Abstract
Introduction
Coronavirus disease 2019 (COVID-19) is characterized by hyperinflammation and coagulopathy. Severe cases often develop respiratory distress, requiring mechanical ventilation and with critical cases progressing to acute respiratory distress syndrome. Control of hyperinflammation has been proposed as a possible therapeutic avenue for COVID-19; extracorporeal blood purification (EBP) modalities offer an attractive mean to ameliorate maladaptive inflammation. With this work, we evaluated the longitudinal changes of systemic inflammatory markers in critically ill COVID-19 patients treated with blood purification using AN69ST (oXiris®) haemofilter.
Methods
We performed a time-series analysis of 44 consecutive COVID-19 cases treated with the AN69ST (oXiris®) cytokine adsorbing haemofilter (CAH) according to local practice; we visualize longitudinal results of biochemical, inflammatory, blood gas, and vital sign parameters focussing on systemic levels of interleukin-6 (IL-6), C-reactive protein (CRP), and procalcitonin.
Results
All patients were treated with ≥1 cycle extracorporeal continuous venovenous haemofiltration (CVVH) with CAH; of these, 30 severe patients received CVVH-CAH within 4–12 h of admission after recognizing a hyper-inflammatory state. Another 14 patients admitted with mild-to-moderate symptoms progressed to severe disease and were placed on EBP during hospitalization. The treatment was associated with a reduction of ferritin, CRP, fibrinogen, several inflammatory markers, and a resolution of numerous cytopenias. The observed mortality across the cohort was 36.3%.
Conclusion
EBP with CAH was associated with a decrease in CRP, and control of IL-6 and procalcitonin.
Keywords: Coronavirus disease 2019, Interleukin-6, Heparin, Coronavirus, Anticoagulation, oXiris
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has dominated our lives since the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) started in Wuhan of Hubei Province, China [1]. Its disruptive nature was confirmed with the World Health Organization's classification as a global epidemic on February 28, 2020 [2].
Severe COVID-19 is characterized by uncontrolled inflammation [3, 4, 5]. Systemic inflammation and immunopathology [6, 7] are considered the essential drivers of disease progression leading to acute respiratory distress syndrome (ARDS) [8], coagulopathy [9, 10] secondary infections [11], and multiorgan failure, in particular, acute kidney injury (AKI) [5, 12, 13].
AKI appears to be a common finding among severely ill patients infected with SARS-CoV-2 [8, 14], and occurring in up to 25% of critically ill COVID-19 patients admitted in the intensive care unit (ICU). Beyond systemic inflammation, other pathophysiologic mechanisms contribute to the development and worsening of AKI in these patients, such as the lung-kidney interaction, and the iatrogenic effects of mechanical ventilation and nephrotoxic drugs [14, 15, 16]. Blood purification therapies have been advocated as adjunctive treatments in COVID-19 patients to support renal function, mitigate maladaptive inflammation, and prevent multiple organ dysfunction [17, 18].
The oXiris membrane (Baxter, IL, USA) is a heparin-coated haemofilter suitable for continuous renal replacement therapy. Interestingly, this device can also be used for unselective removal of cytokines and endotoxin. These characteristics make the oXiris membrane a useful tool for supporting the organ function and restoring immune homoeostasis in COVID-19 patients with AKI [19]. Hence, in this study, we have described the overtime variation of biochemical parameters of systemic inflammation in COVID-19 patients treated with oXiris, along with parameters of organ dysfunction.
Study Methods
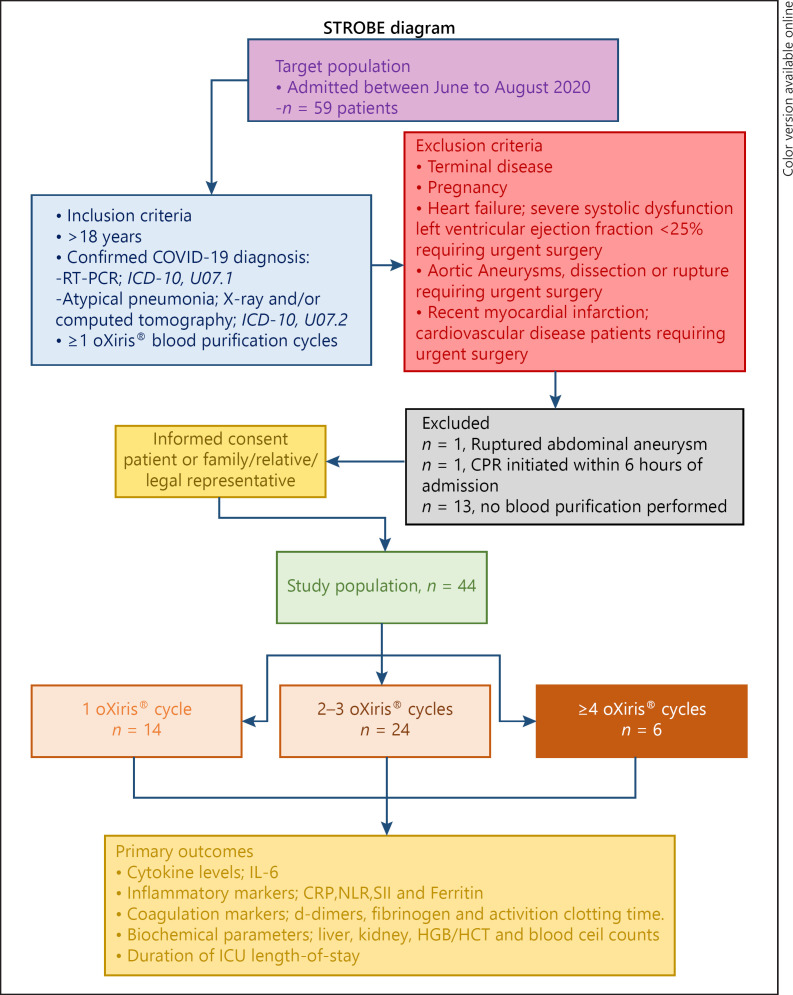
In this prospective monocentric observational study, we have considered all patients consecutively admitted in the ICU between June 14th and August 11th with confirmed International Classification of Diseases 10 code of U07.1 COVID-19 or International Classification of Diseases 10 code of U07.2 COVID-19 diagnosis. Only patients who received treatment with oXiris membrane for immunomodulation and support to renal function during AKI were considered eligible for this study. The study designed is presented in the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) diagram (Fig. 1. Considering the observational nature of this study, no criteria have been a priori defined for oXiris initiation.
Fig. 1.
STROBE diagram. STROBE, STrengthening the Reporting of OBservational studies in Epidemiology; COVID-19, coronavirus disease 2019; ICD-10, International Classification of Diseases 10; IL-6, interleukin-6; FIB, fibrinogen; ICU, intensive care unit.
Patients were classified according to their clinical presentation at the ICU admission in 2 severity degrees:
Mild-moderate cases, showing fever and respiratory symptoms with radiological findings of pneumonia.
Severe-critical cases, with respiratory distress (30 breaths/min), oxygen saturation <93% at rest, or chest imaging showing lesion >50% progression within 24 h, with respiratory failure requiring mechanical ventilation, shock, or multiorgan dysfunction.
All patients included in this prospective observational study received antimicrobials, extracorporeal blood purification (EBP), mechanical ventilation, and any other supportive treatment following the clinical judgement of the treating centre and guidelines. In accordance with local routine practice, the Prismaflex® oXiris® system was considered for those patients suspected of hyperinflammation (= C-reactive protein [CRP] ≥ 100 mg/L and/or interleukin-6 [IL-6] ≥ 40 pg/mL, and/or ferritin ≥ 500 ng/mL). In these patients, oXiris was mounted in the ICU and connected within 4–12 h after recognizing a hyperinflammatory state. Control of the haemostasis was based on an activated coagulation time of 180 s. The patient is connected to the Prismaflex® oXiris® system via a double lumen catheter placed in the femoral, subclavian, or jugular vein.
Biochemistry Analysis
Diagnosis of SARS-CoV-2 infection was defined as a positive outcome to RT-PCR from nasal/oral swab. Blood samples were collected from each patient at the time points shown for routine blood analysis: white blood cell count, lymphocyte (LYM) count, neutrophil (NEU) count, thrombocyte count, monocyte count, and eosinophil count were determined as well as the NEU/LYM and the systemic immune-inflammation index thrombocyte count*NEU/LYM. Moreover, blood biochemistry parameters such as Na+, K+ aspartate aminotransferase, alanine aminotransferase, urea, CRP, IL-6 as well as procalcitonin, and lactate dehydrogenase were assessed using a Siemens ADVIA Centaur XP Immunoassay System.
Data on coagulation parameters were obtained from all patients; coagulation tests included D-dimers, fibrinogen, and international normalized ratio. Tests were performed using a Sysmex CA-600 automatic coagulation analyser. Blood gas analysis (BGA) was performed on a Siemens rapid point 500® system.
Statistical Analysis.
Categorical parameters were summarized as absolute numbers and percentages. Continuous data are shown as mean ± SD or median + interquartile range (IQR).
Continuous variables were evaluated using the D'Agostino and Pearson normality test − independent data that follow the Gaussian distribution were analysed via the Student's t test, and non-Gaussian continuous variables were assessed via the Mann-Whitney test for independent comparisons. Comparisons of preoperative versus postoperative data were performed using a paired t test or Wilcoxon signed-rank test for non-parametric data.
Fisher's exact test was used to evaluate the association between categorical variables with the outcome. Two groups of longitudinal comparison were analysed with the mixed-effects model ANOVA with the Greenhouse-Geisser correction. Asterisks, * <0.05, ** <0.01, *** <0.001, and **** <0.0001, visualize the significance levels of Dunnett's multiple comparisons test at each time point. Regression and/or correlation analysis between the biomarkers over time were performed using Pearson's or Spearman's rank correlation testing. The data were analysed using Graphpad Prism (version 9.0.0) and Statsdirect (version 3.3.3).
Ethical Concerns
Institutional review board approval was obtained from the local Ethical Committee of the Zan Mitrev Clinic in accordance with the Declaration of Helsinki and ICH-Good Clinical Practice.
Results
Patient Demographics and Clinical Characteristics at Admission
Among the 59 patients admitted with COVID-19 in the selected period, 44 were treated with oXiris® and considered in this single-centre case series. At the ICU admission, 68.2% (N = 30) of patients had symptoms classified as severe-critical and 32.8% (N = 14) as mild-moderate. The clinical and demographic characteristics are described overall and for both groups in Table 1.
Table 1.
Patient characteristics and demographics
| Full cohort (N = 44) | Mild/moderate (N = 14) | Severe (N = 30) | Effect size mild/moderate versus severe | p value | |
|---|---|---|---|---|---|
| Age, mean ± SD, years | 59.7±12.0 | 53.9±16.5 | 62.4±8.4 | 8.5 [95% CI1 to 15.9]1 | 0.028 |
| Age > 65 years, N (%) | 16 (36) | 4 (29) | 12 (40) | 1.7 [95% CI 0.4 to 5.6]3 | 0.52 |
| Gender | |||||
| Male, N (%) | 36 (82) | 13 (93) | 23 (77) | 42.3 [95% CI 4.9 to 469]3 | <0.0001 |
| Female, N (%) | 8 (18) | 1 (7) | 7 (23) | ||
| Type 2 diabetes, N (%) | 7 (16) | 0 (0) | 7 (23) | 0.0 [95% CI 0.0 to 0.19]3 | 0.08 |
| Hypertension, N (%) | 22 (53) | 6 (42) | 16 (53) | 1.5 [95% CI 0.4 to 4.9]3 | 0.74 |
| BMI | 27.6±3.5 | 26.7±3.3 | 29±4.8 | 2.6 [95% CI −0.3 to 5.4]1 | 0.081 |
| Obesity,* N (%) | 13 (30) | 2 (14) | 11 (37) | 3.4 [95% CI 0.7 to 17.5]3 | 0.17 |
| SpO2, % | 93.1±5.8 | 94.7±2.8 | 92.4±6.6 | −2.3 [95% CI −2.7 to −1.9]1 | <0.0001 |
| Heart rate, beats/min | 96.4±22.1 | 79.2±13.9 | 102.4±21.3 | 23 [95% CI 2.7 to 24.9]1 | <0.0001 |
| Respiratory rate, breaths/min | 24 (20–29) | 22 (18–26) | 25 (21–29) | 3 [95% CI 3 to 4]2 | <0.0001 |
| Mean blood pressure, mm Hg | 127.4±29.6 | 125.2±16.4 | 127.9±31.2 | 2.7 [95% CI −6.6 to 11.9]1 | 0.201 |
| Symptom duration, days | 7 (5–7) | 5 (5–7) | 7 (6–8) | 2.0 [95% CI 0 to 3]2 | 0.025 |
| Referral | |||||
| Home, N (%) | 19 (43) | 9 (64) | 10 (36) | 3.6 [95% CI 0.98 to 13.3]3 | 0.101 |
| Peripheral clinic, N (%) | 25 (57) | 5 (36) | 20 (67) |
Values are presented as median (IQR) or mean ± standard deviation. ND, not detected; NR, not relevant; IQR, interquartile range.
Mean difference.
Median difference.
Fisher's exact test, odds ratio.
BMI > 30 kg/m2.
Primary symptoms reported were dyspnoea, fever, and breathing difficulties. Patients with severe disease were characterized by more prolonged duration of symptoms; they were admitted on average 7 days (vs. 5 days for non-severe cases, p = 0.025) after symptom onset and were more likely to be referred from peripheral clinics (67 vs. 36%, OR 3.6 [95% CI 0.98 to 13.3], p = 0.101) in comparison to direct admission following self-isolation at home.
We observed non-significant trends suggesting more pronounced respiratory difficulties and lower blood pressure in advanced disease. We aggregated selected laboratory values and patient signs that account for both acute and chronic diseases to determine the Acute Physiology and Chronic Health Evaluation II (APACHE II) at admission; severe cases had an overall APACHE II score of 8.8 ± 4.7 versus 5.1 ± 2.1, mean difference 3.8 [95% CI 1.1 to 6.4], p = 0.007.
Severe cases were admitted with a more prominent inflammatory profile, demonstrated by elevated levels of lactate dehydrogenase, 494.5 U/L (IQR 374–669); ferritin, 1,100 ng/mL (IQR 406–1,650); CRP, 151 mg/L (IQR 82–211); and the immune indices NLR and SII, 11.5 (7.5–18.5) and 2580 (1,554–4,692), respectively (Table 2). Moreover, we observed substantially higher D-dimer levels in severe cases than in those with mild to moderate symptoms, median difference, 630 [95% CI 160.0 to 6,220], p = 0.013 (Table 2). Despite the clinically significant increase of 2 key acute phase proteins and inflammatory markers, there was only a marginal increase in IL-6 across the cohort, 15.5 (7.4–47.3) pg/mL.
Table 2.
Patient clinical data at admission
| Full cohort (N = 44) | Mild/moderate (N = 14) | Severe (N = 30) | Effect size mild/moderate versus severe | p value | |
|---|---|---|---|---|---|
| ALT, U/L | 57 (30–85) | 55 (25–76) | 58 (31–107) | 3.5 [95% CI −13 to 36]2 | 0.327 |
| AST, U/L | 42 (29–66) | 41 (26–66) | 44 (32–67) | 3 [95% CI −10.0 to 20.0]1 | 0.528 |
| Urea, mmol/L | 5.6 (3.9–8.1) | 3.9 (3.4–5.9) | 6.7 (4.9–9.3) | 2.7 [95% CI 0.9 to 4.3]1 | 0.0013 |
| Creatinine, µmol/L | 91.8±32.2 | 81.9±15.2 | 96.4±36.9 | 13.4 [95% CI −6.3 to 35.5]1 | 0.17 |
| GFR, mL/min | 108.3±39.7 | 115.6±33.2 | 104.8±42.6 | −10.8 [95% CI −37.0 to 15.4]2 | 0.410 |
| LDH, U/L | 407 (272–569) | 252 (203–303) | 495 (374–669) | 243 [95% CI 142 to 358]2 | <0.0001 |
| RBC, ×106 counts/µL | 4.8±0.7 | 4.8±0.4 | 4.8±0.8 | 0.02 [95% CI −0.46 to 0.50]1 | 0.929 |
| HCT, % | 39.6±5.8 | 39.5±2.7 | 39.7±6.9 | 0.11 [95% CI −3.8 to 3.9]1 | 0.955 |
| HGB, g/dL | 13.8±2.1 | 13.8±0.9 | 13.8±2.5 | −0.01 [95% CI −1.4 to 1.4]2 | 0.994 |
| WBC, ×103 counts/µL | 7.4 (4.8–12.1) | 4.0 (2.7–6.5) | 9.8 (7.1–13.4) | 5.8 [95% CI 2.6 to 7.8]2 | <0.0001 |
| Basophils, % | 0.14 (0.1–0.24) | 0.27 (0.2–0.4) | 0.14 (0.1–0.14) | −0.1 [95% CI −0.3 to −0.1]1 | 0.0003 |
| EO, % | 0.17 (0.03–0.47) | 0.12 (0.0–0.49) | 0.10 (0.04–0.24) | −0.02 [95% CI −0.2 to 0.1]1 | 0.97 |
| MONO, % | 4.0 (3.0–6.3) | 5.5 (4.0–11.7) | 3.6 (2.4–5.3) | −1.9 [95% CI −5.9 to −0.8]1 | 0.0017 |
| NEU, % | 82.2±11.4 | 72.3±10.3 | 86.9±8.5 | 14.7 [95% CI 8.7 to 20.7]1 | <0.0001 |
| LYM, % | 9.9 (5.5–13.4) | 20.1 (11.1–26.7) | 7.7 (4.9–11.2) | −12.4 [95% CI −17.6 to −5.4]1 | <0.0001 |
| Platelets, ×103 counts/µL | 200 (127–256) | 138 (119–176) | 224 (146–337) | 62 [95% CI 13 to 142]2 | 0.012 |
| NLR, ×103 counts/µL | 8.5 (5.9–16.0) | 3.6 (2.5–7.6) | 11.5 (7.5–18.5) | 7.9 [95% CI 4.4 to 12.6]2 | <0.0001 |
| SII | 2,047 (815–3,594) | 620 (321–1,071) | 2,580 (1,554–4,692) | 1,959 [95% CI 1,224 to 3,215]2 | <0.0001 |
| IL-6, pg/mL | 15.5 (7.4–47.3) | 16.9 (5.9–33.1) | 14.7 (7.9–64.3) | −2.3 [95% CI −9.3 to 38.2]1 | 0.39 |
| CRP, mg/L | 109.0 (57.8–173.1) | 71.1 (8.9–109.7) | 150.6 (81.6–210.6) | 79.5 [95% CI 33.4 to 135.9]2 | 0.001 |
| Ferritin, ng/mL | 948 (352–1,573) | 479 (268–1,155) | 1,100 (406–1,650) | 621 [95% CI 113 to 872]2 | 0.1548 |
| Procalcitonin, ng/mL | 0.07 (0.05–0.13) | 0.05 (0.01–0.05) | 0.11 (0.07–0.19) | 0.08 [95% CI 0.03 to 0.11]2 | 0.0002 |
| D-dimers, ng/mL | 735 (398–2,728) | 595.0 (292.5–850) | 1,225 (595.0–11,503) | 535 [95% CI 110 to 2,860]2 | 0.0108 |
| aPTT, s | 22.4 (20.6–24.8) | 23.6 (21.9–25.6) | 21.8 (20.4–23.7) | −1.8 [95% CI −3.6 to 0.3]1 | 0.086 |
| FIB, g/L | 4.9 (4.1–7.0) | 4.5 (3.9–6.2) | 5.1 (4.2–8.0) | 0.55 [95% CI −0.5 to 1.4]2 | 0.352 |
Values are presented as median (IQR) or mean±standard deviation. ALT, alanine aminotransferase; AST, aspartate aminotransferase; GFR, glomerular filtration rate; LDH, lactate dehydrogenase; WBC, white blood cell count; EO, eosinophil; MONO, monocyte; NEU, neutrophil; LYM, lymphocyte; CRP, C-reactive protein; IL-6, interleukin-6; FIB, fibrinogen.
Median difference.
Mean difference.
EBP: Treatment Approach and Clinical Practice
The oXiris® continuous renal replacement therapy modality was mostly set as continuous venovenous haemofiltration (42/44, 95.5%). Flow rates were maintained as follows: effluent dose 35 mL/kg/h, blood 150 mL/min, and replacement 16–18 mL/kg/h; patient fluid removal was tailored to the individual's volume status, ≈ 100–250 mL/h.
The average levels of urea, creatinine, and the Cockcroft-Gault glomerular filtration rate were 5.6 (3.9–8.1) mmol/L, 91.8 ± 32.2 μmol/L, and 108.3 ± 39.7 mL/min, respectively. We observed 2 cases of significant kidney dysfunction (= glomerular filtration rate < 50 mL/min) in our COVID-19 cohort. Consequently, CVVHDF was prescribed in these two patients.
Total run time on the Prismaflex system was 3303.8 h; on average, severe cases were treated with 2 (IQR 1–3) blood purification cycles, one more than the non-severe patients. The average duration of blood purification was 30.3 h (20.8–44.9 h) (Table 3).
Table 3.
Clinical course and outcome
| Full cohort (N = 44) | Mild/moderate (N = 14) | Severe (N = 30) | Effect size mild/moderate versus severe | p value | |
|---|---|---|---|---|---|
| Hospitalization, days | 10.1±5.8 | 10.6±3.3 | 9.8±5.4 | 2.0 [95% CI −0.68 to 4.74]1 | 0.139 |
| APACHE II | 7.6±4.8 | 5.1±2.1 | 8.8±4.7 | 3.8 [1.1 to 6.4]1 | 0.007 |
| Mechanical ventilation, h | 47.8 (2.8–110.7) | 0 | 47.8 (2.8–110.7) | nd | nd |
| Inotrope support,1 N (%) | 5 (8.5) | 0 | 5 (17.7) | nd | nd |
| Blood purification | |||||
| Cycle(s) per patient, cnt | 1 (0–2) | 1 (0–2) | 2 (1–3) | 1 [95% CI 0 to 2]2 | 0.004 |
| Cumulative duration, h | 3,303.8 | 885.8 | 2,418 | nd | nd |
| Duration per cycle, h | nd | 41.4 (25.5–49.3) | 32.8 (23–48.0) | −8.5 [95% CI −11.2 to 4.3]1 | 0.424 |
| Co-infection,∞ N (%) | 19 (43) | 6 (43) | 13 (43) | 1.0 [95% CI 0.28 to 3.4]3 | 0.999 |
| Mortality, N (%) | 16 (36) | 1 (7) | 15 (50) | 13.0 [95% CI 1.7 to 147]4 | 0.007 |
APACHE II, Acute Physiology and Chronic Health Evaluation II.
Norepinephrine or epinephrine.
Mean difference.
Individual cases with confirmed bacterial secondary infection. Fisher's exact test, odds ratio.
Relative risk.
We observed no complications related to bleeding or thromboembolism. There were 9 occurrences of premature clotting (machine run time < 5 h) resulting in a linearized incidence premature clotting rate of 0.27% (patient hours).
One patient experienced a haematoma following venous cannulation that required a catheter displacement. Our complete treatment approach was previously documented [20]. In parallel, during hospitalization, 12 critical patients were treated with i.v. dexamethasone at a dose of 8 mg q.d.
Time-Series Analyses of Inflammatory Biomarkers, Vital Signs, and BGA Parameters
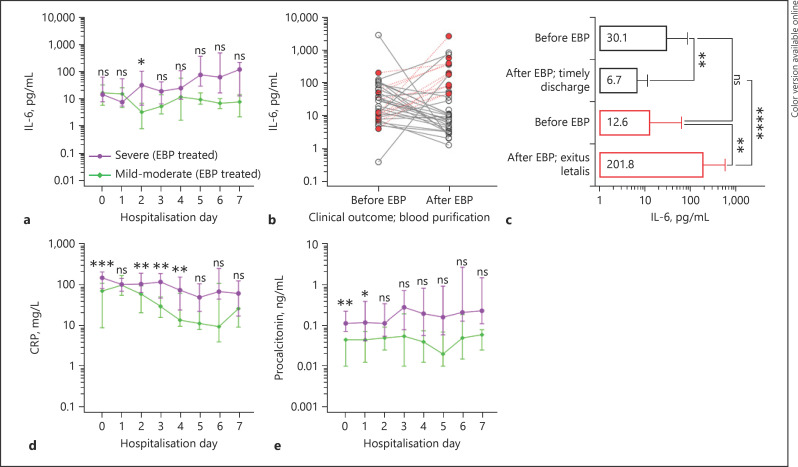
IL-6 is one of the hallmark cytokines associated with COVID-19 [3]; in response to EBP (Fig 2), we observed opposing IL-6 trends associated with disease severity (Fig. 2a). Subsequent individual paired analysis proposes a base for the observed heterogeneity in systemic IL-6 levels in response to blood purification (Fig. 2b); overall, clinical recovery was associated with decreased IL-6 levels, median difference −21.44 pg/mL [95% CI −45.6 to −4.1], p = 0.0001. Whereas IL-6 continued to rise in patients who ultimately succumbed to the disease despite repetitive haemofiltration cycles, median difference 179.7 pg/mL [95% CI 42.02 to 613.3], p = 0.0009 (Fig. 2c).
Fig. 2.
Longitudinal biomarker profiling of severe COVID-19 patients treated with extracorporeal blood purification. Panel (a) shows the median systemic levels of IL-6 over the 1st 7 days in extracorporeal blood purification (EBP) treated patients stratified according to disease severity. Panel (b) represents individual IL-6 values before (pre) and after (post) EBP using oXiris® hemofilter, open circles (○) identify patients that were successfully discharged and closed red circles (●) mark those patients that succumbed to disease; adjacent graphs show the aggregated IL-6 data for COVID-19 patients who were successfully discharged (upper bar graphs), pre-versus post blood purification median difference of −21.44 pg/mL [95% CI −45.60 to −4.100], p = 0.0001. Mortality cases (lower bar graphs), median difference 179.7 pg/mL [95% CI 42.02 to 613.3], p = 0.0009.Panel (d) displays longitudinal concentrations of CRP and panel (e) values of Procalcitonin. For panels A, D, e: purple and green curves indicate COVID-19 patients with severe or mild-to-moderate symptoms.
IL-6 is the primary inducer of hepatic CRP synthesis and secretion; the acute-phase protein has been associated with COVID-19 mortality and morbidity [21, 22]. We observed that EBP was associated with a decrease of CRP in non-severe cohort, showing a significant time-dependent reduction β = −1.9 [95% CI −3.7 to −0.2], p = 0.03 (Fig. 2d; online suppl. Supplemental Fig. 1; for all online suppl. material, see www.karger.com/doi/10.1159/0005515627).
EBP was associated with a gradual normalization of several biomarkers (online suppl. Supplemental Figs. 1–3). For instance, we observed a decrease in inflammatory immune indices NLR, β = −0.49 [95% CI −0.89 to −0.09], p = 0.01 and SII, β = −79.6 [95% CI −131.3 to −27.9], p = 0.003.
We did not routinely screen for SARS-CoV-2 spike protein-specific IgG antibodies at admission; nevertheless, the available data suggest that severe cases presented with higher baseline titres that further increased over time (online suppl. Supplemental Fig. 1). BGA were comparable during the early phases of hospitalization; excluding the individual exceptions, there were no notable differences in BGA parameters over time across the cohort.
Severe cases requiring prolonged hospitalization (>2 weeks) showed possible signs of respiratory acidosis (ARDS) evidenced by decreasing pH values and increasing levels of the partial pressure of carbon dioxide on mechanical circulatory support (online suppl. Supplemental Fig. 3). Clinically, both subgroups were characterized by normalizing vital parameters over time (online suppl. Supplemental Fig. 4).
We observed 19 cases (43.2%) (Table 3) of secondary bacterial co-infections, most confirmed microbiology cultures pertained to samples collected at admission; furthermore, positive microbiology was most likely to occur in (severe) patients admitted from peripheral clinics, OR 3.6 [CI 95% 0.9 to 12.4], p = 0.07 and procalcitonin levels were higher in severe patients than cases with a milder severity profile.
We most frequently detected Staphylococcus aureus, Haemophilus influenzae, and Enterobacteriaceae; however, we also detected Klebsiella pneumoniae and Acinetobacter baumannii. The whole cohort's mortality rate was 27%; the rate in severe cases was 44 versus 4% in non-severe, relative risk (RR) 7 [95% CI 1.49 to 40.2], p = 0.007.
Discussion
COVID-19 is caused by SARS-CoV-2 and was identified by the World Health Organization as an international public health emergency; with that, a multitude of therapeutic approaches have been pioneered to counter the detrimental clinical manifestations [23, 24, 25, 26] linked to inflammatory immune disturbances. We here describe the clinical course, outcome, and longitudinal analysis of select biomarkers, and clinical and blood gas parameters in non-severe versus severe COVID-19 patients treated with blood purification using the cytokine adsorbing oXiris® haemofilter.
We and others have explored the use of cytokine blood purification in an attempt to prevent, control, or reduce (suspected) hyperinflammation [27, 28, 29, 30, 31]. Several blood purification devices are currently on the market, showing a significant reduction of pro-inflammatory cytokines and restore homoeostatic dysregulation associated with systemic inflammatory syndromes [32, 33, 34].
The US Food and Drug Administration gave emergency approval to the oXiris® membrane filter and CytoSorb® column-based filter. Both devices have shown an exceptional capacity to reduce cytokine levels [33, 35], support haemodynamic stabilization, and increase survival probability, especially in patients whom therapy was initiated early [36, 37].
We previously reported our preliminary results on EBP using the oXiris® filter in COVID-19 [20]. The cohort's limited size precluded comparative analyses between patient subgroups stratified according to disease severity. With this follow-up study on an expanded cohort, we show that EBP was paired with a longitudinal reduction of numerous inflammatory mediators, acute phase proteins, and resolution of cytopenias (online suppl. Supplemental Fig. 1).
For instance, EBP was associated with a time-dependent decrease across the cohort in ferritin levels, a well-described biomarker associated with severe COVID-19 [38, 39]. Interestingly, oXiris® was associated with a significant decline over time of CRP in non-severe cases but not in severe cases.
Moreover, our results suggest a weaker association between IL-6 and CRP in COVID-19 patients treated with EBP; the 2 markers showed a weak(er) correlation (r = 0.05, p = 0.66, non-severe and r, = 0.35, p < 0.001, severe cases) (online suppl. Supplemental Fig. 5). IL-6 is the main stimulus for CRP synthesis, and others have described a strong positive correlation between IL-6 and CRP in numerous disease conditions [40, 41, 42].
Systemic levels of CRP were more detected in critical ranges than in IL-6. The cytokine was increased in severe cases, but overall, the systemic levels measured were lower than observed in our historical bacterial sepsis cohort. The higher levels of CRP irrespective of IL-6 might be explained as follows: IL-6 is the primary driver of increased CRP production; however, during injury or other trauma, other pro-inflammatory cytokines such as IL-1, TNF-α, and IL-8 may contribute the production of CRP [43, 44, 45].
Current literature indicates that although IL-6 is essential for CRP gene induction, it is not sufficient to achieve this alone [46] and might require orchestrated stimuli by multiple pro-inflammatory cytokines to boost CRP gene expression. Collectively, the increased levels of IL-1, TNF-α, IL-8, and IL-6 seen in COVID-19 plausibly synergize to enhance CRP gene expression [47].
Recently, 3 studies have compared cytokine levels in COVID-19 to other conditions [47, 48, 49] and hinted that the term “cytokine storm” is perhaps not applicable to COVID-19 as was previously postulated. It is possibly a case of semantics; the immunological disturbances in COVID-19 encompass both innate and adaptive arms [4, 47, 50] and clinically possess many hallmarks of cytokine storm syndrome [51, 52].
The incidence of bacterial co-infection (43%) was higher than previously reported [53, 54, 55]. In compliance with antimicrobial resistance guidelines [56, 57], we collect nasopharyngeal samples and also perform hemocultures in critical COVID-19 cases at admission. We detected bacterial co-infections more frequently in patients previously hospitalized at peripheral clinics than the subgroup admitted from home.
Empirical antibiotics are administered for maximum 48 h or discontinued immediately following negative representative cultures [58]. It is possible that our antimicrobial resistance protocol may be masked by unnecessary antibiotic administration elsewhere, a common clinical practice in south-eastern Europe [59, 60, 61, 62].
Clinically, the heterogeneity among the severe cases was striking; the clinical course of severe COVID-19, the extent of the affected lung area, and ARDS development were often not aligned with systemic levels of biomarkers. Several critical cases in need of mechanical ventilation and inotrope support showed clinical deterioration despite decreasing inflammatory mediators. Interestingly, we observed just 2 cases of AKI during the study period; a surprising finding provided the pooled incidence rate of 8.9% (95% CI 4.6 to 14.5) reported by Chen et al. [63]. Finally, the observed mortality rate of 27% observed in this case series is comparable to what has been recently reported [64].
Limitations
Because of the observational design, the absence of randomization and limited cohort size, we are unable to formally assess the effectiveness of EBP and cannot provide evidence of a causal relationship between this specific EBP and improved clinical outcome. We encourage further research in this setting; large randomized controlled trials are warranted to determine the optimal EBP strategy to control COVID-19 disease progression and prevent ARDS. Nevertheless, with 3,000+ accumulated hours of EBP run-time and real-time data on 44 patients, we collected sufficient data points to establish biomarker fluctuations over time and evaluate the safety profile of oXiris® blood purification.
Conclusion
Our results suggest that EBP with oXiris® haemofilter is safe and was associated with reduced levels of CRP, and control of IL-6 and procalcitonin in COVID-19 patients. Repetitive haemofiltration was associated with a reduction of ferritin, NLR, SII, and restoration of immune cell homoeostasis in COVID-19 patients. EBP may represent an attractive treatment modality to limit systemic damage caused by aberrant immune activation and therefore might stabilize the clinical condition of COVID-19 patients. Despite the encouraging results, high-quality randomized controlled trials are warranted to provide solid evidence and advance clinical practice.
Statement of Ethics
The local Ethical Committee of the Zan Mitrev Clinic reviewed and approved the clinical practice, treatment procedures described, and the results reported in this article and approved the submission, #EBPZ.357 (trial registration: ClinicalTrials.gov, NCT04478539. Registered July 14, 2020 − retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT04478539).
Written informed (or temporary verbal) consent was obtained from all patients for publication of this article and any accompanying images; the use of all health and medical information for scientific research and manuscript preparation was approved. A copy of the written consent is available for review by the editor-in-chief of this journal. For those patients not traceable after discharge, the Ethical Committee waived the need for informed consent.
Conflict of Interest Statement
Dr Zan Mitrev is the hospital director at the Zan Mitrev Clinic. Gianluca Villa is the editor of blood purification and he has received support for travel expenses, hotel accommodations, and registration to meetings from Baxter. The other co-authors do not have any competing interests to disclose.
Funding Sources
Not applicable.
Author Contributions
Z.M. is the study director; P.U., D.P., D.N., L.V.K., and Z.M. were responsible for diagnostics and patient care. L.V.-K. performed the radiological examinations. R.R. coordinated the study, managed data collection, and analysed the data. R.R. and G.V. provided academic assistance, wrote the manuscript with the assistance of G.V., and critically reviewed the manuscript. A.T. and D.K. provided IT support for data validation/extraction. All authors have read and approved the manuscript.
Availability of Data and Material
The data used for this study are currently in transfer in the SCCM COVID-19 registry (https://sccmcovid19.org/). Until upload is completed, the data are available for review upon reasonable request by editorial staff members. This article was posted as a preprint on MedRxiv [65].
Supplementary Material
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Supplementary data
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395((10223)):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio-Med. 2020 Mar 19;91((1)):157–60. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fara A, Mitrev Z, Rosalia RA, Assas BM. Cytokine storm and COVID-19: a chronicle of pro-inflammatory cytokines. Open Biol. 2020;10((9)):200160. doi: 10.1098/rsob.200160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lucas C, Wong P, Klein J, Castro TBR, Silva J, Sundaram M, et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 2020 Aug 1;584((7821)):463–9. doi: 10.1038/s41586-020-2588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020 Mar 23;27:1451–4. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang L, Liu S, Liu J, Zhang Z, Wan X, Huang B, et al. COVID-19: immunopathogenesis and Immunotherapeutics. Signal Transduct Target Ther. 2020 Jul 25;5((1)):128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao Y, Nie HX, Hu K, Wu XJ, Zhang YT, Wang MM, et al. Abnormal immunity of non-survivors with COVID-19: predictors for mortality. Infect Dis Poverty. 2020 Aug 3;9((1)):108. doi: 10.1186/s40249-020-00723-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 11;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135((23)):2033–40. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Lancet Haematology COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020;7((6)):e425. doi: 10.1016/S2352-3026(20)30151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 Mar 3;46:846–8. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. 2020;5:1281–5. doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–73. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadim MK, Forni LG, Mehta RL, Connor MJ, Liu KD, Ostermann M, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat Rev Nephrol. 2020 Dec 1;16((12)):747–64. doi: 10.1038/s41581-020-00356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pei G, Zhang Z, Peng J, Liu L, Zhang C, Yu C, et al. Renal Involvement and early prognosis in patients with COVID-19 pneumonia. J Am Soc Nephrol. 2020;31((6)):1157–65. doi: 10.1681/ASN.2020030276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asgharpour M, Mehdinezhad H, Bayani M, Zavareh MSH, Hamidi SH, Akbari R, et al. Effectiveness of extracorporeal blood purification (hemoadsorption) in patients with severe coronavirus disease 2019 (COVID-19) BMC Nephrol. 2020 Aug 20;21((1)):356. doi: 10.1186/s12882-020-02020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ronco C, Bagshaw SM, Bellomo R, Clark WR, Husain-Syed F, Kellum JA, et al. Extracorporeal blood purification and organ support in the critically Ill patient during COVID-19 pandemic: expert review and recommendation. Blood Purif. 2020;50:17–27. doi: 10.1159/000508125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Villa G, Romagnoli S, De Rosa S, Greco M, Resta M, Pomarè Montin D, et al. Blood purification therapy with a hemodiafilter featuring enhanced adsorptive properties for cytokine removal in patients presenting COVID-19: a pilot study. Crit Care. 2020 Oct 12;24((1)):605. doi: 10.1186/s13054-020-03322-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ugurov P, Popevski D, Gramosli T, Neziri D, Vuckova D, Gjorgon M, et al. Early initiation of extracorporeal blood purification using the AN69ST (oXiris®) hemofilter as a treatment modality for COVID-19 patients: a single-centre case series. Braz J Cardiovasc Surg. 2020 doi: 10.21470/1678-9741-2020-0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luo X, Zhou W, Yan X, Guo T, Wang B, Xia H, et al. Prognostic value of C-reactive protein in patients with coronavirus 2019. Clin Infect Dis. 2020 Nov 19;71((16)):2174–9. doi: 10.1093/cid/ciaa641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharifpour M, Rangaraju S, Liu M, Alabyad D, Nahab FB, Creel-Bulos CM, et al. C-reactive protein as a prognostic indicator in hospitalized patients with COVID-19. PloS One. 2020;15((11)):e0242400. doi: 10.1371/journal.pone.0242400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coronavirus drugs trials must get bigger and more collaborative. Nature. 2020 May 13;581((7807)):120. doi: 10.1038/d41586-020-01391-9. [DOI] [PubMed] [Google Scholar]
- 24.Health NIo Guidelines introduction|coronavirus disease COVID-19. @NIHCOVIDTxGuide. 2020 [Google Scholar]
- 25.Ngo BT, Marik P, Kory P, Shapiro L, Thomadsen R, Iglesias J, et al. A systematic analysis of the time course to develop treatments for COVID-19. medRxiv. 2020 [Google Scholar]
- 26.Riva L, Yuan S, Yin X, Martin-Sancho L, Matsunaga N, Pache L, et al. Discovery of SARS-CoV-2 antiviral drugs through large-scale compound repurposing. Nature. 2020 Jul 24;586:113–9. doi: 10.1038/s41586-020-2577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rieder M, Zahn T, Benk C, Lother A, Bode C, Staudacher D, et al. Cytokine adsorption in a patient with severe coronavirus disease 2019 related acute respiratory distress syndrome requiring extracorporeal membrane oxygenation therapy: a case report. Artif Organs. 2021;45:191–4. doi: 10.1111/aor.13805. [DOI] [PubMed] [Google Scholar]
- 28.Zhang H, Zhu G, Yan L, Lu Y, Fang Q, Shao F. The absorbing filter Oxiris in severe coronavirus disease 2019 patients: a case series. Artif Organs. 2020;44:1296–1302. doi: 10.1111/aor.13786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al Shareef K, Bakouri M. Cytokine blood filtration responses in COVID-19. Blood Purif. 2021;50:141–9. doi: 10.1159/000508278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Damiani M, Gandini L, Landi F, Fabretti F, Gritti G, Riva I. Extracorporeal cytokine hemadsorption in severe COVID-19 respiratory failure. medRxiv. 2020 doi: 10.1016/j.rmed.2021.106477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rieder M, Wengenmayer T, Staudacher D, Duerschmied D, Supady A. Cytokine adsorption in patients with severe COVID-19 pneumonia requiring extracorporeal membrane oxygenation. Crit Care. 2020 Jul 14;24((1)):435. doi: 10.1186/s13054-020-03130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Villa G, Zaragoza JJ, Sharma A, Neri M, De Gaudio AR, Ronco C. Cytokine removal with high cut-off membrane: review of literature. Blood Purif. 2014;38((3–4)):167–73. doi: 10.1159/000369155. [DOI] [PubMed] [Google Scholar]
- 33.Malard B, Lambert C, Kellum JA. In vitro comparison of the adsorption of inflammatory mediators by blood purification devices. Intensive Care Med Exp. 2018 May 4;6((1)):12. doi: 10.1186/s40635-018-0177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen G, Zhou Y, Ma J, Xia P, Qin Y, Li X. Is there a role for blood purification therapies targeting cytokine storm syndrome in critically severe COVID-19 patients? Renal Failure. 2020 Nov;42((1)):483–8. doi: 10.1080/0886022X.2020.1764369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Broman ME, Hansson F, Vincent JL, Bodelsson M. Endotoxin and cytokine reducing properties of the oXiris membrane in patients with septic shock: a randomized crossover double-blind study. PloS One. 2019;14((8)):e0220444. doi: 10.1371/journal.pone.0220444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kogelmann K, Jarczak D, Scheller M, Drüner M. Hemoadsorption by CytoSorb in septic patients: a case series. Crit Care. 2017 Mar 27;21((1)):74. doi: 10.1186/s13054-017-1662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Monard C, Rimmelé T, Ronco C. Extracorporeal blood purification therapies for sepsis. Blood Purif. 2019;47((Suppl 3)):2–15. doi: 10.1159/000499520. [DOI] [PubMed] [Google Scholar]
- 38.Gómez-Pastora J, Weigand M, Kim J, Wu X, Strayer J, Palmer AF, et al. Hyperferritinemia in critically ill COVID-19 patients - Is ferritin the product of inflammation or a pathogenic mediator? Clin Chim Acta. 2020;509:249–51. doi: 10.1016/j.cca.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Velavan TP, Meyer CG. Mild versus severe COVID-19: laboratory markers. Int J Infect Dis. 2020 Jun 1;95:304–7. doi: 10.1016/j.ijid.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pourcyrous M, Korones SB, Crouse D, Bada HS. Interleukin-6 (IL-6) and C-reactive protein (CRP) Responses to Immunization in Premature Babies † 1007. Pediatric Res. 1997 Apr 1;41((4)):170. doi: 10.1542/peds.101.3.e3. [DOI] [PubMed] [Google Scholar]
- 41.McArdle PA, McMillan DC, Sattar N, Wallace AM, Underwood MA. The relationship between interleukin-6 and C-reactive protein in patients with benign and malignant prostate disease. Br J Cancer. 2004 Nov 1;91((10)):1755–7. doi: 10.1038/sj.bjc.6602211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Panichi V, Manca-Rizza G, Paoletti S, Taccola D, Consani C, Filippi C, et al. Effects on inflammatory and nutritional markers of haemodiafiltration with online regeneration of ultrafiltrate (HFR) vs online haemodiafiltration: a cross-over randomized multicentre trial. Nephrol Dial Transplant. 2006 Mar;21((3)):756–62. doi: 10.1093/ndt/gfi189. [DOI] [PubMed] [Google Scholar]
- 43.Wigmore SJ, Fearon KC, Maingay JP, Lai PB, Ross JA. Interleukin-8 can mediate acute-phase protein production by isolated human hepatocytes. Am J Physiol. 1997 Oct;273((4 Pt 1)):E720–6. doi: 10.1152/ajpendo.1997.273.4.E720. [DOI] [PubMed] [Google Scholar]
- 44.Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340((6)):448–54. doi: 10.1056/NEJM199902113400607. [DOI] [PubMed] [Google Scholar]
- 45.Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 2018;9:754. doi: 10.3389/fimmu.2018.00754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weinhold B, Bader A, Poli V, Rüther U. Interleukin-6 is necessary, but not sufficient, for induction of the humanC-reactive protein gene in vivo. Biochem J. 1997 Aug 1;325((Pt 3)):617–21. doi: 10.1042/bj3250617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Del Valle DM, Kim-Schulze S, Huang H-H, Beckmann ND, Nirenberg S, Wang B, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020 Aug 24;26:1636–43. doi: 10.1038/s41591-020-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kox M, Waalders NJB, Kooistra EJ, Gerretsen J, Pickkers P. Cytokine levels in critically Ill patients with COVID-19 and other conditions. JAMA. 2020;324:1565–7. doi: 10.1001/jama.2020.17052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sinha P, Matthay MA, Calfee CS. Is a “Cytokine Storm” relevant to COVID-19? JAMA Intern Med. 2020;180((9)):1152–4. doi: 10.1001/jamainternmed.2020.3313. [DOI] [PubMed] [Google Scholar]
- 50.Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020 Jun 16;11((1446)):1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chau AS, Weber AG, Maria NI, Narain S, Liu A, Hajizadeh N, et al. The longitudinal immune response to coronavirus disease 2019: chasing the cytokine storm. Arthritis Rheumatol. 2021;73:23–35. doi: 10.1002/art.41526. [DOI] [PubMed] [Google Scholar]
- 52.Chen LYC, Hoiland RL, Stukas S, Wellington CL, Sekhon MS. Confronting the controversy: interleukin-6 and the COVID-19 cytokine storm syndrome. Eur Respir J. 2020;56((4)):2003006. doi: 10.1183/13993003.03006-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sieswerda E, De Boer MGJ, Bonten MMJ, Boersma WG, Jonkers RE, Aleva RM, et al. Recommendations for antibacterial therapy in adults with COVID-19 − An evidence based guideline. Clin Microbiol Infect. 2021;27:61–6. doi: 10.1016/j.cmi.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Contou D, Claudinon A, Pajot O, Micaëlo M, Longuet Flandre P, Dubert M, et al. Bacterial and viral co-infections in patients with severe SARS-CoV-2 pneumonia admitted to a French ICU. Ann Intensive Care. 2020 Sep 7;10((1)):119. doi: 10.1186/s13613-020-00736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van den Bosch CM, Hulscher ME, Natsch S, Gyssens IC, Prins JM, Geerlings SE. Development of quality indicators for antimicrobial treatment in adults with sepsis. BMC Infect Dis. 2014 Jun 20;14:345. doi: 10.1186/1471-2334-14-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.WHO . Clinical management of severe acute respiratory infections (SARI) when COVID-19 disease is suspected. World Health Organization Geneva; 2020. [Google Scholar]
- 58.Adler H, Ball R, Fisher M, Mortimer K, Vardhan MS. Low rate of bacterial co-infection in patients with COVID-19. Lancet Microbe. 2020;1((2)):e62. doi: 10.1016/S2666-5247(20)30036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Versporten A, Bolokhovets G, Ghazaryan L, Abilova V, Pyshnik G, Spasojevic T, et al. Antibiotic use in eastern Europe: a cross-national database study in coordination with the WHO Regional Office for Europe. Lancet Infect Dis. 2014 May;14((5)):381–7. doi: 10.1016/S1473-3099(14)70071-4. [DOI] [PubMed] [Google Scholar]
- 60.Horvat O, Mijatović V, Milijasević B, Tomas A, Kusturica MP, Tomić Z, et al. Are there striking differences in outpatient use of antibiotics between South Backa District, Serbia, and Some Scandinavian Countries? Front Public Health. 2018;6:91. doi: 10.3389/fpubh.2018.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jakupi A, Raka D, Kaae S, Sporrong SK. Culture of antibiotic use in Kosovo - an interview study with patients and health professionals. Pharm Pract. 2019 Jul-Sep;17((3)):1540. doi: 10.18549/PharmPract.2019.3.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van den Hof S. Central Asian and European surveillance of antimicrobial resistance. Annual report 2019. 2019 Nov 18 [Google Scholar]
- 63.Chen Y-T, Shao S-C, Hsu C-K, Wu I-W, Hung M-J, Chen Y-C. Incidence of acute kidney injury in COVID-19 infection: a systematic review and meta-analysis. Crit Care. 2020;24((1)):346–6. doi: 10.1186/s13054-020-03009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Quah P, Li A, Phua J. Mortality rates of patients with COVID-19 in the intensive care unit: a systematic review of the emerging literature. Crit Care. 2020 Jun 4;24((1)):285. doi: 10.1186/s13054-020-03006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rosalia R, Ugurov P, Neziri D, Despotovska S, Veljanovska-Kiridjievska L, Kostoska E, et al. Extracorporeal Blood Purification in moderate and severe COVID-19 patients: a prospective cohort study. medRxiv. 2020 doi: 10.1159/000515627. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Supplementary data
Data Availability Statement
The data used for this study are currently in transfer in the SCCM COVID-19 registry (https://sccmcovid19.org/). Until upload is completed, the data are available for review upon reasonable request by editorial staff members. This article was posted as a preprint on MedRxiv [65].