Abstract
Objective:
To identify and summarize the behavior change techniques (BCTs) included in behavior change interventions for promoting physical activity in persons with multiple sclerosis (MS).
Data Sources:
PubMed, PsycINFO, CINAHL Complete, Scopus, and Embase were initially searched in November 2019, and data extraction began in June 2020.
Study Selection:
The inclusion criteria for studies were: adults over 18 years of age with diagnosed MS, English language, clinical trial (i.e., pre-post or randomized controlled trials) designs, group or individual interventions, and home or community-based settings wherein physical activity was defined as a primary or secondary outcome. Exclusion criteria for studies included: protocol manuscripts pending results, case studies, studies focused on multiple chronic disease populations, and interventions targeting multiple behaviors. Two researchers completed screening for study selection and a third researcher served as a referee. Of the initially identified 8,681 studies, 54 studies met selection criteria.
Data Extraction:
Data extraction was completed by three researchers. Each paper was coded by two of the three researchers and a fourth researcher resolved discrepancies. Data extracted from each paper included: study title, authors, country, year, sample size, study design, intervention details, physical activity outcomes, and BCTs.
Data Synthesis:
Thirty-eight unique behavior change interventions were identified and 53 of the 93 possible BCTs were included across the studies. The mean number of BCTs per study was 15 and studies and effect sizes across studies ranged from 0.04–1.49.
Conclusions:
This review provides a comprehensive overview of BCTs as the active ingredients in behavior change interventions targeting physical activity in MS. Results from this study provide a compendium for future intervention development for increasing physical activity and improving overall health in MS.
Keywords: Multiple Sclerosis, Exercise, Health Behavior, Systematic Review, Behavioral Medicine
Introduction
Multiple sclerosis (MS) is an immune-mediated and neurodegenerative disease of white and grey matter tissue in the central nervous system (CNS) with a prevalence of nearly 1 million cases in the United States (U.S.) and 2.8 million Worldwide.1,2 Persons with MS experience debilitating symptoms such as fatigue, depression, pain, mobility dysfunction, and cognitive impairment brought about by CNS damage.3–7 Physical activity is an efficacious method for improving such symptoms and slowing disease progression among those with MS.8 The benefits of physical activity for management of MS are even becoming more widely accepted among health care providers,9 yet fewer than 20% of persons with MS engage in sufficient amounts of health promoting physical activity.10 Indeed, persons with MS must overcome significant challenges and barriers that influence physical activity behavior such as debilitating fatigue and depression, mobility limitations, reduced community accessibility, and lack of social and caregiver support.11
One approach for changing physical activity behavior in MS has involved the delivery of behavior change interventions that integrate behavior change techniques (BCTs) based on behavior change theory,10 and the feasibility and effect of such behavior change interventions for increasing physical activity have been summarized in systematic reviews and/or metaanalyses.12–16 For example, one meta-analysis examined the effects of interventions for increasing physical activity in MS, and reported moderate immediate (d = .56) and sustained (d = .53) increases in physical activity.15 There further were larger effects for behavior change interventions (d = .71) than exercise training (d = .53) or combined (d = .37) interventions.15 Behavior change interventions provide individuals with skills, strategies, and resources for physical activity behavior change, whereas exercise training tests the efficacy of a specific exercise stimulus or prescription on an outcome such as symptoms or disease progression. The behavior change interventions were largely based on Social Cognitive Theory and motivational interviewing, yet there was no information provided regarding BCTs included in the behavior change interventions. Another meta-analysis examined the effects of randomized controlled trials (RCTs) involving behavior change interventions for increasing physical activity behavior in MS, and reported significant increases in self-reported (d = 1.00), but not objectively measured (d = .34), physical activity.16 The theories utilized among the 14 RCTs included Social Cognitive Theory, Transtheoretical Model, Health Belief Model, Self-efficacy Theory, and Pender Model of Health Promotion, and BCTs were coded using the 40-item CALO-RE BCT taxonomy.16 The most common BCT identified was goal setting (behavior) (n=11), followed by barrier identification/problem solving and prompt self-monitoring (n=9) and the most BCTs coded in one study was 13.16 Importantly, the CALO-RE BCT taxonomy provides a relatively limited understanding of the active ingredients underlying change in physical activity behavior among persons with MS as it was a preliminary step in developing more robust tools for assessing BCTs in behavior change interventions.
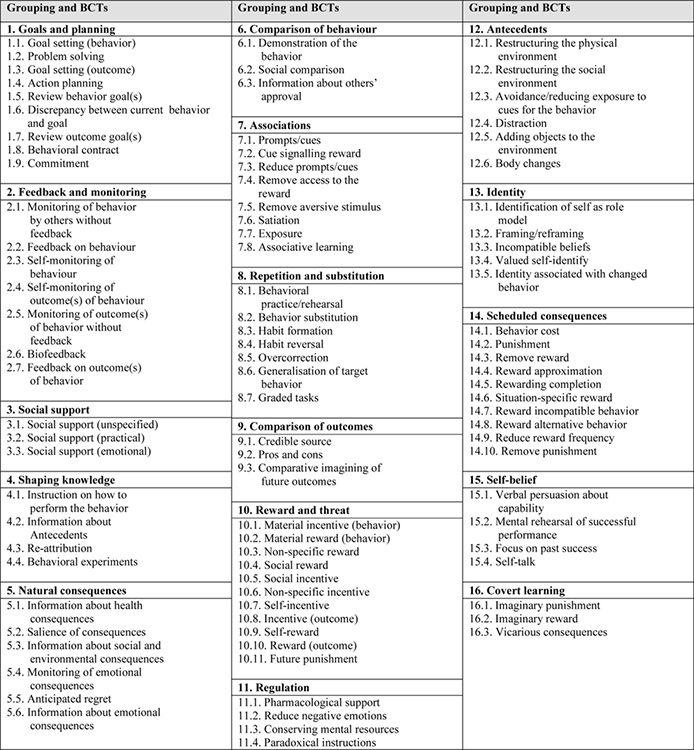
The aforementioned meta-analyses provide an initial step in understanding physical activity behavior change in MS, yet recent initiatives in behavioral medicine underscore the importance of improving the design, delivery, and reporting of such behavior change interventions.17,18 Behavior change interventions are defined as coordinated sets of activities designed for changing specific behaviors such as physical activity, diet, and smoking.19 One key component in the design and delivery of behavior change interventions is the inclusion of BCTs, as these are the active agents of behavior change. The creation of a novel consensus taxonomy was the first step for bringing behavioral scientists together in using common language for BCTs. The Behavior Change Technique Taxonomy was created in collaboration with 14 experts in behavioral science that includes 93 unique BCTs categorized into 16 groups.20 For example, the “Goals and planning” group includes 9 BCTs of goal setting (behavior), problem solving, goal setting (outcome), action planning, review behavior goal(s), discrepancy between current behavior and goal, review outcome goal(s), behavioral contract, and commitment. The taxonomy further provides definitions and examples for each unique BCT. The BCT taxonomy is now accompanied by structured online training and resources that allow for the identification of BCTs in systematic reviews and meta-analyses as a guide for future research.
To date, we are unaware of a focal, comprehensive review and synthesis of BCTs utilized in behavior change interventions promoting physical activity in MS using the novel BCT taxonomy, yet this has been done in other populations such as spinal cord injury and cardiovascular disease.21–23 For example, one recent systematic review was completed in spinal cord injury wherein researchers coded and identified 32 of the possible 93 BCTs included in leisure-time physical activity interventions.23 The most commonly reported BCTs were 4.1. instruction on how to perform the behavior, 1.1. goal setting (behavior), 3.2. social support (practical), 9.1. credible source, 1.2. problem solving, and 1.4. action planning. Similar approaches have been utilized in various other populations with chronic diseases such as cardiac rehabilitation and focused on a range of behaviors, including physical activity and smoking cessation.21,22,24 The commonly used BCTs were 1.1 goal setting (behavior), 3.1 social support (unspecified), and 4.1 instruction on how to perform behavior; however, patterns unique to disease and behavior are apparent such as 11.2 reduce negative emotions in cardiac rehabilitation and 10.4 social-reward in smoking cessation. This growing body of research allows for a better understanding of the most efficacious BCTs as well as the identification of neglected BCTs that may be used in future behavior change interventions.
The current systematic review identified and summarized BCTs included in behavior change interventions for physical activity in persons with MS. This systematic review further highlighted the particular BCTs that may be associated with physical activity change. Such a focus will provide an important road map for future research in this area and may yield better-informed behavior change interventions for physical activity in MS.
Methods
This systematic review is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance, and the protocol was registered on PROSPERO (CRD42020191858).25 Behavior change interventions were identified using the established definition: coordinated sets of activities designed to change specified behavior patterns.19 We created an additional more descriptive definition: programs that provide instruction and application of skills, strategies, and resources for behavior change. The inclusion criteria for studies were: adults over 18 years of age with diagnosed MS, English language, clinical trial (i.e., pre-post and RCT results) designs, group or individual interventions, and home or community-based settings. The studies needed to specify a primary or secondary outcome directly assessing physical activity behavior change, which may include device-measures, self-report, or adherence. Exclusion criteria for studies included: intervention protocols pending results, case studies, studies focused on other chronic disease populations, and interventions targeting multiple behaviors. Inclusion/exclusion criteria were kept broad for an expansive identification and overview of physical activity behavior change interventions in MS.
Five databases were initially searched on November 25th, 2019, and data extraction began on June 11th, 2020. The databases included: PubMed, PsycINFO, CINAHL Complete, Scopus, and Embase. The database searches were restricted to studies published in English, Adults, and Humans. Additional filters were applied in PsychINFO, CINAHL, and Scopus that identify only peer-reviewed, scholarly articles. Search terms included terms specific to physical activity (i.e., exercise, fitness, walking, exercise promotion, leisure activity, physical education, exercise training, exercise therapy, motor activity, physical training, actigraphy, actigraph, and physical activity) behavior change interventions (i.e., behavior change, program evaluation, programme, program, intervention studies, treatment outcome, behavioral intervention, intervention) and multiple sclerosis. The detailed search strategy information for specific databases are included in Appendix 1.
The PRISMA flow diagram is provided in Figure 1. The primary researcher conducted the database search and uploaded data into Covidence, a web-based tool for conducting systematic reviews that identified duplicates. After identification of duplicates, this same researcher completed an initial title review. The primary and secondary researchers then completed the abstract review followed by full-text review; a third researcher served as a referee for resolving discrepancies in both phases.
Figure 1.
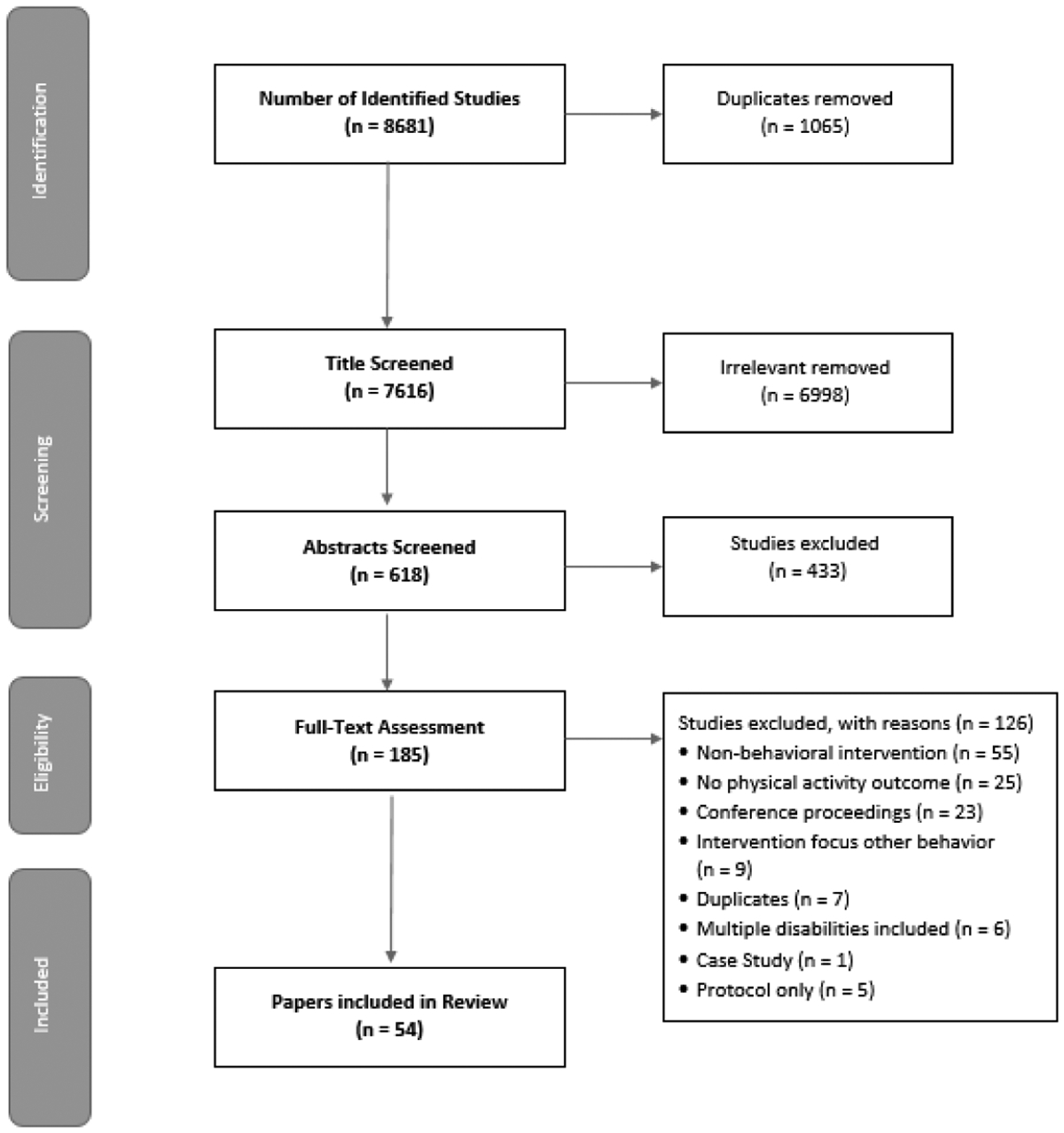
PRISMA Flow Diagram
Data extraction was completed by the initial three researchers, with each paper coded by two of those three researchers. Data extracted from each paper included: study title, authors, country, year, sample size, study design, intervention details, physical activity outcomes, and BCTs. The BCT Taxonomy version 1 (Appendix 2) guided identification and coding of BCTs within the included studies. BCT coding included extraction of relevant text, and a fourth researcher served as a referee for resolving discrepancies after coding of all BCTs in the included studies. All four researchers involved in data extraction completed the BCT Taxonomy online training. When multiple publications for the same study were identified, BCTs were identified and combined across the publications and reported as one overall study or case. Inter-rater reliability of coding BCTs was calculated using interclass correlation (ICC) analyses.
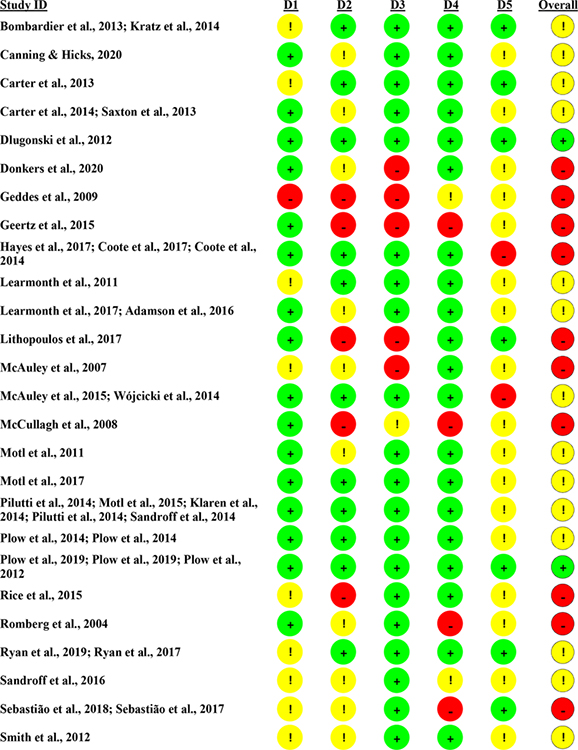
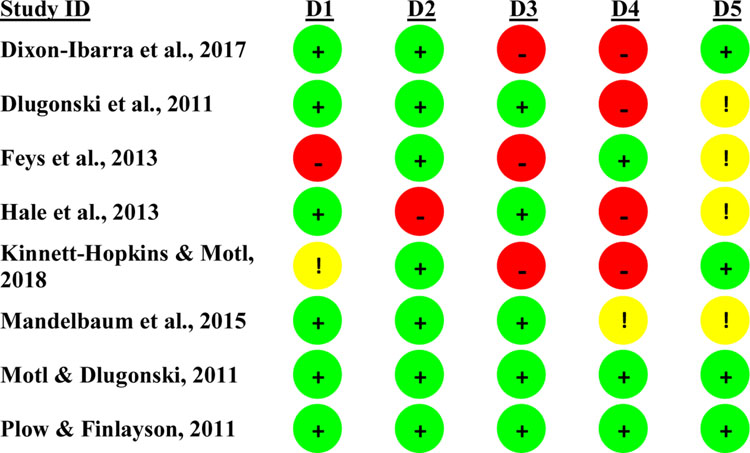
Assessment of Risk Bias was conducted for all included studies. The Cochrane Collaboration’s updated Risk of Bias 2 (RoB 2) tool was applied for RCTs and Mixed Methods Appraisal Tool (MMAT) 2018 version for pre-post studies.26,27 Each study was assessed by two researchers and discrepancies were reconciled between the two assigned researchers. Overall results for Assessment of Risk Bias are presented in Figures 2 and 3 and study-specific results are presented in Appendix 3 and 4.
Figure 2.
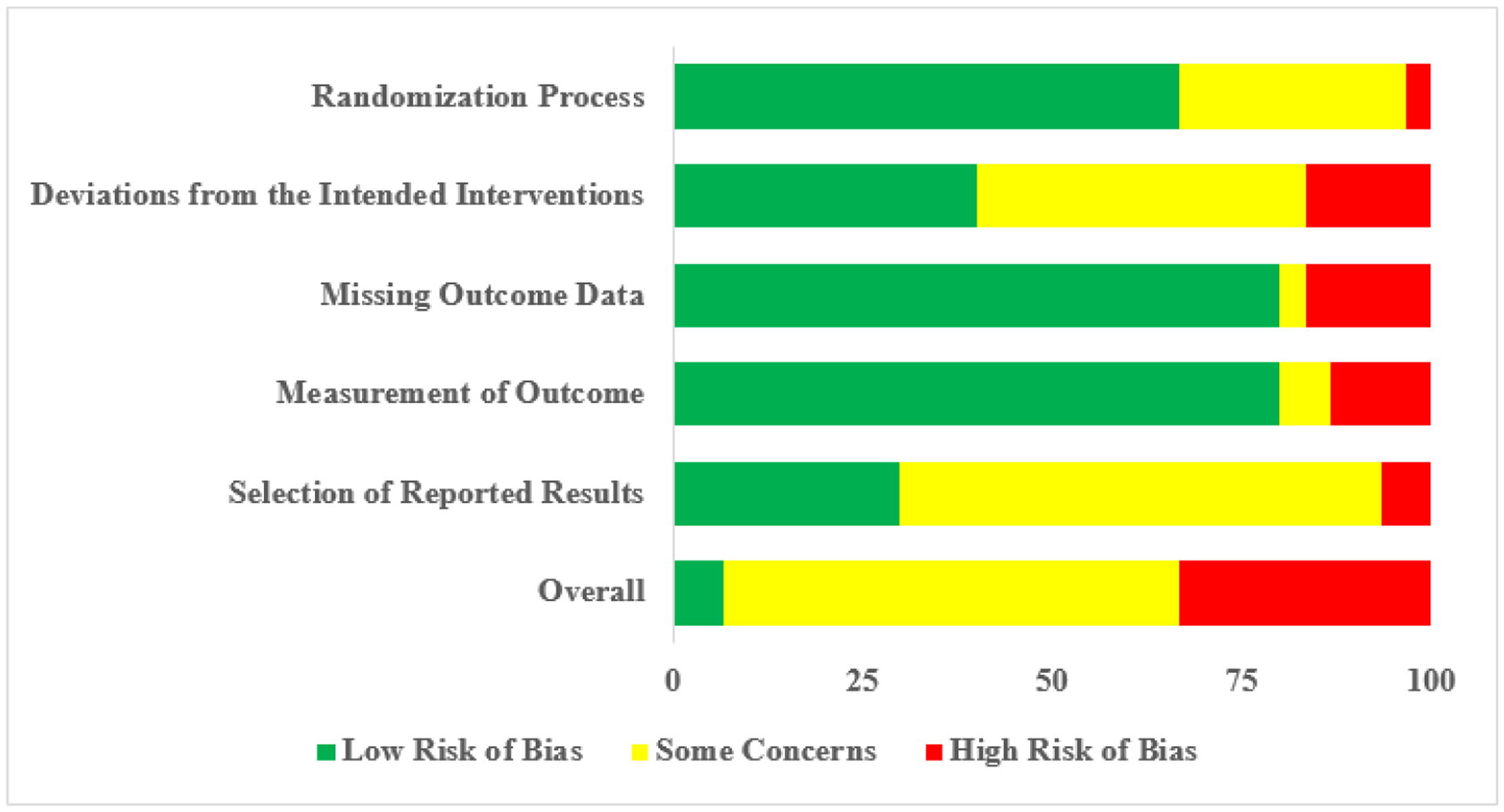
Risk of Bias Results using the RoB2 for Randomized Controlled Trials
Figure 3.
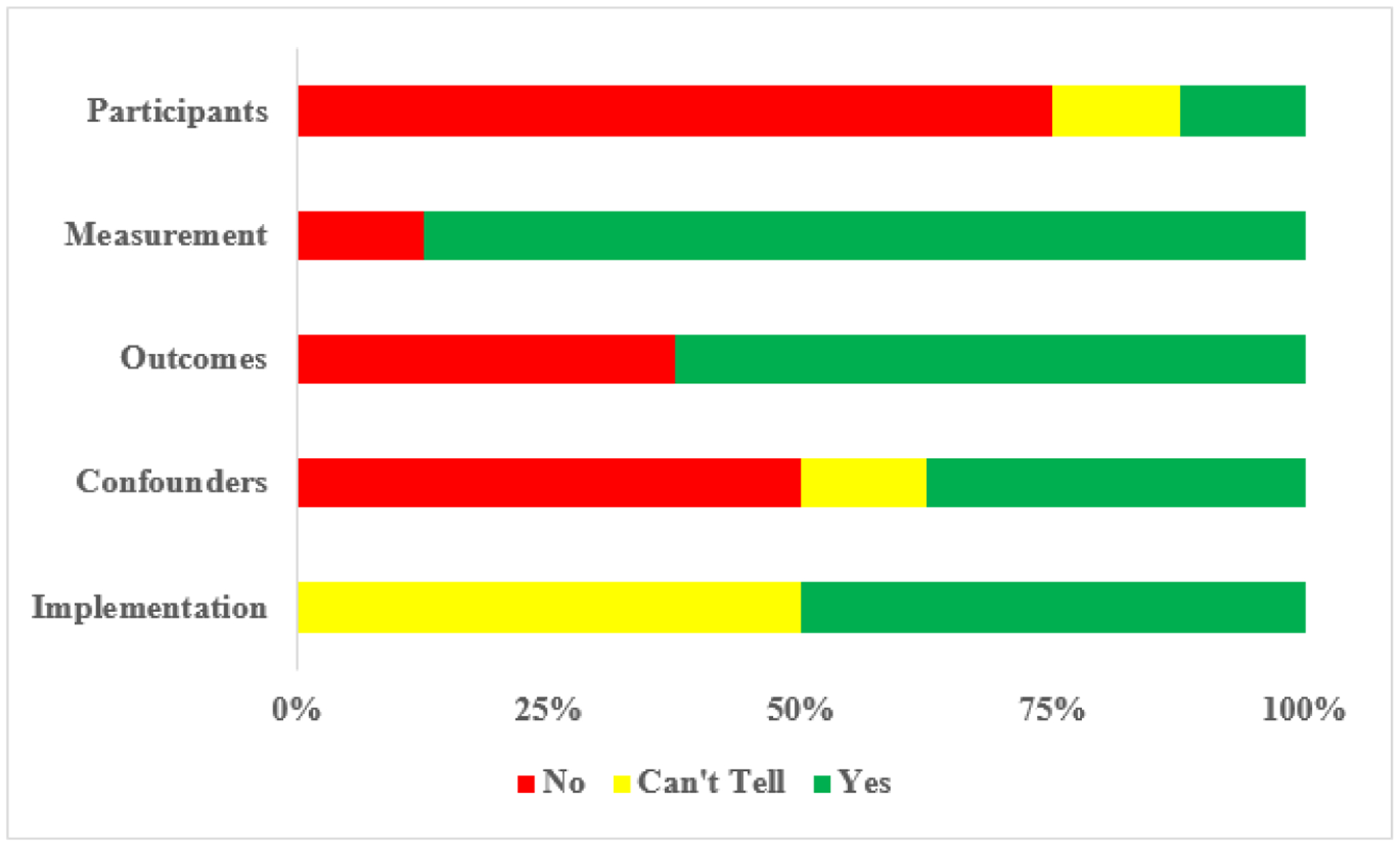
Risk of Bias Results using Mixed-Methods Appraisal Tool for Pre-Post Study Designs
The focus of this report is to provide a compendium of BCTs used in previous physical activity interventions by providing comprehensive descriptive statistics regarding the use and frequency of BCTs across interventions. We further provide effect sizes for change in physical activity where appropriate. Effect sizes were calculated or extracted based on the following criteria: (i) when post-intervention outcome values were available for RCTs, the research team calculated Cohen’s d effect size and where appropriate standard error (SE) was converted to standard deviation (SD), (ii) when post-intervention values were not available for RCTs and mean difference in change between groups was available, Cohen’s d effect size was calculated using pooled baseline SD, (iii) pre-post study design author-reported effect size values are reported. The research team extracted the author-reported significance levels for all applicable physical activity outcomes. Additionally, Chi-Square analyses were used as descriptive post-hoc analysis to examine differences in physical activity change between studies that reported 15 or more BCTs (i.e., mean across studies) and 14 or fewer BCTs.
Results
The overall database search identified 8,861 studies, of which 1,065 were initially identified as duplicates. Title screening by the primary researcher led to the identification of 6,998 irrelevant studies. The primary and secondary researchers screened 618 abstracts in which 433 were excluded for a final total of 185 studies assessed in the full-text assessment phase. Of the 185, we included 54 studies in the final review, of which studies with multiple manuscripts describing primary and secondary results were paired, yielding a final total of 38 behavior change interventions for identifying BCTs.
Study characteristics are reported in Table 1. Studies were grouped by research design (i.e., RCT and pre-post) for reporting of results. Thirty studies were RCTs28–73 and eight were pre-post designs74–81 Twenty-three studies were carried out in the United States, whereas 11 studies were carried out in Europe, three studies in Canada, and one study in New Zealand. Sample size among studies ranged between 8 and 208 participants.
Table 1.
Included Study Location, Sample Size, and Physical Activity Outcomes
| Author, Year | Recruitment Country | Sample (n)* | Objective PA Outcomes Effect Size (d), Significance (p) | Self Report PA Outcomes Effect Size (d), Significance (p) |
|---|---|---|---|---|
| RCT | ||||
| Bombardier et al., 2013; Kratz et al., 2014 | USA | 92 | N/A | 7-day PAR (0.45, 0.02) |
| Canning & Hicks, 2020 | Canada | 91 | Adherence (1.15, <0.05) | N/A |
| Carter et al., 2013 | UK | 28 | Adherence (NR) | GLTEQ (0.11, 0.59) |
| Carter et al., 2014; Saxton et al., 2013 | UK | 120 | Accelerometry (0.28, ≤0.01), Adherence (NR) | GLTEQ (0.51, ≤0.01) |
| Dlugonski et al., 2012 | USA | 45 | N/A | GLTEQ (0.87, 0.001) |
| Donkers et al., 2020 | Canada | 48 | Adherence (0.13, 0.21) | N/A |
| Geddes et al., 2009 | USA | 12 | Adherence (NR) | N/A |
| Geertz et al., 2015 | Germany | 47 | N/A | Self-Reported Physical Activity Outside the Study (NR) |
| Hayes et al., 2017; Coote et al., 2017; Coote et al., 2014 | Ireland | 65 | Accelerometry (−0.52, 0.81), Adherence (NR), | GLTEQ (−0.13, <0.01) |
| Learmonth et al., 2011 | UK | 32 | N/A | PhoneFITT (0.55, <0.001) |
| Learmonth et al., 2017; Adamson et al., 2016 | USA | 57 | Accelerometry (0.21, NS) | GLTEQ (0.64, <0.01) |
| Lithopoulos et al., 2017 | Canada | 206 | N/A | LTPAQ-SCI (0.34, <0.05) |
| McAuley et al., 2007 | USA | 26 | Adherence (0.48, 0.50) | N/A |
| McAuley et al., 2015; Wojcicki et al., 2014 | USA | 48 | N/A | GLTEQ Leisure (0.61, 0.05), GLTEQ MVPA (0.71, 0.02) |
| McCullagh et al., 2008 | Ireland | 30 | Adherence (NR) | N/A |
| Motl et al., 2011 | USA | 54 | N/A | GLTEQ (0.74, 0.01) |
| Motl et al., 2017 | USA | 47 | Accelerometry (0.36, 0.24) | GLTEQ (0.61, 0.05) |
| Pilutti et al., 2014; Motl et al., 2015; Klaren et al., 2014; Pilutti et al., 2014; Sandroff et al., 2014 | USA | 82 | Accelerometry (0.41, 0.07), Adherence (NR) | GLTEQ (0.77, 0.001), IPAQ (0.55, NR) |
| Plow et al., 2014; Plow et al., 2014 | USA | 30 | N/A | GLTEQ (0.61, 0.002), PADS (0.86, 0.004) |
| Plow et al., 2019; Plow et al., 2019; Plow et al., 2012 | USA | 208 | Accelerometry PA vs FM (0.41, 0.29), PA vs Control (0.69, 0.02) | GLTEQ PA vs FM (−0.05, 0.68), PA vs Control (0.36, 0.04) |
| Rice et al., 2015 | USA | 14 | Accelerometry (0.23, 0.65) | N/A |
| Romberg et al., 2004 | Finland | 114 | Adherence (NR) | N/A |
| Ryan et al., 2019; Ryan et al., 2017 | Ireland | 60 | Accelerometry (0.04, NS), Adherence (NR) | IPAQ (−0.54, NS) |
| Sandroff et al., 2016 | USA | 10 | Adherence (NR) | N/A |
| Sebastião et al., 2018; Sebastião et al., 2017 | USA | 26 | Adherence (NR), Pedometry (NR, <0.001) | N/A |
| Smith et al., 2012 | USA | 13 | Adherence (−0.50, NS) | N/A |
| Suh et al., 2015 | USA | 68 | N/A | GLTEQ (0.33, 0.02) |
| Tallner et al., 2016 | Germany | 126 | Adherence (NR) | BQ (0.56, S) |
| Thomas et al., 2017; Thomas et al., 2014 | UK | 30 | Accelerometry (NR), Adherence (NR) | GLTEQ (0.85, NR) |
| Turner et al., 2016 | USA | 64 | N/A | GLTEQ (0.45, 0.049) |
| Pre Post | ||||
| Dixon-Ibarra et al., 2017 | USA | 13 | Adherence (NR) | N/A |
| Dlugonski et al., 2011 | USA | 21 | Accelerometry (0.68, 0.006) | GLTEQ (0.34, 0.07), IPAQ (0.43, 0.03) |
| Feys et al., 2013 | Belgium | 57 | N/A | PASIPD (0.17, 0.08) |
| Hale et al., 2013 | New Zealand | 28 | N/A | Self-Reported Physical Activity Diary (−0.17, NR) |
| Kinnett-Hopkins & Motl, 2018 | USA | 32 | N/A | GLTEQ (1.49, <0.001) |
| Mandelbaum et al., 2015 | USA | 8 | Adherence (NR) | GLTEQ (NR, 0.01) |
| Motl & Dlugonski, 2011 | USA | 18 | Accelerometry (0.92, <0.001), Pedometry (1.04, <0.001) | GLTEQ (0.83, 0.0015), IPAQ (1.12, <0.001) |
| Plow & Finlayson, 2011 | USA | 30 | N/A | PADS (0.65, 0.001) |
Note: RCT= Randomized Controlled Trial; USA= United States of America; UK= United Kingdom; PAR= Physical Activity Recall; GLTEQ= Godin Leisure Time Exercise Questionnaire; IPAQ= International Physical Activity Questionnaire; LTPAQ-SCI= Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury; PADS= Physical Activity and Disability Survey; PASIPD= Physical Activity Scale for Individuals with Physical Disabilities; MVPA= Moderate-Vigorous Physical Activity; BQ= Baecke Questionnaire; NR= Not Reported; N/A= Not Applicable; NS= Not Significant; S= Significant No Value Provided; PA= PA Group; FM= Fatigue Management Group
RCTs= Sample Size Randomized
Overall, the mean number of BCTs identified among the 38 identified behavior change interventions was 15. The top four most frequently included BCTs were (a) 4.1 instructions on how to perform the behavior (89%; n=34), (b) 3.1 social support (unspecified) (84%; n=32), (c) 9.1 credible source (84%; n=32) and (d) 6.1 demonstration of the behavior (82%; n=31). One study reported in three papers included the greatest number of BCTs (n=31),53,56,57 whereas another study only included four BCTs.38 Inter-rated reliability for coding BCTs was high with an average ICC of .954 with a 95% confidence interval between .902 and .977 (F(37,37)= 25.03, p<.001). Tables 2–3 provide an overview, by study design group, of each study and identified BCTs.
Table 2.
Behavior Change Techniques (BCTs) Identified in RCT Designs
| Behavior Change Technique Taxonomy Code | Bombardier et al., 2013; Kratz et al., 2014 | Canning & Hicks, 2020 | Carter et al., 2013 | Carter et al., 2014; Saxton et al., 2013 | Dlugonski et al., 2012 | Donkers et al., 2020 | Geddes et al., 2009 | Geertz et al., 2015 | Hayes et al., 2017; Coote et al., 2017; Coote et al., 2014 | Learmonth et al., 2011 | Learmonth et al., 2017; Adamson et al., 2016 | Lithopoulos et al., 2017 | McAuley et al., 2007 | McAuley et al., 2015; Wojcicki et al., 2014 | McCullagh et al., 2008 | Motl et al., 2011 | Motl et al., 2017 | Pilutti et al., 2014; Motl et al., 2015; Klaren et al., 2014; Pilutti et al., 2014; Sandroff et al., 2014 | Plow et al., 2014; Plow et al., 2014 | Plow et al., 2019; Plow et al., 2019; Plow et al., 2012 | Rice et al., 2015 | Romberg et al., 2004 | Ryan et al., 2019; Ryan et al., 2017 | Sandroff et al., 2016 | Sebastião et al., 2018; Sebastião et al., 2017 | Smith et al., 2012 | Suh et al., 2015 | Tallner et al., 2016 | Thomas et al., 2017; Thomas et al., 2014 | Turner et al., 2016 | Total # of BCTs |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.1 Goal setting (behavior) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 24 | ||||||
| 1.2 Problem solving | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 19 | |||||||||||
| 1.3 Goal setting (outcome) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 17 | |||||||||||||
| 1.4 Action planning | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 14 | ||||||||||||||||
| 1.5 Review behavior goal(s) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 16 | ||||||||||||||
| 1.6 Discrepancy between current behavior and goal | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 1.7 Review outcome goal(s) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | |||||||||||||||||||||||
| 1.8 Behavioral contract | ✓ | ✓ | 2 | ||||||||||||||||||||||||||||
| 1.9 Commitment | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 2.1 Monitoring of behavior by others without feedback | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13 | |||||||||||||||||
| 2.2 Feedback on behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13 | |||||||||||||||||
| 2.3 Self-monitoring of behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 23 | |||||||
| 2.4 Self-monitoring of outcome(s) of behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | ||||||||||||||||||||||||
| 2.5 Monitoring of outcome(s) of behavior without feedback | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | ||||||||||||||||||||||||
| 2.6 Biofeedback | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 3.1 Social support (unspecified) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 26 | ||||
| 3.2 Social support (practical) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | ||||||||||||||||||||
| 3.3 Social support (emotional) | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 4.1 Instruction on how to perform the behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 27 | |||
| 4.2 Information about antecedents | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 4.4 Behavioral experiments | ✓ | 1 | |||||||||||||||||||||||||||||
| 5.1 Information about health consequences | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | |||||||||||||||||||
| 5.2 Salience of consequences | ✓ | ✓ | 2 | ||||||||||||||||||||||||||||
| 5.3 Information about social and environmental consequences | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13 | |||||||||||||||||
| 5.4 Monitoring of emotional consequences | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 5.6 Information about emotional consequences | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 6.1 Demonstration of the behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 26 | ||||
| 6.2 Social comparison | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | ||||||||||||||||||||||
| 6.3 Information about others’ approval | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 7.1 Prompts/cues | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | |||||||||||||||||||||||
| 8.1 Behavioral practice/rehearsal | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 15 | |||||||||||||||
| 8.2 Behavioral substitution | ✓ | 1 | |||||||||||||||||||||||||||||
| 8.3 Habit formation | ✓ | 1 | |||||||||||||||||||||||||||||
| 8.6 Generalisation of target behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | |||||||||||||||||||
| 8.7 Graded tasks | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 23 | |||||||
| 9.1 Credible source | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 25 | |||||
| 9.2 Pros and cons | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 9.3 Comparative imagining of future outcomes | ✓ | 1 | |||||||||||||||||||||||||||||
| 10.1 Material incentive (behavior) | ✓ | ✓ | 2 | ||||||||||||||||||||||||||||
| 10.3 Non-specific reward | ✓ | ✓ | 2 | ||||||||||||||||||||||||||||
| 10.4 Social reward | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 10.7 Self-incentive | ✓ | 1 | |||||||||||||||||||||||||||||
| 10.9 Self-reward | ✓ | 1 | |||||||||||||||||||||||||||||
| 10.10 Reward (outcome) | ✓ | 1 | |||||||||||||||||||||||||||||
| 11.2 Reduce negative emotions | ✓ | ✓ | ✓ | 3 | |||||||||||||||||||||||||||
| 12.1 Restructuring the physical environment | ✓ | 1 | |||||||||||||||||||||||||||||
| 12.2 Restructuring the social environment | ✓ | 1 | |||||||||||||||||||||||||||||
| 12.5 Adding objects to the environment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 18 | ||||||||||||
| 13.2 Framing/reframing | ✓ | 1 | |||||||||||||||||||||||||||||
| 14.5 Rewarding completion | ✓ | ✓ | ✓ | ✓ | 4 | ||||||||||||||||||||||||||
| 15.1 Verbal persuasion about capability | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | |||||||||||||||||||
| 15.3 Focus on past success | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||||||||||||||||||||||||
| 16.3 Vicarious consequences | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||||||||||||||||||||||||
| Total # of BCTs | 20 | 8 | 13 | 23 | 21 | 13 | 9 | 4 | 22 | 9 | 22 | 6 | 14 | 14 | 12 | 23 | 19 | 20 | 18 | 31 | 12 | 11 | 17 | 8 | 15 | 10 | 12 | 10 | 25 | 18 | 459 |
Table 3.
Behavior Change Techniques (BCTs) Identified in Pre-Post Designs
| Behavior Change Technique Taxonomy Code | Dixon-Ibarra et al., 2017 | Dlugonski et al., 2011 | Feys et al., 2013 | Hale et al., 2013 | Kinnett-Hopkins & Motl, 2018 | Mandelbaum et al., 2015 | Motl & Dlugonski, 2011 | Plow & Finlayson, 2011 | Total # of BCTs |
|---|---|---|---|---|---|---|---|---|---|
| 1.1 Goal setting (behavior) | ✓ | ✓ | ✓ | ✓ | 4 | ||||
| 1.2 Problem solving | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | ||
| 1.3 Goal setting (outcome) | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||
| 1.5 Review behavior goal(s) | ✓ | ✓ | 2 | ||||||
| 1.7 Review outcome goal(s) | ✓ | ✓ | 2 | ||||||
| 1.9 Commitment | ✓ | 1 | |||||||
| 2.2 Feedback on behavior | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||
| 2.3 Self-monitoring of behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | ||
| 3.1 Social support (unspecified) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | ||
| 3.2 Social support (practical) | ✓ | ✓ | 2 | ||||||
| 3.3 Social support (emotional) | ✓ | 1 | |||||||
| 4.1 Instruction on how to perform the behavior | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | |
| 5.1 Information about health consequences | ✓ | ✓ | ✓ | ✓ | 4 | ||||
| 5.3 Information about social and environmental consequences | ✓ | ✓ | ✓ | ✓ | 4 | ||||
| 6.1 Demonstration of the behavior | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||
| 6.2 Social comparison | ✓ | ✓ | ✓ | 3 | |||||
| 6.3 Information about others′ approval | ✓ | ✓ | 2 | ||||||
| 7.1 Prompts/cues | ✓ | 1 | |||||||
| 8.1 Behavioral practice/rehearsal | ✓ | ✓ | 2 | ||||||
| 8.6 Generalisation of target behavior | ✓ | 1 | |||||||
| 8.7 Graded tasks | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | |||
| 9.1 Credible source | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | |
| 9.2 Pros and cons | ✓ | 1 | |||||||
| 10.3 Non-specific reward | ✓ | ✓ | 2 | ||||||
| 12.5 Adding objects to the environment | ✓ | ✓ | ✓ | ✓ | 4 | ||||
| 14.5 Rewarding completion | ✓ | 1 | |||||||
| 15.1 Verbal persuasion about capability | ✓ | 1 | |||||||
| 16.3 Vicarious consequences | ✓ | ✓ | ✓ | 3 | |||||
| Total # of BCTs | 10 | 11 | 9 | 8 | 15 | 12 | 16 | 12 | 93 |
Results were generally consistent across study designs with overall frequencies of individual BCTs reported in Table 4. Among completed RCTs, the five most common BCTs were (a) 4.1 instructions on how to perform the behavior, (b) 3.1 social support (unspecified), (c) 6.1 demonstration of the behavior, (d) 9.1 credible source, and (e) 1.1 goal setting (behavior). By comparison, among pre-post study designs, 2.3 self-monitoring of behavior was more common than 1.1 goal setting (behavior), consistent with the overall totals across studies. Several BCTs were used in only one study including: 4.4 behavioral experiments, 8.2 behavior substitution, 8.3 habit formation, 9.3 comparative imagining of future outcomes, 10.7 self-incentive, 10.9 self-reward, 10.10 reward (outcome), 12.1 restructuring the physical environment, 12.2 restructuring the social environment, and 13.2 framing/reframing.
Table 4.
Frequency of behavior change techniques (BCTs)
| Behavior change technique code | Total number of studies N=38 n (%) | Study Design | |
|---|---|---|---|
| RCT N=30 n (%) | Pre-Post N=8 n (%) | ||
| 4.1 Instruction on how to perform the behavior | 34 (89) | 27 (90) | 7 (88) |
| 3.1 Social support (unspecified) | 32 (84) | 26 (87) | 6 (75) |
| 9.1 Credible source | 32 (84) | 25 (83) | 7 (88) |
| 6.1 Demonstration of the behavior | 31 (82) | 26 (87) | 5 (63) |
| 2.3 Self-monitoring of behavior | 29 (76) | 23 (77) | 6 (75) |
| 8.7 Graded tasks | 28 (74) | 23 (77) | 5 (63) |
| 1.1 Goal setting (behavior) | 28 (74) | 24 (80) | 4 (50) |
| 1.2 Problem solving | 25 (66) | 19 (63) | 6 (75) |
| 1.3 Goal setting (outcome) | 22 (58) | 17 (57) | 5 (63) |
| 12.5 Adding objects to the environment | 22 (58) | 18 (60) | 4 (50) |
| 2.2 Feedback on behavior | 18 (47) | 13 (43) | 5 (63) |
| 1.5 Review behavior goal(s) | 18 (47) | 16 (53) | 2 (25) |
| 5.3 Information about social and environmental consequences | 17 (45) | 13 (43) | 4 (50) |
| 8.1 Behavioral practice/rehearsal | 17 (45) | 15 (50) | 2 (25) |
| 5.1 Information about health consequences | 15 (39) | 11 (37) | 4 (50) |
| 1.4 Action planning | 14 (37) | 14 (47) | 0 (0) |
| 2.1 Monitoring of behavior by others without feedback | 13 (34) | 13 (43) | 0 (0) |
| 3.2 Social support (practical) | 12 (32) | 10 (33) | 2 (25) |
| 15.1 Verbal persuasion about capability | 12 (32) | 11 (37) | 1 (13) |
| 8.6 Generalization of target behavior | 12 (32) | 11 (37) | 1 (13) |
| 6.2 Social comparison | 11 (29) | 8 (27) | 3 (38) |
| 1.7 Review outcome goal(s) | 9 (24) | 7 (23) | 2 (25) |
| 7.1 Prompts/cues | 8 (21) | 7 (23) | 1 (13) |
| 16.3 Vicarious consequences | 8 (21) | 5 (17) | 3 (38) |
| 2.4 Self-monitoring of outcome(s) of behavior | 6 (16) | 6 (20) | 0 (0) |
| 2.5 Monitoring of outcome(s) of behavior without feedback | 6 (16) | 6 (20) | 0 (0) |
| 6.3 Information about others’ approval | 5 (13) | 3 (10) | 2 (25) |
| 14.5 Rewarding completion | 5 (13) | 4 (13) | 1 (13) |
| 15.3 Focus on past success | 5 (13) | 5 (17) | 0 (0) |
| 1.9 Commitment | 5 (13) | 4 (13) | 1 (13) |
| 4.2 Information about antecedents | 4 (11) | 4 (13) | 0 (0) |
| 9.2 Pros and cons | 4 (11) | 3 (10) | 1 (13) |
| 10.3 Non-specific reward | 4 (11) | 2 (7) | 2 (25) |
| 2.6 Biofeedback | 4 (11) | 4 (13) | 0 (0) |
| 3.3 Social support (emotional) | 4 (11) | 3 (10) | 1 (13) |
| 5.4 Monitoring of emotional consequences | 4 (11) | 4 (13) | 0 (0) |
| 5.6 Information about emotional consequences | 4 (11) | 4 (13) | 0 (0) |
| 1.6 Discrepancy between current behavior and goal | 3 (8) | 3 (10) | 0 (0) |
| 10.4 Social reward | 3 (8) | 3 (10) | 0 (0) |
| 11.2 Reduce negative emotions | 3 (8) | 3 (10) | 0 (0) |
| 1.8 Behavioral contract | 2 (5) | 2 (7) | 0 (0) |
| 10.1 Material incentive (behavior) | 2 (5) | 2 (7) | 0 (0) |
| 5.2 Salience of consequences | 2 (5) | 2 (7) | 0 (0) |
| 10.10 Reward (outcome) | 1 (3) | 1 (3) | 0 (0) |
| 10.7 Self-incentive | 1 (3) | 1 (3) | 0 (0) |
| 10.9 Self-reward | 1 (3) | 1 (3) | 0 (0) |
| 12.1 Restructuring the physical environment | 1 (3) | 1 (3) | 0 (0) |
| 12.2 Restructuring the social environment | 1 (3) | 1 (3) | 0 (0) |
| 13.2 Framing/reframing | 1 (3) | 1 (3) | 0 (0) |
| 4.4 Behavioral experiments | 1 (3) | 1 (3) | 0 (0) |
| 8.2 Behavioral substitution | 1 (3) | 1 (3) | 0 (0) |
| 8.3 Habit formation | 1 (3) | 1 (3) | 0 (0) |
| 9.3 Comparative imagining of future outcomes | 1 (3) | 1 (3) | 0 (0) |
Table 1 includes effect size and significance values for change in physical activity as appropriate for all included studies. Overall, effect sizes ranged between 0.04 and 1.49. Among RCTs, the range of effect size compared to a control group for objective physical activity outcomes was 0.04 and 1.15 with small effects reported in 7 studies, medium effects in 3 studies, and large effects in 1 study. Regarding objective physical activity outcomes in RCTs, 1 study included multiple measures, 10 did not include a measure, and 8 did not report values for calculating effect size. Among RCTs, the range of effect size compared to control group for self-reported physical activity outcomes was −0.05 and 0.87 with small effects reported in 5 studies, medium effects in 10 studies, and large effects in 3 studies. Regarding self-reported physical activity outcomes in RCTs, 4 studies included multiple measures, 10 did not include a measure, and 1 did not report values for calculating effect size. Among pre-post studies, the range of effect size for objective physical activity outcomes was 0.68 and 1.04 with medium effects reported in one study, and large effects in 2 studies. Regarding objective physical activity outcomes in pre-post studies, 1 study included multiple measures, 4 did not include a measure, and 2 did not report values for calculating effect size. Among pre-post studies, the range of effect size for self-reported physical activity outcomes was 0.17 and 1.49 with small effects reported in 2 studies, medium effects in 1 study, and large effects in 3 studies. Regarding self-reported physical activity outcomes in pre-post studies, 2 studies included multiple measures, 1 did not include a measure, and 1 did not report values for calculating effect size. Five studies did not provide any information that met our criteria for reporting effect size. Among those studies outcomes included Adherence only (n=5), self-report outcome only (n=1), Adherence and one self-report outcome (n=1) and Adherence and one objective outcome (n=1). Among RCTs and pre-post studies, significant positive change in a least one physical activity outcome was identified in 22 studies (58%) no change or lower physical activity in 8 studies (21%), and no significance values were reported in 8 studies (21%). The mean number of BCTs used in the studies with significant positive change was 16 BCTs, no change or lower physical activity was 14 BCTs, and no values reported was 11 BCTs. Most studies that reported no change or lower physical activity used only 1 measure (n=6; 75%). Additionally, among studies not reporting significance values the majority used only 1 measure (n= 7; 88%). Chi-Square analyses indicated significant differences, X2 (1, N = 38) = 6.18, p = .01, in physical activity changes among studies that reported 15 or more BCTs (n=16) and 14 or fewer BCTs (n=22).
Discussion
This study identified 38 unique behavior change interventions and reviewed the use of BCTs for promoting physical activity among persons with MS. The 38 unique behavior change interventions included 53 of the 93 possible BCTs in the consensus BCT Taxonomy. This provides evidence of broad inclusion of BCTs in behavior change interventions for physical activity in MS and indicates that the BCT Taxonomy can be applied for identifying the active ingredients in behavior change interventions for persons with MS. The mean number of BCTs identified per study was 15 with a comprehensive overview provided regarding the most and least frequently reported BCTs across RCTs and pre-post designs. All but three completed studies that used 15 or more BCTs reported a significant increase in a physical activity outcome (i.e., 81%), whereas 60% of those that included 14 or fewer BCTs did not report significant change in physical activity.
The most commonly used BCTs were 4.1 instructions on how to perform the behavior, 3.1 social support (unspecified), 6.1 demonstration of the behavior, 9.1 credible source, 2.3 self-monitoring of behavior, and 8.7 graded tasks. These BCTs are directly linked with mechanisms of action such as knowledge, skills, social influences, beliefs about capability, social learning, attitude towards behavior, and behavioral regulation.82 One recent review of BCTs in leisure-time physical activity interventions for persons with spinal cord injuries identified the most common BCTs, and four were consistent with the current study (i.e., 4.1 instructions on how to perform the behavior, 1.1 goal setting (behavior), 9.1 credible source, 1.2 problem solving) whereas two BCTs (i.e., 3.2 social support (practical) and 1.4 action planning) were not consistent with the current study.23 The authors highlight some modified coding that is not described in the BCT Taxonomy training, specifically coding for unique types of social support that may have yielded such discrepancies. The authors described the coding of social support accordingly: the code 3.2 social support (practical) was applied anytime counseling was mentioned without further detail, 3.3. social support (emotional) was applied any form of emotional or companionship support, and 3.1. social support (unspecified) was applied as a form of validation. BCTs have further been examined in relation to the intervention environment (i.e., eHealth). For example, one systematic review of physical activity eHealth interventions for persons with cardiovascular disease identified most frequently used BCTs as 5.1 information about health consequences, 1.1 goal setting (behavior), 2.3 self-monitoring of behavior and 3.2 social support (practical). The only BCT consistent with the top 10 BCTs identified in the current study was 1.1 goal setting (behavior). Additional examination of BCTs for promoting physical activity in unique populations and distinct environments may provide further guidance for the creation of best practices for promoting physical activity behavior change.
The creation of the BCT Taxonomy is highlighted as a boon for research on health behavior change, as the taxonomy provides a common language for describing interventions and thus clarity regarding the active ingredients underlying intervention effectiveness and further replication.83 The focus on BCTs aligns with the experimental medicine approach for moving beyond standard efficacy trials that examine the direct path between intervention and outcomes, and conducting focal examinations of separate mechanistic paths among putative targets, interventions, and behavioral outcomes (i.e., identification, validation, and engagement).83 Distinctively, the classification of BCTs associated with health behavior change guides future intervention development and refinement by pinpointing the specific targets and procedures that may result in positive outcomes. We further identified protocol papers for five physical activity clinical trials that are currently being conducted with forthcoming results.84–88 Such protocol papers provide a synthesis of currently implemented BCTs based on previous research. Sample sizes among these studies ranges from 80 to 420 and designs include traditional RCTs and pragmatic clinical trials. Researchers currently conducting and designing future clinical trials are encouraged to use this report and protocols for ongoing clinical trials to guide BCT selection and rigorous reporting that can help move forward a compendium and research approaches aligned with the experimental medicine approach.
This study provides critical information regarding BCTs used in physical activity behavior change interventions for persons with MS and initial evidence that inclusion of various BCTs may be related to positive physical activity behavior change. The next step in this line of research is to apply a more comprehensive approach designed to rigorously control and assess the contribution of discrete BCTs. Such approaches may include factorial or fractional factorial experiences such as multiphase optimization strategy (MOST)89 and sequential multiple assignment randomized trial (SMART) designs90 wherein BCTs are directly tested as causal links between health behavior theories and behavior change.
Study limitations
To our knowledge, this is the first focal study that identified and summarized BCTs included in behavior change interventions for physical activity in persons with MS. There are several notable limitations of this study, specifically regarding the coding of BCTs. All researchers involved in coding and refereeing in this study completed the BCT Taxonomy online training; however, there is still a subjective component involved in the research design given lack of direct reporting of BCTs in the majority of studies. Indeed, validation studies report only modest reliability when coding approximately 20% of the 93 BCTs.91 We overcame such a limitation through extensive training of the coders and vetting of the BCT codes per study. Another limitation is the wide variety of research designs and outcomes that preclude directly assessing the magnitude and effectiveness of BCTs for the promotion of physical activity in MS. We conducted post-hoc exploratory analyses exploring the relationship between positive changes in physical activity and the presence of 15 or more BCTS, demonstrating a positive association. However, this association may be attributable to a third variable such as studies with more BCTs having better funding and/or being more adequately powered with an appropriate sample size. Criteria for inclusion in this review were deliberately broad to provide an expansive overview of physical activity behavior change interventions and outcomes, however we acknowledge that studies focused on adherence as a primary behavioral outcome should be interpreted with caution. Specifically, measurement of adherence to an intervention reflects an alternative study design when compared to traditional device- and self-report measures of physical activity wherein there are two or more measures that can be compared within-subjects as opposed to one overarching measure that is compared between-subjects. We did not report the selection of BCTs based on theory or the specific connection between theory and intervention strategies, as this was not explicitly reported by study authors. Accordingly, the research team provided a broad description of BCTs as a guide for future intervention development and reporting. We further highlight a model for future research that aligns with recent calls to rigorously utilize behavior change theories in the promotion of physical activity in MS.92 For example, Social Cognitive Theory is a widely examined and applied theory of health behavior change guiding previous and current physical activity interventions for persons with MS.14 Social Cognitive Theory intervention components such as self-monitoring, modeling, instruction, and social support directly align with the BCT Taxonomy and most frequent BCTs identified in this review. However, the ongoing primary limitation that exists is the reporting of theory and BCTs alignment. One study in the review included a table that is a great example directly identifying BCTs, definitions, and examples for the intervention.54 The increasing frequency of publishing protocol papers focused on intervention fidelity may provide a promising avenue for addressing these limitations, however subsequent reporting of results is critical to identify whether planned BCTs aligned with intervention delivery and overall fidelity. Such reporting aligns with a need for future research guided by the experimental medicine approach that (a) is founded on behavior change theory (b) provides of clear information regarding intervention behavior change strategies and (c) application of intervention designs that experimentally examine the contribution of individual BCTs.83
Conclusions
This systematic review provides a comprehensive description of the use of BCTs in behavior change interventions for physical activity in MS. The mean number of BCTs used across behavior change interventions was 15, yet many studies did not report on the theoretical basis for selecting BCTs nor how BCTs align with theory-based intervention components. The lack of clear reporting precludes the ability to identify active ingredients associated with increased physical activity among persons with MS. Future research is needed regarding the precision and effectiveness of discrete BCTs for changing physical activity behavior among persons with MS, as this has the potential to improve overall health and quality of life in this chronic, lifelong disease of the CNS.
Funding:
This work was supported, in part, by the National Multiple Sclerosis Society (MB 0029) and by the Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health [F32HD101214]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
List of abbreviations:
- BCTs
Behavior Change Techniques
- CNS
Central Nervous System
- MMAT
Mixed Methods Appraisal Tool
- MOST
Multiphase Optimization Strategy
- MS
Multiple Sclerosis
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCTs
Randomized Controlled Trials
- RoB 2
Risk of Bias 2
- SMART
Sequential Multiple Assignment Randomized Trial
- US
United States
Appendix 1.
Database Search Details
| Database | Terms | Filters | Results | Duplicates |
|---|---|---|---|---|
| Pubmed | ((((((((((((((((exercise) OR fitness) OR walking) OR exercise promotion) OR leisure activity) OR physical education) OR exercise training) OR exercise therapy) OR motor activity) OR physical training) OR actigraphy) OR actigraph) OR physical activity)) AND ((((((((behavior change) OR program evaluation) OR programme) OR program) OR intervention studies) OR treatment outcome) OR behavioral intervention) OR Intervention))) AND multiple sclerosis | Humans, Adults, & English | 2254 | |
| PsycINFO | (((((physical activity) OR (exercise) OR actigraphy OR (exercise promotion) OR (physical training) OR (exercise therapy) OR (motor activity) OR (fitness) OR (exercise training) OR (physical education) OR (leisure activity) OR (walking) OR (actigraph)) AND la.exact(“English”)) AND la.exact(“English”)) AND la.exact(“English”)) AND ((((intervention OR (behavioral intervention) OR interventions OR (treatment outcome) OR (intervention studies) OR program OR programmes OR (program evaluation) OR (behavior change) OR programmed) AND la.exact(“English”)) AND la.exact(“English”)) AND la.exact(“English”)) AND ((multiple sclerosis) AND la.exact(“English”)) AND PEER(yes) | English, Scholarly Journals, Full text, & Peer reviewed | 3256 | 92 |
| Scopus | (ALL (multiple AND sclerosis) AND ALL (actigraph OR actigraphy OR physical AND training OR exercise AND therapy OR motor AND activity OR physical AND fitness OR exercise AND training OR physical AND education OR leisure AND activity OR exercise AND promotion OR walking OR fitness OR physical AND activities OR physic) AND ALL (intervention OR behavioral AND intervention OR interventions OR treatment AND outcome OR intervention AND studies OR program OR programs OR programme OR programmes OR programmed OR program AND evaluation OR behavior AND change)) | Humans, English, Article & Review | 1817 | 236 |
| CINAHL | ((((((((((((((((exercise) OR fitness) OR walking) OR exercise promotion) OR leisure activity) OR physical education) OR exercise training) OR exercise therapy) OR motor activity) OR physical training) OR actigraphy) OR actigraph) OR physical activity)) AND ((((((((behavior change) OR program evaluation) OR programme) OR program) OR intervention studies) OR treatment outcome) OR behavioral intervention) OR Intervention))) AND multiple sclerosis | Humans, English, & Academic Journals | 915 | 503 |
| Embase | ((((((((((((((((exercise) OR fitness) OR walking) OR exercise promotion) OR leisure activity) OR physical education) OR exercise training) OR exercise therapy) OR motor activity) OR physical training) OR actigraphy) OR actigraph) OR physical activity)) AND ((((((((behavior change) OR program evaluation) OR programme) OR program) OR intervention studies) OR treatment outcome) OR behavioral intervention) OR Intervention))) AND multiple sclerosis | Humans & English | 471 | 234 |
Appendix 2.
The Behavior Change Technique Taxonomy (v1)
|
Appendix 3
|

|
Note. D1: Randomization Process; D2: Deviations from the Intended Interventions; D3: Missing Outcome Data; D4: Measurement of the Outcome; D5: Selection of the Reported Result
Appendix 4
|
Note. D1: Are the participants representative of the target population?, D2: Are measurements appropriate regarding both the outcome and intervention (or exposure)?; D3: Are there complete outcome data?; D4: Are the confounders accounted for in the design and analysis?; D5: During the study period, is the intervention administered (or exposure occurred) as intended?

Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors report no conflict of interest.
PROSPERO Registration: CRD42020191858
References
- 1.National Multiple Sclerosis Society. MS the Disease. Available at: https://www.nationalmssociety.org/About-the-Society/Press-Room/MS-the-Disease#:~:text=Following%20an%20initial%20period%20of,10%20years%20of%20initial%20diagnosis.[12August2020].
- 2.MS International Federation. Epidemiology: Number of people with MS. Available at: https://www.atlasofms.org/map/global/epidemiology/number-of-people-with-ms. [06 December 2020].
- 3.Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7(12):1139–1151. [DOI] [PubMed] [Google Scholar]
- 4.Krupp LB, Alvarez LA, LaRocca NG, Scheinberg LC. Fatigue in Multiple Sclerosis. Arch Neurol. 1988;45(4):435–437. [DOI] [PubMed] [Google Scholar]
- 5.Osterberg A, Boivie J, Thuomas KA. Central pain in multiple sclerosis--prevalence and clinical characteristics. Eur J Pain. 2005;9(5):531–542. [DOI] [PubMed] [Google Scholar]
- 6.Siegert R, Abernethy D. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry. 2005;76(4):469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sutliff MH. Contribution of impaired mobility to patient burden in multiple sclerosis. Curr Med Res Opin. 2010;26(1):109–119. [DOI] [PubMed] [Google Scholar]
- 8.Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8(9):487. [DOI] [PubMed] [Google Scholar]
- 9.Smith CM, Hale LA, Olson K, Baxter GD, Schneiders AG. Healthcare provider beliefs about exercise and fatigue in people with multiple sclerosis. J Rehabil Res Dev. 2013;50(5): 733–744. [DOI] [PubMed] [Google Scholar]
- 10.Klaren RE, Motl RW, Dlugonski D, Sandroff BM, Pilutti LA. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehabil. 2013;94(12):2342–2348. [DOI] [PubMed] [Google Scholar]
- 11.Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. 2009;31(20):1652–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler. 2005;11(4):459–463. [DOI] [PubMed] [Google Scholar]
- 13.Sangelaji B, Smith CM, Paul L, Sampath KK, Treharne GJ, Hale LA. The effectiveness of behaviour change interventions to increase physical activity participation in people with multiple sclerosis: a systematic review and meta-analysis. Clin Rehabil. 2016;30(6):559–576. [DOI] [PubMed] [Google Scholar]
- 14.Coulter EH, Bond S, Dalgas U, Paul L. The effectiveness of interventions targeting physical activity and/or sedentary behaviour in people with Multiple Sclerosis: a systematic review. Disabil Rehabil. 2020;42(5):594–612. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y, Mehta T, Lai B, Motl RW. Immediate and Sustained Effects of Interventions for Changing Physical Activity in People with Multiple Sclerosis: Meta-Analysis of Randomized Controlled Trials. Arch Phys Med Rehabil. 2020;101(8):1414–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Casey B, Coote S, Hayes S, Gallagher S. Changing Physical Activity Behavior in People With Multiple Sclerosis: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2018;99(10):2059–2075. [DOI] [PubMed] [Google Scholar]
- 17.Borrelli B The Assessment, Monitoring, and Enhancement of Treatment Fidelity In Public Health Clinical Trials. J Public Health Dent. 2011;71(s1):S52–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly MP, Stewart E, Morgan A, et al. A conceptual framework for public health: NICE’s emerging approach. Public Health. 2009;123(1):e14–20. [DOI] [PubMed] [Google Scholar]
- 19.Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–1498. [DOI] [PubMed] [Google Scholar]
- 20.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 21.Duff OM, Walsh DM, Furlong BA, O’Connor NE, Moran KA, Woods CB. Behavior Change Techniques in Physical Activity eHealth Interventions for People With Cardiovascular Disease: Systematic Review. J Med Internet Res. 2017;19(8):e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heron N, Kee F, Donnelly M, Cardwell C, Tully MA, Cupples ME. Behaviour change techniques in home-based cardiac rehabilitation: a systematic review. Br J Gen Pract. 2016;66(651):e747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tomasone JR, Flood SM, Ma JK, et al. Physical activity self-management interventions for adults with spinal cord injury: Part 1–A systematic review of the use and effectiveness of behavior change techniques. Psychol Sport Exerc. 2018;37:274–285. [Google Scholar]
- 24.Black N, Williams AJ, Javornik N, et al. Enhancing Behavior Change Technique Coding Methods: Identifying Behavioral Targets and Delivery Styles in Smoking Cessation Trials. Ann Behav Med. 2018;53(6):583–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22(1):128. [DOI] [PubMed] [Google Scholar]
- 26.Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:I4898. [DOI] [PubMed] [Google Scholar]
- 27.Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I. Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada. [Google Scholar]
- 28.Adamson BC, Learmonth YC, Kinnett-Hopkins D, Bohri M, Motl RW. Feasibility study design and methods for Project GEMS: Guidelines for Exercise in Multiple Sclerosis. Contemp Clin Trials. 2016;47:32–39. [DOI] [PubMed] [Google Scholar]
- 29.Bombardier CH, Ehde DM, Gibbons LE, et al. Telephone-based physical activity counseling for major depression in people with multiple sclerosis. J Consult Clin Psychol. 2013;81(1):89–99. [DOI] [PubMed] [Google Scholar]
- 30.Canning KL, Hicks AL. Physician referral improves adherence to the physical activity guidelines for adults with MS: A randomized controlled trial. Mult Scler Relat Disord. 2020;37:101441. [DOI] [PubMed] [Google Scholar]
- 31.Carter A, Daley A, Humphreys L, et al. Pragmatic intervention for increasing self-directed exercise behaviour and improving important health outcomes in people with multiple sclerosis: a randomised controlled trial. Mult Scler. 2014;20(8):1112–1122. [DOI] [PubMed] [Google Scholar]
- 32.Carter AM, Daley AJ, Kesterton SW, Woodroofe NM, Saxton JM, Sharrack B. Pragmatic exercise intervention in people with mild to moderate multiple sclerosis: a randomised controlled feasibility study. Contemp Clin Trials. 2013;35(2):40–47. [DOI] [PubMed] [Google Scholar]
- 33.Coote S, Gallagher S, Msetfi R, et al. A randomised controlled trial of an exercise plus behaviour change intervention in people with multiple sclerosis: the step it up study protocol. BMC Neurol. 2014;14:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coote S, Uszynski M, Herring MP, et al. Effect of exercising at minimum recommendations of the multiple sclerosis exercise guideline combined with structured education or attention control education - secondary results of the step it up randomised controlled trial. BMC Neurol. 2017;17(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dlugonski D, Motl RW, Mohr DC, Sandroff BM. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol Health Med. 2012;17(6):636–651. [DOI] [PubMed] [Google Scholar]
- 36.Donkers SJ, Nickel D, Paul L, Wiegers SR, Knox KB. Adherence to physiotherapy-guided web-based exercise for persons living with moderate-to-severe multiple sclerosis: a randomized-controlled pilot study. Int J MS Care. 2020. 10.7224/15372073.2019-048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geddes EL, Costello E, Raivel K, Wilson R. The effects of a twelve-week home walking program on cardiovascular parameters and fatigue perception of individuals with multiple sclerosis: a pilot study. Cardiopulm Phys Ther J. 2009;20(1):5–12. [PMC free article] [PubMed] [Google Scholar]
- 38.Geertz W, Dechow AS, Patra S, Heesen C, Gold SM, Schulz KH. Changes of Motivational Variables in Patients with Multiple Sclerosis in an Exercise Intervention: Associations between Physical Performance and Motivational Determinants. Behav Neurol. 2015;2015:248193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hayes S, Uszynski MK, Motl RW, et al. Randomised controlled pilot trial of an exercise plus behaviour change intervention in people with multiple sclerosis: the Step it Up study. BMJ Open. 2017;7(10):e016336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klaren RE, Hubbard EA, Motl RW. Efficacy of a behavioral intervention for reducing sedentary behavior in persons with multiple sclerosis: a pilot examination. Am J Prev Med. 2014;47(5):613–616. [DOI] [PubMed] [Google Scholar]
- 41.Kratz AL, Ehde DM, Bombardier CH. Affective mediators of a physical activity intervention for depression in multiple sclerosis. Rehabil Psychol. 2014;59(1):57–67. [DOI] [PubMed] [Google Scholar]
- 42.Learmonth YC, Adamson BC, Kinnett-Hopkins D, Bohri M, Motl RW. Results of a feasibility randomised controlled study of the guidelines for exercise in multiple sclerosis project. Contemp Clin Trials. 2017;54:84–97. [DOI] [PubMed] [Google Scholar]
- 43.Learmonth YC, Paul L, Miller L, Mattison P, McFadyen AK. The effects of a 12-week leisure centre-based, group exercise intervention for people moderately affected with multiple sclerosis: a randomized controlled pilot study. Clin Rehabil. 2012;26(7):579593. [DOI] [PubMed] [Google Scholar]
- 44.Lithopoulos A, Bassett-Gunter RL, Martin Ginis KA, Latimer-Cheung AE. The Effects of Gain-versus Loss-Framed Messages Following Health Risk Information on Physical Activity in Individuals With Multiple Sclerosis. J Health Commun. 2017;22(6):523–531. [DOI] [PubMed] [Google Scholar]
- 45.McAuley E, Motl RW, Morris KS, et al. Enhancing physical activity adherence and well-being in multiple sclerosis: a randomised controlled trial. Mult Scler. 2007;13(5):652659. [DOI] [PubMed] [Google Scholar]
- 46.McAuley E, Wójcicki TR, Learmonth YC, et al. Effects of a DVD-delivered exercise intervention on physical function in older adults with multiple sclerosis: A pilot randomized controlled trial. Mult Scler J Exp Transl Clin. 2015;1:2055217315584838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCullagh R, Fitzgerald AP, Murphy RP, Cooke G. Long-term benefits of exercising on quality of life and fatigue in multiple sclerosis patients with mild disability: a pilot study. Clin Rehabil. 2008;22(3):206–214. [DOI] [PubMed] [Google Scholar]
- 48.Motl RW, Dlugonski D, Pilutti LA, Klaren RE. Does the effect of a physical activity behavioral intervention vary by characteristics of people with multiple sclerosis? Int J MS Care. 2015;17(2):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Motl RW, Dlugonski D, Wojcicki TR, McAuley E, Mohr DC. Internet intervention for increasing physical activity in persons with multiple sclerosis. Mult Scler. 2011;17(1):116–128. [DOI] [PubMed] [Google Scholar]
- 50.Motl RW, Hubbard EA, Bollaert RE, et al. Randomized controlled trial of an e-learning designed behavioral intervention for increasing physical activity behavior in multiple sclerosis. Mult Scler J Exp Transl Clin. 2017;3(4):2055217317734886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pilutti LA, Dlugonski D, Sandroff BM, Klaren R, Motl RW. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult Scler. 2014;20(5):594–601. [DOI] [PubMed] [Google Scholar]
- 52.Pilutti LA, Dlugonski D, Sandroff BM, Klaren RE, Motl RW. Internet-delivered lifestyle physical activity intervention improves body composition in multiple sclerosis: preliminary evidence from a randomized controlled trial. Arch Phys Med Rehabil. 2014;95(7):1283–1288. [DOI] [PubMed] [Google Scholar]
- 53.Plow M, Bethoux F, Mai K, Marcus B. A formative evaluation of customized pamphlets to promote physical activity and symptom self-management in women with multiple sclerosis. Health Educ Res. 2014;29(5):883–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Plow M, Finlayson M, Motl RW, Bethoux F. Randomized controlled trial of a teleconference fatigue management plus physical activity intervention in adults with multiple sclerosis: rationale and research protocol. BMC Neurol. 2012;12(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Plow M, Bethoux F, McDaniel C, McGlynn M, Marcus B. Randomized controlled pilot study of customized pamphlets to promote physical activity and symptom self-management in women with multiple sclerosis. Clin Rehabil. 2014;28(2):139–148. [DOI] [PubMed] [Google Scholar]
- 56.Plow M, Finlayson M, Liu J, Motl RW, Bethoux F, Sattar A. Randomized Controlled Trial of a Telephone-Delivered Physical Activity and Fatigue Self-management Interventions in Adults With Multiple Sclerosis. Arch Phys Med Rehabil. 2019;100(11):2006–2014. [DOI] [PubMed] [Google Scholar]
- 57.Plow M, Motl RW, Finlayson M, Bethoux F. Intervention Mediators in a Randomized Controlled Trial to Increase Physical Activity and Fatigue Self-management Behaviors Among Adults With Multiple Sclerosis. Ann Behav Med. 2020;54(3):213–221. [DOI] [PubMed] [Google Scholar]
- 58.Rice IM, Rice LA, Motl RW. Promoting Physical Activity Through a Manual Wheelchair Propulsion Intervention in Persons With Multiple Sclerosis. Arch Phys Med Rehabil. 2015;96(10):1850–1858. [DOI] [PubMed] [Google Scholar]
- 59.Romberg A, Virtanen A, Ruutiainen J, et al. Effects of a 6-month exercise program on patients with multiple sclerosis: a randomized study. Neurology. 2004;63(11):2034–2038. [DOI] [PubMed] [Google Scholar]
- 60.Ryan JM, Fortune J, Stennett A, et al. Changing physical activity behaviour for people with multiple sclerosis: protocol of a randomised controlled feasibility trial (iStep-MS). BMJ Open. 2017;7(11):e018875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ryan JM, Fortune J, Stennett A, et al. Safety, feasibility, acceptability and effects of a behavior-change intervention to change physical activity behaviour among people with multiple sclerosis: Results from the iStep-MS randomised controlled trial. Mult Scler. 2019:1352458519886231. [DOI] [PubMed] [Google Scholar]
- 62.Sandroff BM, Balto JM, Klaren RE, Sommer SK, DeLuca J, Motl RW. Systematically developed pilot randomized controlled trial of exercise and cognition in persons with multiple sclerosis. Neurocase. 2016;22(5):443–450. [DOI] [PubMed] [Google Scholar]
- 63.Sandroff BM, Klaren RE, Pilutti LA, Dlugonski D, Benedict RH, Motl RW. Randomized controlled trial of physical activity, cognition, and walking in multiple sclerosis. J Neurol. 2014;261(2):363–372. [DOI] [PubMed] [Google Scholar]
- 64.Saxton JM, Carter A, Daley AJ, et al. Pragmatic exercise intervention for people with multiple sclerosis (ExIMS trial): study protocol for a randomised controlled trial. Contemp Clin Trials. 2013;34(2):205–211. [DOI] [PubMed] [Google Scholar]
- 65.Sebastião E, McAuley E, Shigematsu R, Adamson BC, Bollaert RE, Motl RW. Home-based, square-stepping exercise program among older adults with multiple sclerosis: results of a feasibility randomized controlled study. Contemp Clin Trials. 2018;73:136144. [DOI] [PubMed] [Google Scholar]
- 66.Sebastião E, McAuley E, Shigematsu R, Motl RW. Feasibility study design and methods for a home-based, square-stepping exercise program among older adults with multiple sclerosis: The SSE-MS project. Contemp Clin Trials Commun. 2017;7:200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith DC, Lanesskog D, Cleeland L, Motl R, Weikert M, Dlugonski D. Motivational interviewing may improve exercise experience for people with multiple sclerosis: A small randomized trial. Health Soc Work. 2012;37(2):99–109. [DOI] [PubMed] [Google Scholar]
- 68.Suh Y, Motl RW, Olsen C, Joshi I. Pilot Trial of a Social Cognitive Theory-Based Physical Activity Intervention Delivered by Nonsupervised Technology in Persons With Multiple Sclerosis. J Phys Act Health. 2015;12(7):924–930. [DOI] [PubMed] [Google Scholar]
- 69.Tallner A, Streber R, Hentschke C, et al. Internet-Supported Physical Exercise Training for Persons with Multiple Sclerosis-A Randomised, Controlled Study. Int J Mol Sci. 2016;17(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thomas S, Fazakarley L, Thomas PW, et al. Testing the feasibility and acceptability of using the Nintendo Wii in the home to increase activity levels, vitality and well-being in people with multiple sclerosis (Mii-vitaliSe): protocol for a pilot randomised controlled study. BMJ Open. 2014;4(5):e005172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thomas S, Fazakarley L, Thomas PW, et al. Mii-vitaliSe: a pilot randomised controlled trial of a home gaming system (Nintendo Wii) to increase activity levels, vitality and well-being in people with multiple sclerosis. BMJ Open. 2017;7(9):e016966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Turner AP, Hartoonian N, Sloan AP, et al. Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol. 2016;84(4):297–309. [DOI] [PubMed] [Google Scholar]
- 73.Wojcicki TR, Roberts SA, Learmonth YC, et al. Improving physical functional and quality of life in older adults with multiple sclerosis via a DVD-delivered exercise intervention: a study protocol. BMJ Open. 2014;4(12):e006250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dixon-Ibarra A, Nery-Hurwit M, Driver S, MacDonald M. Using health promotion guidelines for persons with disabilities to develop and evaluate a physical activity program for individuals with multiple sclerosis: A feasibility study. Eval Program Plann. 2017;61:150–159. [DOI] [PubMed] [Google Scholar]
- 75.Dlugonski D, Motl RW, McAuley E. Increasing physical activity in multiple sclerosis: replicating Internet intervention effects using objective and self-report outcomes. J Rehabil Res Dev. 2011;48(9):1129–1136. [DOI] [PubMed] [Google Scholar]
- 76.Feys P, Tytgat K, Gijbels D, De Groote L, Baert I, Van Asch P. Effects of an 1-day education program on physical functioning, activity and quality of life in community living persons with multiple sclerosis. NeuroRehabilitation. 2013;33(3):439–448. [DOI] [PubMed] [Google Scholar]
- 77.Hale LA, Mulligan HF, Treharne GJ, Smith CM. The feasibility and short-term benefits of Blue Prescription: a novel intervention to enable physical activity for people with multiple sclerosis. Disabil Rehabil. 2013;35(14):1213–1220. [DOI] [PubMed] [Google Scholar]
- 78.Kinnett-Hopkins D, Motl R. Results of a feasibility study of a patient informed, racially tailored home-based exercise program for black persons with multiple sclerosis. Contemp Clin Trials. 2018;75:1–8. [DOI] [PubMed] [Google Scholar]
- 79.Mandelbaum R, Triche EW, Fasoli SE, Lo AC. A Pilot Study: examining the effects and tolerability of structured dance intervention for individuals with multiple sclerosis. Disabil Rehabil. 2016;38(3):218–222. [DOI] [PubMed] [Google Scholar]
- 80.Motl RW, Dlugonski D. Increasing physical activity in multiple sclerosis using a behavioral intervention. Behav Med. 2011;37(4):125–131. [DOI] [PubMed] [Google Scholar]
- 81.Plow M, Finlayson M. Potential benefits of nintendo wii fit among people with multiple sclerosis: a longitudinal pilot study. Int J MS Care. 2011;13(1):21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Connell LE, Carey RN, de Bruin M, et al. Links Between Behavior Change Techniques and echanisms of Action: An Expert Consensus Study. Ann Behav Med. 2018;53(8):708–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sheeran P, Klein WM, Rothman AJ. Health Behavior Change: Moving from Observation to Intervention. Annu Rev Psychol. 2017;68:573–600. [DOI] [PubMed] [Google Scholar]
- 84.Aminian S, Motl RW, Rowley J, Manns PJ. Management of multiple sclerosis symptoms through reductions in sedentary behaviour: protocol for a feasibility study. BMJ Open. 2019;9(4):e026622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Griffith G, Klaren RE, Motl RW, Baynard T, Fernhall B. Experimental protocol of a randomized controlled clinical trial investigating exercise, subclinical atherosclerosis, and walking mobility in persons with multiple sclerosis. Contemp Clin Trials. 2015;41:280286. [DOI] [PubMed] [Google Scholar]
- 86.Motl RW, Sandroff BM, Wingo BC, et al. Phase-III, randomized controlled trial of the behavioral intervention for increasing physical activity in multiple sclerosis: Project BIPAMS. Contemp Clin Trials. 2018;71:154–161. [DOI] [PubMed] [Google Scholar]
- 87.Paul L, Renfrew L, Freeman J, et al. Web-based physiotherapy for people affected by multiple sclerosis: a single blind, randomized controlled feasibility study. Clin Rehabil. 2019;33(3):473–484. [DOI] [PubMed] [Google Scholar]
- 88.Rimmer JH, Thirumalai M, Young HJ, et al. Rationale and design of the tele-exercise and multiple sclerosis (TEAMS) study: A comparative effectiveness trial between a clinic- and home-based telerehabilitation intervention for adults with multiple sclerosis (MS) living in the deep south. Contemp Clin Trials. 2018;71:186–193. [DOI] [PubMed] [Google Scholar]
- 89.Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med.. 2005;30(1):65–73. [DOI] [PubMed] [Google Scholar]
- 90.Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A” SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Abraham C, Wood CE, Johnston M, et al. Reliability of Identification of Behavior Change Techniques in Intervention Descriptions. Ann Behav Med. 2015;49(6):885–900. [DOI] [PubMed] [Google Scholar]
- 92.Motl RW, Pekmezi D, Wingo BC. Promotion of physical activity and exercise in multiple sclerosis: Importance of behavioral science and theory. Mult Scler J Exp Transl Clin. 2018;4(3):2055217318786745. [DOI] [PMC free article] [PubMed] [Google Scholar]


