Abstract
Background:
It is strongly recommended that adults aged 50-75 years be screened for colorectal cancer (CRC). Recommended screening options include colonoscopy, sigmoidoscopy, computed tomography colonography, guaiac fecal occult blood testing (FOBT), fecal immunochemical testing (FIT), or the more recently introduced FIT-DNA (FIT in combination with a stool DNA test). CRC screening programs can benefit from knowledge of patterns of use by test type and within population subgroups.
Methods:
Using 2018 National Health Interview Survey data, we examined CRC screening test use for adults aged 50-75 years (N=10,595). We also examined time trends in CRC screening test use from 2010-2018.
Results:
In 2018, an estimated 66.9% of U.S. adults aged 50-75 years had a CRC screening test within recommended time intervals. However, the prevalence was less than 50% among those aged 50-54 years, those without a usual source of health care, those with no doctor visits in the past year, and those who were uninsured. The test types most commonly used within recommended time intervals were colonoscopy within 10 years (61.1%), FOBT or FIT in the past year (8.8%), and FIT-DNA within 3 years (2.7%). After age-standardization to the 2010 census population, the percentage up-to-date with CRC screening increased from 61.2% in 2015 to 65.3% in 2018, driven by increased use of stool testing, including FIT-DNA.
Conclusions:
These results show some progress, driven by a modest increase in stool testing. However, CRC testing remains low in many population subgroups.
Impact:
These results can inform efforts to achieve population CRC screening goals.
Keywords: screening, colorectal cancer, colonoscopy, stool DNA, fecal immunochemical test
Introduction
Screening may substantially reduce the incidence of and mortality from colorectal cancer (CRC), the second leading cause of cancer-related death in the United States (U.S.) (1,2). The U.S. Preventive Services Task Force (USPSTF) recommends that adults aged 50-75 years be screened for CRC (3). According to the most recent recommendation statement from 2016, average risk adults aged 50-75 years have met the screening recommendation if they have had a colonoscopy within 10 years, a guaiac fecal occult blood test (FOBT) or fecal immunochemical test (FIT) within one year, a FIT-DNA test within 3 years, or a sigmoidoscopy or computed tomography (CT) colonography within 5 years (3). In 2015, an estimated 61% of adults aged 50-75 years were up-to-date with CRC screening, an increase from 52% in 2008 (4). However, CRC screening prevalence remained well below the Healthy People 2020 target of 70.5% (5) and the National Colorectal Cancer Roundtable (NCCRT) target of 80% by 2018 (6).
We determined the prevalence of CRC screening test use within recommended intervals in 2018 using self-reported data from participants aged 50-75 years in the 2018 National Health Interview Survey (NHIS), a nationally representative survey of U.S. adults (7). We examined use of CRC screening tests overall and use of specific tests including colonoscopy, stool tests (FOBT, FIT, and FIT-DNA), sigmoidoscopy, and CT colonography. FIT-DNA (FIT in combination with a stool DNA test) is of particular interest because it is the most recently approved test and its prevalence of use nationwide is unknown. We also examined use of CRC screening tests by sociodemographic and health care access factors. In addition, we examined time trends in use of specific types of CRC screening tests using NHIS data from 2010 to 2018, to understand how use of different tests contributed to overall changes in CRC screening prevalence.
Methods
Study population
The NHIS is an in-person survey of a representative sample of the civilian, non-institutionalized U.S. population, conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) (7). The sample design is a probability design that permits representative sampling of households and noninstitutional group quarters (e.g., homeless shelters, rooming houses, and group homes). One adult is randomly selected from each participating family to complete the sample adult questionnaire. The final sample adult response rates were 60.8%, 61.2%, 55.2%, and 53.1% in 2010, 2013, 2015, and 2018, respectively (7-10).
The study sample included adults aged 50-75 years without a personal history of CRC and with complete information for at least one CRC screening test. The total sample size after these exclusions was 10,595 for 2018. For 2010, 2013, and 2015, total sample sizes were 8,825, 12,916, and 12,524, respectively.
CRC screening test use
In 2018, respondents were asked separate questions about whether they had ever had a sigmoidoscopy, colonoscopy, CT colonography or virtual colonoscopy, FOBT or FIT, and Cologuard® or FIT-DNA. If the respondent reported that a FIT they had was part of a FIT-DNA test, the FIT was not included in the results for use of FOBT or FIT. For each test, respondents were asked about the time since their most recent test. Descriptions of each test were provided to respondents. To assist in differentiating between FOBT or FIT and the newer Cologuard® or FIT-DNA, the description of the latter test included the widely advertised brand name Cologuard® and explained that the test was shipped to the respondent’s home in a box that includes a container for the stool sample.
The USPSTF CRC screening recommendation for each time period was used to determine whether an individual was up-to-date (3,11). For 2018, up-to-date CRC screening test use was defined as use of an FOBT or FIT within the past year, colonoscopy within the past 10 years, CT colonography or sigmoidoscopy within the past 5 years, or a FIT-DNA test within the past 3 years. For 2010-2015, it was defined as use of an FOBT or FIT within the past year, colonoscopy within the past 10 years, or the combination of sigmoidoscopy within the past 5 years and FOBT or FIT within the past 3 years. For 2010, 2013, and 2015, questions about Cologuard® or FIT-DNA were not asked. However, Cologuard® was likely rarely used before 2015 since it was not approved by the FDA until August 2014 (12), was not covered by Medicare until October 2015 (13), and was not added to the USPSTF’s recommended screening options until 2016 (3). CRC tests performed for any indication were included in the analysis because the reported indication for a CRC test may not always be accurate (14,15), and even if a test was conducted for non-screening purposes, the person receiving the test can be considered effectively screened if the test was conducted within the recommended time interval. This assumption was similar to the assumption used for the Healthy People 2020 measures and by the NCCRT (5,6).
Covariates
For primary analyses, CRC screening test use in 2018 was examined by sociodemographic factors including age, sex, race and ethnicity, education, marital status, family income as a percentage of the federal poverty threshold (using imputed income files), birthplace in the U.S., U.S. residential region, having a usual source of health care other than the emergency room, health status, number of visits to a doctor or other health professional in the past year, and health insurance coverage. Health insurance was categorized differently for adults aged 50-64 years and 65-75 years because Medicare coverage typically starts at age 65 years. For adults aged 50-64 years, categories included: 1) private insurance (including exchange-based coverage), with or without other coverage; 2) Medicaid or other state-sponsored health plans (without private insurance); 3) other coverage (including military coverage, Medicare, or coverage by other government programs, and excluding anyone who also had private insurance, Medicaid, or a state-sponsored health plan); and 4) uninsured (including only Indian Health Service coverage or a single service plan that only pays for one type of service such as accidents or dental care). For adults aged 65-75 years, health insurance categories were: 1) private insurance, with or without traditional Medicare (if they had Medicare Advantage and also reported private coverage, they were placed in the Medicare Advantage category); 2) dual eligible (dually enrolled in both Medicare and Medicaid or other state-sponsored health plans, without private coverage); 3) Medicare Advantage (plans offered by private companies approved and paid by Medicare to cover Medicare benefits); 4) traditional Medicare coverage only (without private insurance or Medicaid); 5) other coverage (includes Medicaid without traditional Medicare or private coverage, or military coverage with or without traditional Medicare); and 6) uninsured (including only Indian Health Service coverage or a single service plan).
Statistical analysis
Estimates of CRC screening test use were calculated using the sample adult weights and are representative of the civilian, non-institutionalized U.S. adult population. Data weighting procedures are described in detail elsewhere (7,16). Estimates not meeting NCHS data presentation standards for proportions due to small sample sizes were suppressed (17). All analyses were performed using SAS (version 9.4, SAS Institute Inc.) and SAS-callable SUDAAN (version 11.0.3, Research Triangle Institute). P-values for overall associations were calculated using Wald F tests. Linear tests of contrast (t-tests) were used to test for pairwise differences and for differences over time. Statistical significance was defined as a p-value <0.05.
Because sigmoidoscopy and CT colonography were infrequently used, we examined their use only by sex and broad age groups. For associations with characteristics other than sex and age, we did not examine use of FOBT/FIT and FIT-DNA separately but instead analyzed a combined variable for any stool test use.
Adjusted percentages (predictive margins) for screening test use were computed from multivariable logistic regression models with predicted marginal probabilities. Separate models were created to examine any screening test use, colonoscopy use, and any stool test use. Predictive margins are a type of direct standardization that averages the predicted values from the logistic regression models over the covariate distribution in the study population (18). The predictive margin for a specific category of a variable represents the predicted prevalence if everyone in the sample had been in that category. The results in Table 3 for the age and health insurance variables were derived from separate age-specific models (50-64 years, 65-75 years) because the available health insurance options differ by age. The results for all other variables in Table 3 were estimated in a model including all adults aged 50-75 years.
Table 3.
Adjusted percentage of adults aged 50-75 up-to-date with CRC screening by sociodemographic and health care access characteristics, National Health Interview Survey, 2018.
| Any CRC screening test within recommended timea |
Colonoscopy within 10 years |
Any stool test (FOBT/FIT or FIT-DNA) within recommended timea |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | %b | 95% CI | P | %b | 95% CI | P | %b | 95% CI | P | |
| Sex | 0.03 | 0.13 | 0.06 | |||||||
| Male | 4,846 | 68.4 | (66.8-69.9) | 62.1 | (60.5-63.7) | 12.0 | (10.9-13.2) | |||
| Female | 5,749 | 66.0 | (64.6-67.5) | 60.5 | (58.9-62.0) | 10.6 | (9.6-11.7) | |||
| Age (50-64 years) | <0.001 | <0.001 | 0.55 | |||||||
| 50-54 | 1,886 | 49.9 | (47.3-52.5) | 43.5 | (40.7-46.3) | 9.1 | (7.6-11.0) | |||
| 55-59 | 2,145 | 65.7 | (63.3-68.1) | 59.8 | (57.2-62.3) | 10.3 | (8.8-12.1) | |||
| 60-64 | 2,263 | 70.2 | (67.9-72.4) | 64.7 | (62.3-67.1) | 10.2 | (8.8-11.8) | |||
| Age (65-75 years) | 0.02 | 0.009 | 0.48 | |||||||
| 65-69 | 2,230 | 75.6 | (73.5-77.6) | 69.4 | (67.1-71.5) | 14.3 | (12.7-16.0) | |||
| 70-75 | 2,071 | 78.8 | (76.7-80.7) | 73.4 | (71.1-75.5) | 13.4 | (11.8-15.3) | |||
| Race/Ethnicity | 0.006 | 0.02 | 0.02 | |||||||
| Non-Hispanic White | 7,863 | 66.4 | (65.0-67.8) | 60.6 | (59.1-62.1) | 10.4 | (9.5-11.3) | |||
| Non-Hispanic Black | 1,210 | 70.6 | (67.4-73.5) | 64.9 | (61.5-68.2) | 13.9 | (11.2-17.1) | |||
| Hispanic | 958 | 70.5 | (66.6-74.2) | 63.8 | (59.5-67.8) | 13.8 | (11.2-17.0) | |||
| Non-Hispanic Asian | 422 | 61.1 | (55.4-66.5) | 55.3 | (49.5-61.0) | 11.8 | (8.6-16.0) | |||
| Non-Hispanic other races | 142 | 66.0 | (58.2-73.1) | 63.4 | (54.5-71.4) | -- c | -- c | |||
| Education | <0.001 | <0.001 | 0.80 | |||||||
| Less than high school graduate | 1,132 | 60.6 | (56.9-64.1) | 55.4 | (51.6-59.1) | 10.2 | (8.2-12.7) | |||
| High school graduate/GED | 2,704 | 64.7 | (62.5-66.8) | 58.9 | (56.7-61.1) | 11.6 | (10.2-13.1) | |||
| Some college/associate’s degree | 3,218 | 67.2 | (65.2-69.0) | 61.2 | (59.3-63.2) | 11.3 | (10.0-12.8) | |||
| Bachelor’s degree or higher | 3,499 | 71.2 | (69.3-72.9) | 65.0 | (63.0-66.9) | 11.3 | (9.9-12.9) | |||
| Family income (% of federal poverty threshold) | 0.002 | <0.001 | 0.59 | |||||||
| ≤138% | 1,902 | 63.4 | (59.8-66.7) | 55.1 | (51.4-58.8) | 12.0 | (10.0-14.4) | |||
| >138 - <250% | 1,899 | 64.1 | (61.3-66.8) | 56.3 | (53.5-58.9) | 11.9 | (9.9-14.1) | |||
| 250 - <400% | 2,057 | 65.2 | (62.5-67.7) | 59.4 | (56.7-62.1) | 10.6 | (8.9-12.5) | |||
| 400 - <800% | 3,110 | 68.9 | (66.8-70.9) | 64.2 | (62.0-66.3) | 10.6 | (9.3-11.9) | |||
| ≥800% | 1,627 | 72.4 | (69.6-75.0) | 67.8 | (64.9-70.7) | 12.0 | (10.0-14.3) | |||
| Marital status | <0.001 | <0.001 | 0.93 | |||||||
| Never married | 1,175 | 61.2 | (57.7-64.5) | 54.9 | (51.3-58.4) | 11.5 | (9.2-14.3) | |||
| Married/living with partner | 5,714 | 68.9 | (67.6-70.3) | 63.1 | (61.6-64.5) | 11.3 | (10.3-12.4) | |||
| Widowed/divorced/separated | 3,684 | 64.0 | (61.9-66.0) | 58.2 | (56.1-60.2) | 11.1 | (9.8-12.5) | |||
| Born in U.S. | 0.006 | <0.001 | 0.13 | |||||||
| Yes | 9,108 | 68.1 | (66.8-69.4) | 62.5 | (61.1-63.9) | 10.9 | (10.0-11.8) | |||
| No | 1,482 | 62.8 | (59.4-66.1) | 55.6 | (52.0-59.1) | 12.8 | (10.7-15.2) | |||
| Region | 0.03 | 0.002 | <0.001 | |||||||
| Northeast | 1,790 | 69.4 | (66.8-71.9) | 65.8 | (63.0-68.4) | 8.9 | (7.4-10.7) | |||
| Midwest | 2,438 | 67.7 | (65.5-69.7) | 62.2 | (59.7-64.6) | 9.9 | (8.3-11.7) | |||
| South | 3,944 | 65.1 | (63.3-66.9) | 60.6 | (58.7-62.5) | 9.3 | (8.2-10.6) | |||
| West | 2,423 | 68.0 | (65.7-70.2) | 57.6 | (55.2-60.0) | 17.5 | (15.4-19.7) | |||
| Health status | 0.61 | 0.67 | 0.25 | |||||||
| Excellent/very good/good | 8,656 | 67.0 | (65.7-68.2) | 61.1 | (59.8-62.5) | 11.0 | (10.1-12.0) | |||
| Fair/poor | 1,934 | 67.8 | (65.1-70.4) | 61.8 | (58.9-64.6) | 12.2 | (10.5-14.1) | |||
| Usual source of health care other than ER | <0.001 | <0.001 | 0.008 | |||||||
| No | 856 | 50.7 | (46.1-55.4) | 46.7 | (41.8-51.6) | 6.0 | (3.7- 9.7) | |||
| Yes | 9,738 | 68.4 | (67.2-69.6) | 62.3 | (61.0-63.6) | 11.5 | (10.7-12.4) | |||
| Number of doctor visits in past year | <0.001 | <0.001 | <0.001 | |||||||
| 0 | 1,180 | 44.6 | (40.9-48.3) | 41.5 | (37.8-45.2) | 5.1 | (3.5- 7.5) | |||
| 1 | 1,581 | 62.6 | (59.8-65.3) | 55.5 | (52.6-58.3) | 10.3 | (8.6-12.2) | |||
| ≥2 | 7,811 | 71.5 | (70.2-72.7) | 65.3 | (63.9-66.7) | 12.2 | (11.3-13.2) | |||
| Health insurance (ages 50-64) | <0.001 | <0.001 | 0.01 | |||||||
| Private | 4,388 | 62.2 | (60.4-64.0) | 56.6 | (54.7-58.5) | 9.5 | (8.3-10.7) | |||
| Medicaid | 749 | 62.6 | (57.8-67.1) | 55.9 | (51.0-60.6) | 10.8 | (8.1-14.3) | |||
| Other coverage | 522 | 71.4 | (66.9-75.6) | 62.5 | (57.6-67.1) | 14.5 | (11.2-18.5) | |||
| Uninsured | 614 | 49.6 | (43.4-55.7) | 43.9 | (37.9-50.1) | -- c | -- c | |||
| Health insurance (ages 65-75) | <0.001 | 0.10 | <0.001 | |||||||
| Private | 1,813 | 75.6 | (73.0-78.0) | 71.7 | (69.1-74.2) | 10.6 | (9.0-12.5) | |||
| Dual eligible | 329 | 76.4 | (70.4-81.6) | 71.2 | (64.7-77.0) | 15.5 | (11.0-21.5) | |||
| Medicare Advantage | 1,022 | 82.7 | (80.1-85.0) | 71.7 | (68.5-74.7) | 21.1 | (18.3-24.1) | |||
| Traditional Medicare only | 700 | 70.6 | (66.5-74.3) | 67.4 | (63.3-71.3) | 10.3 | (7.9-13.4) | |||
| Other coverage | 408 | 81.7 | (76.9-85.7) | 75.8 | (70.9-80.2) | 13.0 | (9.8-17.1) | |||
| Uninsured | -- c | -- c | -- c | -- c | -- c | -- c | -- c | |||
Any screening test within the recommended time period (up-to-date with CRC screening) defined as either colonoscopy within the past 10 years, CT colonography or sigmoidoscopy within the past 5 years, FOBT or FIT within the past year, or FIT-DNA within the past 3 years.
Adjusted percentages (predictive margins) were computed from multivariable logistic regression models with predicted marginal probabilities, controlling for all variables in Table 3. The results for the age and health insurance variables were derived from separate age-specific models (50-64 years, 65-75 years). The results for all other variables in Table 3 were estimated in a model including all adults aged 50-75 years.
Estimates suppressed because they did not meet National Center for Health Statistics reliability standards.
NHIS data from 2010, 2013, 2015 and 2018 were used to examine differences across years in percentages of adults up-to-date with screening, according to USPSTF recommendations in effect for each year. Percentages in the figures were age-standardized to the 2010 U.S. census population in 5-year age groups (19) to make results comparable across NHIS surveys from different years. Percentages in the tables from the 2018 NHIS were not age-standardized to the 2010 population to better reflect the true U.S. age distribution in 2018.
Results
CRC screening in 2018 by test type and sociodemographic characteristics
Table 1 shows the unadjusted, weighted percentage of adults aged 50-75 years who were up-to-date with CRC screening overall and for each test type, by sex and age. Overall, 66.9% were up-to-date with CRC screening in 2018. The most commonly used CRC screening test was colonoscopy (61.1% within the past 10 years). Other CRC tests were less frequently used (8.8% FOBT or FIT within the past year, 2.7% FIT-DNA within the past 3 years, 2.4% sigmoidoscopy within the past 5 years, 1.0% CT colonography within the past 5 years). Males were slightly more likely than females to have had an FOBT or FIT (males 9.5% (95% CI 8.5-10.6), females 8.1% (95% CI 7.3-9.1)). Adults aged 65-75 years were more likely than adults aged 50-64 years to be up-to-date overall and to have used each type of CRC test except CT colonography.
Table 1.
Percentage of adults aged 50-75 up-to-date with CRC screening by test type, sex, and age, National Health Interview Survey, 2018.
| Any CRC screening testa |
Colonoscopy within 10 years |
FOBT/FITb within 1 year |
FIT-DNA within 3 years |
Sigmoidoscopy within 5 years |
CT colonography within 5 years |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % (95% CI) |
P | % (95% CI) |
P | % (95% CI) |
P | % (95% CI) |
P | % (95% CI) |
P | % (95% CI) |
P | |
| Total | 10,595 | 66.9 (65.8-68.1) |
61.1 (59.9-62.3) |
8.8 (8.1-9.5) |
2.7 (2.4-3.2) |
2.4 (2.1-2.8) |
1.0 (0.8-1.3) |
||||||
| Sex | 0.43 | 0.61 | 0.04 | 0.19 | 0.09 | 0.11 | |||||||
| Male | 4,846 | 67.4 (65.8-69.0) |
61.4 (59.8-63.1) |
9.5 (8.5-10.6) |
2.5 (2.0-3.1) |
2.7 (2.2-3.4) |
1.2 (0.9-1.7) |
||||||
| Female | 5,749 | 66.5 (64.9-68.1) |
60.8 (59.1-62.5) |
8.1 (7.3-9.1) |
3.0 (2.5-3.5) |
2.1 (1.6-2.6) |
0.8 (0.6-1.2) |
||||||
| Age (years) | <0.001 | <0.001 | <0.001 | <0.001 | 0.01 | 0.17 | |||||||
| 50-64 | 6,294 | 61.8 (60.2-63.3) |
55.9 (54.3-57.5) |
7.9 (7.0-8.8) |
2.2 (1.8-2.8) |
2.1 (1.7-2.5) |
0.9 (0.7-1.2) |
||||||
| 65-75 | 4,301 | 76.9 (75.4-78.4) |
71.1 (69.5-72.8) |
10.5 (9.4-11.7) |
3.7 (3.1-4.5) |
3.0 (2.4-3.7) |
1.2 (0.9-1.7) |
||||||
Any CRC screening test within the recommended time period (up-to-date with CRC screening) defined as either colonoscopy within the past 10 years, CT colonography or sigmoidoscopy within the past 5 years, FOBT or FIT within the past year, or FIT-DNA within the past 3 years.
Use of FOBT/FIT does not include a FIT that the respondent reported was conducted as part of a FIT-DNA test.
Table 2 shows the weighted percentages of adults aged 50-75 years who had any CRC screening test, colonoscopy, or any stool test (FOBT/FIT or FIT-DNA) within the recommended time intervals, by sociodemographic and health care access factors. In these unadjusted analyses, use of any CRC screening test was lower for those who were younger, had less education or lower family income, were born outside the U.S., did not have a usual source of health care, or had fewer doctor visits. Use of any CRC screening test was statistically significantly lower for non-Hispanic Black, non-Hispanic Asian, and Hispanic (vs. non-Hispanic White) adults, for those who were never married (compared with other marital status groups), and for those who lived in the South and West (vs. the Northeast). Among adults aged 50-64 years, those who were uninsured had lower CRC screening test use than each of the insured groups, and those with Medicaid coverage had lower use than those with private insurance or those in the “other coverage” category. Among adults aged 65-75 years, those with dual-eligible health coverage or with traditional Medicare only had lower use than those with private insurance, Medicare Advantage, or those in the “other coverage” category.
Table 2.
Percentage of adults aged 50-75 up-to-date with CRC screening by sociodemographic and health care access characteristics, National Health Interview Survey, 2018.
| Any CRC screening test within recommended timea |
Colonoscopy within 10 years |
Any stool test (FOBT/FIT or FIT-DNA) within recommended timea |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | 95% CI | P | % | 95% CI | P | % | 95% CI | P | |
| Total | 10,595 | 66.9 | (65.8-68.1) | 61.1 | (59.9-62.3) | 11.2 | (10.4-12.1) | |||
| Sex | 0.43 | 0.61 | 0.25 | |||||||
| Male | 4,846 | 67.4 | (65.8-69.0) | 61.4 | (59.8-63.1) | 11.7 | (10.6-12.8) | |||
| Female | 5,749 | 66.5 | (64.9-68.1) | 60.8 | (59.1-62.5) | 10.8 | (9.8-11.9) | |||
| Age (years) | <0.001 | <0.001 | <0.001 | |||||||
| 50-54 | 1,886 | 48.1 | (45.4-50.9) | 42.0 | (39.2-44.9) | 8.8 | (7.3-10.6) | |||
| 55-59 | 2,145 | 65.2 | (62.7-67.5) | 59.3 | (56.7-61.9) | 10.2 | (8.7-12.0) | |||
| 60-64 | 2,263 | 72.1 | (69.7-74.4) | 66.5 | (64.0-69.0) | 10.6 | (9.1-12.2) | |||
| 65-69 | 2,230 | 74.9 | (72.7-77.0) | 68.9 | (66.7-71.2) | 13.9 | (12.3-15.6) | |||
| 70-75 | 2,071 | 79.2 | (77.1-81.1) | 73.6 | (71.3-75.8) | 13.8 | (12.2-15.7) | |||
| Race/Ethnicity | <0.001 | <0.001 | 0.002 | |||||||
| Non-Hispanic White | 7,863 | 69.5 | (68.2-70.8) | 64.2 | (62.8-65.6) | 10.0 | (9.2-10.9) | |||
| Non-Hispanic Black | 1,210 | 65.5 | (62.1-68.8) | 60.0 | (56.4-63.5) | 12.6 | (10.3-15.4) | |||
| Hispanic | 958 | 57.6 | (53.5-61.6) | 49.2 | (45.3-53.1) | 15.1 | (12.5-18.2) | |||
| Non-Hispanic Asian | 422 | 58.0 | (52.0-63.7) | 49.3 | (43.4-55.2) | 15.5 | (11.8-20.0) | |||
| Non-Hispanic other races | 142 | 59.1 | (48.1-69.2) | 54.5 | (41.7-66.7) | -- b | --b | |||
| Education | <0.001 | <0.001 | 0.75 | |||||||
| Less than high school graduate | 1,132 | 54.2 | (50.7-57.8) | 47.4 | (43.6-51.2) | 12.5 | (10.2-15.2) | |||
| High school graduate/GED | 2,704 | 63.5 | (61.3-65.7) | 57.8 | (55.6-60.1) | 11.1 | (9.7-12.5) | |||
| Some college/associate's degree | 3,218 | 67.7 | (65.7-69.7) | 61.7 | (59.6-63.7) | 11.2 | (9.9-12.7) | |||
| Bachelor’s degree or higher | 3,499 | 73.5 | (71.7-75.2) | 68.0 | (66.1-69.9) | 11.0 | (9.6-12.5) | |||
| Family income (% of federal poverty threshold) | <0.001 | <0.001 | 0.05 | |||||||
| ≤138% | 1,902 | 57.0 | (53.9-60.0) | 48.8 | (45.7-51.9) | 13.4 | (11.6-15.5) | |||
| >138 - <250% | 1,899 | 59.9 | (56.8-62.8) | 52.5 | (49.6-55.3) | 12.0 | (10.2-14.2) | |||
| 250 - <400% | 2,057 | 66.2 | (63.3-68.9) | 60.5 | (57.6-63.3) | 10.8 | (9.1-12.7) | |||
| 400 - <800% | 3,110 | 70.7 | (68.6-72.7) | 66.0 | (63.9-68.1) | 10.1 | (9.0-11.4) | |||
| ≥800% | 1,627 | 76.3 | (73.8-78.7) | 71.7 | (68.9-74.4) | 11.0 | (9.1-13.2) | |||
| Marital status | <0.001 | <0.001 | 0.88 | |||||||
| Never married | 1,175 | 55.8 | (52.2-59.4) | 49.1 | (45.4-52.7) | 11.9 | (9.5-14.7) | |||
| Married/living with partner | 5,714 | 69.6 | (68.2-71.0) | 64.0 | (62.5-65.4) | 11.2 | (10.2-12.2) | |||
| Widowed/divorced/separated | 3,684 | 62.8 | (60.8-64.8) | 56.8 | (54.8-58.7) | 11.2 | (10.0-12.5) | |||
| Born in U.S. | <0.001 | <0.001 | 0.003 | |||||||
| Yes | 9,108 | 69.2 | (68.0-70.4) | 63.9 | (62.6-65.2) | 10.6 | (9.8-11.4) | |||
| No | 1,482 | 56.8 | (53.7-59.8) | 48.7 | (45.7-51.8) | 14.0 | (12.1-16.3) | |||
| Region | 0.002 | <0.001 | <0.001 | |||||||
| Northeast | 1,790 | 71.1 | (68.2-73.8) | 67.5 | (64.5-70.3) | 8.9 | (7.4-10.6) | |||
| Midwest | 2,438 | 67.6 | (65.3-69.9) | 62.5 | (59.9-65.0) | 9.1 | (7.6-10.8) | |||
| South | 3,944 | 64.5 | (62.6-66.4) | 60.1 | (58.1-62.0) | 9.4 | (8.3-10.6) | |||
| West | 2,423 | 66.8 | (64.2-69.3) | 56.2 | (53.6-58.9) | 18.1 | (16.1-20.4) | |||
| Health status | 0.59 | 0.64 | 0.001 | |||||||
| Excellent/very good/good | 8,656 | 66.8 | (65.5-68.1) | 61.2 | (59.9-62.6) | 10.6 | (9.8-11.5) | |||
| Fair/poor | 1,934 | 67.6 | (65.0-70.1) | 60.5 | (57.7-63.2) | 14.0 | (12.2-16.0) | |||
| Usual source of health care other than ER | <0.001 | <0.001 | <0.001 | |||||||
| No | 856 | 29.4 | (25.6-33.5) | 27.1 | (23.5-31.1) | 3.8 | (2.3-6.0) | |||
| Yes | 9,738 | 70.2 | (69.0-71.3) | 64.0 | (62.7-65.3) | 11.9 | (11.0-12.8) | |||
| Number of doctor visits in past year | <0.001 | <0.001 | <0.001 | |||||||
| 0 | 1,180 | 31.9 | (28.8-35.2) | 29.6 | (26.5-32.8) | 4.2 | (2.9-6.0) | |||
| 1 | 1,581 | 62.0 | (59.0-64.8) | 55.0 | (51.9-58.0) | 10.1 | (8.5-11.9) | |||
| ≥2 | 7,811 | 73.5 | (72.2-74.7) | 67.4 | (66.0-68.7) | 12.6 | (11.6-13.6) | |||
| Health insurance (ages 50-64) | <0.001 | <0.001 | <0.001 | |||||||
| Private | 4,388 | 65.3 | (63.6-67.0) | 60.1 | (58.2-62.0) | 9.3 | (8.2-10.4) | |||
| Medicaid | 749 | 57.6 | (53.4-61.7) | 48.1 | (43.9-52.4) | 13.9 | (11.1-17.4) | |||
| Other coverage | 522 | 73.3 | (68.5-77.7) | 63.8 | (58.7-68.7) | 15.9 | (12.5-20.0) | |||
| Uninsured | 614 | 30.1 | (25.6-35.1) | 26.2 | (21.9-31.0) | -- b | -- b | |||
| Health insurance (ages 65-75) | <0.001 | <0.001 | <0.001 | |||||||
| Private | 1,813 | 78.3 | (76.0-80.5) | 74.9 | (72.5-77.2) | 10.0 | (8.6-11.7) | |||
| Dual eligible | 329 | 70.3 | (64.1-75.8) | 63.6 | (57.2-69.6) | 18.4 | (13.9-24.1) | |||
| Medicare Advantage | 1,022 | 83.2 | (80.6-85.5) | 71.8 | (68.3-75.0) | 22.4 | (19.5-25.6) | |||
| Traditional Medicare only | 700 | 66.0 | (61.7-69.9) | 63.1 | (58.9-67.1) | 9.6 | (7.4-12.3) | |||
| Other coverage | 408 | 78.8 | (73.2-83.5) | 73.1 | (67.3-78.1) | 13.0 | (9.8-17.1) | |||
| Uninsured | -- b | -- b | -- b | -- b | -- b | -- b | -- b | -- b | ||
Any CRC screening test within the recommended time period (up-to-date with CRC screening) defined as either colonoscopy within the past 10 years, CT colonography or sigmoidoscopy within the past 5 years, FOBT or FIT within the past year, or FIT-DNA within the past 3 years.
Estimates suppressed because they did not meet National Center for Health Statistics reliability standards.
The subgroups with the lowest estimated percentages of screening test use (less than 50%) were those aged 50-54 years (48.1%), and those without a usual source of health care (29.4%), with no doctor visits in the past year (31.9%), or who were aged 50-64 years and uninsured (30.1%). The subgroups with the highest estimated percentages of screening test use (75% or greater) were the oldest age group (ages 70-75 years: 79.2%), those with family income 800% or more of the federal poverty threshold (76.3%), and adults aged 65-75 years with private health insurance (78.3%), Medicare Advantage (83.2%), or other health coverage (78.8%).
Since colonoscopy was the most commonly used screening test, the factors significantly associated with use of colonoscopy within the past 10 years were generally similar to the factors associated with any CRC screening test use.
For some of the factors examined, associations with stool test use were different than associations with colonoscopy or any screening test use. Use of any stool test was statistically significantly higher for Hispanic adults and non-Hispanic Asian adults compared with non-Hispanic White adults. Use of any stool test was also higher for those who were not born in the U.S., had fair/poor health status, lived in the West, those aged 50-64 years with Medicaid or in the “other coverage” category (vs. private insurance), and those aged 65-75 years with dual-eligible health coverage or Medicare Advantage (vs. private insurance). Education and marital status were not associated with stool test use. The subgroups with the highest estimated percentages of stool test use (18% or greater) were those living in the West (18.1%), and those aged 65-75 years with Medicare Advantage (22.4%) or dual-eligible health coverage (18.4%).
Table 3 shows results from predictive marginal models adjusted for all factors in the table. Unlike the unadjusted results in Table 2, the multivariable-adjusted results do not estimate the actual prevalence of CRC screening test use within population subgroups, and therefore may sometimes be less appropriate for guiding public health practice. However, the multivariable-adjusted results describe the associations of each factor independent of the other factors in the model. In these multivariable-adjusted analyses, use of any CRC screening test was associated with the same factors as in the unadjusted analyses and was also associated with sex, with females slightly less likely to have had a CRC screening test than males. For race/ethnicity, the pattern of association was different in the adjusted model than in the unadjusted analysis. In the adjusted model, non-Hispanic Black adults had higher use of CRC screening tests than non-Hispanic White adults (p=0.01), unlike in the unadjusted analysis. There was also a suggestion of higher CRC screening test use in Hispanic adults than in non-Hispanic White adults, but this was not statistically significant (p=0.06). The changes in the results for non-Hispanic Black adults and Hispanic adults after multivariable adjustment were primarily due to the effects of adjustment for education and family income, with adjustment for having been born in the U.S. also having an effect for Hispanic adults. There were some differences in associations with health insurance in the adjusted model compared with the unadjusted analysis. Among adults aged 50-64 years, those with Medicaid coverage and those with private insurance had similar CRC screening test use. Among adults aged 65-75 years, those with dual-eligible health coverage and those with private insurance had similar CRC screening test use.
Associations between colonoscopy and most variables were similar in the adjusted and unadjusted analyses. However, there were some differences between the adjusted and unadjusted analyses for associations with race/ethnicity and health insurance. In the adjusted models, non-Hispanic Black adults had statistically significantly higher use of colonoscopy than non-Hispanic White adults (p=0.02). Among adults aged 50-64 years, those with Medicaid coverage and those with private insurance had similar colonoscopy use. In the adjusted model for colonoscopy, the overall association with health insurance among adults aged 65-75 years was not statistically significant, unlike in the unadjusted analysis. Among adults aged 65-75 years, those with dual-eligible health coverage and those with private insurance had similar colonoscopy use.
In the adjusted model for stool test use, most associations were similar to those in the unadjusted analysis. However, age, having been born in the U.S., and health status were no longer statistically significantly associated with stool test use. Stool test use was higher in non-Hispanic Black adults than non-Hispanic White adults (p=0.02) in the adjusted model, while in the unadjusted analysis there was a suggestion of higher stool test use for non-Hispanic Black adults but it was not statistically significant (p=0.06). In the adjusted model, non-Hispanic Asian adults did not have significantly higher stool test use than non-Hispanic White adults, unlike in the unadjusted analysis.
Although this analysis focused primarily on sociodemographic factors, we also conducted exploratory analyses of some psychosocial and medical factors, adjusted for age and sex in predictive marginal models (Supplementary Table S1). Respondents who reported living in a close-knit neighborhood or who had a larger number of comorbid conditions had higher overall screening test use and higher colonoscopy use. Respondents who had diabetes or had a larger number of comorbid conditions had higher stool test use.
Trends in CRC screening test use by test type and race/ethnicity, 2010-2018
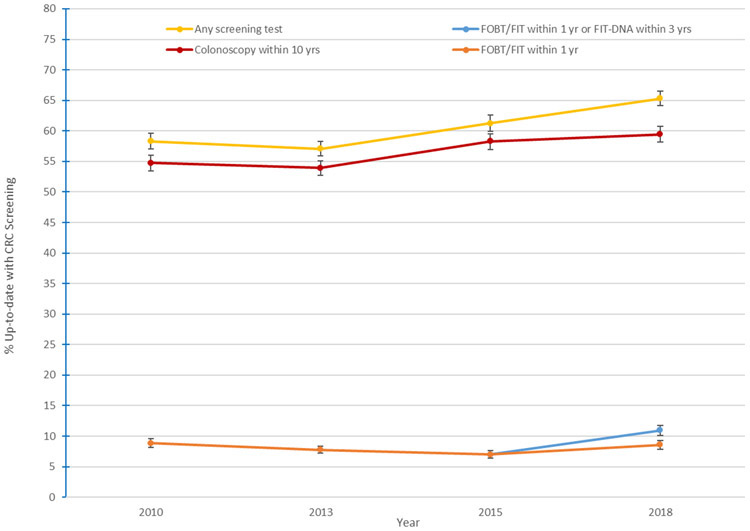
Figure 1 shows trends from 2010 to 2018 in CRC screening test use, overall and by type of test. Percentages are age-standardized to the 2010 census. Because of this age standardization, the percentages in the figures for 2018 are slightly different than the percentages in the tables. CRC screening test use increased significantly over time, from 58.3% in 2010 to 61.2% in 2015 to 65.3% in 2018. Although colonoscopy use increased significantly from 2010 to 2018, there was no significant difference in use from 2015 to 2018 (58.3% in 2015, 59.5% in 2018). However, there was a statistically significant increase in stool test use from 2015 to 2018 (7.0% to 10.9%) (p<0.001). This increase was partly driven by FIT-DNA (Cologuard®) use. However, the increase was statistically significant even if FIT-DNA use was not considered, with use of FOBT/FIT increasing from 7.0% in 2015 to 8.6% in 2018.
Figure 1.
Percentage of U.S. adults aged 50–75 years up-to-date with CRC screening, by test type, 2010–2018. Data are from the National Health Interview Survey and are age-standardized to the 2010 U.S. census in 5-year age groups. Up-to-date was defined as meeting U.S. Preventive Services Task Force screening recommendations. FIT-DNA was not asked about in the 2015 survey or previous surveys and was rarely used before 2015. Error bars are 95% confidence intervals.
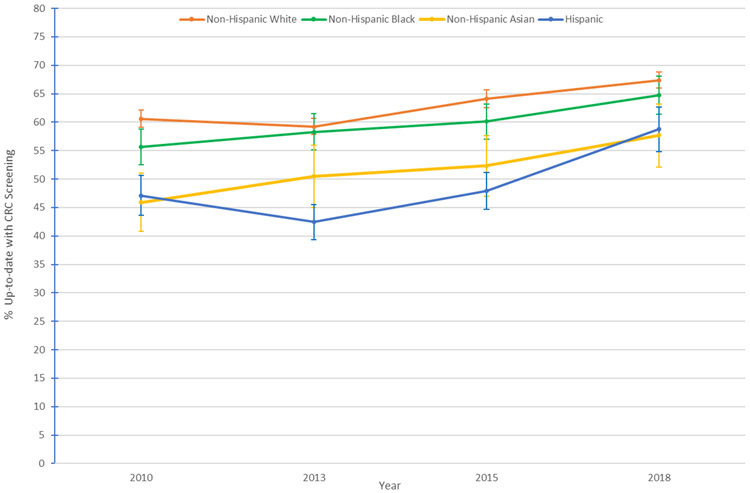
Figure 2 shows age-standardized trends in CRC screening test use by race/ethnicity from 2010 to 2018. Use of any CRC screening test increased significantly from 2010 to 2018 and from 2015 to 2018 for each of the racial/ethnic groups analyzed, except for non-Hispanic Asian adults for whom the change from 2015 to 2018 was not statistically significant. The estimated magnitude of the increase from 2015 to 2018 was greatest for Hispanic adults, for whom prevalence increased by over 10 percentage points (from 47.9% to 58.8%).
Figure 2.
Percentage of U.S. adults aged 50–75 years up-to-date with CRC screening, by race/ethnicity, 2010–2018. Data are from the National Health Interview Survey and are age-standardized to the 2010 U.S. census in 5-year age groups. Up-to-date was defined as meeting U.S. Preventive Services Task Force screening recommendations. Error bars are 95% confidence intervals.
Discussion
In this analysis of NHIS data, an estimated 67% of U.S. adults aged 50-75 were up-to-date with CRC screening in 2018. However, important disparities still exist; the prevalence of being up-to-date was under 50% in several groups, including adults aged 50-54 years, adults without a usual source of health care, those who had no doctor visits in the past year, and those who were uninsured. The most commonly used CRC screening test was colonoscopy, with an estimated 61% of adults aged 50-75 years reporting colonoscopy use within the past 10 years, followed by stool tests (including FOBT, FIT and FIT-DNA), which were used by approximately 11% within the recommended time interval. This analysis shows modest progress towards achieving population screening goals, with the percentage up-to-date with CRC screening (after age-standardization to the 2010 census population) increasing from 61% in 2015 to 65% in 2018. This increase was driven by an increase in the use of stool tests, including the new FIT-DNA test.
In the 2018 NHIS, similar to patterns in other U.S. surveys (4,20-22), overall CRC screening test use and colonoscopy use were lower in adults who were aged 50-64 years, were born outside the U.S, were of lower socioeconomic status (i.e., less educated or lower family income), or had less access to health care (i.e., did not have a usual source of care, had fewer doctor visits, or were uninsured). While the prevalence of being up-to-date on CRC screening reached 83% in people enrolled in Medicare Advantage plans, most population groups fell short of meeting the “80% in Every Community” NCCRT target (6).
While differences in CRC screening test use by race/ethnicity persisted in 2018, the difference in CRC screening test use between Hispanic adults and non-Hispanic White adults appeared to have diminished modestly between 2015 and 2018. Differences by education and income may also have lessened (4).
In unadjusted analyses, CRC screening rates in 2018 were lower for non-Hispanic Black and Hispanic adults compared with non-Hispanic White adults. However, in the multivariable-adjusted model, non-Hispanic Black and Hispanic adults did not have a lower CRC screening prevalence compared with non-Hispanic White adults, suggesting that CRC screening disparities by race and ethnicity could be partially explained by other sociodemographic factors.
CRC screening test use was lower in younger age groups, particularly those aged 50-54 years. Some people may procrastinate in getting their first CRC screening test. Primary care providers can initiate discussions about CRC screening with patients before the recommended age to start screening to ensure screening begins promptly at the recommended age.
While stool test use, like colonoscopy use, was higher in those with a usual source of health care or more doctor visits in the past year, patterns of associations with many other factors were quite different for stool test use than for colonoscopy. Unlike for colonoscopy, stool test use was not higher in those who had more education or higher income. In unadjusted analyses, stool test use was higher for those who were born outside the U.S. than for those born in the U.S., and higher for Hispanic adults than for non-Hispanic White adults, whereas the opposite was true for colonoscopy use. Stool test use was higher for people living in the West than for those in other regions. Adults aged 65-75 years enrolled in Medicare Advantage had the highest prevalence of stool test use (22%).
There are several possible explanations for why stool test use may have been higher in Medicare Advantage enrollees. Approximately 62% of those enrolled in Medicare Advantage plans in 2019 were in HMOs (23). Some HMOs have organized CRC screening programs that mail stool tests to enrollees (24,25). In addition, Medicare Advantage plans are paid a monthly, fixed amount for each enrollee (23). Since these plans are reimbursed per patient instead of per procedure, there may be an incentive to choose stool tests since they are less expensive than colonoscopy. Since 2012, Medicare Advantage plans have been eligible for bonus payments if they have a quality rating of four or more stars based on the Centers for Medicare and Medicaid Services Medicare Advantage Star Ratings (23,26), which incorporate CRC screening as a criterion. Medicare Advantage programs may therefore have a financial incentive to increase CRC screening and may have considered stool testing a feasible and efficient way to increase their CRC screening rates (27).
The reasons for the increase in stool test use since 2015 other than availability of the new FIT-DNA test are unclear, but possible reasons include increasing use of stool tests by Medicare Advantage and other health plans, use of mailed FIT programs, and increasing emphasis on the need to offer CRC screening options besides colonoscopy. In 2014, the NCCRT launched their “80% by 2018” initiative, which included messages emphasizing that multiple screening options were available, including simple take-home options (6).
The FIT-DNA test is more expensive than FOBT or FIT and requires collection of the whole stool instead of a small sample. However, a study of the FIT-DNA test Cologuard® found that it had higher sensitivity than FIT for both cancer and advanced adenomas, although specificity was lower (28).
While increased stool testing has contributed to an increase in overall CRC screening, increased stool testing will contribute to lower CRC mortality only if positive stool tests are followed up by a timely colonoscopy (29). A study of Kaiser Permanente members found that follow-up colonoscopy more than 10 months after a positive FIT was associated with greater CRC risk compared with follow-up colonoscopy within 30 days (30). Studies have found that follow-up colonoscopy rates are not sufficiently high, particularly in lower income populations. In several studies of safety net health systems and federally qualified health centers, follow-up colonoscopy rates within 6 months ranged from 44% to 52% (31-34).
Since these data were collected before the COVID-19 pandemic, they do not reflect the prevalence of screening during the pandemic. CRC screening tests have been delayed or cancelled due to the pandemic (35). The prevalence of being up-to-date on CRC screening could be lower than the prevalence in 2018 for a period of time after the pandemic. The CRC screening data from the 2018 NHIS can be used to help assess when CRC screening has caught up to pre-pandemic levels. In addition, the time trends (e.g. greater use of stool testing) and correlates of CRC screening observed will be relevant in informing post-pandemic efforts to achieve population screening goals.
This analysis has some limitations. The information in the NHIS was self-reported and some respondents may have incorrectly reported use and/or timing of CRC tests. However, studies have generally found moderate to good agreement between self-reported CRC test use and information from medical records (36-41). In addition, the 2018 NHIS adult response rate was relatively low (53%). Survey results were weighted to account for non-response bias (7,16); however, some bias may still exist.
This analysis also has several notable strengths. The 2018 NHIS is a nationally representative study with a large sample size. Because of its large size, we were able to estimate the prevalence of CRC screening both overall and by test type within population subgroups, such as racial/ethnic subgroups. To our knowledge, the 2018 NHIS is the first large nationally representative survey to collect information on FIT-DNA testing. This analysis also examined time-trends in CRC screening, which are important for understanding progress in CRC screening.
These results show progress in CRC screening test use in the last few years, driven by a modest increase in use of stool tests. Further increases in stool test use could contribute to meeting overall screening goals. Overall, the prevalence of CRC screening test use in 2018 fell short of the NCCRT’s 80% goal (6) and the Healthy People 2030 target of 74.4% (42), but approached the Healthy People 2020 target of 70.5% (5). CRC screening prevalence remains substantially lower in people with less access to health care. These results may inform efforts to increase CRC screening, including both colonoscopy and stool testing, in underserved populations.
Supplementary Material
Financial Support:
SF and AJ are employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health-care sector for research outside of the submitted work. The authors, however, were not funded by any of these grants and their salaries were solely funded through American Cancer Society funds.
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
Footnotes
Conflict of Interest Statement: The authors declare no potential conflicts of interest.
References
- 1.Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O'Connor E, et al. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016;315(23):2576–94. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Cancer Statistics Working Group. 2019. May 10. U.S. Cancer Statistics Data Visualizations Tool, based on November 2018 submission data (1999-2016): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. <www.cdc.gov/cancer/dataviz>. Accessed 2020 May 10. [Google Scholar]
- 3.Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr., Garcia FAR, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2016;315(23):2564–75. [DOI] [PubMed] [Google Scholar]
- 4.de Moor JS, Cohen RA, Shapiro JA, Nadel MR, Sabatino SA, Robin Yabroff K, et al. Colorectal cancer screening in the United States: Trends from 2008 to 2015 and variation by health insurance coverage. Prev Med 2018;112:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. April 14. Clinical Preventive Services, Healthy People 2020. <https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services/data>. Accessed 2020 April 14.
- 6.National Colorectal Cancer Roundtable. 2017. April 29. 80% by 2018 Communications Guidebook: Recommended Messaging to Reach the Unscreened. <https://nccrt.org/resource/2017-80-2018-communications-guidebook-recommended-messaging-reach-unscreened/>. Accessed 2020 April 29.
- 7.National Center for Health Statistics. 2019. May 8. Survey Description, National Health Interview Survey, 2018. <ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2018/srvydesc.pdf >. Accessed 2020 May 8.
- 8.National Center for Health Statistics. 2011. June 2. Survey Description, National Health Interview Survey, 2010. <ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf>. Accessed 2020 June 2.
- 9.National Center for Health Statistics. 2014. June 2. Survey Description, National Health Interview Survey, 2013. <ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2013/srvydesc.pdf>. Accessed 2020 June 2.
- 10.National Center for Health Statistics. 2016. June 2. Survey Description, National Health Interview Survey, 2015. <ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2015/srvydesc.pdf>. Accessed 2020 June 2.
- 11.Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008;149(9):627–37. [DOI] [PubMed] [Google Scholar]
- 12.Food and Drug Administration. 2014. July 8. Summary of Safety and Effectiveness Data. Cologuard™–P130017. <https://www.accessdata.fda.gov/cdrh_docs/pdf13/P130017B.pdf >. Accessed 2020 July 8. [Google Scholar]
- 13.Centers for Medicare & Medicaid Services. 2014. July 8. Decision Memo for Screening for Colorectal Cancer - Stool DNA Testing (CAG-00440N) <https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=277 >. Accessed 2020 July 8.
- 14.Hall HI, Van Den Eeden SK, Tolsma DD, Rardin K, Thompson T, Hughes Sinclair A, et al. Testing for prostate and colorectal cancer: comparison of self-report and medical record audit. Prev Med 2004;39(1):27–35. [DOI] [PubMed] [Google Scholar]
- 15.Eberth JM, Vernon SW, White A, Abotchie PN, Coan SP. Accuracy of self-reported reason for colorectal cancer testing. Cancer Epidemiol Biomarkers Prev 2010;19(1):196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the national health interview survey, 2006-2015. Vital Health Stat 2 2014(165):1–53. [PubMed] [Google Scholar]
- 17.Parker JD, Talih M, Malec DJ, Beresovsky V, Carroll M, Gonzalez JF, et al. National Center for Health Statistics Data Presentation Standards for Proportions. Vital Health Stat 2 2017(175):1–22. [PubMed] [Google Scholar]
- 18.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics 1999;55(2):652–9. [DOI] [PubMed] [Google Scholar]
- 19.Li C, Ford ES, Zhao G, Wen XJ, Gotway CA. Age adjustment of diabetes prevalence: use of 2010 U.S. Census data. J Diabetes 2014;6(5):451–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White A, Thompson TD, White MC, Sabatino SA, de Moor J, Doria-Rose PV, et al. Cancer Screening Test Use - United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66(8):201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev 2012;21(6):895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joseph DA, King JB, Dowling NF, Thomas CC, Richardson LC. Vital Signs: Colorectal Cancer Screening Test Use - United States, 2018. MMWR Morb Mortal Wkly Rep 2020;69(10):253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.KFF. 2019. May 10. Medicare Advantage. <https://www.kff.org/medicare/fact-sheet/medicare-advantage/>. Accessed 2020 May 10.
- 24.Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, et al. Effects of Organized Colorectal Cancer Screening on Cancer Incidence and Mortality in a Large Community-Based Population. Gastroenterology 2018;155(5):1383–91 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Colorectal Cancer Roundtable. 2017. June 15. Colorectal Cancer Screening Best Practices Handbook for Health Plans. <http://nccrt.org/wp-content/uploads/NCCRT-Health-Plan-Handbook-Draft-07c.pdf>. Accessed 2020 June 15.
- 26.Center for Medicare and Medicaid Services. 2019. July 8. Medicare 2020 Part C & D Star Ratings Technical Notes. <https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/Star-Ratings-Technical-Notes-Oct-10-2019.pdf>. Accessed 2020 July 8.
- 27.Green BB, Coronado GD, Devoe JE, Allison J. Navigating the murky waters of colorectal cancer screening and health reform. American journal of public health 2014;104(6):982–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imperiale TF, Ransohoff DF, Itzkowitz SH. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med 2014;371(2):187–8 doi 10.1056/NEJMc1405215. [DOI] [PubMed] [Google Scholar]
- 29.Gupta S, Coronado GD, Argenbright K, Brenner AT, Castaneda SF, Dominitz JA, et al. Mailed fecal immunochemical test outreach for colorectal cancer screening: Summary of a Centers for Disease Control and Prevention-sponsored summit. CA Cancer J Clin 2020:283–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corley DA, Jensen CD, Quinn VP, Doubeni CA, Zauber AG, Lee JK, et al. Association Between Time to Colonoscopy After a Positive Fecal Test Result and Risk of Colorectal Cancer and Cancer Stage at Diagnosis. JAMA 2017;317(16):1631–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chubak J, Garcia MP, Burnett-Hartman AN, Zheng Y, Corley DA, Halm EA, et al. Time to Colonoscopy after Positive Fecal Blood Test in Four U.S. Health Care Systems. Cancer Epidemiol Biomarkers Prev 2016;25(2):344–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bharti B, May FFP, Nodora J, Martinez ME, Moyano K, Davis SL, et al. Diagnostic colonoscopy completion after abnormal fecal immunochemical testing and quality of tests used at 8 Federally Qualified Health Centers in Southern California: Opportunities for improving screening outcomes. Cancer 2019;125(23):4203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liss DT, Brown T, Lee JY, Altergott M, Buchanan DR, Newland A, et al. Diagnostic colonoscopy following a positive fecal occult blood test in community health center patients. Cancer Causes Control 2016;27(7):881–7. [DOI] [PubMed] [Google Scholar]
- 34.Somsouk M, Rachocki C, Mannalithara A, Garcia D, Laleau V, Grimes B, et al. Effectiveness and Cost of Organized Outreach for Colorectal Cancer Screening: A Randomized, Controlled Trial. J Natl Cancer Inst 2020;112(3):305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Colorectal Cancer Roundtable. 2020. July 8. Reigniting Colorectal Cancer Screening as Communities Face and Respond to the COVID-19 Pandemic. <https://nccrt.org/resource/a-playbook-for-reigniting-colorectal-cancer-screening-as-communities-respond-to-the-covid-19-pandemic/>. Accessed 2020 July 8.
- 36.White A, Vernon SW, Eberth JM, Tiro JA, Coan SP, Abotchie PN, et al. Correlates of self-reported colorectal cancer screening accuracy in a multi-specialty medical group practice. Open J Epidemiol 2013;3(1):20–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shokar NK, Vernon SW, Carlson CA. Validity of self-reported colorectal cancer test use in different racial/ethnic groups. Fam Pract 2011;28(6):683–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Partin MR, Grill J, Noorbaloochi S, Powell AA, Burgess DJ, Vernon SW, et al. Validation of self-reported colorectal cancer screening behavior from a mixed-mode survey of veterans. Cancer Epidemiol Biomarkers Prev 2008;17(4):768–76. [DOI] [PubMed] [Google Scholar]
- 39.Vernon SW, Tiro JA, Vojvodic RW, Coan S, Diamond PM, Greisinger A, et al. Reliability and validity of a questionnaire to measure colorectal cancer screening behaviors: does mode of survey administration matter? Cancer Epidemiol Biomarkers Prev 2008;17(4):758–67. [DOI] [PubMed] [Google Scholar]
- 40.Jones RM, Mongin SJ, Lazovich D, Church TR, Yeazel MW. Validity of four self-reported colorectal cancer screening modalities in a general population: differences over time and by intervention assignment. Cancer Epidemiol Biomarkers Prev 2008;17(4):777–84. [DOI] [PubMed] [Google Scholar]
- 41.Khoja S, McGregor SE, Hilsden RJ. Validation of self-reported history of colorectal cancer screening. Can Fam Physician 2007;53(7):1192–7. [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. March 1. Healthy People 2030. <https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-adults-who-get-screened-colorectal-cancer-c-07>. Accessed 2021 March 1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.