Abstract
Coronavirus disease (COVID-19) caused by SARS-CoV-2 was notified from Wuhan city, Hubei province, China in the mid of December 2019. The disease is showing dynamic change in the pattern of confirmed cases and death toll in these low and middle-income countries (LMICs). In this study, exponential growth (EG) method was used to calculate the real-time reproductive number (Rt) for initial and later stage of epidemic in South Asian Association for Regional Cooperation (SAARC) member countries (April 2020 – December 2020). Time dependent (TD) method was used to calculate the weekly real-time reproduction number (Rt). We also presented the observations on COVID-19 epidemiology in relation with the health expenditure, poverty, BCG vaccination, literacy population density and Rt for understanding the current scenario, trends, and expected outcome of the disease in SAARC countries. A significant positive correlation was noticed between COVID-19 deaths and health expenditure (% GDP) (r = 0.58, P < 0.05). The other factors such as population density/sq km, literacy %, adult population %, and poverty % were not significantly correlated with number of COVID-19 cases and deaths. Among SAARC countries, the highest Rt was observed in India (Rt = 2.10; 95% CI 2.04–2.17) followed by Bangladesh (Rt = 1.62; 95% CI 1.59–1.64) in initial state of epidemic. A continuous monitoring is necessitated in all countries looking at the medical facilities, available infrastructure and healthcare manpower, constraints which may appear with increased number of critically ill patients if the situation persists longer.
Keywords: COVID-19, SARS-CoV-2, SAARC countries, Reproduction number, Population density, Poverty
1. Introduction
Coronaviruses (CoVs) are a group of viruses that have the crown-like spikes on their outer surface (Latin: Corona = Crown). COVID-19 (coronavirus disease) caused by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), after its first appearance in Wuhan city of China during mid-December 2019, it became a public health emergency of international concern on January 31, 2020 and a pandemic on March 11, 2020, due to rapid spread and colossal loss [1], [2], [3], [4], [5], [6].
Though the COVID-19 disease started as an outbreak, it exploded as a global public health crisis and within a short span spread across the world, irrespective of nations economic status; be it a developed country or developing country; without any border limits causing a major significant havoc globally [7]. The swift transmission of the virus across the globe might be due to the availability of fast mode of transportation (air travel – flights) or it would have got wings to fly - reservoir hosts – bat [8].
At present, there are no standard/exact antiviral therapy/treatment available for COVID-19 [9]. Though, different types of medicines and drug combinations have exposed to hopeful outcomes against COVID-19, like the combination of azithromycin and chloroquine [10]. In addition, the malarial drug chloroquine and antiviral medicine remdesivir have gained great interest worldwide as possible medications for COVID-19 management [11]. COVID-19 is a directly transmissible infection via respiratory (aerosol), droplets, orofaecal and fomite routes [12]. In most developed countries, the BCG vaccination schedule was stopped because of low TB burden, however the SAARC countries practice mandatory BCG vaccination (TB facts, https://tbfacts.org/tb-statistics/). There are speculations on countries with mandatory BCG vaccination reported less COVID-19 mortality and morbidity [13]. Age is one of the significant factors for COVID-19 morbidity and mortality. The countries with higher median age encountered comparatively higher morbidity and morbidity [13]. Gender also plays a major role in COVID-19 mortality and morbidity. A report from China documented that compared to women, number of infected men was higher [14]. Case fatality rate (CFR) of COVID-19 was highest in persons aged >80 years and in patients with one or more co-morbid conditions such as neoplasm, diabetes mellitus, chronic respiratory disease, cardiovascular disease and hypertension. At the initial period, the epidemic size increases in a non-linear way with population density of susceptible individuals [15]. However, no significant correlation of population density was noticed with COVID-19 CFR, morbidity, or mortality [13]. The efficient control of COVID-19 spread could be acheived by strategic diagnostic testing, strict quarantine and contact tracing [16], [17], [18], [19], [20], [21].
The South Asian Association for Regional Cooperation (SAARC) is the regional intergovernmental organization and geopolitical union of states in South Asia [22], [23], [24], [25], [26], [27], [28], [29]. Its secretariat is based in Kathmandu, Nepal. Overall, as on year 2019, the SAARC countries comprise 3% of the world's area, 21% of the world's population and 4.21% (US$3.67 trillion) of the global economy (https://www.officeprimebelem.com.br/blog/3e4690-saarc-chairman). Compared to the developed and Western countries, the South East Asian countries reported lower COVID-19 cases and mortality in 2020 [21].
The primary objective of the study is to find out the convincing demographic factors associated with COVID-19 and estmimation of real-time reproduction number in SAARC countries.
2. Materials & methods
2.1. Data retrieval
The COVID-19 data (April 2020 – December 2020) for the SAARC countries from the available database [30] in public domains were analyzed in relation to population density, literacy (%), poverty (%), adult population (%), BCG vaccination, and health care expenditure (% GDP).
2.2. Calculation of real-time/effective reproduction number
The average number of new infections generated by one infected person during the infectious period is measured by the reproduction number, R0. The actual average number of secondary cases per infected case at time, t is the real-time reproduction number, Rt.
In our study, exponential growth (EG) [31,32] method was used to calculate the real-time reproductive number (Rt) of COVID-19 for initial and later stage of epidemic. The real-time reproduction number is computed as:
Where, M is the moment generating function of the (discretized) generation time (GT) or serial interval (SI) distribution and r denotes the fitted exponential growth rate. In order to calculate the Rt, we need to obtain the serial interval (SI), also known as generation interval, which is defined as the time interval between symptom onset in an index case and secondary case [33]. We used serial interval of 4.4 days with 3.2 standard deviation [34] for estimation of Rt. Time dependent (TD) method was used to calculate the weekly Rt. R Studio software (version 3.6.3) was used for data analysis with “R0” package [32] for calculating Rt with 95% confidence interval.
2.3. Correlation analysis
The data were checked for normality by Shapiro-Wilk test and Spearman correlation analysis was used to study the relationship between COVID-19 cases, deaths and other demographic factors. The correlation coefficients are measured from –1 to +1 and the sign of the Spearman correlation indicates the relationship between the analyzed variables.
3. Results
The reported confirmed cases of COVID-19, its country of origin and death in the respective SAARC countries is depicted in Table 1 . Among SAARC countries initial stage of epidemic, the highest Rt was observed in India (Rt =2.10; 95% CI 2.04 – 2.17) and Bangladesh (Rt=1.62; 95% CI 1.59–1.64). Later, the Rt was on decreasing trend among all the SAARC countries as compared with the initial stage (Table 1). India and Nepal have executed a nation-wide lockdown whereas Pakistan, Bangladesh, Afghanistan, and Maldives have implemented restricted lockdowns. The Island country, Sri Lanka has implemented quarantine and curfews. In India the first positive case of SARS-CoV-2 was reported on 30th January, 2020, and the nationwide lockdown was imposed on 25th March, 2020. The India data analysis depicted that Rt was higher before lockdown and decreased at the end of lockdowns. The weekly Rt of Afghanistan (Rt = 0.99; 95% CI 0.83–1.17), Bangladesh (Rt = 0.92; 95% CI 0.85–0.99), India (Rt = 0.94; 95% CI 0.92-0.95), and Nepal (Rt = 0.89; 95% CI 0.81–0.97) were <1 in the last week of 2020.
Table 1.
Different parameters of SAARC countries and COVID-19 cases and deaths as on December 23, 2020.
| Countries | Population (m) | Density / km2 | Literacy (%) | Adult (%) | Poverty (%) | Health expenditure (% of GDP) | BCG vaccine coverage (%) | Total COVID-19 cases | Total deaths | Cases per Million | Death per Million | Effective Reproduction number Rt (95% CI)# |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial stage of epidemic | Later stage of epidemic | ||||||||||||
| Afghanistan | 37.1 | 60 | 43.2 | 57.7 | 55 | 9.5 | 86 | 50433 | 2117 | 1296 | 54 | 1.31 (1.28 -1.36) | 0.90 (0.30 – 0.92) |
| Bangladesh | 165.4 | 1121 | 72.9 | 72.3 | 4 | 2.6 | 99 | 504868 | 7359 | 3066 | 45 | 1.62 (1.59 – 1.64) | 0.92 (0.83 – 0.97) |
| Bhutan | 0.734 | 20.9 | 64.9 | 73.7 | 8.2 | 3.71 | 99 | 519 | - | 672 | 15 | - | - |
| India | 1358.6 | 382 | 74.0 | 68.9 | 21.9 | 3.9 | 92 | 10123778 | 146756 | 7363 | 106 | 2.10 (2.04 – 2.17) | 0.88 (0.87 – 0.90) |
| Maldives | 0.339 | 1392 | 98.6 | 78.4 | 8.2 | 9.5 | 99 | 13537 | 48 | 25043 | 88 | 1.18 (1.14 – 1.22) | 0.83 (0.79 – 0.87) |
| Nepal | 29.02 | 180 | 67.9 | 65.1 | 25.2 | 6.1 | 96 | 255979 | 1803 | 8785 | 62 | 1.29 (1.17 – 1.43) | 0.86 (0.84 – 0.88) |
| Pakistan | 220.9 | 287 | 62.3 | 64.6 | 17.2 | 9.7 | 85 | 465070 | 9668 | 2105 | 44 | 1.30 (1.29 – 1.31) | 1.08 (1.06 – 1.10) |
| Sri Lanka | 21.69 | 325 | 91.7 | 74.8 | 4.1 | 3 | 99 | 38639 | 184 | 1804 | 9 | 1.15 (0.95 – 1.38) | 1.04 (1.03 – 1.06) |
Calculated for initial 60 and last 60 days effective reproduction number (Rt) estimation and correlation analysis of certain demographic factors of COVID-19 pandemic in South Asian Association for Regional Cooperation (SAARC) countries.
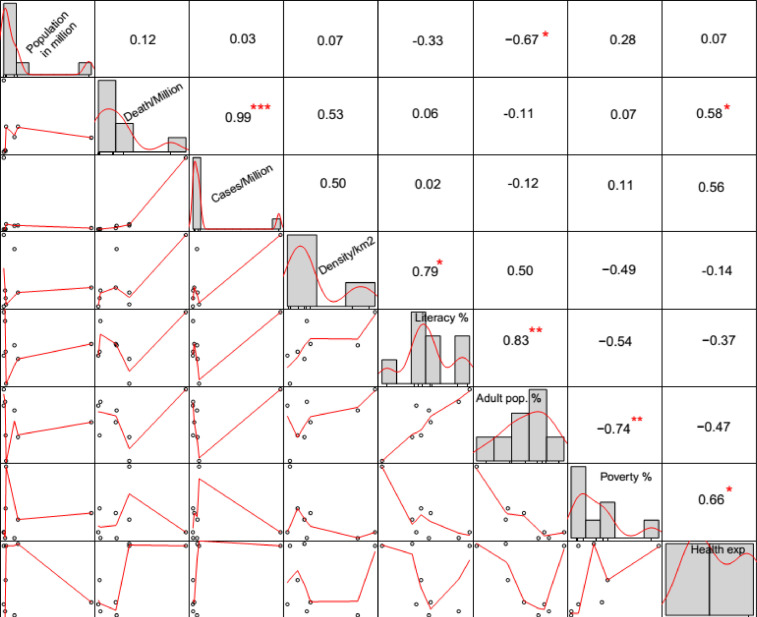
The country-wise analysis showed that the Maldives has higher number of COVID-19 cases and deaths/million populations than other countries. While, Bhutan experienced the lowest COVID-19 cases and deaths compared to other countries (Table 1). The absolute number of COVID-19 cases were the lowest in Bhutan (n = 867) and the highest was reported in India (n = 111,73,761). Among the countries which implemented the country-wide lockdown, Nepal reported a minimum number of cases and deaths per million populations [35]. The data showed that Sri Lanka managed the pandemic effectively without imposing lockdowns [36]. The factors showing the positive or negative correlation with COVID-19 cases and deaths are depicted in Fig. 1 . The COVID-19 cases and morality showed a highly significant (p < 0.001) positive correlation (r = 0.99). COVID-19 deaths and health expenditure (% GDP) depicted significant positive correlation (r = 0.58, p < 0.05). The other factors such as population density/sq km, literacy %, adult population %, and poverty % are not significantly correlated with COVID-19 cases and deaths (p > 0.05).
Fig. 1.
Correlation matrix of COVID-19 cases, deaths with population in millions, population density/km2, literacy %, poverty %, adult population %, and health expenditure (% GDP).
*** - p < 0.001, ** - p < 0.01, * - p < 0.05.
4. Discussion
The COVID‐19 outbreak has enforced a significant infliction worldwide, calling for measures at the regional, national, and global levels. South Asian nations are more susceptible to the pandemic because of their high populace, underdeveloped general and health-care infrastructure, and low surveillance framework. Each of the South Asian nations has taken careful steps by adopting social distancing i.e., physical distancing and travel limitations or restrictions both onward and return travel by air, water or land. India has played the lead role in setting the emergency fund by the SAARC countries for fighting against the COVID-19 pandemic public health crisis. The SAARC countries further supported the idea by establishing an Integrated Disease Surveillance Portal [37]. Furthermore, the Pakistan government has introduced smart lockdowns in hotspots of COVID-19.
The SAARC countries are geographically located near to China, and it was known as the origin of the disease of COVID-19 with a very high case fatality rate (CFR) of 5.33%. The CFR of SAARC countries were significantly less compared to China (5.33%) and United Kingdom (3.09 %). The CFR of SAARC nations are, 1.5 % (India), 2.1% (Pakistan), 0.35% (Maldives ), 0.70% (Nepal), 4.17% (Afghanistan ), 1.46% (Bangladesh), 0.46% (Srilanka) and, 0% (Bhutan). The COVID-19 has been similar in various countries and regions during the intial phase of the outbreak [38], [39], [40]. Many factors are affecting the estimate of the CFR, viz. medical services capacity factors, including the resources, facilities, healthcare workers, and readiness, additionally influence the disease outcomes and results.
Among the SAARC countries, India reported its first case on 30th January 2020 and since then, the disease has been steadily spreading across the country [41]. In Bangladesh the 1st case of COVID-19 was confirmed in 8th March,2020. Being densely populated country, Bangladesh had to face the collapse of healthcare system and daily social life [42]. Recently in Bangladesh, a cross-sectional epidemiological survey jointly conducted by Institute of Epidemiology, Disease Control and Research (IEDCR) and International Centre for Diarrhoeal Disease Research, Bangladesh (ICDRR, Bangladesh) revealed that around 45% people of Dhaka including about 74% slum people are carrying COVID-19 antibody that presumably indicate the start of herd immunity development in Dhaka city. In order to devise an appropriate preventive, control and therapeutic measures for COVID-19 in a particular country, there is a need to understand the clinical, epidemiological, virological and immunological course of the illness in that region along with the seasonality of the outbreak [43,44]. While on 26 February, 2020, Pakistan confirmed its first two cases of the coronavirus (a student in Karachi who had just returned from Iran and another person in the Islamabad Capital Territory) and since then, the disease has been steadily spreading across the country. Pakistan government has adopted smart lockdowns s in COVID-19 hotspots.
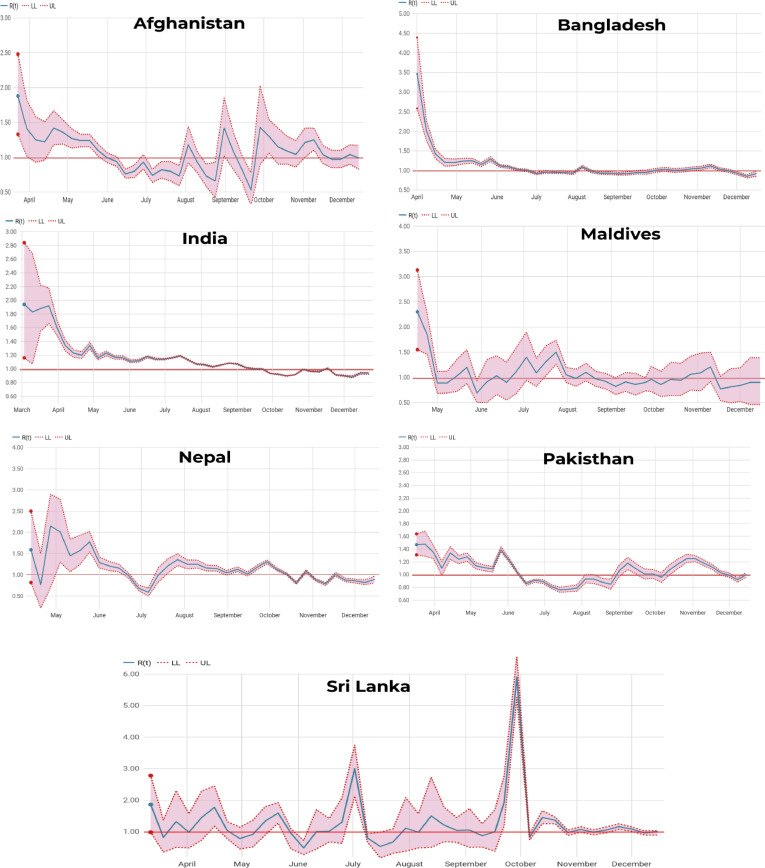
The real-time reproduction number (Rt) is dependent on several factors including (i). the contact rate of the infected population; (ii). probability of infection being transmitted during contact; (iii). the duration of infection [45]. The Rt varies with time and generally decreases with the implementation of control measures. R0 > 1 implies that the outbreak is self-sustaining unless effective control measures are implemented. R0 < 1 implies that the number of new cases will decrease over time and, eventually, the outbreak will cease. Population density is the one of the major factors involve in the transmission of infection [13]. During the initial stage of epidemic, India and Bangladesh observed high Rt, might be attributed to the population density. A report from India documented that the population density/Sq km didn't have significant correlation with COVID-19 CFR, morbidity, or mortality [12]. Initial studies reported a lower values of R0, however subsequent studies reported a increase in R0 [46]. Contrarily, the SAARC countries showed higher initial values of Rt, which later become low (Fig. 2 and Table 1). The serial interval (SI) is one of the methods to estimate the reproduction number (R0) which in turn is used to determine the amount of transmission required to be stopped to prevent an outbreak and control the distribution and shape of the epidemic curve. Shorter SI give lower R0 estimates and also very challengeable for contact tracing and to isolate the patients [47], https://www.sciencedirect.com/science/article/pii/S1201971220301193. Thus, R0 affected by the disease's incidence, prevalence, and epidemic growth, and the methods required by the health workers to prevent the disease [48]. Similarly, Hoque (2020) [49] reported the R0 using SIR model for the sub-continent where the value fluctuated for India and Bangladesh and tends to decrease after reaching a high epidemic peak, whereas it remained constant for Pakistan.
Fig. 2.
Time dependent (Weekly) reproduction number Rt for SAARC countries (April 2020 – December 2020).
All the SAARC countries implement mandatory BCG vaccination and this might be a reason for lower COVID-19 cases in these regions. The countries with mandatory BCG vaccination reported less COVID-19 mortality and morbidity [12]. In all the SAARC countries, extensive immunization coverage of Bacillus Calmette–Guérin (BCG) vaccine, Measles, Mumps and Rubella (MMR) vaccine has resulted in improved innate immune responses. For example, the better induction of interferon's (IFNs) and activated natural killer (NK) cells, thereby offering natural immunity against many of the infectious diseases of bacterial and viral origin among the young population. Possible cross-protective innate immunity offered by these vaccines have even prompted researchers around the world to consider as an appropriate option for repurposing of these commonly used vaccines for immuno-prophylaxis against COVID-19 [50,51] to avert current prevailing crisis due to emergency.
The developed and the developing nations are equally suffering with COVID-19 pandemic. The present study highlighted that the higher spending on health care was positively associated with COVID-19 cases. Similarly, Singh et al., (2020) [13] reported that higher literacy, well-established health care facilities and less poverty could not prevent the transmission and spread of COVID-19 in the advanced technological, highly modernized, economically developed nations. The countries such as New Zealand, Vietnam, and South Korea which followed efficient quarantine, diagnostic testing, and contact tracing effectively prevented the spread as compared to the countries which implemented the country-wide lockdown (Italy, India, and France). Among the SAARC nations, Sri Lanka efficiently controlled the SARS-CoV-2 spread than others without adopting lockdown polices. India showed a marked decrease in Rt at the end of lockdowns suggesting remarkable advantage of lockdowns even though the cases are increasing rapidly after lifting up of the lockdown.
Most parts of the world are experiencing the second wave of COVID-19 in 2021 due to various reasons. The main reason for the surge in COVID -19 cases are viral mutation and socio-political issues. Vaccination of majority of the population is the safe and dependable method to terminate the pandemic without substantial mortality [52,53].
5. Conclusion and future prospects
This study provides a picture of the challenges and responses to COVID-19 outbreak in SAARC countries. The SAARC region is a densely populated region of the world. It is highly susceptible to any large-scale outbreak of disease due to low health structure, and level of development. The SAARC countries followed different approaches to curtail the transmission and spread of the current COVID-19 pandemic. Bhutan, Afghanistan, Bangladesh, Maldives performed better with country-wide lockdown and Sri Lanka managed without any lockdown. The current data found that the estimated Rt for COVID-19 in SAARC countries is around 0.90, with a range of 0.83 – 1.08. However, the situation in these countries is quite changing, and the cases are increasing, which may introduce error in the estimation of Rt. However, the current picture shows the consistent decline in Rt value in SAARC region. Individually, Sri Lanka (Rt=1.04) and Pakistan (Rt=1.08) need more attention in the Rt value but had lower estimates as compared to the values recommended by WHO. Such attention is also applicable for Bangladesh. The overall decline in the Rt value suggested a lower death rate and an improvement in the control of the pandemic using lockdown, limited gathering and maintaining social distancing. However, the value of Rt is still >1, indicates that disease is not in the declining and/or die out phase. The SAARC countries with better health care system, less poverty, better BCG coverage and more young people equally suffered with COVID-19 pandemic compared to its counterparts. The strict quarantine, social distancing, personal hygiene, effective case and contact tracing are the prime factors for reducing the COVID-19 spread. It is also very important to equip all the available diagnostic facilities with adequate diagnostic kits and put in full function. In addition, it is crucial to aware the general public on COVID-19, its consequences and the possible control measures. Further, we recommend the Pakistan government policy of smart lockdown across those regions of different countries that are acting as hotspots of COVID-19. It could be an effective tool to control the COVID-19.
Finally, better understanding of the global epidemiology of COVID-19, continuous surveillance and larger population screening and testing with transparent and accurate reporting of patient characteristics are of utmost importance for appropriate preparedness and management in the coming days to avoid catastrophe and negative cascade effect. Vaccination and educating the public against COVID-19 preventive measure may help to put an end to COVID-19 pandemic.
CRediT authorship contribution statement
Yashpal Singh Malik: Conceptualization, Project administration. Vinodhkumar Obli Rajendran: Conceptualization, Data curation, Formal analysis, Writing – original draft, Project administration. Ikram MA: Writing – review & editing. Tripti Pande: Writing – review & editing. Karthikeyan Ravichandran: Writing – review & editing. Nagaraj Jaganathasamy: Data curation, Formal analysis. Balasubramanian Ganesh: Writing – review & editing. Aridoss Santhakumar: Writing – review & editing. Sina Salajegheh Tazerji: Writing – review & editing. Md. Tanvir Rahman: Writing – review & editing. Muhammad Safdar: Writing – review & editing. Zunjar B Dubal: Writing – review & editing. Kuldeep Dhama: Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that there are no conflicts of interest.
Acknowledgements
The authors are thankful to the Director and Joint Director (Research), ICAR-Indian Veterinary Research Institute, Izatnagar, India, and the first author (YSM) thanks the GADVASU authority for providing necessary facilities for the study.
References
- 1.Rabi F.A., et al. SARS-CoV-2 and coronavirus disease 2019: what we know so far. Pathogens. 2020;9(3):231. doi: 10.3390/pathogens9030231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohrabi C., et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu F., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu C., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahman Md, et al. Zoonotic diseases: etiology, impact, and control. Microorganisms. 2020;8(9):1405. doi: 10.3390/microorganisms8091405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO Coronavirus disease (COVID-19) dashboard. 2020. https://covid19.who.int/. (Accessed on 25th October 2020).
- 8.Zhou Peng, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kolifarhood Goodarz, et al. Epidemiological and clinical aspects of COVID-19; a narrative review. Arch. Acad. Emerg. Med. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- 10.Gautret P., et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Alanagreh L., Alzoughool F., Atoum M. The human coronavirus disease COVID-19: its origin, characteristics, and insights into potential drugs and its mechanisms. Pathogens. 2020;9(5):331. doi: 10.3390/pathogens9050331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siordia J.A., Jr Epidemiology and clinical features of COVID-19: a review of current literature. J Clin Virol. 2020 doi: 10.1016/j.jcv.2020.104357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh B.R., et al. Epidemiological determinants of acute respiratory syndrome coronavirus-2 disease pandemic and the role of the Bacille-Calmette-Guerin vaccine in reducing morbidity and mortality. J. Pure Appl. Microbiol. 2020;14 [Google Scholar]
- 14.Gebhard C., et al. Impact of sex and gender on COVID-19 outcomes in Europe. Biol. Sex Differ. 2020;11(1):1–13. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li R., Richmond P., Roehner B.M. Effect of population density on epidemics. Physica A. 2018;510:713–724. [Google Scholar]
- 16.Jason Beaubien, 2020. Some countries have brought new cases down to nearly zero. How did they do it? https://www.npr.org/sections/goatsandsoda/2020/05/23/861577367/messaging-from-leaders-who-have-tamed-their-countrys-coronavirus-outbreaks. Accessed on 24.06.2020.
- 17.Ravichandran K., et al. Global status of COVID-19 diagnosis: an overview. J Pure Appl Microbiol. 2020;14(suppl 1):879–892. [Google Scholar]
- 18.Ozaslan M., et al. Practical measures to prevent COVID-19: a mini-review. J Biol Sci. 2020;20:100–102. [Google Scholar]
- 19.Kumar V., et al. SARS-CoV-2 (COVID-19): zoonotic origin and susceptibility of domestic and wild animals. J Pure Appl Microbiol. 2020;14(suppl 1):741–747. [Google Scholar]
- 20.Malik, Y.S., et al. "Emerging Coronavirus Disease (COVID-19), a pandemic public health emergency with animal linkages: Current status update." (2020).
- 21.WHO: Coronavirus disease 2019 (COVID-19) Situation Report-153) https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-COVID-19-sitrep-153.pdf?sfvrsn=c896464d_2 (Accessed on 22nd June 2020). 2020.
- 22.Mousavi S.H., et al. Coronavirus disease 2019 (COVID-19) outbreak in Afghanistan; measures and challenges. Infect. Control Hosp. Epidemiol. 2020;1-4 doi: 10.1017/ice.2020.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rana D.R.S.J.B., Pokhrel N. Sequence mismatch in PCR probes may mask the COVID-19 detection in Nepal. Mol Cell Probes. 2020;53 doi: 10.1016/j.mcp.2020.101599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waris A., et al. COVID-19 outbreak: current scenario of Pakistan. New Microbes New Infect. 2020 doi: 10.1016/j.nmni.2020.100681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhutta, Z.A., et al. “Covid-19 risks and response in South Asia” (2020). doi: 10.1136/bmj.m1190. [DOI] [PubMed]
- 26.Jahan Y., Rahman S., Rahman A. COVID-19: a case report from Bangladesh perspective. Respir. Med Case Rep. 2020 doi: 10.1016/j.rmcr.2020.101068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Subbaraman N. Distancing is impossible': refugee camps race to avert coronavirus catastrophe. Nature. 2020:18. doi: 10.1038/d41586-020-01219-6. -18. [DOI] [PubMed] [Google Scholar]
- 28.LeVine S., et al. Case report: the first case of COVID-19 in Bhutan. Am J Trop Med Hyg. 2020;102(6):1205–1207. doi: 10.4269/ajtmh.20-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vieira C.M., et al. COVID-19: The forgotten priorities of the pandemic. Maturitas. 2020 doi: 10.1016/j.maturitas.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/s1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallinga J., Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proc. R. Soc. B. 2007;274(1609):599–604. doi: 10.1098/rspb.2006.3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Obadia T., Haneef R., Boëlle P.-Y. The R0 package: a toolbox to estimate reproduction numbers for epidemic outbreaks. BMC Med Inf Decis Making. 2012;12(1):1–9. doi: 10.1186/1472-6947-12-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallinga J., Teunis P. Different epidemic curves for severe acute respiratory syndrome reveal similar impacts of control measures. Am J Epidemiol. 2004;160(6):509–516. doi: 10.1093/aje/kwh255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.You C., et al. Estimation of the time-varying reproduction number of COVID-19 outbreak in China. Int J Hyg Environ Health. 2020 doi: 10.1101/2020.02.08.20021253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.K. Kapur, O.C. Kurian. COVID19: The New ‘South Asian Enigma’? https://www.orfonline.org/expert-speak/covid19-the-new-south-asian-enigma-73553/. (Accessed on 16th September 2020).
- 36.A. Mukhopadhyay. How Sri Lanka successfully curtailed the coronavirus pandemic. https://p.dw.com/p/3cPhz (Accessed on 18th May 2020).
- 37.Sharma G.D., et al. A qualitative enquiry into strategic and operational responses to Covid-19 challenges in South Asia. J. Public Aff. 2020;20(4):e2195. doi: 10.1002/pa.2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang C., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet North Am Ed. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen N., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet North Am Ed. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mi Y.-n., et al. Estimating the instant case fatality rate of COVID-19 in China. Int J Infect Dis. 2020;97:1–6. doi: 10.1016/j.ijid.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.D. Basu and P. Srivastava. COVID-19 Data in South Asia Shows India is doing worse than its neighbours. https://thewire.in/health/covid-19-data-in-south-asia-shows-india-is-doing-worse-than-its-neighbours. (Accessed on 18th March 2020).
- 42.Rahman T., et al. Is the COVID-19 pandemic masking dengue epidemic in Bangladesh? J Adv Vet Anim Res. 2020;7(2):218–219. doi: 10.5455/javar.2020.g412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Islam M.S., et al. Coronavirus Disease 2019 (COVID-19) pandemic, lessons to be learned! J Adv Vet Anim Res. 2020;7(2):260–280. doi: 10.5455/javar.2020.g418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Junejo Y., et al. Novel SARS-CoV-2/COVID-19: origin, pathogenesis, genes and genetic variations, immune responses and phylogenetic analysis. Gene Rep. 2020;20 doi: 10.1016/j.genrep.2020.100752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rothman K.J., Lash T., Greenland S. 3rd ed. Lippincott Williams & Wilkins; 2013. Modern Epidemiology. [Google Scholar]
- 46.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020 doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nishiura H., Linton N.M., Akhmetzhanov A.R. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tindale L., et al. Transmission interval estimates suggest pre-symptomatic spread of COVID-19. MedRxiv. 2020 [Google Scholar]
- 49.Hoque M.E. Estimation of the number of affected people due to the Covid-19 pandemic using susceptible, infected and recover model. Int. J. Mod. Phys. C. 2020;31(08) [Google Scholar]
- 50.O'Neill L.A.J., Netea M.G. BCG-induced trained immunity: can it offer protection against COVID-19? Nat Rev Immunol. 2020;20(6):335–337. doi: 10.1038/s41577-020-0337-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Anbarasu A., Ramaiah S., Livingstone P. Vaccine repurposing approach for preventing COVID 19: can MMR vaccines reduce morbidity and mortality? Hum Vaccin Immunother. 2020:1–2. doi: 10.1080/21645515.2020.1773141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO Coronavirus Disease (COVID-19) Dashboard. 2021. https://covid19.who.int (Accessed on 23rd June 2021).
- 53.Asrani P., Suji Eapen M., Hassan M.I., Sohal S.S. Implications of the second wave of COVID-19 in India. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(21)00312-X. [DOI] [PMC free article] [PubMed] [Google Scholar]