and wide awake surgery is that it is the right thing to do. Here are 13 ways that work well to achieve the goal.
1. Buffer Local Anesthetic with Sodium Bicarbonate
We prefer to use premixed 1% lidocaine with 1:100,000 epinephrine. However, its pH has been shown to be approximately 4.2, which is roughly 1000 times more acidic than the body pH of 7.4. This is why it stings when it is injected without buffer. We add 1.0 ml of 8.4% sodium bicarbonate to every 10 ml of local anesthetic to decrease the acidic sting.24–27
Refrigerated local anesthetics hurt more than room-temperature solutions.28 Some British hospitals keep their lidocaine and epinephrine refrigerated so that it lasts longer. We store at room temperature and adhere to labeled expiration dates.
2. Use Smaller 27- or 30-gauge Needles
Smaller needles hurt less than larger needles.29–32 We recommend the use of smaller 27-gauge (0.4 mm) or 30-gauge (0.3 mm) needles for injection, instead of 25 gauge or larger needles. Tinier needles also force the injector to slow down the local anesthetic injection speed because of increased resistance. We start most of our injections with a 30-gauge half-inch needle on a 3-ml syringe, and then switch to a 27-gauge 1.25-inch needle on a 10-ml syringe for the rest of the injections.
All hospitals have a designated person who orders needles from commercial sources. Find that designated person and ask her to “check the box” that buys 27- and 30-gauge needles the next time she is ordering. The same goes for ordering premixed lidocaine with epinephrine instead of plain lidocaine without epinephrine.
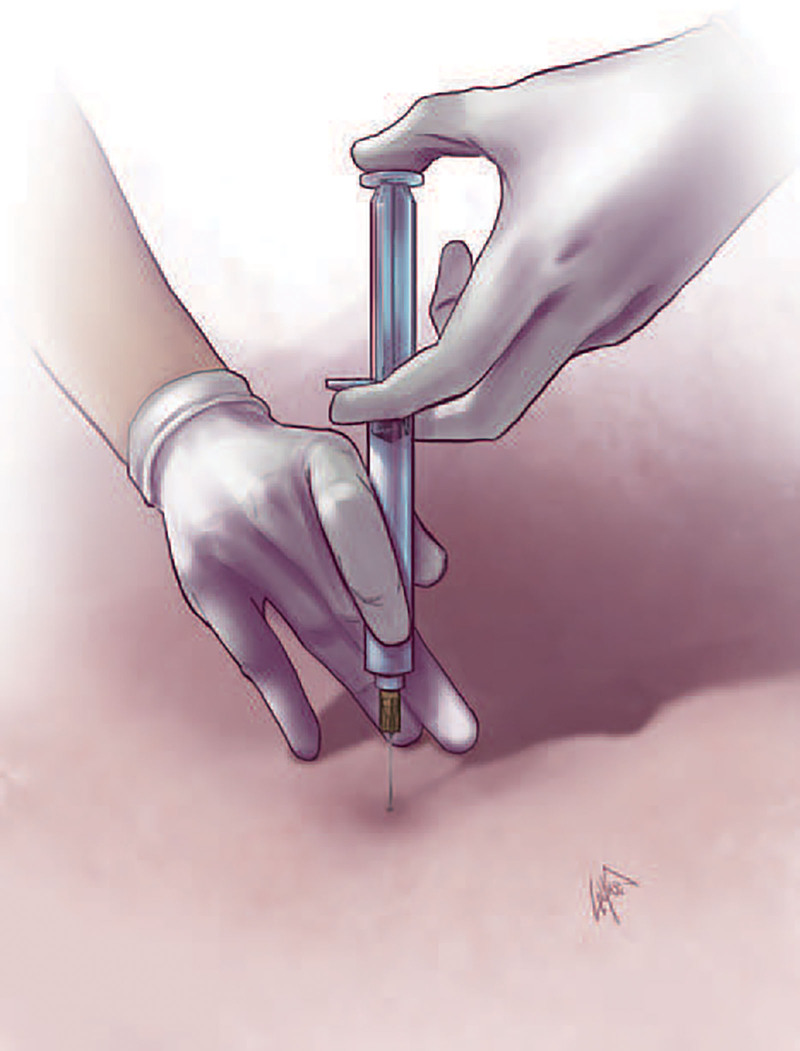
3. Immobilize the Syringe with Two Hands and Have Your Thumb Ready on the Plunger before Inserting the Needle
The senior author has been injected by residents well over 80 times as the first volunteer for many local anesthetic studies. He has felt every little needle movement or wobble until the needle penetration site is numb (Fig. 4.)33 This is why we immobilize the syringe with two stabilized hands and have our thumb ready on the plunger before inserting the needle (Fig. 1). We want zero needle movement in the skin until it is completely numb. Importantly, the hand holding the syringe should not be free in the air, where it is likely to move around before the needle site is numb.
Fig. 4.
Poor technique. Holding the syringe with only one unstabilized hand that can move in space has the patient feeling every little side to side needle movement until the needle site is numb. Needle depth is also not constant as it keeps moving in and out. The thumb is not ready to go on the plunger; so the patient will feel the injector move the needle as he fumbles to get his thumb on the plunger. There is no sensory noise such as pinching the skin proximal to the needle entry site in this image.
Fig. 1.
Stabilize the syringe with both hands, thumb ready on the plunger so that the patient does not feel every little wobble of painful needle movement before the needle entry site is numbed, which can take up to 60 seconds. Reproduced with permission from Plast Reconstr Surg. 2013;132:675–684.
4. Use More Than One Type of Sensory Noise When Inserting Needles into Skin
Our favorite technique is pinching loose skin up into the needle instead of inserting the needle down into the skin (Figs. 2–3). (See Video 1 [online], which displays sensory noise. This illustrates examples of pinching the skin into the needle, inserting needle at mid deep inspiration, and maintaining pinch till sting is all gone.)
Fig. 2.
Sensory noise. Pinch the skin up into the needle instead of pushing the needle down into the skin. Pinch the skin just proximal (relative to nerve origin) to where the needle enters the skin.
Fig. 3.
Good technique. Pinch the skin firmly just proximal to the needle insertion site. Pinch the skin into the needle instead of pushing the needle into the skin. The thumb is ready on the plunger. Both hands are stabilized to immobilize the needle after entry, so that the patient does not feel it moving before the needle site is numbed.
Video 1. Sensory noise. Video 1 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
This creates the sensory noises of pinch, movement, and pressure, which all decrease the volume of the pain sound that the brain hears. Maintain the pressure of the pinch until the patient tells you the needle sting is all gone. We also tell the patients “I will count to 3. When I get to 2, take a nice deep breath. When I get to 3 try not to move when you might feel a little sting. If you move, the needle might come out and might have to sting you twice because I need to put it back in.” Inserting the needle at the mid point of the deep inspiration is good extra sensory noise. If there is no loose skin, press very firmly with a finger just proximal to where the needle goes in until the sting is gone. These simple tricks, along with a 30-gauge needle, will often result in a “hole in zero” where the patient does not feel any pain at all with needle insertion.
Other forms of sensory noise include vibration,34 ice,35,36 music, movies, and virtual reality.37,38 Ask patients to look away because watching the needle insertion may worsen the patient experience.39 Topical local anesthetics are effective in the mucosa, but less so in the impermeable skin. They may numb the upper dermis, but they take a long time to work and do not numb the lower dermis and superficial fat.40 (See Video 2 [online], which displays sensory noise carpal tunnel surgery injection hole in one. When there is not a lot of loose skin, like for the first injection for carpal tunnel surgery, press very firmly with a finger just proximal to the needle insertion site and keep pressing firmly until the patient no longer feels the sting of the needle entry site.)
Video 2. Carpal tunnel local. Video 2 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
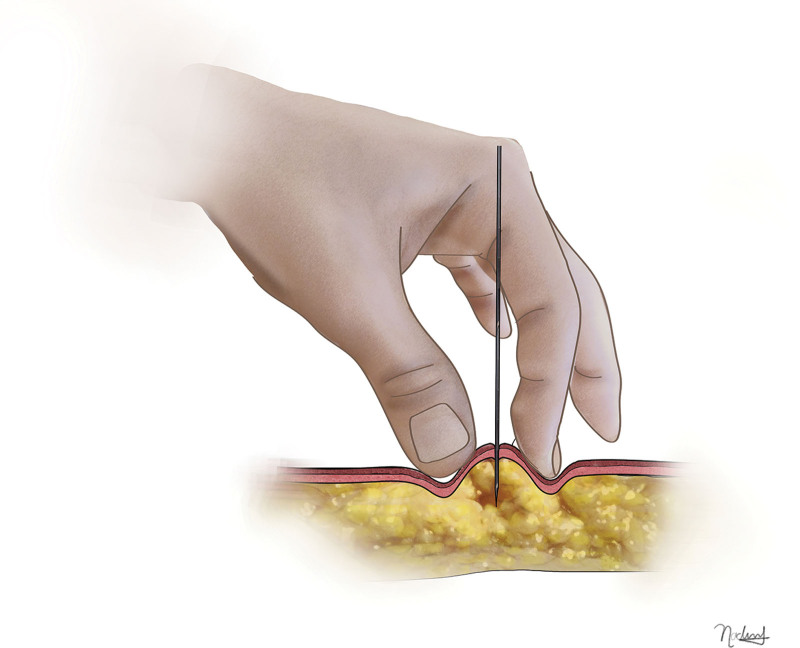
5. Try to Insert the Needle at 90 Degrees Perpendicular to the Skin
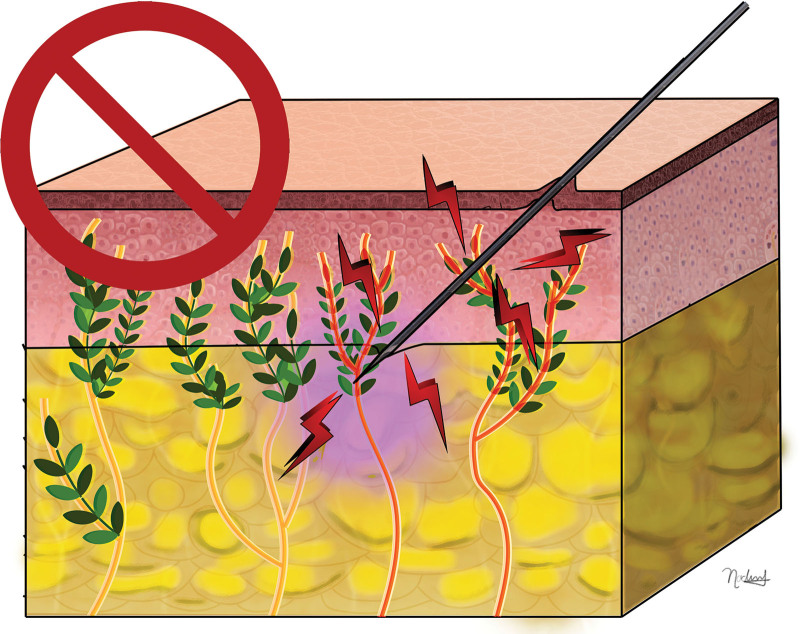
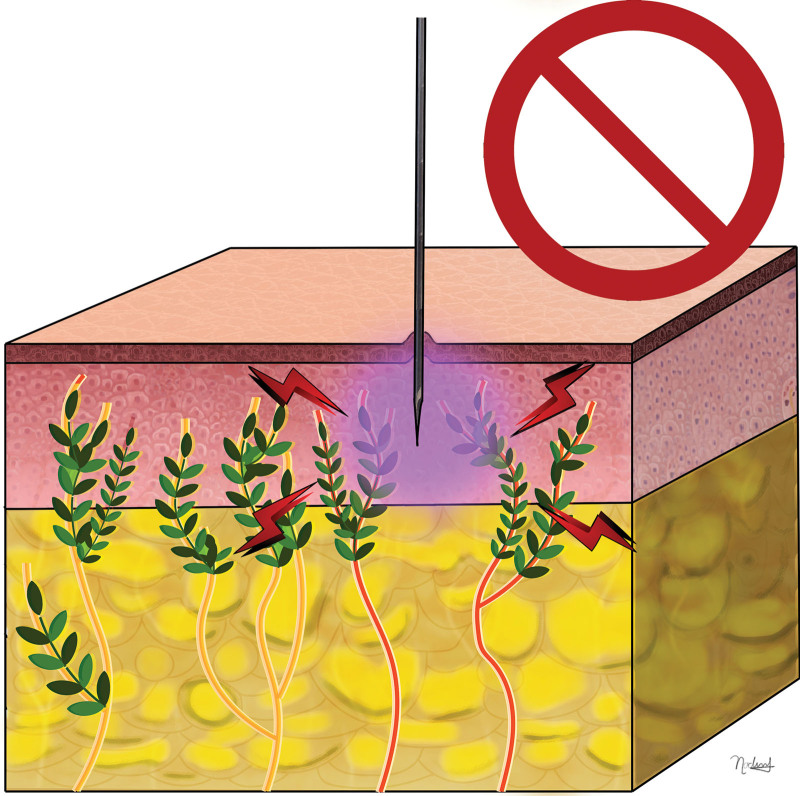
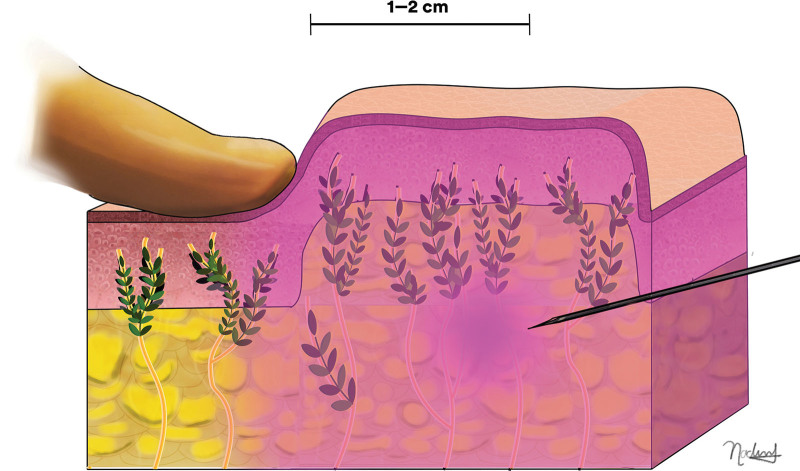
Most skin pain fibers are in the dermis. To compare nerves to trees, the many “leaves” are in the dermis, whereas the fewer “branches and trunks” are in subdermal fat. The injector is less likely to pierce “pain leaves” with perpendicular entry into the skin instead of going in obliquely (45 degrees) or parallel (<45 degrees) across many leaves of the tree (Figs. 5, 6).41,42
Fig. 5.
Do insert the needle perpendicular to the skin to decrease the number of sensory nerve fibers irritated by the needle.
Fig. 6.
Do not insert the needle from 45 degrees to parallel to the skin because it hurts more.
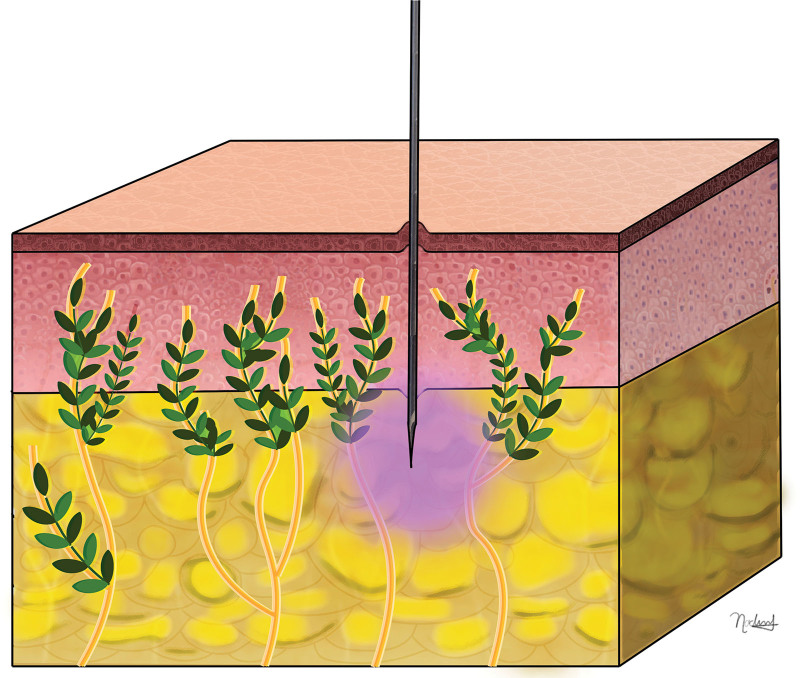
6. Do Not Inject in the Dermis, But in Fat Just Below It
Because nerve endings are concentrated in the dermis, intradermal injections are more painful than subdermal injections (Fig. 7).43 With an open wound such as a laceration, you can avoid putting the needle through sensitive skin altogether. Instead of going through the skin, inject directly into the subcutaneous fat of the open wound where the trunks and branches of the nerve trees are, so that you avoid hurting the many nerves in the skin with transcutaneous needle insertion. As soon as your needle bevel is in the fat, begin slowly injecting until you see tissues swell, and then stop advancing the needle but continue injecting until tissues are very swollen and numb.
Fig. 7.
Do not inject into the dermis because it hurts more.
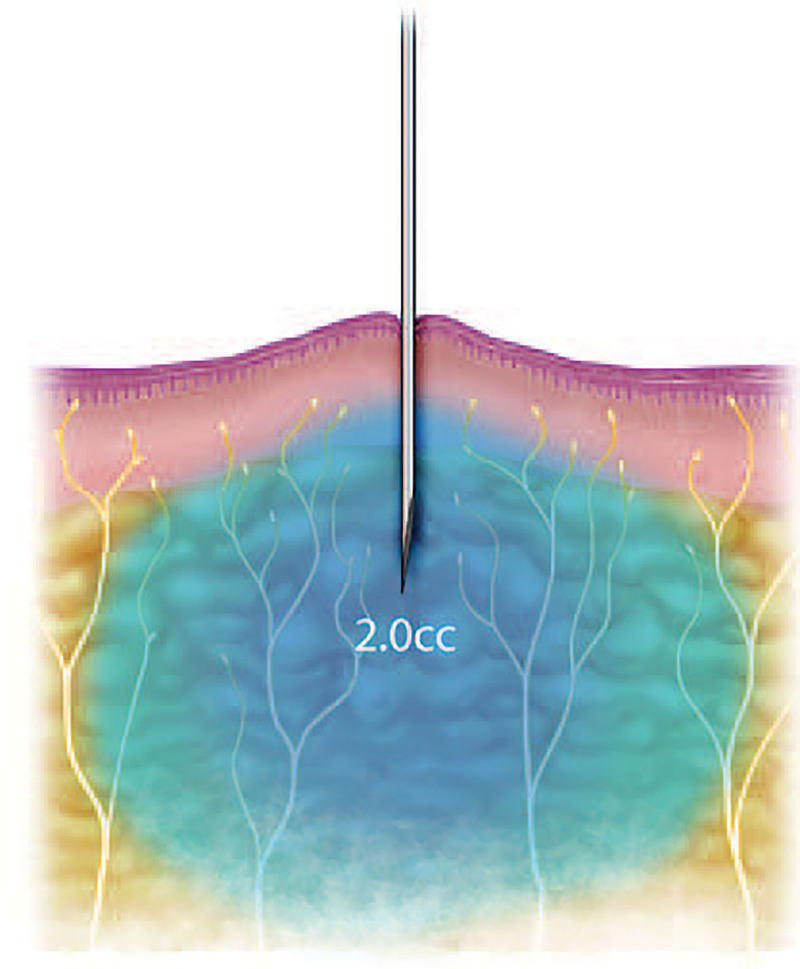
7. Inject At Least 2 ml Slowly Just under the Dermis before Moving the Needle At All (Fig. 8)
Fig. 8.
Do inject at least 2 ml of local anesthesia slowly into the fat just below the skin before moving the needle at all. Reproduced with permission from Plast Reconstr Surg. 2013;132:675–684.
It takes 15–60 seconds for the needle entry site to get numb after penetration. Right after needle penetration, always ask patients to tell you when they no longer feel the needle in the skin. Until they do, keep it perfectly still like a mosquito keeps his mouth’s six needle stylets immobile after they enter your skin. When the needle sting is all gone, you can inject just a little faster until you get at least 2 ml under the skin before you even think of moving the needle. A common mistake is to assume the needle skin is numb and just start moving the needle soon after you get under the skin.
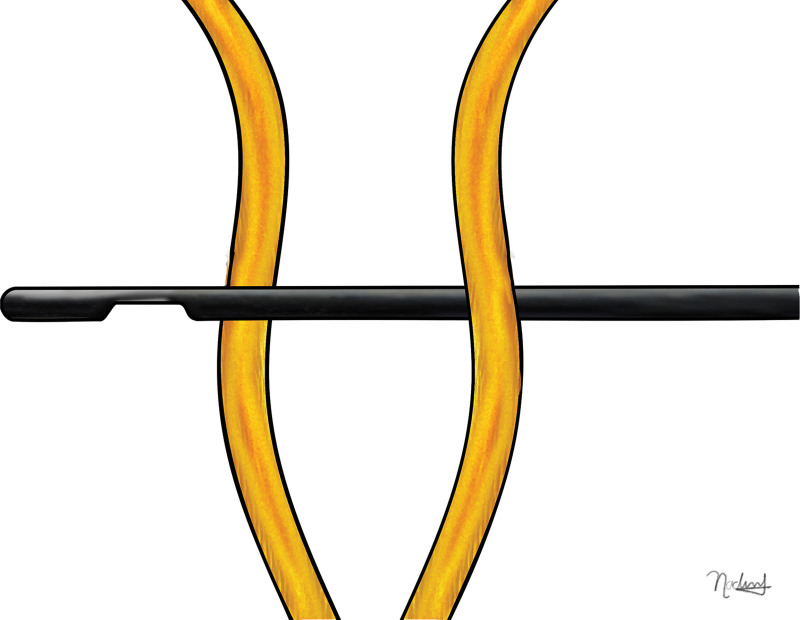
8. Never Advance Sharp Needle Tips Anywhere That is Not Yet Numb
Do not advance sharp needle tips into areas not yet numbed (Fig. 9). Always use a finger of your other hand to palpate ahead of the needle tip so that you can both feel and see where the local anesthesia is swelling the tissue around the needle tip (Fig. 10). Always make sure to have at least 1–2 cm of local anesthesia ahead of where you are advancing sharp needle point. You never want to move your sharp needle tip into an area that is not numb. Move the needle very slowly while injecting antegrade. It is not necessary to draw back on the plunger as minute volumes of intravascular lidocaine and epinephrine are not harmful. Anesthesiologists inject 1 mg/kg of lidocaine slowly intravenously for pain control in some postoperative patients.44 The intravascular half-life of epinephrine is only 1.7 minutes.45 You are not likely to inject intravenously in tumesced fat ahead of the needle in any case.
Fig. 9.
Do not advance sharp needle tip into areas that are not numbered by local anesthesia.
Fig. 10.
Do always see and palpate 1–2 cm of visible palpable local anesthesia ahead of your sharp needle tip so that you never advance the needle anywhere that is not numb. Blow slow before you go… Blow slow before you go…
9. Always Inject from Proximal to Distal
Nerves branch in a proximal-to-distal manner. Injecting proximal to distal increases the likelihood of proximal nerve blockade.46 However, the goal of tumescent local anesthesia is not to provide large nerve blocks. It takes a very long time for local anesthesia to be effective in large nerves: up to 100 minutes for the median nerve at the wrist.47 The goal of tumescence is to bathe all tissue, including all the little nerve branches, affected by surgery. The smaller the nerve, the faster it is numbed. (See Video 3 [online], which displays injection of a nasal cancer reconstruction forehead flap with up to 100 ml of 0.5% lidocaine with 1:200,000 epinephrine. The injections demonstrate starting in an open wound with a 3-ml syringe and a 30-gauge needle, alternating sites to prevent reinsertion pain, saving the columella and alar rims for last so that they do not hurt, and injecting proximal to distal in the forehead.)
Video 3. Forehead flap. Video 3 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
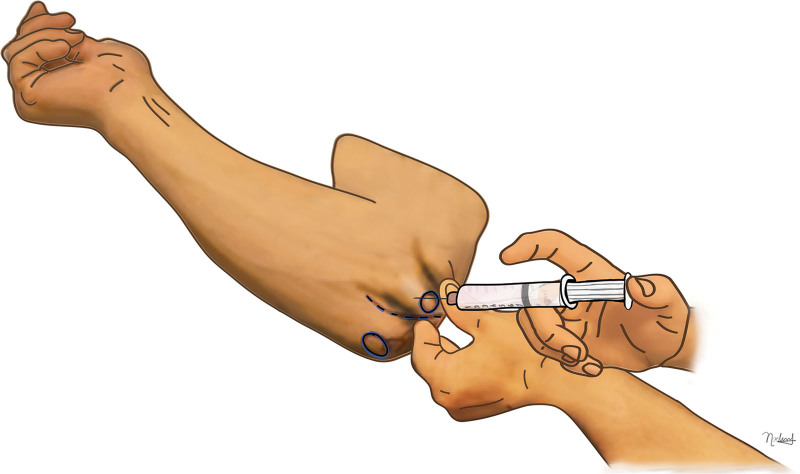
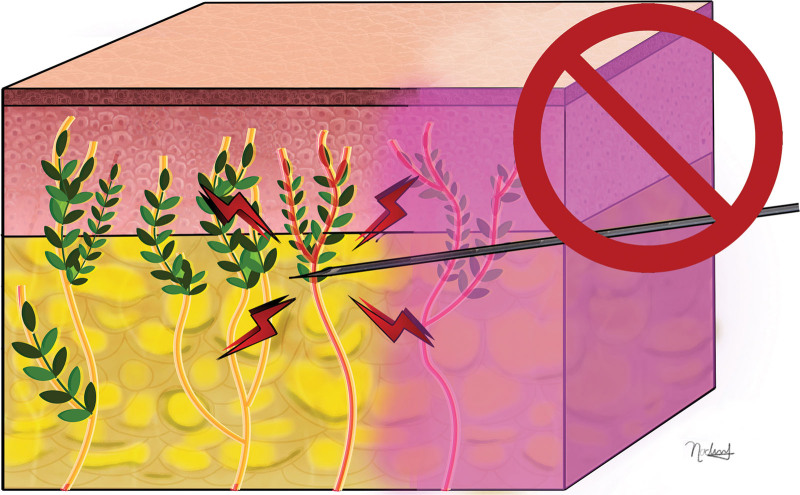
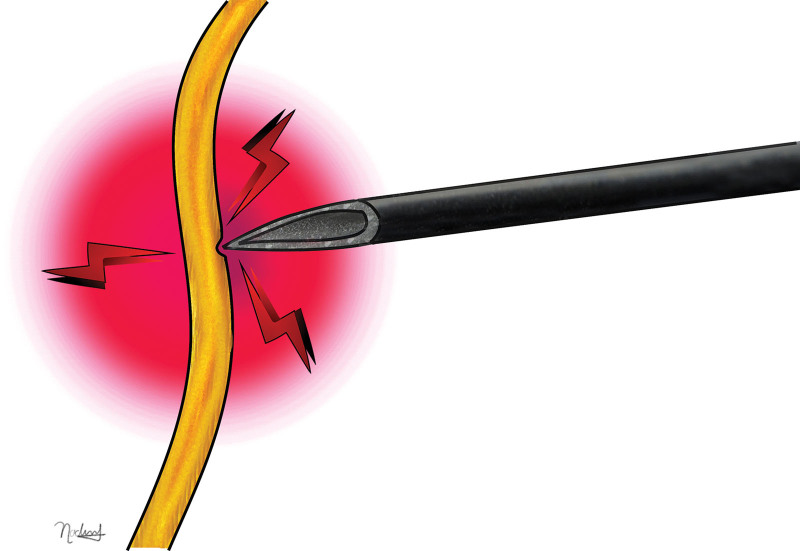
10. Use Blunt-tipped Cannulas When Tumescing Large Areas
A sharp needle makes a skin hole entry site through which you pass a blunt-tipped cannula, which painlessly glides between nerves and blood vessels through subcutaneous fat to anesthetizing large areas more rapidly in procedures such as forearm tendon transfers, skin graft harvest from the thigh, and rhytidectomy.48–51 (Figs. 11, 12). When injecting 200 ml for a forearm tendon transfer or a rhytidectomy, inject the solution from an IV bag with tubing hooked up to a three-way stopcock and a 10-ml syringe. (See Video 4 [online], which displays cannula injection showing some of the tumescent injection of 200 ml of 1/4% lidocaine with 1/400,000 epinephrine for rhytidectomy with a 10-ml syringe connected to an IV bag and tubing with a three-way stopcock. Blunt-tipped cannulas permit more rapid painless injection of large volume cases such as these to provide an even better patient experience. Always reinsert the cannula inside a 1–2 cm border of clearly tumesced numb skin to avoid cannula reinsertion pain.)
Fig. 11.
Sharp needle tips can traumatize nerves through puncture or transection.
Fig. 12.
Blunt tip cannulas slide in the fat with a much lower chance of piercing nerves and blood vessels.
Video 4. Rhytidectomy local. Video 4 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
11. When Tumescing Large Areas, Only Reinsert Needles into Skin that is Already Numb and Alternate Injections from One Side to Another
You need to reinsert the needle when anesthetizing a large area such as a cleft lip reconstruction.52 (See Video 5 [online], which displays injection for simultaneous cubital tunnel and lacertus releases. The injections demonstrate very little movement of the needle as a total of 120 ml is injected into the anterior and medial elbow for proximal median and ulnar nerve decompressions. Always alternate sites of local anesthesia injection with each change of syringe so as to give time for the local to work at the last area injected. Always reinsert needles into clearly tumesced skin so that needle reinsertion does not hurt. Always inject from proximal to distal.) Always reinsert the needle at least 1 cm inside the safe border of clearly blanched, swollen, tumesced skin so that you never insert a needle in skin that is not numb. Patients should never feel pain with the needle reinsertion. Alternate injecting from one side to the other of the surgical field so that needle reinsertion is less likely to hurt because the last side has had more time to get numb. (See Video 5 [online], which displays injection for simultaneous cubital tunnel and lacertus releases. The injections demonstrate very little movement of the needle as a total of 120 ml are injected into the anterior and medial elbow for proximal median and ulnar nerve decompressions. Always alternate sites of local anesthesia injection with each change of syringe so as to give time for the local to work at the last area injected. Always reinsert needles into clearly tumesced skin so that needle reinsertion does not hurt. Always inject from proximal to distal.)
Video 5. Lacertus and ulnar nerve. Video 5 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
12. Always Ask Patients to Tell You Every Time They Feel Pain during the Whole Injection Process so That You Can Score Yourself and Improve Your Technique with Each Injection
Every injection is a learning opportunity. (See Video 6 [online], which displays how to explain to patients about telling the surgeon each time it hurts during the injection process, so that we can get better and better with painless injections. The video also shows stabilizing the syringe with two hands, pinching the skin into the 27-gauge needle, and sensory noise with pinching the skin into the needle and deep inspiration at needle insertion time.) In our practice, if a patient feels pain only once in the whole injection process, the medical student scores a hole in one. If the patient feels pain twice, the resident scores an eagle. If the patient feels pain three times, the lead author scores a birdie. If we all score ourselves every time we inject every patient, our inherent desire to improve our score will drive us to get better and better injectors. (See Video 6 [online].)
Video 6. Explaining pain scoring to patients. Video 6 from “How to Minimize the Pain of Local Anesthetic Injection for Wide Awake Surgery”.
13. Always Inject Too Much Volume Instead of Not Enough Volume to Eliminate Surgery Pain and the Need for “Top Ups”
A very common mistake is to not inject enough volume. The goal is to tumesce all tissues with visible and palpable local anesthesia at least 2 cm beyond wherever you will insert sharp objects or manipulate fractures. You never want to have to add local anesthesia during surgery because a patient feels pain, any more than you want patients to wake up during general anesthesia. We use the extremely safe maximal dosage of 7 mg/kg of lidocaine with epinephrine. We add up to 150 ml of saline to 50 ml of 1% lidocaine with 1:100,000 epinephrine when we need up to 200 ml of volume. We do not need higher concentrations than 0.25% lidocaine with 1:400,000 epinephrine, which provides effective anesthesia for procedures lasting less than 3 hours.
CONCLUSIONS
Patients will truly think you are magical if you take the time to learn these simple techniques that we easily teach all our medical students and residents. They will enable you to almost painlessly tumesce large areas of the body with local anesthesia for safer surgery without the sedation.
Footnotes
Published online 4 August 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. This study did not receive any funding.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132:675–684. [DOI] [PubMed] [Google Scholar]
- 2.Farhangkhoee H, Lalonde J, Lalonde DH. Teaching medical students and residents how to inject local anesthesia almost painlessly. Can J Plast Surg. 2012;20:169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126:1642–1644. [DOI] [PubMed] [Google Scholar]
- 4.MacNeill AL, Wright J, Mayich DJ. Qualitative aspects of patient pain during surgery with wide-awake local anesthesia. J Orthop. 2019;16:105–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lalonde DH, Tang JB. How the wide awake tourniquet-free approach is changing hand surgery in most countries of the world. Hand Clin. 2019;35:xiii–xxiv. [DOI] [PubMed] [Google Scholar]
- 6.Lalonde D. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30:1–6. [DOI] [PubMed] [Google Scholar]
- 7.Yu J, Ji TA, Craig M, et al. Evidence-based sterility: the evolving role of field sterility in skin and minor hand surgery. Plast Reconstr Surg Glob Open. 2019;7:e2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behar BJ, Danso OO, Farhat B, et al. Collaboration in outreach: the Kumasi, Ghana, model. Hand Clin. 2019;35:429–434. [DOI] [PubMed] [Google Scholar]
- 9.Grandizio LC, Graham J, Klena JC. Current trends in WALANT Surgery: a survey of American Society for Surgery of the Hand Members. J Hand Surg Glob Online. 2020;2:186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang S-W, Park H-M, Park J-K, et al. Open cubital and carpal tunnel release using wide-awake technique: reduction of postoperative pain. J Pain Res. 2019;12:2725–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hagert E. Clinical diagnosis and wide-awake surgical treatment of proximal median nerve entrapment at the elbow: a prospective study. Hand (N Y). 2013;8:41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdullah S, Ahmad AA, Lalonde D. Wide awake local anesthesia no tourniquet forearm triple tendon transfer in radial nerve palsy. Plast Reconstr Surg Glob Open. 2020;8:e3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins A, Lalonde DH, Bell M, et al. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. 2010;126:941–945. [DOI] [PubMed] [Google Scholar]
- 14.Lalonde D, Higgins A. Wide awake flexor tendon repair in the finger. Plast Reconstr Surg Glob Open. 2016;4:e797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zukawa M, Osada R, Makino H, et al. Wide-awake flexor pollicis longus tendon reconstruction with evaluation of the active voluntary contraction of the ruptured muscle-tendon. Plast Reconstr Surg. 2019;143:176–180. [DOI] [PubMed] [Google Scholar]
- 16.Tang JB. Wide-awake primary flexor tendon repair, tenolysis, and tendon transfer. Clin Orthop Surg. 2015;7:275–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mckee D, Lalonde D. Minimal pain local anesthetic injection with blunt tipped cannula for wide awake upper blepharoplasty. Plast Reconstr Surg Glob Open. 2017;5:e1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lalonde DH. Conceptual origins, current practice, and views of wide awake hand surgery. J Hand Surg Eur Vol. 2017;42:886–895. [DOI] [PubMed] [Google Scholar]
- 19.Feldman G, Orbach H, Rinat B, et al. Internal fixation of metacarpal fractures using wide awake local anesthesia and no tourniquet. Hand Surg Rehabil. 2020;39:214–217. [DOI] [PubMed] [Google Scholar]
- 20.Tahir M, Chaudhry EA, Zaffar Z, et al. Fixation of distal radius fractures using wide-awake local anaesthesia with no tourniquet (WALANT) technique: A randomized control trial of a cost-effective and resource-friendly procedure. Bone Joint Res. 2020;9:429–439. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21.Orbach H, Rozen N, Rubin G, et al. Open reduction and internal fixation of intra-articular distal radius fractures under wide-awake local anesthesia with no tourniquet. J Int Med Res. 2018;46:4269–4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmad AA, Sabari SS, Ruslan SR, et al. Wide-awake anesthesia for olecranon fracture fixation. Hand (N Y). 2021;16:402–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad AA, Ubaidah Mustapa Kamal MA, Ruslan SR, et al. Plating of clavicle fracture using the wide-awake technique. J Shoulder Elbow Surg. 2020;29:2319–2325. [DOI] [PubMed] [Google Scholar]
- 24.Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plast Surg. 2012;20:71–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesth Analg. 1987;66:572–574. [PubMed] [Google Scholar]
- 26.Kattan S, Lee SM, Hersh EV, et al. Do buffered local anesthetics provide more successful anesthesia than nonbuffered solutions in patients with pulpally involved teeth requiring dental therapy?: A systematic review. J Am Dent Assoc. 2019;150:165–177. [DOI] [PubMed] [Google Scholar]
- 27.Cepeda MS, Tzortzopoulou A, Thackrey M, et al. Adjusting the pH of lidocaine for reducing pain on injection. Cochrane Database Syst Rev. 2010:CD006581. [DOI] [PubMed] [Google Scholar]
- 28.Hogan ME, vanderVaart S, Perampaladas K, et al. Systematic review and meta-analysis of the effect of warming local anesthetics on injection pain. Ann Emerg Med. 2011;58:86–98. e1. [DOI] [PubMed] [Google Scholar]
- 29.Arendt-Nielsen L, Egekvist H, Bjerring P. Pain following controlled cutaneous insertion of needles with different diameters. Somatosens Mot Res. 2006;23:37–43. [DOI] [PubMed] [Google Scholar]
- 30.Zilinsky I, Bar-Meir E, Zaslansky R, et al. Ten commandments for minimal pain during administration of local anesthetics. J Drugs Dermatol. 2005;4:212–216. [PubMed] [Google Scholar]
- 31.Apseloff G, Onel E, Patou G. Time to onset of analgesia following local infiltration of liposome bupivacaine in healthy volunteers: a randomized, single-blind, sequential cohort, crossover study. Int J Clin Pharmacol Ther. 2013;51:367–373. [DOI] [PubMed] [Google Scholar]
- 32.Oni G, Rasko Y, Kenkel J. Topical lidocaine enhanced by laser pretreatment: a safe and effective method of analgesia for facial rejuvenation. Aesthet Surg J. 2013;33:854–861. [DOI] [PubMed] [Google Scholar]
- 33.Strommen JA, Daube JR. Determinants of pain in needle electromyography. Clin Neurophysiol. 2001;112:1414–1418. [DOI] [PubMed] [Google Scholar]
- 34.Nanitsos E, Vartuli R, Forte A, et al. The effect of vibration on pain during local anaesthesia injections. Aust Dent J. 2009;54:94–100. [DOI] [PubMed] [Google Scholar]
- 35.Rasooli F, Sotoodehnia M, Nejati A, et al. The assessment of ice pack effect in pain reduction during digital nerve block: a randomized clinical study. Turk J Emerg Med. 2020;20:81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aminabadi NA, Farahani RM. The effect of pre-cooling the injection site on pediatric pain perception during the administration of local anesthesia. J Contemp Dent Pract. 2009;10:43–50. [PubMed] [Google Scholar]
- 37.Hoxhallari E, Behr IJ, Bradshaw JS, et al. Virtual reality improves the patient experience during wide-awake local anesthesia no tourniquet hand surgery: a single-blind, randomized, prospective study. Plast Reconstr Surg. 2019;144:408–414. [DOI] [PubMed] [Google Scholar]
- 38.Lambert V, Boylan P, Boran L, et al. Virtual reality distraction for acute pain in children. Cochrane Database Syst Rev. 2020;10:CD010686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Höfle M, Hauck M, Engel AK, et al. Viewing a needle pricking a hand that you perceive as yours enhances unpleasantness of pain. Pain. 2012;153:1074–1081. [DOI] [PubMed] [Google Scholar]
- 40.Maxwell D, O’Brien J, Sparkes G, et al. Topical 2% lidocaine gel versus placebo in burn debridement pain. Can J Plast Surg. 1996;6:109. [Google Scholar]
- 41.Kamrul-Hasan A, Paul AK, Amin MN, et al. Insulin injection practice and injection complications - results from the Bangladesh Insulin Injection Technique Survey. Eur Endocrinol. 2020;16:41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martires KJ, Malbasa CL, Bordeaux JS. A randomized controlled crossover trial: lidocaine injected at a 90-degree angle causes less pain than lidocaine injected at a 45-degree angle. J Am Acad Dermatol. 2011;65:1231–1233. [DOI] [PubMed] [Google Scholar]
- 43.Morris R, McKay W, Mushlin P. Comparison of pain associated with intradermal and subcutaneous infiltration with various local anesthetic solutions. Anesth Analg. 1987;66:1180–1182. [PubMed] [Google Scholar]
- 44.Barreveld A, Witte J, Chahal H, et al. Preventive analgesia by local anesthetics: the reduction of postoperative pain by peripheral nerve blocks and intravenous drugs. Anesth Analg. 2013;116:1141–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosen SG, Linares OA, Sanfield JA, et al. Epinephrine kinetics in humans: radiotracer methodology. J Clin Endocrinol Metab. 1989;69:753–761. [DOI] [PubMed] [Google Scholar]
- 46.Shokrzadeh A, Seddighi A, Seddighi AS. Comparison of proximal injections of local anesthetics with distal injections in intravenous block. Glob J Health Sci. 2010;2:215-217. [Google Scholar]
- 47.Lovely LM, Chishti YZ, Woodland JL, et al. How much volume of local anesthesia and how long should you wait after injection for an effective wrist median nerve block? Hand (N Y). 2018;13:281–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lalonde D, Wong A. Local anesthetics: what’s new in minimal pain injection and best evidence in pain control. Plast Reconstr Surg. 2014;134(4 suppl 2):40S–49S. [DOI] [PubMed] [Google Scholar]
- 49.Garcia CP, Avila D, Ferreira V, et al. Anesthesia using microcannula and sharp needle in upper blepharoplasty: a randomized, double-blind clinical trial evaluating pain, bruising, and ecchymoses. J Plast Reconstr Aesthet Surg. 2021;74:364–369. [DOI] [PubMed] [Google Scholar]
- 50.DeJoseph LM. Cannulas for facial filler placement. Facial Plast Surg Clin North Am. 2012;20:215–220, vi. [DOI] [PubMed] [Google Scholar]
- 51.Mckee D, Lalonde D. Minimal pain local anesthetic injection with blunt tipped cannula for wide awake upper blepharoplasty. Plast Reconstr Surg Glob Open. 2017;5:e1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lalonde DH, Price C, Wong AL, et al. Minimally painful local anesthetic injection for cleft lip/nasal repair in grown patients. Plast Reconstr Surg Glob Open. 2014;2:e171. [DOI] [PMC free article] [PubMed] [Google Scholar]