Abstract
Introduction:
The American Heart Association (AHA) introduced the construct of “cardiovascular health (CVH)”, to focus on primordial prevention to reduce the burden of cardiovascular disease (CVD). The CVH score includes 7 health and behavioral metrics (smoking, physical activity, body mass index, diet, total cholesterol, blood pressure, blood glucose), which are characterized as being ideal, intermediate, or poor.
Areas covered:
In this review, we describe the utility of the CVH score for monitoring and promoting wellness, overall and by key sociodemographic groups, and for tracking of temporal trends.
Expert commentary:
Notably, the 7 factors are all modifiable, which differs from 10-year CVD risk scores that include non-modifiable components such as age, sex, and race. Numerous epidemiological studies have shown that achievement of a greater number of ideal CVH metrics is associated with lower incidences of CVD, cardiovascular mortality, and all-cause mortality. Longer duration of favorable CVH is associated with greater longevity and compressed morbidity. Nevertheless, the prevalence of favorable CVH is low, with <20% of U.S. adults meeting ≥5 metrics at ideal levels and significant racial/ethnic disparities persist. Many challenges must be overcome to improve CVH at individual and societal levels if the AHA Impact Goals are to be fully realized.
Keywords: cardiovascular health, prevention, atherosclerotic cardiovascular disease, heart failure
1. Introduction
In 2010, the American Heart Association (AHA) released their 2020 Impact Goals, which stated the goal to reduce deaths from cardiovascular disease (CVD) in the United States (U.S.) by 20% and improve the health of all Americans by 20% [1]. Towards this goal, the AHA introduced the construct of cardiovascular health (CVH), characterized by 7 health behaviors and health factors called the Life’s Simple 7 (LS7) metrics [1]. Favorable CVH is generally considered as having achieved the ideal criteria for at least 5 of these 7 metrics. This construct emphasized the primordial prevention of CVD (i.e., preventing the onset of risk factors) and shifted the focus to the promotion of wellness and health rather than on the treatment of disease [2].
Building on this framework, in 2020, the AHA recently released their 2030 Impact Goals which stated goals of improving health equity in diverse populations and focusing on mental well-being in addition to physical health. Notably, the primary 2030 Impact Goal was to equitably increase healthy life expectancy from age 66 to age 68 years in the U.S. and from 64 to 67 years globally [3]. This is a critical goal in light of data showing that despite 6 decades of prior progress in achieving life extension, the U.S. life expectancy has stalled since 2010 and even declined since 2014 [4]. This stalling in U.S. life expectancy has been attributed to plateauing of progress in CVD death rates [5], and even an increase in CVD death rates in young to middle-aged adults, particularly women [6,7]. Unfortunately AHA surveys from 2009 to 2019 identified a decline in women’s awareness that heart disease was the leading cause of death (from 65% to 44% awareness) [8]. This lack of awareness was greatest among historically marginalized racial/ethnic groups and among younger adults, of whom might benefit the most from primordial prevention. Thus, continued effort towards cardiovascular health promotion, using the framework of the 7 CVH metrics, is more critical than ever.
In this review, we will further the understanding of the CVH score in CVD prevention by describing its utility in public health research and clinical practice for the monitoring and promotion of cardiovascular wellness in the U.S. population, overall and by key sociodemographic groups, and for the tracking of temporal trends in the metrics, in efforts towards achieving the AHA’s 2030 Impact Goals.
2. Selection of the 7 CVH metrics
The process of how the specific 7 CVH metrics were selected has been previously described [1]. Briefly, in 1999, a task force was appointed by the AHA Board of Directors to develop the 2010 AHA Impact Goal. This Task Force decided to begin with a process of a survey, that was administered to approximately 170 scientists from various AHA scientific councils, to review risk factors, risk behaviors and disease states and then rank order them in the importance that these factors need to be addressed to have significant effect on reducing CVD. Among disease states, coronary heart disease (CHD) and stroke were ranked the highest importance. Among risk factors, smoking, high blood pressure, high cholesterol, and physical activity were ranked the most important, in that order, and then obesity and diabetes were added to this list. That is how the 7 CVH metrics were chosen.
3. Definition of favorable CVH
A person is considered to have optimal or favorable CVH by meeting a greater number of metrics at the “ideal” level for each of the specific criteria for the 7 modifiable risk factors, which include smoking, body mass index (BMI), physical activity, diet, cholesterol, blood pressure and blood glucose (Figure 1) [1,9,10]. Typically, in most analyses, points are assigned to each category of the LS7 metrics with 0 indicating poor; 1, intermediate; and 2, ideal for each factor (Table). The points are summed to yield a total CVH score ranging from 0 to 14 [11]. Total CVH scores of 0–8, 9–10, and 11–14 are considered as inadequate, average, and favorable CVH, respectively, but studies are highly variable in their definition and threshold utilized for having favorable CVH [12–14]. For example, other studies have simply counted the number of ideal metrics from 0 to 7, with favorable CVH typically considered if ≥5 metrics at the ideal level are achieved. The use of these 7 CVH metrics and the total CVH score has been used as surveillance tools to measure CVH, CVD mortality, incidence and outcomes in the general population and track national trends over time [1,9,10].
Figure 1: The 7 modifiable health and behavioral metrics included in the CVH score.
Abbreviations: CVH, cardiovascular health; BMI, body mass index
Table:
The seven metrics of CVH characterized by poor, intermediate, or ideal status.
| CVH metrics | Point | Definition |
|---|---|---|
| Smoking | 0 | Current smoker |
| 1 | Former smoker, quit ≤12 months ago | |
| 2 | Never smoker or quit >12 months ago | |
| Body Mass Index | 0 | ≥30 kg/m2 |
| 1 | 25.0–29.99 kg/m2 | |
| 2 | <25.0 kg/m2 | |
| Physical Activity | 0 | No exercise |
| 1 | 1–149 min of moderate exercise or 1–74 min of vigorous exercise/week | |
| 2 | 150+ min of moderate exercise or 75+ min of vigorous exercise/week | |
| Diet | 0 | 0–1 components of healthy diet |
| 1 | 2–3 components of healthy diet | |
| 2 | 4–5 components of healthy diet | |
| Total Cholesterol | 0 | ≥240 mg/dL |
| 1 | 200–239 mg/dL or treated to <200mg/dL | |
| 2 | <200 mg/dL, unmedicated | |
| Blood Pressure | 0 | SBP ≥140 mmHg or DBP ≥90 mmHg |
| 1 | SBP 120–139 mmHg or DBP 80–89 mmHg or treated to <120/80 mm Hg | |
| 2 | <120/80 mm Hg, unmedicated | |
| Blood Glucose | 0 | ≥126 mg/dL fasting |
| 1 | 100–125 mg/dL fasting or treated to <100 mg/dL | |
| 2 | <100 mg/dL fasting, unmedicated |
4. Epidemiology of favorable CVH
Unfortunately, very few U.S. adults are considered to be in optimal or favorable CVH by the LS7 score [15,16]. Data from the 2011–2016 National Health and Nutrition Examination Survey (NHANES) found that the CVH of the U.S. adults is predominantly unfavorable, with 59% having a low/unfavorable score (score 0–8) and only 7.3% of adults having a high CVH score (score 12–14) [17]. Similarly, in the 2013–2014 NHANES survey, only 13% of U.S. adults met ideal levels in 5 metrics, 5% of adults met ideal levels in 6 metrics, and virtually 0% met ideal levels for all 7 metrics [18]. Most U.S. adults (~62%) have 3 or fewer of the 7 metrics in the ideal range [18]. Approximately 92% of U.S. adults have 1 or more metric at poor level, and 36% of adults have 3 or more metrics at poor level. Women are more likely to have more ideal CVH metrics than men across all age groups [18]. The prevalence of meeting ≥5 ideal metrics was 14.8% for men and 21.5% for women (Figure 2). Black and Hispanic adults have poorer CVH than White adults. Asian adults had the greatest prevalence of ≥5 ideal metrics at 29.0%, followed by White (19.4%), Hispanic (14.2%), and Black (10.6%) adults [18] (Figure 2). The prevalence of achieving favorable CVH may be even worse in rural communities [19]. Furthermore, over the decade from 2006 to 2015, the prevalence of meeting ideal status for all CVH metrics declined in the U.S. population [20]. Indeed, there remains great opportunity to improve the CVH status of U.S. adults. A prior AHA statement specifically addressed the critical need to improve CVH among Black adults [21], who experience the most disparities in health equity.
Figure 2: Prevalence of having 5 of more CVH metrics at ideal levels in the U.S. Population by Sex and Race/Ethnicity.
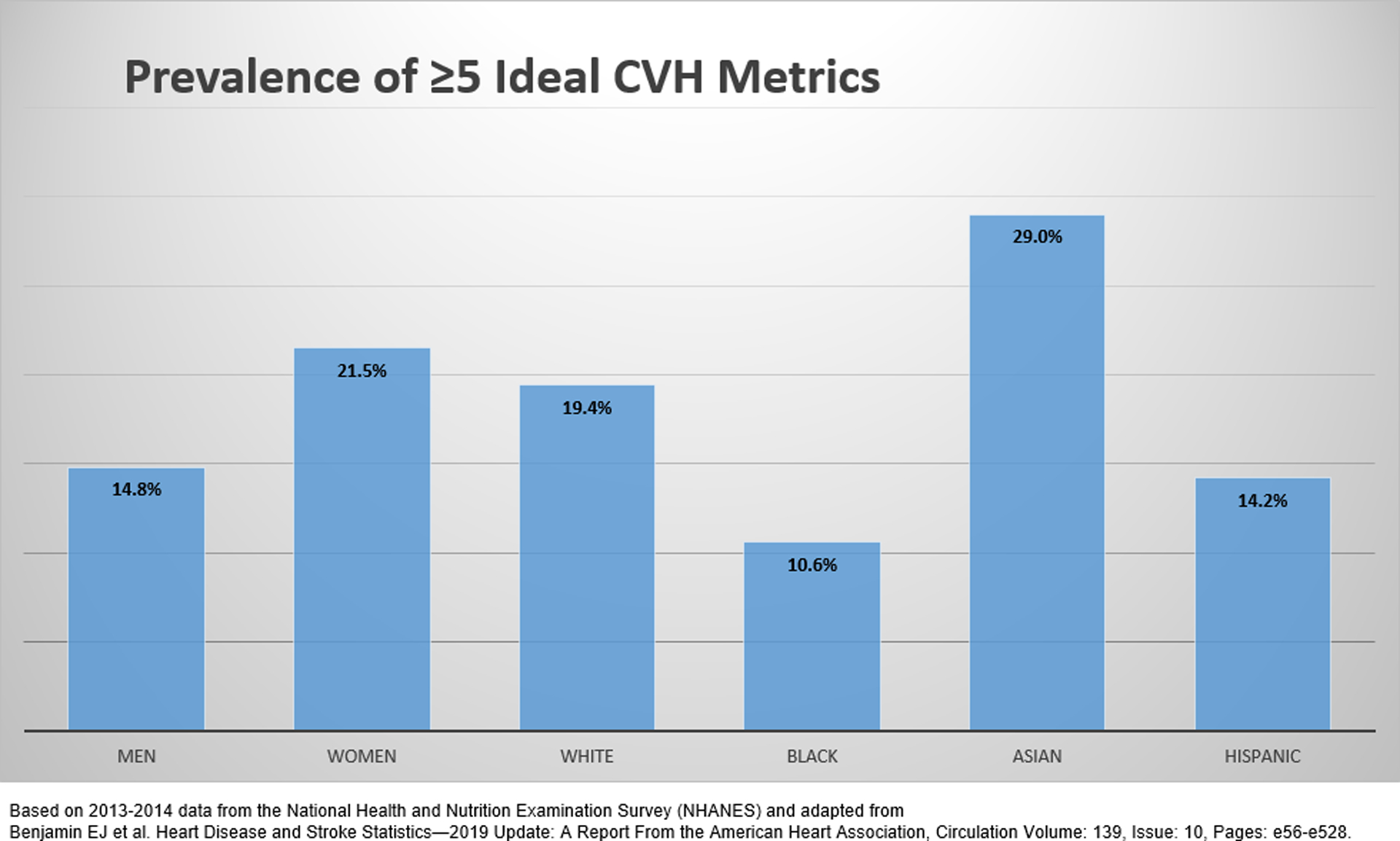
Abbreviations: CVH, cardiovascular health
5. CVH status and future CVD
Numerous epidemiologic studies have demonstrated that the achievement of a greater number of ideal CVH metrics is associated with a lower risk of incident CVD, generally in a linear dose-response manner [22–24]. In a meta-analysis including 12 cohort studies and 210,443 adults, individuals who met 3–4 ideal metrics had a 47% lower risk of incident CVD [HR 0.53 (95% CI 0.47, 0.59)] and those that met 5–7 ideal metrics had a 72% decreased risk of incident CVD [HR 0.28 (0.23, 0.33)], compared to those achieving only 0–2 metrics. This emphasizes the point that even if all metrics of CVH are not ideal, there is still meaningful CVD risk reduction in intermediate compared with poor CVH status [22].
Greater CVH, on basis of LS7 score, is inversely associated across various specific CVD outcomes including a lower risk of incident CHD [25], stroke [25,26], heart failure [27–29], atrial fibrillation [13,30], and peripheral artery disease [31] (Figure 3).
Figure 3: Outcomes Inversely Associated with Greater CVH Score.
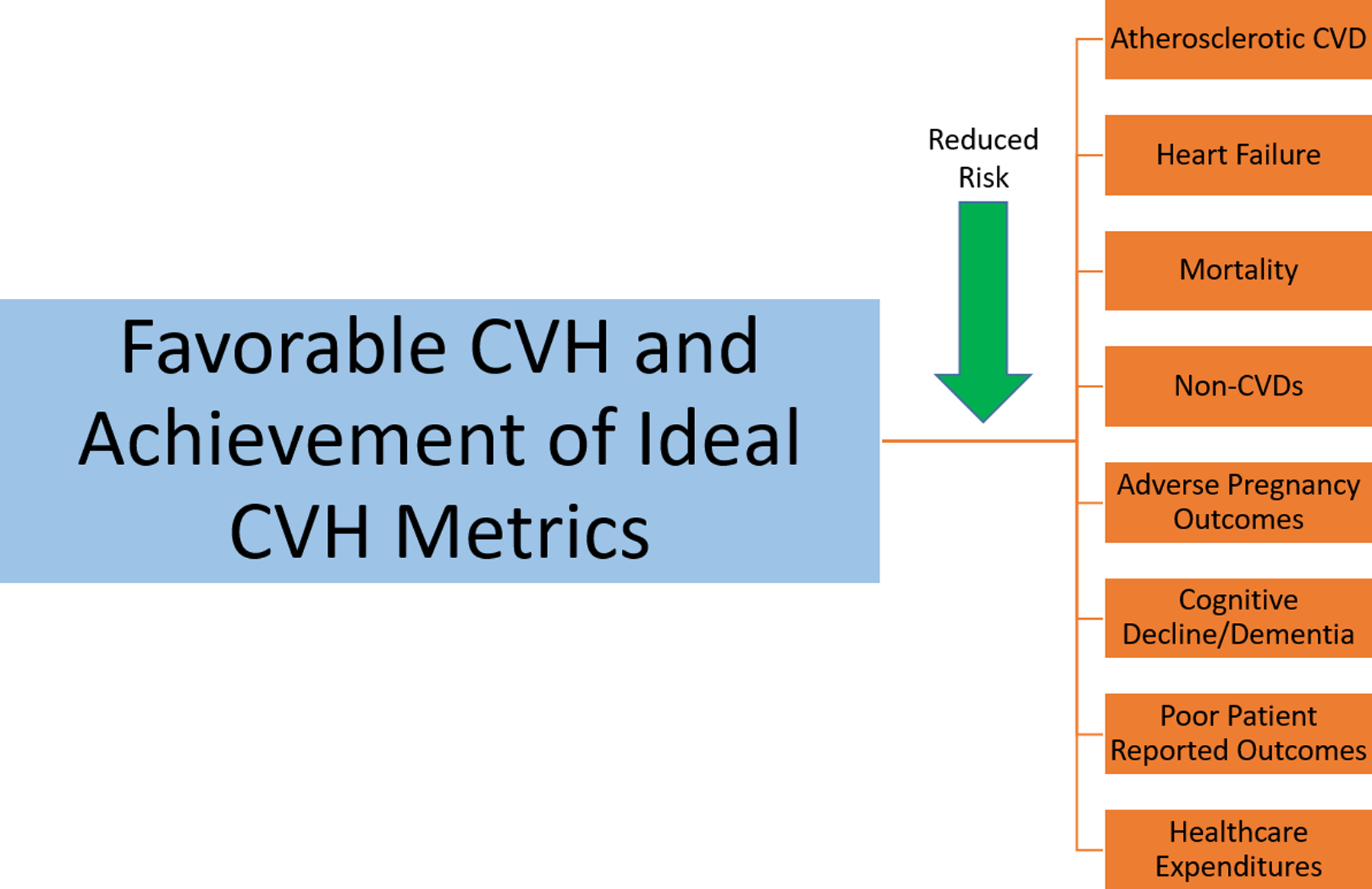
Abbreviations: CVH, cardiovascular health; CVD, cardiovascular disease
Achieving favorable CVH is associated with a number of other important endpoints [32], including lower risk of adverse pregnancy outcomes [33] and cognitive impairment [34], outcomes which are discussed more below, and with a lower risk for all-cause and CVD mortality [16,35,36] (Figure 3). Specifically, a meta-analysis of 9 studies found that the presence of favorable CVH (generally defined as total CVH score ≥10 or ≥5 ideal metrics) was associated with a 45% lower risk of all-cause mortality, a 75% lower risk of cardiovascular mortality, an 80% lower risk of CVD, and a 69% lower risk of stroke [35].
A recent study by Bundy et al examined the impact of what achieving optimal CVH status would be on the U.S. population; for this analysis, the authors utilized the incidence rates of CVD events from 7 U.S. cohorts associated with CVH scores and then applied those rates to NHANES data (2011–2016) to determine nationally representative estimates [17]. The authors determined that the achievement of optimal CVD for adults with low or moderate CVH could prevent an estimated 2 million CVD events each year. Even modest gains in CVH could have big impact [37]. Even if U.S. adults with low CVH were able to move from low to just moderate CVH status, an estimated 1.2 million CVD events could be prevented each year [17].
6. Racial/ethnic differences
As mentioned earlier, there are significant disparities in the prevalence of ideal CVH metrics by race/ethnicity. Across NHANES cycles from 1999 through 2012, the mean CVH scores were lower (by 0.93 points on average) for non-Hispanic Black women than White women at every survey, and Hispanic women had significant lower mean score (0.71 lower) than White women at nearly almost every survey cycle [38]. For men, the racial/ethnic differences in CVH score was less pronounced. Another study that examined the change in CVH score from 1988 to 2014 showed that the racial/ethnic disparities in CVH persisted throughout this period but narrowed in gap, largely due to worsening CVH in White adults and not from improved CVH in Black or Hispanic adults [39].
Nevertheless, the benefits of CVH with improved outcomes have been demonstrated across racial/ethnic groups. For example, in the Jackson Heart Study, Black adults with ≥3 of the 7 metrics optimal had a 47% lower risk of incident heart failure compared to those with <3 metrics achieved [29]. Among Hispanic adults, higher ideal CVH metrics was associated with decreased risk of CHD and stroke [40].
7. Non U.S. populations
The CVH score has been applied to other non-U.S. populations. Even outside of the U.S., the prevalence of favorable CVH is also low, and greater CVH scores are associated with reduced risks of CVD and mortality in these populations too [41–47]. For example, among a community in China, there was a strong inverse relationship between the number of ideal health metrics and cumulative incidence of CVD events over 4-years of follow-up [45]. However only 9% of this Chinese population met criteria for ≥5 ideal metrics and the majority (69%) met criteria for ≤3 ideal metrics [45]. In a population from Australia, each increment in ideal metrics was associated with a 21% lower odds of prevalent CVD [OR 0.79 (0.73, 0.84)], and compared to inadequate scores, those with optimal scores had a 66% lower odds of CVD [0.34 (0.22, 0.54)] [46]. Similarly, in a population from Spain, individuals achieving ≥4 ideal CVH metrics were 66% less likely to develop incident CVD over a 4.8-year follow-up [OR 0.34 (0.21, 0.53)] [47]. Together these studies emphasize the message that while the LS7 construct might have been put forth by the AHA, a coordinated global effort is needed [41].
8. Duration of favorable CVH
The duration of one’s lifetime spent meeting ideal levels of CVH metrics also matters. It has been known for a long time from large epidemiologic cohorts that individuals with low levels of CVD risk factors early in life (young and middle-age adulthood) have decreased risk for cardiovascular and all-cause mortality, and that favorable CVH is associated with longevity [48]. Even the presence of one single risk factor by middle-age (age 55) is associated with increased lifetime risk of CVD compared to someone with all risk factors optimal [49]. By an index age of 45, the lifetime risk of CVD is already 20%; however, those with an optimal risk profile by this age experienced 14 more years free of CVD compared to individuals who already had 2 major risk factors [50]. Indeed, as far as CVD prevention is concerned, it is better to start young [51,52].
Using longitudinal data from the Framingham Heart Offspring Study conducted from 1991 to 2015 (median follow-up 16 years), participants initially at mid-life with a greater duration of favorable CVH across study visits were less likely (by 14–23%) to develop subsequent adverse cardiometabolic outcomes of incident hypertension, incident diabetes, chronic kidney disease, and death compared to those who spent same amount of time in poor CVH [53]. Additionally, data from the CARDIA (Coronary Artery Risk Development in Young Adults) study of adults aged 18–30 years, demonstrated that the presence of high CVH in young adulthood was associated with very low rates of developing premature CVD or mortality over next 32 years [54]. Among these young adults, comparing high vs low CVH status, there was an 86% and 93% reduced risk for subsequent CVD and CVD mortality, respectively, and for combined moderate/high CVH vs low CVH, there was 27% and 19% lower risks, respectively [54]. This underscores the importance of starting health promotion early in life and the need to optimize CVH from childhood through young adulthood.
Notably a healthy cardiovascular risk profile frequently tracks throughout life. Young adults with healthy lifestyle factors are more likely to have favorable CVH profile in middle-age too [55]. Unfortunately, awareness of cardiovascular risk factors remains suboptimal in young adults, with <25% of adults aged 18–39 with borderline levels of risk factors being aware of their risk [56].
9. Pregnancy and CVH
Improving CVH among young adult population should also translate to improve maternal and fetal outcomes too. Data from NHANES 1999 to 2014 showed that less than 1 in 10 pregnant women aged 20 to 44 had high CVH, and the CVH health status for pregnant women was on average worse than for non-pregnant women [57]. Given that the leading cause of maternal mortality is CVD, and that maternal mortality is on the rise in the U.S., and is disproportionately higher in Black women [58], there is much more that needs to be done to optimize the health of expectant mothers. Notably a more favorable CVH profile at 24–32 weeks’ gestation is associated with a lower risk for several adverse pregnancy outcomes such as preeclampsia [33]. Pregnancy has also been defined as a window into future CVH and numerous longitudinal studies have documented that adverse pregnancy outcomes, specifically hypertensive disorders of pregnancy (gestational hypertension, pre-eclampsia), gestational diabetes, preterm delivery, and small for gestational age delivery, are in turn associated with maternal CVD even decades after the index pregnancy [59–63], highlighting the importance of taking a reproductive history for CVD prevention [64].
The CVH of mothers is associated with the subsequent CVH of their offspring [65]. Thus, it is critical to support women before, during, and after pregnancy to optimize maternal and offspring CVH [37]. CVH promotion should be encouraged pre-conception, during pregnancy and during the “4th trimester” post-delivery. Women with a history of multiple live births may be particularly vulnerable to a decline in their own CVH with each delivery. Data from the Multi-Ethnic Study of Atherosclerosis (MESA) found that women with a history of grand multiparity (≥5 live births) were less likely to be in ideal CVH compared to nulliparous women at middle to older ages [66], which tracks along with the increased CVD risk also noted for grand multiparity [67].
10. Secondary CVD prevention
Although we think of the CVH construct for the primordial and primary prevention of CVD, studies have suggested after myocardial infarction that closer adherence to optimal levels of the 7 CVH metrics is associated with better prognosis [68], encouraging the use of this framework even in secondary prevention populations.
11. Non-CVD
Although the construct of the CVH score was derived for the promotion of cardiovascular wellness and the prevention of CVDs, having an optimal CVH score has also been associated with a decreased risk for non-cardiovascular diseases such as decreased risk for cancer, chronic kidney disease, pneumonia, venous thromboembolism, and chronic obstructive pulmonary disease [32,69].
Health promotion is not just about living longer, it is about living longer free of morbidity. A prior study of over 25,000 adults showed that having more favorable CVH in mid-life not only extended survival by 4 years but postponed the onset of morbidity from any cause and from cardiovascular causes by 4.5 and 7 years, respectively [70]. In other words, favorable CVH compresses morbidity to later in life and for shorter duration.
Additionally, we discuss the following non-CVD factors of cognitive health, psychological health, and quality of life below.
11.1. Cognitive function and CVH
Low or poor CVH is also associated with greater risk of cognitive impairment in later life [34,71]. In the Atherosclerosis Risk in Communities (ARIC) study, better CVH in mid-life as assessed by the LS7 metrics, was associated with better cognitive performance at mid-life and reduce cognitive decline over next subsequent 20 years [72]. Favorable CVH at mid-life is also associated with a lower risk of dementia [34]. However even among older adults aged ≥65 years, having a greater number of ideal CVH metrics was linked with lower rates of cognitive decline and dementia [73], suggesting that optimizing CVH even later in life can still confer benefits.
11.2. Psychological health and CVH
There is a strong “mind-body” connection between mental health and physical health [74,75]. In cross-sectional analyses, individuals with more psychological stress and depression were found to be less likely in ideal CVH [76,77]. Among women in mid-life, perceived stress and less rewarding social roles were both associated with having fewer CVH metrics in the ideal range, with longitudinal analyses showing greater stress was associated with lower likelihood of maintaining normal glucose and a normal BMI [78]. Other prospective studies have found that individuals with great ideal CVH metrics had reduced odds of developing depressive symptoms [79], suggesting bidirectional relationship between psychological and CVH. Although a causal relationship cannot be determined, the findings are at least suggestive that improving psychological health may be one strategy to improve CVH.
11.3. Quality of life
Having a greater number of ideal CVH metrics is also associated with better patient reported outcomes including a better self-perception of health [14], a better health-related quality of life, and a more favorable healthcare experience [20]. Thus, preventive measures aimed at optimizing ideal CVH metrics may in turn improve patient experience.
12. Healthcare expenditures
Being in ideal CVH is also associated with reduced health care costs [80,81]. Using cross-sectional data from the 2012 Medical Expenditure Panel Survey which examined 6 of the CVH metrics (diet data were not available), individuals without CVD who had optimal CVH profiles had $4031 lower healthcare expenditures than those with poor CVH profiles, and the difference was even greater ($5946) for those with established CVD [81]. In longitudinal studies, more favorable CVH in midlife was associated with reduced cumulative and annual healthcare costs during Medicare eligibility years (i.e., after age 65) [70].
13. Social determinants of health
There also has been an established link between social determinants of health and CVH. Increasing numbers of social risk factors has been associated with decreased odds of achieving ideal CVH metrics among U.S. adults [82]. For example, both higher educational attainment and a higher household income-to-poverty ratio are consistently associated with greater prevalence of meeting ≥5 ideal CVH metrics [15]. Data from MESA found that factors related to the neighborhood environment, including the walking/physical activity environment, availability of physical activity resources, favorable food stores, and neighborhood socioeconomic status were associated with a higher odds of favorable CVH status (scores 11–14) [83].
A recent AHA statement outlined the importance of housing on CVH and well-being [84]. Employment status has also been linked to CVH scores. Among Hispanic/Latino adults, younger males who were employed had a higher prevalence of an optimal CVH score. On the other hand, Hispanic/Latino women who were unemployed or were homemakers were less likely to meet the ideal CVH metrics [85].
Race is a social construct, either self-identified or assigned by society. Some of aforementioned racial/ethnic disparities in CVH status may be attributed to health inequities related to social determinants of health and structural racism. Prior work from MESA suggested social factors such as neighborhood factors only accounted for a modest difference in the disparities in CVH status by race/ethnicity [86], but no one single social factor or composite score can likely capture all of the social risk contributing to these gaps. A powerful recent statement by the AHA identified structural racism as a fundamental driver of health disparities [87], and highlighted the role that clinicians, scientists, and public health officials can play to be allies and promote anti-racism in order to achieve health equity across the population.
Life course social determinants are important factors to consider and should be further integrated into our approach to CVH promotion.
14. Acculturation and CVH
Acculturation is the process of consciously or subconsciously incorporating the behaviors, customs, values, language of a new country. Voluntary immigrants from minority racial/ethnic groups may have better CVH compared to native-born residents in the U.S. Some studies have examined the degree of acculturation with CVH metrics [39,88–90].
In a cross-sectional study from the MESA study from 6 U.S. communities which included over 6,000 adults free of clinical CVD, greater U.S. acculturation was associated with poorer CVH [88]. Specifically, U.S.-born participants were less likely to have optimal CVH scores compared to foreign-born participants, after accounting for sociodemographic factors [88]. Participants who spoke Chinese or other foreign languages at home had greater odds of having optimal CVH scores compared to participants who spoke English. There was also an inverse association between years lived in the U.S. and the CVH score [88].
Similarly, in another cross-sectional study using 2011–2016 NHANES data of Asian Americans and Latinos found that after adjusting for demographic and socioeconomic factors, participants who spoke their native languages at home were less likely to be in the poor/intermediate category for the CVH metrics of smoking and blood pressure compared to those who spoke English at home [89]. Another cross-sectional study using a community health survey from 2011 to 2014 examined the length of residence in the U.S. and CVH among Afro-Caribbean immigrants in New York City. This study found that after adjusting for sociodemographic factors, immigrants of Guyanese and Haitian origin who had lived in the U.S. for ≥10 years had a higher prevalence of being in the poor/intermediate category of the CVH score compared to those who had lived in the U.S. for less than 10 years [90].
Thus, the available data suggest that greater U.S. acculturation and more years lived in the U.S. are associated with poorer CVH. The CVH score can be one way to monitor CVH among immigrant populations and highlights the need to develop culturally tailored programs that promote CVH and wellness among immigrant populations.
15. Biomarkers
Biomarkers are subclinical indicators of physiological and pathological processes [91] and can help facilitate early detection and prognostication of CVD [92]. Not surprisingly, greater CVH scores have shown an inverse relationship with subclinical biomarkers of disease [93–97]. For example, in the MESA study, even after adjusting for sociodemographic factors, poor CVH status was found to be associated with higher levels of the inflammatory markers of GlycA, high sensitivity C-reactive protein (hsCRP), and interleukin-6 (IL-6), as well as with higher levels of the risk markers of fibrinogen, D-dimer, homocysteine and high-sensitivity cardiac troponin T [94,95], although a direct association was found between CVH score and N-terminal pro-B-type natriuretic peptide [95]. In the Framingham Study, the authors similarly found inverse association of CVH score with CVD subclinical biomarkers except for a direct association with natriuretic peptides, and concluded that the inverse association of CVH with incident clinical CVD events was at least partly attributable to the favorable relationship of CVH with these subclinical biomarkers of risk [97]. Together, these studies suggest that the generally favorable association of CVH with biomarkers of CVD risk may be an intermediary step in the progression to clinical CVD events and may offer a window of opportunity for more intensive preventive efforts. However, it remains unclear if biomarkers would provide additional information in monitoring or clinical prediction above and beyond assessment of CVH.
16. Subclinical atherosclerotic disease
Similar to biomarkers, multiple studies have demonstrated an inverse association between ideal CVH scores and measures of subclinical cardiovascular disease [93,96–107]. For example, there is also an inverse relationship between the number of ideal CVH metrics and the prevalence of coronary artery calcium (CAC) in adults [106,107], which is a surrogate marker of the total burden of coronary atherosclerosis and prognostic of future CVD risk [108]. In the MESA study, adults with moderate and high CVH scores had a 43% and 71% lower odds of having prevalent CAC (CAC score >0) compared to adults with low CVH scores [93]. Additionally, some studies have also found that higher CVH scores were associated with a lower prevalence and incidence of aortic calcification [109,110].
In the Young Fins study, children and young adults (ages 12–24) with better CVH had decreased prevalence of subclinical atherosclerosis, as assessed by CAC and increased carotid intimal medial thickness, once they reached middle age [105], emphasizing the importance that prevention and optimization of CVH should begin early in life. In this study, individuals who started with low CVH but improved their CVH over the follow-up also had lower prevalence of subclinical vascular disease than those with remained at low CVH, thus demonstrating the importance of regaining CVH even if it is initially lost [105].
17. Atherosclerotic CVD Risk Scores vs CVH Score
Most prevention guidelines recommend starting a clinician-patient risk discussion with the estimation of an individual’s 10-year risk for atherosclerotic CVD to guide decisions regarding preventive therapies [111]. After calculation of 10-year risk, individuals are then classified as being at low (<5%), borderline (5–<7.5%), intermediate (7.5–<20%), or high (≥20%) risk for atherosclerotic CVD, and this risk estimation can be further fine-tuned by considering “risk-enhancing” factors and the selective use of CAC among the borderline and intermediate risk groups [111]. Limitations of 10-year CVD risk estimation tools, such as the Pooled Cohort Equations, include that they are heavily driven by non-modifiable factors such as age, sex, and race/ethnicity and can both over- and under-estimate risk among certain populations [112,113]. The advantage of the CVH score is that it considers only modifiable factors, and thus discussion with individuals about their CVH score would be beneficial to emphasize the things that individuals can directly change. However, to really combat the epidemics of CVD, strategies need to move beyond an individual-based (n of 1) approach, especially when tremendous societal pressures are stacked against the optimization of CVH.
18. Expert opinion
In sum, there is robust and ample data about the benefits of CVH for longevity, reduced risk for CVD, and protection from a variety of non-cardiovascular chronic diseases. Despite this, the worsening trends of CVH in U.S. adults suggest effective translational promoting CVH in clinical practice is lacking. Multiple organizations including the AHA and U.S. Preventive Services Task Force (USPSTF) have put forth recommendations on behavioral counseling and population-based approaches for improving the lifestyle components of the CVH score [111,114,115], but their effectiveness has been variable. Since favorable CVH metrics tend to cluster together, comprehensive health promotion strategies are likely to more effective than focusing on any one single measure [116], and community partnerships outside of healthcare professionals should be leveraged [117]. A team-based approach to prevention should be employed [111].
Entire psychological, social, and community factors should be addressed to combat structural and systemic barriers to health inequities. Large population based structural changes are warranted related to access to healthcare, access to healthy food sources, transportation modalities, working hours, structural racism, and poverty. There are a lot of advantages of using the CVH construct in its simplicity of just 7 measures and its demonstrated strong prognostic value, to track population health over time. However, many challenges still remain and must be overcome to improve CVH at the individual and the societal level if the AHA 2030 Impact Goals are to be fully and equitably realized.
Article highlights.
The cardiovascular health (CVH) is characterized by 7 health behaviors and health factors that are all modifiable.
A greater number of ideal CVH metrics and higher composite scores are associated with lower incidences of cardiovascular disease (CVD), cardiovascular mortality, non-cardiovascular diseases, and all-cause mortality
Even modest gains in CVH across the population can have large impact in reducing CVD events.
Maternal CVH influences offspring CVH; it is important to support CVH of women before, during, and after pregnancy
Longer duration spent in optimal CVH is association with longevity and compressed morbidity
Funding
E Michos is supported by the Amato Fund in Women’s Cardiovascular Health at Johns Hopkins School of Medicine. S Khan is supported by grants from the American Heart Association (#19TPA34890060) and National Institutes of Health (P30DK092939; P30AG059988).
Footnotes
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
References
Annotation: ‘*’ – of interest, or “**” – of considerable interest
- 1.**.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]; This AHA statement was the pivotal document that first introduced the construct of cardiovascular health (CVH) score.
- 2.Labarthe DR. From cardiovascular disease to cardiovascular health: a quiet revolution? Circulation Cardiovascular quality and outcomes. 2012. November;5(6):e86–92. [DOI] [PubMed] [Google Scholar]
- 3.Angell SY, McConnell MV, Anderson CAM, et al. The American Heart Association 2030 Impact Goal: A Presidential Advisory From the American Heart Association. Circulation. 2020;141(9):e120–e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolf SH, Schoomaker H. Life Expectancy and Mortality Rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta NK, Abrams LR, Myrskyla M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A. 2020;117(13):6998–7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan SU, Bashir ZS, Khan MZ, et al. Trends in Cardiovascular Deaths Among Young Adults in the United States, 1999 to 2018. Am J Cardiol. 2020;128:216–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curtin SC. Trends in Cancer and Heart Disease Death Rates Among Adults Aged 45–64: United States, 1999–2017. Natl Vital Stat Rep. 2019;68(5):1–9. [PubMed] [Google Scholar]
- 8.Cushman M, Shay CM, Howard VJ, et al. Ten-Year Differences in Women’s Awareness Related to Coronary Heart Disease: Results of the 2019 American Heart Association National Survey: A Special Report From the American Heart Association. Circulation. 2021;143(7):e239–e248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angell SY, McConnell MV, Anderson CAM, et al. The American Heart Association 2030 Impact Goal: A Presidential Advisory From the American Heart Association. Circulation. 2020;141(9):e120–e138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roger VL, Sidney S, Fairchild AL, et al. Recommendations for Cardiovascular Health and Disease Surveillance for 2030 and Beyond: A Policy Statement From the American Heart Association. Circulation. 2020;141(9):e104–e119. [DOI] [PubMed] [Google Scholar]
- 11.Lloyd-Jones DM. Improving the cardiovascular health of the US population. JAMA. 2012;307(12):1314–6. [DOI] [PubMed] [Google Scholar]
- 12.Ogunmoroti O, Utuama OA, Michos ED, et al. Does education modify the effect of ethnicity in the expression of ideal cardiovascular health? The Baptist Health South Florida Employee Study. Clin Cardiol. 2017;40(11):1000–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogunmoroti O, Michos ED, Aronis KN, et al. Life’s Simple 7 and the risk of atrial fibrillation: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2018;275:174–181. [DOI] [PubMed] [Google Scholar]
- 14.Osibogun O, Ogunmoroti O, Spatz ES, et al. Is self-rated health associated with ideal cardiovascular health? The Multi-Ethnic Study of Atherosclerosis. Clin Cardiol. 2018;41(9):1154–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139–e596. [DOI] [PubMed] [Google Scholar]
- 16.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.**.Bundy JD, Zhu Z, Ning H, et al. Estimated Impact of Achieving Optimal Cardiovascular Health Among US Adults on Cardiovascular Disease Events. J Am Heart Assoc. 2021;10(7):e019681. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study estimated that if U.S. adults with low or moderate CVH could achieve high CVH, approximately 2 million CVD events could be prevented each year.
- 18.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56–e528. [DOI] [PubMed] [Google Scholar]
- 19.Kim JI, Sillah A, Boucher JL, et al. Prevalence of the American Heart Association’s “ideal cardiovascular health” metrics in a rural, cross-sectional, community-based study: the Heart of New Ulm Project. J Am Heart Assoc. 2013;2(3):e000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tibuakuu M, Okunrintemi V, Savji N, et al. Nondietary Cardiovascular Health Metrics With Patient Experience and Loss of Productivity Among US Adults Without Cardiovascular Disease: The Medical Expenditure Panel Survey 2006 to 2015. J Am Heart Assoc. 2020;9(19):e016744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.**.Carnethon MR, Pu J, Howard G, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136(21):e393–e423. [DOI] [PubMed] [Google Scholar]; This AHA Scientific Statement highlighted health disparities experience by Black adults and strategies needed to improve CVH in this population.
- 22.Ramirez-Velez R, Saavedra JM, Lobelo F, et al. Ideal Cardiovascular Health and Incident Cardiovascular Disease Among Adults: A Systematic Review and Meta-analysis. Mayo Clin Proc. 2018;93(11):1589–1599. [DOI] [PubMed] [Google Scholar]
- 23.Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: A meta-analysis of prospective studies. Clin Cardiol. 2017;40(12):1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaye B, Tafflet M, Arveiler D, et al. Ideal Cardiovascular Health and Incident Cardiovascular Disease: Heterogeneity Across Event Subtypes and Mediating Effect of Blood Biomarkers: The PRIME Study. J Am Heart Assoc. 2017;6(10):e006389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kulshreshtha A, Vaccarino V, Judd SE, et al. Life’s Simple 7 and risk of incident stroke: the reasons for geographic and racial differences in stroke study. Stroke. 2013;44(7):1909–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogunmoroti O, Oni E, Michos ED, et al. Life’s Simple 7 and Incident Heart Failure: The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2017;6(6):e005180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nayor M, Enserro DM, Vasan RS, et al. Cardiovascular Health Status and Incidence of Heart Failure in the Framingham Offspring Study. Circ Heart Fail. 2016;9(1):e002416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spahillari A, Talegawkar S, Correa A, et al. Ideal Cardiovascular Health, Cardiovascular Remodeling, and Heart Failure in Blacks: The Jackson Heart Study. Circ Heart Fail. 2017;10(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garg PK, O’Neal WT, Chen LY, et al. American Heart Association’s Life Simple 7 and Risk of Atrial Fibrillation in a Population Without Known Cardiovascular Disease: The ARIC (Atherosclerosis Risk in Communities) Study. J Am Heart Assoc. 2018;7(8):e008424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang D, Zhang Q, Wang A, et al. Ideal Cardiovascular Health Metrics on the New Occurrence of Peripheral Artery Disease: A Prospective Cohort Study in Northern China. Sci Rep. 2020;10(1):9660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.*.Ogunmoroti O, Allen NB, Cushman M, et al. Association Between Life’s Simple 7 and Noncardiovascular Disease: The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2016;5(10):e003954. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study linked the CVH score to incidence of non-cardiovascular diseases.
- 33.Perak AM, Lancki N, Kuang A, et al. Associations of gestational cardiovascular health with pregnancy outcomes: the Hyperglycemia and Adverse Pregnancy Outcome study. Am J Obstet Gynecol. 2021;224(2):210.e1–210.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabia S, Fayosse A, Dumurgier J, et al. Association of ideal cardiovascular health at age 50 with incidence of dementia: 25 year follow-up of Whitehall II cohort study. BMJ. 2019;366:l4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: A meta-analysis. Int J Cardiol. 2016;214:279–83. [DOI] [PubMed] [Google Scholar]
- 36.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125(8):987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Michos ED, Khan SS. Modest Gains Confer Large Impact: Achievement of Optimal Cardiovascular Health in the US Population. J Am Heart Assoc. 2021;10(7):e021142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pool LR, Ning H, Lloyd-Jones DM, et al. Trends in Racial/Ethnic Disparities in Cardiovascular Health Among US Adults From 1999–2012. J Am Heart Assoc. 2017. September 22;6(9):e006027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown AF, Liang LJ, Vassar SD, et al. Trends in Racial/Ethnic and Nativity Disparities in Cardiovascular Health Among Adults Without Prevalent Cardiovascular Disease in the United States, 1988 to 2014. Ann Intern Med. 2018;168(8):541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gonzalez HM, Tarraf W, Rodriguez CJ, et al. Cardiovascular health among diverse Hispanics/Latinos: Hispanic Community Health Study/Study of Latinos (HCHS/SOL) results. Am Heart J. 2016. June;176:134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.*.Younus A, Aneni EC, Spatz ES, et al. A Systematic Review of the Prevalence and Outcomes of Ideal Cardiovascular Health in US and Non-US Populations. Mayo Clinic proceedings. 2016. May;91(5):649–70. [DOI] [PubMed] [Google Scholar]; This study determined the prevalence of optimal CVH was also low in non-U.S. populations and similarly, unfavorable CVH was associated with incident CVD; this emphases that global strategies for health promotion are warranted.
- 42.Zhou L, Zhao L, Wu Y, et al. Ideal cardiovascular health metrics and its association with 20-year cardiovascular morbidity and mortality in a Chinese population. J Epidemiol Community Health. 2018;72(8):752–758. [DOI] [PubMed] [Google Scholar]
- 43.Kim JY, Ko YJ, Rhee CW, et al. Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: the Seoul male cohort study. J Prev Med Public Health. 2013;46(6):319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu Y, Chi HJ, Cui LF, et al. The ideal cardiovascular health metrics associated inversely with mortality from all causes and from cardiovascular diseases among adults in a Northern Chinese industrial city. PloS One. 2014;9(2):e89161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu S, Huang Z, Yang X, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–93. [DOI] [PubMed] [Google Scholar]
- 46.Peng Y, Wang Z. Association of Life’s Simple 7 and presence of cardiovascular disease in general Australians. Open Heart. 2017;4(2):e000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diez-Espino J, Buil-Cosiales P, Babio N, et al. Impact of Life’s Simple 7 on the incidence of major cardiovascular events in high-risk Spanish adults in the PREDIMED study cohort. Rev Esp Cardiol (Engl Ed). 2020;73(3):205–211. [DOI] [PubMed] [Google Scholar]
- 48.**.Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282(21):2012–8. [DOI] [PubMed] [Google Scholar]; This study highlighted that a more favorable CVH status in youth and middle age is associated with longevity.
- 49.Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilkins JT, Ning H, Berry J, et al. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308(17):1795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martin SS, Michos ED. Mapping hyperlipidemia in young adulthood to coronary risk: importance of cumulative exposure and how to stay young. Circulation. 2015;131(5):445–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Michos ED, Choi AD. Coronary Artery Disease in Young Adults: A Hard Lesson But a Good Teacher. J Am Coll Cardiol. 2019;74(15):1879–1882. [DOI] [PubMed] [Google Scholar]
- 53.Corlin L, Short MI, Vasan RS, et al. Association of the Duration of Ideal Cardiovascular Health Through Adulthood With Cardiometabolic Outcomes and Mortality in the Framingham Offspring Study. JAMA Cardiol. 2020;5(5):549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perak AM, Ning H, Khan SS, et al. Associations of Late Adolescent or Young Adult Cardiovascular Health With Premature Cardiovascular Disease and Mortality. J Am Coll Cardiol. 2020;76(23):2695–2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu K, Daviglus ML, Loria CM, et al. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125(8):996–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bucholz EM, Gooding HC, de Ferranti SD. Awareness of Cardiovascular Risk Factors in U.S. Young Adults Aged 18–39 Years. Am J Prev Med. 2018;54(4):e67–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Perak AM, Ning H, Khan SS, et al. Cardiovascular Health Among Pregnant Women, Aged 20 to 44 Years, in the United States. J Am Heart Assoc. 2020;9(4):e015123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Petersen EE, Davis NL, Goodman D, et al. Vital Signs: Pregnancy-Related Deaths, United States, 2011–2015, and Strategies for Prevention, 13 States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68(18):423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elder P, Sharma G, Gulati M, Michos ED. Identification of female-specific risk enhancers throughout the lifespan of women to improve cardiovascular disease prevention. Am J Prev Cardiol. 2020;2:100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hauspurg A, Ying W, Hubel CA, et al. Adverse pregnancy outcomes and future maternal cardiovascular disease. Clin Cardiol. 2018;41(2):239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gunderson EP, Sun B, Catov JM, et al. Gestational Diabetes History and Glucose Tolerance After Pregnancy Associated With Coronary Artery Calcium in Women During Midlife: The CARDIA Study. Circulation. 2021;143(10):974–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Crump C, Sundquist J, Howell EA, et al. Pre-Term Delivery and Risk of Ischemic Heart Disease in Women. J Am Coll Cardiol. 2020. July 7;76(1):57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Crump C, Sundquist J, Sundquist K. Preterm delivery and long term mortality in women: national cohort and co-sibling study. BMJ. 2020;370:m2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parikh NI, Gonzalez JM, Anderson CAM, et al. Adverse Pregnancy Outcomes and Cardiovascular Disease Risk: Unique Opportunities for Cardiovascular Disease Prevention in Women: A Scientific Statement From the American Heart Association. Circulation. 2021. March 29:CIR0000000000000961 [online ahead of print]. [DOI] [PubMed] [Google Scholar]
- 65.*.Perak AM, Lancki N, Kuang A, et al. Associations of Maternal Cardiovascular Health in Pregnancy With Offspring Cardiovascular Health in Early Adolescence. JAMA. 2021. February 16;325(7):658–668. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study links the association of maternal CVH with offspring CVH, emphasizing the need to improve CVH of young women before, during and after pregnancy.
- 66.Ogunmoroti O, Osibogun O, Kolade OB, et al. Multiparity is associated with poorer cardiovascular health among women from the Multi-Ethnic Study of Atherosclerosis. Am J Obstet Gynecol. 2019;221(6):631 e1–631 e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Parikh NI, Cnattingius S, Dickman PW, et al. Parity and risk of later-life maternal cardiovascular disease. Am Jeart J. 2010;159(2):215–221 e6. [DOI] [PubMed] [Google Scholar]
- 68.*.Mok Y, Sang Y, Ballew SH, et al. American Heart Association’s Life’s Simple 7 at Middle Age and Prognosis After Myocardial Infarction in Later Life. J Am Heart Assoc. 2018;7(4) e007658. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study examined the CVH in a secondary prevention cohort.
- 69.Olson NC, Cushman M, Judd SE, et al. American Heart Association’s Life’s Simple 7 and risk of venous thromboembolism: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. J Am Heart Assoc. 2015;4(3):e001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.*.Allen NB, Zhao L, Liu L, et al. Favorable Cardiovascular Health, Compression of Morbidity, and Healthcare Costs: Forty-Year Follow-Up of the CHA Study (Chicago Heart Association Detection Project in Industry). Circulation. 2017;135(18):1693–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed that more favorable CVH in middle age is associated with compression of morbidity and reduced healthcare expenditures during subsequent years of Medicare eligibility.
- 71.Thacker EL, Gillett SR, Wadley VG, et al. The American Heart Association Life’s Simple 7 and incident cognitive impairment: The REasons for Geographic And Racial Differences in Stroke (REGARDS) study. J Am Heart Assoc 2014;3(3):e000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gonzalez HM, Tarraf W, Harrison K, et al. Midlife cardiovascular health and 20-year cognitive decline: Atherosclerosis Risk in Communities Study results. Alzheimers Dement. 2018;14(5):579–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Samieri C, Perier MC, Gaye B, et al. Association of Cardiovascular Health Level in Older Age With Cognitive Decline and Incident Dementia. JAMA. 2018;320(7):657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Levine GN. The Mind-Heart-Body Connection. Circulation. 2019;140(17):1363–1365. [DOI] [PubMed] [Google Scholar]
- 75.Levine GN, Cohen BE, Commodore-Mensah Y, et al. Psychological Health, Well-Being, and the Mind-Heart-Body Connection: A Scientific Statement From the American Heart Association. Circulation. 2021;143(10):e763–e783. [DOI] [PubMed] [Google Scholar]
- 76.Kronish IM, Carson AP, Davidson KW, et al. Depressive symptoms and cardiovascular health by the American Heart Association’s definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PloS One. 2012;7(12):e52771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mathews L, Ogunmoroti O, Nasir K, et al. Psychological Factors and Their Association with Ideal Cardiovascular Health Among Women and Men. J Womens Health. 2018;27(5):709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stewart AL, Magnani JW, Barinas-Mitchell E, et al. Social Role Stress, Reward, and the American Heart Association Life’s Simple 7 in Midlife Women: The Study of Women’s Health Across the Nation. J Am Heart Assoc. 2020;9(24):e017489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Espana-Romero V, Artero EG, Lee DC, et al. A prospective study of ideal cardiovascular health and depressive symptoms. Psychosomatics. 2013;54(6):525–35. [DOI] [PubMed] [Google Scholar]
- 80.Osondu CU, Aneni EC, Valero-Elizondo J, et al. Favorable Cardiovascular Health Is Associated With Lower Health Care Expenditures and Resource Utilization in a Large US Employee Population: The Baptist Health South Florida Employee Study. Mayo Clin Proc. 2017:S0025–6196(17)30088–5. [DOI] [PubMed] [Google Scholar]
- 81.Valero-Elizondo J, Salami JA, Ogunmoroti O, et al. Favorable Cardiovascular Risk Profile Is Associated With Lower Healthcare Costs and Resource Utilization: The 2012 Medical Expenditure Panel Survey. Circ Cardiovasc Qual Outcomes. 2016;9(2):143–53. [DOI] [PubMed] [Google Scholar]
- 82.Caleyachetty R, Echouffo-Tcheugui JB, Muennig P, et al. Association between cumulative social risk and ideal cardiovascular health in US adults: NHANES 1999–2006. Int J Cardiol. 2015;191:296–300. [DOI] [PubMed] [Google Scholar]
- 83.Unger E, Diez-Roux AV, Lloyd-Jones DM, et al. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7(4):524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sims M, Kershaw KN, Breathett K, et al. Importance of Housing and Cardiovascular Health and Well-Being: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes. 2020;13(8):e000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Estrella ML, Rosenberg NI, Durazo-Arvizu RA, et al. The association of employment status with ideal cardiovascular health factors and behaviors among Hispanic/Latino adults: Findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). PloS one. 2018;13(11):e0207652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mujahid MS, Moore LV, Petito LC, et al. Neighborhoods and racial/ethnic differences in ideal cardiovascular health (the Multi-Ethnic Study of Atherosclerosis). Health Place. 2017;44:61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Churchwell K, Elkind MSV, Benjamin RM, et al. Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation. 2020;142(24):e454–e468. [DOI] [PubMed] [Google Scholar]
- 88.*.Osibogun O, Ogunmoroti O, Mathews L, et al. Greater Acculturation is Associated With Poorer Cardiovascular Health in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2021;10(8):e019828. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that greater acculturation, such as having lived in U.S. for longer duration, among foreign-born individuals is associated with less favorable CVH.
- 89.Rodriguez F, Echeverria SE, Pentakota SR, et al. Comparison of Ideal Cardiovascular Health Attainment and Acculturation among Asian Americans and Latinos. Ethn Dis. 2019;29(2):287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Thomas SC, Umer A, Commodore-Mensah Y, et al. Length of Residence and Cardiovascular Health among Afro-Caribbean Immigrants in New York City. J Racial Ethn Health Disparities. 2019;6(3):487–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clinl Pharmacol Ther. 2001;69(3):89–95. [DOI] [PubMed] [Google Scholar]
- 92.Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation. 2006;113(19):2335–62. [DOI] [PubMed] [Google Scholar]
- 93.Polonsky TS, Ning H, Daviglus ML, et al. Association of Cardiovascular Health With Subclinical Disease and Incident Events: The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2017;6(3): e004894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Benson EA, Tibuakuu M, Zhao D, et al. Associations of ideal cardiovascular health with GlycA, a novel inflammatory marker: The Multi-Ethnic Study of Atherosclerosis. Clin Cardiol. 2018;41(11):1439–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Osibogun O, Ogunmoroti O, Tibuakuu M, et al. Sex differences in the association between ideal cardiovascular health and biomarkers of cardiovascular disease among adults in the United States: a cross-sectional analysis from the multiethnic study of atherosclerosis. BMJ Open. 2019;9(11):e031414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang YQ, Wang CF, Zhu L, et al. Ideal cardiovascular health and the subclinical impairments of cardiovascular diseases: a cross-sectional study in central south China. BMC Cardiovasc Disord. 2017;17(1):269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xanthakis V, Enserro DM, Murabito JM, et al. Ideal cardiovascular health: associations with biomarkers and subclinical disease and impact on incidence of cardiovascular disease in the Framingham Offspring Study. Circulation. 2014;130(19):1676–83. [DOI] [PubMed] [Google Scholar]
- 98.Benschop L, Schalekamp-Timmermans S, Schelling SJC, et al. Early Pregnancy Cardiovascular Health and Subclinical Atherosclerosis. J Am Heart Assoc. 2019;8(15):e011394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wang L, Niu JY, Zhao ZY, et al. Ideal Cardiovascular Health is Inversely Associated with Subclinical Atherosclerosis: A Prospective Analysis. Biomed Environ Sci. 2019;32(4):260–271. [DOI] [PubMed] [Google Scholar]
- 100.Shpilsky D, Bambs C, Kip K, et al. Association between ideal cardiovascular health and markers of subclinical cardiovascular disease. Clin Cardiol. 2018;41(12):1593–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Enserro DM, Vasan RS, Xanthakis V. Twenty-Year Trends in the American Heart Association Cardiovascular Health Score and Impact on Subclinical and Clinical Cardiovascular Disease: The Framingham Offspring Study. J Am Heart Assoc. 2018;7(11): e008741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fernández-Alvira JM, Fuster V, Pocock S, et al. Predicting Subclinical Atherosclerosis in Low-Risk Individuals: Ideal Cardiovascular Health Score and Fuster-BEWAT Score. J Am Coll Cardiol. 2017;70(20):2463–2473. [DOI] [PubMed] [Google Scholar]
- 103.Talegawkar SA, Jin Y, Kandula NR, et al. Cardiovascular health metrics among South Asian adults in the United States: Prevalence and associations with subclinical atherosclerosis. Prev Med. 2017;96:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gaye B, Mustafic H, Laurent S, et al. Ideal Cardiovascular Health and Subclinical Markers of Carotid Structure and Function: The Paris Prospective Study III. Arterioscler Thromb Vasc Biol. 2016;36(10):2115–24. [DOI] [PubMed] [Google Scholar]
- 105.Laitinen TT, Pahkala K, Magnussen CG, et al. Lifetime measures of ideal cardiovascular health and their association with subclinical atherosclerosis: The Cardiovascular Risk in Young Finns Study. Int J Cardiol. 2015;185:186–91. [DOI] [PubMed] [Google Scholar]
- 106.Robbins JM, Petrone AB, Carr JJ, et al. Association of ideal cardiovascular health and calcified atherosclerotic plaque in the coronary arteries: the National Heart, Lung, and Blood Institute Family Heart Study. Am Heart J. 2015;169(3):371–378 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Saleem Y, DeFina LF, Radford NB, et al. Association of a favorable cardiovascular health profile with the presence of coronary artery calcification. Circ Cardiovasc Imaging. 2014;8(1):e001851. [DOI] [PubMed] [Google Scholar]
- 108.Michos ED, Blaha MJ, Blumenthal RS. Use of the Coronary Artery Calcium Score in Discussion of Initiation of Statin Therapy in Primary Prevention. Mayo Clinic proceedings. 2017;92(12):1831–1841. [DOI] [PubMed] [Google Scholar]
- 109.Sengeløv M, Cheng S, Biering-Sørensen T, et al. Ideal Cardiovascular Health and the Prevalence and Severity of Aortic Stenosis in Elderly Patients. J Am Heart Assoc. 2018;7(3):e007234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Perrot N, Boekholdt SM, Mathieu P, et al. Life’s simple 7 and calcific aortic valve stenosis incidence in apparently healthy men and women. Int J Cardiol. 2018;269:226–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.**.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563–e595. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the most recent U.S. guideline providing recommendations for primary prevention of CVD, which additionally highlights the role of social determinants of health and “risk-enhancing” factors such as adverse pregnancy outcomes in women.
- 112.Amin NP, Martin SS, Blaha MJ, et al. Headed in the right direction but at risk for miscalculation: a critical appraisal of the 2013 ACC/AHA risk assessment guidelines. J Am Coll Cardiol. 2014;63(25 Pt A):2789–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.DeFilippis AP, Young R, McEvoy JW, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38(8):598–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.US Preventive Services Task Force, Krist AH, Davidson KW, et al. Behavioral Counseling Interventions to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults With Cardiovascular Risk Factors: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(20):2069–2075. [DOI] [PubMed] [Google Scholar]
- 116.Khan SS, Greenland P. Comprehensive Cardiovascular Health Promotion for Successful Prevention of Cardiovascular Disease. JAMA. 2020;324(20):2036–2037. [DOI] [PubMed] [Google Scholar]
- 117.Victor RG, Lynch K, Li N, et al. A Cluster-Randomized Trial of Blood-Pressure Reduction in Black Barbershops. N Engl J Med. 2018;378(14):1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]


